Search
- Page Path
- HOME > Search
- Thyroid
- Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
- Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
- Endocrinol Metab. 2023;38(6):729-738. Published online November 2, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1769
- 1,154 View
- 73 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study investigates the association between thyroid function and frailty in the old patients using representative data.
Methods
The study was conducted using data from the Korea National Health and Nutrition Examination Survey conducted from 2013 to 2015. The study population included 2,416 participants aged 50 years and older with available thyroid function test data. Frailty assessment was performed using the Fried frailty phenotype. The prevalence of frailty was analyzed across different thyroid diseases and thyroid function parameters.
Results
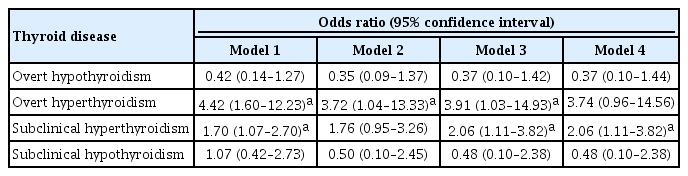
The significant association between thyroid dysfunction and frailty was observed in overt hyperthyroidism and subclinical hyperthyroidism. After adjusting for various factors, the association between thyroid dysfunction and frailty remained significant. On the other hand, overt hypothyroidism did not show a significant association with frailty in the adjusted analysis. For individuals with overt hyperthyroidism and subclinical hyperthyroidism, higher levels of free thyroxine (FT4) were significantly associated with an increased risk of frailty (aOR >999; 95% CI, >999 to 999). Among individuals with overt hypothyroidism, lower level of FT4 levels and high thyrotropin (TSH) levels showed a significant association with frailty risk (FT4: aOR, <0.01; TSH: aOR, 999). In participants with subclinical hypothyroidism, there were no significant associations between parameters for thyroid and frailty risk.
Conclusion
These findings suggest that thyroid dysfunction, particularly overt hyperthyroidism and subclinical hyperthyroidism, may be associated with an increased risk of frailty in the old patients. -
Citations
Citations to this article as recorded by- Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China
Heng Wan, Genfeng Yu, Yajun He, Siyang Liu, Xingying Chen, Yuqi Jiang, Hualin Duan, Xu Lin, Lan Liu, Jie Shen
Annals of Medicine.2024;[Epub] CrossRef
- Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China

- Thyroid
- Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study
- Kyungsik Kim, Sun Wook Cho, Young Joo Park, Kyu Eun Lee, Dong-Wook Lee, Sue K. Park
- Endocrinol Metab. 2021;36(4):790-799. Published online August 11, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1034
- 4,793 View
- 237 Download
- 9 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to assess the effects of iodine intake, thyroid function, and their combined effect on the risk of papillary thyroid cancer (PTC) and papillary thyroid microcarcinoma (PTMC).
Methods
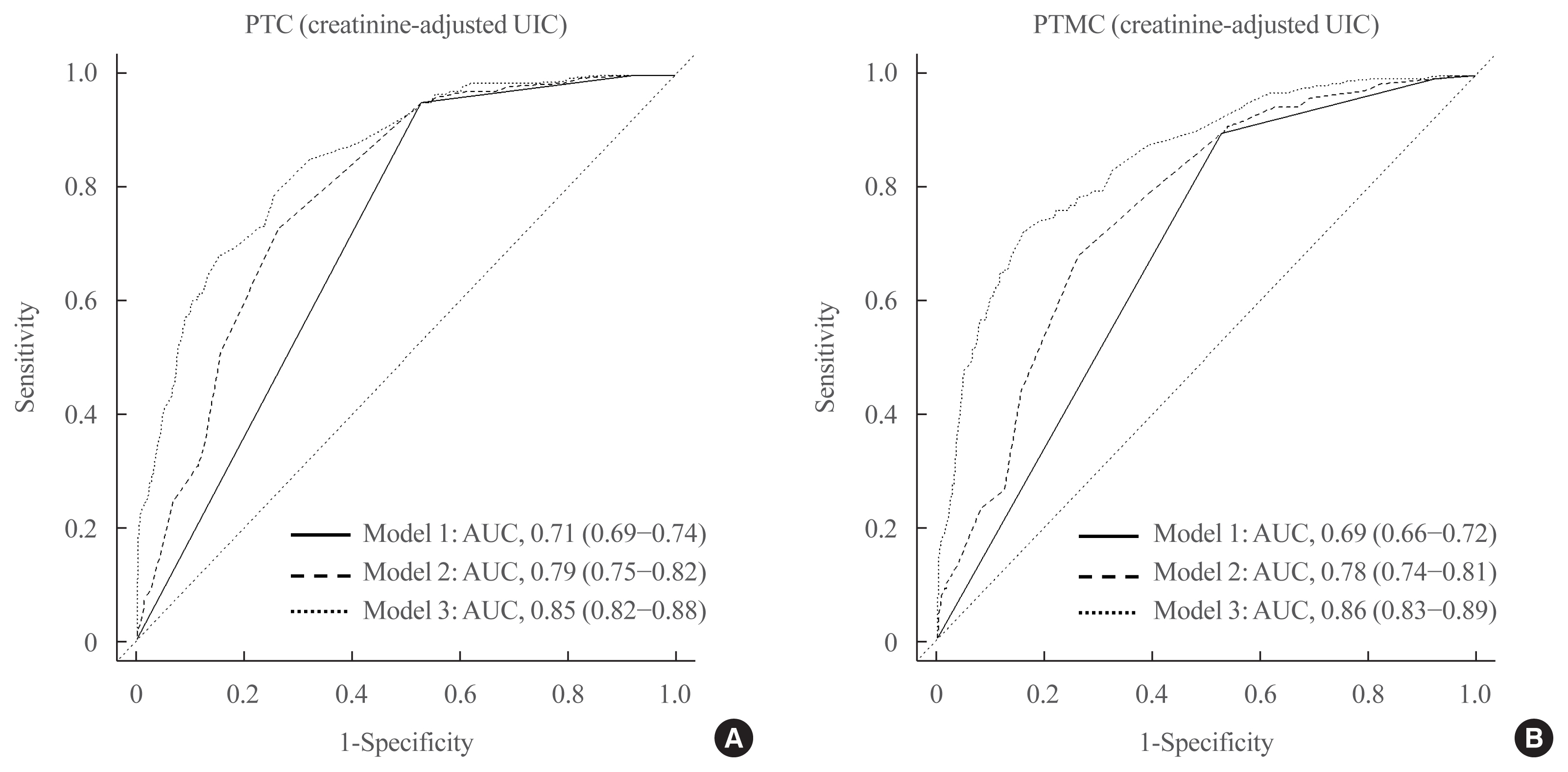
A case-control study was conducted including 500 community-based controls who had undergone a health check-up, and 446 overall PTC cases (209 PTC and 237 PTMC) from the Thyroid Cancer Longitudinal Study. Urinary iodine concentration (UIC), was used as an indicator of iodine intake, and serum for thyroid function. The risk of PTC and PTMC was estimated using unconditional logistic regression.
