Article type
- Page Path
- HOME > BROWSE ARTICLES > Article type
Review Articles
- Diabetes, Obesity and Metabolism
- Overcoming Therapeutic Inertia as the Achilles’ Heel for Improving Suboptimal Diabetes Care: An Integrative Review
- Boon-How Chew, Barakatun-Nisak Mohd-Yusof, Pauline Siew Mei Lai, Kamlesh Khunti
- Endocrinol Metab. 2023;38(1):34-42. Published online February 16, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1649
- 2,947 View
- 219 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
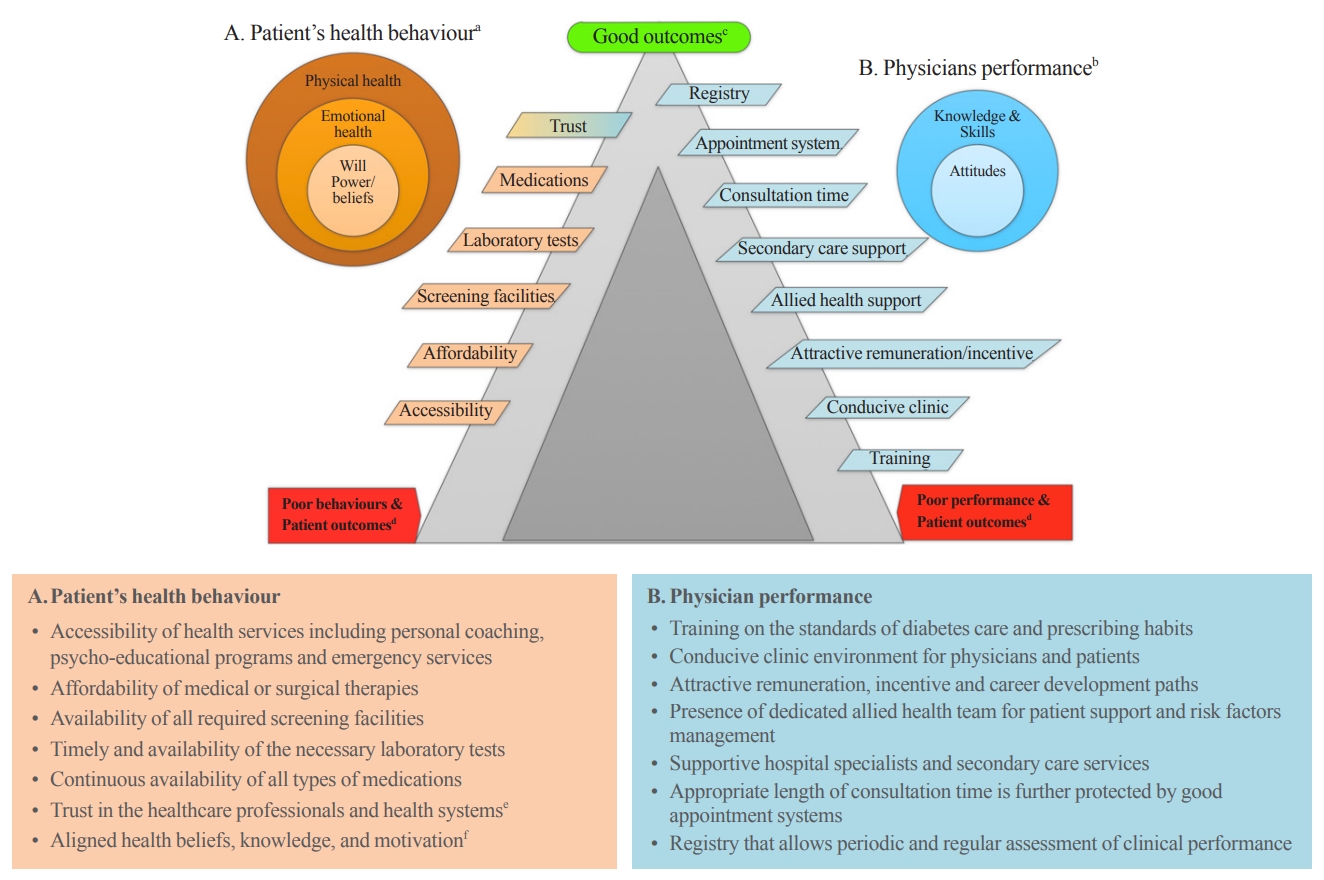
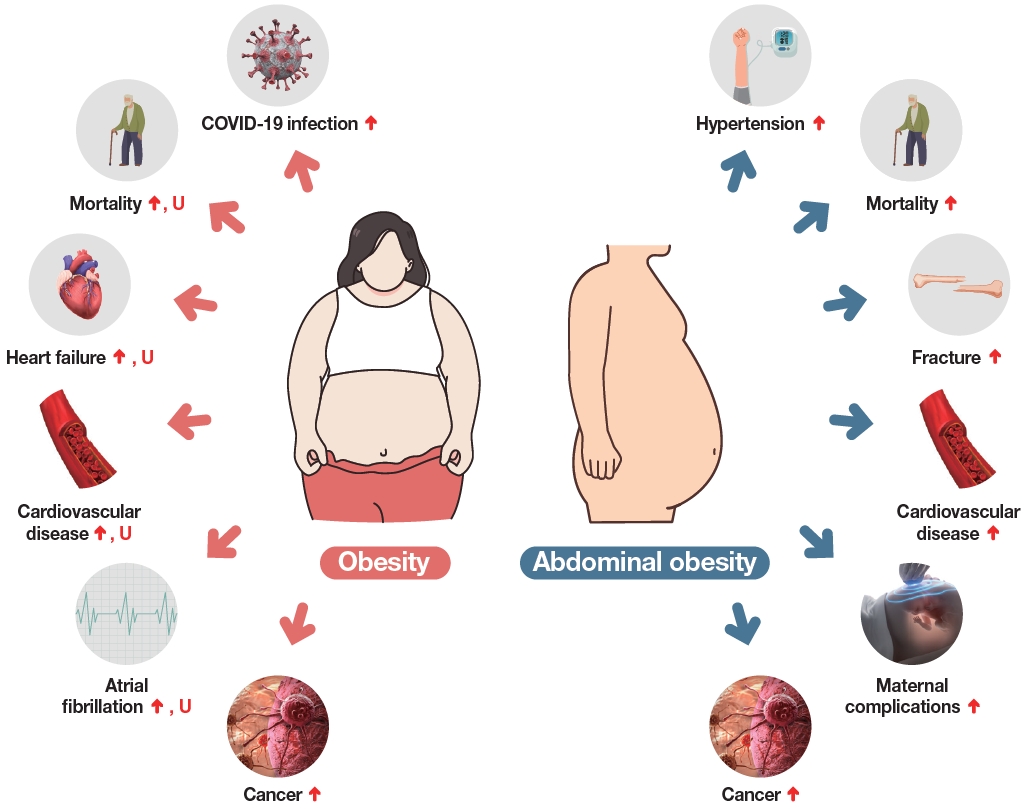
ePub - The ultimate purpose of diabetes care is achieving the outcomes that patients regard as important throughout the life course. Despite advances in pharmaceuticals, nutraceuticals, psychoeducational programs, information technologies, and digital health, the levels of treatment target achievement in people with diabetes mellitus (DM) have remained suboptimal. This clinical care of people with DM is highly challenging, complex, costly, and confounded for patients, physicians, and healthcare systems. One key underlying problem is clinical inertia in general and therapeutic inertia (TI) in particular. TI refers to healthcare providers’ failure to modify therapy appropriately when treatment goals are not met. TI therefore relates to the prescribing decisions made by healthcare professionals, such as doctors, nurses, and pharmacists. The known causes of TI include factors at the level of the physician (50%), patient (30%), and health system (20%). Although TI is often multifactorial, the literature suggests that 28% of strategies are targeted at multiple levels of causes, 38% at the patient level, 26% at the healthcare professional level, and only 8% at the healthcare system level. The most effective interventions against TI are shorter intervals until revisit appointments and empowering nurses, diabetes educators, and pharmacists to review treatments and modify prescriptions.
-
Citations
Citations to this article as recorded by- Obesity management from the perspectives of people living with obesity in Canada: A mixed‐methods study
David C. W. Lau, Ian Patton, Reena Lavji, Adel Belloum, Ginnie Ng, Renuca Modi
Diabetes, Obesity and Metabolism.2024; 26(4): 1529. CrossRef - Bridging the gap in cardiovascular care in diabetic patients: are cardioprotective antihyperglycemic agents underutilized?
André J Scheen
Expert Review of Clinical Pharmacology.2023; 16(11): 1053. CrossRef
- Obesity management from the perspectives of people living with obesity in Canada: A mixed‐methods study

