Article type
- Page Path
- HOME > BROWSE ARTICLES > Article type
Letter
- Diabetes, obesity and metabolism
- Multiple Definitions of Fatty Liver Disease: Which One Most Accurately Predicts Diabetes?
- Eun-Jung Rhee
- Endocrinol Metab. 2024;39(2):397-398. Published online April 25, 2024
- DOI: https://doi.org/10.3803/EnM.2024.202

- 19 View
- 3 Download

Original Articles
- Hypothalamus and pituitary gland
- Clinical Characteristics, Diagnosis, and Treatment of Thyroid Stimulating Hormone-Secreting Pituitary Neuroendocrine Tumor (TSH PitNET): A Single-Center Experience
- Jung Heo, Yeon-Lim Suh, Se Hoon Kim, Doo-Sik Kong, Do-Hyun Nam, Won-Jae Lee, Sung Tae Kim, Sang Duk Hong, Sujin Ryu, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim, Kyu Yeon Hur
- Endocrinol Metab. 2024;39(2):387-396. Published online February 5, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1877
- 826 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
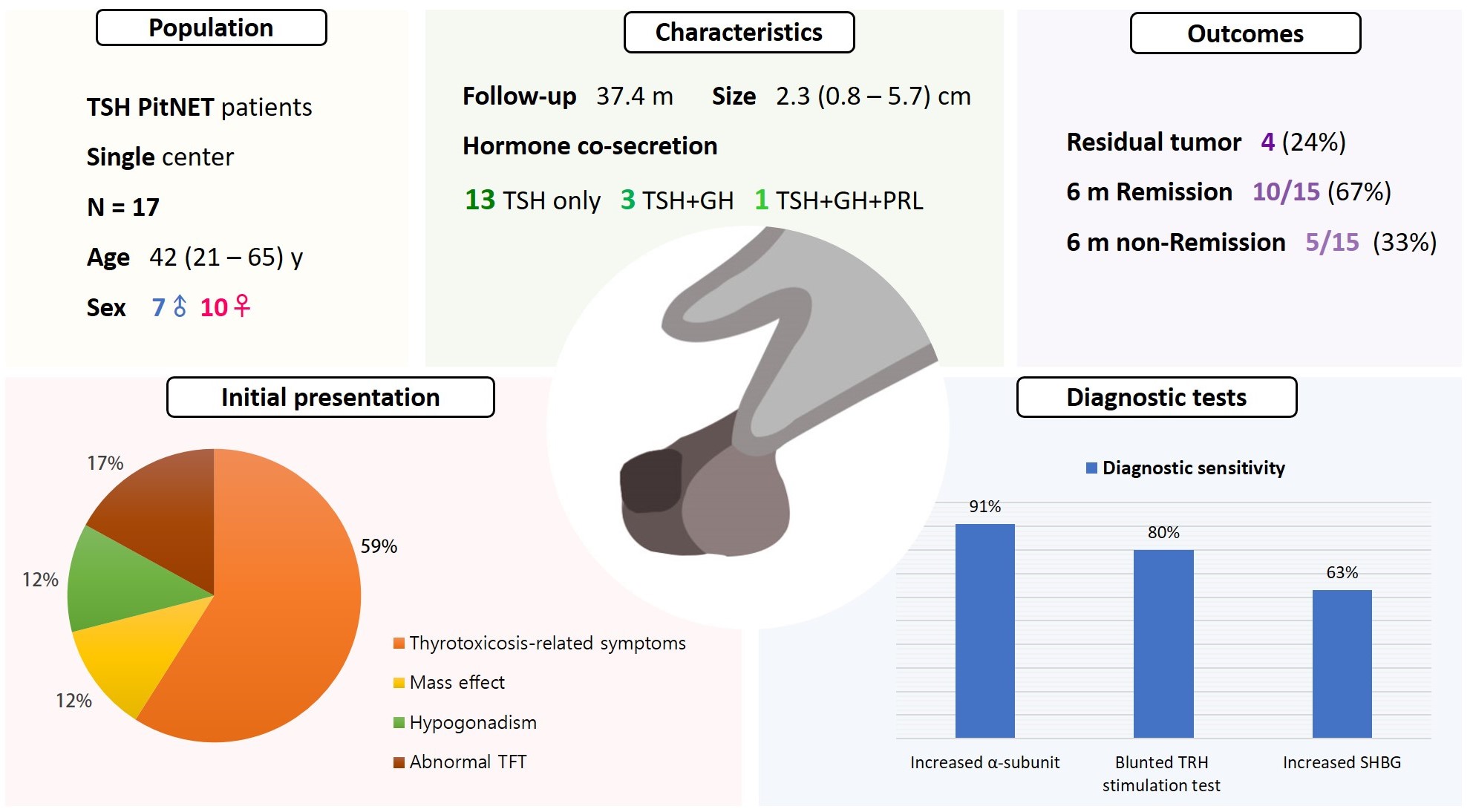
Thyroid-stimulating hormone (TSH)-secreting pituitary neuroendocrine tumor (TSH PitNET) is a rare subtype of PitNET. We investigated the comprehensive characteristics and outcomes of TSH PitNET cases from a single medical center. Also, we compared diagnostic methods to determine which showed superior sensitivity.
Methods
A total of 17 patients diagnosed with TSH PitNET after surgery between 2002 and 2022 in Samsung Medical Center was retrospectively reviewed. Data on comprehensive characteristics and treatment outcomes were collected. The sensitivities of diagnostic methods were compared.
Results
Seven were male (41%), and the median age at diagnosis was 42 years (range, 21 to 65); the median follow-up duration was 37.4 months. The most common (59%) initial presentation was hyperthyroidism-related symptoms. Hormonal co-secretion was present in four (23%) patients. Elevated serum alpha-subunit (α-SU) showed the greatest diagnostic sensitivity (91%), followed by blunted response at thyrotropin-releasing hormone (TRH) stimulation (80%) and elevated sex hormone binding globulin (63%). Fourteen (82%) patients had macroadenoma, and a specimen of one patient with heavy calcification was negative for TSH. Among 15 patients who were followed up for more than 6 months, 10 (67%) achieved hormonal and structural remission within 6 months postoperatively. A case of growth hormone (GH)/TSH/prolactin (PRL) co-secreting mixed gangliocytoma-pituitary adenoma (MGPA) was discovered.
Conclusion
The majority of the TSH PitNET cases was macroadenoma, and 23% showed hormone co-secretion. A rare case of GH/TSH/PRL co-secreting MGPA was discovered. Serum α-SU and TRH stimulation tests showed great diagnostic sensitivity. Careful consideration is needed in diagnosing TSH PitNET. Achieving remission requires complete tumor resection. In case of nonremission, radiotherapy or medical therapy can improve the long-term remission rate.