Results
Excessive iodine intake (UIC ≥220 μg/gCr) was associated with both PTC (odds ratio [OR], 18.13 95% confidence interval [CI], 8.87 to 37.04) and PTMC (OR, 8.02; 95% CI, 4.64 to 13.87), compared to adequate iodine intake (UIC, 85 to 219 μg/gCr). Free thyroxine (T4) levels ≥1.25 ng/dL were associated with PTC (OR, 1.97; 95% CI, 1.36 to 2.87) and PTMC (OR, 2.98; 95% CI, 2.01 to 4.41), compared to free T4 levels of 0.7 to 1.24 ng/dL. Individuals with excessive iodine intake and high free T4 levels had a greatly increased OR of PTC (OR, 43.48; 95% CI, 12.63 to 149.62), and PTMC (OR, 26.96; 95% CI, 10.26 to 70.89), compared to individuals with adequate iodine intake and low free T4 levels.
Conclusion
Excessive iodine intake using creatinine-adjusted UIC and high free T4 levels may have a synergistic effect on PTC and PTMC. Considering both iodine intake and thyroid function is important to assess PTC and PTMC risk. -
Citations
Citations to this article as recorded by- Association between urinary iodine concentration and the risk of papillary thyroid cancer by sex and age: a case–control study
Yerin Hwang, Hyun-Kyung Oh, Jae Hoon Chung, Sun Wook Kim, Jung-Han Kim, Jee Soo Kim, Myung-Hee Shin
Scientific Reports.2023;[Epub] CrossRef - Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma
Hengqiang Zhao, Jin Hu, Le Cui, Yiping Gong, Tao Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sex-specific Associations between Body Mass Index and Thyroid Cancer Incidence among Korean Adults
Kyoung-Nam Kim, Kyungsik Kim, Sangjun Lee, Sue K. Park
Cancer Epidemiology, Biomarkers & Prevention.2023; 32(9): 1227. CrossRef - Nomogram Model Based on Iodine Nutrition and Clinical Characteristics of Papillary Thyroid Carcinoma to Predict Lateral Lymph Node Metastasis
Junrong Wang, Yuzhang Gao, Yuxuan Zong, Weitong Gao, Xueying Wang, Ji Sun, Susheng Miao
Cancer Control.2023;[Epub] CrossRef - Content of Copper, Iron, Iodine, Rubidium, Strontium and Zinc in Thyroid Malignant Nodules and Thyroid Tissue adjacent to Nodules
Vladimir Zaichick, Qiping Dong
Journal of Clinical and Diagnostic Pathology.2022; 1(4): 7. CrossRef - Distinguish Thyroid Malignant from Benign Alterations using Trace Element Contents in Nodular Tissue determined by Neutron Activation and Inductively Coupled Plasma Mass Spectrometry
Vladimir Zaichick
Journal of Clinical and Diagnostic Pathology.2022; 1(4): 18. CrossRef - Seaweed and Iodine Intakes and SLC5A5 rs77277498 in Relation to Thyroid Cancer
Tung Hoang, Eun Kyung Lee, Jeonghee Lee, Yul Hwangbo, Jeongseon Kim
Endocrinology and Metabolism.2022; 37(3): 513. CrossRef - Iodine nutrition and papillary thyroid cancer
Xueqi Zhang, Fan Zhang, Qiuxian Li, Chuyao Feng, Weiping Teng
Frontiers in Nutrition.2022;[Epub] CrossRef - The relationship between urinary iodine concentration and papillary thyroid cancer: A systematic review and meta-analysis
Xueqi Zhang, Fan Zhang, Qiuxian Li, Renaguli Aihaiti, Chuyao Feng, Deshi Chen, Xu Zhao, Weiping Teng
Frontiers in Endocrinology.2022;[Epub] CrossRef - Screening and validation of lymph node metastasis risk-factor genes in papillary thyroid carcinoma
Qiaoyue Zhang, Jing Li, Hengyan Shen, Xinyu Bai, Tao Zhang, Ping Liu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnosis of Thyroid Malignancy using Levels of Chemical Element Contents in Nodular Tissue
Vladimir Zaichick
Journal of Health Care and Research.2022; 3(1): 16. CrossRef - Associations of Habitual Mineral Intake with New-Onset Prediabetes/Diabetes after Acute Pancreatitis
Claire F. Norbitt, Wandia Kimita, Juyeon Ko, Sakina H. Bharmal, Maxim S. Petrov
Nutrients.2021; 13(11): 3978. CrossRef
- Association between urinary iodine concentration and the risk of papillary thyroid cancer by sex and age: a case–control study

- Thyroid
- Insights from a Prospective Follow-up of Thyroid Function and Autoimmunity among COVID-19 Survivors
- David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung, Karen Siu Ling Lam
- Endocrinol Metab. 2021;36(3):582-589. Published online June 8, 2021
- DOI: https://doi.org/10.3803/EnM.2021.983
- 10,972 View
- 267 Download
- 32 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The occurrence of Graves’ disease and Hashimoto thyroiditis after coronavirus disease 2019 (COVID-19) raised concerns that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may trigger thyroid autoimmunity. We aimed to address the current uncertainties regarding incident thyroid dysfunction and autoimmunity among COVID-19 survivors.
