Search
- Page Path
- HOME > Search
- Adrenal gland
- The Fascinating Interplay between Growth Hormone, Insulin-Like Growth Factor-1, and Insulin
- Eline C. Nijenhuis-Noort, Kirsten A. Berk, Sebastian J. C. M. M. Neggers, Aart J. van der Lely
- Endocrinol Metab. 2024;39(1):83-89. Published online January 9, 2024
- DOI: https://doi.org/10.3803/EnM.2024.101
- 1,785 View
- 133 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
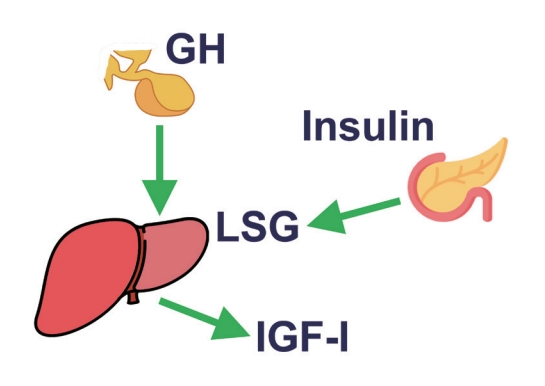
ePub - This review intends to provide the reader with a practical overview of several (patho)physiological conditions in which knowledge of the interplay between growth hormone (GH), insulin-like growth factor-1 (IGF-1), and insulin is important. This might help treating physicians in making the right decisions on how to intervene and improve metabolism for the benefit of patients, and to understand why and how metabolism responds in their specific cases. We will specifically address the interplay between GH, IGF-1, and insulin in type 1 and 2 diabetes mellitus, liver cirrhosis, and acromegaly as examples in which this knowledge is truly necessary.
-
Citations
Citations to this article as recorded by- IGF-1 and IGF-2 as Molecules Linked to Causes and Consequences of Obesity from Fetal Life to Adulthood: A Systematic Review
Justyna Szydlowska-Gladysz, Adrianna Edyta Gorecka, Julia Stepien, Izabela Rysz, Iwona Ben-Skowronek
International Journal of Molecular Sciences.2024; 25(7): 3966. CrossRef
- IGF-1 and IGF-2 as Molecules Linked to Causes and Consequences of Obesity from Fetal Life to Adulthood: A Systematic Review

- Miscellaneous
- AM1638, a GPR40-Full Agonist, Inhibited Palmitate- Induced ROS Production and Endoplasmic Reticulum Stress, Enhancing HUVEC Viability in an NRF2-Dependent Manner
- Hwan-Jin Hwang, Joo Won Kim, SukHwan Yun, Min Jeong Park, Eyun Song, Sooyeon Jang, Ahreum Jang, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Endocrinol Metab. 2023;38(6):760-769. Published online November 2, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1774

- 1,269 View
- 85 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
G protein-coupled receptor 40 (GPR40) is a key molecule in diabetes and fatty liver, but its role in endothelial dysfunction remains unclear. Our objective in this study was to determine whether GPR40 agonists protect endothelial cells against palmitatemediated oxidative stress.
Methods
Human umbilical vein endothelial cells (HUVECs) were used to investigate effects of various GPR40 agonists on vascular endothelium.
Results
In HUVECs, AM1638, a GPR40-full agonist, enhanced nuclear factor erythroid 2–related factor 2 (NRF2) translocation to the nucleus and heme oxygenase-1 (HO-1) expression, which blocked palmitate-induced superoxide production. Those antioxidant effects were not detected after treatment with LY2922470 or TAK875, GPR40-partial agonists, suggesting that GPR40 regulates reactive oxygen species (ROS) removal in a ligand-dependent manner. We also found that palmitate-induced CCAAT/enhancer‐binding protein homologous protein expression; X-box binding protein-1 splicing, nuclear condensation, and fragmentation; and caspase-3 cleavage were all blocked in an NRF2-dependent manner after AM1638 treatment. Both LY2922470 and TAK875 also improved cell viability independent of the NRF2/ROS pathway by reducing palmitate-mediated endoplasmic reticulum stress and nuclear damage. GPR40 agonists thus have beneficial effects against palmitate in HUVECs. In particular, AM1638 reduced palmitate-induced superoxide production and cytotoxicity in an NRF2/HO-1 dependent manner.
Conclusion
GPR40 could be developed as a good therapeutic target to prevent or treat cardiovascular diseases such as atherosclerosis.

- Diabetes, obesity and metabolism
- Inhibition of Fatty Acid β-Oxidation by Fatty Acid Binding Protein 4 Induces Ferroptosis in HK2 Cells Under High Glucose Conditions
- Jiasi Chen, Keping Wu, Yan Lei, Mingcheng Huang, Lokyu Cheng, Hui Guan, Jiawen Lin, Ming Zhong, Xiaohua Wang, Zhihua Zheng
- Endocrinol Metab. 2023;38(2):226-244. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1604
- 3,668 View
- 180 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
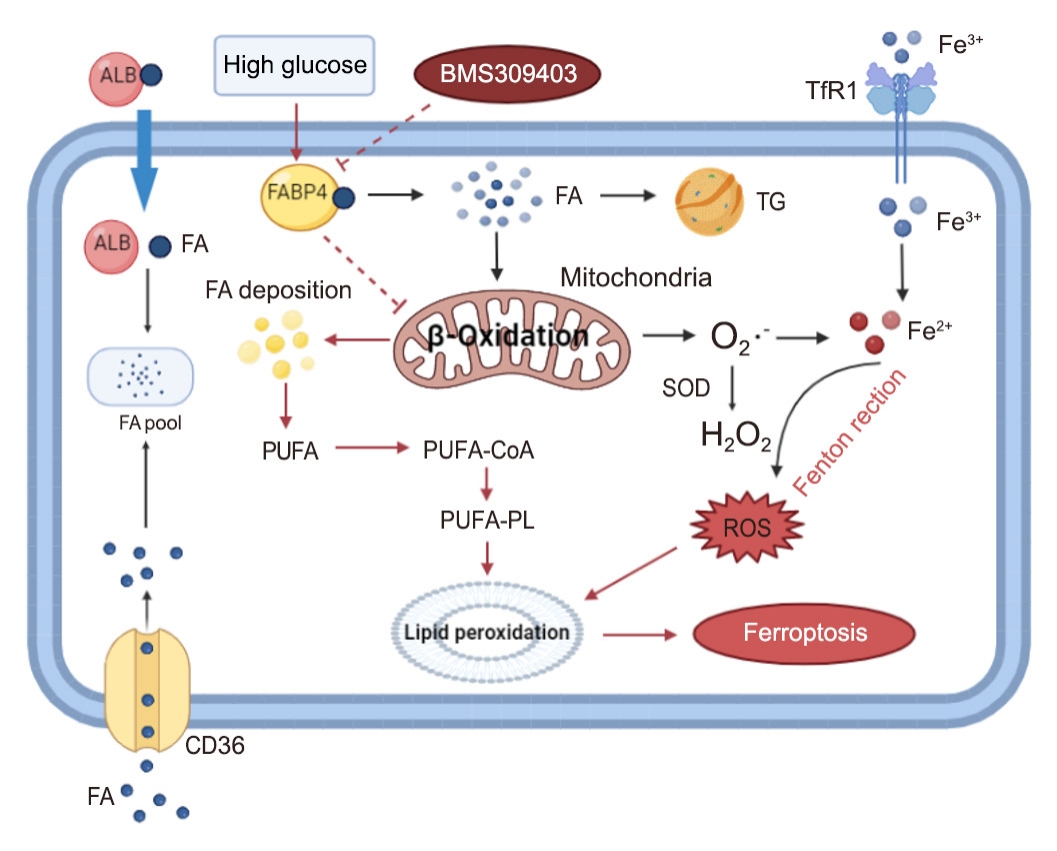
Ferroptosis, which is caused by an iron-dependent accumulation of lipid hydroperoxides, is a type of cell death linked to diabetic kidney disease (DKD). Previous research has shown that fatty acid binding protein 4 (FABP4) is involved in the regulation of ferroptosis in diabetic retinopathy. The present study was constructed to explore the role of FABP4 in the regulation of ferroptosis in DKD.
Methods
We first detected the expression of FABP4 and proteins related to ferroptosis in renal biopsies of patients with DKD. Then, we used a FABP4 inhibitor and small interfering RNA to investigate the role of FABP4 in ferroptosis induced by high glucose in human renal proximal tubular epithelial (HG-HK2) cells.
Results
In kidney biopsies of DKD patients, the expression of FABP4 was elevated, whereas carnitine palmitoyltransferase-1A (CP-T1A), glutathione peroxidase 4, ferritin heavy chain, and ferritin light chain showed reduced expression. In HG-HK2 cells, the induction of ferroptosis was accompanied by an increase in FABP4. Inhibition of FABP4 in HG-HK2 cells changed the redox state, sup-pressing the production of reactive oxygen species, ferrous iron (Fe2+), and malondialdehyde, increasing superoxide dismutase, and reversing ferroptosis-associated mitochondrial damage. The inhibition of FABP4 also increased the expression of CPT1A, reversed lipid deposition, and restored impaired fatty acid β-oxidation. In addition, the inhibition of CPT1A could induce ferroptosis in HK2 cells.
Conclusion
Our results suggest that FABP4 mediates ferroptosis in HG-HK2 cells by inhibiting fatty acid β-oxidation. -
Citations
Citations to this article as recorded by- Fatty Acid Binding Protein-4 Silencing Inhibits Ferroptosis to Alleviate Lipopolysaccharide-induced Injury of Renal Tubular Epithelial Cells by Blocking Janus Kinase 2/Signal Transducer and Activator of Transcription 3 Signaling
Suo Xu, Jiye Luo, Yanli Wang, Xiaobing Chen
Chinese Journal of Physiology.2024; 67(1): 47. CrossRef - Ferroptosis in Liver Disease: Natural Active Compounds and Therapeutic Implications
Zhili Wu, Yanru Zhu, Wenchao Liu, Balamuralikrishnan Balasubramanian, Xiao Xu, Junhu Yao, Xinjian Lei
Antioxidants.2024; 13(3): 352. CrossRef - Investigating the Role of FABP4 in Diabetes and Obesity and the Influence of Age and Ethnicity: A Comprehensive Analysis of a Cohort from the KEDP-Study
Mohammed A. Abdalla, Jehad Abubaker, Mohamed Abu-Farha, Irina Al-Khairi, Preethi Cherian, Mohammad G. Qaddoumi, Fatema Al-Rashed, Thangavel Alphonse Thanaraj, Ahmed N. Albatineh, Fahd Al-Mulla
International Journal of Molecular Sciences.2024; 25(9): 4578. CrossRef - Mechanisms and regulations of ferroptosis
Xu-Dong Zhang, Zhong-Yuan Liu, Mao-Sen Wang, Yu-Xiang Guo, Xiang-Kun Wang, Kai Luo, Shuai Huang, Ren-Feng Li
Frontiers in Immunology.2023;[Epub] CrossRef - Targeting epigenetic and posttranslational modifications regulating ferroptosis for the treatment of diseases
Yumin Wang, Jing Hu, Shuang Wu, Joshua S. Fleishman, Yulin Li, Yinshi Xu, Wailong Zou, Jinhua Wang, Yukuan Feng, Jichao Chen, Hongquan Wang
Signal Transduction and Targeted Therapy.2023;[Epub] CrossRef
- Fatty Acid Binding Protein-4 Silencing Inhibits Ferroptosis to Alleviate Lipopolysaccharide-induced Injury of Renal Tubular Epithelial Cells by Blocking Janus Kinase 2/Signal Transducer and Activator of Transcription 3 Signaling