- Calcium & bone metabolism
- Protein Signatures of Parathyroid Adenoma according to Tumor Volume and Functionality
- Sung Hye Kong, Jeong Mo Bae, Jung Hee Kim, Sang Wan Kim, Dohyun Han, Chan Soo Shin
- Endocrinol Metab. 2024;39(2):375-386. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1827
- 402 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
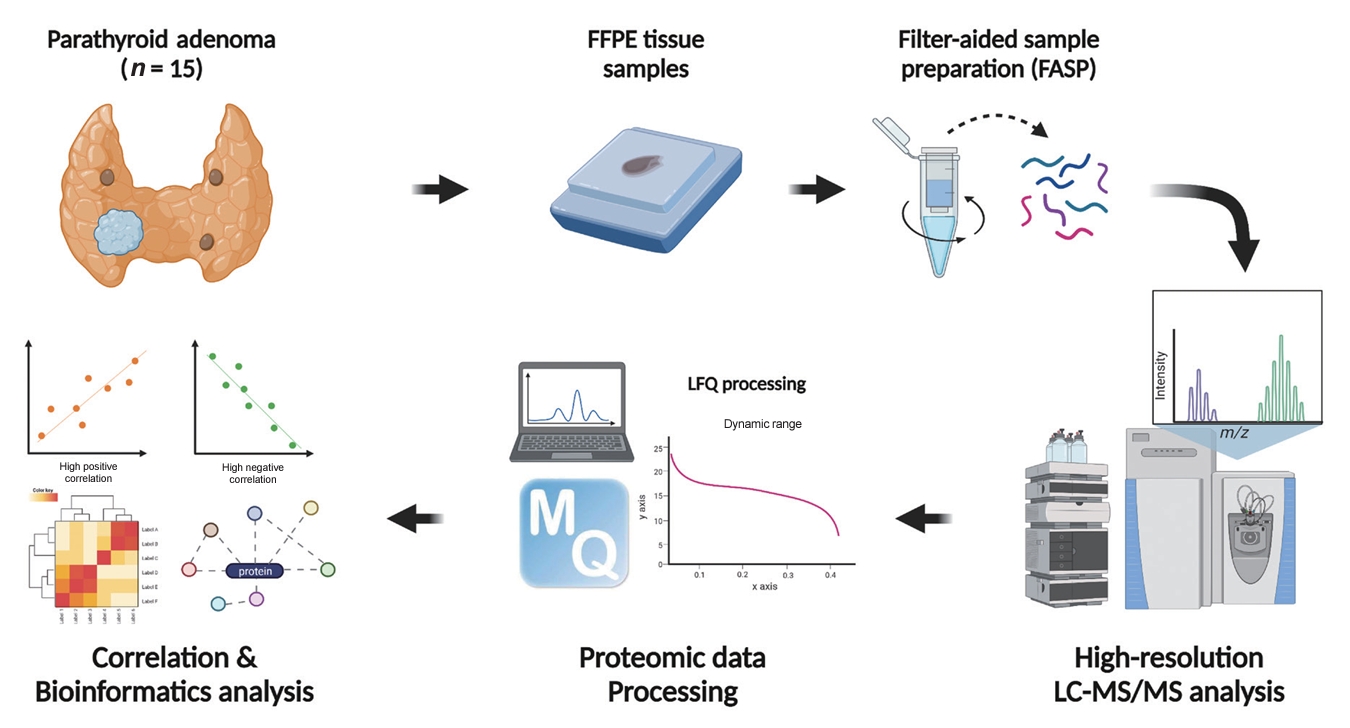
Parathyroid adenoma (PA) is a common endocrine disease linked to multiple complications, but the pathophysiology of the disease remains incompletely understood. The study aimed to identify the key regulator proteins and pathways of PA according to functionality and volume through quantitative proteomic analyses.
Methods
We conducted a retrospective study of 15 formalin-fixed, paraffin-embedded PA samples from tertiary hospitals in South Korea. Proteins were extracted, digested, and the resulting peptides were analyzed using liquid chromatography-tandem mass spectrometry. Pearson correlation analysis was employed to identify proteins significantly correlated with clinical variables. Canonical pathways and transcription factors were analyzed using Ingenuity Pathway Analysis.
Results
The median age of the participants was 52 years, and 60.0% were female. Among the 8,153 protein groups analyzed, 496 showed significant positive correlations with adenoma volume, while 431 proteins were significantly correlated with parathyroid hormone (PTH) levels. The proteins SLC12A9, LGALS3, and CARM1 were positively correlated with adenoma volume, while HSP90AB2P, HLA-DRA, and SCD5 showed negative correlations. DCPS, IRF2BPL, and FAM98A were the main proteins that exhibited positive correlations with PTH levels, and SLITRK4, LAP3, and AP4E1 had negative correlations. Canonical pathway analysis demonstrated that the RAN and sirtuin signaling pathways were positively correlated with both PTH levels and adenoma volume, while epithelial adherence junction pathways had negative correlations.
Conclusion
Our study identified pivotal proteins and pathways associated with PA, offering potential therapeutic targets. These findings accentuate the importance of proteomics in understanding disease pathophysiology and the need for further research.

