Previous issues
- Page Path
- HOME > BROWSE ARTICLES > Previous issues
Review Articles
- Diabetes, Obesity and Metabolism
- Recent Advances in Understanding Peripheral Taste Decoding I: 2010 to 2020
- Jea Hwa Jang, Obin Kwon, Seok Jun Moon, Yong Taek Jeong
- Endocrinol Metab. 2021;36(3):469-477. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2021.302
- 13,640 View
- 374 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
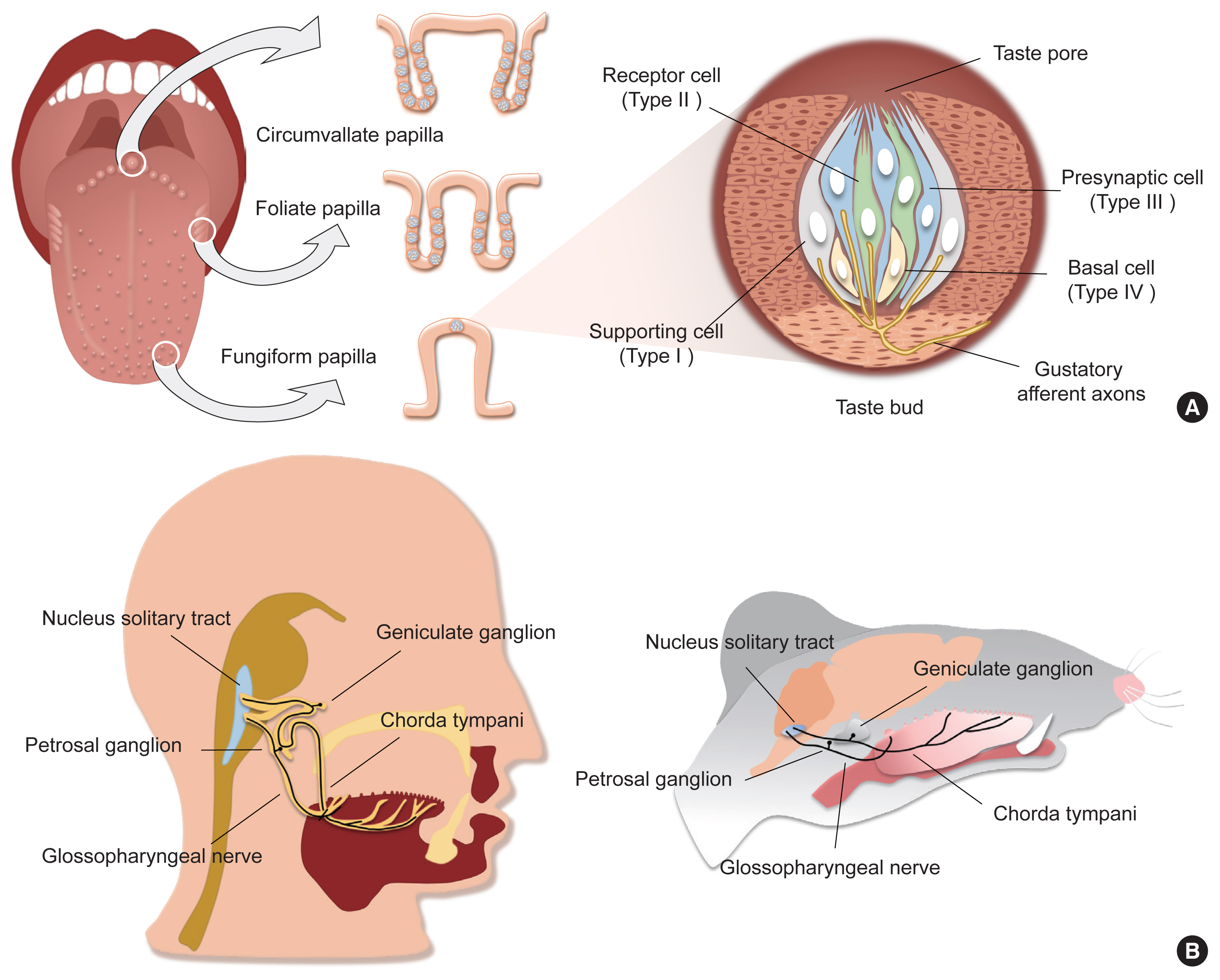
ePub - Taste sensation is the gatekeeper for direct decisions on feeding behavior and evaluating the quality of food. Nutritious and beneficial substances such as sugars and amino acids are represented by sweet and umami tastes, respectively, whereas noxious substances and toxins by bitter or sour tastes. Essential electrolytes including Na+ and other ions are recognized by the salty taste. Gustatory information is initially generated by taste buds in the oral cavity, projected into the central nervous system, and finally processed to provide input signals for food recognition, regulation of metabolism and physiology, and higher-order brain functions such as learning and memory, emotion, and reward. Therefore, understanding the peripheral taste system is fundamental for the development of technologies to regulate the endocrine system and improve whole-body metabolism. In this review article, we introduce previous widely-accepted views on the physiology and genetics of peripheral taste cells and primary gustatory neurons, and discuss key findings from the past decade that have raised novel questions or solved previously raised questions.
-
Citations
Citations to this article as recorded by- Multidimensional exploration of the bitterness amelioration effect of roasting on Wuyi Rock tea
Weiying Su, Li Ni, Yizhe Chen, Daoliang Wang, Chih-Cheng Lin, Yuan Liu, Zhibin Liu
Food Chemistry.2024; 437: 137954. CrossRef - Physiology of the tongue with emphasis on taste transduction
Máire E. Doyle, Hasitha U. Premathilake, Qin Yao, Caio H. Mazucanti, Josephine M. Egan
Physiological Reviews.2023; 103(2): 1193. CrossRef - Polycystic kidney disease 2-like 1 channel contributes to the bitter aftertaste perception of quinine
Takahiro Shimizu, Takuto Fujii, Keisuke Hanita, Ryo Shinozaki, Yusaku Takamura, Yoshiro Suzuki, Teppei Kageyama, Mizuki Kato, Hisao Nishijo, Makoto Tominaga, Hideki Sakai
Scientific Reports.2023;[Epub] CrossRef - Sweet Taste Preference: Relationships with Other Tastes, Liking for Sugary Foods and Exploratory Genome-Wide Association Analysis in Subjects with Metabolic Syndrome
Rebeca Fernández-Carrión, Jose V. Sorlí, Oscar Coltell, Eva C. Pascual, Carolina Ortega-Azorín, Rocío Barragán, Ignacio M. Giménez-Alba, Andrea Alvarez-Sala, Montserrat Fitó, Jose M. Ordovas, Dolores Corella
Biomedicines.2021; 10(1): 79. CrossRef
- Multidimensional exploration of the bitterness amelioration effect of roasting on Wuyi Rock tea

- Diabetes, Obesity and Metabolism
- Receptor-Mediated Muscle Homeostasis as a Target for Sarcopenia Therapeutics
- Jong Hyeon Yoon, Ki-Sun Kwon
- Endocrinol Metab. 2021;36(3):478-490. Published online June 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1081

- 8,841 View
- 335 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Sarcopenia is a disease characterized by age-related decline of skeletal muscle mass and function. The molecular mechanisms of the pathophysiology of sarcopenia form a complex network due to the involvement of multiple interconnected signaling pathways. Therefore, signaling receptors are major targets in pharmacological strategies in general. To provide a rationale for pharmacological interventions for sarcopenia, we herein describe several druggable signaling receptors based on their role in skeletal muscle homeostasis and changes in their activity with aging. A brief overview is presented of the efficacy of corresponding drug candidates under clinical trials. Strategies targeting the androgen receptor, vitamin D receptor, Insulin-like growth factor-1 receptor, and ghrelin receptor primarily focus on promoting anabolic action using natural ligands or mimetics. Strategies involving activin receptors and angiotensin receptors focus on inhibiting catabolic action. This review may help to select specific targets or combinations of targets in the future.
-
Citations
Citations to this article as recorded by- The Current Landscape of Pharmacotherapies for Sarcopenia
Gulistan Bahat, Serdar Ozkok
Drugs & Aging.2024; 41(2): 83. CrossRef - Associations of micronutrient dietary patterns with sarcopenia among US adults: a population-based study
Yining Liu, Xiangliang Liu, Linnan Duan, Yixin Zhao, Yuwei He, Wei Li, Jiuwei Cui
Frontiers in Nutrition.2024;[Epub] CrossRef - Impact of Vitamin D Level on Sarcopenia in Elderly People: A Critical Review
Saniya Khan, Sunil Kumar, Sourya Acharya, Anil Wanjari
Journal of Health and Allied Sciences NU.2023; 13(04): 453. CrossRef - Novel Potential Targets for Function-Promoting Therapies: Orphan Nuclear Receptors, Anti-inflammatory Drugs, Troponin Activators, Mas Receptor Agonists, and Urolithin A
Waly Dioh, Vihang Narkar, Anurag Singh, Fady Malik, Luigi Ferrucci, Cendrine Tourette, Jean Mariani, Rob van Maanen, Roger A Fielding, Lewis A Lipsitz
The Journals of Gerontology: Series A.2023; 78(Supplement): 44. CrossRef - Alverine citrate promotes myogenic differentiation and ameliorates muscle atrophy
Jong Hyeon Yoon, Seung-Min Lee, Younglang Lee, Min Ju Kim, Jae Won Yang, Jeong Yi Choi, Ju Yeon Kwak, Kwang-Pyo Lee, Yong Ryoul Yang, Ki-Sun Kwon
Biochemical and Biophysical Research Communications.2022; 586: 157. CrossRef - Adeno-associated virus-mediated expression of an inactive CaMKIIβ mutant enhances muscle mass and strength in mice
Takahiro Eguchi, Yuji Yamanashi
Biochemical and Biophysical Research Communications.2022; 589: 192. CrossRef - Gastric Mobility and Gastrointestinal Hormones in Older Patients with Sarcopenia
Hsien-Hao Huang, Tse-Yao Wang, Shan-Fan Yao, Pei-Ying Lin, Julia Chia-Yu Chang, Li-Ning Peng, Liang-Kung Chen, David Hung-Tsang Yen
Nutrients.2022; 14(9): 1897. CrossRef - Molecular Mechanisms Underlying Intensive Care Unit-Acquired Weakness and Sarcopenia
Marcela Kanova, Pavel Kohout
International Journal of Molecular Sciences.2022; 23(15): 8396. CrossRef
- The Current Landscape of Pharmacotherapies for Sarcopenia

- Thyroid
- Antithyroid Drug Treatment in Graves’ Disease
- Jae Hoon Chung
- Endocrinol Metab. 2021;36(3):491-499. Published online June 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1070
- 4,973 View
- 338 Download
- 6 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
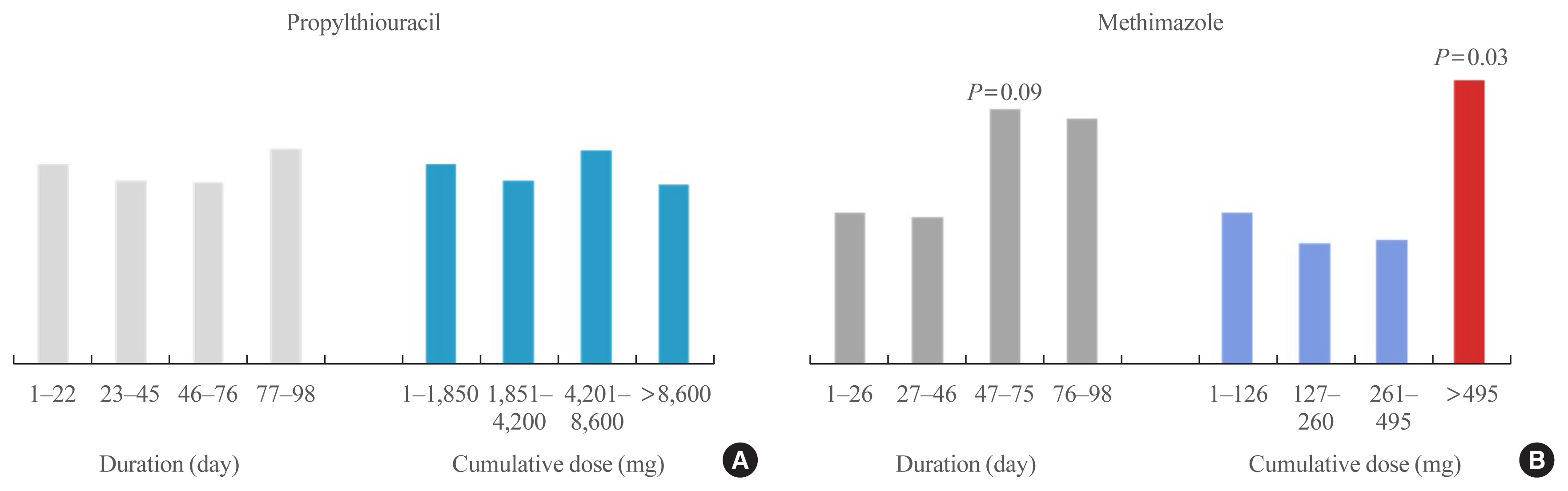
ePub - Graves’ disease is associated with thyrotropin (TSH) receptor stimulating antibody, for which there is no therapeutic agent. This disease is currently treated through inhibition of thyroid hormone synthesis or destruction of the thyroid gland. Recurrence after antithyroid drug (ATD) treatment is common. Recent studies have shown that the longer is the duration of use of ATD, the higher is the remission rate. Considering the relationship between clinical outcomes and iodine intake, recurrence of Graves’ disease is more common in iodine-deficient areas than in iodine-sufficient areas. Iodine restriction in an iodine-excessive area does not improve the effectiveness of ATD or increase remission rates. Recently, Danish and Korean nationwide studies noted significantly higher prevalence of birth defects in newborns exposed to ATD during the first trimester compared to that of those who did not have such exposure. The prevalence of birth defects was lowest when propylthiouracil (PTU) was used and decreased by only 0.15% when methimazole was changed to PTU in the first trimester. Therefore, it is best not to use ATD in the first trimester or to change to PTU before pregnancy.
-
Citations
Citations to this article as recorded by- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза
М. А. Дудина, С. А. Догадин, А. А. Савченко, И. И. Гвоздев
Ateroscleroz.2023; 18(4): 411. CrossRef - Application of oral inorganic iodine in the treatment of Graves’ disease
Yixuan Huang, Yihang Xu, Murong Xu, Xiaotong Zhao, Mingwei Chen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sex-specific risk factors associated with graves’ orbitopathy in Korean patients with newly diagnosed graves’ disease
Jooyoung Lee, Jinmo Kang, Hwa Young Ahn, Jeong Kyu Lee
Eye.2023; 37(16): 3382. CrossRef - Methimazole, an Effective Neutralizing Agent of the Sulfur Mustard Derivative 2-Chloroethyl Ethyl Sulfide
Albert Armoo, Tanner Diemer, Abigail Donkor, Jerrod Fedorchik, Severine Van slambrouck, Rachel Willand-Charnley, Brian A. Logue
ACS Bio & Med Chem Au.2023; 3(5): 448. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The influence of thionamides on intra-thyroidal uptake of 131I during radioiodine-131 treatment of Graves’ disease
Christian Happel, Benjamin Bockisch, Britta Leonhäuser, Amir Sabet, Frank Grünwald, Daniel Groener
Scientific Reports.2023;[Epub] CrossRef - Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
Endocrinology and Metabolism.2022; 37(2): 323. CrossRef - The chemiluminescent and enzymatic activity of blood neutrophils in patients with Graves' disease depending on hyperthyroidism compensation
M. A. Dudina, A. A. Savchenko, S. A. Dogadin, I. I. Gvozdev
Clinical and experimental thyroidology.2022; 18(1): 4. CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef
- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза

- Thyroid
- Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
- Won Sang Yoo, Hyun Kyung Chung
- Endocrinol Metab. 2021;36(3):500-513. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1066

- 9,143 View
- 548 Download
- 16 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Subclinical hypothyroidism (sHypo) is defined as normal serum free thyroid hormone levels coexisting with elevated serum thyroid-stimulating hormone (TSH) levels. sHypo is a common condition observed in clinical practice with several unique features. Its diagnosis should be based on an understanding of geographic and demographic differences in biochemical criteria versus a global reference range for TSH that is based on the 95% confidence interval of a healthy population. During the differential diagnosis, it is important to remember that a considerable proportion of sHypo cases are transient and reversible in nature; the focus is better placed on persistent or progressive forms, which mainly result from chronic autoimmune thyroiditis. Despite significant evidence documenting the health impacts of sHypo, the effects of levothyroxine treatment (LT4-Tx) in patients with sHypo remains controversial, especially in patients with grade 1 sHypo and older adults. Existing evidence suggests that it is reasonable to refrain from immediate LT4-Tx in most patients if they are closely monitored, except in women who are pregnant or in progressive cases. Future research is needed to further characterize the risks and benefits of LT4-Tx in different patient cohorts.
-
Citations
Citations to this article as recorded by- THYROID FUNCTION ABNORMALITIES IN PATIENTS WITH CHOLELITHIASIS: A HOSPITAL-BASED CROSS-SECTIONAL STUDY
AVANISH KUMAR SAXENA, ANAM FATIMA, KUNDRAPU VEERA VENKATA SIVA, ANUSHKA PARIYA, VAYALAPALLI SYAMA CHINMAYI
Asian Journal of Pharmaceutical and Clinical Research.2024; : 138. CrossRef - Subclinical hypothyroidism and clinical outcomes after cardiac surgery: A systematic review and meta-analysis
Michele Dell’Aquila, Camilla S. Rossi, Tulio Caldonazo, Gianmarco Cancelli, Lamia Harik, Giovanni J. Soletti, Kevin R. An, Jordan Leith, Hristo Kirov, Mudathir Ibrahim, Michelle Demetres, Arnaldo Dimagli, Mohamed Rahouma, Mario Gaudino
JTCVS Open.2024; 18: 64. CrossRef - The Relationship between Subclinical Hypothyroidism and Carotid Intima-Media Thickness as a Potential Marker of Cardiovascular Risk: A Systematic Review and a Meta-Analysis
Oana-Maria Isailă, Victor Eduard Stoian, Iuliu Fulga, Alin-Ionut Piraianu, Sorin Hostiuc
Journal of Cardiovascular Development and Disease.2024; 11(4): 98. CrossRef - Variability of Thyroid Hormones in Newborns from Mothers with Endemic Goiter
Turdieva Shokhida Tolkunovna, Ganieva Durdona Kamalovna
Journal of Nature and Science of Medicine.2024; 7(2): 129. CrossRef - Thyroid dysfunction in the ageing patient
O.V. Bilookyi, V.L. Vasiuk, O.A. Shupik
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2024; 20(2): 143. CrossRef - Subclinical hypothyroidism, outcomes and management guidelines: a narrative review and update of recent literature
Bogumila Urgatz, Salman Razvi
Current Medical Research and Opinion.2023; 39(3): 351. CrossRef - Indicator of thyroid hormones in newborns from mothers with diffuse-endemic goiter
G. T. Makhkamova, Sh. T. Turdieva
Meditsinskiy sovet = Medical Council.2023; (1): 212. CrossRef - Diagnóstico y tratamiento del hipotiroidismo subclínico en adultos mayores
Debbie Noelia Tebanta Albán, Gabriel Aníbal Hugo Merino, María Valentina Muñoz Arteaga, Ariana Lisseth Vázquez López
Ciencia Digital.2023; 7(1): 6. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Subclinical Hypothyroidism
Hyun Kyung Chung, Eu Jeong Ku, Won Sang Yoo, Yea Eun Kang, Kyeong Jin Kim, Bo Hyun Kim, Tae-Yong Kim, Young Joo Park, Chang Ho Ahn, Jee Hee Yoon, Eun Kyung Lee, Jong Min Lee, Eui Dal Jung, Jae Hoon Chung, Yun Jae Chung, Won Bae Kim, Ka Hee Yi, Ho-Cheol Ka
International Journal of Thyroidology.2023; 16(1): 32. CrossRef - Gut microbiota short-chain fatty acids and their impact on the host thyroid function and diseases
María José Mendoza-León, Ashutosh K. Mangalam, Alejandro Regaldiz, Enrique González-Madrid, Ma. Andreina Rangel-Ramírez, Oscar Álvarez-Mardonez, Omar P. Vallejos, Constanza Méndez, Susan M. Bueno, Felipe Melo-González, Yorley Duarte, Ma. Cecilia Opazo, Al
Frontiers in Endocrinology.2023;[Epub] CrossRef - Human amnion-derived mesenchymal stem cells improve subclinical hypothyroidism by immunocompetence mediating apoptosis inhibition on thyroid cells in aged mice
Chuyu Li, Qiang Rui, Xiaohan Dong, Song Ning, Jing Zhou, Huimin Wu, Chunyan Jiang, Yugui Cui, Jiayin Liu, Jun Jiang, Lianju Qin
Cell and Tissue Research.2023; 394(2): 309. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - The Role of Global Longitudinal Strain in Subclinical Hypothyroid Patients With Heart Failure
Nismat Javed, Vibha Hayagreev, Angel DeLaCruz, Muhammad Saad, Amandeep Singh, Timothy Vittorio
Cureus.2023;[Epub] CrossRef - Association between shift work and the risk of hypothyroidism in adult male workers in Korea: a cohort study
Seonghyeon Kwon, Yesung Lee, Eunhye Seo, Daehoon Kim, Jaehong Lee, Youshik Jeong, Jihoon Kim, Jinsook Jeong, Woncheol Lee
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef - Estimation of left ventricular functions in patients with subclinical hypothyroidism: a meta-analysis
Binyi Li, Yong Huang, Zheng Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Comparison of Five Different Criteria for Diagnosis of Subclinical Hypothyroidism in a Large-Scale Chinese Population
Yan-song Zheng, Sheng-yong Dong, Yan Gong, Jia-hong Wang, Fei Wang, Qiang Zeng
Frontiers in Endocrinology.2022;[Epub] CrossRef - Subclinical Hypothyroidism and Cognitive Impairment
Jung-Min Pyun, Young Ho Park, SangYun Kim
Journal of Alzheimer's Disease.2022; 88(2): 757. CrossRef - Effect of Levothyroxine Supplementation on the Cardiac Morphology and Function in Patients With Subclinical Hypothyroidism: A Systematic Review and Meta-analysis
Xichang Wang, Haoyu Wang, Qiuxian Li, Ping Wang, Yumin Xing, Fan Zhang, Jiashu Li, Zhongyan Shan
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): 2674. CrossRef - Natural history of subclinical hypothyroidism and prognostic factors for the development of overt hypothyroidism: Tehran Thyroid Study (TTS)
A. Amouzegar, M. Dehghani, H. Abdi, L. Mehran, S. Masoumi, F. Azizi
Journal of Endocrinological Investigation.2022; 45(12): 2353. CrossRef - Retrospective cohort analysis comparing changes in blood glucose level and body composition according to changes in thyroid‐stimulating hormone level
Hyunah Kim, Da Young Jung, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyeon Woo Yim, Hun‐Sung Kim
Journal of Diabetes.2022; 14(9): 620. CrossRef - Long working hours and the risk of hypothyroidism in healthy Korean workers: a cohort study
Yesung Lee, Woncheol Lee, Hyoung-Ryoul Kim
Epidemiology and Health.2022; 44: e2022104. CrossRef
- THYROID FUNCTION ABNORMALITIES IN PATIENTS WITH CHOLELITHIASIS: A HOSPITAL-BASED CROSS-SECTIONAL STUDY

