Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Treatment of Hypoparathyroidism by Re-Establishing the Effects of Parathyroid Hormone
- Lars Rejnmark
- Endocrinol Metab. 2024;39(2):262-266. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1916

- 1,131 View
- 61 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The conventional treatment of hypoparathyroidism (HypoPT) includes active vitamin D and calcium. Despite normalization of calcium levels, the conventional treatment is associated with fluctuations in calcium levels, hypercalciuria, renal impairment, and decreased quality of life (QoL). Replacement therapy with parathyroid hormone (PTH)(1-84) is an option in some countries. However, convincing beneficial effects have not been demonstrated, which may be due to the short duration of action of this treatment. Recently, palopegteriparatide (also known as TransCon PTH) has been marketed in Europe and is expected also to be approved in other countries. Palopegteriparatide is a prodrug with sustained release of PTH(1-34) designed to provide stable physiological PTH levels for 24 hours/day. A phase 3 study demonstrated maintenance of normocalcemia in patients with chronic HypoPT, with no need for conventional therapy. Furthermore, this treatment lowers urinary calcium and improves QoL. Another long-acting PTH analog with effects on the parathyroid hormone receptor (eneboparatide) is currently being tested in a phase 3 trial. Furthermore, the treatment of autosomal dominant hypocalcemia type 1 with a calcilytic (encaleret) is also being tested. All in all, improved treatment options are on the way that will likely take the treatment of HypoPT to the next level.

