Guidelines in EnM
- Page Path
- HOME > BROWSE ARTICLES > Guidelines in EnM
- Thyroid
- A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
- Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
- Endocrinol Metab. 2024;39(1):61-72. Published online February 14, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1938
- 1,507 View
- 95 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
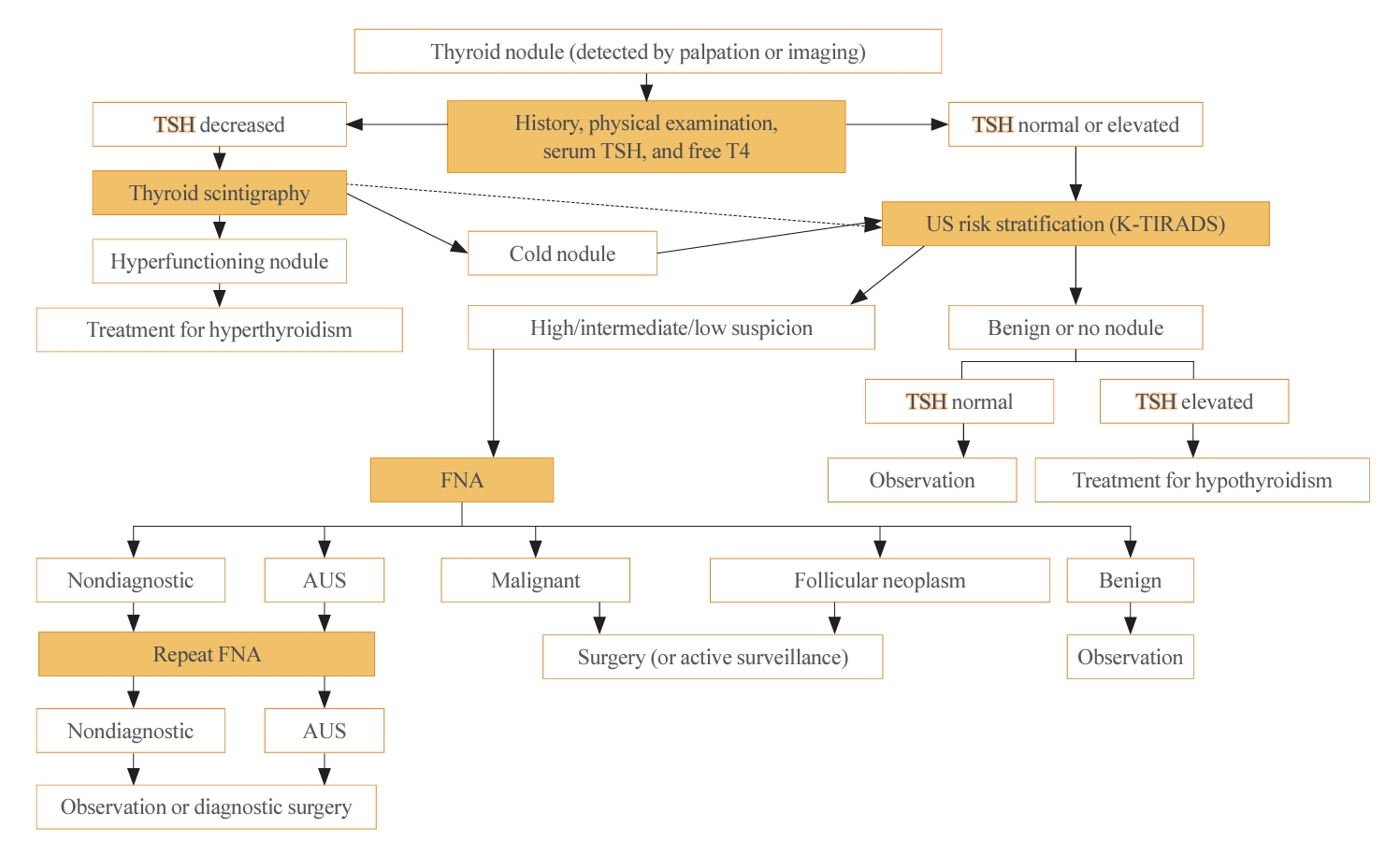
ePub - The 2023 Korean Thyroid Association (KTA) Management Guideline for Patients with Thyroid Nodules constitute an update of the 2016 KTA guideline for thyroid nodules and cancers that focuses specifically on nodules. The 2023 guideline aim to offer updated guidance based on new evidence that reflects the changes in clinical practice since the 2016 KTA guideline. To update the 2023 guideline, a comprehensive literature search was conducted from January 2022 to May 2022. The literature search included studies, reviews, and other evidence involving human subjects that were published in English in MEDLINE (PubMed), Embase, and other relevant databases. Additional significant clinical trials and research studies published up to April 2023 were also reviewed. The limitations of the current evidence are discussed, and suggestions for areas in need of further research are identified. The purpose of this review is to provide a summary of the 2023 KTA guideline for the management of thyroid nodules released in May 2023 and to give a balanced insight with comparison of recent guidelines from other societies.

- Thyroid
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
- Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
- Endocrinol Metab. 2024;39(1):47-60. Published online February 15, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1937

- 1,898 View
- 173 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The indolent nature and favorable outcomes associated with papillary thyroid microcarcinoma have prompted numerous prospective studies on active surveillance (AS) and its adoption as an alternative to immediate surgery in managing low-risk thyroid cancer. This article reviews the current status of AS, as outlined in various international practice guidelines. AS is typically recommended for tumors that measure 1 cm or less in diameter and do not exhibit aggressive subtypes on cytology, extrathyroidal extension, lymph node metastasis, or distant metastasis. To determine the most appropriate candidates for AS, factors such as tumor size, location, multiplicity, and ultrasound findings are considered, along with patient characteristics like medical condition, age, and family history. Moreover, shared decision-making, which includes patient-reported outcomes such as quality of life and cost-effectiveness, is essential. During AS, patients undergo regular ultrasound examinations to monitor for signs of disease progression, including tumor growth, extrathyroidal extension, or lymph node metastasis. In conclusion, while AS is a feasible and reliable approach for managing lowrisk thyroid cancer, it requires careful patient selection, effective communication for shared decision-making, standardized follow-up protocols, and a clear definition of disease progression.

- Adrenal gland
- 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
- Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung, The Committee of Clinical Practice Guideline of Korean Endocrine Society, The Korean Adrenal Study Group of Korean Endocrine Society
- Endocrinol Metab. 2023;38(6):597-618. Published online October 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1789

- 3,459 View
- 483 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Primary aldosteronism (PA) is a common, yet underdiagnosed cause of secondary hypertension. It is characterized by an overproduction of aldosterone, leading to hypertension and/or hypokalemia. Despite affecting between 5.9% and 34% of patients with hypertension, PA is frequently missed due to a lack of clinical awareness and systematic screening, which can result in significant cardiovascular complications. To address this, medical societies have developed clinical practice guidelines to improve the management of hypertension and PA. The Korean Endocrine Society, drawing on a wealth of research, has formulated new guidelines for PA. A task force has been established to prepare PA guidelines, which encompass epidemiology, pathophysiology, clinical presentation, diagnosis, treatment, and follow-up care. The Korean clinical guidelines for PA aim to deliver an evidence-based protocol for PA diagnosis, treatment, and patient monitoring. These guidelines are anticipated to ease the burden of this potentially curable condition.
-
Citations
Citations to this article as recorded by- Correlation of Histopathologic Subtypes of Primary Aldosteronism with Clinical Phenotypes and Postsurgical Outcomes
Chang Ho Ahn, You-Bin Lee, Jae Hyeon Kim, Young Lyun Oh, Jung Hee Kim, Kyeong Cheon Jung
The Journal of Clinical Endocrinology & Metabolism.2023;[Epub] CrossRef
- Correlation of Histopathologic Subtypes of Primary Aldosteronism with Clinical Phenotypes and Postsurgical Outcomes

- Thyroid
- Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
- Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
- Endocrinol Metab. 2023;38(4):381-391. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1778

- 3,028 View
- 462 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
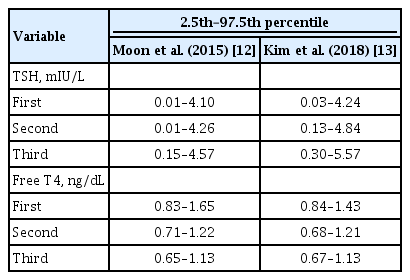
ePub - Subclinical hypothyroidism (SCH) is characterized by elevated thyroid-stimulating hormone (TSH) and normal free thyroxine levels. The Korean Thyroid Association recently issued a guideline for managing SCH, which emphasizes Korean-specific TSH diagnostic criteria and highlights the health benefits of levothyroxine (LT4) treatment. A serum TSH level of 6.8 mIU/L is presented as the reference value for diagnosing SCH. SCH can be classified as mild (TSH 6.8 to 10.0 mIU/L) or severe (TSH >10.0 mIU/L), and patients can be categorized as adults (age <70 years) or elderly (age ≥70 years), depending on the health effects of LT4 treatment. An initial increase in serum TSH levels should be reassessed with a subsequent measurement, including a thyroid peroxidase antibody test, preferably 2 to 3 months after the initial assessment. While LT4 treatment is not generally recommended for mild SCH in adults, it is necessary for severe SCH in patients with underlying coronary artery disease or heart failure and it may be considered for those with concurrent dyslipidemia. Conversely, LT4 treatment is generally not recommended for elderly patients, regardless of SCH severity. For those SCH patients who are prescribed LT4 treatment, the dosage should be personalized, and serum TSH levels should be regularly monitored to maintain the optimal LT4 regimen.
-
Citations
Citations to this article as recorded by- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism
Won Sang Yoo
Endocrinology and Metabolism.2024; 39(1): 188. CrossRef
- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism

- Thyroid
- Diagnosis and Management of Thyroid Disease during Pregnancy and Postpartum: 2023 Revised Korean Thyroid Association Guidelines
- Hwa Young Ahn, Ka Hee Yi
- Endocrinol Metab. 2023;38(3):289-294. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1696
- 6,500 View
- 706 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thyroid hormone plays a critical role in fetal growth and development, and thyroid dysfunction during pregnancy is associated with several adverse outcomes, such as miscarriage and preterm birth. In this review, we introduce and explain three major changes in the revised Korean Thyroid Association (KTA) guidelines for the diagnosis and management of thyroid disease during pregnancy: first, the normal range of thyroid-stimulating hormone (TSH) during pregnancy; second, the treatment of subclinical hypothyroidism; and third, the management of euthyroid pregnant women with positive thyroid autoantibodies. The revised KTA guidelines adopt 4.0 mIU/L as the upper limit of TSH in the first trimester. A TSH level between 4.0 and 10.0 mIU/L, combined with free thyroxine (T4) within the normal range, is defined as subclinical hypothyroidism, and a TSH level over 10 mIU/L is defined as overt hypothyroidism regardless of the free T4 level. Levothyroxine treatment is recommended when the TSH level is higher than 4 mIU/L in subclinical hypothyroidism, regardless of thyroid peroxidase antibody positivity. However, thyroid hormone therapy to prevent miscarriage is not recommended in thyroid autoantibody-positive women with normal thyroid function.
-
Citations
Citations to this article as recorded by- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2023; 38(4): 381. CrossRef - Maternal isolated hypothyroxinemia in the first trimester is not associated with adverse pregnancy outcomes, except for macrosomia: a prospective cohort study in China
Jing Du, Linong Ji, Xiaomei Zhang, Ning Yuan, Jianbin Sun, Dan Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia

- Miscellaneous
- Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
- Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim, The Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2022;37(6):839-850. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1627
- 3,491 View
- 321 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
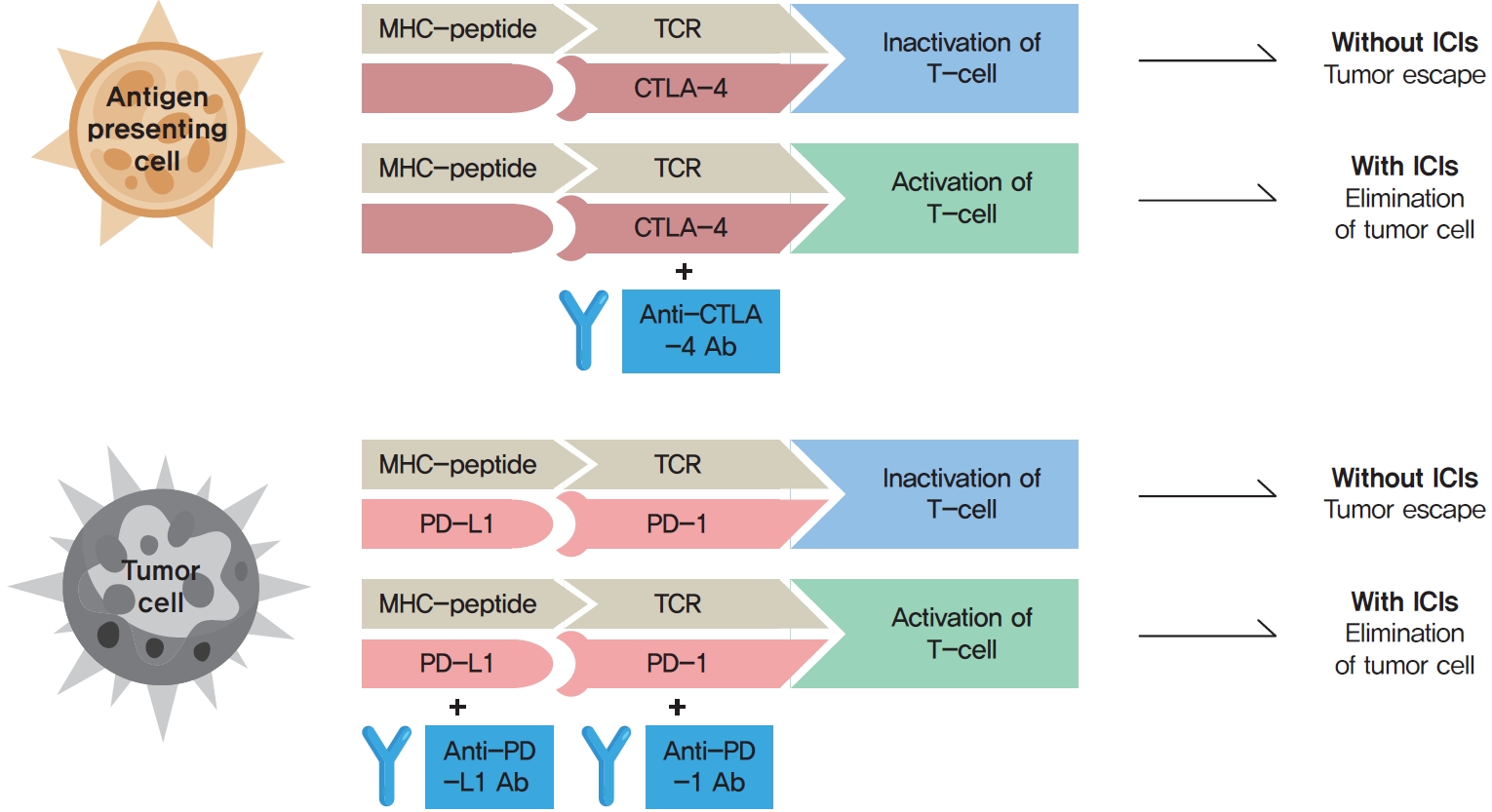
ePub - Immune checkpoint inhibitors (ICIs) including an anti-cytotoxic T-lymphocyte-associated antigen 4 inhibitor, anti-programmed cell death protein 1 (PD-1) inhibitors, and anti-PD-ligand 1 inhibitors are representative therapeutics for various malignancies. In oncology, the application of ICIs is currently expanding to a wider range of malignancies due to their remarkable clinical outcomes. ICIs target immune checkpoints which suppress the activity of T-cells that are specific for tumor antigens, thereby allowing tumor cells to escape the immune response. However, immune checkpoints also play a crucial role in preventing autoimmune reactions. Therefore, ICIs targeting immune checkpoints can trigger various immune-related adverse events (irAEs), especially in endocrine organs. Considering the endocrine organs that are frequently involved, irAEs associated endocrinopathies are frequently life-threatening and have unfavorable clinical implications for patients. However, there are very limited data from large clinical trials that would inform the development of clinical guidelines for patients with irAEs associated endocrinopathies. Considering the current clinical situation, in which the scope and scale of the application of ICIs are increasing, position statements from clinical specialists play an essential role in providing the appropriate recommendations based on both medical evidence and clinical experience. As endocrinologists, we would like to present precautions and recommendations for the management of immune-related endocrine disorders, especially those involving the adrenal, thyroid, and pituitary glands caused by ICIs.
-
Citations
Citations to this article as recorded by- Pembrolizumab plus lenvatinib for radically unresectable or metastatic renal cell carcinoma in the Japanese population
Ryo Fujiwara, Takeshi yuasa, kenichi kobayashi, tetsuya yoshida, susumu kageyama
Expert Review of Anticancer Therapy.2023; 23(5): 461. CrossRef - Incidence of Endocrine-Related Dysfunction in Patients Treated with New Immune Checkpoint Inhibitors: A Meta-Analysis and Comprehensive Review
Won Sang Yoo, Eu Jeong Ku, Eun Kyung Lee, Hwa Young Ahn
Endocrinology and Metabolism.2023; 38(6): 750. CrossRef
- Pembrolizumab plus lenvatinib for radically unresectable or metastatic renal cell carcinoma in the Japanese population