- Thyroid
- Identification of Mutations in the Thyroxine-Binding Globulin (TBG) Gene in Patients with TBG Deficiency in Korea
- Jung Heo, Sang-Mi Kim, Hyun Jin Ryu, Hyunju Park, Tae Hyuk Kim, Jae Hoon Chung, Hyung-Doo Park, Sun Wook Kim
- Endocrinol Metab. 2022;37(6):870-878. Published online December 7, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1591
- 1,791 View
- 198 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
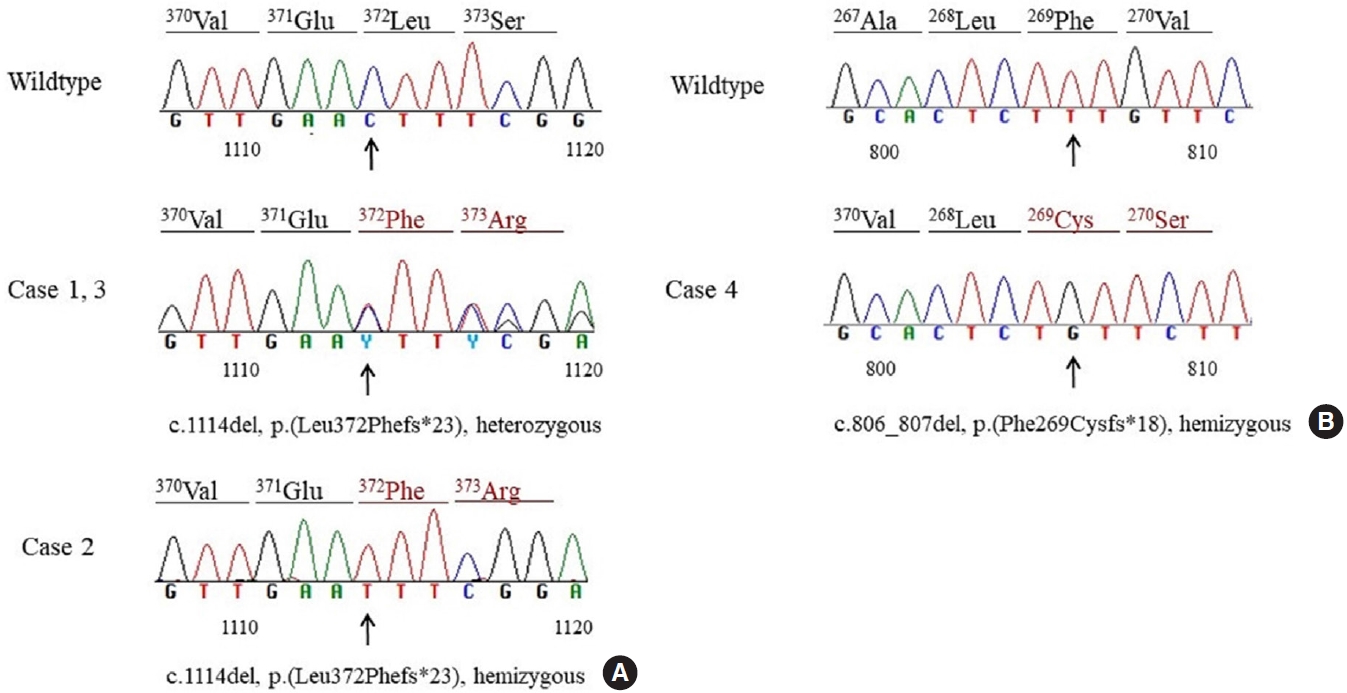
Thyroxine-binding globulin (TBG) is a major transporter protein for thyroid hormones. The serpin family A member 7 (SERPINA7) gene codes for TBG, and mutations of the SERPINA7 gene result in TBG deficiency. Although more than 40 mutations have been reported in several countries, only a few studies of TBG deficiency and SERPINA7 gene mutation have been performed in Korea. The aim of this study is to review the clinical presentations and laboratory findings of patients with TBG deficiency and to investigate the types of SERPINA7 gene mutation.
Methods
Five unrelated Korean adults with TBG deficiency attending endocrinology clinic underwent SERPINA7 gene sequencing. Four patients harbored a SERPINA7 gene mutation. Serum thyroid hormones, anti-microsomal antibodies, and TBG were measured. Genomic DNA was extracted from whole blood. All exons and intron-exon boundaries of the TBG gene were amplified and sequencing was performed.
Results
Two patients were heterozygous females, and the other two were hemizygous males. One heterozygous female had coexisting hypothyroidism. The other heterozygous female was erroneously prescribed levothyroxine at a local clinic. One hemizygous male harbored a novel mutation, p.Phe269Cysfs*18, which caused TBG partial deficiency. Three patients had the p.Leu372Phefs*23 mutation, which is known as TBG-complete deficiency Japan (TBG-CDJ) and was also presented in previous mutation analyses in Korea.
Conclusion
This study presents four patients diagnosed with TBG deficiency and provides the results of SERPINA7 gene sequencing. One novel mutation, p.Phe269Cysfs*18, causing TBD-partial deficiency and three cases of TBG-CDJ were demonstrated. It is necessary to identify TBG deficiency to prevent improper treatment. Also, sequencing of the SERPINA7 gene would provide valuable information about the TBG variants in Korea. -
Citations
Citations to this article as recorded by- Development and basic performance verification of a rapid homogeneous bioassay for agonistic antibodies against the thyroid-stimulating hormone receptor
Motoki Hoshina, Shiomi Ojima, Atsushi Kawasaki, Kosuke Doi, Satoshi Ohta, Asuka Inoue, Hiroshi Murayama
Journal of Immunological Methods.2024; 528: 113655. CrossRef
- Development and basic performance verification of a rapid homogeneous bioassay for agonistic antibodies against the thyroid-stimulating hormone receptor

- Miscellaneous
- Protective Effect of Delta-Like 1 Homolog Against Muscular Atrophy in a Mouse Model
- Ji Young Lee, Minyoung Lee, Dong-Hee Lee, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
- Endocrinol Metab. 2022;37(4):684-697. Published online August 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1446
- 3,267 View
- 129 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
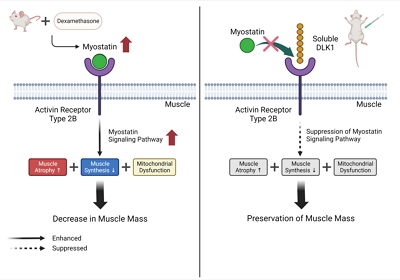
ePub - Background
Muscle atrophy is caused by an imbalance between muscle growth and wasting. Delta-like 1 homolog (DLK1), a protein that modulates adipogenesis and muscle development, is a crucial regulator of myogenic programming. Thus, we investigated the effect of exogenous DLK1 on muscular atrophy.
Methods
We used muscular atrophy mouse model induced by dexamethasone (Dex). The mice were randomly divided into three groups: (1) control group, (2) Dex-induced muscle atrophy group, and (3) Dex-induced muscle atrophy group treated with DLK1. The effects of DLK1 were also investigated in an in vitro model using C2C12 myotubes.
Results
Dex-induced muscular atrophy in mice was associated with increased expression of muscle atrophy markers and decreased expression of muscle differentiation markers, while DLK1 treatment attenuated these degenerative changes together with reduced expression of the muscle growth inhibitor, myostatin. In addition, electron microscopy revealed that DLK1 treatment improved mitochondrial dynamics in the Dex-induced atrophy model. In the in vitro model of muscle atrophy, normalized expression of muscle differentiation markers by DLK1 treatment was mitigated by myostatin knockdown, implying that DLK1 attenuates muscle atrophy through the myostatin pathway.
Conclusion
DLK1 treatment inhibited muscular atrophy by suppressing myostatin-driven signaling and improving mitochondrial biogenesis. Thus, DLK1 might be a promising candidate to treat sarcopenia, characterized by muscle atrophy and degeneration.