Methods
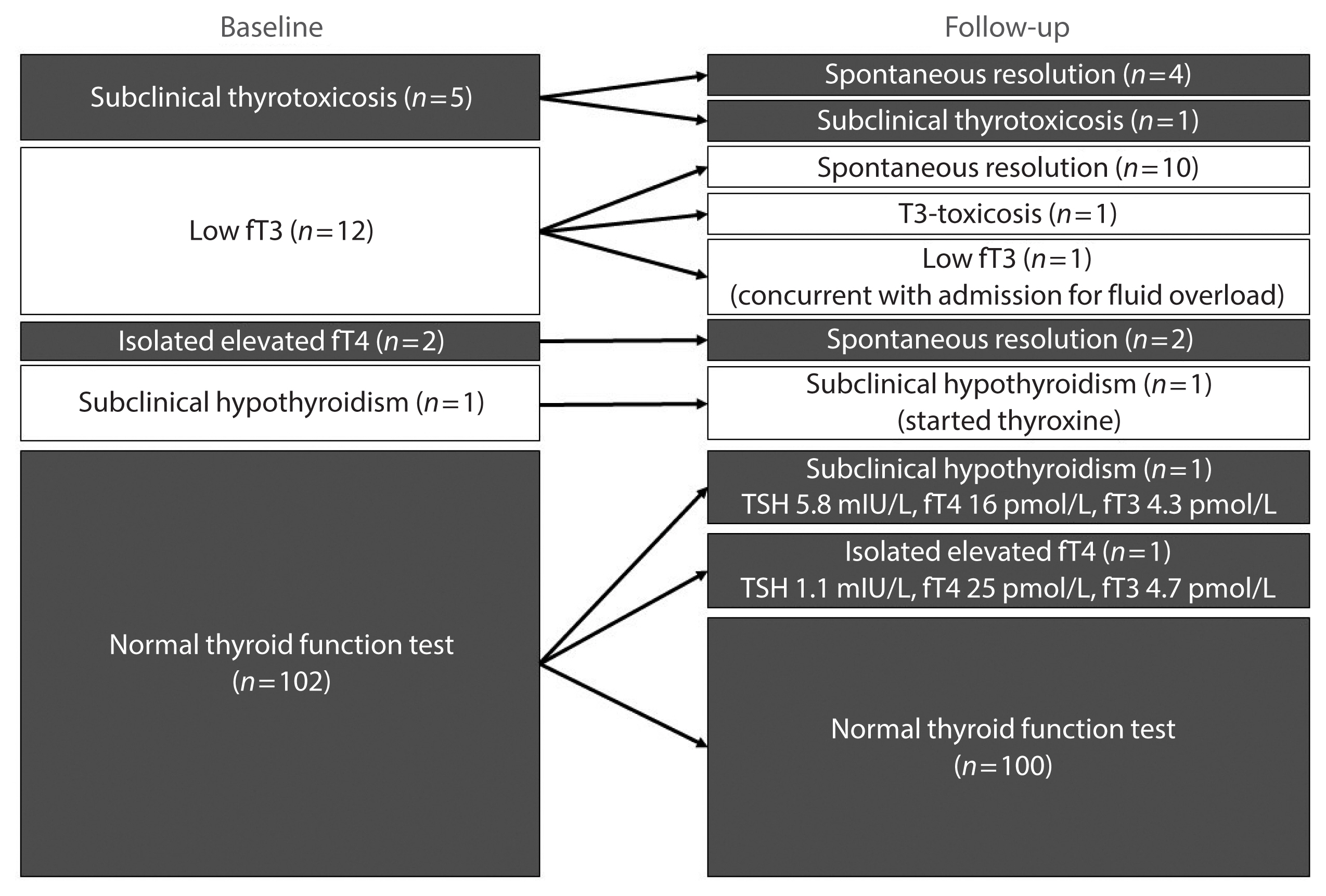
We included consecutive adult COVID-19 patients without known thyroid disorders, who were admitted to Queen Mary Hospital from July 21 to September 21, 2020 and had serum levels of thyroid-stimulating hormone, free thyroxine, free triiodothyronine (fT3), and anti-thyroid antibodies measured both on admission and at 3 months.
Results
In total, 122 patients were included. Among 20 patients with abnormal thyroid function tests (TFTs) on admission (mostly low fT3), 15 recovered. Among 102 patients with initial normal TFTs, two had new-onset abnormalities that could represent different phases of thyroiditis. Among 104 patients whose anti-thyroid antibody titers were reassessed, we observed increases in anti-thyroid peroxidase (TPO) (P<0.001) and anti-thyroglobulin (P<0.001), but not anti-thyroid stimulating hormone receptor titers (P=0.486). Of 82 patients with negative anti-TPO findings at baseline, 16 had a significant interval increase in anti-TPO titer by >12 U, and four became anti-TPO-positive. Worse baseline clinical severity (P=0.018), elevated C-reactive protein during hospitalization (P=0.033), and higher baseline anti-TPO titer (P=0.005) were associated with a significant increase in anti-TPO titer.
Conclusion
Most patients with thyroid dysfunction on admission recovered during convalescence. Abnormal TFTs suggestive of thyroiditis occurred during convalescence, but infrequently. Importantly, our novel observation of an increase in anti-thyroid antibody titers post-COVID-19 warrants further follow-up for incident thyroid dysfunction among COVID-19 survivors. -
Citations
Citations to this article as recorded by- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis
Sadra Ashrafi, Hossein Hatami, Razieh Bidhendi-Yarandi, Mohammad Hossein Panahi
BMC Endocrine Disorders.2024;[Epub] CrossRef - Does COVID-19 affect thyroid more than non-COVID-19 infections? A retrospective study
Yasemin Ucal, Muhittin Serdar, Hande Karpuzoğlu, Neval Yurttutan Uyar, Meltem Kilercik, Mustafa Serteser, Aysel Ozpinar
Turkish Journal of Biochemistry.2024;[Epub] CrossRef - Thyroiditis and COVID-19: focus on pediatric age. A narrative review
F. d’Aniello, M. E. Amodeo, A. Grossi, G. Ubertini
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - The most common persistent symptoms in patients with COVID-19 who were evaluated in the Internal Medicine polyclinic
Zeynep KOÇ, Seydahmet AKIN
The European Research Journal.2023; 9(1): 97. CrossRef - Clinical assessment of children with long COVID syndrome
Réka Garai, Péter Krivácsy, Vivien Herczeg, Fanni Kovács, Bálint Tél, Judit Kelemen, Anna Máthé, Eszter Zsáry, Johanna Takács, Dániel Sándor Veres, Attila J. Szabó
Pediatric Research.2023; 93(6): 1616. CrossRef - T Cell Receptor Sequences Amplified during Severe COVID-19 and Multisystem Inflammatory Syndrome in Children Mimic SARS-CoV-2, Its Bacterial Co-Infections and Host Autoantigens
Robert Root-Bernstein, Elizabeth Churchill, Shelby Oliverio
International Journal of Molecular Sciences.2023; 24(2): 1335. CrossRef - A Literature Review on SARS-CoV-2 and Other Viruses in Thyroid Disorders: Environmental Triggers or No-Guilty Bystanders?