- Thyroid
- Current Guidelines for Management of Medullary Thyroid Carcinoma
- Mijin Kim, Bo Hyun Kim
- Endocrinol Metab. 2021;36(3):514-524. Published online June 22, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1082
- 17,980 View
- 1,710 Download
- 29 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
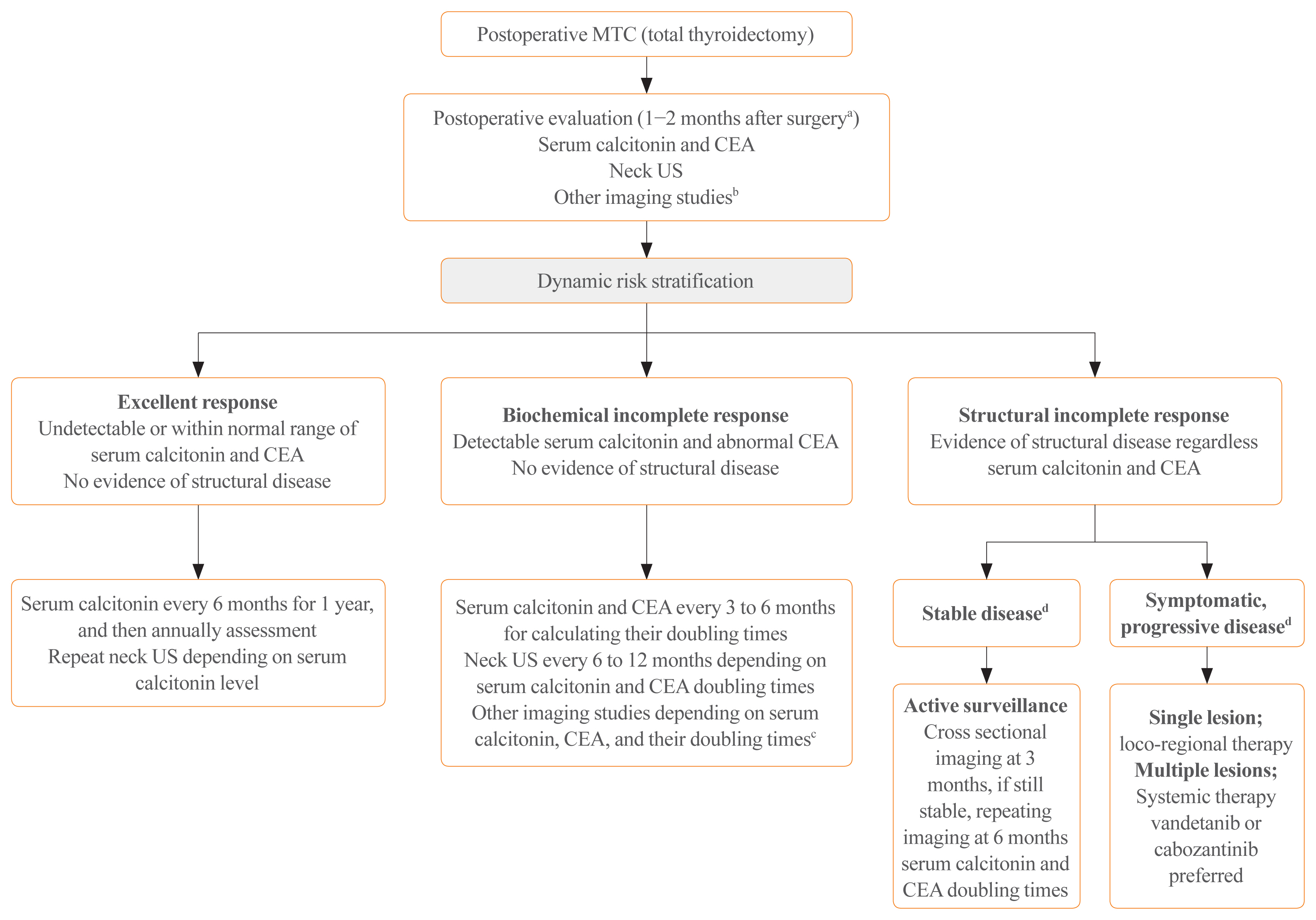
ePub - Medullary thyroid carcinoma (MTC) is a rare neuroendocrine tumor originating from the parafollicular cells. The diagnostic and therapeutic strategies for the condition are different from those used for well-differentiated thyroid cancer. Since the 2015 American Thyroid Association guidelines for the diagnosis and treatment of MTC, the latest, including the National Comprehensive Cancer Network and European Association for Medical Oncology guidelines have been updated to reflect several recent advances in the management of MTC. Advances in molecular diagnosis and postoperative risk stratification systems have led to individualized treatment and follow-up strategies. Multi-kinase inhibitors, such as vandetanib and cabozantinib, can prolong disease progression-free survival with favorable adverse effects. In addition, potent selective rearranged during transfection (RET) inhibitors (selpercatinib and pralsetinib) have shown a promising efficacy in recent clinical trials. This review summarizes the management of MTC in recent guidelines focused on sporadic MTC.
-
Citations
Citations to this article as recorded by- Molecular imaging and related therapeutic options for medullary thyroid carcinoma: state of the art and future opportunities
Alessio Imperiale, Valentina Berti, Mickaël Burgy, Roberto Luigi Cazzato, Arnoldo Piccardo, Giorgio Treglia
Reviews in Endocrine and Metabolic Disorders.2024; 25(1): 187. CrossRef - Diffuse C-Cells Hyperplasia Is the Source of False Positive Calcitonin Measurement in FNA Washout Fluids of Thyroid Nodules: A Rational Clinical Approach to Avoiding Unnecessary Surgery
Chiara Mura, Rossella Rodia, Silvia Corrias, Antonello Cappai, Maria Letizia Lai, Gian Luigi Canu, Fabio Medas, Pietro Giorgio Calò, Stefano Mariotti, Francesco Boi
Cancers.2024; 16(1): 210. CrossRef - Meta-Analysis of the Efficacy and Safety Evaluation of Vandetanib in
the Treatment of Medullary Thyroid Cancer
Tong-cheng Xian, Min-ye Yang, Xue-lin Zhang, Jie Wang, Yi Luo
Hormone and Metabolic Research.2024;[Epub] CrossRef - Successful localisation of recurrent thyroid cancer using preoperative patent blue dye injection
B. O. Evranos, N. Ince, H. Ataş, S. B. Polat, H. Ahsen, N. N. Imga, A. Dirikoc, O. Topaloglu, T. Tutuncu, R. Ersoy, B. Cakir
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Current and future of immunotherapy for thyroid cancer based on bibliometrics and clinical trials
Ke Wang, Ying Zhang, Yang Xing, Hong Wang, Minghua He, Rui Guo
Discover Oncology.2024;[Epub] CrossRef - Combining radiomics with thyroid imaging reporting and data system to predict lateral cervical lymph node metastases in medullary thyroid cancer
Zhiqiang Liu, Xiwei Zhang, Xiaohui Zhao, Qianqian Guo, Zhengjiang Li, Minghui Wei, Lijuan Niu, Changming An
BMC Medical Imaging.2024;[Epub] CrossRef - Potentials and future perspectives of multi-target drugs in cancer treatment: the next generation anti-cancer agents
Ali Doostmohammadi, Hossein Jooya, Kimia Ghorbanian, Sargol Gohari, Mehdi Dadashpour
Cell Communication and Signaling.2024;[Epub] CrossRef - Diagnostic capabilities of PET/CT with 18F-DOPA in biochemical recurrence of medullary thyroid carcinoma: a retrospective study
N. V. Tsentr, A. A. Zyryanova, M. A. Rusnak, D. V. Ryzhkova
Diagnostic radiology and radiotherapy.2024; 15(1): 87. CrossRef - LINC00887 Acts as an Enhancer RNA to Promote Medullary Thyroid
Carcinoma Progression by Binding with FOXQ1
Daxiang Liu, Wenjing Wang, Yanzhao Wu, Yongle Qiu, Lan Zhang
Current Cancer Drug Targets.2024; 24(5): 519. CrossRef - Update on Management of Medullary Thyroid Carcinoma: Focus on Nuclear Medicine
Giorgio Treglia, Vittoria Rufini, Arnoldo Piccardo, Alessio Imperiale
Seminars in Nuclear Medicine.2023; 53(4): 481. CrossRef - Cabozantinib, Vandetanib, Pralsetinib and Selpercatinib as Treatment for Progressed Medullary Thyroid Cancer with a Main Focus on Hypertension as Adverse Effect
Linnea Højer Wang, Markus Wehland, Petra M. Wise, Manfred Infanger, Daniela Grimm, Michael C. Kreissl
International Journal of Molecular Sciences.2023; 24(3): 2312. CrossRef - A proposed grading scheme for predicting recurrence in medullary thyroid cancer based on the Ki67 index and metastatic lymph node ratio
Pengfei Xu, Di Wu, Xuekui Liu
Endocrine.2023; 81(1): 107. CrossRef - Efficacy and Safety of [177Lu]Lu-DOTA-TATE in Adults with Inoperable or Metastatic Somatostatin Receptor-Positive Pheochromocytomas/Paragangliomas, Bronchial and Unknown Origin Neuroendocrine Tumors, and Medullary Thyroid Carcinoma: A Systematic Literatur
Marianna Hertelendi, Oulaya Belguenani, Azzeddine Cherfi, Ilya Folitar, Gabor Kollar, Berna Degirmenci Polack
Biomedicines.2023; 11(4): 1024. CrossRef - PET/CT with various radiopharmaceuticals in the complex diagnosis of medullary thyroid carcinoma: a review
N. V. Tsentr, A. E. Ertman, D. V. Ryzhkova
Diagnostic radiology and radiotherapy.2023; 14(2): 31. CrossRef - Physical activity and reduced risk of fracture in thyroid cancer patients after thyroidectomy — a nationwide cohort study
Jinyoung Kim, Kyungdo Han, Jin-Hyung Jung, Jeonghoon Ha, Chaiho Jeong, Jun-Young Heu, Se-Won Lee, Jeongmin Lee, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Ki-Hyun Baek
Frontiers in Endocrinology.2023;[Epub] CrossRef - Different RONS Generation in MTC-SK and NSCL Cells Lead to Varying Antitumoral Effects of Alpha-Ketoglutarate + 5-HMF
Joachim Greilberger, Katharina Erlbacher, Philipp Stiegler, Reinhold Wintersteiger, Ralf Herwig
Current Issues in Molecular Biology.2023; 45(8): 6503. CrossRef - Medullary thyroid carcinoma
Maria Rosa Pelizzo, Esmeralda Isabella Mazza, Caterina Mian, Isabella Merante Boschin
Expert Review of Anticancer Therapy.2023; 23(9): 943. CrossRef - Mixed medullary‑follicular thyroid carcinoma: A case report and literature review
Yonghui Wang, Dandan Yin, Guifang Ren, Zhengjiang Wang, Fanhua Kong
Oncology Letters.2023;[Epub] CrossRef - Circulating cell-free DNA (cfDNA) in patients with medullary thyroid carcinoma is characterized by specific fragmentation and methylation changes with diagnostic value
Anna Citarella, Zein Mersini Besharat, Sofia Trocchianesi, Tanja Milena Autilio, Antonella Verrienti, Giuseppina Catanzaro, Elena Splendiani, Zaira Spinello, Silvia Cantara, Patrizia Zavattari, Eleonora Loi, Cristina Romei, Raffaele Ciampi, Luciano Pezzul
Biomarker Research.2023;[Epub] CrossRef - Advances in Diagnostics and Therapy of Medullary Thyroid Carcinoma (MTC)– A Mini-Review
Michał Miciak, Krzysztof Jurkiewicz
Clinical Cancer Investigation Journal.2023; 12(5): 1. CrossRef - The Evolving Treatment Landscape of Medullary Thyroid Cancer
Marta Laganà, Valentina Cremaschi, Andrea Alberti, Danica M. Vodopivec Kuri, Deborah Cosentini, Alfredo Berruti
Current Treatment Options in Oncology.2023; 24(12): 1815. CrossRef - Pralsetinib: chemical and therapeutic development with FDA authorization for the management of RET fusion-positive non-small-cell lung cancers
Faraat Ali, Kumari Neha, Garima Chauhan
Archives of Pharmacal Research.2022; 45(5): 309. CrossRef - Psychosocial Characteristics and Experiences in Patients with Multiple Endocrine Neoplasia Type 2 (MEN2) and Medullary Thyroid Carcinoma (MTC)
Robin Lockridge, Sima Bedoya, Taryn Allen, Brigitte Widemann, Srivandana Akshintala, John Glod, Lori Wiener
Children.2022; 9(6): 774. CrossRef - Aggressive clinical course of medullary thyroid microcarcinoma
Tamara Janić, Mirjana Stojković, Sanja Klet, Bojan Marković, Beleslin Nedeljković, Jasmina Ćirić, Miloš Žarković
Medicinski glasnik Specijalne bolnice za bolesti štitaste žlezde i bolesti metabolizma.2022; 27(85): 63. CrossRef - Comparative evaluation of somatostatin and CXCR4 receptor expression in different types of thyroid carcinoma using well-characterised monoclonal antibodies
Max Czajkowski, Daniel Kaemmerer, Jörg Sänger, Guido Sauter, Ralph M. Wirtz, Stefan Schulz, Amelie Lupp
BMC Cancer.2022;[Epub] CrossRef - Metastatic Risk Stratification of 2526 Medullary Thyroid Carcinoma Patients: A Study Based on Surveillance, Epidemiology, and End Results Database
Minh-Khang Le, Masataka Kawai, Toru Odate, Huy Gia Vuong, Naoki Oishi, Tetsuo Kondo
Endocrine Pathology.2022; 33(3): 348. CrossRef - Update on the Diagnosis and Management of Medullary Thyroid Cancer: What Has Changed in Recent Years?
Krzysztof Kaliszewski, Maksymilian Ludwig, Bartłomiej Ludwig, Agnieszka Mikuła, Maria Greniuk, Jerzy Rudnicki
Cancers.2022; 14(15): 3643. CrossRef - Immunotherapy of Neuroendocrine Neoplasms: Any Role for the Chimeric Antigen Receptor T Cells?
Giuseppe Fanciulli, Roberta Modica, Anna La Salvia, Federica Campolo, Tullio Florio, Nevena Mikovic, Alice Plebani, Valentina Di Vito, Annamaria Colao, Antongiulio Faggiano
Cancers.2022; 14(16): 3991. CrossRef - Preclinical Evaluation of Novel Tyrosine-Kinase Inhibitors in Medullary Thyroid Cancer
Davide Saronni, Germano Gaudenzi, Alessandra Dicitore, Silvia Carra, Maria Celeste Cantone, Maria Orietta Borghi, Andrea Barbieri, Luca Mignani, Leo J. Hofland, Luca Persani, Giovanni Vitale
Cancers.2022; 14(18): 4442. CrossRef - Rapid and long-lasting response to selpercatinib of paraneoplastic Cushing’s syndrome in medullary thyroid carcinoma
Marine Sitbon, Porhuoy Chou, Seydou Bengaly, Brigitte Poirot, Marie Laloi-Michelin, Laure Deville, Atanas Pachev, Ahouefa Kowo-Bille, Clement Dumont, Cécile N Chougnet
European Thyroid Journal.2022;[Epub] CrossRef - Ginsenoside Rg3 Alleviates Antithyroid Cancer Drug Vandetanib-Induced QT Interval Prolongation
Juan Zhang, Dan Luo, Fang Li, Zhiyi Li, Xiaoli Gao, Jie Qiao, Lin Wu, Miaoling Li, Shao Liang
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - THE ROLE OF CALCITONIN IN THE PREOPERATIVE STAGE AS THE PREDICTOR OF MEDULLARY THYROID CANCER METASTASES
Volodymyr Palamarchuk , Viktor Smolyar , Oleksandr Tovkay, Oleksandr Nechay, Volodymyr Kuts , Revaz Sichinava , Oleh Mazur
Ukrainian Scientific Medical Youth Journal.2021; 127(4): 68. CrossRef - THE ROLE OF CALCITONIN IN THE PREOPERATIVE STAGE AS THE PREDICTOR OF MEDULLARY THYROID CANCER METASTASES
Volodymyr Palamarchuk , Viktor Smolyar , Oleksandr Tovkay , Oleksandr Nechay , Volodymyr Kuts , Revaz Sichinava , Oleh Mazur
The Ukrainian Scientific Medical Youth Journal.2021; 4(127): 68. CrossRef
- Molecular imaging and related therapeutic options for medullary thyroid carcinoma: state of the art and future opportunities