- Diabetes, Obesity and Metabolism
- Musclin Is Related to Insulin Resistance and Body Composition, but Not to Body Mass Index or Cardiorespiratory Capacity in Adults
- Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis Valbuena, Andrés F. Milán, María C. Trillos-Almanza, Sergio Granados, Miguel Peña, Mauricio Estrada-Castrillón, Juan C. Aristizábal, Raúl Narvez-Sanchez, Jaime Gallo-Villegas, Juan C. Calderón
- Endocrinol Metab. 2021;36(5):1055-1068. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1104
- 5,125 View
- 137 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
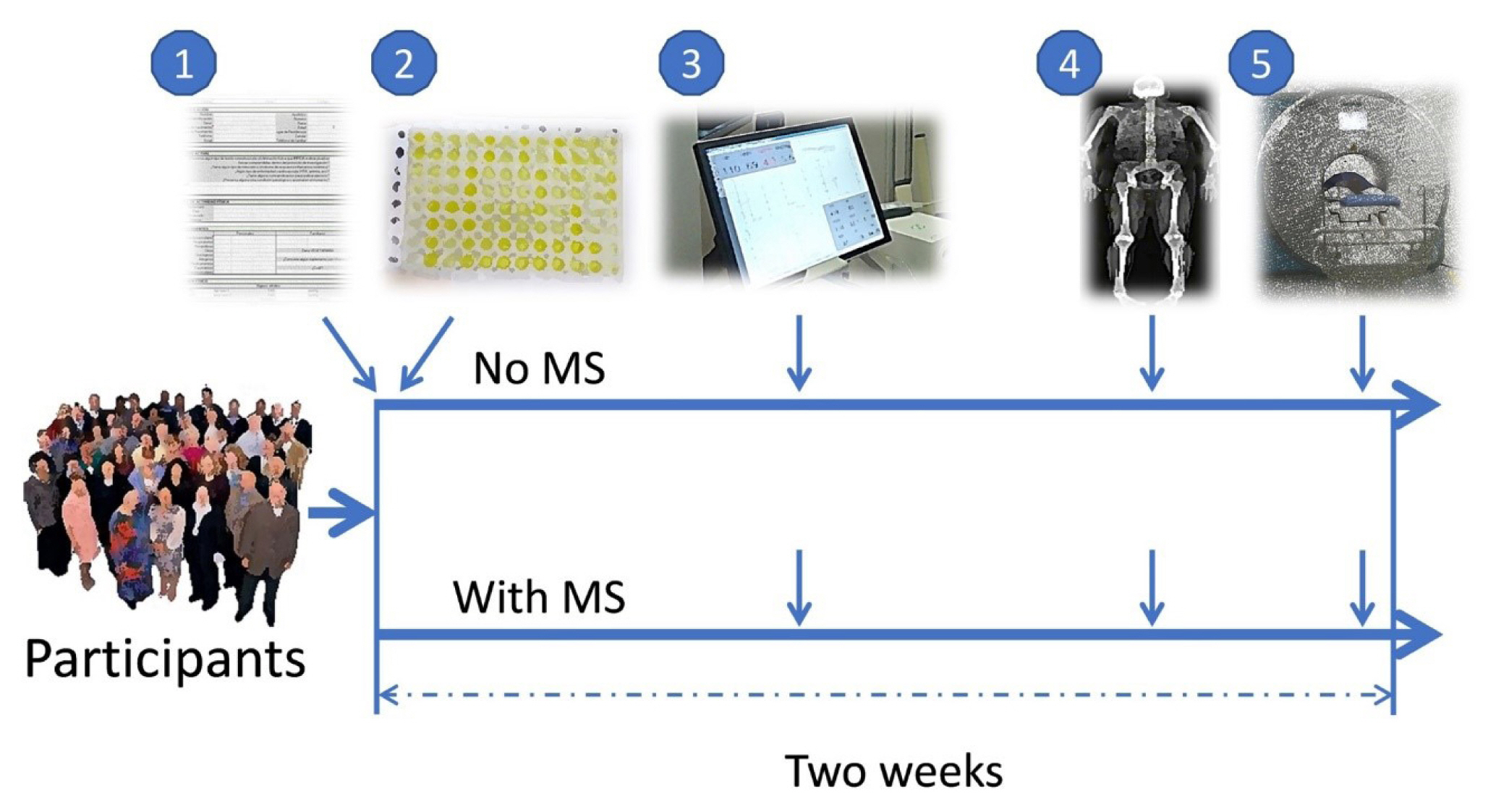
We studied whether musclin function in humans is related to glycemic control, body composition, and cardiorespiratory capacity.
Methods
A cross-sectional study was performed in sedentary adults with or without metabolic syndrome (MS). Serum musclin was measured by enzyme-linked immunosorbent assay. Insulin resistance (IR) was evaluated by the homeostatic model assessment (HOMA-IR). Body composition was determined by dual-energy X-ray absorptiometry and muscle composition by measuring carnosine in the thigh, a surrogate of fiber types, through proton magnetic resonance spectroscopy. Cardiorespiratory capacity was assessed through direct ergospirometry.
Results
The control (n=29) and MS (n=61) groups were comparable in age (51.5±6.5 years old vs. 50.7±6.1 years old), sex (72.4% vs. 70.5% women), total lean mass (58.5%±7.4% vs. 57.3%±6.8%), and peak oxygen consumption (VOpeak) (31.0±5.8 mL O2./kg.min vs. 29.2±6.3 mL O2/kg.min). Individuals with MS had higher body mass index (BMI) (30.6±4.0 kg/m2 vs. 27.4± 3.6 kg/m2), HOMA-IR (3.5 [95% confidence interval, CI, 2.9 to 4.6] vs. 1.7 [95% CI, 1.1 to 2.0]), and musclin (206.7 pg/mL [95% CI, 122.7 to 387.8] vs. 111.1 pg/mL [95% CI, 63.2 to 218.5]) values than controls (P˂0.05). Musclin showed a significant relationship with HOMA-IR (β=0.23; 95% CI, 0.12 to 0.33; P˂0.01), but not with VOpeak, in multiple linear regression models adjusted for age, sex, fat mass, lean mass, and physical activity. Musclin was significantly associated with insulin, glycemia, visceral fat, and regional muscle mass, but not with BMI, VCO2peak, maximum heart rate, maximum time of work, or carnosine.
Conclusion
In humans, musclin positively correlates with insulinemia, IR, and a body composition profile with high visceral adiposity and lean mass, but low body fat percentage. Musclin is not related to BMI or cardiorespiratory capacity. -
Citations
Citations to this article as recorded by- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation
Wonjun Cho, Heeseung Oh, Sung Woo Choi, A. M. Abd El-Aty, Fatma Yeşilyurt, Ji Hoon Jeong, Tae Woo Jung
Inflammation.2024; 47(1): 1. CrossRef - Glucose restriction enhances oxidative fiber formation: A multi-omic signal network involving AMPK and CaMK2
Kaiyi Zhang, Ning Xie, Huaqiong Ye, Jiakun Miao, Boce Xia, Yu Yang, Huanqi Peng, Shuang Xu, Tianwen Wu, Cong Tao, Jinxue Ruan, Yanfang Wang, Shulin Yang
iScience.2024; 27(1): 108590. CrossRef - Myokines: metabolic regulation in obesity and type 2 diabetes
Zhi-Tian Chen, Zhi-Xuan Weng, Jiandie D Lin, Zhuo-Xian Meng
Life Metabolism.2024;[Epub] CrossRef - Epidemiological, mechanistic, and practical bases for assessment of cardiorespiratory fitness and muscle status in adults in healthcare settings
Jaime A. Gallo-Villegas, Juan C. Calderón
European Journal of Applied Physiology.2023; 123(5): 945. CrossRef - Serum Levels of Myonectin Are Lower in Adults with Metabolic Syndrome and Are Negatively Correlated with Android Fat Mass
Jorge L. Petro, María Carolina Fragozo-Ramos, Andrés F. Milán, Juan C. Aristizabal, Jaime A. Gallo-Villegas, Juan C. Calderón
International Journal of Molecular Sciences.2023; 24(8): 6874. CrossRef - The correlation of serum musclin with diabetic nephropathy
Jie Zhang, Jing Shi, Zengguang Cheng, Wenchao Hu
Cytokine.2023; 167: 156211. CrossRef - Efficacy of high-intensity interval- or continuous aerobic-training on insulin resistance and muscle function in adults with metabolic syndrome: a clinical trial
Jaime Gallo-Villegas, Leonardo A. Castro-Valencia, Laura Pérez, Daniel Restrepo, Oscar Guerrero, Sergio Cardona, Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis H. Valbuena, Miguel Peña, Andrés F. Milán, Maria C. Trillos-Almanza, Sergio Granados, Juan C.
European Journal of Applied Physiology.2022; 122(2): 331. CrossRef - Reactive Oxygen and Nitrogen Species (RONS) and Cytokines—Myokines Involved in Glucose Uptake and Insulin Resistance in Skeletal Muscle
Paola Llanos, Jesus Palomero
Cells.2022; 11(24): 4008. CrossRef
- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation

- Diabetes, Obesity and Metabolism
- Role of TRPV4 Channel in Human White Adipocytes Metabolic Activity
- Julio C. Sánchez, Aníbal Valencia-Vásquez, Andrés M. García
- Endocrinol Metab. 2021;36(5):997-1006. Published online October 14, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1167

- 3,685 View
- 122 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Intracellular calcium (Ca2+) homeostasis plays an essential role in adipocyte metabolism and its alteration is associated with obesity and related disorders. Transient receptor potential vanilloid 4 (TRPV4) channels are an important Ca2+ pathway in adipocytes and their activity is regulated by metabolic mediators such as insulin. In this study, we evaluated the role of TRPV4 channels in metabolic activity and adipokine secretion in human white adipocytes.
Methods
Human white adipocytes were freshly cultured and the effects of the activation and inhibition of TRPV4 channels on lipolysis, glucose uptake, lactate production, and leptin and adiponectin secretion were evaluated.
Results
Under basal and isoproterenol-stimulated conditions, TRPV4 activation by GSK1016709A decreased lipolysis whereas HC067047, an antagonist, increased lipolysis. The activation of TRPV4 resulted in increased glucose uptake and lactate production under both basal conditions and insulin-stimulated conditions; in contrast HC067047 decreased both parameters. Leptin production was increased, and adiponectin production was diminished by TRPV4 activation and its inhibition had the opposite effect.
Conclusion
Our results suggested that TRPV4 channels are metabolic mediators involved in proadipogenic processes and glucose metabolism in adipocyte biology. TRPV4 channels could be a potential pharmacological target to treat metabolic disorders. -
Citations
Citations to this article as recorded by- Obesity, bone marrow adiposity, and leukemia: Time to act
Vijay Kumar, John H. Stewart
Obesity Reviews.2024;[Epub] CrossRef - TRP channels associated with macrophages as targets for the treatment of obese asthma
Wenzhao Zhu, Dinxi Bai, Wenting Ji, Jing Gao
Lipids in Health and Disease.2024;[Epub] CrossRef - Multidisciplinary Advances Address the Challenges in Developing Drugs against Transient Receptor Potential Channels to Treat Metabolic Disorders
Yibing Wang
ChemMedChem.2023;[Epub] CrossRef - Ion channels regulate energy homeostasis and the progression of metabolic disorders: Novel mechanisms and pharmacology of their modulators
Wenyi Wu, Jianan Zheng, Ru Wang, Yibing Wang
Biochemical Pharmacology.2023; 218: 115863. CrossRef - Potential lipolytic regulators derived from natural products as effective approaches to treat obesity
Xi-Ding Yang, Xing-Cheng Ge, Si-Yi Jiang, Yong-Yu Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Adipokines: Deciphering the cardiovascular signature of adipose tissue
Joseph C. Galley, Shubhnita Singh, Wanessa M.C. Awata, Juliano V. Alves, Thiago Bruder-Nascimento
Biochemical Pharmacology.2022; 206: 115324. CrossRef
- Obesity, bone marrow adiposity, and leukemia: Time to act