Francesca Gorini, Cristina Vassalle
International Journal of Environmental Research and Public Health.2023; 20(3): 2389. CrossRef - Thyroid dysfunction as a long-term post-COVID-19 complication in mild-to-moderate COVID-19
Vesselina Yanachkova, Teodora Stankova, Radiana Staynova
Biotechnology & Biotechnological Equipment.2023; 37(1): 194. CrossRef - The Influence of SARS-CoV-2 Infection on the Thyroid Gland
Aleksandra Piekarska, Marta Góral, Marta Kozula, Aleksandra Jawiarczyk-Przybyłowska, Katarzyna Zawadzka, Marek Bolanowski
Biomedicines.2023; 11(2): 614. CrossRef - Thyroid Function Abnormalities and Outcomes in Hospitalized Patients
with COVID-19 Infection: A Cross-Sectional Study
Deepika Patel, Dukhabandhu Naik, Sadishkumar Kamalanathan, Kadhiravan Tamilarasu, Jayaprakash Sahoo, Ayan Roy, Chandhana Merugu, Varun Suryadevara
Hormone and Metabolic Research.2023; 55(03): 169. CrossRef - The Spectrum of Thyroid Function Tests and Autoantibodies During Hospitalization and After Six Months of Discharge in COVID-19 Patients: Does COVID-19 Trigger Autoimmunity?
Ziynet Alphan Uc, Pinar Yagcı, Zelal Adibelli, Cevdet Duran
Endocrine Research.2023; 48(2-3): 44. CrossRef - Increased prevalence of autoimmune thyroid disease after COVID-19: A single-center, prospective study
Alessandro Rossini, Sara Cassibba, Francesca Perticone, Simone Vasilij Benatti, Serena Venturelli, Greta Carioli, Arianna Ghirardi, Marco Rizzi, Tiziano Barbui, Roberto Trevisan, Silvia Ippolito
Frontiers in Endocrinology.2023;[Epub] CrossRef - A prospective follow-up of thyroid volume and thyroiditis features on ultrasonography among survivors of predominantly mild to moderate COVID-19
Man Him Matrix Fung, David Tak Wai Lui, Keith Wan Hang Chiu, Sherman Haynam Lee, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Chun Yiu Law, Kelvin Kai Wang To, Ching W
PeerJ.2023; 11: e15034. CrossRef - Study on Clinicopathological Features and Risk Factors of Patients with Multiple Primary Breast Cancers and Thyroid Disease
Jie Li, Yonghong Liu, Jian Jin, Qingfeng Shi, Yanting Ji, Bo Zhang, Pengfei Hu, Jinghua Pan
Mediators of Inflammation.2023; 2023: 1. CrossRef - Beyond Acute COVID-19: Investigating the Incidence of Subacute Thyroiditis in Long COVID-19 in Korea
Jeongmin Lee, Gi Hyeon Seo, Keeho Song
Endocrinology and Metabolism.2023; 38(4): 455. CrossRef - Thyroid Autoimmunity and SARS-CoV-2 Infection
Poupak Fallahi, Giusy Elia, Francesca Ragusa, Sabrina Rosaria Paparo, Armando Patrizio, Eugenia Balestri, Valeria Mazzi, Salvatore Benvenga, Gilda Varricchi, Laura Gragnani, Chiara Botrini, Enke Baldini, Marco Centanni, Clodoveo Ferri, Alessandro Antonell
Journal of Clinical Medicine.2023; 12(19): 6365. CrossRef - Autoimmune complications of COVID‐19
Niloufar Yazdanpanah, Nima Rezaei
Journal of Medical Virology.2022; 94(1): 54. CrossRef - The Independent Association of TSH and Free Triiodothyronine Levels With Lymphocyte Counts Among COVID-19 Patients
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Chloe Yu Yan Cheung, Carol Ho Yi Fong, Chun Yiu Law, Kelvin Kai Wang To, Ching Wan Lam, Kathryn Choon Beng Tan, Yu Cho Woo, Ivan Fan Ngai Hung,
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comment on Khunti et al. COVID-19, Hyperglycemia, and New-Onset Diabetes. Diabetes Care 2021;44:2645–2655
Carmine Gazzaruso, Adriana Coppola, Pietro Gallotti, Ileana Terruzzi, Tiziana Montalcini, Livio Luzi
Diabetes Care.2022; 45(2): e45. CrossRef - The potential impact of COVID-19 on thyroid gland volumes among COVID-19 survivors
Emre Urhan, Zuleyha Karaca, Canan Sehit Kara, Zeynep Ture Yuce, Kursad Unluhizarci
Endocrine.2022; 76(3): 635. CrossRef - Systematic review of COVID-19 and autoimmune thyroiditis
Esra Tutal, Resat Ozaras, Hakan Leblebicioglu
Travel Medicine and Infectious Disease.2022; 47: 102314. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Should we expect a wave of type 1 diabetes following SARS‐CoV‐2 pandemic?
Laura Montefusco, Andrea Mario Bolla, Paolo Fiorina
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - COVID-19 and Thyroid Function: A Bi-Directional Two-Sample Mendelian Randomization Study
Gloria Hoi-Yee Li, Ching-Man Tang, Ching-Lung Cheung
Thyroid.2022; 32(9): 1037. CrossRef - Development of a prediction score (ThyroCOVID) for identifying abnormal thyroid function in COVID-19 patients
D. T. W. Lui, C. H. Lee, W. S. Chow, A. C. H. Lee, A. R. Tam, C. Y. Y. Cheung, C. H. Y. Fong, S. T. M. Kwok, C. Y. Law, K. K. W. To, C. W. Lam, K. C. B. Tan, Y. C. Woo, I. F. N. Hung, K. S. L. Lam
Journal of Endocrinological Investigation.2022; 45(11): 2149. CrossRef - Symptomatic Bradycardia Manifesting as Acute Hypothyroidism Following COVID-19 Infection: A Case Report
Jaydip Desai, Arsh N Patel, Courtney L Evans, Molly Triggs, Fulton Defour
Cureus.2022;[Epub] CrossRef - Schilddrüse und SARS-CoV-2
Georg Zettinig
Journal für Klinische Endokrinologie und Stoffwechsel.2022; 15(3): 100. CrossRef - Thyroid diseases are associated with coronavirus disease 2019 infection
Yutian Tian, Junyu Zhao, Tingting Wang, Haipeng Wang, Jinming Yao, Song Wang, Yaru Mou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Thyrotropin Levels in Patients with Coronavirus Disease 2019: Assessment during Hospitalization and in the Medium Term after Discharge
Abdallah Al-Salameh, Noémie Scherman, Imane Adda, Juliette André, Yoann Zerbib, Julien Maizel, Jean-Daniel Lalau, Etienne Brochot, Claire Andrejak, Rachel Desailloud
Life.2022; 12(12): 2014. CrossRef - Long COVID in Patients With Mild to Moderate Disease: Do Thyroid Function and Autoimmunity Play a Role?