- Diabetes, Obesity and Metabolism
- Glucagon-Like Peptide 1 Therapy: From Discovery to Type 2 Diabetes and Beyond
- Adie Viljoen, Stephen C. Bain
- Endocrinol Metab. 2023;38(1):25-33. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1642
- 2,777 View
- 306 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The therapeutic benefits of the incretin hormone, glucagon-like peptide 1 (GLP1), for people with type 2 diabetes and/or obesity, are now firmly established. The evidence-base arising from head-to-head comparative effectiveness studies in people with type 2 diabetes, as well as the recommendations by professional guidelines suggest that GLP1 receptor agonists should replace more traditional treatment options such as sulfonylureas and dipeptidyl-peptidase 4 (DPP4) inhibitors. Furthermore, their benefits in reducing cardiovascular events in people with type 2 diabetes beyond improvements in glycaemic control has led to numerous clinical trials seeking to translate this benefit beyond type 2 diabetes. Following early trial results their therapeutic benefit is currently being tested in other conditions including fatty liver disease, kidney disease, and Alzheimer’s disease.
-
Citations
Citations to this article as recorded by- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update
Agnieszka Jakubowska, Carel W. le Roux, Adie Viljoen
Endocrinology and Metabolism.2024; 39(1): 12. CrossRef - Glucagon-like peptide 1 receptor agonists: cardiovascular benefits and mechanisms of action
John R. Ussher, Daniel J. Drucker
Nature Reviews Cardiology.2023; 20(7): 463. CrossRef - A new class of glucose-lowering therapy for type 2 diabetes: the latest development in the incretin arena
Stephen C Bain, Thinzar Min
The Lancet.2023; 402(10401): 504. CrossRef - Flattening the biological age curve by improving metabolic health: to taurine or not to taurine, that’ s the question
Kwok M. Ho, Anna Lee, William Wu, Matthew T.V. Chan, Lowell Ling, Jeffrey Lipman, Jason Roberts, Edward Litton, Gavin M. Joynt, Martin Wong
Journal of Geriatric Cardiology.2023; 20(11): 813. CrossRef
- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
- Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
- Endocrinol Metab. 2023;38(1):10-24. Published online February 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.102
- 3,739 View
- 262 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - The Korean National Health Information Database (NHID) contains big data combining information obtained from the National Health Insurance Service and health examinations. Data are provided in the form of a cohort, and the NHID can be used to conduct longitudinal studies and research on rare diseases. Moreover, data on the cause and date of death are provided by Statistics Korea. Research and publications based on the NHID have increased explosively in the field of endocrine disorders. However, because the data were not collected for research purposes, studies using the NHID have limitations, particularly the need for the operational definition of diseases. In this review, we describe the characteristics of the Korean NHID, operational definitions of endocrine diseases used for research, and an overview of recent studies in endocrinology using the Korean NHID.
-
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Diabetes severity and the risk of depression: A nationwide population-based study
Yunjung Cho, Bongsung Kim, Hyuk-Sang Kwon, Kyungdo Han, Mee Kyoung Kim
Journal of Affective Disorders.2024; 351: 694. CrossRef - Information Bias Might Exaggerate Lung Cancer Risk of Patients With Rheumatoid Arthritis
Nobuyuki Horita, Kaoru Takase-Minegishi
Journal of Thoracic Oncology.2024; 19(2): 348. CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
Endocrinology and Metabolism.2023; 38(6): 690. CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study

