Search
- Page Path
- HOME > Search
- Thyroid
- Clinicopathological Features and Molecular Signatures of Lateral Neck Lymph Node Metastasis in Papillary Thyroid Microcarcinoma
- Jinsun Lim, Han Sai Lee, Jin-Hyung Heo, Young Shin Song
- Endocrinol Metab. 2024;39(2):324-333. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1885

- 370 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The predictive factors for lateral neck lymph node metastasis (LLNM) in papillary thyroid microcarcinoma (PTMC) remain undetermined. This study investigated the clinicopathological characteristics, transcriptomes, and tumor microenvironment in PTMC according to the LLNM status. We aimed to identify the biomarkers associated with LLNM development.
Methods
We retrospectively reviewed the medical records of patients with PTMC from two independent institutions between 2018 and 2022 (n=597 and n=467). We compared clinicopathological features between patients without lymph node metastasis (N0) and those with LLNM (N1b). Additionally, laser capture microdissection and RNA sequencing were performed on primary tumors from both groups, including metastatic lymph nodes from the N1b group (n=30; 20 primary tumors and 10 paired LLNMs). We corroborated the findings using RNA sequencing data from 16 BRAF-like PTMCs from The Cancer Genome Atlas. Transcriptomic analyses were validated by immunohistochemical staining.
Results
Clinicopathological characteristics, such as male sex, multifocality, extrathyroidal extension, lymphatic invasion, and central node metastasis showed associations with LLNM in PTMCs. Transcriptomic profiles between the N0 and N1b PTMC groups were similar. However, tumor microenvironment deconvolution from RNA sequencing and immunohistochemistry revealed an increased abundance of tumor-associated macrophages, particularly M2 macrophages, in the N1b group.
Conclusion
Patients with PTMC who have a male sex, multifocality, extrathyroidal extension, lymphatic invasion, and central node metastasis exhibited an elevated risk for LLNM. Furthermore, infiltration of M2 macrophages in the tumor microenvironment potentially supports tumor progression and LLNM in PTMCs.

- Hypothalamus and pituitary gland
- Update on Current Evidence for the Diagnosis and Management of Nonfunctioning Pituitary Neuroendocrine Tumors
- Elizabeth Whyte, Masahiro Nezu, Constance Chik, Toru Tateno
- Endocrinol Metab. 2023;38(6):631-654. Published online November 15, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1838

- 2,265 View
- 142 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Pituitary neuroendocrine tumors (PitNETs) are the third most frequently diagnosed intracranial tumors, with nonfunctioning PitNETs (nfPitNETs) accounting for 30% of all pituitary tumors and representing the most common type of macroPitNETs. NfPitNETs are usually benign tumors with no evidence of hormone oversecretion except for hyperprolactinemia secondary to pituitary stalk compression. Due to this, they do not typically present with clinical syndromes like acromegaly, Cushing’s disease or hyperthyroidism and instead are identified incidentally on imaging or from symptoms of mass effects (headache, vision changes, apoplexy). With the lack of effective medical interventions, first-line treatment is transsphenoidal surgical resection, however, nfPitNETs often have supra- or parasellar extension, and total resection of the tumor is often not possible, resulting in residual tumor regrowth or reoccurrence. While functional PitNETs can be easily followed for recurrence using hormonal biomarkers, there is no similar parameter to predict recurrence in nfPitNETs, hence delaying early recognition and timely management. Therefore, there is a need to identify prognostic biomarkers that can be used for patient surveillance and as therapeutic targets. This review focuses on summarizing the current evidence on nfPitNETs, with a special focus on potential new biomarkers and therapeutics.

- Calcium & bone metabolism
- Higher Plasma Stromal Cell-Derived Factor 1 Is Associated with Lower Risk for Sarcopenia in Older Asian Adults
- Sunghwan Ji, Kyunggon Kim, So Jeong Park, Jin Young Lee, Hee-Won Jung, Hyun Ju Yoo, Il-Young Jang, Eunju Lee, Ji Yeon Baek, Beom-Jun Kim
- Endocrinol Metab. 2023;38(6):701-708. Published online October 18, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1783

- 1,681 View
- 77 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Despite the protective effects of stromal cell-derived factor 1 (SDF-1) in stimulating muscle regeneration shown in experimental research, there is a lack of clinical studies linking circulating SDF-1 concentrations with muscle phenotypes. In order to elucidate the role of SDF-1 as a potential biomarker reflecting human muscle health, we investigated the association of plasma SDF-1 levels with sarcopenia in older adults.
Methods
This cross-sectional study included 97 community-dwelling participants who underwent a comprehensive geriatric assessment at a tertiary hospital in South Korea. Sarcopenia was defined by specific cutoff values applicable to the Asian population, whereas plasma SDF-1 levels were determined using an enzyme immunoassay.
Results
After accounting for sex, age, and body mass index, participants with sarcopenia and low muscle mass exhibited plasma SDF-1 levels that were 21.8% and 18.3% lower than those without these conditions, respectively (P=0.008 and P=0.009, respectively). Consistently, higher plasma SDF-1 levels exhibited a significant correlation with higher skeletal muscle mass index (SMI) and gait speed (both P=0.043), and the risk of sarcopenia and low muscle mass decreased by 58% and 55% per standard deviation increase in plasma SDF-1 levels, respectively (P=0.045 and P=0.030, respectively). Furthermore, participants in the highest SDF-1 tertile exhibited significantly higher SMI compared to those in the lowest tertile (P=0.012).
Conclusion
These findings clinically corroborate earlier experimental discoveries highlighting the muscle anabolic effects of SDF- 1 and support the potential role of circulating SDF-1 as a biomarker reflecting human muscle health in older adults.