- Obesity and Metabolism
- Role of PCSK9 Inhibitors in Patients with Familial Hypercholesterolemia
- Brian Tomlinson, Nivritti Gajanan Patil, Manson Fok, Christopher Wai Kei Lam
- Endocrinol Metab. 2021;36(2):279-295. Published online April 19, 2021
- DOI: https://doi.org/10.3803/EnM.2021.964
- 6,579 View
- 297 Download
- 14 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
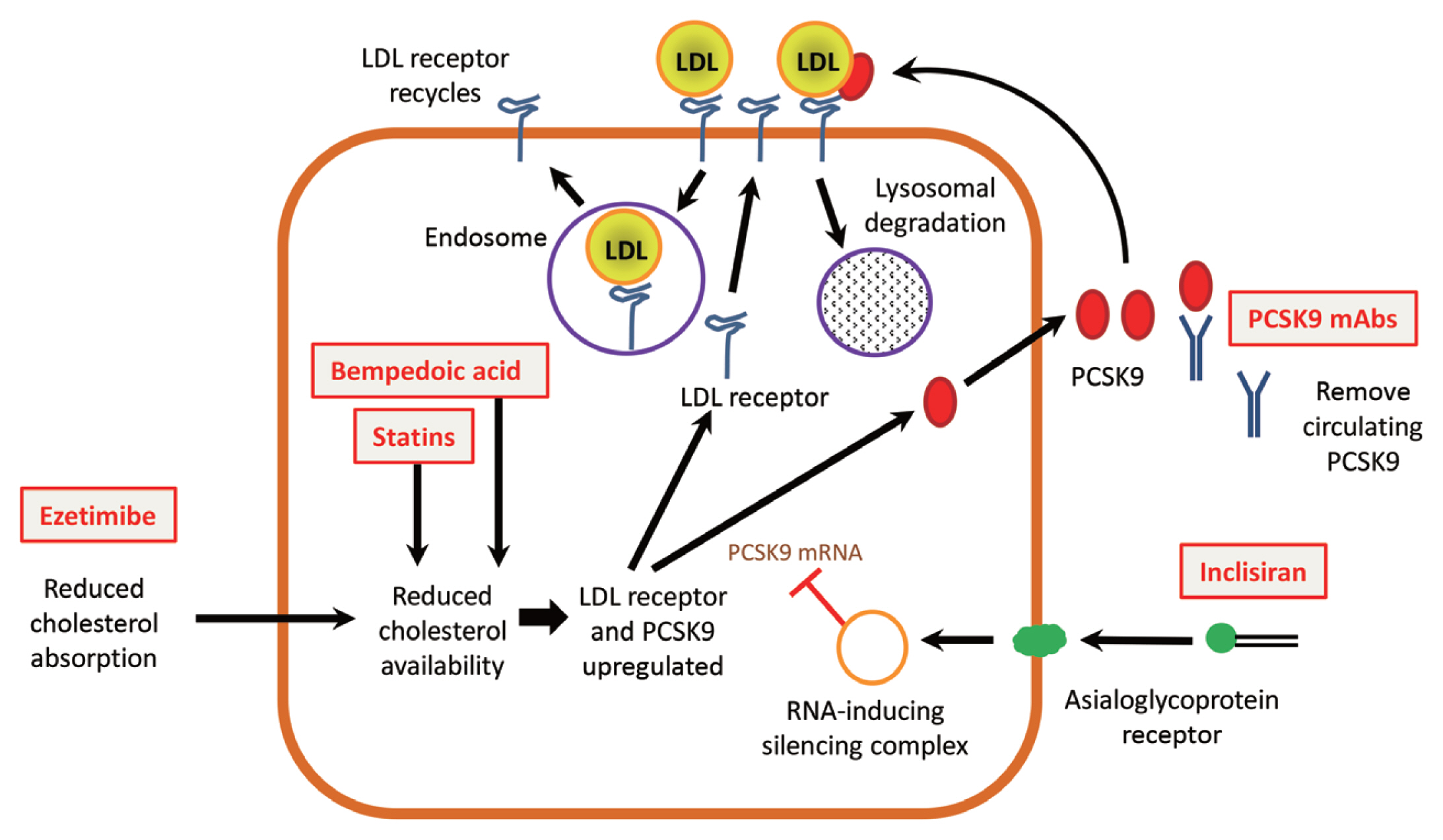
ePub - Patients with familial hypercholesterolemia (FH) are at high or very high risk for cardiovascular disease. Those with heterozygous FH (HeFH) often do not reach low-density lipoprotein cholesterol (LDL-C) targets with statin and ezetimibe therapy, and those with homozygous FH (HoFH) usually require additional lipid-modifying therapies. Drugs that inhibit proprotein convertase subtilisin/kexin type 9 (PCSK9) offer a novel approach to reduce LDL-C. The monoclonal antibodies, alirocumab and evolocumab, given by subcutaneous injection every 2 or 4 weeks produce reductions in LDL-C of 50% to 60% in patients with HeFH, allowing many of them to achieve their LDL-C goals. Patients with HoFH show a reduced and more variable LDL-C response, which appears to depend on residual LDL receptor activity, and those with receptor-negative mutations may show no response. Inclisiran is a long-acting small interfering RNA therapeutic agent that inhibits the synthesis of PCSK9. Subcutaneous doses of 300 mg can reduce LDL-C by more than 50% for at least 6 months and the responses in HeFH and HoFH patients are similar to those achieved with monoclonal antibodies. These PCSK9 inhibitors are generally well tolerated and they provide a new opportunity for effective treatment for the majority of patients with FH.
-
Citations
Citations to this article as recorded by- Phenotypic homozygous familial hypercholesterolemia successfully treated with proprotein convertase subtilisin/kexin type 9 inhibitors
Ryosuke Tani, Keiji Matsunaga, Yuta Toda, Tomoko Inoue, Hai Ying Fu, Tetsuo Minamino
Clinical Case Reports.2024;[Epub] CrossRef - Targeting Lipoprotein(a): Can RNA Therapeutics Provide the Next Step in the Prevention of Cardiovascular Disease?
Henriette Thau, Sebastian Neuber, Maximilian Y. Emmert, Timo Z. Nazari-Shafti
Cardiology and Therapy.2024; 13(1): 39. CrossRef - Technologies of gene editing and related clinical trials for the treatment of genetic and acquired diseases: a systematic review
Wessam Sharaf-Eldin
Egyptian Journal of Medical Human Genetics.2024;[Epub] CrossRef - Qualitative and Quantitative Effects of PCSK9 Inhibitors in familial Hypercholesterolemia: a Synthetic Review
Aamina Shakir, Kyle Barron, Kalgi Modi
Current Problems in Cardiology.2023; 48(4): 101550. CrossRef - Inhibition of PCSK9 Improves the Development of Pulmonary Arterial Hypertension Via Down-Regulating Notch3 Expression
Peng Ye, Xiao-Min Jiang, Wei-Chun Qian, Juan Zhang
Cardiovascular Drugs and Therapy.2023;[Epub] CrossRef - Barriers and shortcomings in access to cardiovascular management and prevention for familial hypercholesterolemia during the COVID‐19 pandemic
Helen Huang, Keith S. K. Leung, Tulika Garg, Adele Mazzoleni, Goshen D. Miteu, Farida Zakariya, Wireko A. Awuah, Elaine T. S. Yin, Faaraea Haroon, Zarish Hussain, Narjiss Aji, Vikash Jaiswal, Gary Tse
Clinical Cardiology.2023; 46(8): 831. CrossRef - Familial Hypercholesterolemia in Children. The Current State of the Problem
Dinara I. Sadykova, Karina R. Salakhova, Liliya F. Galimova, Eugeniya S. Slastnikova, Chulpan D. Khaliullina
Current Pediatrics.2023; 22(3): 231. CrossRef - Long-term safety and effectiveness of alirocumab and evolocumab in familial hypercholesterolemia (FH) in Belgium
Marc Snel, Olivier S. Descamps
Acta Cardiologica.2023; : 1. CrossRef - PCSK9 inhibitors revisited: Effectiveness and safety of PCSK9 inhibitors in a real-life Spanish cohort
Juan Vicente-Valor, Xandra García-González, Sara Ibáñez-García, María Esther Durán-García, Ana de Lorenzo-Pinto, Carmen Rodríguez-González, Irene Méndez-Fernández, Juan Carlos Percovich-Hualpa, Ana Herranz-Alonso, María Sanjurjo-Sáez
Biomedicine & Pharmacotherapy.2022; 146: 112519. CrossRef - Development of small-molecule PCSK9 inhibitors for the treatment of hypercholesterolemia
Shakir Ahamad, Shintu Mathew, Waqas A. Khan, Kishor Mohanan
Drug Discovery Today.2022; 27(5): 1332. CrossRef - The biological relevance of PCSK9: when less is better…
Majambu Mbikay, Michel Chrétien
Biochemistry and Cell Biology.2022; 100(3): 189. CrossRef - Fenofibrate add-on to statin treatment is associated with low all-cause death and cardiovascular disease in the general population with high triglyceride levels
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Metabolism.2022; 137: 155327. CrossRef - Homozygous Familial Hypercholesterolemia
Lisa Young, Emily E. Brown, Seth S. Martin
JACC: Case Reports.2022; 4(23): 101666. CrossRef - Familial Hypercholesterolemia and Its Current Diagnostics and Treatment Possibilities: A Literature Analysis
Kristina Zubielienė, Gintarė Valterytė, Neda Jonaitienė, Diana Žaliaduonytė, Vytautas Zabiela
Medicina.2022; 58(11): 1665. CrossRef - Efficacy and Safety of Alirocumab in Children and Adolescents With Homozygous Familial Hypercholesterolemia: Phase 3, Multinational Open-Label Study
Eric Bruckert, Sonia Caprio, Albert Wiegman, Min-Ji Charng, Cézar A. Zárate-Morales, Marie T. Baccara-Dinet, Garen Manvelian, Anne Ourliac, Michel Scemama, Stephen R. Daniels
Arteriosclerosis, Thrombosis, and Vascular Biology.2022; 42(12): 1447. CrossRef
- Phenotypic homozygous familial hypercholesterolemia successfully treated with proprotein convertase subtilisin/kexin type 9 inhibitors