Namgok Lecture 2022
- Diabetes, Obesity and Metabolism
- Incretin and Pancreatic β-Cell Function in Patients with Type 2 Diabetes
- Chang Ho Ahn, Tae Jung Oh, Se Hee Min, Young Min Cho
- Endocrinol Metab. 2023;38(1):1-9. Published online February 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.103
- 3,330 View
- 362 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
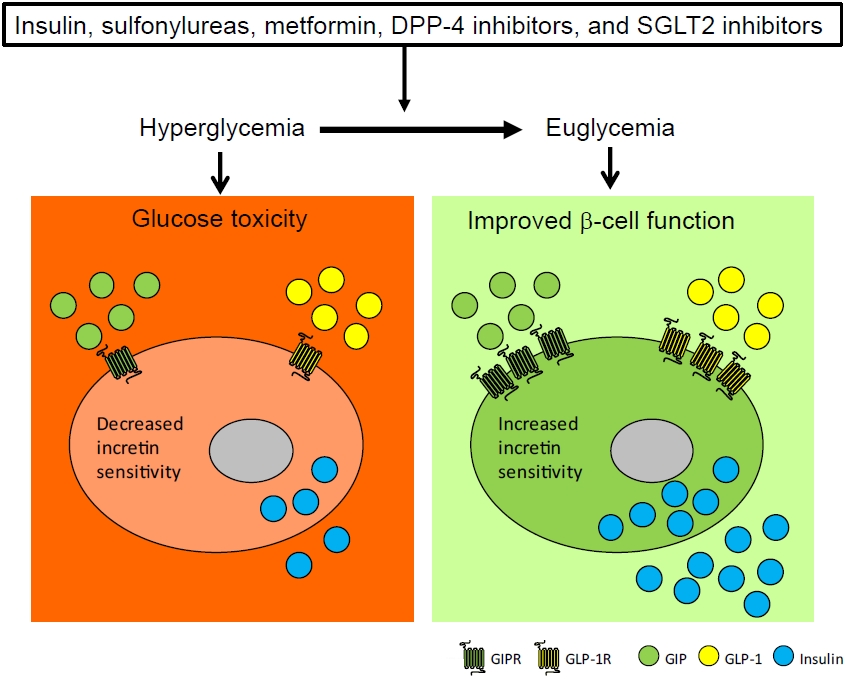
ePub - To maintain normal glucose homeostasis after a meal, it is essential to secrete an adequate amount of insulin from pancreatic β-cells. However, if pancreatic β-cells solely depended on the blood glucose level for insulin secretion, a surge in blood glucose levels would be inevitable after the ingestion of a large amount of carbohydrates. To avoid a deluge of glucose in the bloodstream after a large carbohydrate- rich meal, enteroendocrine cells detect the amount of nutrient absorption from the gut lumen and secrete incretin hormones at scale. Since insulin secretion in response to incretin hormones occurs only in a hyperglycemic milieu, pancreatic β-cells can secrete a “Goldilocks” amount of insulin (i.e., not too much and not too little) to keep the blood glucose level in the normal range. In this regard, pancreatic β-cell sensitivity to glucose and incretin hormones is crucial for maintaining normal glucose homeostasis. In this Namgok lecture 2022, we review the effects of current anti-diabetic medications on pancreatic β-cell sensitivity to glucose and incretin hormones.
-
Citations
Citations to this article as recorded by- Initial Combination Therapy in Type 2 Diabetes
Ji Yoon Kim, Nam Hoon Kim
Endocrinology and Metabolism.2024; 39(1): 23. CrossRef
- Initial Combination Therapy in Type 2 Diabetes