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung,
Endocrine Practice.2021; 27(9): 894. CrossRef - Hashimoto’s thyroiditis following SARS-CoV-2 infection
Rafael Silvestre Knack, Taliê Hanada, Renata Silvestre Knack, Kamilla Mayr
BMJ Case Reports.2021; 14(8): e244909. CrossRef - Higher SARS-CoV-2 viral loads correlated with smaller thyroid volumes on ultrasound among male COVID-19 survivors
David Tak Wai Lui, Matrix Man Him Fung, Keith Wan Hang Chiu, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Wade Wei Wong, Cassandra Yuen Yan Lee, Chun Yiu Law, Kelvin K
Endocrine.2021; 74(2): 205. CrossRef - SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases
Avaniyapuram Kannan Murugan, Ali S Alzahrani
Journal of Inflammation Research.2021; Volume 14: 6191. CrossRef - POST-COVID ENDOCRINOPATHY :ABOUT A CASE ENDOCRINOPATHIE POST- COVID :À PROPOS D’UN CAS
S. Rafi, G. Elmghari, N, Elansari
INDIAN JOURNAL OF APPLIED RESEARCH.2021; : 13. CrossRef
- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis

- Clinical Study
- Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study
- Mijin Kim, Bo Hyun Kim, Hyungi Lee, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
- Endocrinol Metab. 2020;35(1):106-114. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.106
- 6,176 View
- 121 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
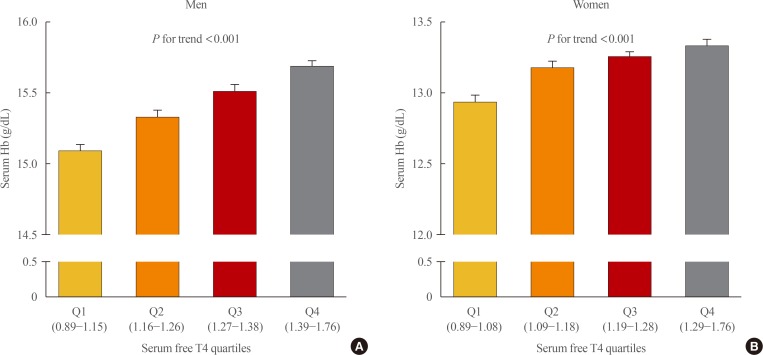
ePub Background Studies on the relationship between thyroid function and anemia in the euthyroid range are scarce. We aimed to evaluate the association between anemia and serum free thyroxine (fT4) and thyrotropin (TSH) in euthyroid adults.
Methods Data on 5,352 participants aged ≥19 years were obtained from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015). Anemia was defined as hemoglobin (Hb) <13 and <12 g/dL for men and women, respectively.
Results Overall, 6.1% of participants had anemia, and more women (9.9%) had anemia than men (2.8%,
P <0.001). In multivariate analysis, serum fT4 levels, but not TSH, were positively associated with serum Hb levels in both sexes (P <0.001, each). Serum Hb levels linearly reduced across decreasing serum fT4 quartile groups in both sexes (P <0.001, each). After adjusting for potential confounding factors, participants with low-normal fT4 had 4.4 (P =0.003) and 2.8 times (P <0.001) higher risk for anemia than those with high-normal fT4 among men and women, respectively. When participants were divided into two groups at 50 years of age, in younger participants, men and women with the first quartile were at higher risk of anemia than men with the second quartile (odds ratio [OR], 3.3;P =0.029) and women with the forth quartile (OR, 3.2;P <0.001), respectively. This association was not observed in older participants.Conclusion These results suggest that a low-normal level of serum fT4 was associated with a lower serum Hb level and a higher risk of anemia in euthyroid adults, especially in younger participants.
-
Citations
Citations to this article as recorded by- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank
Nicolien A van Vliet, Annelies E P Kamphuis, Wendy P J den Elzen, Gerard J Blauw, Jacobijn Gussekloo, Raymond Noordam, Diana van Heemst
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e643. CrossRef - Thyroid function, pernicious anemia and erythropoiesis: a two-sample Mendelian randomization study
Alisa D Kjaergaard, Alexander Teumer, Eirini Marouli, Panos Deloukas, Aleksander Kuś, Rosalie Sterenborg, Bjørn O Åsvold, Marco Medici, Christina Ellervik
Human Molecular Genetics.2022; 31(15): 2548. CrossRef - Changes of hematological indices in patients with diffuse toxic goiter
F. H. Saidova, L. M. Ahmedova, Zh. B. Aslanova, N. A. Najafov
Klinicheskaia khirurgiia.2021; 88(3-4): 76. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Zheng Feei Ma
Endocrinology and Metabolism.2020; 35(2): 484. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2020; 35(3): 669. CrossRef
- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank

- Thyroid
- Genome-Wide Association Studies of Autoimmune Thyroid Diseases, Thyroid Function, and Thyroid Cancer
- Yul Hwangbo, Young Joo Park
- Endocrinol Metab. 2018;33(2):175-184. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.175
- 8,096 View
- 142 Download
- 59 Web of Science
- 58 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Thyroid diseases, including autoimmune thyroid diseases and thyroid cancer, are known to have high heritability. Family and twin studies have indicated that genetics plays a major role in the development of thyroid diseases. Thyroid function, represented by thyroid stimulating hormone (TSH) and free thyroxine (T4), is also known to be partly genetically determined. Before the era of genome-wide association studies (GWAS), the ability to identify genes responsible for susceptibility to thyroid disease was limited. Over the past decade, GWAS have been used to identify genes involved in many complex diseases, including various phenotypes of the thyroid gland. In GWAS of autoimmune thyroid diseases, many susceptibility loci associated with autoimmunity (human leukocyte antigen [
HLA ], protein tyrosine phosphatase, non-receptor type 22 [PTPN22 ], cytotoxic T-lymphocyte associated protein 4 [CTLA4 ], and interleukin 2 receptor subunit alpha [IL2RA ]) or thyroid-specific genes (thyroid stimulating hormone receptor [TSHR ] and forkhead box E1 [FOXE1 ]) have been identified. Regarding thyroid function, many susceptibility loci for levels of TSH and free T4 have been identified through genome-wide analyses. In GWAS of differentiated thyroid cancer, associations atFOXE1 , MAP3K12 binding inhibitory protein 1 (MBIP )-NK2 homeobox 1 (NKX2-1 ), disrupted in renal carcinoma 3 (DIRC3 ), neuregulin 1 (NRG1 ), and pecanex-like 2 (PCNXL2 ) have been commonly identified in people of European and Korean ancestry, and many other susceptibility loci have been found in specific populations. Through GWAS of various thyroid-related phenotypes, many susceptibility loci have been found, providing insights into the pathogenesis of thyroid diseases and disease co-clustering within families and individuals.-