- Clinical Study
- Efficacy and Safety of the Novel Dipeptidyl Peptidase-4 Inhibitor Gemigliptin in the Management of Type 2 Diabetes: A Meta-Analysis
- Deep Dutta, Anshita Agarwal, Indira Maisnam, Rajiv Singla, Deepak Khandelwal, Meha Sharma
- Endocrinol Metab. 2021;36(2):374-387. Published online April 6, 2021
- DOI: https://doi.org/10.3803/EnM.2020.818
- 6,453 View
- 226 Download
- 17 Web of Science
- 26 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
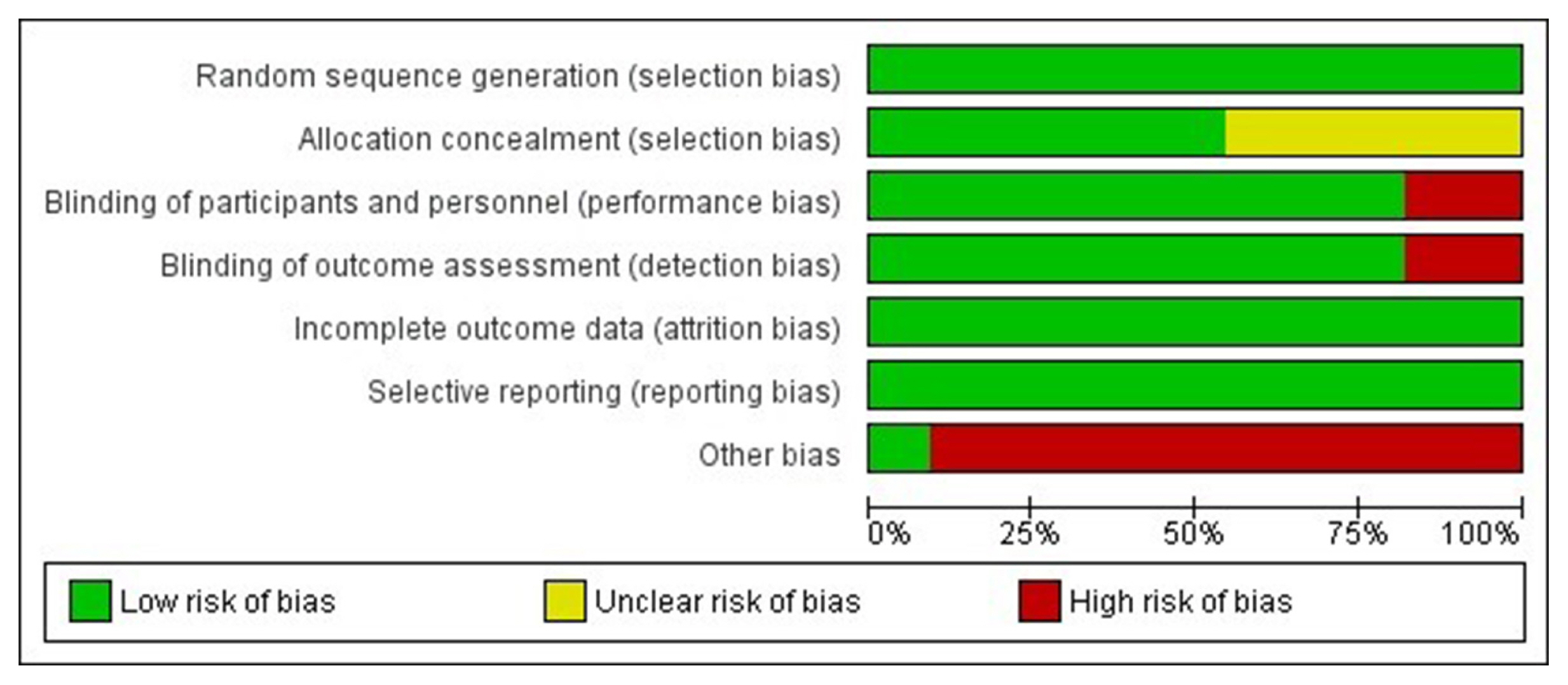
No meta-analysis has holistically analysed and summarised the efficacy and safety of gemigliptin in type 2 diabetes. The meta-analysis addresses this knowledge gap.
Methods
Electronic databases were searched for randomised controlled trials (RCTs) involving diabetes patients receiving gemigliptin in the intervention arm and placebo/active comparator in the control arm. The primary outcome was change in haemoglobin A1c (HbA1c). The secondary outcomes were alterations in glucose, glycaemic targets, lipids, insulin resistance, and adverse events.
Results
Data from 10 RCTs involving 1,792 patients were analysed. Four had an active control group (ACG), with metformin/dapagliflozin/sitagliptin/glimepiride as the active comparator; six had a passive control group (PCG), with placebo/rosuvastatin as controls. HbA1c reduction by gemigliptin at 24 weeks was comparable to ACG (mean difference [MD], 0.09%; 95% confidence interval [CI], –0.06 to 0.23; P=0.24; I2=0%; moderate certainty of evidence [MCE]), but superior to PCG (MD, –0.91%; 95% CI, –1.18 to –0.63); P<0.01; I2=89%; high certainty of evidence [HCE]). Gemigliptin was superior to PCG regarding achieving HbA1c <7% (12 weeks: odds ratio [OR], 5.91; 95% CI, 1.34 to 26.08; P=0.02; I2=74%; 24 weeks: OR, 4.48; 95% CI, 2.09 to 9.60; P<0.01; I2=69%; HCE). Gemigliptin was comparable to ACG regarding achieving HbA1c <7% after 24 weeks (OR, 0.92; 95% CI, 0.52 to 1.63; P=0.77; I2=66%; MCE). Adverse events were similar between the gemigliptin and control groups (risk ratio [RR], 1.06; 95% CI, 0.82 to 1.36; P=0.66; I2=35%; HCE). The gemigliptin group did not have increased hypoglycaemia (RR, 1.19; 95% CI, 0.62 to 2.28; P=0.61; I2=19%; HCE).
Conclusion
Gemigliptin has good glycaemic efficacy and is well-tolerated over 6 months of use. -
Citations
Citations to this article as recorded by- Hyperprolactinemia Due to Prolactinoma has an Adverse Impact on Bone Health with Predominant Impact on Trabecular Bone: A Systematic Review and Meta-Analysis
Lakshmi Nagendra, Deep Dutta, Sunetra Mondal, Nitin Kapoor, Ameya Joshi, Saptarshi Bhattacharya
Journal of Clinical Densitometry.2024; 27(1): 101453. CrossRef - Impact of early initiation of ezetimibe in patients with acute coronary syndrome: A systematic review and meta-analysis
Kunal Mahajan, Lakshmi Nagendra, Anil Dhall, Deep Dutta
European Journal of Internal Medicine.2024;[Epub] CrossRef - Efficacy and safety of dorzagliatin, a novel glucokinase activators, in the treatment of T2DM: A meta-analysis of randomized controlled trials
Yuqian Wu, Kai Wang, Jingyang Su, Xin Liu
Medicine.2024; 103(8): e36916. CrossRef - Glucagon-Like Peptide-1 Receptor Agonists in Post-bariatric Surgery Patients: A Systematic Review and Meta-analysis
Deep Dutta, Lakshmi Nagendra, Ameya Joshi, Suryashri Krishnasamy, Meha Sharma, Naresh Parajuli
Obesity Surgery.2024; 34(5): 1653. CrossRef - Orforglipron, a novel non‐peptide oral daily glucagon‐like peptide‐1 receptor agonist as an anti‐obesity medicine: A systematic review and meta‐analysis
Deep Dutta, Lakshmi Nagendra, Beatrice Anne, Manoj Kumar, Meha Sharma, A. B. M. Kamrul‐Hasan
Obesity Science & Practice.2024;[Epub] CrossRef - Safety and tolerability of sodium-glucose cotransporter-2 inhibitors in children and young adults: a systematic review and meta-analysis
Lakshmi Nagendra, Deep Dutta, Harish Bukkasagar Girijashankar, Deepak Khandelwal, Tejal Lathia, Meha Sharma
Annals of Pediatric Endocrinology & Metabolism.2024; 29(2): 82. CrossRef - Efficacy and safety of novel dual glucokinase activator dorzagliatin in type-2 diabetes A meta-analysis
Deep Dutta, Deepak Khandelwal, Manoj Kumar, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102695. CrossRef - Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Effects of Initial Combinations of Gemigliptin Plus Metformin Compared with Glimepiride Plus Metformin on Gut Microbiota and Glucose Regulation in Obese Patients with Type 2 Diabetes: The INTESTINE Study
Soo Lim, Minji Sohn, Jose C. Florez, Michael A. Nauck, Jiyoung Ahn
Nutrients.2023; 15(1): 248. CrossRef - Systematic review and meta-analysis of teneligliptin for treatment of type 2 diabetes
R. Pelluri, S. Kongara, V. R. Nagasubramanian, S. Mahadevan, J. Chimakurthy
Journal of Endocrinological Investigation.2023; 46(5): 855. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Verapamil improves One-Year C-Peptide Levels in Recent Onset Type-1 Diabetes: A Meta-Analysis
Deep Dutta, Lakshmi Nagendra, Nishant Raizada, Saptarshi Bhattacharya, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(3): 192. CrossRef - Role of novel sodium glucose co-transporter-2 inhibitor enavogliflozin in type-2 diabetes: A systematic review and meta-analysis
Deep Dutta, B.G. Harish, Beatrice Anne, Lakshmi Nagendra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(8): 102816. CrossRef - Semaglutide and cancer: A systematic review and meta-analysis
Lakshmi Nagendra, Harish BG, Meha Sharma, Deep Dutta
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(9): 102834. CrossRef - Efficacy and Safety of Novel Thiazolidinedione Rivoglitazone in Type-2 Diabetes a Meta-Analysis
Deep Dutta, Jyoti Kadian, Indira Maisnam, Ashok Kumar, Saptarshi Bhattacharya, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(4): 286. CrossRef - Impact of early initiation of proprotein convertase subtilisin/kexin type 9 inhibitors in patients with acute coronary syndrome: A systematic review meta-analysis
Lakshmi Nagendra, Kunal Mahajan, Gunjan Gupta, Deep Dutta
Indian Heart Journal.2023; 75(6): 416. CrossRef - Optimal use of once weekly icodec insulin in type-2 diabetes: An updated meta-analysis of phase-2 and phase-3 randomized controlled trials
Deep Dutta, Lakshmi Nagendra, Sowrabha Bhat, Ritin Mohindra, Vineet Surana, Anoop Misra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(10): 102877. CrossRef - Impact of Enhanced External Counter-pulsation Therapy on Glycaemic Control in People With Prediabetes and Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
Lakshmi Nagendra, Deep Dutta, Meha Sharma, Harish Bg
touchREVIEWS in Endocrinology.2023; 19(2): 8. CrossRef - Role of Novel Glucagon-like Peptide-1 Receptor Analogue Polyethylene Glycol Loxenatide in Type 2 Diabetes: A Systematic Review and Meta-analysis
Deep Dutta, Subhankar Chatterjee, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(5): 377. CrossRef - Efficacy and Safety of Ultra-rapid Lispro Insulin in Managing Type-1 and Type-2 Diabetes: A Systematic Review and Meta-Analysis
Deep Dutta, Lakshmi Nagendra, Saptarshi Bhattacharya, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2023; 27(6): 467. CrossRef - Safety and efficacy of once weekly dipeptidyl-peptidase-4 inhibitor trelagliptin in type-2 diabetes: A meta-analysis
Deep Dutta, Ritin Mohindra, Vineet Surana, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(4): 102469. CrossRef - Efficacy and safety of hydroxychloroquine for managing glycemia in type-2 diabetes: A systematic review and meta-analysis
D Dutta, R Jindal, D Mehta, M Kumar, M Sharma
Journal of Postgraduate Medicine.2022; 68(2): 85. CrossRef - Gemigliptin exerts protective effects against doxorubicin-induced hepatotoxicity by inhibiting apoptosis via the regulation of fibroblast growth factor 21 expression
Kyeong-Min Lee, Yeo Jin Hwang, Gwon-Soo Jung
Biochemical and Biophysical Research Communications.2022; 626: 135. CrossRef - Reporting and methodological quality of systematic reviews of DPP-4 inhibitors for patients with type 2 diabetes mellitus: an evidence-based mapping
Zouxi Du, Tingting Lu, Mingdong Gao, Limin Tian
Acta Diabetologica.2022; 59(12): 1539. CrossRef - Ranirestat improves electrophysiologic but not clinical measures of diabetic polyneuropathy: A meta-analysis
Deep Dutta, Ritin Mohindra, Manoj Kumar, Ashok Kumar, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2022; 26(5): 399. CrossRef - Efficacy and safety of novel twincretin tirzepatide a dual GIP and GLP-1 receptor agonist in the management of type-2 diabetes: A Cochrane meta-analysis
Deep Dutta, Vineet Surana, Rajiv Singla, Sameer Aggarwal, Meha Sharma
Indian Journal of Endocrinology and Metabolism.2021; 25(6): 475. CrossRef
- Hyperprolactinemia Due to Prolactinoma has an Adverse Impact on Bone Health with Predominant Impact on Trabecular Bone: A Systematic Review and Meta-Analysis