- Diabetes, obesity and metabolism
- Effects of an Electronic Medical Records-Linked Diabetes Self-Management System on Treatment Targets in Real Clinical Practice: Retrospective, Observational Cohort Study
- So Jung Yang, Sun-Young Lim, Yoon Hee Choi, Jin Hee Lee, Kun-Ho Yoon
- Endocrinol Metab. 2024;39(2):364-374. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1878

- 413 View
- 9 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study evaluated the effects of a mobile diabetes management program called “iCareD” (College of Medicine, The Catholic University of Korea) which was integrated into the hospital’s electronic medical records system to minimize the workload of the healthcare team in the real clinical practice setting.
Methods
In this retrospective observational study, we recruited 308 patients. We categorized these patients based on their compliance regarding their use of the iCareD program at home; compliance was determined through self-monitored blood glucose inputs and message subscription rates. We analyzed changes in the ABC (hemoglobin A1c, blood pressure, and low-density lipoprotein cholesterol) levels from the baseline to 12 months thereafter, based on the patients’ iCareD usage patterns.
Results
The patients comprised 92 (30%) non-users, 170 (55%) poor-compliance users, and 46 (15%) good-compliance users; the ABC target achievement rate showed prominent changes in good-compliance groups from baseline to 12 months (10.9% vs. 23.9%, P<0.05), whereas no significant changes were observed for poor-compliance users and non-users (13.5% vs. 18.8%, P=0.106; 20.7% vs. 14.1%, P=0.201; respectively).
Conclusion
Implementing the iCareD can improve the ABC levels of patients with diabetes with minimal efforts of the healthcare team in real clinical settings. However, the improvement of patients’ compliance concerning the use of the system without the vigorous intervention of the healthcare team needs to be solved in the future.

- Diabetes, obesity and metabolism
- Docosahexanoic Acid Attenuates Palmitate-Induced Apoptosis by Autophagy Upregulation via GPR120/mTOR Axis in Insulin-Secreting Cells
- Seok-Woo Hong, Jinmi Lee, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2024;39(2):353-363. Published online January 23, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1809
- 901 View
- 40 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
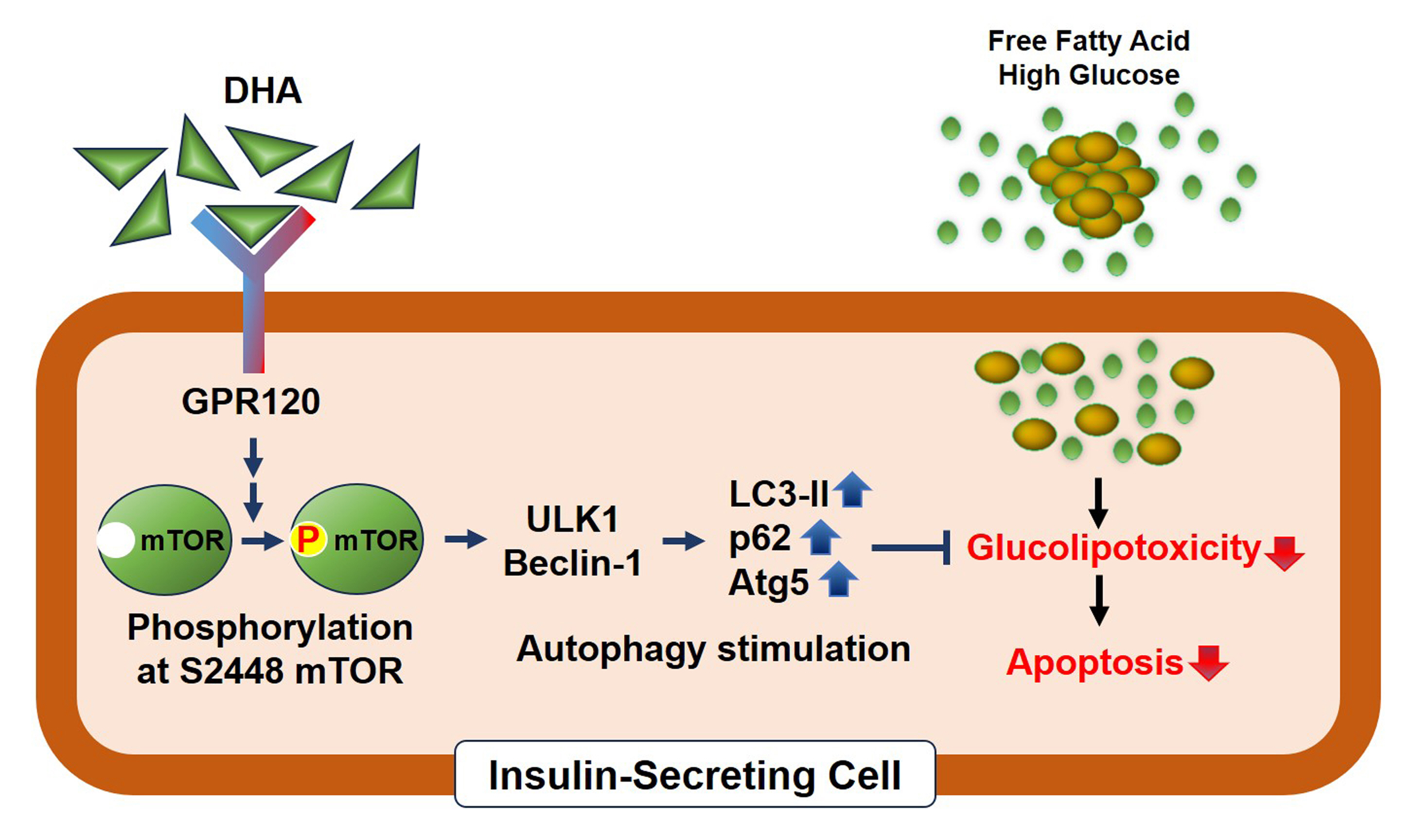
Polyunsaturated fatty acids (PUFAs) reportedly have protective effects on pancreatic β-cells; however, the underlying mechanisms are unknown.
Methods
To investigate the cellular mechanism of PUFA-induced cell protection, mouse insulinoma 6 (MIN6) cells were cultured with palmitic acid (PA) and/or docosahexaenoic acid (DHA), and alterations in cellular signaling and apoptosis were examined.
Results
DHA treatment remarkably repressed caspase-3 cleavage and terminal deoxynucleotidyl transferase-mediated UTP nick end labeling (TUNEL)-positive red dot signals in PA-treated MIN6 cells, with upregulation of autophagy, an increase in microtubule- associated protein 1-light chain 3 (LC3)-II, autophagy-related 5 (Atg5), and decreased p62. Upstream factors involved in autophagy regulation (Beclin-1, unc51 like autophagy activating kinase 1 [ULK1], phosphorylated mammalian target of rapamycin [mTOR], and protein kinase B) were also altered by DHA treatment. DHA specifically induced phosphorylation on S2448 in mTOR; however, phosphorylation on S2481 decreased. The role of G protein-coupled receptor 120 (GPR120) in the effect of DHA was demonstrated using a GPR120 agonist and antagonist. Additional treatment with AH7614, a GPR120 antagonist, significantly attenuated DHA-induced autophagy and protection. Taken together, DHA-induced autophagy activation with protection against PA-induced apoptosis mediated by the GPR120/mTOR axis.
Conclusion
These findings indicate that DHA has therapeutic effects on PA-induced pancreatic β-cells, and that the cellular mechanism of β-cell protection by DHA may be a new research target with potential pharmacotherapeutic implications in β-cell protection.