- Bone Metabolism
- Normocalcemic Primary Hyperparathyroidism: Need for a Standardized Clinical Approach
- Guido Zavatta, Bart L. Clarke
- Endocrinol Metab. 2021;36(3):525-535. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1061
- 6,264 View
- 377 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
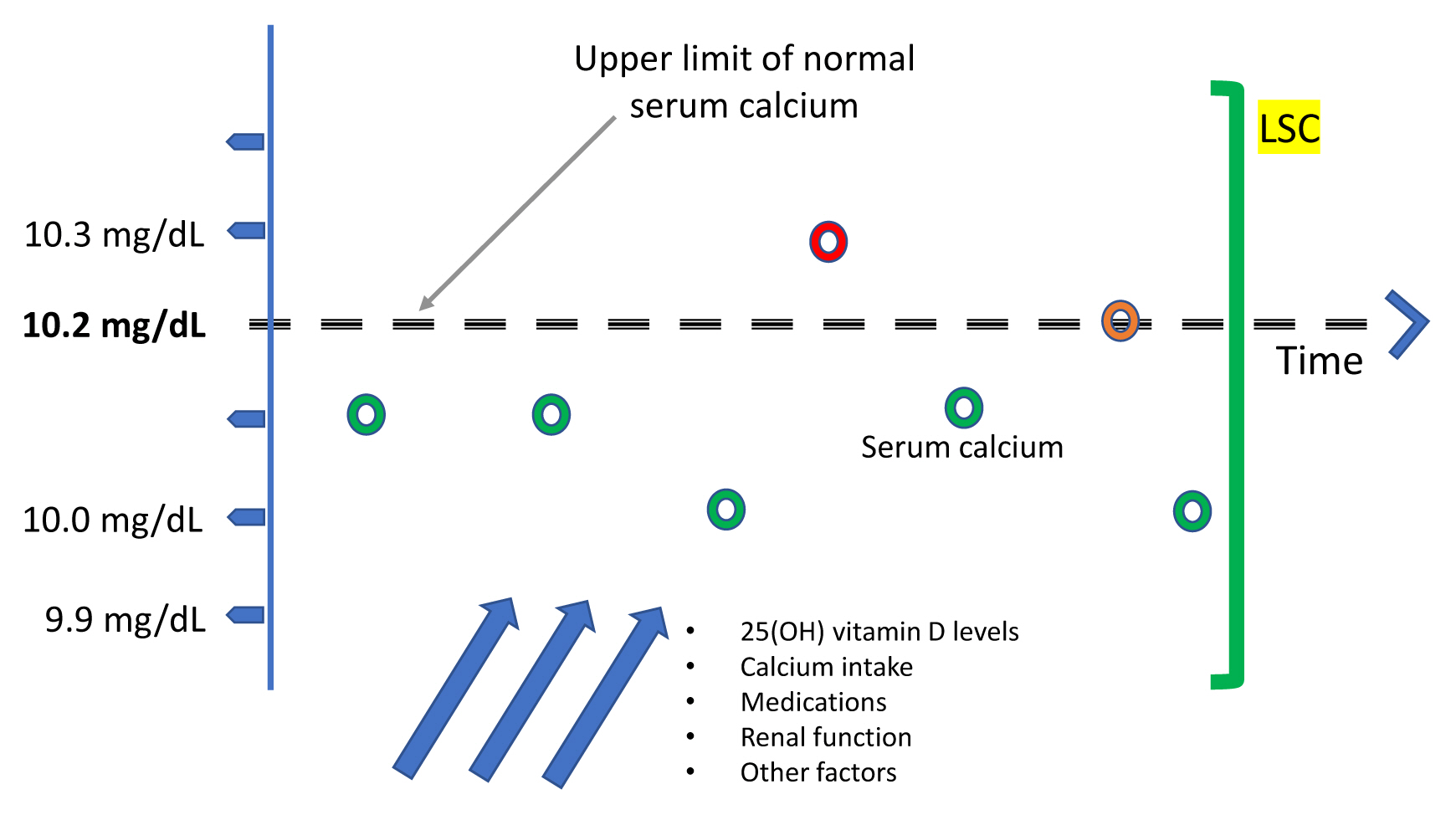
ePub - Since normocalcemic primary hyperparathyroidism (NHPT) was first defined at the Third International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism in 2008, many papers have been published describing its prevalence and possible complications. Guidelines for the management of this condition are still lacking, and making the diagnosis requires fulfillment of strict criteria. Recent studies have shown that intermittent oscillations of serum calcium just below and slightly above the normal limits are very frequent, therefore challenging the assumption that serum calcium must be consistently normal to make the diagnosis. There is debate if these variations in serum calcium outside the normal range should be included under the rubric of NHPT or, rather, a milder form of classical primary hyperparathyroidism. Innovative approaches to define NHPT have been proposed that still need to be validated in prospective studies. Non-classical complications, especially cardiovascular complications, have been associated with NHPT, indicating that hyperparathyroidism may be a cardiovascular risk factor. New associations between parathyroid hormone (PTH) and several other comorbidities have also been reported from observational studies, suggesting that excessive PTH secretion might cause tissue dysfunction independent of serum calcium. Heterogeneous studies using different definitions of NHPT, however, make it difficult to draw definitive conclusions regarding the role of PTH excess when complications other than osteoporosis or kidney stones are described. This review will focus on clinical aspects and suggest an approach to NHPT.
-
Citations
Citations to this article as recorded by- Surgery for Normocalcemic Hyperparathyroidism
Pallavi Kulkarni, David Goldenberg
Otolaryngologic Clinics of North America.2024; 57(1): 111. CrossRef - Linea guida sulla gestione terapeutica dell’iperparatiroidismo primario sporadico nell’adulto
Fabio Vescini, Marco Boniardi, Marina Carotti, Elena Castellano, Cristiana Cipriani, Cristina Eller-Vainicher, Sandro Giannini, Maurizio Iacobone, Francesca Pace, Antonio Stefano Salcuni, Federica Saponaro, Stefano Spiezia, Annibale Versari, Guido Zavatta
L'Endocrinologo.2024; 25(2): 222. CrossRef - DXA-based bone strain index in normocalcemic primary hyperparathyroidism
Gaia Tabacco, Anda Mihaela Naciu, Carmelo Messina, Gianfranco Sanson, Luca Rinaudo, Roberto Cesareo, Stefania Falcone, Nicola Napoli, Fabio Massimo Ulivieri, Andrea Palermo
Osteoporosis International.2023; 34(5): 999. CrossRef - Iperparatiroidismo primario normocalcemico
Silvia Egiddi, Luigi Bonifazi Meffe, Anda Mihaela Naciu, Gaia Tabacco, Nicola Napoli, Andrea Palermo
L'Endocrinologo.2023; 24(3): 249. CrossRef - The Russian registry of primary hyperparathyroidism, latest update
Natalia G. Mokrysheva, Anna K. Eremkina, Alina R. Elfimova, Elena V. Kovaleva, Anastasiia P. Miliutina, Ekaterina E. Bibik, Anna M. Gorbacheva, Ekaterina A. Dobreva, Irina S. Maganeva, Julia A. Krupinova, Rustam H. Salimkhanov, Lizaveta A. Aboishava, Elen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Incidental Normocalcemic Primary Hyperparathyroidism Presenting With Symptomatic Hypophosphatemia: A Case Report
Omar Tabbikha, Joanne Chamy, Michael El Khoury
Cureus.2023;[Epub] CrossRef - Long-term effects of hypercalcemia in kidney transplant recipients with persistent hyperparathyroidism
Juan Carlos Ramirez-Sandoval, Lluvia Marino, Gabriel Cojuc-Konigsberg, Estefania Reul-Linares, Nathalie Desire Pichardo-Cabrera, Cristino Cruz, Elisa Naomi Hernández-Paredes, Nathan Berman-Parks, Vanessa Vidal-Ruíz, Jonathan Mauricio Estrada-Linares, Alfr
Journal of Nephrology.2023;[Epub] CrossRef - Evaluating Patients for Secondary Causes of Osteoporosis
E. Michael Lewiecki
Current Osteoporosis Reports.2022; 20(1): 1. CrossRef - Preoperative Thoracic Muscle Mass Predicts Bone Density Change After Parathyroidectomy in Primary Hyperparathyroidism
Seung Won Burm, Namki Hong, Seunghyun Lee, Gi Jeong Kim, Sang Hyun Hwang, Jongju Jeong, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2474. CrossRef - Applications of Metabolomics in Calcium Metabolism Disorders in Humans
Beata Podgórska, Marta Wielogórska-Partyka, Joanna Godzień, Julia Siemińska, Michał Ciborowski, Małgorzata Szelachowska, Adam Krętowski, Katarzyna Siewko
International Journal of Molecular Sciences.2022; 23(18): 10407. CrossRef - Serum Calcium/Phosphorus Ratio in Biochemical Screening of Primary Hyperparathyroidism
Nagihan Bestepe, Fatma Neslihan Cuhaci, Burcak Polat, Berna Evranos Ogmen, Didem Ozdemir, Reyhan Ersoy, Bekir Cakir
Revista da Associação Médica Brasileira.2022; 68(12): 1668. CrossRef
- Surgery for Normocalcemic Hyperparathyroidism

- Bone Metabolism
- Update on Glucocorticoid Induced Osteoporosis
- Soo-Kyung Cho, Yoon-Kyoung Sung
- Endocrinol Metab. 2021;36(3):536-543. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1021

- 5,199 View
- 350 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
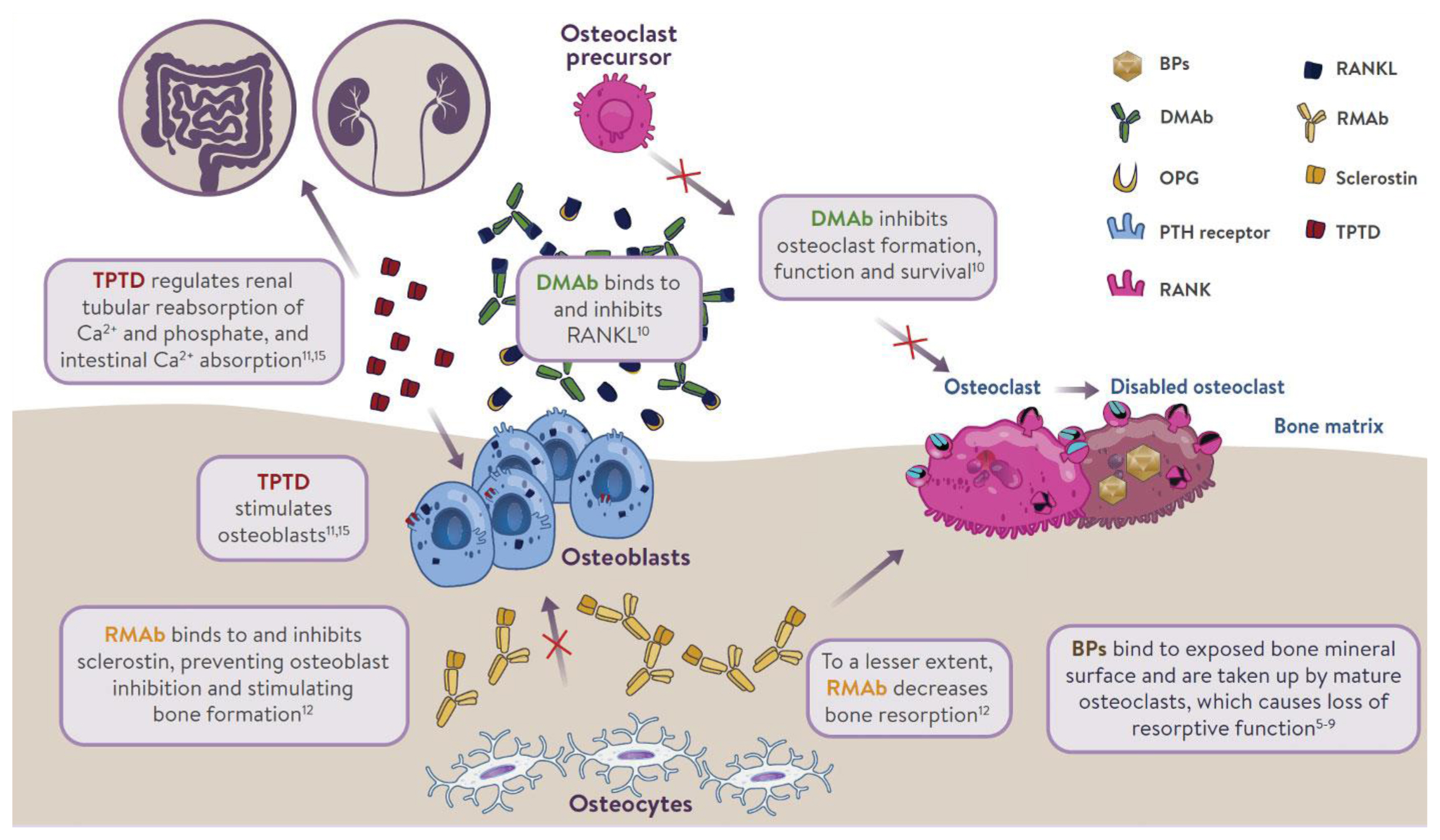
ePub - Glucocorticoids are used to treat many autoimmune and inflammatory diseases. However, an adverse systemic effect is a deleterious effect on bone, which may lead to glucocorticoid-induced osteoporosis, characterized by a rapid and transient increase in bone resorption and fracture risk, which may increase rapidly within 3 months of commencing oral glucocorticoids. Therefore, early risk assessment and intervention are crucial for preventing fractures in patients receiving glucocorticoids. Recent practice guidelines recommend an assessment for fracture risk in patients beginning or receiving glucocorticoids for more than 3 months, and they have suggested fracture risk assessment tool values for identifying patients who need preventive treatment. Bisphosphonates are currently the recommended first-line therapy for the prevention and treatment of glucocorticoid-induced osteoporosis. These have been shown to increase the bone mineral density in the spine and hip and to decrease the incidence of vertebral fractures. Recently, a more potent antiresorptive agent, denosumab, has been shown to increase the bone density in patients receiving glucocorticoids. Teriparatide has been shown to have a preventive effect on vertebral fractures, but not on nonvertebral fractures. In this article we aimed to provide an update on glucocorticoid-induced osteoporosis by focusing on the assessment of its risk and treatment options.
-
Citations
Citations to this article as recorded by- Protective role of 3-oxypyridine derivatives in rats’ steroid-induced osteoporosis associated with reduced oxidative stress and recovery of nitric oxide formation
A. P. Danilenko, K. S. Trunov, M. V. Pokrovsky, L. M. Danilenko, M. V. Korokin, O. S. Gudyrev, A. A. Khentov, N. P. Masalytina, I. A. Tatarenkova, A. V. Cherednichenko, E. V. Boeva, I. S. Koklin, E. I. Taran
Pharmacy & Pharmacology.2023; 11(1): 48. CrossRef - Guía de práctica clínica para la prevención, el diagnóstico y el tratamiento de la osteoporosis inducida por glucocorticoides. Asociación Colombiana de Reumatología, 2023
Monique Chalem, Noemi Casas, Aura María Domínguez, Daniel Gerardo Fernández, Andrés González, Edwin Jáuregui, José Fernando Molina, Diana Nathalie Rincón, Carlos Enrique Toro-Gutiérrez, Francisco Juan Vargas Grajales, Susan Martínez, Linda Ibatá
Revista Colombiana de Reumatología.2023;[Epub] CrossRef - Influence of Piper sarmentosum Aqueous Extract on the Expression of Osteocalcin in Glucocorticoid-induced Osteoporotic Rats
Elvy Suhana Mohd Ramli, Ima Nirwana Soelaiman, Suryati Mohd Thani, Nurul Huda Mohd Nor, Nurul Hayati Mohamad Zainal, Siti Saleha Masrudin, Siti Fadziyah Mohamad Asri
Malaysian Journal of Medicine and Health Sciences.2023; 19(s12): 115. CrossRef - Vitamin D Supplementation in Patients with Juvenile Idiopathic Arthritis
Chao-Yi Wu, Huang-Yu Yang, Shue-Fen Luo, Jing-Long Huang, Jenn-Haung Lai
Nutrients.2022; 14(8): 1538. CrossRef - A Review on the Molecular Mechanisms of Action of Natural Products in Preventing Bone Diseases
Innocent U. Okagu, Timothy P. C. Ezeorba, Rita N. Aguchem, Ikenna C. Ohanenye, Emmanuel C. Aham, Sunday N. Okafor, Carlotta Bollati, Carmen Lammi
International Journal of Molecular Sciences.2022; 23(15): 8468. CrossRef - Antiosteoporosis and bone protective effect of nimbolide in steroid‐induced osteoporosis rats
Jiang Huo, Yu Ding, Xinyuan Wei, Qi Chen, Bin Zhao
Journal of Biochemical and Molecular Toxicology.2022;[Epub] CrossRef - Comparison of denosumab and oral bisphosphonates for the treatment of glucocorticoid-induced osteoporosis: a systematic review and meta-analysis
Lianghai Jiang, Jian Dong, Jianwei Wei, Lantao Liu
BMC Musculoskeletal Disorders.2022;[Epub] CrossRef - Improvement in Glucocorticoid-Induced Osteoporosis on Switching from Bisphosphonates to Once-Weekly Teriparatide: A Randomized Open-Label Trial
Toshihiro Nanki, Mai Kawazoe, Kiyoko Uno, Wataru Hirose, Hiroaki Dobashi, Hiroshi Kataoka, Toshihide Mimura, Hiroshi Hagino, Hajime Kono
Journal of Clinical Medicine.2022; 12(1): 292. CrossRef - Understanding of Glucocorticoid Induced Osteoporosis
Chang-Nam Son
Keimyung Medical Journal.2021; 40(2): 69. CrossRef
- Protective role of 3-oxypyridine derivatives in rats’ steroid-induced osteoporosis associated with reduced oxidative stress and recovery of nitric oxide formation