- Diabetes, Obesity and Metabolism
- Human Leukocyte Antigens and Biomarkers in Type 1 Diabetes Mellitus Induced by Immune-Checkpoint Inhibitors
- Hidefumi Inaba, Yosuke Kaido, Saya Ito, Tomonao Hirobata, Gen Inoue, Takakazu Sugita, Yuki Yamamoto, Masatoshi Jinnin, Hiroaki Kimura, Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima, Takaaki Matsuoka
- Endocrinol Metab. 2022;37(1):84-95. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1282
- 4,209 View
- 159 Download
- 16 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 1 diabetes mellitus induced by immune-checkpoint inhibitors (ICI-T1DM) is a rare critical entity. However, the etiology of ICI-T1DM remains unclear.
Methods
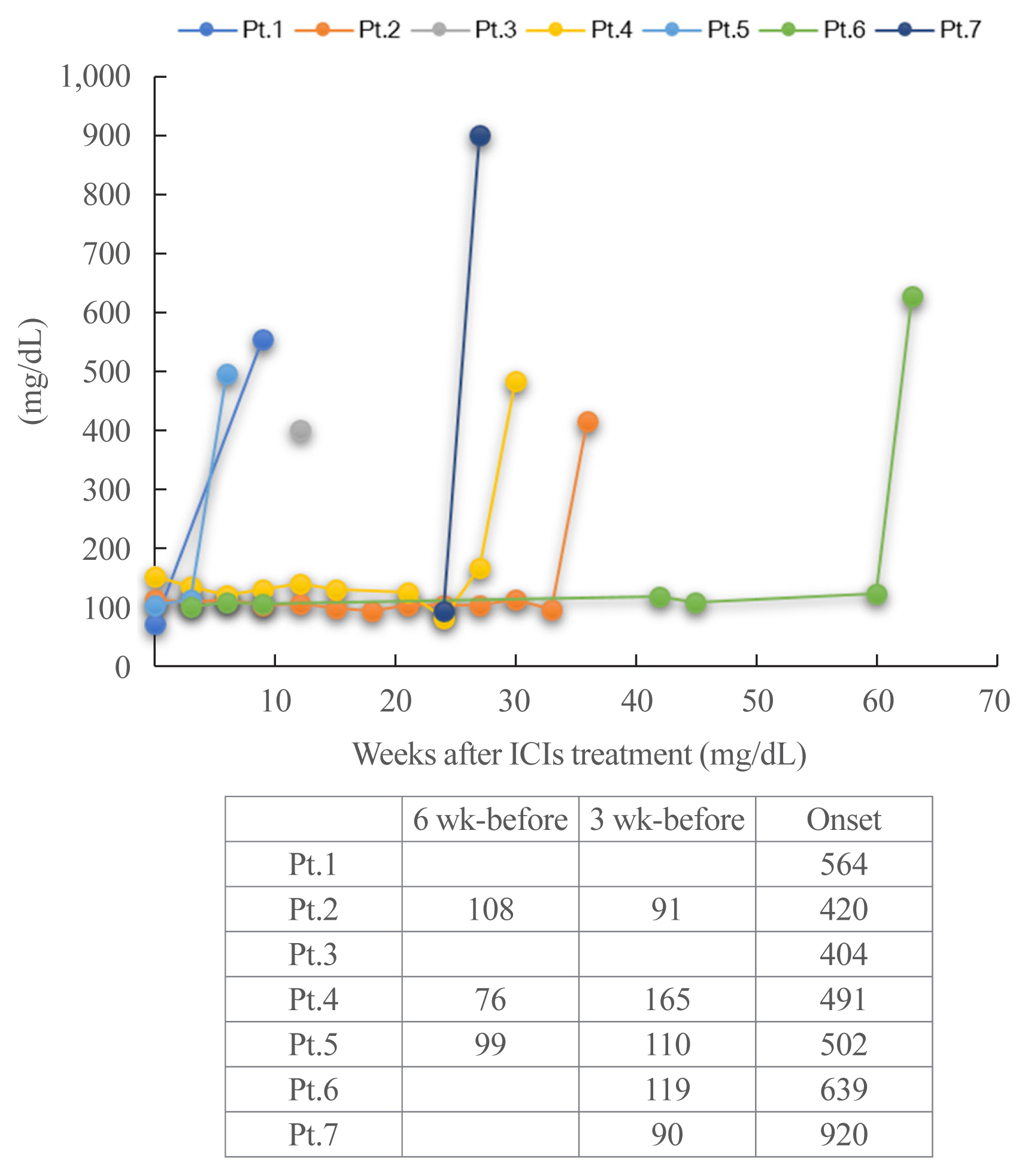
In order to elucidate risk factors for ICI-T1DM, we evaluated the clinical course and immunological status of patients with ICI-T1DM who had been diagnosed during 2016 to 2021.
Results
Seven of 871 (0.8%, six men and one woman) patients developed ICI-T1DM. We revealed that the allele frequencies of human leukocyte antigen (HLA)-DPA1*02:02 and DPB1*05:01 were significantly higher in the patients with ICI-T1DM In comparison to the controls who received ICI (11/14 vs. 10/26, P=0.022; 11/14 vs. 7/26, P=0.0027, respectively). HLA-DRB1*04:05, which has been found to be a T1DM susceptibility allele in Asians, was also observed as a high-risk allele for ICI-T1DM. The significance of the HLA-DPB1*05:01 and DRB1*04:05 alleles was confirmed by an analysis of four additional patients. The absolute/relative neutrophil count, neutrophils-lymphocyte ratio, and neutrophil-eosinophil ratio increased, and the absolute lymphocyte count and absolute/relative eosinophil count decreased at the onset as compared with 6 weeks before. In two patients, alterations in cytokines and chemokines were found at the onset.
Conclusion
Novel high-risk HLA alleles and haplotypes were identified in ICI-T1DM, and peripheral blood factors may be utilized as biomarkers. -
Citations
Citations to this article as recorded by- Type 1 diabetes mellitus affected by potential toxicity from long-term use of nivolumab
Yuma Motomura, Shin Urai, Yushi Hirota, Naoki Takegawa, Hironori Bando, Masaaki Yamamoto, Hidenori Fukuoka, Masahiro Tsuda, Wataru Ogawa
Diabetology International.2024; 15(1): 130. CrossRef - Review – The impact of pharmacogenetics on the outcome of immune checkpoint inhibitors
Karlijn de Joode, Niels Heersche, Edwin A. Basak, Sander Bins, Astrid A.M. van der Veldt, Ron H.N. van Schaik, Ron H.J. Mathijssen
Cancer Treatment Reviews.2024; 122: 102662. CrossRef - Reaching the Diagnosis of Checkpoint Inhibitor-Induced Diabetes Mellitus in Different Clinical Scenarios: A Real-World Application of Updated Diagnostic Criteria
Anna Angelousi, Dimitrios C. Ziogas, Vasiliki Siampanopoulou, Chrysoula Mytareli, Amalia Anastasopoulou, George Lyrarakis, Helen Gogas
Diseases.2024; 12(2): 40. CrossRef - Non-Invasive Predictive Biomarkers for Immune-Related Adverse Events Due to Immune Checkpoint Inhibitors
Ben Ponvilawan, Abdul Wali Khan, Janakiraman Subramanian, Dhruv Bansal
Cancers.2024; 16(6): 1225. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - A single center case series of immune checkpoint inhibitor-induced type 1 diabetes mellitus, patterns of disease onset and long-term clinical outcome
John Marsiglio, Jordan P. McPherson, Magdalena Kovacsovics-Bankowski, Joanne Jeter, Christos Vaklavas, Umang Swami, Douglas Grossmann, Alyssa Erickson-Wayman, Heloisa P. Soares, Katie Kerrigan, Berit Gibson, Jennifer Anne Doherty, John Hyngstrom, Sheetal
Frontiers in Immunology.2023;[Epub] CrossRef - Predictive Biomarkers for Immune-Related Endocrinopathies following Immune Checkpoint Inhibitors Treatment
Almog Shalit, Panagiotis Sarantis, Evangelos Koustas, Eleni-Myrto Trifylli, Dimitris Matthaios, Michalis V. Karamouzis
Cancers.2023; 15(2): 375. CrossRef - Predictive Biomarkers for Checkpoint Inhibitor Immune-Related Adverse Events
Iñigo Les, Mireia Martínez, Inés Pérez-Francisco, María Cabero, Lucía Teijeira, Virginia Arrazubi, Nuria Torrego, Ana Campillo-Calatayud, Iñaki Elejalde, Grazyna Kochan, David Escors
Cancers.2023; 15(5): 1629. CrossRef - Amino acid polymorphisms in human histocompatibility leukocyte antigen class II and proinsulin epitope have impacts on type 1 diabetes mellitus induced by immune-checkpoint inhibitors
Hidefumi Inaba, Shuhei Morita, Daisuke Kosugi, Yuki Asai, Yosuke Kaido, Saya Ito, Tomonao Hirobata, Gen Inoue, Yuki Yamamoto, Masatoshi Jinnin, Hiroaki Kimura, Masao Ota, Yuko Okudaira, Hiroyasu Nakatani, Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima, T
Frontiers in Immunology.2023;[Epub] CrossRef - Clinical characteristics and human leukocyte antigens in patients with immune checkpoint inhibitor-induced type 1 diabetes and pituitary dysfunction: a single center prospective study
Natsuko Hara, Hirotsugu Suwanai, Fumiyoshi Yakou, Keitaro Ishii, Hajime Iwasaki, Hironori Abe, Jumpei Shikuma, Hiroyuki Sakai, Takashi Miwa, Ryo Suzuki
Endocrine.2023; 81(3): 477. CrossRef - Autoimmunity in immune checkpoint inhibitor‐induced immune‐related adverse events: A focus on autoimmune skin toxicity and pneumonitis
Fiamma Berner, Lukas Flatz
Immunological Reviews.2023; 318(1): 37. CrossRef - Prediction-based prompt levothyroxine replacement to prevent a hypothyroid state after immune-related adverse events involving the thyroid gland
Ichiro Yamauchi, Takuro Hakata, Taku Sugawa, Daisuke Kosugi, Haruka Fujita, Kentaro Okamoto, Yohei Ueda, Toshihito Fujii, Daisuke Taura, Norio Harada, Nobuya Inagaki
Endocrine Journal.2023; 70(10): 987. CrossRef - Key Determinants of Immune-Mediated Adverse Reactions to Oncology Drugs
Yihan Zhou, Shan Ding
Cancers.2023; 15(23): 5622. CrossRef - Risk factors and predictors of immune-related adverse events: implications for patients with non-small cell lung cancer
Majd Issa, Joy Tang, Yizhen Guo, Chris Coss, Thomas A. Mace, Jason Bischof, Mitch Phelps, Carolyn J Presley, Dwight H Owen
Expert Review of Anticancer Therapy.2022; 22(8): 861. CrossRef - Risk Factors and Biomarkers for Immune-Related Adverse Events: A Practical Guide to Identifying High-Risk Patients and Rechallenging Immune Checkpoint Inhibitors
Adithya Chennamadhavuni, Laith Abushahin, Ning Jin, Carolyn J. Presley, Ashish Manne
Frontiers in Immunology.2022;[Epub] CrossRef - Flash Glucose Monitoring and Diabetes Mellitus Induced by Immune Checkpoint Inhibitors: An Approach to Clinical Practice
Pablo Rodríguez de Vera-Gómez, Ana Piñar-Gutiérrez, Raquel Guerrero-Vázquez, Virginia Bellido, Cristóbal Morales-Portillo, María Pilar Sancho-Márquez, Pablo Espejo-García, Noelia Gros-Herguido, Gema López-Gallardo, María Asunción Martínez-Brocca, Alfonso
Journal of Diabetes Research.2022; 2022: 1. CrossRef
- Type 1 diabetes mellitus affected by potential toxicity from long-term use of nivolumab