- Diabetes, Obesity and Metabolism
- Recent Updates to Clinical Practice Guidelines for Diabetes Mellitus
- Jin Yu, Seung-Hwan Lee, Mee Kyoung Kim
- Endocrinol Metab. 2022;37(1):26-37. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.105
- 17,074 View
- 1,147 Download
- 22 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
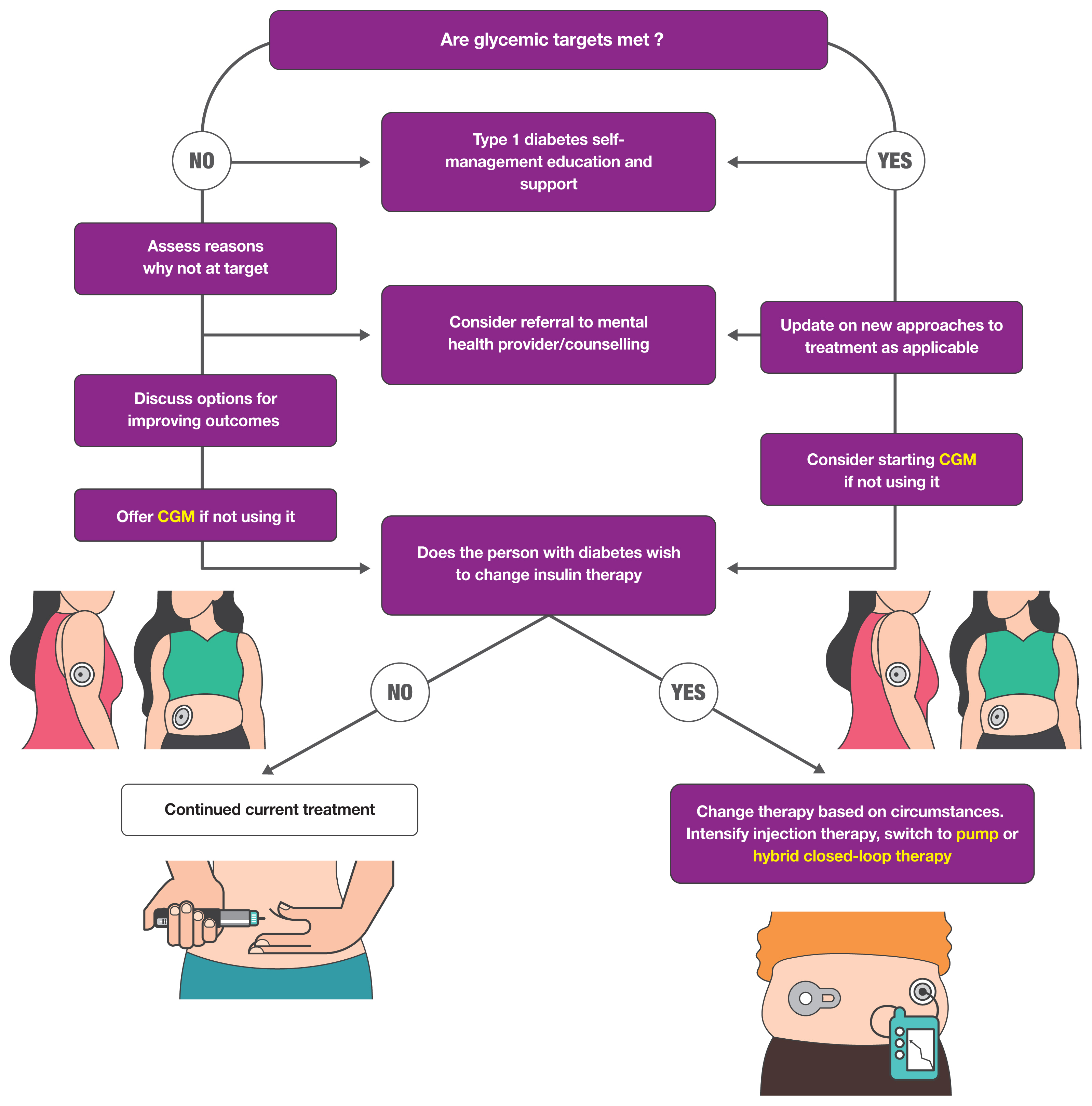
ePub - Guidelines for the management of patients with diabetes have become an important part of clinical practice that improve the quality of care and help establish evidence-based medicine in this field. With rapidly accumulating evidence on various aspects of diabetes care, including landmark clinical trials of treatment agents and newer technologies, timely updates of the guidelines capture the most current state of the field and present a consensus. As a leading academic society, the Korean Diabetes Association publishes practice guidelines biennially and the American Diabetes Association does so annually. In this review, we summarize the key changes suggested in the most recent guidelines. Some of the important updates include treatment algorithms emphasizing comorbid conditions such as atherosclerotic cardiovascular disease, heart failure, and chronic kidney disease in the selection of anti-diabetic agents; wider application of continuous glucose monitoring (CGM), insulin pump technologies and indices derived from CGM such as time in range; more active screening of subjects at high-risk of diabetes; and more detailed individualization in diabetes care. Although there are both similarities and differences among guidelines and some uncertainty remains, these updates provide a good approach for many clinical practitioners who are battling with diabetes.
-
Citations
Citations to this article as recorded by- Finerenone: Efficacy of a New Nonsteroidal Mineralocorticoid Receptor Antagonist in Treatment of Patients With Chronic Kidney Disease and Type 2 Diabetes
Subo Dey, Jasmine Garg, Andy Wang, Eva Holzner, William H. Frishman, Wilbert S. Aronow
Cardiology in Review.2024; 32(3): 285. CrossRef - Use of Diabetes Medications before and after a Heart Failure–Related Hospitalization among Nursing Home Residents
Tingting Zhang, Andrew R. Zullo, Kaleen (Kaley) N. Hayes, Dae Hyun Kim, Yoojin Lee, Lori A. Daiello, Douglas P. Kiel, Sarah D. Berry
Journal of the American Medical Directors Association.2024; 25(3): 454. CrossRef - Accuracy and Safety of the 15-Day CareSens Air Continuous Glucose Monitoring System
Kyung-Soo Kim, Seung-Hwan Lee, Won Sang Yoo, Cheol-Young Park
Diabetes Technology & Therapeutics.2024; 26(4): 222. CrossRef - Body composition and metabolic syndrome in patients with type 1 diabetes
Qiong Zeng, Xiao-Jing Chen, Yi-Ting He, Ze-Ming Ma, Yi-Xi Wu, Kun Lin
World Journal of Diabetes.2024; 15(1): 81. CrossRef - The best internal structure of the Diabetes Quality of Life Measure (DQOL) in Brazilian patients
Denilson Menezes Almeida, Aldair Darlan Santos-de-Araújo, José Mário Costa Brito Júnior, Marcela Cacere, André Pontes-Silva, Cyrene Piazera Costa, Maria Cláudia Gonçalves, José Márcio Soares Leite, Almir Vieira Dibai-Filho, Daniela Bassi-Dibai
BMC Public Health.2024;[Epub] CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - SGLT2 inhibitors and their possible use in prevention and treatment of neurological diseases
Mateusz Sobczyk, Daria Żuraw, Paulina Oleksa, Kacper Jasiński, Mikołaj Porzak, Michał Dacka
Prospects in Pharmaceutical Sciences.2024; 22(1): 16. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - Innovative Therapeutic Approaches in Non-Alcoholic Fatty Liver Disease: When Knowing Your Patient Is Key
Marta Alonso-Peña, Maria Del Barrio, Ana Peleteiro-Vigil, Carolina Jimenez-Gonzalez, Alvaro Santos-Laso, Maria Teresa Arias-Loste, Paula Iruzubieta, Javier Crespo
International Journal of Molecular Sciences.2023; 24(13): 10718. CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Access to novel anti-diabetic agents in resource limited settings: A brief commentary
Poobalan Naidoo, Kiolan Naidoo, Sumanth Karamchand, Rory F Leisegang
World Journal of Diabetes.2023; 14(7): 939. CrossRef - Comparative efficacy and safety profile of once-weekly Semaglutide versus once-daily Sitagliptin as an add-on to metformin in patients with type 2 diabetes: a systematic review and meta-analysis
Tirath Patel, Fnu Nageeta, Rohab Sohail, Tooba Shaukat Butt, Shyamala Ganesan, Fnu Madhurita, Muhammad Ahmed, Mahrukh Zafar, Wirda Zafar, Mohammad Uzair Zaman, Giustino Varrassi, Mahima Khatri, Satesh Kumar
Annals of Medicine.2023;[Epub] CrossRef - Bexagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, for improvement of glycemia in type 2 diabetes mellitus: a systematic review and meta-analysis
Sagar Dholariya, Siddhartha Dutta, Ragini Singh, Deepak Parchwani, Amit Sonagra, Mehul Kaliya
Expert Opinion on Pharmacotherapy.2023; 24(18): 2187. CrossRef - Analysis of the management and therapeutic performance of diabetes mellitus employing special target
Hong-Yan Sun, Xiao-Yan Lin
World Journal of Diabetes.2023; 14(12): 1721. CrossRef - Zinc Chloride Enhances the Antioxidant Status, Improving the Functional and Structural Organic Disturbances in Streptozotocin-Induced Diabetes in Rats
Irina Claudia Anton, Liliana Mititelu-Tartau, Eliza Gratiela Popa, Mihaela Poroch, Vladimir Poroch, Ana-Maria Pelin, Liliana Lacramioara Pavel, Ilie Cristian Drochioi, Gina Eosefina Botnariu
Medicina.2022; 58(11): 1620. CrossRef
- Finerenone: Efficacy of a New Nonsteroidal Mineralocorticoid Receptor Antagonist in Treatment of Patients With Chronic Kidney Disease and Type 2 Diabetes

- Miscellaneous
- COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
- Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim, the Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2021;36(4):757-765. Published online August 17, 2021
- DOI: https://doi.org/10.3803/EnM.2021.404
- 10,361 View
- 419 Download
- 19 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since the first outbreak of coronavirus disease 2019 (COVID-19), ongoing efforts have been made to discover an efficacious vaccine against COVID-19 to combat the pandemic. In most countries, both mRNA and DNA vaccines have been administered, and their side effects have also been reported. The clinical course of COVID-19 and the effects of vaccination against COVID-19 are both influenced by patients’ health status and involve a systemic physiological response. In view of the systemic function of endocrine hormones, endocrine disorders themselves and the therapeutics used to treat them can influence the outcomes of vaccination for COVID-19. However, there are very limited data to support the development of clinical guidelines for patients with specific medical backgrounds based on large clinical trials. In the current severe circumstances of the COVID-19 pandemic, position statements made by clinical specialists are essential to provide appropriate recommendations based on both medical evidence and clinical experiences. As endocrinologists, we would like to present the medical background of COVID-19 vaccination, as well as precautions to prevent the side effects of COVID-19 vaccination in patients with specific endocrine disorders, including adrenal insufficiency, diabetes mellitus, osteoporosis, autoimmune thyroid disease, hypogonadism, and pituitary disorders.
-
Citations
Citations to this article as recorded by- COVID-19 mRNA vaccine may trigger subacute thyroiditis
Mehmet Sözen, Ömercan Topaloğlu, Berrin Çetinarslan, Alev Selek, Zeynep Cantürk, Emre Gezer, Damla Köksalan, Taner Bayraktaroğlu
Human Vaccines & Immunotherapeutics.2024; 17(12): 5120. CrossRef - The role of co-morbidities in the development of an AEFI after COVID-19 vaccination in a large prospective cohort with patient-reported outcomes in the Netherlands
C. Ouaddouh, J.W. Duijster, T. Lieber, F.P.A.M. van Hunsel
Expert Opinion on Drug Safety.2024; 23(3): 323. CrossRef - Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
Hyeyeon Moon, Sunghwan Suh, Mi Kyoung Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Prior immunization status of COVID-19 patients and disease severity: A multicenter retrospective cohort study assessing the different types of immunity
Javaria Aslam, Faisal Shahzad Khan, Muhammad Talha Haris, Hewad Hewadmal, Maryam Khalid, Mohammad Y. Alshahrani, Qurrat-ul-ain Aslam, Irrum Aneela, Urooj Zafar
Vaccine.2023; 41(2): 598. CrossRef - Mortality and Severity of Coronavirus Disease 2019 in Patients with Long-Term Glucocorticoid Therapy: A Korean Nationwide Cohort Study
Eu Jeong Ku, Keeho Song, Kyoung Min Kim, Gi Hyeon Seo, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(2): 253. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Inactivated SARS-CoV-2 vaccination does not disturb the clinical course of Graves’ disease: An observational cohort study
Shichen Xu, Huixin Yu, Xian Cheng, Jing Wu, Jiandong Bao, Li Zhang
Vaccine.2023; 41(38): 5648. CrossRef - Adrenal Crisis Associated With COVID-19 Vaccination in Patients With Adrenal Insufficiency
Yukako Kurematsu, Takako Mohri, Sadanori Okada, Yutaka Takahashi
JCEM Case Reports.2023;[Epub] CrossRef - Adverse Events Associated with COVID-19 Vaccination in Adolescents with Endocrinological Disorders: A Cross-Sectional Study
İbrahim Mert Erbaş, İrem Ceren Erbaş, Gözde Akın Kağızmanlı, Kübra Yüksek Acinikli, Özge Besci, Korcan Demir, Ece Böber, Nurşen Belet, Ayhan Abacı
Journal of Clinical Research in Pediatric Endocrinology.2023; 15(3): 248. CrossRef - Neue Aspekte der Glukokortikoidsubstitution bei Nebennierenrindeninsuffizienz
Tina Kienitz, Gesine Meyer
Der Internist.2022; 63(1): 12. CrossRef - Endocrine Follow-up During Post-Acute COVID-19: Practical Recommendations Based on Available Clinical Evidence
Rimesh Pal, Ameya Joshi, Sanjay K. Bhadada, Mainak Banerjee, Suresh Vaikkakara, Satinath Mukhopadhyay
Endocrine Practice.2022; 28(4): 425. CrossRef - Safety of Inactivated and mRNA COVID-19 Vaccination Among Patients Treated for Hypothyroidism: A Population-Based Cohort Study
Xi Xiong, Carlos King Ho Wong, Ivan Chi Ho Au, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Kristy Tsz Kwan Lau, Chi Ho Lee, Yu Cho Woo, David Tak Wai Lui, Ian Chi Kei Wong
Thyroid.2022; 32(5): 505. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Adrenal Crisis Secondary to COVID-19 Vaccination in a Patient With Hypopituitarism
Nikolina Markovic, Anila Faizan, Chirag Boradia, Sridhar Nambi
AACE Clinical Case Reports.2022; 8(4): 171. CrossRef - The Effect of Inactivated SARS-CoV-2 Vaccines on TRAB in Graves’ Disease
LingHong Huang, ZhengRong Jiang, JingXiong Zhou, YuPing Chen, HuiBin Huang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Osteoporosis in Patients With Respiratory Diseases
Yue Ma, Shui Qiu, Renyi Zhou
Frontiers in Physiology.2022;[Epub] CrossRef - Pilot Findings on SARS-CoV-2 Vaccine-Induced Pituitary Diseases: A Mini Review from Diagnosis to Pathophysiology
Ach Taieb, El Euch Mounira
Vaccines.2022; 10(12): 2004. CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - No need of glucocorticoid dose adjustment in patients with adrenal insufficiency before COVID-19 vaccine
Tania Pilli, Cristina Dalmiglio, Gilda Dalmazio, Alfonso Sagnella, Raffaella Forleo, Lucia Brilli, Fabio Maino, Cristina Ciuoli, Maria Grazia Castagna
European Journal of Endocrinology.2022; 187(1): K7. CrossRef - Diabetes and COVID-19 Vaccination
Hae Dong Choi, Jun Sung Moon
The Journal of Korean Diabetes.2021; 22(4): 221. CrossRef
- COVID-19 mRNA vaccine may trigger subacute thyroiditis

- Adrenal Gland
- Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
- Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
- Endocrinol Metab. 2021;36(3):553-563. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1008