- Diabetes, obesity and metabolism
- Effectiveness of a Social Networking Site Based Automatic Mobile Message Providing System on Glycemic Control in Patients with Type 2 Diabetes Mellitus
- Kyuho Kim, Jae-Seung Yun, Joonyub Lee, Yeoree Yang, Minhan Lee, Yu-Bae Ahn, Jae Hyoung Cho, Seung-Hyun Ko
- Endocrinol Metab. 2024;39(2):344-352. Published online December 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1871
- 524 View
- 33 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
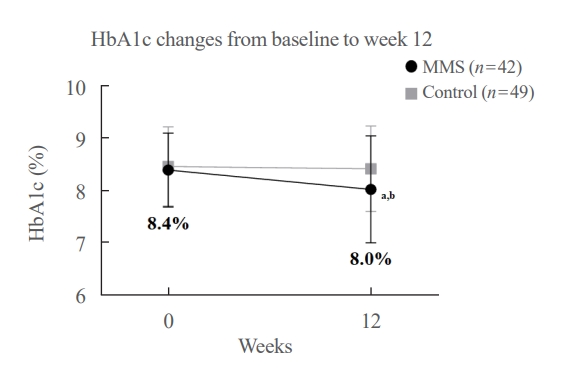
This study investigated the effectiveness of a social networking site (SNS)-based automatic mobile message providing system on glycemic control in patients with type 2 diabetes mellitus (T2DM).
Methods
A 3-month, randomized, open-label, controlled, parallel-group trial was conducted. One hundred and ten participants with T2DM were randomized to a mobile message system (MMS) (n=55) or control group (n=55). The MMS group received protocolbased automated messages two times per day for 10 weeks regarding diabetes self-management through KakaoTalk SNS messenger. The primary outcome was the difference in the change in glycated hemoglobin (HbA1c) levels (%) from baseline to week 12.
Results
HbA1c levels were more markedly decreased in the MMS group (8.4%±0.7% to 8.0%±1.1%) than in the control group (8.5%±0.8% to 8.4%±0.8%), resulting in a significant between-group difference (P=0.027). No differences were observed in changes in fasting glucose levels, lipid profiles, and the number of participants who experienced hypoglycemia, or in changes in lifestyle behavior between groups. However, the self-monitoring of blood glucose frequency was significantly increased in the MMS group compared to the control group (P=0.003). In addition, sleep duration was increased in the MMS group, but was not changed in the control group.
Conclusion
An SNS-based automatic mobile message providing system was effective in improving glycemic control in patients in T2DM. Studies which based on a more individualized protocol, and investigate longer beneficial effect and sustainability will be required in the future.