- Thyroid
- Whole-Exome Sequencing in Papillary Microcarcinoma: Potential Early Biomarkers of Lateral Lymph Node Metastasis
- Mijin Kim, Chae Hwa Kwon, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, Kyung-Un Choi, In Joo Kim, Meeyoung Park, Bo Hyun Kim
- Endocrinol Metab. 2021;36(5):1086-1094. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1132
- 3,593 View
- 109 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
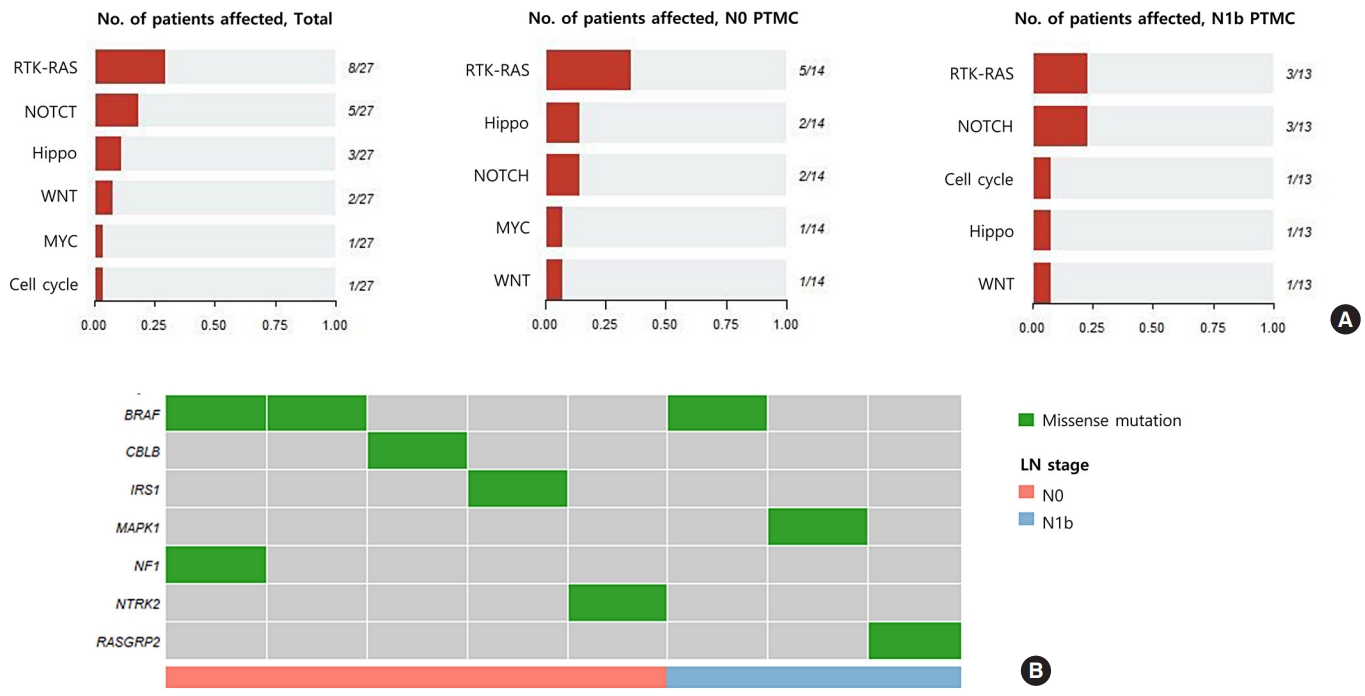
Early identification of patients with high-risk papillary thyroid microcarcinoma (PTMC) that is likely to progress has become a critical challenge. We aimed to identify somatic mutations associated with lateral neck lymph node (LN) metastasis (N1b) in patients with PTMC.
Methods
Whole-exome sequencing (WES) of 14 PTMCs with no LN metastasis (N0) and 13 N1b PTMCs was performed using primary tumors and matched normal thyroid tissues.
Results
The mutational burden was comparable in N0 and N1b tumors, as the median number of mutations was 23 (range, 12 to 46) in N0 and 24 (range, 12 to 50) in N1b PTMC (P=0.918). The most frequent mutations were detected in PGS1, SLC4A8, DAAM2, and HELZ in N1b PTMCs alone, and the K158Q mutation in PGS1 (four patients, Fisher’s exact test P=0.041) was significantly enriched in N1b PTMCs. Based on pathway analysis, somatic mutations belonging to the receptor tyrosine kinase-RAS and NOTCH pathways were most frequently affected in N1b PTMCs. We identified four mutations that are predicted to be pathogenic in four genes based on Clinvar and Combined Annotation-Dependent Depletion score: BRAF, USH2A, CFTR, and PHIP. A missense mutation in CFTR and a nonsense mutation in PHIP were detected in N1b PTMCs only, although in one case each. BRAF mutation was detected in both N0 and N1b PTMCs.
Conclusion
This first comprehensive WES analysis of the mutational landscape of N0 and N1b PTMCs identified pathogenic genes that affect biological functions associated with the aggressive phenotype of PTMC. -
Citations
Citations to this article as recorded by- What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?
Bobby White, Pawel Swietach
Pflügers Archiv - European Journal of Physiology.2024; 476(4): 673. CrossRef - Comprehensive Long-Read Sequencing Analysis Discloses the Transcriptome Features of Papillary Thyroid Microcarcinoma
Yanqiang Wang, Binbin Zou, Yanyan Zhang, Jin Zhang, Shujing Li, Bo Yu, Zhekun An, Lei Li, Siqian Cui, Yutong Zhang, Jiali Yao, Xiuzhi Shi, Jing Liu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(5): 1263. CrossRef - Feasibility of whole‐exome sequencing in fine‐needle aspiration specimens of papillary thyroid microcarcinoma for the identification of novel gene mutations
Liyuan Ma, Luying Gao, Ya Hu, Xiaoyi Li, Chunhao Liu, Jiang Ji, Xinlong Shi, Aonan Pan, Yuang An, Nengwen Luo, Yu Xia, Yuxin Jiang
Clinical Genetics.2024; 105(5): 567. CrossRef - Multi-omics analysis reveals a molecular landscape of the early recurrence and early metastasis in pan-cancer
Dan-ni He, Na Wang, Xiao-Ling Wen, Xu-Hua Li, Yu Guo, Shu-heng Fu, Fei-fan Xiong, Zhe-yu Wu, Xu Zhu, Xiao-ling Gao, Zhen-zhen Wang, Hong-jiu Wang
Frontiers in Genetics.2023;[Epub] CrossRef
- What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?