- Miscellaneous
- Clinical Characteristics, Management, and Potential Biomarkers of Endocrine Dysfunction Induced by Immune Checkpoint Inhibitors
- Shintaro Iwama, Tomoko Kobayashi, Hiroshi Arima
- Endocrinol Metab. 2021;36(2):312-321. Published online April 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1007
- 5,524 View
- 268 Download
- 15 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
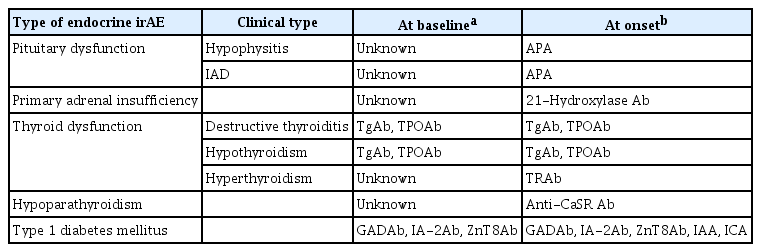
ePub - Immune-related adverse events (irAEs) affecting the endocrine glands are among the most frequent irAEs induced by immune checkpoint inhibitors (ICIs) and include hypopituitarism, primary adrenal insufficiency, thyrotoxicosis, hypothyroidism, hypoparathyroidism, and type 1 diabetes mellitus. Since the incidence and clinical features of endocrine irAEs vary according to the ICI used, it is important to understand the characteristics of these irAEs and to manage each one appropriately. Since some endocrine irAEs, including adrenal crisis and diabetic ketoacidosis, are potentially life-threatening, predicting the risk of endocrine irAEs before their onset is critical. Several autoantibodies have been detected in patients who develop endocrine irAEs, among which anti-thyroid antibodies may be predictive biomarkers of thyroid dysfunction. In this review, we describe the clinical features of each endocrine irAE induced by ICIs and discuss their potential biomarkers, including autoantibodies.
-
Citations
Citations to this article as recorded by- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events
Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima
Endocrine Journal.2024; 71(1): 23. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - Endocrinopathies Associated With Immune Checkpoint Inhibitor Use
Anupam Kotwal, Randol Kennedy, Nupur Kikani, Sonali Thosani, Whitney Goldner, Afreen Shariff
Endocrine Practice.2024;[Epub] CrossRef - Recovery from insulin dependence in immune checkpoint inhibitor‐associated diabetes mellitus: A case report
Marie Okubo, Yuji Hataya, Kanta Fujimoto, Toshio Iwakura, Naoki Matsuoka
Journal of Diabetes Investigation.2023; 14(1): 147. CrossRef - Case Report: A Rising Cause of New-Onset Endocrinopathies After Immunotherapy
Charity Tan, Sarah Hendricks, Kristina Hernandez, Martha Benavides, Rupinderjit Samra
The Journal for Nurse Practitioners.2023; 19(5): 104582. CrossRef - Risk of Thyroid Dysfunction in PD-1 Blockade Is Stratified by the Pattern of TgAb and TPOAb Positivity at Baseline
Xin Zhou, Shintaro Iwama, Tomoko Kobayashi, Masahiko Ando, Hiroshi Arima
The Journal of Clinical Endocrinology & Metabolism.2023; 108(10): e1056. CrossRef - Severe thyrotoxicosis induced by tislelizumab: a case report and literature review
Liman Huo, Chao Wang, Haixia Ding, Xuelian Shi, Bin Shan, Ruoying Zhou, Ping Liang, Juan Hou
Frontiers in Oncology.2023;[Epub] CrossRef - Life-Threatening Endocrinological Immune-Related Adverse Events of Immune Checkpoint Inhibitor Therapy
Aleksandra Basek, Grzegorz K. Jakubiak, Grzegorz Cieślar, Agata Stanek
Cancers.2023; 15(24): 5786. CrossRef - Increased Risk of Thyroid Dysfunction by PD-1 and CTLA-4 Blockade in Patients Without Thyroid Autoantibodies at Baseline
Shintaro Iwama, Tomoko Kobayashi, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Masahiko Ando, Xin Zhou, Ayana Yamagami, Takeshi Onoue, Yohei Kawaguchi, Takashi Miyata, Mariko Sugiyama, Hiroshi Takagi, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tets
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): e1620. CrossRef - Biomarkers and risk factors for the early prediction of immune-related adverse events: a review
Ying Zhang, Xiaoling Zhang, Weiling Li, Yunyi Du, Wenqing Hu, Jun Zhao
Human Vaccines & Immunotherapeutics.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors as a Threat to the Hypothalamus–Pituitary Axis: A Completed Puzzle
Agnese Barnabei, Andrea Corsello, Rosa Maria Paragliola, Giovanni Maria Iannantuono, Luca Falzone, Salvatore Maria Corsello, Francesco Torino
Cancers.2022; 14(4): 1057. CrossRef - Elevated TSH Level, TgAb, and Prior Use of Ramucirumab or TKIs as Risk Factors for Thyroid Dysfunction in PD-L1 Blockade
Tomoko Kobayashi, Shintaro Iwama, Ayana Yamagami, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Xin Zhou, Masahiko Ando, Takeshi Onoue, Takashi Miyata, Mariko Sugiyama, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tetsunari Hase, Masahiro Morise, Taka
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4115. CrossRef - Preconditioning of the immune system modulates the response of papillary thyroid cancer to immune checkpoint inhibitors
Fabiana Pani, Yoshinori Yasuda, Sylvie T Rousseau, Kevin C Bermea, Solmaz Roshanmehr, Rulin Wang, Srinivasan Yegnasubramanian, Patrizio Caturegli, Luigi Adamo
Journal for ImmunoTherapy of Cancer.2022; 10(12): e005538. CrossRef - Survival benefit of endocrine dysfunction following immune checkpoint inhibitors for nonthyroidal cancers
Anupam Kotwal, Mabel Ryder
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 517. CrossRef
- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events

- Miscellaneous
- Rare PTH Gene Mutations Causing Parathyroid Disorders: A Review
- Joon-Hyop Lee, Munkhtugs Davaatseren, Sihoon Lee
- Endocrinol Metab. 2020;35(1):64-70. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.64