- Bone Metabolism
- Long-Term Treatment of Postmenopausal Osteoporosis
- Jacques P. Brown
- Endocrinol Metab. 2021;36(3):544-552. Published online June 22, 2021
- DOI: https://doi.org/10.3803/EnM.2021.301
- 14,892 View
- 934 Download
- 37 Web of Science
- 37 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Osteoporosis is an incurable chronic condition, like heart disease, diabetes, or hypertension. A large gap currently exists in the primary prevention of fractures, and studies show that an estimated 80% to 90% of adults do not receive appropriate osteoporosis management even in the secondary prevention setting. Case finding strategies have been developed and effective pharmacological interventions are available. This publication addresses how best to use the pharmacological options available for postmenopausal osteoporosis to provide lifelong fracture protection in patients at high and very high risk of fracture. The benefit of osteoporosis therapies far outweighs the rare risks.
-
Citations
Citations to this article as recorded by- Effects of stepwise administration of osteoprotegerin and parathyroid hormone-related peptide DNA vectors on bone formation in ovariectomized rat model
Ye Ji Eom, Jang-Woon Kim, Yeri Alice Rim, Jooyoung Lim, Se In Jung, Ji Hyeon Ju
Scientific Reports.2024;[Epub] CrossRef - Glycolithocholic acid increases the frequency of circulating Tregs through constitutive androstane receptor to alleviate postmenopausal osteoporosis
Xiaoyu Cai, Zhi Li, Yao Yao, Yongquan Zheng, Meng Zhang, Yiqing Ye
Biochemical Pharmacology.2024; 219: 115951. CrossRef - Cucumber seed polypeptides regulate RANKL-induced osteoclastogenesis through OPG/RANKL/RANK and NF-κB
Tao Yu, Xiao Liu, Meng Jiang, Yuanyue Li, Heng Su, Ben Niu
In Vitro Cellular & Developmental Biology - Animal.2024; 60(1): 54. CrossRef - Eupatilin ameliorates postmenopausal osteoporosis via elevating microRNA‐211‐5p and repressing JAK2/STAT3 pathway
Liu Hong, Chao Yang
Environmental Toxicology.2024; 39(4): 2218. CrossRef - Strontium-Doped Mesoporous Bioactive Glass-Loading Bisphosphonates Inhibit Osteoclast Differentiation and Prevent Osteoporosis in Ovariectomized Mice
Zhi Zhou, Shicheng Huo, Zhanchun Li
Coatings.2024; 14(1): 97. CrossRef - A novel PDIA3/FTO/USP20 positive feedback regulatory loop induces osteogenic differentiation of preosteoblast in osteoporosis
Fei Zhang, Chen Liu, Zhiyong Chen, Chengyi Zhao
Cell Biology International.2024; 48(4): 541. CrossRef - Research Progress of Zoledronic Acid in the Treatment of Osteoarthritis
保成 刘
Advances in Clinical Medicine.2024; 14(02): 2821. CrossRef - A novel mechanism of Vildagliptin in regulating bone metabolism and mitigating osteoporosis
Jinwen He, Dacheng Zhao, Bo Peng, Xingwen Wang, Shenghong Wang, Xiaobing Zhao, Peng Xu, Bin Geng, Yayi Xia
International Immunopharmacology.2024; 130: 111671. CrossRef - Positive benefit-risk ratio of Psoraleae Fructus: Comprehensive safety assessment and osteogenic effects in rats
Zhuo Shi, Jin-chao Pan, Yi Ru, Ning-ning Shen, Yu-fu Liu, Cheng Zhang, Xiang-jun Wu, Fang-yang Li, Jia-lu Cui, Chun-qi Yang, Jun-ling Yang, Mao-xing Li, Cheng-rong Xiao, Zeng-chun Ma, Chuan Li, Yu-guang Wang, Yue Gao
Journal of Ethnopharmacology.2024; 326: 117967. CrossRef - Function-oriented mechanism discovery of coumarins from Psoralea corylifolia L. in the treatment of ovariectomy-induced osteoporosis based on multi-omics analysis
Qianyi Wei, Yongrong Zhou, Zhengtao Hu, Ye Shi, Qing Ning, Keyun Ren, Xinyu Guo, Ronglin Zhong, Zhi Xia, Yinghao Yin, Yongxin Hu, Yingjie Wei, Ziqi Shi
Journal of Ethnopharmacology.2024; 329: 118130. CrossRef - Efficacy and Possible Mechanisms of Astragali Radix and its Ingredients
in Animal Models of Osteoporosis: A Preclinical Review and Metaanalysis
Ning Cao, Zhangxuan Shou, Yi Xiao, Puqing Liu
Current Drug Targets.2024; 25(2): 135. CrossRef - Enhanced oral bioavailability of levormeloxifene and raloxifene by nanoemulsion: simultaneous bioanalysis using liquid chromatography-tandem mass spectrometry
Divya Chauhan, Debalina Maity, Pavan K Yadav, Sachin Vishwakarma, Arun Agarwal, Manish K Chourasia, Jiaur R Gayen
Nanomedicine.2024;[Epub] CrossRef - Changes in Testing and Treatment Methods in Osteoporosis Care
Takashi Nagai, Koji Ishikawa, Koki Tsuchiya, Soji Tani, Yusuke Dodo, Yusuke Oshita, Keizo Sakamoto, Nobuyuki Kawate, Yoshifumi Kudo, Deepak Kumar Khajuria
Journal of Osteoporosis.2024; 2024: 1. CrossRef - CircRNA hsa_circ_0006859 inhibits the osteogenic differentiation of BMSCs and aggravates osteoporosis by targeting miR-642b-5p/miR-483-3p and upregulating EFNA2/DOCK3
Peng Yin, Yuan Xue
International Immunopharmacology.2023; 116: 109844. CrossRef - Resveratrol induces proliferation and differentiation of mouse pre-osteoblast MC3T3-E1 by promoting autophagy
Weiye Cai, Bin Sun, Chao Song, Fei Liu, Zhengliang Wu, Zongchao Liu
BMC Complementary Medicine and Therapies.2023;[Epub] CrossRef - Oridonin Attenuates Thioacetamide-Induced Osteoclastogenesis Through MAPK/NF-κB Pathway and Thioacetamide-Inhibited Osteoblastogenesis Through BMP-2/RUNX2 Pathway
XiaoLi Jin, Jia Xu, Fanfan Yang, Jin Chen, Feng Luo, Bin Xu, Jian Xu
Calcified Tissue International.2023; 112(6): 704. CrossRef - Phytochemical Compounds Involved in the Bone Regeneration Process and Their Innovative Administration: A Systematic Review
Alina Hanga-Farcaș, Florina Miere (Groza), Gabriela Adriana Filip, Simona Clichici, Luminita Fritea, Laura Grațiela Vicaș, Eleonora Marian, Annamaria Pallag, Tunde Jurca, Sanda Monica Filip, Mariana Eugenia Muresan
Plants.2023; 12(10): 2055. CrossRef - Screening of superior anti‐osteoporotic flavonoids from Epimedii Folium with dual effects of reversing iron overload and promoting osteogenesis
Jun Jiang, Jinjin He, Shichang Xiao, Jiayi Shenyuan, Tong Chen, Dan Pei
Biomedical Chromatography.2023;[Epub] CrossRef - Study on the Effect of Bushen Zhuanggu Tablet Combined with Conventional Regimen on Bone Mineral Density Improvement, Functional Recovery and Fracture Risk Prevention in Patients with Postmenopausal Osteoporosis
Tianliang Chen, Guilan Li, Yongtao Xu, Min Tang
Computational and Mathematical Methods in Medicine.2023; 2023: 1. CrossRef - Circ_0001825 promotes osteogenic differentiation in human-derived mesenchymal stem cells via miR-1270/SMAD5 axis
Changjun Zheng, Lingzhi Ding, Ziming Xiang, Mingxuan Feng, Fujiang Zhao, Zhaoxin Zhou, Chang She
Journal of Orthopaedic Surgery and Research.2023;[Epub] CrossRef - Identification of ROCK1 as a novel biomarker for postmenopausal osteoporosis and pan-cancer analysis
Bowen Lai, Heng Jiang, Yuan Gao, Xuhui Zhou
Aging.2023; 15(17): 8873. CrossRef - The Mechanotransduction Signaling Pathways in the Regulation of Osteogenesis
Zhaoshuo Liu, Qilin Wang, Junyou Zhang, Sihan Qi, Yingying Duan, Chunyan Li
International Journal of Molecular Sciences.2023; 24(18): 14326. CrossRef - Decoding the mechanism of Eleutheroside E in treating osteoporosis via network pharmacological analysis and molecular docking of osteoclast-related genes and gut microbiota
Tianyu Zhou, Yilin Zhou, Dongdong Ge, Youhong Xie, Jiangyan Wang, Lin Tang, Qunwei Dong, Ping Sun
Frontiers in Endocrinology.2023;[Epub] CrossRef - Epigallocatechin gallate alleviates osteoporosis by regulating the gut microbiota and serum metabolites in rats
Xuebing Han, Yifeng Fu, Keyu Wang, Siying Li, Chang Jiang, Shuangshuang Wang, Zheng Wang, Gang Liu, Siwang Hu
Food & Function.2023; 14(23): 10564. CrossRef - The Molecular Role of Polyamines in Age-Related Diseases: An Update
Guadalupe Elizabeth Jimenez Gutierrez, Fabiola V. Borbolla Jiménez, Luis G. Muñoz, Yessica Sarai Tapia Guerrero, Nadia Mireya Murillo Melo, José Melesio Cristóbal-Luna, Norberto Leyva Garcia, Joaquín Cordero-Martínez, Jonathan J. Magaña
International Journal of Molecular Sciences.2023; 24(22): 16469. CrossRef - Pueraria lobata-derived exosome-like nanovesicles alleviate osteoporosis by enhacning autophagy
Weiqiang Zhan, Mingzhu Deng, Xinqia Huang, Dong Xie, Xiang Gao, Jiaxian Chen, Zhen Shi, Jiaxu Lu, Hao Lin, Peng Li
Journal of Controlled Release.2023; 364: 644. CrossRef - Based on network pharmacology and molecular docking to explore the molecular mechanism of Ginseng and Astragalus decoction against postmenopausal osteoporosis
Wei Fan, Zong-Zhe Jiang, Sheng-Rong Wan
Medicine.2023; 102(46): e35887. CrossRef - Network pharmacology-based pharmacological mechanism prediction of Lycii Fructus against postmenopausal osteoporosis
Jianbo Wang, Yi Wang, Leyan Li, Shuiqi Cai, Dandan Mao, Hongkan Lou, Jian Zhao
Medicine.2023; 102(48): e36292. CrossRef - Benefits of lumican on human bone health: clinical evidence using bone marrow aspirates
Yun Sun Lee, So Jeong Park, Jin Young Lee, Eunah Choi, Beom-Jun Kim
The Korean Journal of Internal Medicine.2022; 37(4): 821. CrossRef - ED-71 inhibited osteoclastogenesis by enhancing EphrinB2–EphB4 signaling between osteoclasts and osteoblasts in osteoporosis
Yuan Zhang, Yuying Kou, Panpan Yang, Xing Rong, Rong Tang, Hongrui Liu, Minqi Li
Cellular Signalling.2022; 96: 110376. CrossRef - Effects of Muscles on Bone Metabolism—with a Focus on Myokines
Beom-Jun Kim
Annals of Geriatric Medicine and Research.2022; 26(2): 63. CrossRef - Evaluation of the tolerability of zoledronic acid preparations for parenteral administration
I. A. Shafieva, S. V. Bulgakova, A. V. Shafieva
Meditsinskiy sovet = Medical Council.2022; (11): 96. CrossRef - Impact of Alendronate Sodium plus Elcatonin on Postoperative Bone Pain in Patients with Osteoporotic Fractures
Baohui Wang, Yindi Sun, Da Shi, Xiuwei Han, Na Liu, Bo Wang, Zhijun Liao
BioMed Research International.2022; 2022: 1. CrossRef - Current use of bone turnover markers in the management of osteoporosis
Jacques P. Brown, Andrew Don-Wauchope, Pierre Douville, Caroline Albert, Samuel D. Vasikaran
Clinical Biochemistry.2022; 109-110: 1. CrossRef - Study on the influence of balloon dilation mode on the intravertebral cleft of osteoporotic fracture
Nanning Lv, Xiaoxiao Feng, Haojun Liu, Xuejun Jia, Shanqin Han, Mingming Liu
BMC Surgery.2022;[Epub] CrossRef - An Acid-Sensitive Bone Targeting Delivery System Carrying Acacetin Prevents Osteoporosis in Ovariectomized Mice
Xiaochen Sun, Chenyu Song, Chenxi Zhang, Chunlei Xing, Juan Lv, Huihui Bian, Nanning Lv, Dagui Chen, Xin Dong, Mingming Liu, Li Su
Pharmaceuticals.2022; 16(1): 2. CrossRef - Changes in Serum Dickkopf-1, RANK Ligand, Osteoprotegerin, and Bone Mineral Density after Allogeneic Hematopoietic Stem Cell Transplantation Treatment
Eunhee Jang, Jeonghoon Ha, Ki-Hyun Baek, Moo Il Kang
Endocrinology and Metabolism.2021; 36(6): 1211. CrossRef
- Effects of stepwise administration of osteoprotegerin and parathyroid hormone-related peptide DNA vectors on bone formation in ovariectomized rat model