- Thyroid
- Prognostic Roles of Inflammatory Biomarkers in Radioiodine-Refractory Thyroid Cancer Treated with Lenvatinib
- Chae A Kim, Mijin Kim, Meihua Jin, Hee Kyung Kim, Min Ji Jeon, Dong Jun Lim, Bo Hyun Kim, Ho-Cheol Kang, Won Bae Kim, Dong Yeob Shin, Won Gu Kim
- Endocrinol Metab. 2024;39(2):334-343. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1854
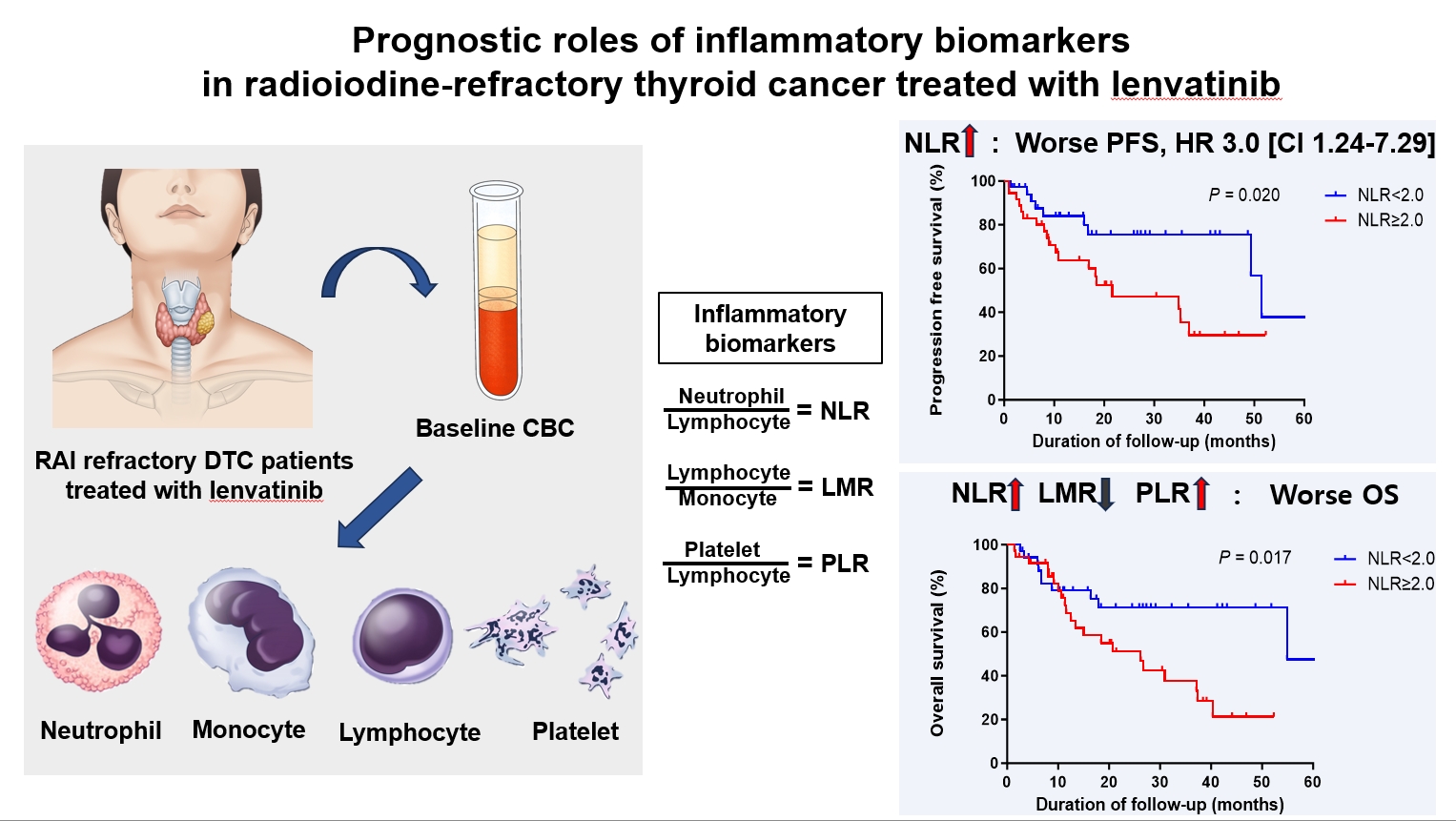
- 333 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Inflammatory biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR), serve as valuable prognostic indicators in various cancers. This multicenter, retrospective cohort study assessed the treatment outcomes of lenvatinib in 71 patients with radioactive iodine (RAI)-refractory thyroid cancer, considering the baseline inflammatory biomarkers.
Methods
This study retrospectively included patients from five tertiary hospitals in Korea whose complete blood counts were available before lenvatinib treatment. Progression-free survival (PFS) and overall survival (OS) were evaluated based on the median value of inflammatory biomarkers.
Results
No significant differences in baseline characteristics were observed among patients grouped according to the inflammatory biomarkers, except for older patients with a higher-than-median NLR (≥2) compared to their counterparts with a lower NLR (P= 0.01). Patients with a higher-than-median NLR had significantly shorter PFS (P=0.02) and OS (P=0.017) than those with a lower NLR. In multivariate analysis, a higher-than-median NLR was significantly associated with poor OS (hazard ratio, 3.0; 95% confidence interval, 1.24 to 7.29; P=0.015). However, neither the LMR nor the PLR was associated with PFS. A higher-than-median LMR (≥3.9) was significantly associated with prolonged OS compared to a lower LMR (P=0.036). In contrast, a higher-than-median PLR (≥142.1) was associated with shorter OS compared to a lower PLR (P=0.039).
Conclusion
Baseline inflammatory biomarkers can serve as predictive indicators of PFS and OS in patients with RAI-refractory thyroid cancer treated with lenvatinib.