- 3,660 View
- 142 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thermal ablation is a good alternative treatment in patients who are unable to undergo adrenalectomy. Even though the Asian Conference on Tumor Ablation (ACTA) has been held for many years, adrenal ablation guidelines have not been established. No guidelines for adrenal ablation are established in American and European countries, either. The aim of this review was to introduce the first version of ACTA guidelines for adrenal tumor ablation.
-
Citations
Citations to this article as recorded by- Treatment of primary aldosteronism: Clinical practice guidelines of the Taiwan Society of Aldosteronism
Chi-Shin Tseng, Chieh-Kai Chan, Hsiang-Ying Lee, Chien-Ting Pan, Kang-Yung Peng, Shuo-Meng Wang, Kuo-How Huang, Yao-Chou Tsai, Vin-Cent Wu, Jeff S. Chueh
Journal of the Formosan Medical Association.2024; 123: S125. CrossRef - Development and preclinical evaluation of multifunctional hydrogel for precise thermal protection during thermal ablation
Bowen Zheng, Peng Zhang, Qijun Lv, Tao Wu, Yadong Liu, Junjie Tang, Yanping Ma, Lili Cheng, Langtao Xu, Yizhen Wang, Yifan Xue, Jie Liu, Jie Ren
Bioactive Materials.2024; 31: 119. CrossRef - Case report of trans-renal ablation procedures for a recurrent pheochromocytoma in von Hippel-Lindau disease
Byung Kwan Park
Precision and Future Medicine.2023; 7(2): 90. CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef
- Treatment of primary aldosteronism: Clinical practice guidelines of the Taiwan Society of Aldosteronism

- Thyroid
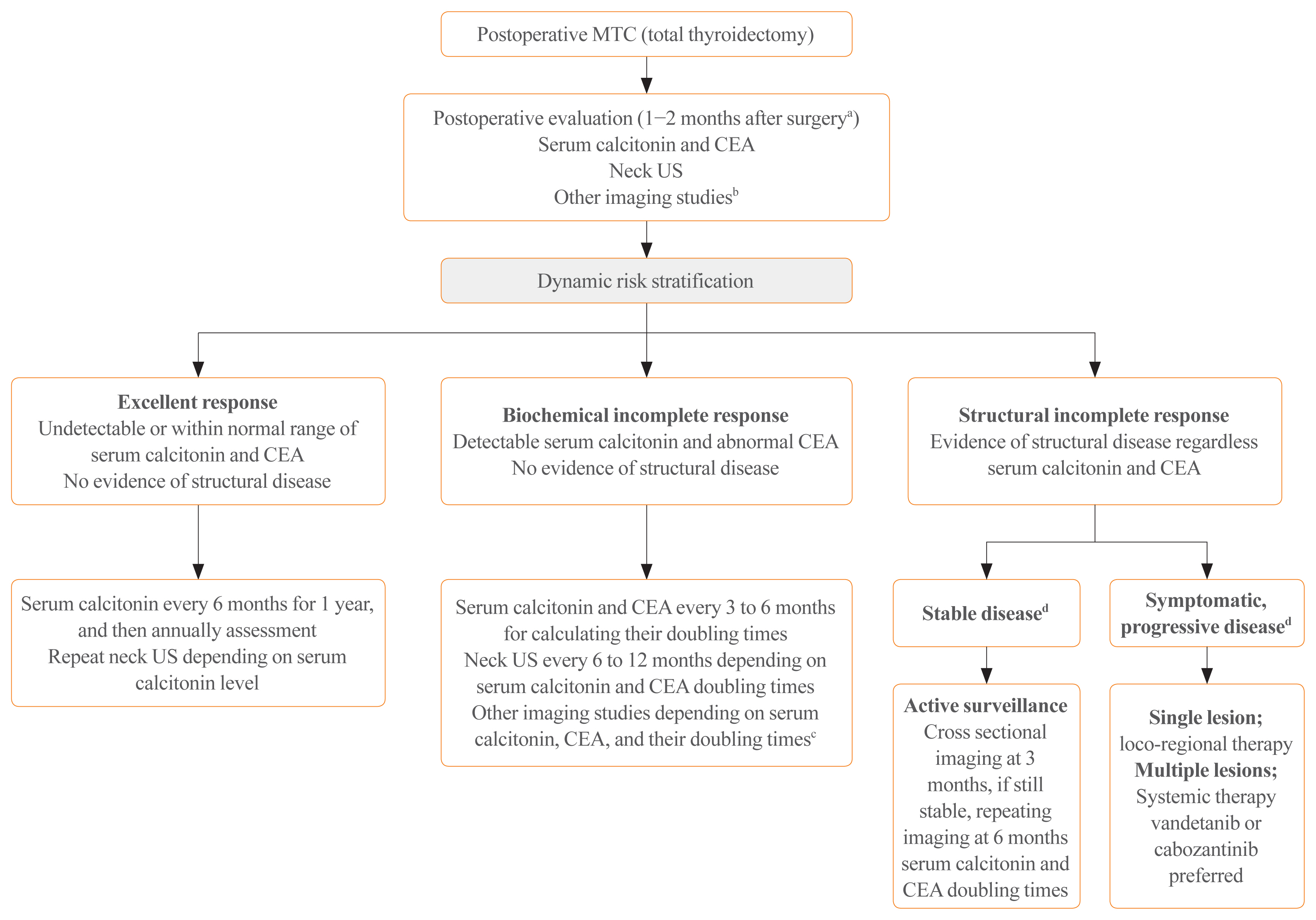
- Current Guidelines for Management of Medullary Thyroid Carcinoma
- Mijin Kim, Bo Hyun Kim
- Endocrinol Metab. 2021;36(3):514-524. Published online June 22, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1082
- 17,986 View
- 1,711 Download
- 29 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Medullary thyroid carcinoma (MTC) is a rare neuroendocrine tumor originating from the parafollicular cells. The diagnostic and therapeutic strategies for the condition are different from those used for well-differentiated thyroid cancer. Since the 2015 American Thyroid Association guidelines for the diagnosis and treatment of MTC, the latest, including the National Comprehensive Cancer Network and European Association for Medical Oncology guidelines have been updated to reflect several recent advances in the management of MTC. Advances in molecular diagnosis and postoperative risk stratification systems have led to individualized treatment and follow-up strategies. Multi-kinase inhibitors, such as vandetanib and cabozantinib, can prolong disease progression-free survival with favorable adverse effects. In addition, potent selective rearranged during transfection (RET) inhibitors (selpercatinib and pralsetinib) have shown a promising efficacy in recent clinical trials. This review summarizes the management of MTC in recent guidelines focused on sporadic MTC.
-
Citations
Citations to this article as recorded by- Molecular imaging and related therapeutic options for medullary thyroid carcinoma: state of the art and future opportunities
Alessio Imperiale, Valentina Berti, Mickaël Burgy, Roberto Luigi Cazzato, Arnoldo Piccardo, Giorgio Treglia
Reviews in Endocrine and Metabolic Disorders.2024; 25(1): 187. CrossRef - Diffuse C-Cells Hyperplasia Is the Source of False Positive Calcitonin Measurement in FNA Washout Fluids of Thyroid Nodules: A Rational Clinical Approach to Avoiding Unnecessary Surgery
Chiara Mura, Rossella Rodia, Silvia Corrias, Antonello Cappai, Maria Letizia Lai, Gian Luigi Canu, Fabio Medas, Pietro Giorgio Calò, Stefano Mariotti, Francesco Boi
Cancers.2024; 16(1): 210. CrossRef - Meta-Analysis of the Efficacy and Safety Evaluation of Vandetanib in
the Treatment of Medullary Thyroid Cancer
Tong-cheng Xian, Min-ye Yang, Xue-lin Zhang, Jie Wang, Yi Luo
Hormone and Metabolic Research.2024;[Epub] CrossRef - Successful localisation of recurrent thyroid cancer using preoperative patent blue dye injection
B. O. Evranos, N. Ince, H. Ataş, S. B. Polat, H. Ahsen, N. N. Imga, A. Dirikoc, O. Topaloglu, T. Tutuncu, R. Ersoy, B. Cakir
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Current and future of immunotherapy for thyroid cancer based on bibliometrics and clinical trials
Ke Wang, Ying Zhang, Yang Xing, Hong Wang, Minghua He, Rui Guo
Discover Oncology.2024;[Epub] CrossRef - Combining radiomics with thyroid imaging reporting and data system to predict lateral cervical lymph node metastases in medullary thyroid cancer
Zhiqiang Liu, Xiwei Zhang, Xiaohui Zhao, Qianqian Guo, Zhengjiang Li, Minghui Wei, Lijuan Niu, Changming An
BMC Medical Imaging.2024;[Epub] CrossRef - Potentials and future perspectives of multi-target drugs in cancer treatment: the next generation anti-cancer agents
Ali Doostmohammadi, Hossein Jooya, Kimia Ghorbanian, Sargol Gohari, Mehdi Dadashpour
Cell Communication and Signaling.2024;[Epub] CrossRef - Diagnostic capabilities of PET/CT with 18F-DOPA in biochemical recurrence of medullary thyroid carcinoma: a retrospective study
N. V. Tsentr, A. A. Zyryanova, M. A. Rusnak, D. V. Ryzhkova
Diagnostic radiology and radiotherapy.2024; 15(1): 87. CrossRef - LINC00887 Acts as an Enhancer RNA to Promote Medullary Thyroid
Carcinoma Progression by Binding with FOXQ1
Daxiang Liu, Wenjing Wang, Yanzhao Wu, Yongle Qiu, Lan Zhang
Current Cancer Drug Targets.2024; 24(5): 519. CrossRef - Update on Management of Medullary Thyroid Carcinoma: Focus on Nuclear Medicine
Giorgio Treglia, Vittoria Rufini, Arnoldo Piccardo, Alessio Imperiale
Seminars in Nuclear Medicine.2023; 53(4): 481. CrossRef - Cabozantinib, Vandetanib, Pralsetinib and Selpercatinib as Treatment for Progressed Medullary Thyroid Cancer with a Main Focus on Hypertension as Adverse Effect
Linnea Højer Wang, Markus Wehland, Petra M. Wise, Manfred Infanger, Daniela Grimm, Michael C. Kreissl
International Journal of Molecular Sciences.2023; 24(3): 2312. CrossRef - A proposed grading scheme for predicting recurrence in medullary thyroid cancer based on the Ki67 index and metastatic lymph node ratio
Pengfei Xu, Di Wu, Xuekui Liu
Endocrine.2023; 81(1): 107. CrossRef - Efficacy and Safety of [177Lu]Lu-DOTA-TATE in Adults with Inoperable or Metastatic Somatostatin Receptor-Positive Pheochromocytomas/Paragangliomas, Bronchial and Unknown Origin Neuroendocrine Tumors, and Medullary Thyroid Carcinoma: A Systematic Literatur
Marianna Hertelendi, Oulaya Belguenani, Azzeddine Cherfi, Ilya Folitar, Gabor Kollar, Berna Degirmenci Polack
Biomedicines.2023; 11(4): 1024. CrossRef - PET/CT with various radiopharmaceuticals in the complex diagnosis of medullary thyroid carcinoma: a review
N. V. Tsentr, A. E. Ertman, D. V. Ryzhkova
Diagnostic radiology and radiotherapy.2023; 14(2): 31. CrossRef - Physical activity and reduced risk of fracture in thyroid cancer patients after thyroidectomy — a nationwide cohort study
Jinyoung Kim, Kyungdo Han, Jin-Hyung Jung, Jeonghoon Ha, Chaiho Jeong, Jun-Young Heu, Se-Won Lee, Jeongmin Lee, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Ki-Hyun Baek
Frontiers in Endocrinology.2023;[Epub] CrossRef - Different RONS Generation in MTC-SK and NSCL Cells Lead to Varying Antitumoral Effects of Alpha-Ketoglutarate + 5-HMF
Joachim Greilberger, Katharina Erlbacher, Philipp Stiegler, Reinhold Wintersteiger, Ralf Herwig
Current Issues in Molecular Biology.2023; 45(8): 6503. CrossRef - Medullary thyroid carcinoma
Maria Rosa Pelizzo, Esmeralda Isabella Mazza, Caterina Mian, Isabella Merante Boschin
Expert Review of Anticancer Therapy.2023; 23(9): 943. CrossRef - Mixed medullary‑follicular thyroid carcinoma: A case report and literature review
Yonghui Wang, Dandan Yin, Guifang Ren, Zhengjiang Wang, Fanhua Kong
Oncology Letters.2023;[Epub] CrossRef - Circulating cell-free DNA (cfDNA) in patients with medullary thyroid carcinoma is characterized by specific fragmentation and methylation changes with diagnostic value
Anna Citarella, Zein Mersini Besharat, Sofia Trocchianesi, Tanja Milena Autilio, Antonella Verrienti, Giuseppina Catanzaro, Elena Splendiani, Zaira Spinello, Silvia Cantara, Patrizia Zavattari, Eleonora Loi, Cristina Romei, Raffaele Ciampi, Luciano Pezzul
Biomarker Research.2023;[Epub] CrossRef - Advances in Diagnostics and Therapy of Medullary Thyroid Carcinoma (MTC)– A Mini-Review
Michał Miciak, Krzysztof Jurkiewicz
Clinical Cancer Investigation Journal.2023; 12(5): 1. CrossRef - The Evolving Treatment Landscape of Medullary Thyroid Cancer
Marta Laganà, Valentina Cremaschi, Andrea Alberti, Danica M. Vodopivec Kuri, Deborah Cosentini, Alfredo Berruti
Current Treatment Options in Oncology.2023; 24(12): 1815. CrossRef - Pralsetinib: chemical and therapeutic development with FDA authorization for the management of RET fusion-positive non-small-cell lung cancers
Faraat Ali, Kumari Neha, Garima Chauhan
Archives of Pharmacal Research.2022; 45(5): 309. CrossRef - Psychosocial Characteristics and Experiences in Patients with Multiple Endocrine Neoplasia Type 2 (MEN2) and Medullary Thyroid Carcinoma (MTC)
Robin Lockridge, Sima Bedoya, Taryn Allen, Brigitte Widemann, Srivandana Akshintala, John Glod, Lori Wiener
Children.2022; 9(6): 774. CrossRef - Aggressive clinical course of medullary thyroid microcarcinoma
Tamara Janić, Mirjana Stojković, Sanja Klet, Bojan Marković, Beleslin Nedeljković, Jasmina Ćirić, Miloš Žarković
Medicinski glasnik Specijalne bolnice za bolesti štitaste žlezde i bolesti metabolizma.2022; 27(85): 63. CrossRef - Comparative evaluation of somatostatin and CXCR4 receptor expression in different types of thyroid carcinoma using well-characterised monoclonal antibodies
Max Czajkowski, Daniel Kaemmerer, Jörg Sänger, Guido Sauter, Ralph M. Wirtz, Stefan Schulz, Amelie Lupp
BMC Cancer.2022;[Epub] CrossRef - Metastatic Risk Stratification of 2526 Medullary Thyroid Carcinoma Patients: A Study Based on Surveillance, Epidemiology, and End Results Database
Minh-Khang Le, Masataka Kawai, Toru Odate, Huy Gia Vuong, Naoki Oishi, Tetsuo Kondo
Endocrine Pathology.2022; 33(3): 348. CrossRef - Update on the Diagnosis and Management of Medullary Thyroid Cancer: What Has Changed in Recent Years?
Krzysztof Kaliszewski, Maksymilian Ludwig, Bartłomiej Ludwig, Agnieszka Mikuła, Maria Greniuk, Jerzy Rudnicki
Cancers.2022; 14(15): 3643. CrossRef - Immunotherapy of Neuroendocrine Neoplasms: Any Role for the Chimeric Antigen Receptor T Cells?
Giuseppe Fanciulli, Roberta Modica, Anna La Salvia, Federica Campolo, Tullio Florio, Nevena Mikovic, Alice Plebani, Valentina Di Vito, Annamaria Colao, Antongiulio Faggiano
Cancers.2022; 14(16): 3991. CrossRef - Preclinical Evaluation of Novel Tyrosine-Kinase Inhibitors in Medullary Thyroid Cancer
Davide Saronni, Germano Gaudenzi, Alessandra Dicitore, Silvia Carra, Maria Celeste Cantone, Maria Orietta Borghi, Andrea Barbieri, Luca Mignani, Leo J. Hofland, Luca Persani, Giovanni Vitale
Cancers.2022; 14(18): 4442. CrossRef - Rapid and long-lasting response to selpercatinib of paraneoplastic Cushing’s syndrome in medullary thyroid carcinoma
Marine Sitbon, Porhuoy Chou, Seydou Bengaly, Brigitte Poirot, Marie Laloi-Michelin, Laure Deville, Atanas Pachev, Ahouefa Kowo-Bille, Clement Dumont, Cécile N Chougnet
European Thyroid Journal.2022;[Epub] CrossRef - Ginsenoside Rg3 Alleviates Antithyroid Cancer Drug Vandetanib-Induced QT Interval Prolongation
Juan Zhang, Dan Luo, Fang Li, Zhiyi Li, Xiaoli Gao, Jie Qiao, Lin Wu, Miaoling Li, Shao Liang
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - THE ROLE OF CALCITONIN IN THE PREOPERATIVE STAGE AS THE PREDICTOR OF MEDULLARY THYROID CANCER METASTASES
Volodymyr Palamarchuk , Viktor Smolyar , Oleksandr Tovkay, Oleksandr Nechay, Volodymyr Kuts , Revaz Sichinava , Oleh Mazur
Ukrainian Scientific Medical Youth Journal.2021; 127(4): 68. CrossRef - THE ROLE OF CALCITONIN IN THE PREOPERATIVE STAGE AS THE PREDICTOR OF MEDULLARY THYROID CANCER METASTASES
Volodymyr Palamarchuk , Viktor Smolyar , Oleksandr Tovkay , Oleksandr Nechay , Volodymyr Kuts , Revaz Sichinava , Oleh Mazur
The Ukrainian Scientific Medical Youth Journal.2021; 4(127): 68. CrossRef
- Molecular imaging and related therapeutic options for medullary thyroid carcinoma: state of the art and future opportunities