- Diabetes, Obesity and Metabolism
- Association of Protein Z with Prediabetes and Type 2 Diabetes
- Yun-Ui Bae, Ji Hong You, Nan Hee Cho, Leah Eunjung Kim, Hye Min Shim, Jae-Hyung Park, Ho Chan Cho
- Endocrinol Metab. 2021;36(3):637-646. Published online June 2, 2021
- DOI: https://doi.org/10.3803/EnM.2021.962

- 5,164 View
- 147 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes mellitus (T2DM) is a progressive metabolic disease. Early detection of prediabetes is important to reduce the risk of T2DM. Some cytokines are known to be associated with T2DM. Therefore, we aimed to identify cytokines as novel biomarkers of glucose dysmetabolism.
Methods
The first stage of the study included 43 subjects (13 subjects with newly diagnosed T2DM, 13 with prediabetes, and 16 with normoglycemia) for cytokine microarray analysis. Blood samples of the subjects were assessed for 310 cytokines to identify potential indicators of prediabetes. The second stage included 142 subjects (36 subjects with T2DM, 35 with prediabetes, and 71 with normoglycemia) to validate the potential cytokines associated with prediabetes.
Results
We identified 41 cytokines that differed by 1.5-fold or more in at least one out of the three comparisons (normoglycemia vs. prediabetes, normoglycemia vs. T2DM, and prediabetes vs. T2DM) among 310 cytokines. Finally, we selected protein Z (PROZ) and validated this finding to determine its association with prediabetes. Plasma PROZ levels were found to be decreased in patients with prediabetes (1,490.32±367.19 pg/mL) and T2DM (1,583.34±465.43 pg/mL) compared to those in subjects with normoglycemia (1,864.07±450.83 pg/mL) (P<0.001). There were significantly negative correlations between PROZ and fasting plasma glucose (P=0.001) and hemoglobin A1c (P=0.010).
Conclusion
PROZ levels were associated with prediabetes and T2DM. We suggest that PROZ may be a promising biomarker for the early detection of prediabetes. Further large-scale studies are needed to evaluate the relationship and mechanism between PROZ and prediabetes and T2DM. -
Citations
Citations to this article as recorded by- On the human health benefits of microalgal phytohormones: An explorative in silico analysis
Angelo Del Mondo, Annamaria Vinaccia, Luigi Pistelli, Christophe Brunet, Clementina Sansone
Computational and Structural Biotechnology Journal.2023; 21: 1092. CrossRef - Role of F-box WD Repeat Domain Containing 7 in Type 1 Diabetes
Sarah W. Mohammed, Zainab M. Qassam, Ekhlass M. Taha, Nameer M. Salih
Ibn AL-Haitham Journal For Pure and Applied Sciences.2023; 36(3): 167. CrossRef - Identification of Protein Z as a Potential Novel Biomarker for the Diagnosis of Prediabetes
Seung-Hoi Koo
Endocrinology and Metabolism.2021; 36(3): 572. CrossRef - Association of Protein Z with Prediabetes and Type 2 Diabetes (Endocrinol Metab 2021;36:637-46, Yun-Ui Bae et al.)
Ji Hong You, Yun-Ui Bae, Ho Chan Cho
Endocrinology and Metabolism.2021; 36(5): 1149. CrossRef - Association of Protein Z with Prediabetes and Type 2 Diabetes (Endocrinol Metab 2021;36:637-46, Yun-Ui Bae et al.)
Tiffany Pascreau, Maia Tchikviladze, Emilie Jolly, Sara Zia-Chahabi, Bertrand Lapergue, Marc Vasse
Endocrinology and Metabolism.2021; 36(5): 1147. CrossRef
- On the human health benefits of microalgal phytohormones: An explorative in silico analysis

- Endocrine Research
- Effect of CCL11 on In Vitro Myogenesis and Its Clinical Relevance for Sarcopenia in Older Adults
- Da Ae Kim, So Jeong Park, Jin Young Lee, Jeoung Hee Kim, Seungjoo Lee, Eunju Lee, Il-Young Jang, Hee-Won Jung, Jin Hoon Park, Beom-Jun Kim
- Endocrinol Metab. 2021;36(2):455-465. Published online April 14, 2021
- DOI: https://doi.org/10.3803/EnM.2020.942