- Miscellaneous
- Intraoperative Parathyroid Hormone Monitoring in the Surgical Management of Sporadic Primary Hyperparathyroidism
- Zahra F. Khan, John I. Lew
- Endocrinol Metab. 2019;34(4):327-339. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.327
- 5,470 View
- 122 Download
- 22 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Intraoperative parathyroid hormone monitoring (IPM) has been shown to be a useful adjunct during parathyroidectomy to ensure operative success at many specialized medical centers worldwide. Using the Miami or “>50% intraoperative PTH drop” criterion, IPM confirms the complete excision of all hyperfunctioning parathyroid tissue before the operation is finished, and helps guide the surgeon to identify additional hyperfunctioning parathyroid glands that may necessitate further extensive neck exploration when intraoperative parathyroid hormone (PTH) levels do not drop sufficiently. The intraoperative PTH assay is also used to differentiate parathyroid from non-parathyroid tissues during operations using fine needle aspiration samples and to lateralize the side of the neck harboring the hypersecreting parathyroid through differential jugular venous sampling when preoperative localization studies are negative or equivocal. The use of IPM underscores the recognition and understanding of sporadic primary hyperparathyroidism (SPHPT) as a disease of function rather than form, where the surgeon is better equipped to treat such patients with quantitative instead of qualitative information for durable long-term operative success. There has been a significant paradigm shift over the last 2 decades from conventional to focused parathyroidectomy guided by IPM. This approach has proven to be a safe and rapid operation requiring minimal dissection performed in an ambulatory setting for the treatment of SPHPT.
-
Citations
Citations to this article as recorded by- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy
Phillip Staibano, Kevin Um, Sheila Yu, Mohit Bhandari, Michael K. Gupta, Michael Au, JEM (Ted) Young, Han Zhang
Frontiers in Surgery.2024;[Epub] CrossRef - Primary Hyperparathyroidism
Saba Kurtom, Sally E. Carty
Surgical Clinics of North America.2024;[Epub] CrossRef - Characteristics, management and outcomes of primary hyperparathyroidism from 2009 to 2021: a single centre report from South Africa
Kamal Govind, Imran M. Paruk, Ayesha A. Motala
BMC Endocrine Disorders.2024;[Epub] CrossRef - Parathyroidectomy for primary hyperparathyroidism: A retrospective analysis of localization, surgical characteristics, and treatment outcomes
Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee, Jin Ho Sohn
Asian Journal of Surgery.2023; 46(2): 788. CrossRef - Magnitude of parathyroid hormone elevation in primary hyperparathyroidism: Does time of day matter?
C. Corbin Frye, Janessa Sullivan, Sai Anusha Sanka, Jingxia Liu, L. Michael Brunt, William Gillanders, Taylor C. Brown, T.K. Pandian
Surgery.2023; 173(3): 659. CrossRef - Analysis of intraoperative laboratory measurements and imaging techniques such as Tc-99 m-MIBI SPECT/CT, 18F-fluorocholine PET/CT and ultrasound in patients operated with prediagnosis of parathyroid adenoma
Nurullah Bilen, Mehmet Avni Gokalp, Latif Yilmaz, Alper Aytekin, Ilyas Baskonus
Irish Journal of Medical Science (1971 -).2023; 192(4): 1695. CrossRef - Intraoperative Parathyroid Hormone Monitoring Is of Limited Usefulness in Guiding Autotransplantation in Reoperative or Subtotal Parathyroidectomy for Primary Hyperparathyroidism
Bradley A. Richards, Robert A. Vierkant, Benzon M. Dy, Trenton R. Foster, Travis J. McKenzie, Melanie L. Lyden
The American Surgeon™.2023; 89(12): 5421. CrossRef - Does 18F-Fluorocholine PET/CT add value to positive parathyroid scintigraphy in the presurgical assessment of primary hyperparathyroidism?
Alessio Imperiale, Jacob Bani, Gianluca Bottoni, Adrien Latgé, Céline Heimburger, Ugo Catrambone, Michel Vix, Giorgio Treglia, Arnoldo Piccardo
Frontiers in Medicine.2023;[Epub] CrossRef - Intraoperative Identification of Thyroid and Parathyroid Tissues During Human Endocrine Surgery Using the MasSpec Pen
Rachel J. DeHoog, Mary E. King, Michael F. Keating, Jialing Zhang, Marta Sans, Clara L. Feider, Kyana Y. Garza, Alena Bensussan, Anna Krieger, John Q. Lin, Sunil Badal, Elizabeth Alore, Christopher Pirko, Kirtan Brahmbhatt, Wendong Yu, Raymon Grogan, Livi
JAMA Surgery.2023; 158(10): 1050. CrossRef - A Rare Case of Recurrent Parathyroid Adenomas After Initial Parathyroidectomy
Grant N Schalet, Luke Vincent, Carl Eguez, Gerardo Diaz, Mark S Shachner
Cureus.2023;[Epub] CrossRef - Surgical treatment of tertiary hyperparathyroidism: does one fit for all?
Claudio Casella, Claudio Guarneri, Manuela Campanile, Xavier Adhoute, Pier Paolo Gelera, Riccardo Morandi
Frontiers in Endocrinology.2023;[Epub] CrossRef - A >50% Intraoperative Parathyroid Hormone Decrease Into Normal Reference Range Predicts Complete Excision of Malignancy in Patients With Parathyroid Carcinoma
Valerie L. Armstrong, Tanaz M. Vaghaiwalla, Cima Saghira, Cheng-Bang Chen, Yujie Wang, Johan Anantharaj, Mehmet Ackin, John I. Lew
Journal of Surgical Research.2023;[Epub] CrossRef - Variation in parathyroid adenoma size in patients with sporadic, primary hyperparathyroidism: small gland size does not preclude single gland disease
Sophie Dream, Tina W. F. Yen, Kara Doffek, Douglas B. Evans, Tracy S. Wang
Langenbeck's Archives of Surgery.2022; 407(5): 2067. CrossRef - Role and Recent Trend of Intraoperative Parathyroid Hormone Monitoring During Parathyroidectomy in Patients With Primary Hyperparathyroidism
Dongbin Ahn, Ji Hye Kwak
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2022; 65(5): 253. CrossRef - Parathyroid Adenoma: Rare Cause of Acute Recurrent Pancreatitis
Shikha Mahajan, Alka Kumar, Vivek Aggarwal, Vikas Jain, Vipul Baweja, Ajay Ajmani, Diplomate CBNC, Fellow EBNM LNU
Annals of Pediatric Gastroenterology and Hepatology.2022; 2(3-4): 9. CrossRef - Long-term outcome of surgical techniques for sporadic primary hyperparathyroidism in a tertiary referral center in Belgium
Klaas Van Den Heede, Amélie Bonheure, Nele Brusselaers, Sam Van Slycke
Langenbeck's Archives of Surgery.2022; 407(7): 3045. CrossRef - Contribution of intraoperative parathyroid hormone monitoring to the surgical success in minimal invasive parathyroidectomy
Ismail Ethem Akgün, Mehmet Taner Ünlü, Nurcihan Aygun, Mehmet Kostek, Mehmet Uludag
Frontiers in Surgery.2022;[Epub] CrossRef - Surgery for primary hyperparathyroidism
Murilo Catafesta das Neves, Rodrigo Oliveira Santos, Monique Nakayama Ohe
Archives of Endocrinology and Metabolism.2022; 66(5): 678. CrossRef - Використання інтраопераційного моніторингу рівня паратиреоїдного гормону в мінімально інвазивній хірургії щитоподібної та паращитоподібних залоз
S.V. Chernyshov, A.V. Tymkiv, A.V. Vovkanych, I.I. Komisarenko
Endokrynologia.2022; 27(4): 311. CrossRef - Diagnostic Values of Intraoperative (1-84) Parathyroid Hormone Levels are Superior to Intact Parathyroid Hormone for Successful Parathyroidectomy in Patients With Chronic Kidney Disease
Fangyan Xu, Yaoyu Huang, Ming Zeng, Lina Zhang, Wenkai Ren, Hanyang Qian, Ying Cui, Guang Yang, Wenbin Zhou, Shui Wang, Hui Huang, Huimin Chen, Yujie Xiao, Xueyan Gao, Zhanhui Gao, Jing Wang, Cuiping Liu, Jing Zhang, Baiqiao Zhao, Anning Bian, Fan Li, Hui
Endocrine Practice.2021; 27(11): 1065. CrossRef - Delayed Calcium Normalization after Successful Parathyroidectomy in Primary Hyperparathyroidism
Iván Emilio de la Cruz Rodríguez, Elsy Sarahí García Montesinos, María Fernanda Rodríguez-Delgado, Guadalupe Vargas Ortega, Lourdes Balcázar Hernández, Victoria Mendoza Zubieta, Victor Hernández Avendaño, Baldomero González Virla, Micha�l R. Laurent
Case Reports in Endocrinology.2021; 2021: 1. CrossRef - Parathyroid Surgery
Aditya S. Shirali, Uriel Clemente-Gutierrez, Nancy D. Perrier
Neuroimaging Clinics of North America.2021; 31(3): 397. CrossRef - Focused parathyroidectomy without intraoperative parathyroid hormone measurement in primary hyperparathyroidism: Still a valid approach?
Shelby Holt
Surgery.2021; 170(6): 1860. CrossRef - Response to the Comment on “Risk Factors of Redo Surgery After Unilateral Focused Parathyroidectomy – Conclusions From a Comprehensive Nationwide Database of 13,247 Interventions Over 6 Years”
Robert Caiazzo, Camille Marciniak, Francois Pattou
Annals of Surgery.2021; 274(6): e861. CrossRef
- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy

- Effects of Interleukin-6 on mRNA Expression of Alkaline Phosphatase, Osteopontin, Decorin and a1(1)-collagen in Human Bone Marrow Stromal Cells.
- Chul Hee Kim, Dong Kwan Kim, Seung Il Park, Kwang Hyun Sohn, Ghi Su Kim
- J Korean Endocr Soc. 1996;11(2):156-162. Published online November 7, 2019
- 1,063 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Inter1eukin-6(IL-6) is known to be produced by osteoblastic cells and to have impartant role in regulation of bone remodelling, Most previous studies indicated that IL-6 bas a major role in stimulating osteoclastic resorption by increasing recruitment and proliferation of preosteoclasts. But its autocrine effect on osteoblastic cells has not been well established yet. Therefore, we studied the effects of IL-6 on messenger RNA (mRNA) expression of proteins that are characteristic of osteoblastic cells in human bone marrow stromal (osteoprogenitor) cells (hRMSC). Methods: The expression of mRNAs for alkaline phosphatase, al(1)-collagen, osteopontin and decorin were studied by northern blot analysis after 3 7 days' treatrnent with IL-6 in the concenttation range of 101,000 U/ml. Results: The mRNA levels for any of the osteoblastic proteins studied did not change significantly by IL-6 treatment up to the concentration of 1,000 U/ml. Conclusion: These results suggest that IL-6 does not have a significant role in differentiatian or activities of human bone rnarrow stromal.

- Clinical Effects of E. coli Derived Recombinant Human Growth Hormone (DA - 3001) in Patients with Growth Hormone Deficiency.
- Sei Won Yang, Jeh Hoon Shin, Duk Hi Kim, Byung Churl Lee, Hyung Ro Moon
- J Korean Endocr Soc. 1995;10(4):377-385. Published online November 7, 2019
- 1,299 View
- 31 Download
-
 Abstract
Abstract
 PDF
PDF - Recently, methionyl-hGH was produced in the E. coil K-12, W3110 by recombinant DNA technology in Korea. In this paper, the clinical efficacy and immunogenicity of this GH were studied in 43 patients with growth hormone deficency.The subjects of this study were aged 4.3-18.5 years and each patient received GH 0.5-0.71U/kg week subcutaneously, 6-7 times a week for 1 year. During treatment, height, body weight and bone age were checked. Blood count, urinalysis, blood chemistry and thyroid hormonal concentrations were checked before and every 3 months. The measurement of IGF-1 was performed and assay of antibody against hGH was performed before and every 6 months.The height velocities significantly increased from 3.7+-3.0 cm/year to 11.0+-4.2 cm/year and 9.9+-3.2 cm/year at 6 and 12 months after GH therapy, respectively. The Height SDS were significantly improved after GH therapy with increasing ratio of bone age to chronological age from 0.60+-0.19 at pretreatment to 0.68+-0.16 at 6 month, 0.69+-0.16 at 12 month of therapy. The plasma IGF-1 levels significantly increased during treatment. Three out of 35 patients(8.3%) showed antibody against hGH after 1 year of treatment. Thoughout study, we could not observe any remarkable side effect with GH treatment.These results indicate that this E. coli derived methionyl recombinant growth hormone is effective in improving the index of linear growth in the children with growth hormone deficiency without significant side effect.

- Clinical Study
- Effects of Maternal Iodine Status during Pregnancy and Lactation on Maternal Thyroid Function and Offspring Growth and Development: A Prospective Study Protocol for the Ideal Breast Milk Cohort
- Young Ah Lee, Sun Wook Cho, Ho Kyung Sung, Kyungsik Kim, Young Shin Song, Sin Je Moon, Jung Won Oh, Dal Lae Ju, Sooyeon Choi, Sang Hoon Song, Gi Jeong Cheon, Young Joo Park, Choong Ho Shin, Sue K. Park, Jong Kwan Jun, June-Key Chung
- Endocrinol Metab. 2018;33(3):395-402. Published online September 18, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.395
- 4,983 View
- 84 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Iodine is an intrinsic element of thyroid hormone, which is essential for childhood growth and development. The Ideal Breast Milk (IBM) cohort study aims to evaluate the effects of maternal iodine status during pregnancy and lactation on maternal thyroid function, offspring growth and development, and offspring thyroid function.
Methods The IBM cohort study recruited pregnant women from Seoul National University Hospital between June 2016 and August 2017, followed by enrollment of their offspring after delivery. For the maternal participants, iodine status is evaluated by urinary iodine concentration (UIC) and dietary records in the third trimester and at 3 to 4 weeks and 12 to 15 months postpartum. For the child participants, cord blood sampling and UIC measurements are performed at birth. At 3 to 4 weeks of age, UIC and breastmilk iodine concentrations are measured. At 12 to 15 months of age, growth and development are assessed and measurements of UIC, a thyroid function test, and ultrasonography are performed.
Results A total of 198 pregnant women in their third trimester were recruited. Their mean age was 35.1±3.5 years, and 78 (39.4%) of them were pregnant with twins. Thirty-three (16.7%) of them had a previous history of thyroid disease.
Conclusion Korea is an iodine-replete area. In particular, lactating women in Korea are commonly exposed to excess iodine due to the traditional practice of consuming brown seaweed soup postpartum. The study of the IBM cohort is expected to contribute to developing guidelines for optimal iodine nutrition in pregnant or lactating women.
-
Citations
Citations to this article as recorded by- High intakes of iodine among women during pregnancy and the postpartum period has no adverse effect on thyroid function
Dal Lae Ju, Sun Wook Cho, Chae Won Chung, Young Ah Lee, Gi Jeong Cheon, Young Joo Park, Choong Ho Shin, Jong Kwan Jun, June-Key Chung, Sue K. Park, YoonJu Song
European Journal of Nutrition.2023; 62(1): 239. CrossRef - Associations between maternal thyroid function in pregnancy and child neurodevelopmental outcomes at 20 months in the Seychelles Child Development Study, Nutrition Cohort 2 (SCDS NC2)
Anna M. Monaghan, Maria S. Mulhern, Emeir M. Mc Sorley, J.J. Strain, Theresa Winter, Edwin van Wijngaarden, Gary J. Myers, Philip W. Davidson, Conrad Shamlaye, Jude Gedeon, Alison J. Yeates
Journal of Nutritional Science.2021;[Epub] CrossRef
- High intakes of iodine among women during pregnancy and the postpartum period has no adverse effect on thyroid function