- Thyroid
- Clinicopathological Features and Molecular Signatures of Lateral Neck Lymph Node Metastasis in Papillary Thyroid Microcarcinoma
- Jinsun Lim, Han Sai Lee, Jin-Hyung Heo, Young Shin Song
- Endocrinol Metab. 2024;39(2):324-333. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1885

- 377 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The predictive factors for lateral neck lymph node metastasis (LLNM) in papillary thyroid microcarcinoma (PTMC) remain undetermined. This study investigated the clinicopathological characteristics, transcriptomes, and tumor microenvironment in PTMC according to the LLNM status. We aimed to identify the biomarkers associated with LLNM development.
Methods
We retrospectively reviewed the medical records of patients with PTMC from two independent institutions between 2018 and 2022 (n=597 and n=467). We compared clinicopathological features between patients without lymph node metastasis (N0) and those with LLNM (N1b). Additionally, laser capture microdissection and RNA sequencing were performed on primary tumors from both groups, including metastatic lymph nodes from the N1b group (n=30; 20 primary tumors and 10 paired LLNMs). We corroborated the findings using RNA sequencing data from 16 BRAF-like PTMCs from The Cancer Genome Atlas. Transcriptomic analyses were validated by immunohistochemical staining.
Results
Clinicopathological characteristics, such as male sex, multifocality, extrathyroidal extension, lymphatic invasion, and central node metastasis showed associations with LLNM in PTMCs. Transcriptomic profiles between the N0 and N1b PTMC groups were similar. However, tumor microenvironment deconvolution from RNA sequencing and immunohistochemistry revealed an increased abundance of tumor-associated macrophages, particularly M2 macrophages, in the N1b group.
Conclusion
Patients with PTMC who have a male sex, multifocality, extrathyroidal extension, lymphatic invasion, and central node metastasis exhibited an elevated risk for LLNM. Furthermore, infiltration of M2 macrophages in the tumor microenvironment potentially supports tumor progression and LLNM in PTMCs.

- Thyroid
Thyroid Cancer Screening - Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
- Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
- Endocrinol Metab. 2024;39(2):310-323. Published online April 9, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1870

- 402 View
- 11 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There is debate about ultrasonography screening for thyroid cancer and its cost-effectiveness. This study aimed to evaluate the cost-effectiveness of early screening (ES) versus symptomatic detection (SD) for differentiated thyroid cancer (DTC) in Korea.
Methods
A Markov decision analysis model was constructed to compare the cost-effectiveness of ES and SD. The model considered direct medical costs, health outcomes, and different diagnostic and treatment pathways. Input data were derived from literature and Korean population studies. Incremental cost-effectiveness ratio (ICER) was calculated. Willingness-to-pay (WTP) threshold was set at USD 100,000 or 20,000 per quality-adjusted life year (QALY) gained. Sensitivity analyses were conducted to address uncertainties of the model’s variables.
Results
In a base case scenario with 50 years of follow-up, ES was found to be cost-effective compared to SD, with an ICER of $2,852 per QALY. With WTP set at $100,000, in the case with follow-up less than 10 years, the SD was cost-effective. Sensitivity analysis showed that variables such as lobectomy probability, age, mortality, and utility scores significantly influenced the ICER. Despite variations in costs and other factors, all ICER values remained below the WTP threshold.
Conclusion
Findings of this study indicate that ES is a cost-effective strategy for DTC screening in the Korean medical system. Early detection and subsequent lobectomy contribute to the cost-effectiveness of ES, while SD at an advanced stage makes ES more cost-effective. Expected follow-up duration should be considered to determine an optimal strategy for DTC screening.

- Thyroid
- The Diagnostic Role of Repeated Biopsy of Thyroid Nodules with Atypia of Undetermined Significance with Architectural Atypia on Core-Needle Biopsy
- Hye Hyeon Moon, Sae Rom Chung, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee, Jung Hwan Baek
- Endocrinol Metab. 2024;39(2):300-309. Published online January 3, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1818

- 466 View
- 31 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We aimed to evaluate the utility of repeat biopsy of thyroid nodules classified as atypia of undetermined significance with architectural atypia (IIIB) on core-needle biopsy (CNB).
Methods
This retrospective study evaluated patients with thyroid nodules categorized as IIIB on CNB between 2013 and 2015. Demographic characteristics, subsequent biopsy results, and ultrasound (US) images were evaluated. The malignancy rates of nodules according to number of CNBs and the number of IIIB diagnoses was compared. Demographic and US features were evaluated to determine factors predictive of malignancy.
Results
Of 1,003 IIIB nodules on CNB, the final diagnosis was determined for 328 (32.7%) nodules, with 121 of them confirmed as malignant, resulting in a malignancy rate of 36.9% (95% confidence interval, 31.7% to 42.1%). Repeat CNB was performed in 248 nodules (24.7%), with 75 (30.2%), 131 (52.8%), 13 (5.2%), 26 (10.5%), one (0.4%), and two (0.8%) reclassified into categories II, IIIB, IIIA, IV, V, and VI, respectively. Malignancy rates were not significantly affected by the number of CNBs (P=0.291) or the number of IIIB diagnoses (P=0.473). None of the nodules confirmed as category II on repeat CNB was malignant. US features significantly associated with malignancy (P<0.003) included solid composition, irregular margins, microcalcifications, and high suspicion on the US risk stratification system.
Conclusion
Repeat biopsy of nodules diagnosed with IIIB on CNB did not increase the detection of malignancy but can potentially reduce unnecessary surgery. Repeat biopsy should be performed selectively, with US features guiding the choice between repeat biopsy and diagnostic surgery.