- 5,190 View
- 146 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The C-C motif chemokine ligand 11 (CCL11) has been receiving attention as a potential pro-aging factor. Accordingly, it may be involved in muscle metabolism and sarcopenia, a key component of aging phenotypes. To clarify this potential, we investigated the effects of CCL11 on in vitro muscle biology and its clinical relevance for sarcopenia parameters in older adults.
Methods
Myogenesis was induced in mouse C2C12 myoblasts with 2% horse serum. Human blood samples were collected from 79 participants who underwent a functional assessment. Thereafter, CCL11 level was measured using a quantikine ELISA kit. Sarcopenia was defined using the Asian-specific guideline.
Results
Recombinant CCL11 treatment significantly stimulated myogenesis in a dose-dependent manner, and consistently increased the expression of myogenic differentiation markers. Among the C-C chemokine receptors (CCRs), CCR5, not CCR2 and CCR3, was predominantly expressed in muscle cells. Further, the CCR5 inhibitor blocked recombinant CCL11-stimulated myogenesis. In a clinical study, serum CCL11 level was not significantly different according to the status of sarcopenia, low muscle mass, weak muscle strength, and poor physical performance, and was not associated with skeletal muscle index, grip strength, short physical performance battery score, gait speed, and time to complete 5 chair stands, after adjusting for sex, age, and body mass index.
Conclusion
Contrary to expectations, CCL11 exerted beneficial effects on muscle metabolism at least in vitro system. However, its impact on human muscle health was not evident, suggesting that circulating CCL11 may not be a useful biomarker for sarcopenia risk assessment in older adults. -
Citations
Citations to this article as recorded by- Mapping the causal associations of cytokines with sarcopenia and aging traits: Evidence from bidirectional Mendelian randomization
Mingchong Liu, Xiao Fu, Daqian Yu, Meng Li, Yutao Pan, Chensong Yang, Guixin Sun
Journal of Cachexia, Sarcopenia and Muscle.2024;[Epub] CrossRef - C-C motif chemokine CCL11 is a novel regulator and a potential therapeutic target in non-alcoholic fatty liver disease
Zhiwen Fan, Xinyue Sun, Xuelian Chen, Huimin Liu, Xiulian Miao, Yan Guo, Yong Xu, Jie Li, Xiaoping Zou, Zilong Li
JHEP Reports.2023; : 100754. CrossRef - C–C motif chemokine CCL11 is a novel regulator and a potential therapeutic target in non-alcoholic fatty liver disease
Zhiwen Fan, Xinyue Sun, Xuelian Chen, Huimin Liu, Xiulian Miao, Yan Guo, Yong Xu, Jie Li, Xiaoping Zou, Zilong Li
JHEP Reports.2023; 5(9): 100805. CrossRef - Lumican Inhibits Osteoclastogenesis and Bone Resorption by Suppressing Akt Activity
Jin-Young Lee, Da-Ae Kim, Eun-Young Kim, Eun-Ju Chang, So-Jeong Park, Beom-Jun Kim
International Journal of Molecular Sciences.2021; 22(9): 4717. CrossRef - Aldosterone Inhibits In Vitro Myogenesis by Increasing Intracellular Oxidative Stress via Mineralocorticoid Receptor
Jin Young Lee, Da Ae Kim, Eunah Choi, Yun Sun Lee, So Jeong Park, Beom-Jun Kim
Endocrinology and Metabolism.2021; 36(4): 865. CrossRef
- Mapping the causal associations of cytokines with sarcopenia and aging traits: Evidence from bidirectional Mendelian randomization

- Clinical Study
- Lactate Dehydrogenase A as a Potential New Biomarker for Thyroid Cancer
- Eun Jeong Ban, Daham Kim, Jin Kyong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Kunhong Kim
- Endocrinol Metab. 2021;36(1):96-105. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.819

- 5,809 View
- 188 Download
- 14 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Several cancers show increased levels of lactate dehydrogenase A (LDHA), which are associated with cancer progression. However, it remains unclear whether LDHA levels are associated with papillary thyroid cancer (PTC) aggressiveness or with the presence of the PTC prognostic marker, the BRAFV600E mutation. This study aimed to evaluate the potential of LDHA as a PTC prognostic marker.
Methods
LDHA expression was examined in 83 PTC tissue specimens by immunohistochemistry. Human thyroid cell lines were genetically manipulated to overexpress BRAFV600E or were treated with a BRAF-specific short hairpin RNA (shBRAF), whose effects on LDHA expression were evaluated by Western blotting. Data from 465 PTC patients were obtained from The Cancer Genome Atlas (TCGA) database and analyzed to validate the in vitro results.
Results
LDHA was aberrantly overexpressed in PTC. Intense immunostaining for LDHA was observed in PTC specimens carrying mutated BRAF, whereas the intensity was less in wild-type BRAF samples. Overexpression of BRAFV600E resulted in LDHA upregulation, whereas treatment with shBRAF downregulated LDHA in human thyroid cell lines. Furthermore, LDHA mRNA expression was significantly elevated and associated with BRAFV600E expression in thyroid cancer tissues from TCGA database. Additionally, LDHA overexpression was found to be correlated with aggressive clinical features of PTC, such as lymph node metastases and advanced tumor stages.
Conclusion
LDHA overexpression is associated with the BRAFV600E mutation and an aggressive PTC behavior. Therefore, LDHA may serve as a biomarker and therapeutic target in PTC. -
Citations
Citations to this article as recorded by- Integrated proteogenomic and metabolomic characterization of papillary thyroid cancer with different recurrence risks
Ning Qu, Di Chen, Ben Ma, Lijun Zhang, Qiuping Wang, Yuting Wang, Hongping Wang, Zhaoxian Ni, Wen Wang, Tian Liao, Jun Xiang, Yulong Wang, Shi Jin, Dixin Xue, Weili Wu, Yu Wang, Qinghai Ji, Hui He, Hai-long Piao, Rongliang Shi
Nature Communications.2024;[Epub] CrossRef - Peripheral lymphocytes and lactate dehydrogenase correlate with response and survival in head and neck cancers treated with immune checkpoint inhibitors
Cassie Pan, Qian Vicky Wu, Jenna Voutsinas, Jeffrey J. Houlton, Brittany Barber, Zain H. Rizvi, Emily Marchiano, Neal Futran, George E. Laramore, Jay J. Liao, Upendra Parvathaneni, Renato G. Martins, Jonathan R. Fromm, Cristina P. Rodriguez
Cancer Medicine.2023; 12(8): 9384. CrossRef - LncRNA GLTC targets LDHA for succinylation and enzymatic activity to promote progression and radioiodine resistance in papillary thyroid cancer
Liang Shi, Rui Duan, Zhenhua Sun, Qiong Jia, Wenyu Wu, Feng Wang, Jianjun Liu, Hao Zhang, Xue Xue
Cell Death & Differentiation.2023; 30(6): 1517. CrossRef - Integrated analysis of circulating and tissue proteomes reveals that fibronectin 1 is a potential biomarker in papillary thyroid cancer
Guochao Ye, Xiaomei Zhang, Mansheng Li, Zixiang Lin, Yongcan Xu, Haoru Dong, Jie Zhou, Jiaqi Zhang, Sheng Wang, Yunping Zhu, Xiaobo Yu, Xu Qian
BMC Cancer.2023;[Epub] CrossRef - Targeting metabolism by B-raf inhibitors and diclofenac restrains the viability of BRAF-mutated thyroid carcinomas with Hif-1α-mediated glycolytic phenotype
Marianna Aprile, Simona Cataldi, Caterina Perfetto, Antonio Federico, Alfredo Ciccodicola, Valerio Costa
British Journal of Cancer.2023; 129(2): 249. CrossRef - circNFATC3 facilitated the progression of oral squamous cell carcinoma via the miR-520h/LDHA axis
Hongguo Xie, Xiaopeng Lu
Open Medicine.2023;[Epub] CrossRef - The potential role of reprogrammed glucose metabolism: an emerging actionable codependent target in thyroid cancer
Sai-li Duan, Min Wu, Zhe-Jia Zhang, Shi Chang
Journal of Translational Medicine.2023;[Epub] CrossRef - CENPE and LDHA were potential prognostic biomarkers of chromophobe renal cell carcinoma
Hui-feng Wu, Hao Liu, Zhe-wei Zhang, Ji-min Chen
European Journal of Medical Research.2023;[Epub] CrossRef - Classification for Staging and Managing Patients with Biopolymer-induced Human Adjuvant Disease
Jaime Eduardo Pachón Suárez, Marcela C. Salazar, Victor Z. Rizo
Plastic and Reconstructive Surgery - Global Open.2022; 10(2): e4137. CrossRef - Development of Metabolic Synthetic Lethality and Its Implications for Thyroid Cancer
Sang-Hyeon Ju, Seong Eun Lee, Yea Eun Kang, Minho Shong
Endocrinology and Metabolism.2022; 37(1): 53. CrossRef - Drug delivery for metabolism targeted cancer immunotherapy
Taravat Khodaei, Sahil Inamdar, Abhirami P. Suresh, Abhinav P. Acharya
Advanced Drug Delivery Reviews.2022; 184: 114242. CrossRef - Sulfur quantum dot based fluorescence assay for lactate dehydrogenase activity detection
Shengnan Fan, Xiaoqing Li, Fanghui Ma, Minghui Yang, Juan Su, Xiang Chen
Journal of Photochemistry and Photobiology A: Chemistry.2022; 430: 113989. CrossRef - STAT3/LINC00671 axis regulates papillary thyroid tumor growth and metastasis via LDHA-mediated glycolysis
Nan Huo, Rui Cong, Zhi-jia Sun, Wen-chao Li, Xiang Zhu, Chun-yuan Xue, Zhao Chen, Lu-yuan Ma, Zhong Chu, Yu-chen Han, Xiao-feng Kang, Song-hao Jia, Nan Du, Lei Kang, Xiao-jie Xu
Cell Death & Disease.2021;[Epub] CrossRef
- Integrated proteogenomic and metabolomic characterization of papillary thyroid cancer with different recurrence risks