- Adrenal gland
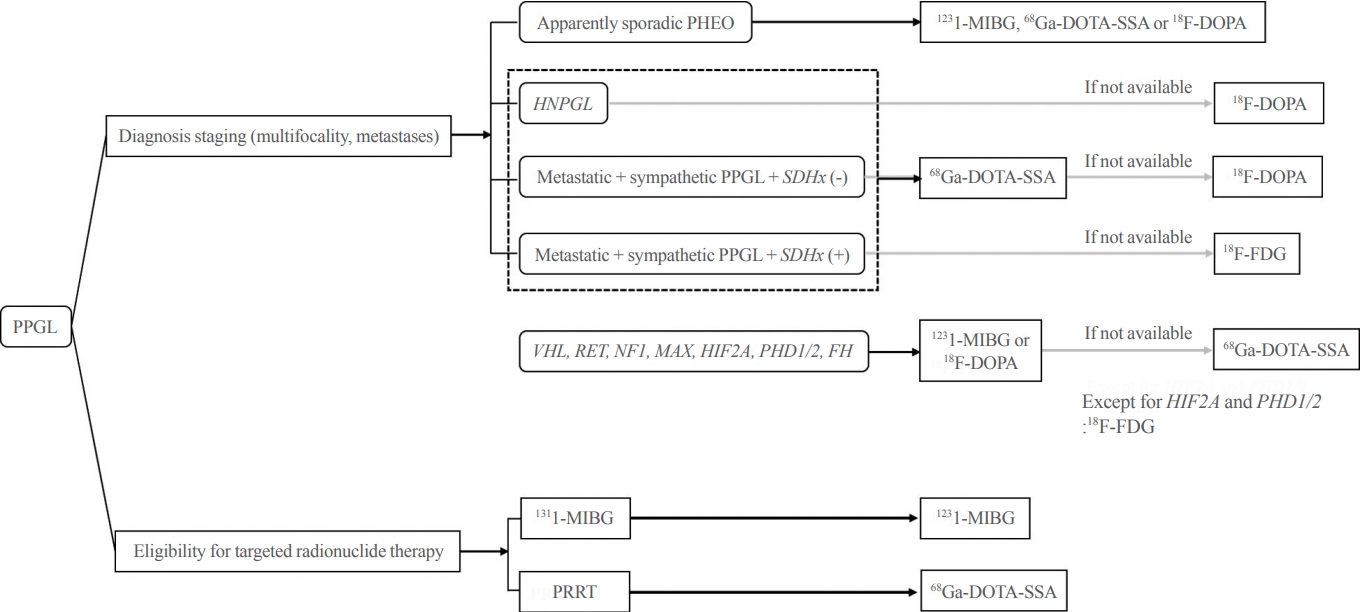
- Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
- Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan Kwon Jung, Young Seok Cho, Jin Chul Paeng, Jae Hyeon Kim, Ohk-Hyun Ryu, Yumie Rhee, Chong Hwa Kim, Eun Jig Lee
- Endocrinol Metab. 2021;36(2):322-338. Published online April 6, 2021
- DOI: https://doi.org/10.3803/EnM.2020.908
- 7,504 View
- 572 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Pheochromocytoma and paraganglioma (PPGLs) are rare catecholamine-secreting neuroendocrine tumors but can be life-threatening. Although most PPGLs are benign, approximately 10% have metastatic potential. Approximately 40% cases are reported as harboring germline mutations. Therefore, timely and accurate diagnosis of PPGLs is crucial. For more than 130 years, clinical, molecular, biochemical, radiological, and pathological investigations have been rapidly advanced in the field of PPGLs. However, performing diagnostic studies to localize lesions and detect metastatic potential can be still challenging and complicated. Furthermore, great progress on genetics has shifted the paradigm of genetic testing of PPGLs. The Korean PPGL task force team consisting of the Korean Endocrine Society, the Korean Surgical Society, the Korean Society of Nuclear Medicine, the Korean Society of Pathologists, and the Korean Society of Laboratory Medicine has developed this position statement focusing on the comprehensive and updated diagnosis for PPGLs.
-
Citations
Citations to this article as recorded by- A Prospective Comparative Study of 18F-FDOPA PET/CT Versus 123I-MIBG Scintigraphy With SPECT/CT for the Diagnosis of Pheochromocytoma and Paraganglioma
Changhwan Sung, Hyo Sang Lee, Dong Yun Lee, Yong-il Kim, Jae Eun Kim, Sang Ju Lee, Seung Jun Oh, Tae-Yon Sung, Yu-Mi Lee, Young Hoon Kim, Beom-Jun Kim, Jung-Min Koh, Seung Hun Lee, Jin-Sook Ryu
Clinical Nuclear Medicine.2024; 49(1): 27. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
A Ram Hong, Ho-Cheol Kang
Endocrinology and Metabolism.2023; 38(2): 175. CrossRef - Lesion-based indicators predict long-term outcomes of pheochromocytoma and paraganglioma– SIZEPASS
Helena Hanschell, Salvador Diaz-Cano, Alfredo Blanes, Nadia Talat, Gabriele Galatá, Simon Aylwin, Klaus Martin Schulte
Frontiers in Endocrinology.2023;[Epub] CrossRef - Interleukin-6-producing paraganglioma as a rare cause of systemic inflammatory response syndrome: a case report
Yin Young Lee, Seung Min Chung
Journal of Yeungnam Medical Science.2023; 40(4): 435. CrossRef - (Extremely rare intrapericardial location of paraganglioma)
Jaroslav Zajíc, Aleš Mokráček, Ladislav Pešl, Jiří Haniš, Dita Schaffelhoferová
Cor et Vasa.2023; 65(4): 692. CrossRef - A Case of Von Hippel-Lindau Disease With Recurrence of Paraganglioma and No Other Associated Symptoms: The Importance of Genetic Testing and Establishing Follow-Up Policies
Naoki Okada, Akihiro Shioya, Sumihito Togi, Hiroki Ura, Yo Niida
Cureus.2023;[Epub] CrossRef - KSNM60 in Nuclear Endocrinology: from the Beginning to the Future
Chae Moon Hong, Young Jin Jeong, Hae Won Kim, Byeong-Cheol Ahn
Nuclear Medicine and Molecular Imaging.2022; 56(1): 17. CrossRef - Change of Computed Tomography-Based Body Composition after Adrenalectomy in Patients with Pheochromocytoma
Yousun Ko, Heeryoel Jeong, Seungwoo Khang, Jeongjin Lee, Kyung Won Kim, Beom-Jun Kim
Cancers.2022; 14(8): 1967. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Pheochromocytoma with Retroperitoneal Metastasis: A Case Report
建新 崔
Advances in Clinical Medicine.2021; 11(05): 2239. CrossRef
- A Prospective Comparative Study of 18F-FDOPA PET/CT Versus 123I-MIBG Scintigraphy With SPECT/CT for the Diagnosis of Pheochromocytoma and Paraganglioma

- Hypothalamus and Pituitary gland
- Current National and International Guidelines for the Management of Male Hypogonadism: Helping Clinicians to Navigate Variation in Diagnostic Criteria and Treatment Recommendations
- Ahmed Al-Sharefi, Richard Quinton
- Endocrinol Metab. 2020;35(3):526-540. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.760

- 9,470 View
- 504 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Male hypogonadism—rebadged by some as testosterone deficiency syndrome—is a clinical and biochemical diagnosis of increasing worldwide interest. Organic male hypogonadism—usually permanent—is well-established, but aging men may also exhibit lower serum testosterone levels; principally due to burden of extra-gonadal comorbidities such as obesity, diabetes and metabolic syndrome, but with an underlying intact hypothalamo-pituitary-testicular (HPT) axis capable of springing back into operation once comorbidities are addressed. Despite encouraging observational data and plausible theoretical underpinning, evidence for efficacy and safety of testosterone in this “aging” group of men is lacking; addressing comorbid illnesses remains the key priority instead. Nevertheless, in recent years, accumulation of misleading information online has triggered a global tsunami of testosterone prescriptions. Despite this, many men with organic hypogonadism remain undiagnosed or untreated; many more face a diagnostic odyssey before achieving care by the appropriate specialist. As testosterone therapy is not without risk several clinical practice guidelines have been published specialist societies to guide physicians on best practice. However, these are heterogeneous in key areas, reflecting divergent approaches to the same evidence basis. Herein, we navigate the major clinical practice guidelines on male hypogonadism and test their respective recommendations against current best evidence.
-
Citations
Citations to this article as recorded by- Expert Opinion on the Diagnosis and Management of Male Hypogonadism in India
Sanjay Kalra, Jubbin Jacob, A. G. Unnikrishnan, Ganapathi Bantwal, Abhay Sahoo, Rakesh Sahay, Sushil Jindal, Madhu Sudan Agrawal, Nitin Kapoor, Banshi Saboo, Mangesh Tiwaskar, Kapil Kochhar, Henrik Falhammar
International Journal of Endocrinology.2023; 2023: 1. CrossRef - Management Outcomes in Males With Hypogonadotropic Hypogonadism Treated With Gonadotropins
Bahaa O Sahib, Ibrahim H Hussein, Nassar T Alibrahim, Abbas A Mansour
Cureus.2023;[Epub] CrossRef - The Association between Inflammation, Testosterone and SHBG in men: A cross‐sectional Multi‐Ethnic Study of Atherosclerosis
Amar Osmancevic, Bledar Daka, Erin D. Michos, Penelope Trimpou, Matthew Allison
Clinical Endocrinology.2023; 99(2): 190. CrossRef - The Illusory Case for Treatment of an Invented Disease
David J. Handelsman
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of Chronic Heart Failure Complicated with Type 2 Diabetes Mellitus on Cognitive Function in the Elderly
Yang Liu, Rui Meng, Jianzeng Dong, Xiaonan Xi
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Different Factors Are Associated With Sex Hormones and Leydig Cell Function in Israelis and Palestinians in Jerusalem
Guy Vishnevsky, Ronit Sinnreich, Hisham Nassar, Dafna Merom, Maya Ish-Shalom, Jeremy D. Kark, Hagai Levine
American Journal of Men's Health.2022; 16(4): 155798832211060. CrossRef - Association of rs9939609 polymorphism in the FTO gene with features of androgen status in men
S. V. Yankovskaya, K. I. Mosalev, I. D. Ivanov, B. B. Pinkhasov, V. G. Selyatitskaya
Сибирский научный медицинский журнал.2022; 42(2): 18. CrossRef - Clinical and pharmacological basis of the use of testosterone drugs for hormonal replacement therapy for hypogonadism in men
N. I. Volkova, A. V. Safronenko, E. V. Gantsgorn, Yu. S. Degtyareva
Obesity and metabolism.2022; 19(2): 233. CrossRef - Monitoring and Management of Bardet-Biedl Syndrome: What the Multi-Disciplinary Team Can Do
Lavinia Caba, Laura Florea, Elena Emanuela Braha, Valeriu Vasile Lupu, Eusebiu Vlad Gorduza
Journal of Multidisciplinary Healthcare.2022; Volume 15: 2153. CrossRef - Non-alcoholic fatty liver disease across endocrinopathies: Interaction with sex hormones
Sara Arefhosseini, Mehrangiz Ebrahimi-Mameghani, Farzad Najafipour, Helda Tutunchi
Frontiers in Endocrinology.2022;[Epub] CrossRef - Recommendations on the diagnosis, treatment and monitoring of testosterone deficiency in men
Bruno Lunenfeld, George Mskhalaya, Michael Zitzmann, Giovanni Corona, Stefan Arver, Svetlana Kalinchenko, Yuliya Tishova, Abraham Morgentaler
The Aging Male.2021; 24(1): 119. CrossRef
- Expert Opinion on the Diagnosis and Management of Male Hypogonadism in India