Citations
Citations to this article as recorded by- A new, all‐encompassing aetiology of type 1 diabetes
Piet C. de Groen
Immunology.2024; 171(1): 77. CrossRef - The role of primary cilia in thyroid diseases
Zijiao Tian, Xinlin Li, Xue Yu, Shuxin Yan, Jingwei Sun, Wenxin Ma, Xiaoyun Zhu, Yang Tang
Frontiers in Endocrinology.2024;[Epub] CrossRef - Investigating the Association of Polygenic Risk Scores With Thyroid Cancer Susceptibility in a Han Chinese Population
Yi-Hao Chen, I Chieh Chen, Chia-Man Chou, Sheng-Yang Huang
Journal of the Endocrine Society.2024;[Epub] CrossRef - Causal relationship between inflammatory cytokines and autoimmune thyroid disease: a bidirectional two-sample Mendelian randomization analysis
Zhiwei Yao, Fengli Guo, Yanlu Tan, Yiyuan Zhang, Yichen Geng, Guang Yang, Song Wang
Frontiers in Immunology.2024;[Epub] CrossRef - Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management
Jin Wang, Ke Wan, Xin Chang, Rui-Feng Mao
World Journal of Diabetes.2024; 15(3): 348. CrossRef - Multidimensional data analysis revealed thyroiditis-associated TCF19 SNP rs2073724 as a highly ranked protective variant in thyroid cancer
Xianhui Ruan, Yu Liu, Shuping Wu, Guiming Fu, Mei Tao, Yue Huang, Dapeng Li, Songfeng Wei, Ming Gao, Shicheng Guo, Junya Ning, Xiangqian Zheng
Aging.2024;[Epub] CrossRef - Exome sequencing to explore the possibility of predicting genetic susceptibility to the joint occurrence of polycystic ovary syndrome and Hashimoto’s thyroiditis
Natalia Zeber-Lubecka, Katarzyna Suchta, Maria Kulecka, Anna Kluska, Magdalena Piątkowska, Michal J. Dabrowski, Katarzyna Jankowska, Monika Grymowicz, Roman Smolarczyk, Ewa E. Hennig
Frontiers in Immunology.2023;[Epub] CrossRef - Molecular Mechanisms in Autoimmune Thyroid Disease
Hernando Vargas-Uricoechea
Cells.2023; 12(6): 918. CrossRef - Identification of multiple novel susceptibility genes associated with autoimmune thyroid disease
Xueying Liu, Yahu Miao, Chao Liu, Wan Lu, Qing Feng, Qiu Zhang
Frontiers in Immunology.2023;[Epub] CrossRef - Novel Susceptibility Genes Drive Familial Non-Medullary Thyroid Cancer in a Large Consanguineous Kindred
Pierre Majdalani, Uri Yoel, Tayseer Nasasra, Merav Fraenkel, Alon Haim, Neta Loewenthal, Raz Zarivach, Eli Hershkovitz, Ruti Parvari
International Journal of Molecular Sciences.2023; 24(9): 8233. CrossRef - An Optimized Flow Cytometric Method to Demonstrate the Differentiation Stage-Dependent Ca2+ Flux Responses of Peripheral Human B Cells
Anna Bajnok, Timea Serény-Litvai, Viktória Temesfői, Jasper Nörenberg, Róbert Herczeg, Ambrus Kaposi, Timea Berki, Emese Mezosi
International Journal of Molecular Sciences.2023; 24(10): 9107. CrossRef - FOXE1 Contributes to the Development of Psoriasis by Regulating WNT5A
Meng Liu, Guanfei Zhang, Ziyang Wang, Xinyi Liu, Ke He, Ruiting Luo, Qiqi Duan, Ruimin Bai, Yuqian Wang, Wenqian Du, Yan Zheng, Yongping Shao
Journal of Investigative Dermatology.2023; 143(12): 2366. CrossRef - Correlation analysis of HHV-6A viral load and anti-TPO antibody levels in patients with Hashimoto's thyroiditis
Noorossadat Seyyedi, Fariba Esfandiyari, Gholamreza Rafiei Dehbidi, Ali Farhadi, Farahnaz Zare, Sepide Namdari, Golrokh Bahmani, Banafsheh Rastegari, Farzaneh Zarghampoor, Abbas Behzad-Behbahani
Future Virology.2023; 18(8): 527. CrossRef - Primary cell cultures for the personalized therapy in aggressive thyroid cancer of follicular origin
Poupak Fallahi, Silvia Martina Ferrari, Giusy Elia, Francesca Ragusa, Armando Patrizio, Sabrina Rosaria Paparo, Gianni Marone, Maria Rosaria Galdiero, Giovanni Guglielmi, Rudy Foddis, Alfonso Cristaudo, Alessandro Antonelli
Seminars in Cancer Biology.2022; 79: 203. CrossRef - The Relationship between PTPN22 R620W Polymorphisms and the Susceptibility to Autoimmune Thyroid Diseases: An Updated Meta-analysis
Huaiyong Wu, Siyuan Wan, Mengying Qu, Bingxuan Ren, Lixiang Liu, Hongmei Shen
Immunological Investigations.2022; 51(2): 438. CrossRef - Identification of Transcriptional Pattern Related to Immune Cell Infiltration With Gene Co-Expression Network in Papillary Thyroid Cancer
Meiye Li, Jimei Zhang, Zongjing Zhang, Ying Qian, Wei Qu, Zhaoshun Jiang, Baochang Zhao
Frontiers in Endocrinology.2022;[Epub] CrossRef - Analysis of rare genetic variation underlying cardiometabolic diseases and traits among 200,000 individuals in the UK Biobank
Sean J. Jurgens, Seung Hoan Choi, Valerie N. Morrill, Mark Chaffin, James P. Pirruccello, Jennifer L. Halford, Lu-Chen Weng, Victor Nauffal, Carolina Roselli, Amelia W. Hall, Matthew T. Oetjens, Braxton Lagerman, David P. vanMaanen, Goncalo Abecasis, Xiao
Nature Genetics.2022; 54(3): 240. CrossRef - Factors affecting recurrence in subacute granulomatous thyroiditis
Çiğdem Tura Bahadir, Merve Yilmaz, Elif Kiliçkan
Archives of Endocrinology and Metabolism.2022;[Epub] CrossRef - Shared etiology of type 1 diabetes and Hashimoto’s thyroiditis: a population-based twin study
Jakob Skov, Ralf Kuja-Halkola, Patrik K E Magnusson, Soffia Gudbjörnsdottir, Olle Kämpe, Sophie Bensing
European Journal of Endocrinology.2022; 186(6): 677. CrossRef - High Prevalence of Common Human Viruses in Thyroid Tissue
Therese Weider, Angelo Genoni, Francesco Broccolo, Trond H. Paulsen, Knut Dahl-Jørgensen, Antonio Toniolo, Sara Salehi Hammerstad
Frontiers in Endocrinology.2022;[Epub] CrossRef - B cells from anti-thyroid antibody positive, infertile women show hyper-reactivity to BCR stimulation
Timea Serény-Litvai, Anna Bajnok, Viktoria Temesfoi, Jasper Nörenberg, Greta Pham-Dobor, Ambrus Kaposi, Akos Varnagy, Kalman Kovacs, Sandor Pentek, Tamas Koszegi, Emese Mezosi, Timea Berki
Frontiers in Immunology.2022;[Epub] CrossRef - What do the structures of GCN5-containing complexes teach us about their function?