- Obesity and Metabolism
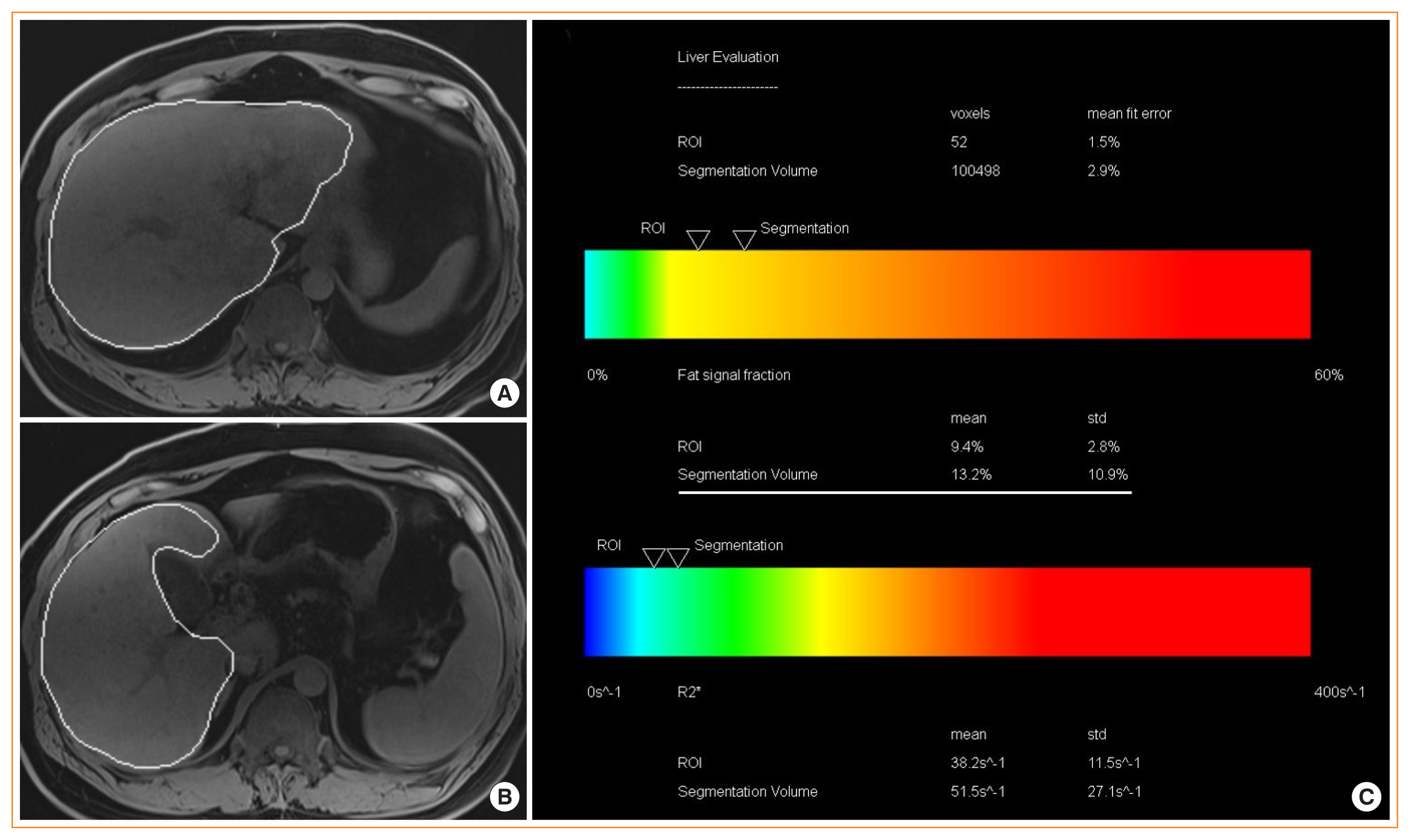
- Noninvasive Evaluation of Nonalcoholic Fatty Liver Disease
- Dae Ho Lee
- Endocrinol Metab. 2020;35(2):243-259. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.243
- 11,045 View
- 296 Download
- 19 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Nonalcoholic fatty liver disease (NAFLD) is the most prevalent liver diseases and can progress to advanced fibrosis and end-stage liver disease. Thus, intensive research has been performed to develop noninvasive methods for the diagnosis of nonalcoholic steatohepatitis (NASH) and fibrosis. Currently, no single noninvasive tool covers all of the stages of pathologies and conditions of NAFLD, and the cost and feasibility of known techniques are also important issues. Blood biomarkers for NAFLD may be useful to select subjects who need ultrasonography (US) screening for NAFLD, and noninvasive tools for assessing fibrosis may be helpful to exclude the probability of significant fibrosis and to predict advanced fibrosis, thus guiding the decision of whether to perform liver biopsy in patients with NAFLD. Among various methods, magnetic resonance-based methods have been shown to perform better than other methods in assessing steatosis as well as in detecting hepatic fibrosis. Many genetic markers are associated with the development and progression of NAFLD. Further well-designed studies are needed to determine which biomarker panels, imaging studies, genetic marker panels, or combinations thereof perform well for diagnosing NAFLD, differentiating NASH and fibrosis, and following-up NAFLD, respectively.
-
Citations
Citations to this article as recorded by- Recent Progresses on Pathophysiology, Diagnosis, Therapeutic Modalities,
and Management of Non-alcoholic Fatty Liver Disorder
Mahdi Barazesh, Sajad Jalili, Morteza Akhzari, Fouzieyeh Faraji, Ebrahim Khorramdin
Current Drug Therapy.2024; 19(1): 20. CrossRef - Intact ketogenesis predicted reduced risk of moderate-severe metabolic-associated fatty liver disease assessed by liver transient elastography in newly diagnosed type 2 diabetes
Sejeong Lee, Jaehyun Bae, Seung Up Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Non-invasive diagnosis and monitoring of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis
Monica A Tincopa, Rohit Loomba
The Lancet Gastroenterology & Hepatology.2023; 8(7): 660. CrossRef - Hepatic Involvement across the Metabolic Syndrome Spectrum: Non-Invasive Assessment and Risk Prediction Using Machine Learning
Adelaida Solomon, Călin Remus Cipăian, Mihai Octavian Negrea, Adrian Boicean, Romeo Mihaila, Corina Beca, Mirela Livia Popa, Sebastian Mihai Grama, Minodora Teodoru, Bogdan Neamtu
Journal of Clinical Medicine.2023; 12(17): 5657. CrossRef - Greater Severity of Steatosis Is Associated with a Higher Risk of Incident Diabetes: A Retrospective Longitudinal Study
Ji Min Han, Jung Hwan Cho, Hye In Kim, Sunghwan Suh, Yu-Ji Lee, Jung Won Lee, Kwang Min Kim, Ji Cheol Bae
Endocrinology and Metabolism.2023; 38(4): 418. CrossRef - Advances in Noninvasive Biomarkers for Nonalcoholic Fatty Liver Disease
Georgiana-Emmanuela Gîlcă-Blanariu, Daniela Simona Budur, Dana Elena Mitrică, Elena Gologan, Oana Timofte, Gheorghe Gh Bălan, Vasile Andrei Olteanu, Gabriela Ștefănescu
Metabolites.2023; 13(11): 1115. CrossRef - Plasma Aldo-Keto Reductase Family 1 Member B10 as a Biomarker Performs Well in the Diagnosis of Nonalcoholic Steatohepatitis and Fibrosis
Aron Park, Seung Joon Choi, Sungjin Park, Seong Min Kim, Hye Eun Lee, Minjae Joo, Kyoung Kon Kim, Doojin Kim, Dong Hae Chung, Jae Been Im, Jaehun Jung, Seung Kak Shin, Byung-Chul Oh, Cheolsoo Choi, Seungyoon Nam, Dae Ho Lee