- Clinical Guidelines for the Management of Adrenal Incidentaloma
- Jung-Min Lee, Mee Kyoung Kim, Seung-Hyun Ko, Jung-Min Koh, Bo-Yeon Kim, Sang Wan Kim, Soo-Kyung Kim, Hae Jin Kim, Ohk-Hyun Ryu, Juri Park, Jung Soo Lim, Seong Yeon Kim, Young Kee Shong, Soon Jib Yoo
- Endocrinol Metab. 2017;32(2):200-218. Published online June 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.200
- 16,177 View
- 688 Download
- 80 Web of Science
- 78 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader An adrenal incidentaloma is an adrenal mass found in an imaging study performed for other reasons unrelated to adrenal disease and often accompanied by obesity, diabetes, or hypertension. The prevalence and incidence of adrenal incidentaloma increase with age and are also expected to rise due to the rapid development of imaging technology and frequent imaging studies. The Korean Endocrine Society is promoting an appropriate practice guideline to meet the rising incidence of adrenal incidentaloma, in cooperation with the Korean Adrenal Gland and Endocrine Hypertension Study Group. In this paper, we discuss important core issues in managing the patients with adrenal incidentaloma. After evaluating core proposition, we propose the most critical 20 recommendations from the initially organized 47 recommendations by Delphi technique.
-
Citations
Citations to this article as recorded by- The improvement of postoperative blood pressure and associated factors in patients with hormone‐negative adrenal adenoma and hypertension
Jiaxing Sun, Yingchun Dong, Hanbo Wang, Xudong Guo, Ning Suo, Shangjian Li, Xiangbin Ren, Shaobo Jiang
Journal of Surgical Oncology.2024; 129(6): 1073. CrossRef - Clinical features and treatment options for pediatric adrenal incidentalomas: a retrospective single center study
Xiaojiang Zhu, Saisai Liu, Yimin Yuan, Nannan Gu, Jintong Sha, Yunfei Guo, Yongji Deng
BMC Pediatrics.2024;[Epub] CrossRef - Characterizing incidental mass lesions in abdominal dual-energy CT compared to conventional contrast-enhanced CT
Jack Junchi Xu, Peter Sommer Ulriksen, Camilla Wium Bjerrum, Michael Patrick Achiam, Timothy Andrew Resch, Lars Lönn, Kristoffer Lindskov Hansen
Acta Radiologica.2023; 64(3): 945. CrossRef - Metastatic Adrenal PEComa: Case Report and Short Review of the Literature
Enrico Battistella, Luca Pomba, Marica Mirabella, Michele Gregianin, Antonio Scapinello, Marco Volante, Antonio Toniato
Medicina.2023; 59(1): 149. CrossRef - Surgical management and outcomes of spinal metastasis of malignant adrenal tumor: A retrospective study of six cases and literature review
Xiangzhi Ni, Jing Wang, Jiashi Cao, Kun Zhang, Shuming Hou, Xing Huang, Yuanjin Song, Xin Gao, Jianru Xiao, Tielong Liu
Frontiers in Oncology.2023;[Epub] CrossRef - An adrenal incidentaloma that had appeared to produce dehydroepiandrosterone-sulfate in excess before immunohistochemical study of the tumor
Toshihide Yamamoto, Takuma Kimura, Yuki Kubo, Shin-ichi Nakatsuka, Hiromasa Harada, Takashi Suzuki, Hironobu Sasano
Endocrine Journal.2023; 70(1): 43. CrossRef - Mortality Not Increased in Patients With Nonfunctional Adrenal Adenomas: A Matched Cohort Study
Albin Kjellbom, Ola Lindgren, Malin Danielsson, Henrik Olsen, Magnus Löndahl
The Journal of Clinical Endocrinology & Metabolism.2023; 108(8): e536. CrossRef - Construction of a novel clinical nomogram to predict cancer-specific survival in patients with primary malignant adrenal tumors: a large population-based retrospective study
Mingzhen Li, Xiaoying Duan, Di You, Linlin Liu
Frontiers in Medicine.2023;[Epub] CrossRef - Primary Aldosteronism Prevalence – An Unfolding
Story
Suranut Charoensri, Adina F. Turcu
Experimental and Clinical Endocrinology & Diabetes.2023; 131(07/08): 394. CrossRef - Management of Adrenal Cortical Adenomas: Assessment of Bone Status in Patients with (Non-Functioning) Adrenal Incidentalomas
Alexandra-Ioana Trandafir, Mihaela Stanciu, Simona Elena Albu, Vasile Razvan Stoian, Irina Ciofu, Cristian Persu, Claudiu Nistor, Mara Carsote
Journal of Clinical Medicine.2023; 12(13): 4244. CrossRef - Clinical manifestations of functionally autonomous cortisol secretion in patients with adrenal masse
T. R. Chzhen, T. P. Kiseleva
Ural Medical Journal.2023; 22(3): 13. CrossRef - Tumor enlargement in adrenal incidentaloma is related to glaucoma: a new prognostic feature?
M. Caputo, T. Daffara, A. Ferrero, M. Romanisio, E. Monti, C. Mele, M. Zavattaro, S. Tricca, A. Siani, A. Clemente, C. Palumbo, S. De Cillà, A. Carriero, A. Volpe, P. Marzullo, G. Aimaretti, F. Prodam
Journal of Endocrinological Investigation.2023; 47(2): 377. CrossRef - Adrenal ganglioneuroma: Features and outcomes of cases series
Pei Li, Rongchang Zhang, Guang Wang, Jiongming Li
Asian Journal of Surgery.2023; 46(11): 5272. CrossRef - Recent Updates on the Management of Adrenal Incidentalomas
Seung Shin Park, Jung Hee Kim
Endocrinology and Metabolism.2023; 38(4): 373. CrossRef - Adrenal malakoplakia a rare lesion that mimics a neoplasm
Orión Erenhú Rodríguez González, Jesus Eduardo Osorio, Edgar Iván Bravo Castro
Urology Case Reports.2023; 51: 102568. CrossRef - LC-MS based simultaneous profiling of adrenal hormones of steroids, catecholamines, and metanephrines
Jongsung Noh, Chaelin Lee, Jung Hee Kim, Seung Woon Myung, Man Ho Choi
Journal of Lipid Research.2023; 64(11): 100453. CrossRef - Incidentaloma adrenal. Del hallazgo casual al diagnóstico definitivo
Mercedes Retamal Ortíz, Ana Belén Vicario Parada, Elena Vázquez Jarén
Actualización en Medicina de Familia.2023;[Epub] CrossRef - Diagnosis and management of adrenal incidentaloma: use of clinical judgment and evidence in dialog with the patient
Yusaku Yoshida, Kiyomi Horiuchi, Michio Otsuki, Takahiro Okamoto
Surgery Today.2023;[Epub] CrossRef - Can MDCT Enhancement Patterns Be Helpful in Differentiating Secretory from Non-Functional Adrenal Adenoma?
Svetlana Kocic, Vladimir Vukomanovic, Aleksandar Djukic, Jovica Saponjski, Dusan Saponjski, Vuk Aleksic, Vesna Ignjatovic, Katarina Vuleta Nedic, Vladan Markovic, Radisa Vojinovic
Medicina.2023; 60(1): 72. CrossRef - Computer-assisted Reporting and Decision Support Increases Compliance with Follow-up Imaging and Hormonal Screening of Adrenal Incidentalomas
Renata R. Almeida, Bernardo C. Bizzo, Ramandeep Singh, Katherine P. Andriole, Tarik K. Alkasab
Academic Radiology.2022; 29(2): 236. CrossRef - Incidental Adrenal Masses: Adherence to Guidelines and Methods to Improve Initial Follow-Up: A Systematic Review
Timothy Feeney, Andrea Madiedo, Philip E. Knapp, Avneesh Gupta, David McAneny, Frederick Thurston Drake
Journal of Surgical Research.2022; 269: 18. CrossRef - Incidental Adrenal Lesions May Not Always Require Further Imaging Work-up
Deborah A. Baumgarten
Radiology.2022; 302(1): 138. CrossRef - Adrenal Nodules Detected at Staging CT in Patients with Resectable Gastric Cancers Have a Low Incidence of Malignancy
Hae Young Kim, Won Chang, Yoon Jin Lee, Ji Hoon Park, Jungheum Cho, Hee Young Na, Hyungwoo Ahn, Sung Il Hwang, Hak Jong Lee, Young Hoon Kim, Kyoung Ho Lee
Radiology.2022; 302(1): 129. CrossRef - Management of incidental adrenal nodules: a survey of abdominal radiologists conducted by the Society of Abdominal Radiology Disease-Focused Panel on Adrenal Neoplasms
Michael T. Corwin, Nicola Schieda, Erick M. Remer, Elaine M. Caoili
Abdominal Radiology.2022; 47(4): 1360. CrossRef - Primary hyperaldosteronism: indications for screening
Novella M. Chikhladze
Terapevticheskii arkhiv.2022; 94(1): 107. CrossRef - Pathophysiological Link between Insulin Resistance and Adrenal Incidentalomas
Jordan A. Higgs, Alyssa P. Quinn, Kevin D. Seely, Zeke Richards, Shad P. Mortensen, Cody S. Crandall, Amanda E. Brooks
International Journal of Molecular Sciences.2022; 23(8): 4340. CrossRef - Can Radiomics Provide Additional Diagnostic Value for Identifying Adrenal Lipid-Poor Adenomas From Non-Adenomas on Unenhanced CT?
Binhao Zhang, Huangqi Zhang, Xin Li, Shengze Jin, Jiawen Yang, Wenting Pan, Xue Dong, Jin Chen, Wenbin Ji
Frontiers in Oncology.2022;[Epub] CrossRef - Adrenal Surgery in the Era of Multidisciplinary Endocrine Tumor
Boards
Costanza Chiapponi, Daniel Pinto Dos Santos, Milan Janis Michael Hartmann, Matthias Schmidt, Michael Faust, Roger Wahba, Christiane Josephine Bruns, Anne Maria Schultheis, Hakan Alakus
Hormone and Metabolic Research.2022; 54(05): 294. CrossRef - Optimal and novel imaging of the adrenal glands
Patrick J. Navin, Michael R. Moynagh
Current Opinion in Endocrinology, Diabetes & Obesity.2022; 29(3): 253. CrossRef - Adrenal Tumors in Young Adults: Case Reports and Literature Review
Małgorzata Zdrojewska, Emilia Mech-Siebieszuk, Renata Świątkowska-Stodulska, Bartosz Regent, Michał Kunc, Łukasz Zdrojewski, Krzysztof Sworczak
Medicina.2022; 58(6): 746. CrossRef - Incidence of malignancy in adrenal nodules detected on staging CTs of patients with potentially resectable colorectal cancer
Hae Young Kim, Yoon Jin Lee, Won Chang, Ji Hoon Park, Jungheum Cho, Hyeon Jeong Oh, Young Hoon Kim, Kyoung Ho Lee
European Radiology.2022; 32(12): 8560. CrossRef - Appendiceal Incidentalomas: Prevalence, Radiographic Characteristics, Management, and Outcomes
Adam Kelly, Stacy O’Connor, Diana Kane, Chiang-Ching Huang, Harveshp Mogal
Annals of Surgical Oncology.2022; 29(13): 8265. CrossRef - Laparoscopic large adrenal mass resection: why we should be more careful?
Mohsen Varyani, Mahmood Parvin, Hamidreza Akbari Gilani
African Journal of Urology.2022;[Epub] CrossRef - Serum Visfatin/NAMPT as a Potential Risk Predictor for Malignancy of Adrenal Tumors
Nadia Sawicka-Gutaj, Hanna Komarowska, Dawid Gruszczyński, Aleksandra Derwich, Anna Klimont, Marek Ruchała
Journal of Clinical Medicine.2022; 11(19): 5563. CrossRef - Application of radiomics in adrenal incidentaloma: a literature review
Cheng Li, Yan Fu, Xiaoping Yi, Xiao Guan, Longfei Liu, Bihong T. Chen
Discover Oncology.2022;[Epub] CrossRef - Hormone-inactive adrenal tumors in clinician’s practice
T. R. Chzhen, T. P. Kiseleva
Perm Medical Journal.2022; 39(5): 48. CrossRef - The diagnostic value of salivary cortisol and salivary cortisone in patients with suspected hypercortisolism
Vendela Berndt, Per Dahlqvist, Jennie de Verdier, Henrik Ryberg, Oskar Ragnarsson
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Role of Intraoperative Indocyanine Green (ICG) and Preoperative 3-Dimensional (3D) Reconstruction in Laparoscopic Adrenalectomy: A Propensity Score-matched Analysis
Giuseppe Palomba, Vincenza Paola Dinuzzi, Francesca Pegoraro, Roberto Ivan Troisi, Roberto Montalti, Giovanni Domenico De Palma, Giovanni Aprea
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2022; 32(6): 643. CrossRef - The Etiological Profile of Adrenal Incidentalomas
Fatima-Zahra Lahmamssi, Loubna Saadaoui, Hayat Aynaou, Houda Salhi, Hanan El Ouahabi
Cureus.2022;[Epub] CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - Conduite à tenir face à un fortuitome surrénalien chez le chien ou le chat
Diane Pichard, Ghita Benckekroun
Le Nouveau Praticien Vétérinaire canine & féline.2022; 19(82): 40. CrossRef - Laparoscopic transperitoneal adrenalectomy: a comparative study of different techniques for vessel sealing
Luca Cardinali, Edlira Skrami, Elisa Catani, Flavia Carle, Monica Ortenzi, Andrea Balla, Mario Guerrieri
Surgical Endoscopy.2021; 35(2): 673. CrossRef - Epidemiology and Comorbidity of Adrenal Cushing Syndrome: A Nationwide Cohort Study
Chang Ho Ahn, Jung Hee Kim, Man Young Park, Sang Wan Kim
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): e1362. CrossRef - Urine steroid profile as a new promising tool for the evaluation of adrenal tumors. Literature review
Marta Araujo-Castro, Pablo Valderrábano, Héctor F. Escobar-Morreale, Felicia A. Hanzu, Gregori Casals
Endocrine.2021; 72(1): 40. CrossRef - A Rare Neoplasm: Primary Adrenal Leiomyosarcoma
Jack T. Barnett, Christine W. Liaw, Reza Mehrazin
Urology.2021; 148: e11. CrossRef - Adrenal Ganglioneuroma Presenting as an Incidentaloma in an Adolescent Patient
Sonia G. Sharma, Steven N. Levine, Xin Gu
AACE Clinical Case Reports.2021; 7(1): 61. CrossRef - Feasibility of Iodine-131 6β-Methyl-Iodo-19 Norcholesterol (NP-59) Scintigraphy to Complement Adrenal Venous Sampling in Management of Primary Aldosteronism: A Case Series
Jeongmin Lee, Jeonghoon Ha, Sang-Kuon Lee, Hye Lim Park, Sung-Hoon Kim, Dong-Jun Lim, Jung Min Lee, Sang-Ah Chang, Moo Il Kang, Min-Hee Kim
International Journal of General Medicine.2021; Volume 14: 673. CrossRef - Best Achievements in Pituitary and Adrenal Diseases in 2020
Chang Ho Ahn, Jung Hee Kim
Endocrinology and Metabolism.2021; 36(1): 51. CrossRef - Adrenal surgery: Review of 35 years experience in a single centre
Enrico Battistella, Stefania Ferrari, Luca Pomba, Antonio Toniato
Surgical Oncology.2021; 37: 101554. CrossRef - Adrenocortical Carcinoma: A Case of Missed Diagnosis
Yusef Hazimeh, Carlie Sigel, Carsello Carie, Mathew Leinung, Zaynab Khalaf
Cureus.2021;[Epub] CrossRef - Imagerie fonctionnelle en endocrinologie : nouveaux paradigmes à l’horizon 2020
E. Marchal
Médecine Nucléaire.2021; 45(3): 158. CrossRef - Adrenal Incidentaloma
Caren G. Solomon, Electron Kebebew
New England Journal of Medicine.2021; 384(16): 1542. CrossRef - Can Hematological Parameters Play a Role in the Differential Diagnosis of Adrenal Tumors?
Mehmet Gürkan Arıkan, Göktan Altuğ Öz, Nur Gülce İşkan, Necdet Süt, İlkan Yüksel, Ersan Arda
Uro.2021; 1(2): 39. CrossRef - Incidental Adrenal Nodules
Daniel I. Glazer, Michael T. Corwin, William W. Mayo-Smith
Radiologic Clinics of North America.2021; 59(4): 591. CrossRef - Antioxidant Barrier and Oxidative Damage to Proteins, Lipids, and DNA/RNA in Adrenal Tumor Patients
Barbara Choromańska, Piotr Myśliwiec, Tomasz Kozłowski, Magdalena Łuba, Piotr Wojskowicz, Jacek Dadan, Hanna Myśliwiec, Katarzyna Choromańska, Anna Gibała, Anna Starzyńska, Małgorzata Żendzian-Piotrowska, Anna Zalewska, Mateusz Maciejczyk, Jos L. Quiles
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Laparoscopic Retroperitoneoscopic Removal of an Adrenal Hemangioma: a Case Report
Kristin McCoy, Katherine Howe, Daniel Tershak
Journal of Endocrine Surgery.2021; 21(3): 70. CrossRef - Metabolic Subtyping of Adrenal Tumors: Prospective Multi-Center Cohort Study in Korea
Eu Jeong Ku, Chaelin Lee, Jaeyoon Shim, Sihoon Lee, Kyoung-Ah Kim, Sang Wan Kim, Yumie Rhee, Hyo-Jeong Kim, Jung Soo Lim, Choon Hee Chung, Sung Wan Chun, Soon-Jib Yoo, Ohk-Hyun Ryu, Ho Chan Cho, A Ram Hong, Chang Ho Ahn, Jung Hee Kim, Man Ho Choi
Endocrinology and Metabolism.2021; 36(5): 1131. CrossRef - Cross-Talk Between Nitrosative Stress, Inflammation and Hypoxia-Inducible Factor in Patients with Adrenal Masses
Barbara Choromańska, Piotr Myśliwiec, Tomasz Kozłowski, Magdalena Łuba, Piotr Wojskowicz, Jacek Dadan, Hanna Myśliwiec, Katarzyna Choromańska, Katarzyna Makarewicz, Anna Zalewska, Mateusz Maciejczyk
Journal of Inflammation Research.2021; Volume 14: 6317. CrossRef - Cirugía laparoscópica en incidentaloma suprarrenal para el cirujano general: serie de casos
Martín Adrián Bolívar-Rodríguez, Marcel Antonio Cázarez-Aguilar, Pedro Alejandro Magaña-Zavala, Francisco Magaña-Olivas, José Martín Niebla-Moreno
Revista Mexicana de Cirugía Endoscópica.2021; 22(1): 8. CrossRef - Adrenal adenomas: what to do with them? Review 2
S. Rybakov
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(3): 241. CrossRef - Is Follow-up of Adrenal Incidentalomas Always Mandatory?
Giuseppe Reimondo, Alessandra Muller, Elisa Ingargiola, Soraya Puglisi, Massimo Terzolo
Endocrinology and Metabolism.2020; 35(1): 26. CrossRef - Imaging Findings of Primary Adrenal Leiomyosarcoma: A Case Report
Hye Ran Yoon, Dong Hee Park
Journal of the Korean Society of Radiology.2020; 81(2): 459. CrossRef - WFUMB position paper on the management incidental findings: adrenal incidentaloma
Christoph F. Dietrich, Jean Michel Correas, Yi Dong, Christian Nolsoe, Susan Campbell Westerway, Christian Jenssen
Ultrasonography.2020; 39(1): 11. CrossRef - A nationwide survey of adrenal incidentalomas in Japan: the first report of clinical and epidemiological features
Takamasa Ichijo, Hajime Ueshiba, Hajime Nawata, Toshihiko Yanase
Endocrine Journal.2020; 67(2): 141. CrossRef - Mimics, pitfalls, and misdiagnoses of adrenal masses on CT and MRI
Khaled M. Elsayes, Mohab M. Elmohr, Sanaz Javadi, Christine O. Menias, Erick M. Remer, Ajaykumar C. Morani, Akram M. Shaaban
Abdominal Radiology.2020; 45(4): 982. CrossRef - Adrenal Incidentaloma
Mark Sherlock, Andrew Scarsbrook, Afroze Abbas, Sheila Fraser, Padiporn Limumpornpetch, Rosemary Dineen, Paul M Stewart
Endocrine Reviews.2020; 41(6): 775. CrossRef - A Web Application for Adrenal Incidentaloma Identification, Tracking, and Management Using Machine Learning
Wasif Bala, Jackson Steinkamp, Timothy Feeney, Avneesh Gupta, Abhinav Sharma, Jake Kantrowitz, Nicholas Cordella, James Moses, Frederick Thurston Drake
Applied Clinical Informatics.2020; 11(04): 606. CrossRef - Presentation and outcome of patients with an adrenal mass: A retrospective observational study
Nadeema Rafiq, Tauseef Nabi, SajadAhmad Dar, Shahnawaz Rasool
Clinical Cancer Investigation Journal.2020; 9(5): 198. CrossRef - Evaluation of Functionality and Growth Rates in Adrenal Incidentalomas: Single Center Experience
Suna AVCI, Yüksel Aslı OZTURKMEN, Sayid ZUHUR, Gulkan OZKAN, Elif GUVEN, Nazan DEMİR, Yuksel ALTUNTAS
Phoenix Medical Journal.2020; 2(3): 125. CrossRef - Percutaneous Adrenal Radiofrequency Ablation: A Short Review for Endocrinologists
Byung Kwan Park
Endocrinology and Metabolism.2020; 35(4): 750. CrossRef - Autonomous cortisol secretion in adrenal incidentalomas
Marta Araujo-Castro, Miguel Antonio Sampedro Núñez, Mónica Marazuela
Endocrine.2019; 64(1): 1. CrossRef - Primary adrenal schwannoma: a series of 31 cases emphasizing their clinicopathologic features and favorable prognosis
Jun Zhou, Dandan Zhang, Wencai Li, Luting Zhou, Haimin Xu, Saifang Zheng, Chaofu Wang
Endocrine.2019; 65(3): 662. CrossRef - Challenging risk factors for right and left laparoscopic adrenalectomy: A single centre experience with 272 cases
Kadir Omur Gunseren, Mehmet Cagatay Cicek, Hakan Vuruskan, Yakup Kordan, Ismet Yavascaoglu
International braz j urol.2019; 45(4): 747. CrossRef - A case report on 111In chloride bone marrow scintigraphy in management of adrenal myelolipoma
Tatsuya Yamamoto, Mitsuru Koizumi, Atsushi Kohno, Noboru Numao, Kentaro Inamura
Medicine.2019; 98(8): e14625. CrossRef - PRACTICAL ASPECTS OF LAPAROSCOPIC ADRENALECTOMY IN CHILDREN WITH BENIGN ADRENAL TUMORS
I. V. Poddubny, R. S. Oganesyan, K. N. Tolstov, M. A. Kareva
Russian Journal of Pediatric Surgery.2019; 23(5): 248. CrossRef - Incidental neuroblastoma with bilateral retinoblastoma: what are the chances?
Kelsey Roelofs, Furqan Shaikh, William Astle, Brenda L. Gallie, Sameh E. Soliman
Ophthalmic Genetics.2018; 39(3): 410. CrossRef - Surgical Considerations in Subclinical Cushing’s Syndrome. When is it Time to Operate?
Alexander M. Nixon, C Aggeli, C Tserkezis, GN Zografos
Hellenic Journal of Surgery.2018; 90(1): 27. CrossRef - Adrenal incidentaloma – diagnostic and treating problem – own experience
Ryszard Pogorzelski, Krzysztof Celejewski, Sadegh Toutounchi, Ewa Krajewska, Tomasz Wołoszko, Małgorzata Szostek, Wawrzyniec Jakuczun, Patryk Fiszer, Małgorzata Legocka, Zbigniew Gałązka
Open Medicine.2018; 13(1): 281. CrossRef
- The improvement of postoperative blood pressure and associated factors in patients with hormone‐negative adrenal adenoma and hypertension