Dominique Helmlinger, Gábor Papai, Didier Devys, László Tora
Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms.2021; 1864(2): 194614. CrossRef - Genetic Susceptibility to Joint Occurrence of Polycystic Ovary Syndrome and Hashimoto’s Thyroiditis: How Far Is Our Understanding?
Natalia Zeber-Lubecka, Ewa E. Hennig
Frontiers in Immunology.2021;[Epub] CrossRef - Type 1 Diabetes and Autoimmune Thyroid Disease—The Genetic Link
Lara Frommer, George J. Kahaly
Frontiers in Endocrinology.2021;[Epub] CrossRef - Familial Risk of Hashimoto's Thyroiditis Among First-Degree Relatives: A Population-Based Study in Korea
Hyun Jung Kim, Sayada Zartasha Kazmi, Taeuk Kang, Seo Young Sohn, Dong-Sook Kim, Hoo Jae Hann, Hyeong Sik Ahn
Thyroid.2021; 31(7): 1096. CrossRef - Limited Genetic Overlap Between Overt Hashimoto’s Thyroiditis and Graves’ Disease in Twins: A Population-based Study
Jakob Skov, Jan Calissendorff, Daniel Eriksson, Patrik Magnusson, Olle Kämpe, Sophie Bensing, Ralf Kuja-Halkola
The Journal of Clinical Endocrinology & Metabolism.2021; 106(4): e1101. CrossRef - Endogenous and Synthetic Regulators of the Peripheral Components of the Hypothalamo-Hypophyseal-Gonadal and -Thyroid Axes
A. O. Shpakov
Neuroscience and Behavioral Physiology.2021; 51(3): 332. CrossRef - Programmed Cell Death-Ligand 1 (PD-L1) gene Single Nucleotide Polymorphism in Graves’ Disease and Hashimoto’s Thyroiditis in Korean Patients
Jee Hee Yoon, Min-ho Shin, Hee Nam Kim, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2021; 36(3): 599. CrossRef - Predisposition to Graves’ disease and Graves’ ophthalmopathy by genetic variants of IL2RA
Juan Du, Xin Wang, Guiqin Tan, Wenwen Wei, Fangyu Zhou, Zhongzhi Liang, Hua Li, Hongsong Yu
Journal of Molecular Medicine.2021; 99(10): 1487. CrossRef - Association of IL-1β, NLRP3, and COX-2 Gene Polymorphisms with Autoimmune Thyroid Disease Risk and Clinical Features in the Iranian Population
Zahra Heidari, Saeedeh Salimi, Mohsen Rokni, Mahnaz Rezaei, Neshat Khalafi, Mahdieh Jafari Shahroudi, Azizallah Dehghan, Mohsen Saravani, Rafael S. De Molon
BioMed Research International.2021; 2021: 1. CrossRef - Genetic polymorphisms in the PCNXL2 gene are risk factors for thyroid cancer in the Chinese population
Runmei Hao, Peng Han, Ling Zhang, Ying Bi, Jinfeng Yan, Honghui Li, Yanxia Bai, Chongwen Xu, Baiya Li, Huajing Li
Future Oncology.2021; 17(34): 4677. CrossRef - Genetic Variants Associated with Thyroid Cancer Risk: Comprehensive Research Synopsis, Meta-Analysis, and Cumulative Epidemiological Evidence
Ran Ran, Gang Tu, Hui Li, Hao Wang, Exian Mou, Caiyang Liu, Yuan Seng Wu
Journal of Oncology.2021; 2021: 1. CrossRef - The Identification of Three Key Genes Related to Stemness in Thyroid Carcinoma through Comprehensive Analysis
Tonglong Zhang, Chunhong Yan, Zhengdu Ye, Xingling Yin, Tian-an Jiang
Combinatorial Chemistry & High Throughput Screening.2021; 24(3): 423. CrossRef - Епідеміологія автоімунного тиреоїдиту
V.I. Кravchenko, О.А. Тоvkay, О.V. Rakov, М.D. Тronko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(2): 136. CrossRef - Thyroid autoimmune disorders and cancer
Silvia Martina Ferrari, Poupak Fallahi, Giusy Elia, Francesca Ragusa, Ilaria Ruffilli, Sabrina Rosaria Paparo, Alessandro Antonelli
Seminars in Cancer Biology.2020; 64: 135. CrossRef - Association of FCRL3 rs7528684 polymorphism with risk of Hashimoto's thyroiditis in Iranian patients
Kurosh Kalantar, Farzad Ghandehari, Saeed Malek-Hosseini, Hossein Golmoghaddam, Davood Rostamzadeh, Mohamad Hossein Dabbaghmanesh, Zahra Amirghofran
Meta Gene.2020; 24: 100663. CrossRef - Differentiated thyroid cancer and Hashimoto thyroiditis: Utility of the Afirma gene expression classifier
Vardan Papoian, Jennifer E. Rosen, Wen Lee, Leonard Wartofsky, Erin A. Felger
Journal of Surgical Oncology.2020; 121(7): 1053. CrossRef - Familial risks between Graves disease and Hashimoto thyroiditis and other autoimmune diseases in the population of Sweden
Hauke Thomsen, Xinjun Li, Kristina Sundquist, Jan Sundquist, Asta Försti, Kari Hemminki
Journal of Translational Autoimmunity.2020; 3: 100058. CrossRef - Association of rs944289, rs965513, and rs1443434 in TITF1/TITF2 with Risks of Papillary Thyroid Carcinoma and with Nodular Goiter in Northern Chinese Han Populations
Xin Zhang, Yulu Gu, Yong Li, Heran Cui, Xiaoli Liu, Hui Sun, Qiong Yu, Yaqin Yu, Yawen Liu, Siyan Zhan, Yi Cheng
International Journal of Endocrinology.2020; 2020: 1. CrossRef - FLT3 stop mutation increases FLT3 ligand level and risk of autoimmune thyroid disease
Saedis Saevarsdottir, Thorunn A. Olafsdottir, Erna V. Ivarsdottir, Gisli H. Halldorsson, Kristbjorg Gunnarsdottir, Asgeir Sigurdsson, Ari Johannesson, Jon K. Sigurdsson, Thorhildur Juliusdottir, Sigrun H. Lund, Asgeir O. Arnthorsson, Edda L. Styrmisdottir