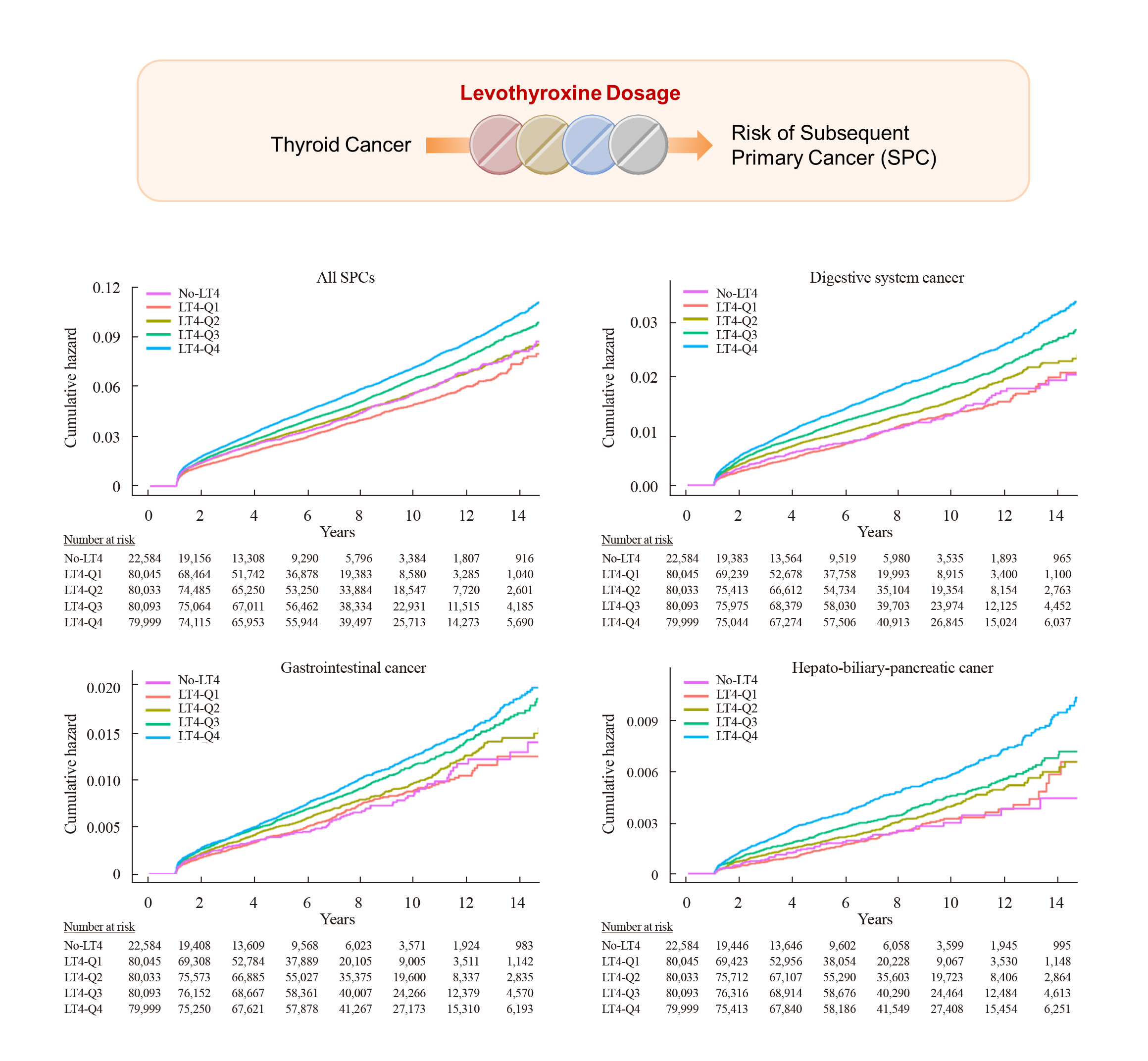
- Thyroid
- Risk of Subsequent Primary Cancers in Thyroid Cancer Survivors according to the Dose of Levothyroxine: A Nationwide Cohort Study
- Min-Su Kim, Jang Won Lee, Min Kyung Hyun, Young Shin Song
- Endocrinol Metab. 2024;39(2):288-299. Published online March 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1815
- 681 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Current research has not investigated the effect of thyroid-stimulating hormone suppression therapy with levothyroxine on the risk for developing subsequent primary cancers (SPCs). This study aimed to investigate the association between levothyroxine dosage and the risk for SPCs in thyroid cancer patients.
Methods
We conducted a nationwide population-based retrospective cohort study form Korean National Health Insurance database. This cohort included 342,920 thyroid cancer patients between 2004 and 2018. Patients were divided into the non-levothyroxine and the levothyroxine groups, the latter consisting of four dosage subgroups according to quartiles. Cox proportional hazard models were performed to evaluate the risk for SPCs by adjusting for variables including cumulative doses of radioactive iodine (RAI) therapy.
Results
A total of 17,410 SPC cases were observed over a median 7.3 years of follow-up. The high-dose levothyroxine subgroups (Q3 and Q4) had a higher risk for SPC (adjusted hazard ratio [HR], 1.14 and 1.27; 95% confidence interval [CI], 1.05–1.24 and 1.17– 1.37; respectively) compared to the non-levothyroxine group. In particular, the adjusted HR of stomach (1.31), colorectal (1.60), liver and biliary tract (1.95), and pancreatic (2.48) cancers were increased in the Q4 subgroup. We consistently observed a positive association between high levothyroxine dosage per body weight and risk of SPCs, even after adjusting for various confounding variables. Moreover, similar results were identified in the stratified analyses according to thyroidectomy type and RAI therapy, as well as in a subgroup analysis of patients with good adherence.
Conclusion
High-dose levothyroxine use was associated with increased risk of SPCs among thyroid cancer patients regardless of RAI therapy.