Response
- Adrenal Gland
- Contralateral Suppression at Adrenal Venous Sampling Is Associated with Renal Impairment Following Adrenalectomy for Unilateral Primary Aldosteronism (Endocrinol Metab 2021;36:875-84, Ye Seul Yang et al.)
- Ye Seul Yang, Sang Wan Kim
- Endocrinol Metab. 2022;37(6):953-954. Published online December 12, 2022
- DOI: https://doi.org/10.3803/EnM.2022.603
- [Original]
- 1,365 View
- 151 Download

Letter
- Adrenal Gland
- Contralateral Suppression at Adrenal Venous Sampling Is Associated with Renal Impairment Following Adrenalectomy for Unilateral Primary Aldosteronism (Endocrinol Metab 2021;36:875-84, Ye Seul Yang et al.)
- Zhimin Tan, Qiyu He, Liang Zhou
- Endocrinol Metab. 2022;37(6):951-952. Published online November 25, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1606
- 1,284 View
- 144 Download

Response
- Thyroid
- Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
- Hyunju Park, Jae Hoon Chung
- Endocrinol Metab. 2022;37(6):949-950. Published online November 10, 2022
- DOI: https://doi.org/10.3803/EnM.2022.601
- [Original]
- 1,372 View
- 152 Download

Letter
- Thyroid
- Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
- Sue Youn Kim, Chan Kwon Jung
- Endocrinol Metab. 2022;37(6):947-948. Published online November 10, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1596
- 1,676 View
- 158 Download
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules
Young Joo Park, Eun Kyung Lee, Young Shin Song, Soo Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung
International Journal of Thyroidology.2023; 16(1): 1. CrossRef
- 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules

Response
- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
- Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
- Endocrinol Metab. 2022;37(6):945-946. Published online December 2, 2022
- DOI: https://doi.org/10.3803/EnM.2022.602
- [Original]
- 1,732 View
- 165 Download