- Thyroid
- The Revised 2016 Korean Thyroid Association Guidelines for Thyroid Nodules and Cancers: Differences from the 2015 American Thyroid Association Guidelines
- Ka Hee Yi
- Endocrinol Metab. 2016;31(3):373-378. Published online September 26, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.373
- 7,350 View
- 177 Download
- 90 Web of Science
- 85 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Increased detection of thyroid nodules using high-resolution ultrasonography has resulted in a world-wide increase in the incidence of differentiated thyroid cancer (DTC). Despite the steep increase in its incidence, the age-standardized mortality rate of thyroid cancer has remained stable, which leads toward a trend of more conservative treatment. The latest American Thyroid Association (ATA) guidelines for thyroid nodules and thyroid cancer revised in 2015 suggested that fine needle aspiration biopsy should be performed for thyroid nodules larger than 1 cm and lobectomy might be sufficient for 1 to 4 cm intrathyroidal DTC. In addition, active surveillance instead of immediate surgical treatment was also recommended as a treatment option for papillary thyroid microcarcinoma based on the results of a few observational studies from Japan. The Korean Thyroid Association (KTA) has organized a task force team to develop revised guidelines for thyroid nodules and DTC after an extensive review of articles and intense discussion on whether we should accept the changes in the 2015 ATA guidelines. This paper introduces and discusses the updated major issues and differences in the ATA and the KTA guidelines.
-
Citations
Citations to this article as recorded by- Intraoperative pathologic evaluation of central compartment lymph nodes in patients undergoing lobectomy for unilateral papillary thyroid carcinoma
Hye Lim Bae, Jong-hyuk Ahn, JungHak Kwak, Hyun Soo Kim, Sang Gab Yoon, Jin Wook Yi, Su-jin Kim, Kyu Eun Lee
Asian Journal of Surgery.2024; 47(1): 360. CrossRef - Global scientific trends on thyroid disease in early 21st century: a bibliometric and visualized analysis
Mingyuan Song, Wei Sun, Qi Liu, Zhongqing Wang, Hao Zhang
Frontiers in Endocrinology.2024;[Epub] CrossRef - A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - Lowering Barriers to Health Risk Assessments in Promoting Personalized Health Management
Hayoung Park, Se Young Jung, Min Kyu Han, Yeonhoon Jang, Yeo Rae Moon, Taewook Kim, Soo-Yong Shin, Hee Hwang
Journal of Personalized Medicine.2024; 14(3): 316. CrossRef - Clinicopathological Features and Molecular Signatures of Lateral Neck Lymph Node Metastasis in Papillary Thyroid Microcarcinoma
Jinsun Lim, Han Sai Lee, Jin-Hyung Heo, Young Shin Song
Endocrinology and Metabolism.2024; 39(2): 324. CrossRef - Prognostic Utility of Tumor Stage versus American Thyroid Association Risk Class in Thyroid Cancer
Arash Abiri, Jonathan Pang, Karthik R. Prasad, Khodayar Goshtasbi, Edward C. Kuan, William B. Armstrong, Yarah M. Haidar, Tjoson Tjoa
The Laryngoscope.2023; 133(1): 205. CrossRef - Active surveillance for PTMC warranted for the UK population?
Pavithran Maniam, Noah Harding, Lucy Li, Richard Adamson, Ashley Hay, Ian Nixon
Clinical Otolaryngology.2023; 48(1): 88. CrossRef - Cost-effectiveness of active surveillance versus early surgery for thyroid micropapillary carcinoma based on diagnostic and treatment norms in China
Min Lai, Miao Miao Zhang, Qing Qing Qin, Yu An, Yan Ting Li, Wen Zhen Yuan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biopsy strategies for intermediate and high suspicion thyroid nodules with macrocalcifications
Sungmok Kim, Jae Ho Shin, Yon Kwon Ihn
Current Medical Research and Opinion.2023; 39(2): 179. CrossRef - Active surveillance versus immediate surgery: A comparison of clinical and quality of life outcomes among patients with highly suspicious thyroid nodules 1 cm or smaller in China
Chunhao Liu, Hao Zhao, Yu Xia, Yue Cao, Liyang Zhang, Ya Zhao, Luying Gao, Ruifeng Liu, Yuewu Liu, Hongfeng Liu, Zhilan Meng, Shuzhou Liu, Ying Lu, Xiaoyi Li
European Journal of Surgical Oncology.2023; 49(9): 106917. CrossRef - SThy-Net: a feature fusion-enhanced dense-branched modules network for small thyroid nodule classification from ultrasound images
Abdulrhman H. Al-Jebrni, Saba Ghazanfar Ali, Huating Li, Xiao Lin, Ping Li, Younhyun Jung, Jinman Kim, David Dagan Feng, Bin Sheng, Lixin Jiang, Jing Du
The Visual Computer.2023; 39(8): 3675. CrossRef - Response to Letter to the Editor on Surgical Outcomes in Patients With Low-Risk Papillary Thyroid Microcarcinoma From MAeSTro Study: Immediate Operation Versus Delayed Operation Following Active Surveillance: A Multicenter Prospective Cohort Study
Hyeonuk Hwang, June Young Choi, Jae Hoon Moon, Eun Kyung Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jung
Annals of Surgery Open.2023; 4(3): e311. CrossRef - The Association of Pregnancy with Disease Progression in Patients Previously Treated for Differentiated Thyroid Cancer: A Propensity Score-Matched Retrospective Cohort Study
Xin Li, Wu-Cai Xiao, Fang Mei, Rui Shan, Shi-Bing Song, Bang-Kai Sun, He-Ling Bao, Jing Chen, Chun-Hui Yuan, Zheng Liu
Journal of Women's Health.2023; 32(11): 1174. CrossRef - Mortality rate and causes of death in papillary thyroid microcarcinoma
Jung Heo, Hyun Jin Ryu, Hyunju Park, Tae Hyuk Kim, Sun Wook Kim, Young Lyun Oh, Jae Hoon Chung
Endocrine.2023; 83(3): 671. CrossRef - Surgical Outcomes in Patients With Low-risk Papillary Thyroid Microcarcinoma From MAeSTro Study
Hyeonuk Hwang, June Young Choi, Hyeong Won Yu, Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Yeo Koon Kim, Chang Yoon Lee, Sun Wook Cho, Eun-Jae Chung, Chang Hwan Ryu, Junsun Ryu, Ka Hee Yi, Do Joon Park, Kyu Eun Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jun
Annals of Surgery.2023; 278(5): e1087. CrossRef - US Predictors of Papillary Thyroid Microcarcinoma Progression at Active Surveillance
Ji Ye Lee, Ji-hoon Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Jae Hoon Moon, Hoon Sung Choi, Hwangbo Yul, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Do Joon Park, Young Joo Park
Radiology.2023;[Epub] CrossRef - Bilaterality as a Risk Factor for Recurrence in Papillary Thyroid Carcinoma
Hyeji Kim, Hyungju Kwon
Cancers.2023; 15(22): 5414. CrossRef - Clinical and molecular genetic analysis of cytologically uncertain thyroid nodules in patients with thyroid disease
Jindrich Lukas, Barbora Hintnausova, Vlasta Sykorova, Martin Syrucek, Marek Maly, David Lukas, Jaroslava Duskova
Biomedical Papers.2023;[Epub] CrossRef - Thyroid Papillary Microcarcinoma - Carcinoma with Clinically Benign Behaviour
Hitesh R Singhavi, Manish Mair, Burhanuddin Qayyumi, Arjun Singh, Pankaj Chaturvedi
Journal of Head & Neck Physicians and Surgeons.2023; 11(2): 95. CrossRef - Trends in Diagnosis of Noninvasive Follicular Thyroid Neoplasm With Papillarylike Nuclear Features and Total Thyroidectomies for Patients With Papillary Thyroid Neoplasms
Lisa Caulley, Antoine Eskander, Weining Yang, Edel Auh, Lydia Cairncross, Nancy L. Cho, Bahar Golbon, Subramania Iyer, Jeffrey C. Liu, Paul J. Lee, Brenessa Lindeman, Charles Meltzer, Nicole Molin, Alessandra Moore, Julia Noel, Halie Nozolino, Jesse Paste
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(2): 99. CrossRef - What's in a Name? A Cost-Effectiveness Analysis of the Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features' Nomenclature Revision
Vikas Mehta, Ankita Naraparaju, David Liao, Louise Davies, Bryan R. Haugen, Peter A. Kopp, Susan J. Mandel, Yuri E. Nikiforov, Douglas S. Ross, Jennifer J. Shin, R. Michael Tuttle, Gregory W. Randolph
Thyroid.2022; 32(4): 421. CrossRef - Clinical management of low-risk papillary thyroid microcarcinoma
Chie MASAKI, Kiminori SUGINO, Koichi ITO
Minerva Endocrinology.2022;[Epub] CrossRef - Can Active Surveillance Management be Developed for Patients With Low-Risk Papillary Thyroid Microcarcinoma? A Preliminary Investigation in a Chinese Population
Wen Liu, Weihan Cao, Zhizhong Dong, Ruochuan Cheng
Endocrine Practice.2022; 28(4): 391. CrossRef - Assessment of Radiofrequency Ablation for Papillary Microcarcinoma of the Thyroid
Sam P. J. van Dijk, Hannelore I. Coerts, Sabrina T. G. Gunput, Evert F. S. van Velsen, Marco Medici, Adriaan Moelker, Robin P. Peeters, Cornelis Verhoef, Tessa M. van Ginhoven
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(4): 317. CrossRef - The Future of Thyroid Nodule Risk Stratification
Nydia Burgos, Naykky Singh Ospina, Jennifer A. Sipos
Endocrinology and Metabolism Clinics of North America.2022; 51(2): 305. CrossRef - Complication Rates of Total Thyroidectomy vs Hemithyroidectomy for Treatment of Papillary Thyroid Microcarcinoma
Vivian Hsiao, Tyler J. Light, Abdullah A. Adil, Michael Tao, Alexander S. Chiu, Mary Hitchcock, Natalia Arroyo, Sara Fernandes-Taylor, David O. Francis
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(6): 531. CrossRef - Malignancy risk stratification of thyroid nodules smaller than 10 mm with ACR-TIRADS, K-TIRADS, and ATA-2015 guidelines: a prospective study
Mehrdad Nabahati, Zoleika Moazezi
Egyptian Journal of Radiology and Nuclear Medicine.2022;[Epub] CrossRef - Thyroglobulin-Based Risk Factor Repositioning for Determining Radioactive Iodine Activity in Patients with Papillary Thyroid Carcinoma: a Multicenter Retrospective Cohort Study
Subin Jeon, Seong Young Kwon, Sang-Woo Lee, Sang Kyun Bae
Nuclear Medicine and Molecular Imaging.2022; 56(4): 173. CrossRef - Quality of Life of Survivors of Thyroid Cancer Is Not Inferior to That in Subjects without Cancer: Long-Term after Over 5 Years
Jeongmin Lee, Youn-Ju Lee, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Min-Hee Kim
Endocrinology and Metabolism.2022; 37(4): 664. CrossRef - Residual, regrowth, and new growth of radiofrequency ablation for benign thyroid nodules of different volumes: two-year follow-up results
Meng-Hsiang Chen, Wei-Che Lin, Sheng-Dean Luo, Pi-Ling Chiang, Yueh-Sheng Chen, Wei-Chih Chen, An-Ni Lin, Cheng-Kang Wang, Jung-Hwan Baek, Hsiu-Ling Chen
International Journal of Hyperthermia.2022; 39(1): 1172. CrossRef - Progression of Low-Risk Papillary Thyroid Microcarcinoma During Active Surveillance: Interim Analysis of a Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma in Korea
Eun Kyung Lee, Jae Hoon Moon, Yul Hwangbo, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Woo-Jin Jeong, Yuh-Seog Jung, Junsun Ryu, Su-jin Kim, Min Joo Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, Hyeong Won Yu, Jeong Hun Hah, Kyu Eun Lee,
Thyroid.2022; 32(11): 1328. CrossRef - Recent Changes in the Incidence of Thyroid Cancer in Korea between 2005 and 2018: Analysis of Korean National Data
Yun Mi Choi, Jiwoo Lee, Mi Kyung Kwak, Min Ji Jeon, Tae Yong Kim, Eun-Gyoung Hong, Won Bae Kim, Won Gu Kim
Endocrinology and Metabolism.2022; 37(5): 791. CrossRef - Strain Versus 2D Shear-Wave Elastography Parameters—Which Score Better in Predicting Thyroid Cancer?
Andreea Borlea, Ioan Sporea, Alexandru Popa, Mihnea Derban, Laura Taban, Dana Stoian
Applied Sciences.2022; 12(21): 11147. CrossRef - Estimating the risk of completion total thyroidectomy using real-world data to guide initial surgical decision-making for patients with clinical low-risk papillary thyroid carcinoma
Wen Liu, Xiangxiang Zhan, Zhizhong Dong, Yanjun Su, Jianming Zhang, Jun Qian, Yunhai Ma, Chang Diao, Ruochuan Cheng
Holistic Integrative Oncology.2022;[Epub] CrossRef - Rigorous radiofrequency ablation can completely treat low-risk small papillary thyroid carcinoma without affecting subsequent surgical management
Xinyang Li, Jie Li, Zhi Qiao, Lin Yan, Jing Xiao, Yingying Li, Mingbo Zhang, Yukun Luo
European Radiology.2022; 33(6): 4189. CrossRef - Whirling technique for thyroid fine needle aspiration biopsy: a preliminary study of effectiveness and safety
Jae Ho Shin, Seung Wan Han, Hyang Lim Lee, Yon Kwon Ihn
Ultrasonography.2021; 40(1): 147. CrossRef - Value of dual-phase, contrast-enhanced CT combined with ultrasound for the diagnosis of metastasis to central lymph nodes in patients with papillary thyroid cancer
Ying Liu, Sheng Li, Cuiju Yan, Caiyun He, Miao Yun, Min Liu, Jianhua Zhou, Longzhong Liu
Clinical Imaging.2021; 75: 5. CrossRef - Clinical outcomes of T4a papillary thyroid cancer with recurrent laryngeal nerve involvement: a retrospective analysis