International Journal of Molecular Sciences.2022; 23(9): 5035. CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - The Impact of Insulin Resistance on Hepatic Fibrosis among United States Adults with Non-Alcoholic Fatty Liver Disease: NHANES 2017 to 2018
Ji Cheol Bae, Lauren A. Beste, Kristina M. Utzschneider
Endocrinology and Metabolism.2022; 37(3): 455. CrossRef - Plasma Metabolomics and Machine Learning-Driven Novel Diagnostic Signature for Non-Alcoholic Steatohepatitis
Moongi Ji, Yunju Jo, Seung Joon Choi, Seong Min Kim, Kyoung Kon Kim, Byung-Chul Oh, Dongryeol Ryu, Man-Jeong Paik, Dae Ho Lee
Biomedicines.2022; 10(7): 1669. CrossRef - Evaluation of Liver Changes in Type-2 Diabetes Mellitus Patients using Computed Tomography
Nayyar Ashfaq, Akash John, Abid Ali, Amina Sharif Bhatti, Hateem Qaiser
DIET FACTOR (Journal of Nutritional & Food Sciences).2022; : 14. CrossRef - Accuracy of FIB-4 to Detect Elevated Liver Stiffness Measurements in Patients with Non-Alcoholic Fatty Liver Disease: A Cross-Sectional Study in Referral Centers
Mauro Viganò, Nicola Pugliese, Federica Cerini, Federica Turati, Vincenzo Cimino, Sofia Ridolfo, Simone Rocchetto, Francesca Foglio, Maria Terrin, Carlo La Vecchia, Maria Grazia Rumi, Alessio Aghemo
International Journal of Molecular Sciences.2022; 23(20): 12489. CrossRef - MAFLD vs. NAFLD: shared features and potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy
Ying-Xin Xian, Jian-Ping Weng, Fen Xu
Chinese Medical Journal.2021; 134(1): 8. CrossRef - Prognostic accuracy of FIB‐4, NAFLD fibrosis score and APRI for NAFLD‐related events: A systematic review
Jenny Lee, Yasaman Vali, Jerome Boursier, Rene Spijker, Quentin M. Anstee, Patrick M. Bossuyt, Mohammad H. Zafarmand
Liver International.2021; 41(2): 261. CrossRef - Serum syndecan‐4 is associated with nonalcoholic fatty liver disease
Shu Jing Xia, Li Zhong Tang, Wen Hua Li, Zhao Shan Xu, Li Li Zhang, Feng Gan Cheng, Hong Xia Chen, Zi Hua Wang, Yu Cheng Luo, An Na Dai, Jian Gao Fan
Journal of Digestive Diseases.2021; 22(9): 536. CrossRef - Non-Laboratory-Based Simple Screening Model for Nonalcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Developed Using Multi-Center Cohorts
Jiwon Kim, Minyoung Lee, Soo Yeon Kim, Ji-Hye Kim, Ji Sun Nam, Sung Wan Chun, Se Eun Park, Kwang Joon Kim, Yong-ho Lee, Joo Young Nam, Eun Seok Kang
Endocrinology and Metabolism.2021; 36(4): 823. CrossRef - Pemafibrate Ameliorates Liver Dysfunction and Fatty Liver in Patients with Non-Alcoholic Fatty Liver Disease with Hypertriglyceridemia: A Retrospective Study with the Outcome after a Mid-Term Follow-Up
Suguru Ikeda, Takaaki Sugihara, Takuya Kihara, Yukako Matsuki, Takakazu Nagahara, Tomoaki Takata, Sonoko Kitao, Tsuyoshi Okura, Kazuhiro Yamamoto, Hajime Isomoto
Diagnostics.2021; 11(12): 2316. CrossRef - Triglyceride Glucose-Waist Circumference Is Superior to the Homeostasis Model Assessment of Insulin Resistance in Identifying Nonalcoholic Fatty Liver Disease in Healthy Subjects
Hwi Seung Kim, Yun Kyung Cho, Eun Hee Kim, Min Jung Lee, Chang Hee Jung, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee
Journal of Clinical Medicine.2021; 11(1): 41. CrossRef - The Leg Fat to Total Fat Ratio Is Associated with Lower Risks of Non-Alcoholic Fatty Liver Disease and Less Severe Hepatic Fibrosis: Results from Nationwide Surveys (KNHANES 2008–2011)
Hyun Min Kim, Yong-ho Lee
Endocrinology and Metabolism.2021; 36(6): 1232. CrossRef
- Recent Progresses on Pathophysiology, Diagnosis, Therapeutic Modalities,
and Management of Non-alcoholic Fatty Liver Disorder