Letter
- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
- May Thu Hla Aye, Sajid Adhi Raja, Vui Heng Chong
- Endocrinol Metab. 2022;37(6):943-944. Published online November 23, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1601

- 1,744 View
- 165 Download

Brief Report
- Adrenal Gland
- Aldosterone Immunoassay-Specific Cutoff Value for Seated Saline Suppression Test for Diagnosing Primary Aldosteronism
- So Yoon Kwon, Jiyun Park, So Hee Park, So Hyun Cho, You-Bin Lee, Soo-Youn Lee, Jae Hyeon Kim
- Endocrinol Metab. 2022;37(6):938-942. Published online December 6, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1535
- 1,767 View
- 194 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - A seated saline loading test (SLT) using liquid chromatography-tandem mass spectrometry (LC-MS/MS) is one of the most accepted confirmatory tests of primary aldosteronism. However, LC-MS/MS is time-consuming and is not widely available in diagnostic laboratories compared to immunoassay. With immunoassay, it is unknown whether SLT in the seated position is more accurate than that of the supine position, and a cutoff value of post-seated SLT plasma aldosterone concentration (PAC) must be established in the Korean population. Ninety-eight patients underwent SLT in both positions, and post-SLT PAC was measured by LC-MS/MS and radioimmunoassay. We confirmed primary aldosteronism if post-seated SLT PAC by LC-MS/MS exceeded 5.8 ng/dL. The area under the receiver operating characteristic curve was greater for seated than supine SLT (0.928 vs. 0.834, P=0.003). The optimal cutoff value of post-seated SLT by radioimmunoassay was 6.6 ng/dL (sensitivity 83.3%, specificity 92.2%).
-
Citations
Citations to this article as recorded by- Investigating the cut-off values of captopril challenge test for primary aldosteronism using the novel chemiluminescent enzyme immunoassay method: a retrospective cohort study
Yuta Tezuka, Kei Omata, Yoshikiyo Ono, Kengo Kambara, Hiroki Kamada, Sota Oguro, Yuto Yamazaki, Celso E. Gomez-Sanchez, Akihiro Ito, Hironobu Sasano, Kei Takase, Tetsuhiro Tanaka, Hideki Katagiri, Fumitoshi Satoh
Hypertension Research.2024;[Epub] CrossRef
- Investigating the cut-off values of captopril challenge test for primary aldosteronism using the novel chemiluminescent enzyme immunoassay method: a retrospective cohort study

Original Articles
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Metformin and Cervical Cancer Risk in Patients with Newly Diagnosed Type 2 Diabetes: A Population-Based Study in Korea
- Hyun Min Kim, Min Jin Kang, Sun Ok Song
- Endocrinol Metab. 2022;37(6):929-937. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1613
- Correction in: Endocrinol Metab 2023;38(1):174
- 2,447 View
- 218 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Cervical cancer is a prevalent malignancy that is a major health problem for women worldwide. The cancer-preventive properties of metformin are well-known, but insufficient data have been reported regarding its relationship to cervical cancer. Therefore, in a nationwide population-based study, we investigated the association between metformin use and cervical cancer incidence in patients with newly diagnosed type 2 diabetes.
Methods
This retrospective cohort study used the Korean National Health Insurance claims database. Individuals newly diagnosed with type 2 diabetes between January 2005 and December 2009 were included. The occurrence of cervical cancer was explored by matching for age, economic status, region of residence, and use of anti-diabetic medication.
Results
In total, 66,013 metformin users and 64,756 non-users were analyzed. Cervical cancer occurred in 219 metformin users (0.33%) and 274 metformin non-users (0.42%) (hazard ratio [HR], 0.783; 95% confidence interval [CI], 0.655 to 0.036; P=0.007). Moreover, cervical cancer risk was considerably reduced in those treated with a high dose (>1,200,000 mg) or for an extended period (≥2,000 days) compared to non-users (HR, 0.151; 95% CI, 0.093 to 0.243; P<0.001; and HR, 0.141; 95% CI, 0.077 to 0.258; P<0.001). The incidence was also significantly lower in metformin users among those over 50 years old (HR, 0.791; 95% CI, 0.650 to 0.961; P<0.001).
Conclusion
Metformin use in patients with newly diagnosed diabetes was associated with a lower risk of cervical cancer in Korea. Furthermore, a significant association was found between the use of metformin and cervical cancer in a dose- and duration-dependent manner and among those over 50 years old. -
Citations
Citations to this article as recorded by- Repurposing of Chronically Used Drugs in Cancer Therapy: A Chance to Grasp
Mohamad Ali Hijazi, André Gessner, Nahed El-Najjar
Cancers.2023; 15(12): 3199. CrossRef - Network-based drug repurposing for HPV-associated cervical cancer
Faheem Ahmed, Young Jin Yang, Anupama Samantasinghar, Young Woo Kim, Jeong Beom Ko, Kyung Hyun Choi
Computational and Structural Biotechnology Journal.2023; 21: 5186. CrossRef - The Use of Metformin and Postoperative Insulin Pump Were Predictive Factors for Outcomes of Diabetic Colorectal Cancer Patients after Surgery
Xu-Rui Liu, Fei Liu, Zi-Wei Li, Quan Lv, Xin-Peng Shu, Lian-Shuo Li, Yue Tong, Wei Zhang, Dong Peng
Nutrition and Cancer.2023; 75(10): 1926. CrossRef
- Repurposing of Chronically Used Drugs in Cancer Therapy: A Chance to Grasp