- Adrenal Gland
- Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
- Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
- Endocrinol Metab. 2021;36(3):553-563. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1008

- 3,657 View
- 142 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thermal ablation is a good alternative treatment in patients who are unable to undergo adrenalectomy. Even though the Asian Conference on Tumor Ablation (ACTA) has been held for many years, adrenal ablation guidelines have not been established. No guidelines for adrenal ablation are established in American and European countries, either. The aim of this review was to introduce the first version of ACTA guidelines for adrenal tumor ablation.
-
Citations
Citations to this article as recorded by- Treatment of primary aldosteronism: Clinical practice guidelines of the Taiwan Society of Aldosteronism
Chi-Shin Tseng, Chieh-Kai Chan, Hsiang-Ying Lee, Chien-Ting Pan, Kang-Yung Peng, Shuo-Meng Wang, Kuo-How Huang, Yao-Chou Tsai, Vin-Cent Wu, Jeff S. Chueh
Journal of the Formosan Medical Association.2024; 123: S125. CrossRef - Development and preclinical evaluation of multifunctional hydrogel for precise thermal protection during thermal ablation
Bowen Zheng, Peng Zhang, Qijun Lv, Tao Wu, Yadong Liu, Junjie Tang, Yanping Ma, Lili Cheng, Langtao Xu, Yizhen Wang, Yifan Xue, Jie Liu, Jie Ren
Bioactive Materials.2024; 31: 119. CrossRef - Case report of trans-renal ablation procedures for a recurrent pheochromocytoma in von Hippel-Lindau disease
Byung Kwan Park
Precision and Future Medicine.2023; 7(2): 90. CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef
- Treatment of primary aldosteronism: Clinical practice guidelines of the Taiwan Society of Aldosteronism

- Miscellanenous
- Cushing Syndrome Associated Myopathy: It Is Time for a Change
- Martin Reincke
- Endocrinol Metab. 2021;36(3):564-571. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1069
- 4,778 View
- 174 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
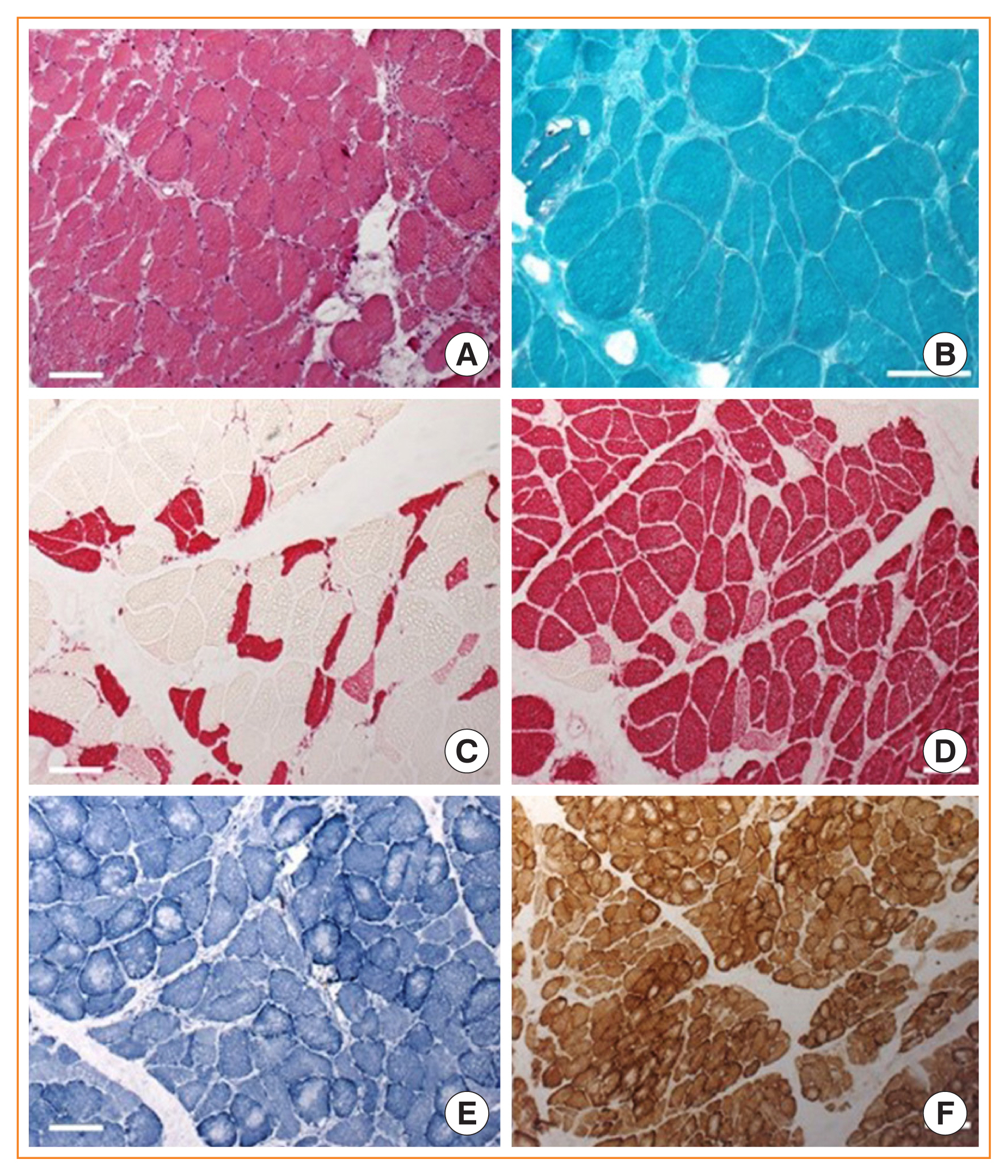
ePub - Cushing syndrome is the result of excessive levels of glucocorticoids. Endogenous Cushing syndrome is rare with an incidence of two to three cases per million per year. Clinically, the presentation consists of a characteristic phenotype including skin symptoms and metabolic manifestations. A frequent co-morbidity with high impact on quality of life is Cushing syndrome associated myopathy. It characteristically affects the proximal myopathy, impairing stair climbing and straightening up. The pathophysiology is complex and involves protein degradation via the forkhead box O3 (FOXO3) pathway, intramuscular fat accumulation, and inactivity-associated muscle atrophy. Surgical remission of Cushing syndrome is the most important step for recovery of muscle function. Restoration depends on age, co-morbidities and postoperative insulin-like growth factor concentrations. At average, functionality remains impaired during the long-term compared to age and sex matched control persons. Growth hormone therapy in individuals with impaired growth hormone secretion could be an option but has not been proved in a randomized trial.
-
Citations
Citations to this article as recorded by- Long-Term Consequences of Cushing Syndrome: A Systematic Literature Review
Soraya Puglisi, Anna Maria Elena Perini, Cristina Botto, Francesco Oliva, Massimo Terzolo
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e901. CrossRef - The Link between Mitochondrial Dysfunction and Sarcopenia: An Update Focusing on the Role of Pyruvate Dehydrogenase Kinase 4
Min-Ji Kim, Ibotombi Singh Sinam, Zerwa Siddique, Jae-Han Jeon, In-Kyu Lee
Diabetes & Metabolism Journal.2023; 47(2): 153. CrossRef - Intelligent Systems for Muscle Tracking: A Review on Sensor‐Algorithm Synergy
Arjun Putcha, Tien Nguyen, Regina Smith, Rachel Choffin, Wubin Bai
Advanced Intelligent Systems.2023;[Epub] CrossRef - Sarcopenia in youth
Han Na Jung, Chang Hee Jung, You-Cheol Hwang
Metabolism.2023; 144: 155557. CrossRef - Cushing Syndrome
Martin Reincke, Maria Fleseriu
JAMA.2023; 330(2): 170. CrossRef - Musculoskeletal complications of Cushing syndrome
Dorota Leszczyńska, Alicja Szatko, Lucyna Papierska, Wojciech Zgliczyński, Piotr Glinicki
Rheumatology.2023; 61(4): 271. CrossRef - Circulating myomiRNAs as biomarkers in patients with Cushing’s syndrome
C. Pivonello, R. Patalano, C. Simeoli, T. Montò, M. Negri, F. Amatrudo, N. Di Paola, A. Larocca, E. M. Crescenzo, R. Pirchio, D. Solari, C. de Angelis, R. S. Auriemma, L. M. Cavallo, A. Colao, R. Pivonello
Journal of Endocrinological Investigation.2023; 47(3): 655. CrossRef - Low-grade inflammation during the glucocorticoid withdrawal phase in patients with Cushing's syndrome
Frederick Vogel, Leah Braun, Stephanie Zopp, Elisabeth Nowak, Jochen Schreiner, Irina Benz, German Rubinstein, Heike Künzel, Katrin Ritzel, Matthias Kroiss, Jürgen Honegger, Felix Beuschlein, Katharina Schilbach, Daniel Teupser, Martin Bidlingmaier, Marti
European Journal of Endocrinology.2023; 188(4): 375. CrossRef - An odd case of immune-mediated necrotizing myopathy, complicated with sagittal, transverse and sigmoid sinus thrombosis
Andreea Trandafir, Violeta Claudia Bonjincă, Delia Tulba, Gelu Onose
Balneo and PRM Research Journal.2023; 14(Vol.14, no): 630. CrossRef - Morbidität und Mortalität beim Cushing-Syndrom
Frederick Vogel, Leah Braun, Martin Reincke
Der Internist.2022; 63(1): 34. CrossRef - Pathophysiology of Mild Hypercortisolism: From the Bench to the Bedside
Vittoria Favero, Arianna Cremaschi, Chiara Parazzoli, Alberto Falchetti, Agostino Gaudio, Luigi Gennari, Alfredo Scillitani, Fabio Vescini, Valentina Morelli, Carmen Aresta, Iacopo Chiodini
International Journal of Molecular Sciences.2022; 23(2): 673. CrossRef - Long‐term morbidity and mortality in patients with Cushing's syndrome
Leah T. Braun, Frederick Vogel, Martin Reincke
Journal of Neuroendocrinology.2022;[Epub] CrossRef - Clinical presentation and etiology of Cushing's syndrome: Data from ERCUSYN
Elena Valassi
Journal of Neuroendocrinology.2022;[Epub] CrossRef - Pyruvate dehydrogenase kinase 4 promotes ubiquitin–proteasome system‐dependent muscle atrophy
Ibotombi Singh Sinam, Dipanjan Chanda, Themis Thoudam, Min‐Ji Kim, Byung‐Gyu Kim, Hyeon‐Ji Kang, Jung Yi Lee, Seung‐Hoon Baek, Shin‐Yoon Kim, Bum Jin Shim, Dongryeol Ryu, Jae‐Han Jeon, In‐Kyu Lee
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(6): 3122. CrossRef - Consensus on diagnosis and management of Cushing's disease: a guideline update
Maria Fleseriu, Richard Auchus, Irina Bancos, Anat Ben-Shlomo, Jerome Bertherat, Nienke R Biermasz, Cesar L Boguszewski, Marcello D Bronstein, Michael Buchfelder, John D Carmichael, Felipe F Casanueva, Frederic Castinetti, Philippe Chanson, James Findling
The Lancet Diabetes & Endocrinology.2021; 9(12): 847. CrossRef
- Long-Term Consequences of Cushing Syndrome: A Systematic Literature Review

Editorial
- Diabetes, Obesity and Metabolism
- Identification of Protein Z as a Potential Novel Biomarker for the Diagnosis of Prediabetes
- Seung-Hoi Koo
- Endocrinol Metab. 2021;36(3):572-573. Published online June 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.303
- 2,809 View
- 115 Download