Editorials
- Thyroid
- Selective Agonists of Thyroid Hormone Receptor Beta: Promising Tools for the Treatment of Nonalcoholic Fatty Liver Disease
- Sun Wook Cho
- Endocrinol Metab. 2024;39(2):285-287. Published online April 25, 2024
- DOI: https://doi.org/10.3803/EnM.2024.203

- 44 View
- 2 Download

- Thyroid
- The Levothyroxine Odyssey: Navigating the Path of Survivorship in Thyroid Cancer
- Jin Hwa Kim
- Endocrinol Metab. 2024;39(2):283-284. Published online April 25, 2024
- DOI: https://doi.org/10.3803/EnM.2024.201
- 38 View
- 2 Download

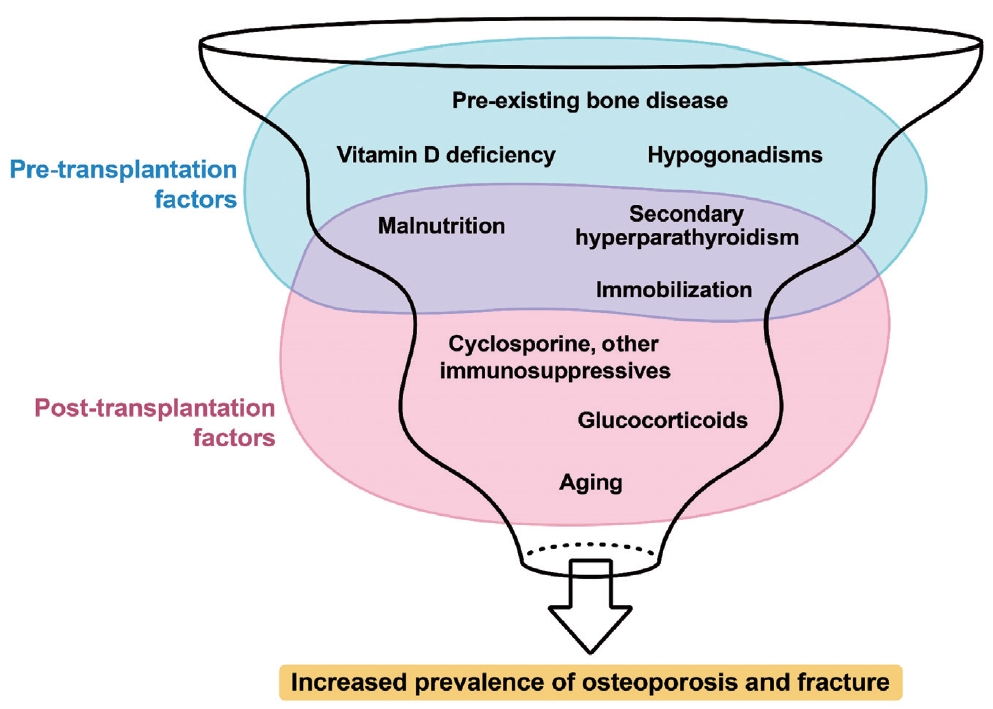
Review Articles
- Calcium & bone metabolism
- Bone Loss after Solid Organ Transplantation: A Review of Organ-Specific Considerations
- Kyoung Jin Kim, Jeonghoon Ha, Sang Wan Kim, Jung-Eun Kim, Sihoon Lee, Han Seok Choi, Namki Hong, Sung Hye Kong, Seong Hee Ahn, So Young Park, Ki-Hyun Baek, on Behalf of Metabolic Bone Disease Study Group of Korean Endocrine Society
- Endocrinol Metab. 2024;39(2):267-282. Published online April 25, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1939
- 46 View
- 3 Download
-
 Abstract
Abstract
 PDF
PDF - This review article investigates solid organ transplantation-induced osteoporosis, a critical yet often overlooked issue, emphasizing its significance in post-transplant care. The initial sections provide a comprehensive understanding of the prevalence and multifactorial pathogenesis of transplantation osteoporosis, including factors such as deteriorating post-transplantation health, hormonal changes, and the impact of immunosuppressive medications. Furthermore, the review is dedicated to organ-specific considerations in transplantation osteoporosis, with separate analyses for kidney, liver, heart, and lung transplantations. Each section elucidates the unique challenges and management strategies pertinent to transplantation osteoporosis in relation to each organ type, highlighting the necessity of an organ-specific approach to fully understand the diverse manifestations and implications of transplantation osteoporosis. This review underscores the importance of this topic in transplant medicine, aiming to enhance awareness and knowledge among clinicians and researchers. By comprehensively examining transplantation osteoporosis, this study contributes to the development of improved management and care strategies, ultimately leading to improved patient outcomes in this vulnerable group. This detailed review serves as an essential resource for those involved in the complex multidisciplinary care of transplant recipients.

- Calcium & bone metabolism
- Treatment of Hypoparathyroidism by Re-Establishing the Effects of Parathyroid Hormone
- Lars Rejnmark
- Endocrinol Metab. 2024;39(2):262-266. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1916

- 417 View
- 51 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The conventional treatment of hypoparathyroidism (HypoPT) includes active vitamin D and calcium. Despite normalization of calcium levels, the conventional treatment is associated with fluctuations in calcium levels, hypercalciuria, renal impairment, and decreased quality of life (QoL). Replacement therapy with parathyroid hormone (PTH)(1-84) is an option in some countries. However, convincing beneficial effects have not been demonstrated, which may be due to the short duration of action of this treatment. Recently, palopegteriparatide (also known as TransCon PTH) has been marketed in Europe and is expected also to be approved in other countries. Palopegteriparatide is a prodrug with sustained release of PTH(1-34) designed to provide stable physiological PTH levels for 24 hours/day. A phase 3 study demonstrated maintenance of normocalcemia in patients with chronic HypoPT, with no need for conventional therapy. Furthermore, this treatment lowers urinary calcium and improves QoL. Another long-acting PTH analog with effects on the parathyroid hormone receptor (eneboparatide) is currently being tested in a phase 3 trial. Furthermore, the treatment of autosomal dominant hypocalcemia type 1 with a calcilytic (encaleret) is also being tested. All in all, improved treatment options are on the way that will likely take the treatment of HypoPT to the next level.


 KES
KES
 First
First Prev
Prev