- Diabetes, Obesity and Metabolism
- Gemigliptin Alleviates Succinate-Induced Hepatic Stellate Cell Activation by Ameliorating Mitochondrial Dysfunction
- Giang Nguyen, So Young Park, Dinh Vinh Do, Dae-Hee Choi, Eun-Hee Cho
- Endocrinol Metab. 2022;37(6):918-928. Published online November 15, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1530
- 3,462 View
- 230 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Dipeptidyl peptidase-4 inhibitors (DPP-4Is) are used clinically as oral antidiabetic agents. Although DPP-4Is are known to ameliorate liver fibrosis, the protective mechanism of DPP-4Is in liver fibrosis remains obscure. In this study, gemigliptin was used to investigate the potential of DPP-4Is to alleviate the progression of liver fibrosis.
Methods
To clarify the effects and mechanisms of gemigliptin, we conducted various experiments in LX-2 cells (immortalized human hepatic stellate cells [HSCs], the principal effectors of hepatic fibrogenesis), which were activated by succinate and exhibited elevated expression of α-smooth muscle actin, collagen type 1, and pro-inflammatory cytokines and increased cell proliferation. In vivo, we examined the effects and mechanisms of gemigliptin on a high-fat, high-cholesterol–induced mouse model of nonalcoholic steatohepatitis (NASH).
Results
Gemigliptin decreased the expression of fibrogenesis markers and reduced the abnormal proliferation of HSCs. In addition, gemigliptin reduced the succinate-induced production of mitochondrial reactive oxygen species (ROS), intracellular ROS, and mitochondrial fission in HSCs. Furthermore, in the mouse model of NASH-induced liver fibrosis, gemigliptin alleviated both liver fibrosis and mitochondrial dysfunction.
Conclusion
Gemigliptin protected against HSC activation and liver fibrosis by alleviating mitochondrial dysfunction and ROS production, indicating its potential as a strategy for preventing the development of liver disease. -
Citations
Citations to this article as recorded by- Improvement effect of gemigliptin on salivary gland dysfunction in exogenous methylglyoxal-injected rats
Woo Kwon Jung, Su-Bin Park, Hwa Young Yu, Junghyun Kim
Heliyon.2024; 10(8): e29362. CrossRef - Gemigliptin, a DPP4 inhibitor, ameliorates nonalcoholic steatohepatitis through AMP-activated protein kinase-independent and ULK1-mediated autophagy
Youngmi Song, Hyekyung Yang, Juhee Kim, Yoonjin Lee, Sung-Ho Kim, In-Gu Do, Cheol-Young Park
Molecular Metabolism.2023; 78: 101806. CrossRef - DPP-4 Inhibitor in Type 2 Diabetes Mellitus Patient with Non-Alcoholic Fatty Liver Disease: Achieving Two Goals at Once?
Ji Cheol Bae
Endocrinology and Metabolism.2022; 37(6): 858. CrossRef
- Improvement effect of gemigliptin on salivary gland dysfunction in exogenous methylglyoxal-injected rats