- Poorly Differentiated Thyroid Carcinoma: 10-Year Experience in a Southeast Asian Population
- Marc Gregory Yu, Jonathan Rivera, Cecilia Jimeno
- Endocrinol Metab. 2017;32(2):288-295. Published online June 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.288
- 4,454 View
- 60 Download
- 14 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background No previous studies have been published on poorly differentiated thyroid carcinoma (PDTC) in Southeast Asia.
Methods We included all adult PDTC patients diagnosed using the Turin criteria at the Philippine General Hospital from 2006 to 2015. The data collected included demographics, clinical presentation, histopathology, treatment, and outcomes. Tests of association were employed to compare these data with foreign studies on PDTC, as well as with local studies on well differentiated thyroid carcinoma (WDTC) and anaplastic thyroid carcinoma (ATC).
Results Eighteen PDTC cases were identified. The median age was 62 years old, with the majority being females. All patients had goiter on presentation, and most were stage IV at the time of diagnosis. In terms of PDTC subtype, insular and trabecular patterns were equally common. Extrathyroidal extension was documented in eight patients, while five patients each had nodal and distant metastasis. All but one patient underwent surgery; however, less than half received adjuvant radioiodine therapy. The 5-year survival rate was 83%. Three patients (16.7%) died at a median of 12 months after diagnosis. Nine (50%) are still alive with persistent and/or recurrent disease at a median of 39 months after diagnosis.
Conclusion The behavior of PDTC in this Southeast Asian population was found to be similar to patterns observed in other regions, and exhibited intermediate features between WDTC and ATC. Appropriate surgery provided excellent 5-year survival rates, but the role of adjuvant therapy remains unclear. Larger studies are needed to identify prognostic factors in this population.
-
Citations
Citations to this article as recorded by- Poorly differentiated thyroid carcinomas: conceptual controversy and clinical impact
Andrés Coca-Pelaz, Juan P. Rodrigo, Abbas Agaimy, Michelle D. Williams, Nabil F. Saba, Sandra Nuyts, Gregory W. Randolph, Fernando López, Vincent Vander Poorten, Luiz P. Kowalski, Francisco J. Civantos, Mark E. Zafereo, Antti A. Mäkitie, Oded Cohen, Iain
Virchows Archiv.2024;[Epub] CrossRef - Management of Poorly Differentiated Thyroid Cancer and Differentiated High-Grade Thyroid Carcinoma
Iram S. Alam, Kepal N. Patel
Surgical Clinics of North America.2024;[Epub] CrossRef - I-131 Avid Tumor Thrombus in a Case of Poorly Differentiated Thyroid Cancer
Sana Munir Gill, Aamna Hassan, Humayun Bashir, Waqas Shafiq
Molecular Imaging and Radionuclide Therapy.2023; 32(2): 178. CrossRef - Prognostic Impact of Focal Poorly Differentiated Areas in Follicular Differentiated Thyroid Cancer: Is It a Distinct Entity from Poorly Differentiated Thyroid Cancer?
Ramakanth Bhargav Panchangam, Pradeep Puthenveetil, Sabaretnam Mayilvaganan
Indian Journal of Surgical Oncology.2022; 13(1): 157. CrossRef - Newly proposed survival staging system for poorly differentiated thyroid cancer: a SEER-based study
W. Sun, Z. Wang, J. Xiang, Y. Qin, F. Zhang, H. Zhang
Journal of Endocrinological Investigation.2022; 46(5): 947. CrossRef - Clinicopathological Characteristics and Prognosis of Poorly Differentiated Thyroid Carcinoma Diagnosed According to the Turin Criteria
Jiapeng Huang, Wei Sun, Qingfu Zhang, Zhihong Wang, Wenwu Dong, Dalin Zhang, Chengzhou Lv, Liang Shao, Ping Zhang, Hao Zhang
Endocrine Practice.2021; 27(5): 401. CrossRef - Osteopontin Expression in Thyroid Cancer: Deciphering EMT-Related Molecular Mechanisms
Bruna Prunes Pena Baroni Viana, Amanda Vitória Pampolha Gomes, Etel Rodrigues Pereira Gimba, Luciana Bueno Ferreira
Biomedicines.2021; 9(10): 1372. CrossRef - Poorly differentiated thyroid carcinoma (PDTC) characteristics and the efficacy of radioactive iodine (RAI) therapy as an adjuvant treatment in a tertiary cancer care center
Shivakumar Thiagarajan, Aamir Yousuf, Ratan Shetty, Harsh Dhar, Yash Mathur, Deepa Nair, Sandeep Basu, Asawari Patil, Shubadha Kane, Sarbani Ghosh-Laskar, Devendra Chaukar
European Archives of Oto-Rhino-Laryngology.2020; 277(6): 1807. CrossRef - Major vessel invasion by thyroid cancer: a comprehensive review
Michael S. Xu, Jennifer Li, Sam M. Wiseman
Expert Review of Anticancer Therapy.2019; 19(2): 191. CrossRef - Poorly differentiated thyroid carcinoma and poorly differentiated area in differentiated thyroid carcinoma: is there any difference?
Raouef Ahmed Bichoo, Anjali Mishra, Niraj Kumari, Narendra Krishnani, Gyan Chand, Gaurav Agarwal, Amit Agarwal, Saroj Kanta Mishra
Langenbeck's Archives of Surgery.2019; 404(1): 45. CrossRef
- Poorly differentiated thyroid carcinomas: conceptual controversy and clinical impact

- Update on Familial Hypercholesterolemia: Diagnosis, Cardiovascular Risk, and Novel Therapeutics
- Sang-Hak Lee
- Endocrinol Metab. 2017;32(1):36-40. Published online January 19, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.36
- 4,065 View
- 57 Download
- 11 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader In recent studies, the reported prevalence of heterozygous familial hypercholesterolemia (FH) has been higher than in previous reports. Although cascade genetic screening is a good option for efficient identification of affected patients, diagnosis using only clinical criteria is more common in real clinical practice. Cardiovascular risk is much higher in FH patients due to longstanding low density lipoprotein cholesterol (LDL-C) burden and is also influenced by other risk factors. Although guidelines emphasize aggressive LDL-C reduction, the majority of patients cannot reach the LDL-C goal by conventional pharmacotherapy. Novel therapeutics such as proprotein convertase subtilisin/kexin type 9 inhibitors have shown strong lipid lowering efficacy and are expected to improve treatment results in FH patients.
-
Citations
Citations to this article as recorded by- Effectiveness and Safety of a Fixed-Dose Combination of Valsartan and Rosuvastatin (Rovatitan® Tablet) in Patients with Concomitant Hypertension and Hyperlipidemia: An Observational Study
Kwang Je Lee, Jae-Kean Ryu, Yun-Hyeong Cho, Won Yong Shin, Jeong Su Kim, Young Won Yoon, Ji Yong Jang, Won Ho Kim, Jong Wook Beom, Seok-Min Kang
Drug Design, Development and Therapy.2023; Volume 17: 1047. CrossRef - Role of PCSK9 Inhibitors in Patients with Familial Hypercholesterolemia
Brian Tomlinson, Nivritti Gajanan Patil, Manson Fok, Christopher Wai Kei Lam
Endocrinology and Metabolism.2021; 36(2): 279. CrossRef - Identification and Functional Characterization of a Low-Density Lipoprotein Receptor Gene Pathogenic Variant in Familial Hypercholesterolemia
Hong-Yan Shu, Wei Zhang, Cong-Cong Zheng, Man-Yun Gao, Yong-Cun Li, Yan-Gang Wang
Frontiers in Genetics.2021;[Epub] CrossRef - Gut Microbiota and Complications of Type-2 Diabetes
Camelia Oana Iatcu, Aimee Steen, Mihai Covasa
Nutrients.2021; 14(1): 166. CrossRef - LDLR Gene Mutation p.Asp360His and Familial Hypercholesterolemia in a Mexican Community
Teresita De Jesús Hernández Flores, Juan Ramón González García, Yoaly Josefina Sánchez López, Norma Alejandra Vázquez Cárdenas, Ana Gabriela Colima Fausto, Sergio Yair Rodríguez Preciado, María Teresa Magaña Torres
Archives of Medical Research.2020; 51(2): 153. CrossRef - A Rare Double Heterozygous Mutation in Low-Density Lipoprotein Receptor and Apolipoprotein B-100 Genes in a Severely Affected Familial Hypercholesterolaemia Patient
Lilla Juhász, István Balogh, László Madar, Beáta Kovács, Mariann Harangi
Cureus.2020;[Epub] CrossRef - Efficacy and Safety of a Fixed-Dose Combination of Candesartan and Rosuvastatin on Blood Pressure and Cholesterol in Patients With Hypertension and Hypercholesterolemia: A Multicenter, Randomized, Double-Blind, Parallel Phase III Clinical Study
Kyoung Im Cho, Bo Hyun Kim, Yong Hyun Park, Jeong-Cheon Ahn, Sang Hyun Kim, Wook Jin Chung, Weon Kim, Il Suk Sohn, Jin Ho Shin, Yong Jin Kim, Kiyuk Chang, Cheol Woong Yu, Soe Hee Ahn, Seok Yeon Kim, Jae Kean Ryu, Jong Young Lee, Bum Kee Hong, Taek Jong Ho
Clinical Therapeutics.2019; 41(8): 1508. CrossRef - Diagnosis and Treatment of Heterozygous Familial Hypercholesterolemia
Mary P. McGowan, Seyed Hamed Hosseini Dehkordi, Patrick M. Moriarty, P. Barton Duell
Journal of the American Heart Association.2019;[Epub] CrossRef - Autosomal recessive hypercholesterolemia: Case report
Zaneta Petrulioniene, Urte Gargalskaite, Violeta Mikstiene, Rimvydas Norvilas, Egle Skiauteryte, Algirdas Utkus
Journal of Clinical Lipidology.2019; 13(6): 887. CrossRef -
Q192R polymorphism in the
PON1
gene and familial hypercholesterolemia in a Saudi population
Khalid Khalaf Alharbi, May Salem Alnbaheen, Fawiziah Khalaf Alharbi, Rana M. Hasanato, Imran Ali Khan
Annals of Saudi Medicine.2017; 37(6): 425. CrossRef
- Effectiveness and Safety of a Fixed-Dose Combination of Valsartan and Rosuvastatin (Rovatitan® Tablet) in Patients with Concomitant Hypertension and Hyperlipidemia: An Observational Study


 KES
KES

 First
First Prev
Prev