Han-Seul Na, Hyun-Keun Kwon, Sung-Chan Shin, Yong-Il Cheon, Myeonggu Seo, Jin-Choon Lee, Eui-Suk Sung, Minhyung Lee, In-Joo Kim, Bo Hyun Kim, Byung-Joo Lee
Scientific Reports.2021;[Epub] CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef - Thyroid nodules in childhood‐onset Hashimoto's thyroiditis: Frequency, risk factors, follow‐up course and genetic alterations of thyroid cancer
Yun Jeong Lee, Yeon Jin Cho, You Joung Heo, Eun‐Jae Chung, Young Hun Choi, Jong‐Il Kim, Young Joo Park, Choong Ho Shin, Young Ah Lee
Clinical Endocrinology.2021; 95(4): 638. CrossRef - Clinical implications of age and excellent response to therapy in patients with high‐risk differentiated thyroid carcinoma
Meihua Jin, Jonghwa Ahn, Yu‐Mi Lee, Tae‐Yon Sung, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jin‐Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Won Gu Kim
Clinical Endocrinology.2021; 95(6): 882. CrossRef - Ecografía clínica de la glándula tiroides y del cuello
Pepa Bertrán Culla, David Teixidó Gimeno, Pere Guirado Vila
FMC - Formación Médica Continuada en Atención Primaria.2021; 28(7): 390. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef - Clinical Effects of Microwave Ablation in the Treatment of Low-Risk Papillary Thyroid Microcarcinomas and Related Histopathological Changes
Chenya Lu, Xingjia Li, Xiaoqiu Chu, Ruiping Li, Jie Li, Jianhua Wang, Yalin Wang, Yang Xu, Guofang Chen, Shuhang Xu, Chao Liu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Optimization of follow-up in patients with papillary thyroid cancer who show no evidence of disease 9–12 months after treatment
Fabian Nordell, Ghadir Hallal, Pernilla Asp, Martin Almquist
BJS Open.2021;[Epub] CrossRef - The most reliable time point for intact parathyroid hormone measurement to predict hypoparathyroidism after total thyroidectomy with central neck dissection to treat papillary thyroid carcinoma: a prospective cohort study
Jae Won Chang, Ki Wan Park, Seung-Nam Jung, Lihua Liu, Sung Min Kim, Bon Seok Koo
European Archives of Oto-Rhino-Laryngology.2020; 277(2): 549. CrossRef - Time Trends for Prostate Cancer Incidence from 2003 to 2013 in South Korea: An Age-Period-Cohort Analysis
Hyun Young Lee, Do Kyoung Kim, Seung Whan Doo, Won Jae Yang, Yun Seob Song, Bora Lee, Jae Heon Kim
Cancer Research and Treatment.2020; 52(1): 301. CrossRef - Clinical behavior and outcome of papillary T1 thyroid cancers: South Korea vs. Turkey vs. Colombia in a cohort study analyzing oncological outcomes
Murat Ozdemir, Yong-Sang Lee, Ozer Makay, Juan Pablo Dueñas, Bulent Yazici, Aysegul Akgun, Gokhan Icoz, Mahir Akyildiz, Soo Young Kim, Seok-Mo Kim, Hojin Chang, Hang-Seok Chang, Cheong Soo Park
Asian Journal of Surgery.2020; 43(8): 795. CrossRef - Radioiodine ablation in thyroid cancer patients: renal function and external radiation dose rate at discharge according to patient preparation
Yeon-Hee Han, Hwan-Jeong Jeong, Myung-Hee Sohn, Sun Y. Lee, Seok T. Lim
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2020;[Epub] CrossRef - Effect of the location and size of thyroid nodules on the diagnostic performance of ultrasound elastography: A retrospective analysis
Xinxin Xie, Yongqiang Yu
Clinics.2020; 75: e1720. CrossRef Fine-Needle Aspiration of Subcentimeter Thyroid Nodules in the Real-World Management
Chaiho Jeong, Hyunsam Kim, Jeongmin Lee, Jeonghoon Ha, Min-Hee Kim, Moo Il Kang, Dong-Jun Lim
Cancer Management and Research.2020; Volume 12: 7611. CrossRef- Continuing controversy regarding individualized surgical decision-making for patients with 1–4 cm low-risk differentiated thyroid carcinoma: A systematic review
Wen Liu, Xuejing Yan, Ruochuan Cheng
European Journal of Surgical Oncology.2020; 46(12): 2174. CrossRef - Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2020; 35(3): 618. CrossRef - Clinical Outcomes of N1b Papillary Thyroid Cancer Patients Treated with Two Different Doses of Radioiodine Ablation Therapy
Meihua Jin, Jonghwa Ahn, Yu-Mi Lee, Tae-Yon Sung, Won Gu Kim, Tae Yong Kim, Jin-Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon
Endocrinology and Metabolism.2020; 35(3): 602. CrossRef - A Propensity Score‐matched Comparison Study of Surgical Outcomes in Patients with Differentiated Thyroid Cancer After Robotic Versus Open Total Thyroidectomy
Dong Sik Bae, Do Hoon Koo
World Journal of Surgery.2019; 43(2): 540. CrossRef - Diagnostic value of cytology, thyroglobulin, and combination of them in fine-needle aspiration of metastatic lymph nodes in patients with differentiated thyroid cancer
Yixin Xu, Dapeng Wu, Wenting Wu, Jian Jiang, Cheng Xi, Nianyuan Ye, Yibo Wang, Xuezhong Xu
Medicine.2019; 98(45): e17859. CrossRef - Investigation of blood groups in benign thyroid diseases in Turkey
Murat Dağdeviren, İhsan Ateş, Burak Furkan Demir, Emine Ergün, Canan Yıldız, Mustafa Altay
Endocrine Journal.2019; 66(11): 1001. CrossRef - Tumor Volume Doubling Time in Active Surveillance of Papillary Thyroid Carcinoma
Hye-Seon Oh, Hyemi Kwon, Eyun Song, Min Ji Jeon, Tae Yong Kim, Jeong Hyun Lee, Won Bae Kim, Young Kee Shong, Ki-Wook Chung, Jung Hwan Baek, Won Gu Kim
Thyroid.2019; 29(5): 642. CrossRef - Tumor doubling time predicts response to sorafenib in radioactive iodine-refractory differentiated thyroid cancer
Min Joo Kim, Seok-Mo Kim, Eun Kyung Lee, Yul Hwangbo, You Jin Lee, Sun Wook Cho, Do Joon Park, Yumi Lee, Young Joo Park
Endocrine Journal.2019; 66(7): 597. CrossRef - Total thyroidectomy's association with survival in papillary thyroid cancers and the high proportion of total thyroidectomy in low-risk patients: Analysis of Korean nationwide data
Hyun-Soo Zhang, Eun-Kyung Lee, Yuh-Seog Jung, Byung-Ho Nam, Kyu-Won Jung, Hyun-Joo Kong, Young-Joo Won, Boyoung Park
Surgery.2019; 165(3): 629. CrossRef - Individualized Follow-Up Strategy for Patients with an Indeterminate Response to Initial Therapy for Papillary Thyroid Carcinoma
Hye-Seon Oh, Jong Hwa Ahn, Eyun Song, Ji Min Han, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon
Thyroid.2019; 29(2): 209. CrossRef - Differentiated Thyroid Cancer and Radioactive Iodine: Past, Present and Future
Jaetae Lee, Il Jo
International Journal of Thyroidology.2019; 12(2): 71. CrossRef - Diagnostic performance of HMGA2 gene expression for differentiation of malignant thyroid nodules: A systematic review and meta‐analysis
Bo Hyun Kim, Seong Jang Kim, Mijin Kim, Sang‐Woo Lee, Shin Young Jeong, Kyoungjune Pak, Keunyoung Kim, In Joo Kim
Clinical Endocrinology.2018; 89(6): 856. CrossRef - Ultrasound risk evaluation of thyroid nodules that are “unspecified” in the 2015 American Thyroid Association management guidelines
Luying Gao, Xuehua Xi, Juanjuan Wang, Xiao Yang, Ying Wang, Shenling Zhu, Xingjian Lai, Xiaoyan Zhang, Ruina Zhao, Bo Zhang
Medicine.2018; 97(52): e13914. CrossRef - Refining the eighth edition AJCC TNM classification and prognostic groups for papillary thyroid cancer with lateral nodal metastasis
Hye In Kim, Kyunga Kim, So Young Park, Jun-Ho Choe, Jung-Han Kim, Jee Soo Kim, Young Lyun Oh, Soo Yeon Hahn, Jung Hee Shin, Hyeon Seon Ahn, Sun Wook Kim, Tae Hyuk Kim, Jae Hoon Chung
Oral Oncology.2018; 78: 80. CrossRef - Thyroid cancer surgery guidelines in an era of de-escalation
K.J. Kovatch, C.W. Hoban, A.G. Shuman
European Journal of Surgical Oncology.2018; 44(3): 297. CrossRef - Changes in Serum Thyroglobulin Levels After Lobectomy in Patients with Low-Risk Papillary Thyroid Cancer
Suyeon Park, Min Ji Jeon, Hye-Seon Oh, Yu-Mi Lee, Tae-Yon Sung, Minkyu Han, Ji Min Han, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2018; 28(8): 997. CrossRef - Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-jin Jung, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun Jae Jung, June Young Choi, Chang Hwan Ryu, You Jin Lee
Endocrinology and Metabolism.2018; 33(2): 278. CrossRef - Low-Dose Radioactive Iodine Ablation Is Sufficient in Patients With Small Papillary Thyroid Cancer Having Minor Extrathyroidal Extension and Central Lymph Node Metastasis (T3 N1a): Reply
Minjung Seo, Yon Seon Kim, Jong Cheol Lee, Myung Woul Han, Eun Sook Kim, Kyung Bin Kim, Seol Hoon Park
Clinical Nuclear Medicine.2018; 43(8): 635. CrossRef - Diagnosis and treatment of low-risk papillary thyroid microcarcinoma
Jae Hoon Moon, Young Joo Park
Journal of the Korean Medical Association.2018; 61(4): 232. CrossRef - Efficacy of a Home-Based Exercise Program After Thyroidectomy for Thyroid Cancer Patients
Kyunghee Kim, Mee Ock Gu, Jung Hwa Jung, Jong Ryeal Hahm, Soo Kyoung Kim, Jin Hyun Kim, Seung Hoon Woo
Thyroid.2018; 28(2): 236. CrossRef - Genome-Wide Association Study Reveals Distinct Genetic Susceptibility of Thyroid Nodules From Thyroid Cancer
Yul Hwangbo, Eun Kyung Lee, Ho-Young Son, Sun-Wha Im, Soo-Jung Kwak, Ji Won Yoon, Min Joo Kim, Jeongseon Kim, Hoon Sung Choi, Chang Hwan Ryu, You Jin Lee, Jong-Il Kim, Nam H Cho, Young Joo Park
The Journal of Clinical Endocrinology & Metabolism.2018; 103(12): 4384. CrossRef - Active Surveillance of Low-Risk Papillary Thyroid Microcarcinoma: A Multi-Center Cohort Study in Korea
Hye-Seon Oh, Jeonghoon Ha, Hye In Kim, Tae Hyuk Kim, Won Gu Kim, Dong-Jun Lim, Tae Yong Kim, Sun Wook Kim, Won Bae Kim, Young Kee Shong, Jae Hoon Chung, Jung Hwan Baek
Thyroid.2018; 28(12): 1587. CrossRef - Ultrasound criteria for risk stratification of thyroid nodules in the previously iodine deficient area of Austria - a single centre, retrospective analysis
Christina Tugendsam, Veronika Petz, Wolfgang Buchinger, Brigitta Schmoll-Hauer, Iris Pia Schenk, Karin Rudolph, Michael Krebs, Georg Zettinig
Thyroid Research.2018;[Epub] CrossRef - Practical Initial Risk Stratification Based on Lymph Node Metastases in Pediatric and Adolescent Differentiated Thyroid Cancer
Min Ji Jeon, Young Nam Kim, Tae-Yong Sung, Suck Joon Hong, Yoon Young Cho, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Sun Wook Kim, Jae Hoon Chung, Tae Hyuk Kim, Won Gu Kim
Thyroid.2018; 28(2): 193. CrossRef - Current Radiological Approach in Thyroid Nodules
Duzgun Yildirim, Deniz Alis, Sabri Sirolu, Cesur Samanci, Fethi Emre Ustabasioglu, Bulent Colakoglu
Journal of Cancer Therapy.2017; 08(05): 423. CrossRef - A new paradigm in low-risk papillary microcarcinoma: active surveillance
Alex González Bóssolo, Michelle Mangual Garcia, Paula Jeffs González, Miosotis Garcia, Guillermo Villarmarzo, Jose Hernán Martinez
Endocrinology, Diabetes & Metabolism Case Reports.2017;[Epub] CrossRef - Serial Neck Ultrasonographic Evaluation of Changes in Papillary Thyroid Carcinoma During Pregnancy
Hye-Seon Oh, Won Gu Kim, Suyeon Park, Mijin Kim, Hyemi Kwon, Min Ji Jeon, Jeong Hyun Lee, Jung Hwan Baek, Dong Eun Song, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(6): 773. CrossRef - Restratification of survival prognosis of N1b papillary thyroid cancer by lateral lymph node ratio and largest lymph node size
Hye In Kim, Tae Hyuk Kim, Jun‐Ho Choe, Jung‐Han Kim, Jee Soo Kim, Young Lyun Oh, Soo Yeon Hahn, Jung Hee Shin, Hye Won Jang, Young Nam Kim, Hosu Kim, Hyeon Seon Ahn, Kyunga Kim, Sun Wook Kim, Jae Hoon Chung
Cancer Medicine.2017; 6(10): 2244. CrossRef - Comparison on Fine Needle Aspiration Cytology (FNAC) and Thyroid Ultrasonography in Management of Thyroid Nodules
Sandini A Gunaratne
International Clinical Pathology Journal.2017;[Epub] CrossRef - Current Practices of Thyroid Fine-Needle Aspiration in Asia: A Missing Voice
Andrey Bychkov, Kennichi Kakudo, SoonWon Hong
Journal of Pathology and Translational Medicine.2017; 51(6): 517. CrossRef - Clinical outcomes after delayed thyroid surgery in patients with papillary thyroid microcarcinoma
Min Ji Jeon, Won Gu Kim, Hyemi Kwon, Mijin Kim, Suyeon Park, Hye-Seon Oh, Minkyu Han, Tae-Yon Sung, Ki-Wook Chung, Suck Joon Hong, Tae Yong Kim, Young Kee Shong, Won Bae Kim
European Journal of Endocrinology.2017; 177(1): 25. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - The Impact of Thyroid Nodule Size and Fine-Needle Aspiration Biopsy Result on the Risk of Malignancy in the Patients Who Underwent Thyroidectomy
Hwibin Im, Yu-Young Park, Jae-Gu Cho, Seung-Kuk Baek, Soon-Young Kwon, Kwang-Yoon Jung, Jeong-Soo Woo
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2017; 60(6): 308. CrossRef - Active Surveillance of Papillary Thyroid Microcarcinoma: A Mini-Review from Korea
Tae Yong Kim, Young Kee Shong
Endocrinology and Metabolism.2017; 32(4): 399. CrossRef
- Intraoperative pathologic evaluation of central compartment lymph nodes in patients undergoing lobectomy for unilateral papillary thyroid carcinoma