- Diabetes, Obesity and Metabolism
- Inhibition of miR-146a-5p and miR-8114 in Insulin-Secreting Cells Contributes to the Protection of Melatonin against Stearic Acid-Induced Cellular Senescence by Targeting Mafa
- Shenghan Su, Qingrui Zhao, Lingfeng Dan, Yuqing Lin, Xuebei Li, Yunjin Zhang, Chunxiao Yang, Yimeng Dong, Xiaohan Li, Romano Regazzi, Changhao Sun, Xia Chu, Huimin Lu
- Endocrinol Metab. 2022;37(6):901-917. Published online December 7, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1565
- 2,410 View
- 220 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Chronic exposure to elevated levels of saturated fatty acids results in pancreatic β-cell senescence. However, targets and effective agents for preventing stearic acid-induced β-cell senescence are still lacking. Although melatonin administration can protect β-cells against lipotoxicity through anti-senescence processes, the precise underlying mechanisms still need to be explored. Therefore, we investigated the anti-senescence effect of melatonin on stearic acid-treated mouse β-cells and elucidated the possible role of microRNAs in this process.
Methods
β-Cell senescence was identified by measuring the expression of senescence-related genes and senescence-associated β-galactosidase staining. Gain- and loss-of-function approaches were used to investigate the involvement of microRNAs in stearic acid-evoked β-cell senescence and dysfunction. Bioinformatics analyses and luciferase reporter activity assays were applied to predict the direct targets of microRNAs.
Results
Long-term exposure to a high concentration of stearic acid-induced senescence and upregulated miR-146a-5p and miR- 8114 expression in both mouse islets and β-TC6 cell lines. Melatonin effectively suppressed this process and reduced the levels of these two miRNAs. A remarkable reversibility of stearic acid-induced β-cell senescence and dysfunction was observed after silencing miR-146a-5p and miR-8114. Moreover, V-maf musculoaponeurotic fibrosarcoma oncogene homolog A (Mafa) was verified as a direct target of miR-146a-5p and miR-8114. Melatonin also significantly ameliorated senescence and dysfunction in miR-146a-5pand miR-8114-transfected β-cells.
Conclusion
These data demonstrate that melatonin protects against stearic acid-induced β-cell senescence by inhibiting miR-146a- 5p and miR-8114 and upregulating Mafa expression. This not only provides novel targets for preventing stearic acid-induced β-cell dysfunction, but also points to melatonin as a promising drug to combat type 2 diabetes progression. -
Citations
Citations to this article as recorded by- Genome-wide analysis in PC6 electroacupuncture to ameliorate carfilzomib-induced cardiotoxicity in mice
Yuxuan Chen, Rou Peng, Yi Qian, Yizhou Lu, Liyao Chen, Meiling Yu, Minjiao Jiang, Wei Wu, Shengfeng Lu
Gene.2024; 897: 148090. CrossRef - MiR-126 and miR-146a as Melatonin-Responsive Biomarkers for Neonatal Brain Ischemia
Maria Cristina Albertini, Tania Vanzolini, Serafina Perrone, Michael D. Weiss, Giuseppe Buonocore, Valentina Dell’Orto, Walter Balduini, Silvia Carloni
Journal of Molecular Neuroscience.2023; 73(9-10): 763. CrossRef
- Genome-wide analysis in PC6 electroacupuncture to ameliorate carfilzomib-induced cardiotoxicity in mice