Original Articles
- Thyroid
- A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
- Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang, MASTER study group
- Endocrinol Metab. 2021;36(3):574-581. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.943
- 6,288 View
- 268 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
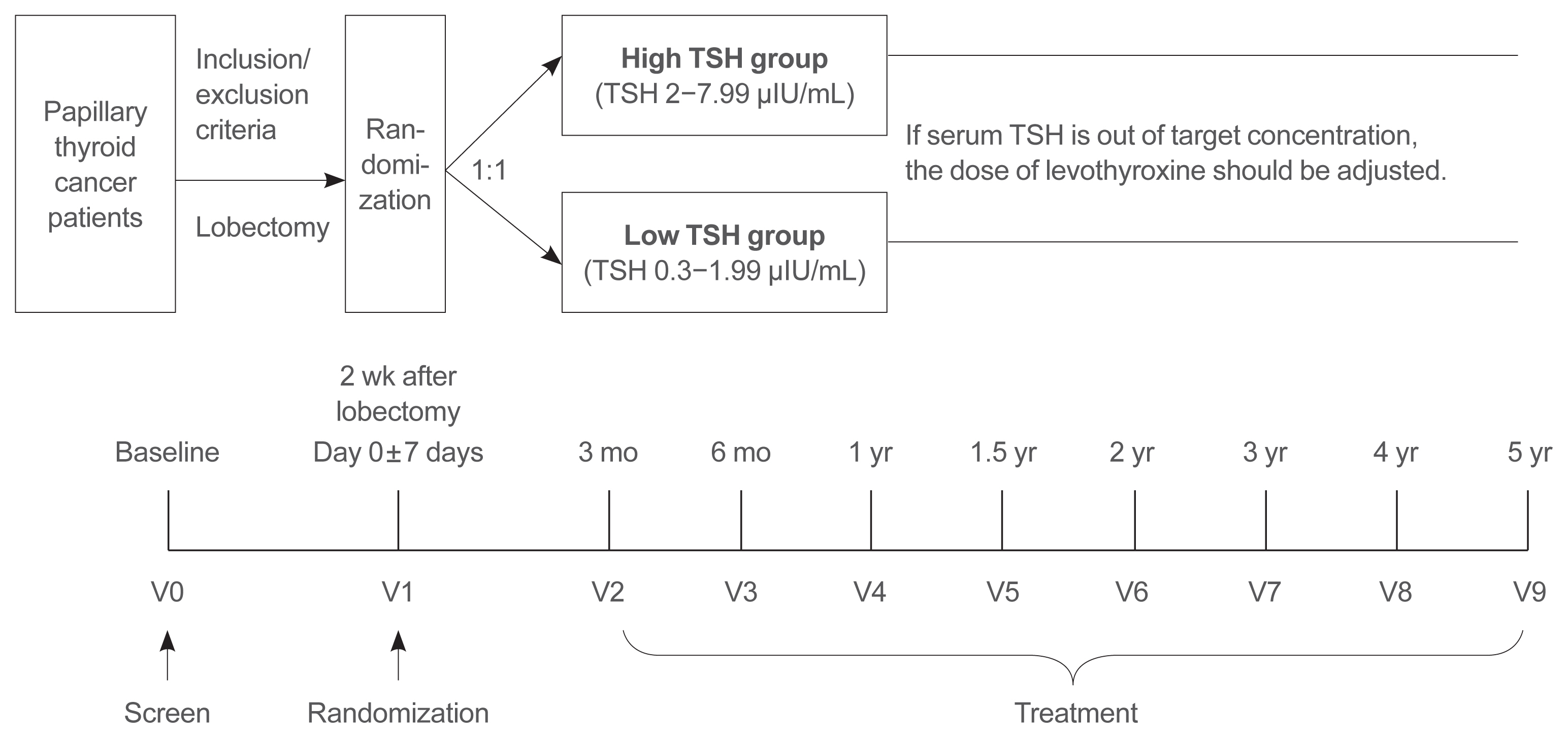
Postoperative thyroid stimulating hormone (TSH) suppression therapy is recommended for patients with intermediate- and high-risk differentiated thyroid cancer to prevent the recurrence of thyroid cancer. With the recent increase in small thyroid cancer cases, the extent of resection during surgery has generally decreased. Therefore, questions have been raised about the efficacy and long-term side effects of TSH suppression therapy in patients who have undergone a lobectomy.
Methods
This is a multicenter, prospective, randomized, controlled clinical trial in which 2,986 patients with papillary thyroid cancer are randomized into a high-TSH group (intervention) and a low-TSH group (control) after having undergone a lobectomy. The principle of treatment includes a TSH-lowering regimen aimed at TSH levels between 0.3 and 1.99 μIU/mL in the low-TSH group. The high-TSH group targets TSH levels between 2.0 and 7.99 μIU/mL. The dose of levothyroxine will be adjusted at each visit to maintain the target TSH level. The primary outcome is recurrence-free survival, as assessed by neck ultrasound every 6 to 12 months. Secondary endpoints include disease-free survival, overall survival, success rate in reaching the TSH target range, the proportion of patients with major cardiovascular diseases or bone metabolic disease, the quality of life, and medical costs. The follow-up period is 5 years.
Conclusion
The results of this trial will contribute to establishing the optimal indication for TSH suppression therapy in low-risk papillary thyroid cancer patients by evaluating the benefit and harm of lowering TSH levels in terms of recurrence, metabolic complications, costs, and quality of life. -
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Clinical impact of coexistent chronic lymphocytic thyroiditis on central lymph node metastasis in low- to intermediate-risk papillary thyroid carcinoma: The MASTER study
Da Beom Heo, Ho-Ryun Won, Kyung Tae, Yea Eun Kang, Eonju Jeon, Yong Bae Ji, Jae Won Chang, June Young Choi, Hyeong Won Yu, Eu Jeong Ku, Eun Kyung Lee, Mijin Kim, Jun-Ho Choe, Bon Seok Koo
Surgery.2024; 175(4): 1049. CrossRef - Dynamic Changes in Treatment Response af-ter 131I in Differentiated Thyroid Cancer and Their Relationship with Recurrence Risk Stratification and TNM Staging
璐 狄
Advances in Clinical Medicine.2024; 14(03): 1083. CrossRef - ASO Author Reflections: Active Surveillance may be Possible in Patients with T1b Papillary Thyroid Carcinoma Over 55 Years of Age Without High-Risk Features on Preoperative Examinations
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2254. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis
Timothy M Ullmann, Maria Papaleontiou, Julie Ann Sosa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(2): 271. CrossRef - Age-Dependent Clinicopathological Characteristics of Patients with T1b Papillary Thyroid Carcinoma: Implications for the Possibility of Active Surveillance
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2246. CrossRef - Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Mijin Kim, Yae Eun Kang, Young Joo Park, Bon Seok Koo, Eu Jeong Ku, June Young Choi, Eun Kyung Lee, Bo Hyun Kim
Endocrine.2023; 82(1): 134. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Thyroid stimulating hormone suppression and recurrence after thyroid lobectomy for papillary thyroid carcinoma
Mi Rye Bae, Sung Hoon Nam, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
Endocrine.2022; 75(2): 487. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Thyroid
- Insights from a Prospective Follow-up of Thyroid Function and Autoimmunity among COVID-19 Survivors
- David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung, Karen Siu Ling Lam
- Endocrinol Metab. 2021;36(3):582-589. Published online June 8, 2021
- DOI: https://doi.org/10.3803/EnM.2021.983
- 10,868 View
- 266 Download
- 32 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The occurrence of Graves’ disease and Hashimoto thyroiditis after coronavirus disease 2019 (COVID-19) raised concerns that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may trigger thyroid autoimmunity. We aimed to address the current uncertainties regarding incident thyroid dysfunction and autoimmunity among COVID-19 survivors.
Methods
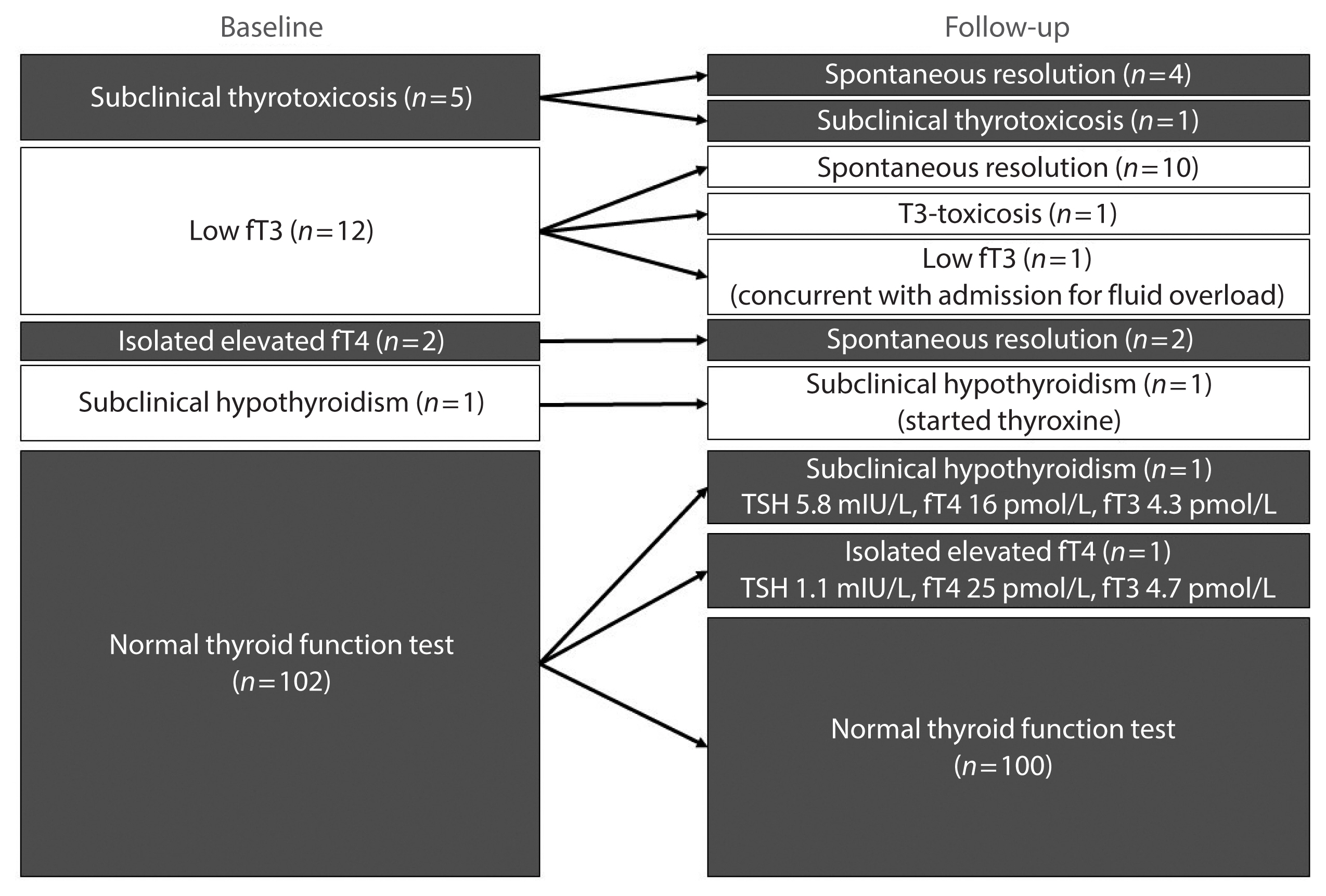
We included consecutive adult COVID-19 patients without known thyroid disorders, who were admitted to Queen Mary Hospital from July 21 to September 21, 2020 and had serum levels of thyroid-stimulating hormone, free thyroxine, free triiodothyronine (fT3), and anti-thyroid antibodies measured both on admission and at 3 months.
Results
In total, 122 patients were included. Among 20 patients with abnormal thyroid function tests (TFTs) on admission (mostly low fT3), 15 recovered. Among 102 patients with initial normal TFTs, two had new-onset abnormalities that could represent different phases of thyroiditis. Among 104 patients whose anti-thyroid antibody titers were reassessed, we observed increases in anti-thyroid peroxidase (TPO) (P<0.001) and anti-thyroglobulin (P<0.001), but not anti-thyroid stimulating hormone receptor titers (P=0.486). Of 82 patients with negative anti-TPO findings at baseline, 16 had a significant interval increase in anti-TPO titer by >12 U, and four became anti-TPO-positive. Worse baseline clinical severity (P=0.018), elevated C-reactive protein during hospitalization (P=0.033), and higher baseline anti-TPO titer (P=0.005) were associated with a significant increase in anti-TPO titer.
Conclusion
Most patients with thyroid dysfunction on admission recovered during convalescence. Abnormal TFTs suggestive of thyroiditis occurred during convalescence, but infrequently. Importantly, our novel observation of an increase in anti-thyroid antibody titers post-COVID-19 warrants further follow-up for incident thyroid dysfunction among COVID-19 survivors. -
Citations
Citations to this article as recorded by- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis
Sadra Ashrafi, Hossein Hatami, Razieh Bidhendi-Yarandi, Mohammad Hossein Panahi
BMC Endocrine Disorders.2024;[Epub] CrossRef - Does COVID-19 affect thyroid more than non-COVID-19 infections? A retrospective study
Yasemin Ucal, Muhittin Serdar, Hande Karpuzoğlu, Neval Yurttutan Uyar, Meltem Kilercik, Mustafa Serteser, Aysel Ozpinar
Turkish Journal of Biochemistry.2024;[Epub] CrossRef - Thyroiditis and COVID-19: focus on pediatric age. A narrative review
F. d’Aniello, M. E. Amodeo, A. Grossi, G. Ubertini
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - The most common persistent symptoms in patients with COVID-19 who were evaluated in the Internal Medicine polyclinic
Zeynep KOÇ, Seydahmet AKIN
The European Research Journal.2023; 9(1): 97. CrossRef - Clinical assessment of children with long COVID syndrome
Réka Garai, Péter Krivácsy, Vivien Herczeg, Fanni Kovács, Bálint Tél, Judit Kelemen, Anna Máthé, Eszter Zsáry, Johanna Takács, Dániel Sándor Veres, Attila J. Szabó
Pediatric Research.2023; 93(6): 1616. CrossRef - T Cell Receptor Sequences Amplified during Severe COVID-19 and Multisystem Inflammatory Syndrome in Children Mimic SARS-CoV-2, Its Bacterial Co-Infections and Host Autoantigens
Robert Root-Bernstein, Elizabeth Churchill, Shelby Oliverio
International Journal of Molecular Sciences.2023; 24(2): 1335. CrossRef - A Literature Review on SARS-CoV-2 and Other Viruses in Thyroid Disorders: Environmental Triggers or No-Guilty Bystanders?
Francesca Gorini, Cristina Vassalle
International Journal of Environmental Research and Public Health.2023; 20(3): 2389. CrossRef - Thyroid dysfunction as a long-term post-COVID-19 complication in mild-to-moderate COVID-19
Vesselina Yanachkova, Teodora Stankova, Radiana Staynova
Biotechnology & Biotechnological Equipment.2023; 37(1): 194. CrossRef - The Influence of SARS-CoV-2 Infection on the Thyroid Gland
Aleksandra Piekarska, Marta Góral, Marta Kozula, Aleksandra Jawiarczyk-Przybyłowska, Katarzyna Zawadzka, Marek Bolanowski
Biomedicines.2023; 11(2): 614. CrossRef - Thyroid Function Abnormalities and Outcomes in Hospitalized Patients
with COVID-19 Infection: A Cross-Sectional Study
Deepika Patel, Dukhabandhu Naik, Sadishkumar Kamalanathan, Kadhiravan Tamilarasu, Jayaprakash Sahoo, Ayan Roy, Chandhana Merugu, Varun Suryadevara
Hormone and Metabolic Research.2023; 55(03): 169. CrossRef - The Spectrum of Thyroid Function Tests and Autoantibodies During Hospitalization and After Six Months of Discharge in COVID-19 Patients: Does COVID-19 Trigger Autoimmunity?
Ziynet Alphan Uc, Pinar Yagcı, Zelal Adibelli, Cevdet Duran
Endocrine Research.2023; 48(2-3): 44. CrossRef - Increased prevalence of autoimmune thyroid disease after COVID-19: A single-center, prospective study
Alessandro Rossini, Sara Cassibba, Francesca Perticone, Simone Vasilij Benatti, Serena Venturelli, Greta Carioli, Arianna Ghirardi, Marco Rizzi, Tiziano Barbui, Roberto Trevisan, Silvia Ippolito
Frontiers in Endocrinology.2023;[Epub] CrossRef - A prospective follow-up of thyroid volume and thyroiditis features on ultrasonography among survivors of predominantly mild to moderate COVID-19
Man Him Matrix Fung, David Tak Wai Lui, Keith Wan Hang Chiu, Sherman Haynam Lee, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Chun Yiu Law, Kelvin Kai Wang To, Ching W
PeerJ.2023; 11: e15034. CrossRef - Study on Clinicopathological Features and Risk Factors of Patients with Multiple Primary Breast Cancers and Thyroid Disease
Jie Li, Yonghong Liu, Jian Jin, Qingfeng Shi, Yanting Ji, Bo Zhang, Pengfei Hu, Jinghua Pan
Mediators of Inflammation.2023; 2023: 1. CrossRef - Beyond Acute COVID-19: Investigating the Incidence of Subacute Thyroiditis in Long COVID-19 in Korea
Jeongmin Lee, Gi Hyeon Seo, Keeho Song
Endocrinology and Metabolism.2023; 38(4): 455. CrossRef - Thyroid Autoimmunity and SARS-CoV-2 Infection
Poupak Fallahi, Giusy Elia, Francesca Ragusa, Sabrina Rosaria Paparo, Armando Patrizio, Eugenia Balestri, Valeria Mazzi, Salvatore Benvenga, Gilda Varricchi, Laura Gragnani, Chiara Botrini, Enke Baldini, Marco Centanni, Clodoveo Ferri, Alessandro Antonell
Journal of Clinical Medicine.2023; 12(19): 6365. CrossRef - Autoimmune complications of COVID‐19
Niloufar Yazdanpanah, Nima Rezaei
Journal of Medical Virology.2022; 94(1): 54. CrossRef - The Independent Association of TSH and Free Triiodothyronine Levels With Lymphocyte Counts Among COVID-19 Patients
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Chloe Yu Yan Cheung, Carol Ho Yi Fong, Chun Yiu Law, Kelvin Kai Wang To, Ching Wan Lam, Kathryn Choon Beng Tan, Yu Cho Woo, Ivan Fan Ngai Hung,
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comment on Khunti et al. COVID-19, Hyperglycemia, and New-Onset Diabetes. Diabetes Care 2021;44:2645–2655
Carmine Gazzaruso, Adriana Coppola, Pietro Gallotti, Ileana Terruzzi, Tiziana Montalcini, Livio Luzi
Diabetes Care.2022; 45(2): e45. CrossRef - The potential impact of COVID-19 on thyroid gland volumes among COVID-19 survivors
Emre Urhan, Zuleyha Karaca, Canan Sehit Kara, Zeynep Ture Yuce, Kursad Unluhizarci
Endocrine.2022; 76(3): 635. CrossRef - Systematic review of COVID-19 and autoimmune thyroiditis
Esra Tutal, Resat Ozaras, Hakan Leblebicioglu
Travel Medicine and Infectious Disease.2022; 47: 102314. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Should we expect a wave of type 1 diabetes following SARS‐CoV‐2 pandemic?
Laura Montefusco, Andrea Mario Bolla, Paolo Fiorina
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - COVID-19 and Thyroid Function: A Bi-Directional Two-Sample Mendelian Randomization Study
Gloria Hoi-Yee Li, Ching-Man Tang, Ching-Lung Cheung
Thyroid.2022; 32(9): 1037. CrossRef - Development of a prediction score (ThyroCOVID) for identifying abnormal thyroid function in COVID-19 patients
D. T. W. Lui, C. H. Lee, W. S. Chow, A. C. H. Lee, A. R. Tam, C. Y. Y. Cheung, C. H. Y. Fong, S. T. M. Kwok, C. Y. Law, K. K. W. To, C. W. Lam, K. C. B. Tan, Y. C. Woo, I. F. N. Hung, K. S. L. Lam
Journal of Endocrinological Investigation.2022; 45(11): 2149. CrossRef - Symptomatic Bradycardia Manifesting as Acute Hypothyroidism Following COVID-19 Infection: A Case Report
Jaydip Desai, Arsh N Patel, Courtney L Evans, Molly Triggs, Fulton Defour
Cureus.2022;[Epub] CrossRef - Schilddrüse und SARS-CoV-2
Georg Zettinig
Journal für Klinische Endokrinologie und Stoffwechsel.2022; 15(3): 100. CrossRef - Thyroid diseases are associated with coronavirus disease 2019 infection
Yutian Tian, Junyu Zhao, Tingting Wang, Haipeng Wang, Jinming Yao, Song Wang, Yaru Mou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Thyrotropin Levels in Patients with Coronavirus Disease 2019: Assessment during Hospitalization and in the Medium Term after Discharge
Abdallah Al-Salameh, Noémie Scherman, Imane Adda, Juliette André, Yoann Zerbib, Julien Maizel, Jean-Daniel Lalau, Etienne Brochot, Claire Andrejak, Rachel Desailloud
Life.2022; 12(12): 2014. CrossRef - Long COVID in Patients With Mild to Moderate Disease: Do Thyroid Function and Autoimmunity Play a Role?
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung,
Endocrine Practice.2021; 27(9): 894. CrossRef - Hashimoto’s thyroiditis following SARS-CoV-2 infection
Rafael Silvestre Knack, Taliê Hanada, Renata Silvestre Knack, Kamilla Mayr
BMJ Case Reports.2021; 14(8): e244909. CrossRef - Higher SARS-CoV-2 viral loads correlated with smaller thyroid volumes on ultrasound among male COVID-19 survivors
David Tak Wai Lui, Matrix Man Him Fung, Keith Wan Hang Chiu, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Wade Wei Wong, Cassandra Yuen Yan Lee, Chun Yiu Law, Kelvin K
Endocrine.2021; 74(2): 205. CrossRef - SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases
Avaniyapuram Kannan Murugan, Ali S Alzahrani
Journal of Inflammation Research.2021; Volume 14: 6191. CrossRef - POST-COVID ENDOCRINOPATHY :ABOUT A CASE ENDOCRINOPATHIE POST- COVID :À PROPOS D’UN CAS
S. Rafi, G. Elmghari, N, Elansari
INDIAN JOURNAL OF APPLIED RESEARCH.2021; : 13. CrossRef
- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis

- Thyroid
- Effect of Cigarette Smoking on Thyroid Cancer: Meta-Analysis
- Joon-Hyop Lee, Young Jun Chai, Ka Hee Yi
- Endocrinol Metab. 2021;36(3):590-598. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.954
- 12,507 View
- 191 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Although smoking is generally carcinogenic, its effect on thyroid cancers is still subject to controversy. The purpose of this study was to summarize the role of smoking in relation to thyroid cancer occurrence.
Methods
We performed a meta-analysis of 24 eligible studies: 21 case-control studies and three prospective cohort studies. The summary odds ratio (OR) and 95% confidence interval (CI) of all studies were acquired based on random effect model. Further subgroup analyses were conducted according to gender, histological type of thyroid cancer, and smoking status of patients for the case-control studies.
Results
The summary effect size indicated a negative association of smoking for thyroid cancer (OR, 0.798; 95% CI, 0.681 to 0.935). From the subgroup analyses for the case-control studies, reduced risk of thyroid cancer was observed in both men (OR, 0.734; 95% CI, 0.553 to 0.974) and women (OR, 0.792; 95% CI, 0.700 to 0.897). The protective effect of smoking was observed in studies in which thyroid cancer was limited to differentiated thyroid cancers (DTCs) (OR, 0.798; 95% CI, 0.706 to 0.902).
Conclusion
Our results suggests that smoking may have a protective effect on thyroid cancer, especially on DTCs. Further studies with larger sample sizes should be conducted in elucidating the dose and time dependent effect of smoking on thyroid cancer with specific focus on the types of thyroid cancers. -
Citations
Citations to this article as recorded by- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders
I. M. Belovalova, E. S. Shugurova, M. O. Korchagina, T. N. Borkhoeva, M. S. Sheremeta
Clinical and experimental thyroidology.2024; 19(2): 11. CrossRef - Relationship between Serum Levels of Selenium and Thyroid Cancer: A Systematic Review and Meta-Analysis
Runhua Hao, Ping Yu, Lanlan Gui, Niannian Wang, Da Pan, Shaokang Wang
Nutrition and Cancer.2023; 75(1): 14. CrossRef - Potentially inappropriate medication and frailty in older adults: A systematic review and meta-analysis
Wenlian Ma, Hongyan Wang, Zhifei Wen, Linfeng Liu, Xiangeng Zhang
Archives of Gerontology and Geriatrics.2023; 114: 105087. CrossRef - Inflammation biomarkers are associated with the incidence of cardiovascular disease: a meta-analysis
Yifei Liu, Suzhen Guan, Haiming Xu, Na Zhang, Min Huang, Zhihong Liu
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Maternal gestational weight gain and offspring’s neurodevelopmental outcomes: A systematic review and meta-analysis
Dan Wu, Yicheng Li, Lingyan Chen, Marieke Klein, Barbara Franke, Jinjin Chen, Jan Buitelaar
Neuroscience & Biobehavioral Reviews.2023; 153: 105360. CrossRef - Association of preoperative hypoprotein malnutrition with spinal postoperative complications and other conditions: A systematic review and meta-analysis
Yongrong Hu, Liping Wang, Hao Liu, Kunhai Yang, Song Wang, Xiang Zhang, Bo Qu, Hongsheng Yang
Clinical Nutrition ESPEN.2023; 57: 448. CrossRef - Metabolic syndrome and risk of ovarian cancer: a systematic review and meta-analysis
Ziyu Chen, Zesi Liu, Hongxia Yang, Chaosheng Liu, Fandou Kong
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cigarette smoking and thyroid cancer risk: A Mendelian randomization study
Hongzhan Jiang, Yi Li, Jiali Shen, Huihui Lin, Siyue Fan, Rongliang Qiu, Jiaxi He, Ende Lin, Lijuan Chen
Cancer Medicine.2023; 12(19): 19866. CrossRef - Longitudinal Changes in Smoking Habits in Women and Subsequent Risk of Cancer
Thi Xuan Mai Tran, Soyeoun Kim, Huiyeon Song, Boyoung Park
American Journal of Preventive Medicine.2022; 63(6): 894. CrossRef
- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders

- Thyroid
- Programmed Cell Death-Ligand 1 (PD-L1) gene Single Nucleotide Polymorphism in Graves’ Disease and Hashimoto’s Thyroiditis in Korean Patients
- Jee Hee Yoon, Min-ho Shin, Hee Nam Kim, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2021;36(3):599-606. Published online June 2, 2021
- DOI: https://doi.org/10.3803/EnM.2021.965

- 3,997 View
- 117 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Programmed cell death-ligand 1 (PD-L1) has an important role in regulating immune reactions by binding to programmed death 1 (PD-1) on immune cells, which could prevent the exacerbation of autoimmune thyroid disease (AITD). The aim of this study was to evaluate the association of PD-L1 polymorphism with AITD, including Graves’ disease (GD) and Hashimoto’s thyroiditis (HT).
Methods
A total of 189 GD patients, 234 HT patients, and 846 healthy age- and sex-matched controls were enrolled in this study. We analyzed PD-L1 single nucleotide polymorphism (SNP) (rs822339) and investigated the associations with clinical disease course and outcome.
Results
Genotype frequency at the PD-L1 marker RS822339 in GD (P=0.219) and HT (P=0.764) patients did not differ from that among healthy controls. In patients with GD, the A/G or G/G genotype group demonstrated higher TBII titer (20.6±20.5 vs. 28.0± 25.8, P=0.044) and longer treatment duration (39.0±40.4 months vs. 62.4±65.0 months, P=0.003) compared to the A/A genotype group. Among patients in whom anti-thyroid peroxidase (TPO) antibody was measured after treatment of GD, post-treatment antiTPO positivity was higher in the A/G or G/G genotype group compared to the A/A genotype group (48.1% vs. 69.9%, P=0.045). Among patients with HT, there was no significant difference of anti-TPO antibody positivity (79.4% vs. 68.6%, P=0.121), anti-thyroglobulin antibody positivity (80.9% vs. 84.7%, P=0.661), or development to overt hypothyroidism (68.0% vs. 71.1%, P=0.632) between the A/A genotype group and the A/G or G/G genotype group.
Conclusion
The genotype frequency of PD-L1 (rs822339) is not different in patients with AITD compared with healthy controls. The intact PD-1/PD-L1 pathway in GD and HT might be important to maintain chronicity of AITD by protecting immune tolerance. However, the PD-L1 SNP could be associated with difficulty in achieving remission in patients with GD, which may be helpful to predict the possibility of longer treatment. Further studies are required to investigate the complex immune tolerance system in patients with AITD. -
Citations
Citations to this article as recorded by- Synergistic effects of BTN3A1, SHP2, CD274, and STAT3 gene polymorphisms on the risk of systemic lupus erythematosus: a multifactorial dimensional reduction analysis
Yang-Yang Tang, Wang-Dong Xu, Lu Fu, Xiao-Yan Liu, An-Fang Huang
Clinical Rheumatology.2024; 43(1): 489. CrossRef - Relationship between CD274 gene polymorphism and systemic lupus erythematosus risk in a Chinese Han population
Lu‐Qi Yang, Zhen Qin, Lu Fu, Wang‐Dong Xu
International Journal of Rheumatic Diseases.2024;[Epub] CrossRef
- Synergistic effects of BTN3A1, SHP2, CD274, and STAT3 gene polymorphisms on the risk of systemic lupus erythematosus: a multifactorial dimensional reduction analysis


 KES
KES



 First
First Prev
Prev