Nature.2020; 584(7822): 619. CrossRef - Genetic relationship between Hashimoto`s thyroiditis and papillary thyroid carcinoma with coexisting Hashimoto`s thyroiditis
Ohoud Subhi, Hans-Juergen Schulten, Nadia Bagatian, Roa'a Al-Dayini, Sajjad Karim, Sherin Bakhashab, Reem Alotibi, Alaa Al-Ahmadi, Manar Ata, Aisha Elaimi, Saad Al-Muhayawi, Majid Mansouri, Khalid Al-Ghamdi, Osman Abdel Hamour, Awatif Jamal, Jaudah Al-Mag
PLOS ONE.2020; 15(6): e0234566. CrossRef - Thyroid cancer and thyroid autoimmune disease: A review of molecular aspects and clinical outcomes
Natália Medeiros Dias Lopes, Hannah Hamada Mendonça Lens, André Armani, Poliana Camila Marinello, Alessandra Lourenço Cecchini
Pathology - Research and Practice.2020; 216(9): 153098. CrossRef - Immune gene signature delineates a subclass of thyroid cancer with unfavorable clinical outcomes
Jingtai Zhi, Jiaoyu Yi, Mengran Tian, Huijuan Wang, Ning Kang, Xiangqian Zheng, Ming Gao
Aging.2020; 12(7): 5733. CrossRef - VARIETY OF COMBINATIONS OF HASHIMOTO’S THYROIDITIS WITH OTHER BACKGROUND PATHOLOGY OF THYROID PARENCHEMA IN DIFFERENT FORMS OF THYROID CANCER
Yu. I. Karachentsev, V. M. Dubovik, I. V. Gopkalova, V. V. Khaziev, S. S. Sokolova, Y. P. Korchagin, N. G. Filonenko, M. Y. Sazonov, L. V. Gerasimenko
Bulletin of Problems Biology and Medicine.2020; 3(1): 105. CrossRef - Analysis of Polymorphisms rs7093069-IL-2RA, rs7138803-FAIM2, and rs1748033-PADI4 in the Group of Adolescents With Autoimmune Thyroid Diseases
Beata Sawicka, Hanna Borysewicz-Sańczyk, Natalia Wawrusiewicz-Kurylonek, Tommaso Aversa, Domenico Corica, Joanna Gościk, Adam Krętowski, Małgorzata Waśniewska, Artur Bossowski
Frontiers in Endocrinology.2020;[Epub] CrossRef - Familial associations for rheumatoid autoimmune diseases
Hauke Thomsen, Xinjun Li, Kristina Sundquist, Jan Sundquist, Asta Försti, Kari Hemminki
Rheumatology Advances in Practice.2020;[Epub] CrossRef - Familial risks between giant cell arteritis and Takayasu arteritis and other autoimmune diseases in the population of Sweden
Hauke Thomsen, Xinjun Li, Kristina Sundquist, Jan Sundquist, Asta Försti, Kari Hemminki
Scientific Reports.2020;[Epub] CrossRef - The Association of Obesity with Autoimmune Thyroiditis and Thyroid Function-Possible Mechanisms of Bilateral Interaction
Agnieszka Baranowska-Bik, Wojciech Bik, Henrik Falhammar
International Journal of Endocrinology.2020; 2020: 1. CrossRef - The Risk of Recurrence of Subacute Thyroiditis Is HLA-Dependent
Magdalena Stasiak, Bogusław Tymoniuk, Bartłomiej Stasiak, Andrzej Lewiński
International Journal of Molecular Sciences.2019; 20(5): 1089. CrossRef - FOXE1 inhibits cell proliferation, migration and invasion of papillary thyroid cancer by regulating PDGFA
Zheng Ding, Ronghu Ke, Yong Zhang, Youben Fan, Jianxia Fan
Molecular and Cellular Endocrinology.2019; 493: 110420. CrossRef - Current Knowledge of Germline Genetic Risk Factors for the Development of Non-Medullary Thyroid Cancer
Kinga Hińcza, Artur Kowalik, Aldona Kowalska
Genes.2019; 10(7): 482. CrossRef - Thyroid Cancer: The Quest for Genetic Susceptibility Involving DNA Repair Genes
Santos, Gomes, Bastos, Gil, Azevedo, Ferreira, Limbert, Silva, Rueff
Genes.2019; 10(8): 586. CrossRef - Genetic Polymorphisms on 4q21.1 Contributed to the Risk of Hashimoto's Thyroiditis
Dachao Mo, Junjiu Li, Liang Peng, Zhiyuan Liu, Jieyun Wang, Jiru Yuan
Genetic Testing and Molecular Biomarkers.2019; 23(12): 837. CrossRef - A Weighted Genetic Risk Score Using Known Susceptibility Variants to Predict Graves Disease Risk
Yu-Ru Ma, Shuang-Xia Zhao, Lu Li, Feng Sun, Xiao-Ping Ye, Fei-Fei Yuan, Dan Jiang, Zheng Zhou, Qian-Yue Zhang, Yue-Yue Wan, Guang-Ya Zhang, Jing Wu, Rui-Jia Zhang, Ya Fang, Huai-Dong Song
The Journal of Clinical Endocrinology & Metabolism.2019; 104(6): 2121. CrossRef - Architects meets Repairers: The interplay between homeobox genes and DNA repair
Bruno César Feltes
DNA Repair.2019; 73: 34. CrossRef - Development of a prognostic index based on an immunogenomic landscape analysis of papillary thyroid cancer
Peng Lin, Yi-nan Guo, Lin Shi, Xiao-jiao Li, Hong Yang, Yun He, Qing Li, Yi-wu Dang, Kang-lai Wei, Gang Chen
Aging.2019; 11(2): 480. CrossRef - Selenium and Selenoproteins in Immune Mediated Thyroid Disorders
Liliana Santos, Celestino Neves, Miguel Melo, Paula Soares
Diagnostics.2018; 8(4): 70. CrossRef - Sex-specific genetic influence on thyroid-stimulating hormone and free thyroxine levels, and interactions between measurements: KNHANES 2013–2015
Young Ki Lee, Dong Yeob Shin, Hyejung Shin, Eun Jig Lee, Silvia Naitza
PLOS ONE.2018; 13(11): e0207446. CrossRef
- A new, all‐encompassing aetiology of type 1 diabetes


 KES
KES

 First
First Prev
Prev