- Thyroid
- Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
- Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
- Endocrinol Metab. 2022;37(6):891-900. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1590
- 2,504 View
- 255 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
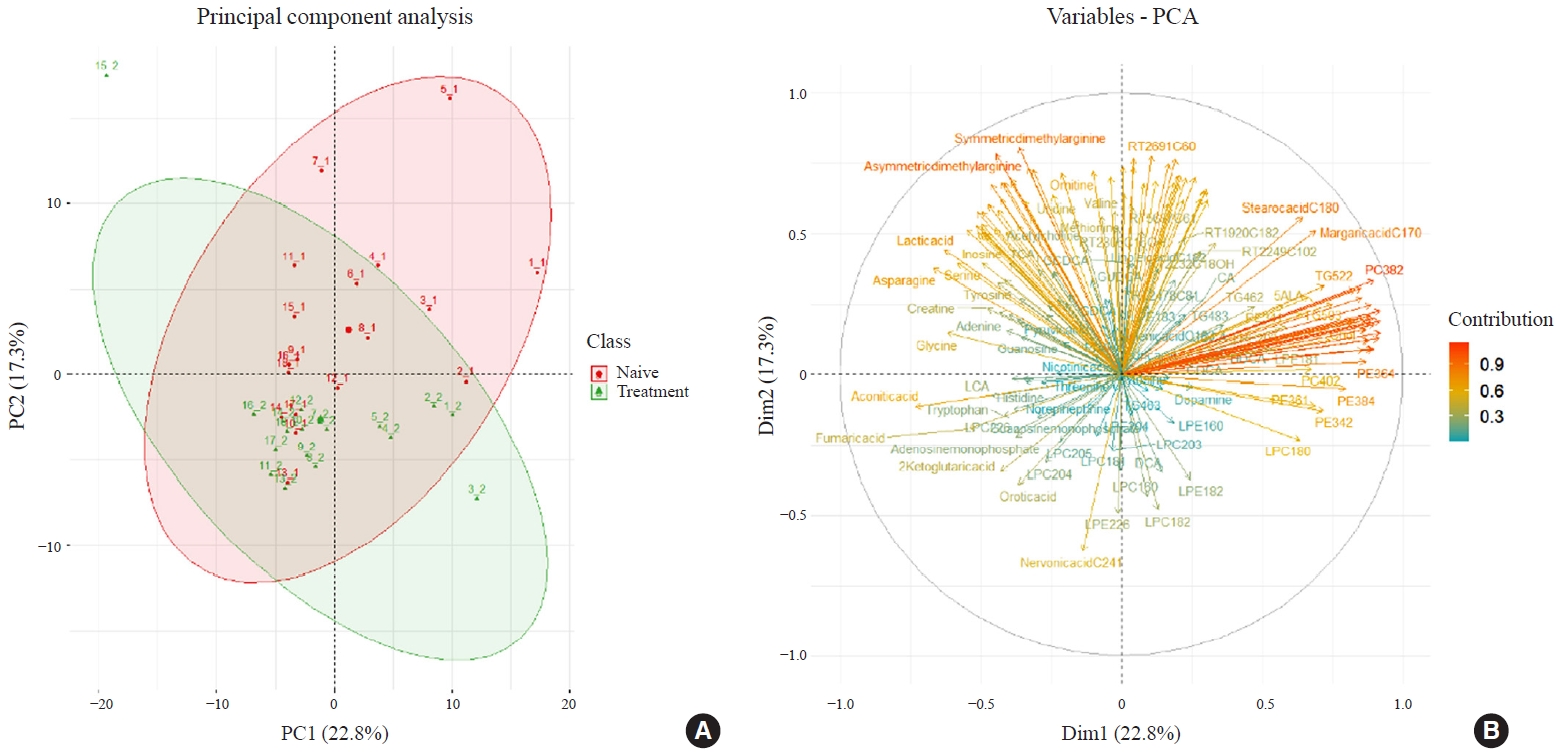
An excess of thyroid hormones in Graves’ disease (GD) has profound effects on systemic energy metabolism that are currently partially understood. In this study, we aimed to provide a comprehensive understanding of the metabolite changes that occur when patients with GD transition from hyperthyroidism to euthyroidism with methimazole treatment.
Methods
Eighteen patients (mean age, 38.6±14.7 years; 66.7% female) with newly diagnosed or relapsed GD attending the endocrinology outpatient clinics in a single institution were recruited between January 2019 and July 2020. All subjects were treated with methimazole to achieve euthyroidism. We explored metabolomics by performing liquid chromatography-mass spectrometry analysis of plasma samples of these patients and then performed multivariate statistical analysis of the metabolomics data.
Results
Two hundred metabolites were measured before and after 12 weeks of methimazole treatment in patients with GD. The levels of 61 metabolites, including palmitic acid (C16:0) and oleic acid (C18:1), were elevated in methimazole-naïve patients with GD, and these levels were decreased by methimazole treatment. The levels of another 15 metabolites, including glycine and creatinine, were increased after recovery of euthyroidism upon methimazole treatment in patients with GD. Pathway analysis of metabolomics data showed that hyperthyroidism was closely related to aminoacyl-transfer ribonucleic acid biosynthesis and branched-chain amino acid biosynthesis pathways.
Conclusion
In this study, significant variations of plasma metabolomic patterns that occur during the transition from hyperthyroidism to euthyroidism were detected in patients with GD via untargeted metabolomics analysis. -
Citations
Citations to this article as recorded by- Associations of serum keratin 1 with thyroid function and immunity in Graves’ disease
Chao-Wen Cheng, Wen-Fang Fang, Jiunn-Diann Lin, Appuwawadu Mestri Nipun Lakshitha de Silva
PLOS ONE.2023; 18(11): e0289345. CrossRef
- Associations of serum keratin 1 with thyroid function and immunity in Graves’ disease


 KES
KES

 First
First Prev
Prev