- Obesity and Metabolism
- The Diabetes Epidemic in Korea
- Junghyun Noh
- Endocrinol Metab. 2016;31(3):349-353. Published online August 26, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.349
- 6,283 View
- 50 Download
- 51 Web of Science
- 53 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetes is one of the foremost public health issues worldwide that can lead to complications in many organ systems, and has become a significant cause of morbidity and mortality in Korea. According to data from the National Health Insurance Service (NHIS), about 2.7 million Koreans (8.0%) aged 30 years or older had type 2 diabetes mellitus (T2DM) in 2013. The prevalence of T2DM increased with age and rose from 5.6% in 2006 to 8.0% in 2013. Using data based on The Health Screening Service of the NHIS, 25% of Korean adults were reported to have prediabetes in 2013. The prevalence of an impaired fasting glucose tended to increase over time from 21.5% in 2006 to 25.0% in 2013. Even though nationwide health screening has been regularly conducted as a public service, the proportion of undiagnosed cases of diabetes was still reported to be on the higher side in the latest study. Based on the results of these epidemic studies, further actions will be needed to effectively implement lifestyle changes on a social level and increase measures for the early detection of diabetes to stem the tide of the epidemic.
-
Citations
Citations to this article as recorded by- A Nationwide Population‐Based Study for the Recurrence and Comorbidities in Sudden Sensorineural Hearing Loss
Hye Yeon Ko, Hae Jeong Nam, Min Hee Kim
The Laryngoscope.2024; 134(3): 1417. CrossRef - Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - Cancer risk according to fasting blood glucose trajectories: a population-based cohort study
Thi Minh Thu Khong, Thi Tra Bui, Hee-Yeon Kang, Jinhee Lee, Eunjung Park, Jin-Kyoung Oh
BMJ Open Diabetes Research & Care.2024; 12(1): e003696. CrossRef - Nomenclature Dilemma of Metabolic Associated Fatty Liver Disease (MAFLD): Considerable Proportions of MAFLD Are Metabolic Healthy
Huiyul Park, Eileen L. Yoon, Mimi Kim, Seon Cho, Eun-Hee Nah, Dae Won Jun
Clinical Gastroenterology and Hepatology.2023; 21(4): 1041. CrossRef - Efficacy of Polydeoxyribonucleotide in Promoting the Healing of Diabetic Wounds in a Murine Model of Streptozotocin-Induced Diabetes: A Pilot Experiment
Jiyoung Yun, SaeGwang Park, Ha Young Park, Kyung Ah Lee
International Journal of Molecular Sciences.2023; 24(3): 1932. CrossRef - Influence of Fasting Glucose Level on Gastric Cancer Incidence in a Prospective Cohort Study
Tao Thi Tran, Jeonghee Lee, Madhawa Gunathilake, Hyunsoon Cho, Jeongseon Kim
Cancer Epidemiology, Biomarkers & Prevention.2022; 31(1): 254. CrossRef - A Comparative analysis of type 2 diabetes management quality indicators in cancer survivors
Eun J. Ko, Su J. Lee
Asia-Pacific Journal of Oncology Nursing.2022; 9(11): 100116. CrossRef - Comparative Effects of Sodium-Glucose Cotransporter 2 Inhibitor and Thiazolidinedione Treatment on Risk of Stroke among Patients with Type 2 Diabetes Mellitus
Seung Eun Lee, Hyewon Nam, Han Seok Choi, Hoseob Kim, Dae-Sung Kyoung, Kyoung-Ah Kim
Diabetes & Metabolism Journal.2022; 46(4): 567. CrossRef - Prevalence and diagnosis experience of osteoporosis in postmenopausal women over 50: Focusing on socioeconomic factors
Min Hyeok Choi, Ji Hee Yang, Jae Seung Seo, Yoon-ji Kim, Suk-Woong Kang, Jose M. Moran
PLOS ONE.2021; 16(3): e0248020. CrossRef - Effect of Teneligliptin versus Sulfonylurea on Major Adverse Cardiovascular Outcomes in People with Type 2 Diabetes Mellitus: A Real-World Study in Korea
Da Hea Seo, Kyoung Hwa Ha, So Hun Kim, Dae Jung Kim
Endocrinology and Metabolism.2021; 36(1): 70. CrossRef - A nationwide study of patients with monoclonal gammopathy of undetermined significance with a 10-year follow-up in South Korea
Ka-Won Kang, Ji Eun Song, Byung-Hyun Lee, Min Ji Jeon, Eun Sang Yu, Dae Sik Kim, Se Ryeon Lee, Hwa Jung Sung, Chul Won Choi, Yong Park, Byung Soo Kim
Scientific Reports.2021;[Epub] CrossRef - Fibrosis Burden of Missed and Added Populations According to the New Definition of Metabolic Dysfunction-Associated Fatty Liver
Huiyul Park, Eileen L. Yoon, Mimi Kim, Jung-Hwan Kim, Seon Cho, Dae Won Jun, Eun-Hee Nah
Journal of Clinical Medicine.2021; 10(19): 4625. CrossRef - The Effects of Glucose Lowering Agents on the Secondary Prevention of Coronary Artery Disease in Patients with Type 2 Diabetes
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(5): 977. CrossRef - Decreased Vagal Activity and Deviation in Sympathetic Activity Precedes Development of Diabetes
Da Young Lee, Mi Yeon Lee, Jung Hwan Cho, Hyemi Kwon, Eun-Jung Rhee, Cheol-Young Park, Ki-Won Oh, Won-Young Lee, Sung-Woo Park, Seungho Ryu, Se Eun Park
Diabetes Care.2020; 43(6): 1336. CrossRef - Efficacy and safety of ertugliflozin in East/Southeast Asian patients with type 2 diabetes mellitus
Jie Liu, Shrita Patel, Nilo B. Cater, Larry Wu, Susan Huyck, Steven G. Terra, Anne Hickman, Amanda Darekar, Annpey Pong, Ira Gantz
Diabetes, Obesity and Metabolism.2020; 22(4): 574. CrossRef - Outcomes for Inappropriate Renal Dose Adjustment of Dipeptidyl Peptidase-4 Inhibitors in Patients With Type 2 Diabetes Mellitus: Population-Based Study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
Mayo Clinic Proceedings.2020; 95(1): 101. CrossRef - Longitudinal Study of Diabetic Differences between International Migrants and Natives among the Asian Population
Heng Piao, Jae Moon Yun, Aesun Shin, Belong Cho
Biomolecules & Therapeutics.2020; 28(1): 110. CrossRef - Risk of active tuberculosis development in contacts exposed to infectious tuberculosis in congregate settings in Korea
Shin Young Park, Sunmi Han, Young-Man Kim, Jieun Kim, Sodam Lee, Jiyeon Yang, Un-Na Kim, Mi-sun Park
Scientific Reports.2020;[Epub] CrossRef - The Combined Impact of Chronic Kidney Disease and Diabetes on the Risk of Colorectal Cancer Depends on Sex: A Nationwide Population-Based Study
Hyung Jung Oh, Hye Ah Lee, Chang Mo Moon, Dong-Ryeol Ryu
Yonsei Medical Journal.2020; 61(6): 506. CrossRef - Coffee Consumption, Genetic Polymorphisms, and the Risk of Type 2 Diabetes Mellitus: A Pooled Analysis of Four Prospective Cohort Studies
An Na Kim, Hyun Jeong Cho, Jiyoung Youn, Taiyue Jin, Moonil Kang, Joohon Sung, Jung Eun Lee
International Journal of Environmental Research and Public Health.2020; 17(15): 5379. CrossRef - Current findings of kidney biopsy including nephropathy associated with hypertension and diabetes mellitus in Korea
Kipyo Kim, Sang Ho Lee, Sung Woo Lee, Jung Pyo Lee, Ho Jun Chin
The Korean Journal of Internal Medicine.2020; 35(5): 1173. CrossRef - A Diabetes-Related Dietary Pattern Is Associated with Incident Diabetes in Obese Men in the Korean Genome Epidemiology Study
Hye Ah Lee, NaYeong Son, Won Kyung Lee, Hyesook Park
The Journal of Nutrition.2019; 149(2): 323. CrossRef - Associations of postmenopausal hormone therapy with metabolic syndrome among diabetic and non-diabetic women
Ji-Eun Kim, Jaesung Choi, JooYong Park, Jong-koo Lee, Aesun Shin, Sang Min Park, Daehee Kang, Ji-Yeob Choi
Maturitas.2019; 121: 76. CrossRef - The changing epidemiology of herpes zoster over a decade in South Korea, 2006–2015
Jae-Ki Choi, Sun Hee Park, Sanghyun Park, Sung-Yeon Cho, Hyo-Jin Lee, Si-Hyun Kim, Su-Mi Choi, Dong-Gun Lee, Jung-Hyun Choi, Jin-Hong Yoo
Vaccine.2019; 37(36): 5153. CrossRef - Prevalence of undiagnosed diabetes and pre-diabetes and its associated risk factors in Vietnam
Van Dat Nguyen, Quang Mai Vien, Thai Hung Do, Cong Danh Phan, Huu Chau Nguyen, Van Tuyen Nguyen, Dinh Luong Nguyen, Won Seok Sir, Yun Chon
Journal of Global Health Science.2019;[Epub] CrossRef - Heterogeneous Trajectories of Cognitive Function in Older Adults with Diabetes: Findings from the Korean Longitudinal Study of Aging (KLoSA)
Chanhee Kim, Min Jung Kim, Chang Gi Park
Stress.2019; 27(1): 1. CrossRef - The Effect of Coffee Consumption on the Prevalence of Diabetes Mellitus: The 2012–2016 Korea National Health and Nutrition Examination Survey
Yejee Lim, Youngmi Park, Sun Kyu Choi, Soyeon Ahn, Jung Hun Ohn
Nutrients.2019; 11(10): 2377. CrossRef - Effects of sodium-glucose cotransporter-2 inhibitors and dipeptidyl peptidase-4 inhibitors on diabetic retinopathy and its progression: A real-world Korean study
Yoo-Ri Chung, Kyoung Hwa Ha, Kihwang Lee, Dae Jung Kim, Ping-Hsun Wu
PLOS ONE.2019; 14(10): e0224549. CrossRef - Letter: Projection of Diabetes Prevalence in Korean Adults for the Year 2030 Using Risk Factors Identified from National Data (Diabetes Metab J 2019;43:90–6)
Bo Kyung Koo
Diabetes & Metabolism Journal.2019; 43(2): 242. CrossRef - Changes of computed tomography‐based body composition after adrenalectomy in patients with endogenous hypercortisolism
Namki Hong, Jooyeon Lee, Cheol Ryong Ku, Kichang Han, Cho Rok Lee, Sang Wook Kang, Yumie Rhee
Clinical Endocrinology.2019; 90(2): 267. CrossRef - Estimating Lifetime Duration of Diabetes by Age and Gender in the Korean Population Using a Markov Model
Seung Woo Cho, Seon Ha Kim, Young-Eun Kim, Seok-Jun Yoon, Min-Woo Jo
Journal of Korean Medical Science.2019;[Epub] CrossRef - Hospital-Based Korean Diabetes Prevention Study: A Prospective, Multi-Center, Randomized, Open-Label Controlled Study
Sang Youl Rhee, Suk Chon, Kyu Jeung Ahn, Jeong-Taek Woo
Diabetes & Metabolism Journal.2019; 43(1): 49. CrossRef - Medical Big Data Is Not Yet Available: Why We Need Realism Rather than Exaggeration
Hun-Sung Kim, Dai-Jin Kim, Kun-Ho Yoon
Endocrinology and Metabolism.2019; 34(4): 349. CrossRef - Implementation of the Chronic Disease Care System and its association with health care costs and continuity of care in Korean adults with type 2 diabetes mellitus
Woorim Kim, Yoon Soo Choy, Sang Ah Lee, Eun-Cheol Park
BMC Health Services Research.2018;[Epub] CrossRef - Trends in diabetes prevalence among Korean adults based on Korean National Health and Nutrition Examination Surveys III–VI
Jae-woo Lee, Hee-Taik Kang, Hyoung-Ji Lim, Byoungjin Park
Diabetes Research and Clinical Practice.2018; 138: 57. CrossRef - Insulin Resistance and the Risk of Diabetes and Dysglycemia in Korean General Adult Population
Jong Ha Baek, Hosu Kim, Kyong Young Kim, Jaehoon Jung
Diabetes & Metabolism Journal.2018; 42(4): 296. CrossRef - Relationship Between Circulating Netrin-1 Concentration, Impaired Fasting Glucose, and Newly Diagnosed Type 2 Diabetes
Jisook Yim, Gyuri Kim, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Jeong-Ho Kim, Jin Won Cho, Sang-Guk Lee, Yong-ho Lee
Frontiers in Endocrinology.2018;[Epub] CrossRef - Serum metabolite profile associated with incident type 2 diabetes in Koreans: findings from the Korean Genome and Epidemiology Study
Soo Jin Yang, So-Young Kwak, Garam Jo, Tae-Jin Song, Min-Jeong Shin
Scientific Reports.2018;[Epub] CrossRef - Trends in the prevalence of metabolic syndrome and its components in South Korea: Findings from the Korean National Health Insurance Service Database (2009–2013)
Seung Eun Lee, Kyungdo Han, Yu Mi Kang, Seon-Ok Kim, Yun Kyung Cho, Kyung Soo Ko, Joong-Yeol Park, Ki-Up Lee, Eun Hee Koh, Ying-Mei Feng
PLOS ONE.2018; 13(3): e0194490. CrossRef - Effect of Change in Total Cholesterol Levels on Cardiovascular Disease Among Young Adults
Su‐Min Jeong, Seulggie Choi, Kyuwoong Kim, Sung Min Kim, Gyeongsil Lee, Seong Yong Park, Yeon‐Yong Kim, Joung Sik Son, Jae‐Moon Yun, Sang Min Park
Journal of the American Heart Association.2018;[Epub] CrossRef - Age, sex, and the association of chronic kidney disease with all-cause mortality in Buddhist priests
Hyo Jin Kim, Yunmi Kim, Sejoong Kim, Ho Jun Chin, Hajeong Lee, Jung Pyo Lee, Dong Ki Kim, Kook-Hwan Oh, Kwon Wook Joo, Yon Su Kim, Deuk-Young Nah, Sung Joon Shin, Kyung Soo Kim, Jae Yoon Park, Kyung Don Yoo
Medicine.2018; 97(45): e13099. CrossRef - Association of change in total cholesterol level with mortality: A population-based study
Su-Min Jeong, Seulggie Choi, Kyuwoong Kim, Sung-Min Kim, Gyeongsil Lee, Joung Sik Son, Jae-Moon Yun, Sang Min Park, Katriina Aalto-Setala
PLOS ONE.2018; 13(4): e0196030. CrossRef - High hemoglobin levels are associated with decreased risk of diabetic retinopathy in Korean type 2 diabetes
Min-Kyung Lee, Kyung-Do Han, Jae-Hyuk Lee, Seo-Young Sohn, Jee-Sun Jeong, Mee-Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Scientific Reports.2018;[Epub] CrossRef - Impact of systemic inflammation on the relationship between insulin resistance and all-cause and cancer-related mortality
Da Young Lee, Eun-Jung Rhee, Yoosoo Chang, Chong Il Sohn, Ho-Cheol Shin, Seungho Ryu, Won-Young Lee
Metabolism.2018; 81: 52. CrossRef - The two isoforms of matrix metalloproteinase- 2 have distinct renal spatial and temporal distributions in murine models of types 1 and 2 diabetes mellitus
Il Young Kim, Sang Soo Kim, Hye Won Lee, Sun Sik Bae, Hong Koo Ha, Eun Soon Jung, Min Young Lee, Miyeun Han, Harin Rhee, Eun Young Seong, Dong Won Lee, Soo Bong Lee, David H. Lovett, Sang Heon Song
BMC Nephrology.2018;[Epub] CrossRef - The optimal cut-off of blood pressure related to left ventricular diastolic dysfunction and remodeling in Asian diabetic patients
Ju Young Jung, Sung Keun Park, Jae-Hong Ryoo, Chang-Mo Oh, Jeong Gyu Kang, Kanghee Moon, Keum Ok Lee, Joong-Myung Choi
Journal of Cardiology.2018; 71(1): 16. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Factors Associated with Smoking Cessation Intention among Current Smokers with Diabetes: Analysis of the 2013 Community Health Survey in Korea
Young-Hoon Lee, Jum Suk Ko
Korean Journal of Health Promotion.2017; 17(3): 184. CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Associations of Dietary Antioxidants and Risk of Type 2 Diabetes: Data from the 2007–2012 Korea National Health and Nutrition Examination Survey
Dan Quansah, Kyungho Ha, Shinyoung Jun, Seong-Ah Kim, Sangah Shin, Gyung-Ah Wie, Hyojee Joung
Molecules.2017; 22(10): 1664. CrossRef - Accuracy of Capillary Blood Glucose Test When Fasting in Diabetes Patients or General Population: Performance Evaluation of G300 Based on ISO 15197:2013 Standards
Young-min Jee, Min-hee Seo, Byung-wook Yoo, Sung-ho Hong, Choo-yon Cho, Yong-jin Cho, Jung-eun Oh, Kyung-suk Shin
Korean Journal of Health Promotion.2017; 17(4): 259. CrossRef - Increased Vascular Disease Mortality Risk in Prediabetic Korean Adults Is Mainly Attributable to Ischemic Stroke
Nam Hoon Kim, Tae Yeon Kwon, Sungwook Yu, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yousung Park, Sin Gon Kim
Stroke.2017; 48(4): 840. CrossRef
- A Nationwide Population‐Based Study for the Recurrence and Comorbidities in Sudden Sensorineural Hearing Loss


 KES
KES

 First
First Prev
Prev