- Bone Metabolism
- Potential Biomarkers to Improve the Prediction of Osteoporotic Fractures
- Beom-Jun Kim, Seung Hun Lee, Jung-Min Koh
- Endocrinol Metab. 2020;35(1):55-63. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.55
- 4,797 View
- 115 Download
- 14 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
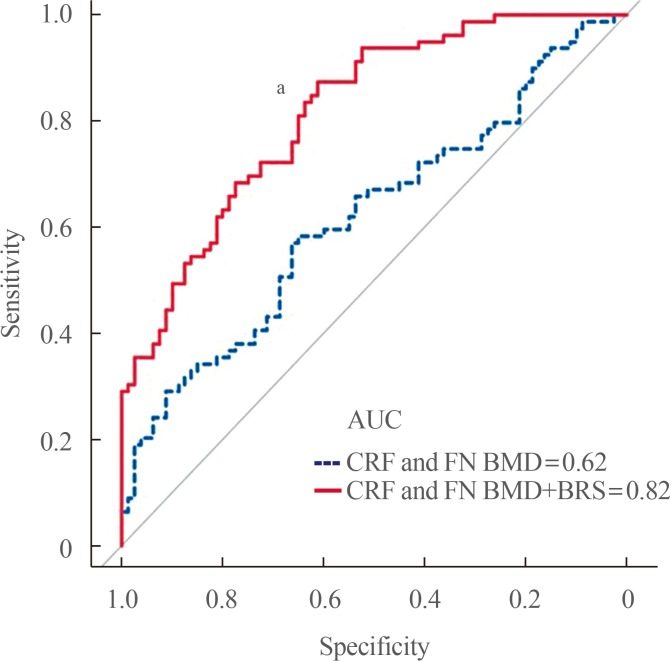
ePub Osteoporotic fracture (OF) is associated with high disability and morbidity rates. The burden of OF may be reduced by early identification of subjects who are vulnerable to fracture. Although the current fracture risk assessment model includes clinical risk factors (CRFs) and bone mineral density (BMD), its overall ability to identify individuals at high risk for fracture remains suboptimal. Efforts have therefore been made to identify potential biomarkers that can predict the risk of OF, independent of or combined with CRFs and BMD. This review highlights the emerging biomarkers of bone metabolism, including sphongosine-1-phosphate, leucine-rich repeat-containing 17, macrophage migration inhibitory factor, sclerostin, receptor activator of nuclear factor-κB ligand, and periostin, and the importance of biomarker risk score, generated by combining these markers, in enhancing the accuracy of fracture prediction.
-
Citations
Citations to this article as recorded by- The administration of bovine hydroxyapatite-alendronate implant accelerates bone defect healing in an osteoporotic rat
Toetik Aryani, Aniek Setiya Budiatin, Samirah, Aulia Maulidina, Aulia Intan Firdaus, Maria Apriliani Gani, Khoirotin Nisak, Junaidi Khotib, Alvi Jauharotus Syukriya
Technology and Health Care.2023; 31(5): 1747. CrossRef - Impact of Intravenous Iron Substitution on Serum Phosphate Levels and Bone Turnover Markers—An Open-Label Pilot Study
Alexandra Struppe, Jakob E. Schanda, Andreas Baierl, Paul Watzl, Christian Muschitz
Nutrients.2023; 15(12): 2693. CrossRef - Dynamics of Bone Disease Biomarkers Dickkopf-1 and Sclerostin in Patients with Multiple Myeloma
Vladimir Gerov, Daniela Gerova, Ilina Micheva, Miglena Nikolova, Galya Mihaylova, Bistra Galunska
Journal of Clinical Medicine.2023; 12(13): 4440. CrossRef - Impact of vitamin D supplementation on markers of bone turnover: Systematic review and meta‐analysis of randomised controlled trials
Mohammad Hassan Sohouli, Sicong Wang, Faisal Almuqayyid, Mariana Papini Gabiatti, Fateme Mozaffari, Zahra Mohamadian, Nazanin Koushki, Kamar Allayl Alras, Abdullah M. AlHossan, Saud K. Albatati, Aya Alfardous Alazm, Saeed Baradwan, Mihnea‐Alexandru Găman,
European Journal of Clinical Investigation.2023;[Epub] CrossRef - Night shift work and serum markers of bone turnover in male shift workers
Margherita Martelli, Gianmaria Salvio, Raffaella Lazzarini, Marijana Milinkovic, Alessandro Ciarloni, Giancarlo Balercia, Lory Santarelli, Massimo Bracci
Chronobiology International.2023; 40(9): 1270. CrossRef - Circulating sRANKL, Periostin, and Osteopontin as Biomarkers for the Assessment of Activated Osteoclastogenesis in Myeloma Related Bone Disease
Vladimir Gerov, Daniela Gerova, Ilina Micheva, Miglena Nikolova, Milena Pasheva, Neshe Nazifova, Bistra Galunska
Cancers.2023; 15(23): 5562. CrossRef - Oral Administration of Isovitexin, a Naturally Occurring Apigenin Derivative Showed Osteoanabolic Effect in Ovariectomized Mice: A Comparative Study with Teriparatide
Subhashis Pal, Shivani Sharma, Konica Porwal, Mohammed Riyazuddin, Chirag Kulkarni, Sourav Chattopadhyay, Sabyasachi Sanyal, Jiaur R. Gayen, Naibedya Chattopadhyay
Calcified Tissue International.2022; 111(2): 196. CrossRef - Serum sclerostin levels in osteoporotic fracture patients
Erwin A. Gorter, Casper R. Reinders, Pieta Krijnen, Natasha M. Appelman-Dijkstra, Inger B. Schipper
European Journal of Trauma and Emergency Surgery.2022; 48(6): 4857. CrossRef - Elevated gamma-glutamyl transpeptidase level is associated with an increased risk of hip fracture in postmenopausal women
Kyoung Jin Kim, Namki Hong, Min Heui Yu, Seunghyun Lee, Sungjae Shin, Sin Gon Kim, Yumie Rhee
Scientific Reports.2022;[Epub] CrossRef - Effect of androgen deprivation therapy on serum levels of sclerostin, Dickkopf-1, and osteoprotegerin: a cross-sectional and longitudinal analysis
Alice Wang, Nishi Karunasinghe, Lindsay D. Plank, Shuotun Zhu, Sue Osborne, Charis Brown, Karen Bishop, Tiffany Schwass, Sofian Tijono, Michael Holmes, Jonathan Masters, Roger Huang, Christine Keven, Lynnette R. Ferguson, Ross Lawrenson
Scientific Reports.2021;[Epub] CrossRef - Update on Glucocorticoid Induced Osteoporosis
Soo-Kyung Cho, Yoon-Kyoung Sung
Endocrinology and Metabolism.2021; 36(3): 536. CrossRef - Nobiletin promotes osteogenic differentiation of human osteoblastic cell line (MG-63) through activating the BMP-2/RUNX-2 signaling pathway
Ying Pang, Lili Liu, Hong Mu, Vishnu Priya Veeraraghavan
Saudi Journal of Biological Sciences.2021; 28(9): 4916. CrossRef
- The administration of bovine hydroxyapatite-alendronate implant accelerates bone defect healing in an osteoporotic rat


 KES
KES

 First
First Prev
Prev