- 5,095 View
- 108 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Since parathyroid hormone (PTH) was first isolated and its gene (
PTH ) was sequenced, only eightPTH mutations have been discovered. The C18R mutation inPTH , discovered in 1990, was the first to be reported. This autosomal dominant mutation induces endoplasmic reticulum stress and subsequent apoptosis in parathyroid cells. The next mutation, which was reported in 1992, is associated with exon skipping. The substitution of G with C in the first nucleotide of the second intron results in the exclusion of the second exon; since this exon includes the initiation codon, translation initiation is prevented. An S23P mutation and an S23X mutation at the same residue were reported in 1999 and 2012, respectively. Both mutations resulted in hypoparathyroidism. In 2008, a somatic R83X mutation was detected in a parathyroid adenoma tissue sample collected from a patient with hyperparathyroidism. In 2013, a heterozygous p.Met1_Asp6del mutation was incidentally discovered in a case-control study. Two years later, the R56C mutation was reported; this is the only reported hypoparathyroidism-causing mutation in the mature bioactive part ofPTH . In 2017, another heterozygous mutation, M14K, was detected. The discovery of these eight mutations in thePTH gene has provided insights into its function and broadened our understanding of the molecular mechanisms underlying mutation progression. Further attempts to detect other such mutations will help elucidate the functions of PTH in a more sophisticated manner.-
Citations
Citations to this article as recorded by- The Intricacies of Renal Phosphate Reabsorption—An Overview
Valerie Walker
International Journal of Molecular Sciences.2024; 25(9): 4684. CrossRef - Molecular and Clinical Spectrum of Primary Hyperparathyroidism
Smita Jha, William F Simonds
Endocrine Reviews.2023; 44(5): 779. CrossRef - Rare cause of persistent hypocalcaemia in infancy due to PTH gene mutation
Savita Khadse, Vrushali Satish Takalikar, Radha Ghildiyal, Nikhil Shah
BMJ Case Reports.2023; 16(9): e256358. CrossRef - Homozygous Ser-1 to Pro-1 mutation in parathyroid hormone identified in hypocalcemic patients results in secretion of a biologically inactive pro-hormone
Patrick Hanna, Ashok Khatri, Shawn Choi, Severine Brabant, Matti L. Gild, Marie L. Piketty, Bruno Francou, Dominique Prié, John T. Potts, Roderick J. Clifton-Bligh, Agnès Linglart, Thomas J. Gardella, Harald Jüppner
Proceedings of the National Academy of Sciences.2023;[Epub] CrossRef - Genetics of monogenic disorders of calcium and bone metabolism
Paul J. Newey, Fadil M. Hannan, Abbie Wilson, Rajesh V. Thakker
Clinical Endocrinology.2022; 97(4): 483. CrossRef - Homozygous missense variant of PTH (c.166C>T, p.(Arg56Cys)) as the cause of familial isolated hypoparathyroidism in a three-year-old child
Stine Linding Andersen, Anja Lisbeth Frederiksen, Astrid Bruun Rasmussen, Mette Madsen, Ann-Margrethe Rønholt Christensen
Journal of Pediatric Endocrinology and Metabolism.2022; 35(5): 691. CrossRef - Novel PTH Gene Mutations Causing Isolated Hypoparathyroidism
Colin P Hawkes, Jamal M Al Jubeh, Dong Li, Susan E Tucker, Tara Rajiyah, Michael A Levine
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2449. CrossRef
- The Intricacies of Renal Phosphate Reabsorption—An Overview

- Miscellaneous
- Novel Mutation in PTHLH Related to Brachydactyly Type E2 Initially Confused with Unclassical Pseudopseudohypoparathyroidism
- Jihong Bae, Hong Seok Choi, So Young Park, Do-Eun Lee, Sihoon Lee
- Endocrinol Metab. 2018;33(2):252-259. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.252
- 4,447 View
- 65 Download
- 10 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Autosomal-dominant brachydactyly type E is a congenital abnormality characterized by small hands and feet, which is a consequence of shortened metacarpals and metatarsals. We recently encountered a young gentleman exhibiting shortening of 4th and 5th fingers and toes. Initially, we suspected him having pseudopseudohypoparathyroidism (PPHP) because of normal biochemical parameters, including electrolyte, Ca, P, and parathyroid hormone (PTH) levels; however, his mother and maternal grandmother had the same conditions in their hands and feet. Furthermore, his mother showed normal biochemical parameters. To the best of our knowledge, PPHP is inherited via a mutated paternal allele, owing to the paternal imprinting of GNAS (guanine nucleotide binding protein, alpha stimulating) in the renal proximal tubule. Therefore, we decided to further analyze the genetic background in this family.
Methods Whole exome sequencing was performed using genomic DNA from the affected mother, son, and the unaffected father as a negative control.
Results We selected the intersection between 45,490 variants from the mother and 45,646 variants from the son and excluded 27,512 overlapping variants identified from the father. By excluding homogenous and compound heterozygous variants and removing all previously reported variants, 147 variants were identified to be shared by the mother and son. Variants that had least proximities among species were excluded and finally 23 variants remained.
Conclusion Among them, we identified a defect in parathyroid hormone like hormone (
PTHLH ), encoding the PTH-related protein, to be disease-causative. Herein, we report a family affected with brachydactyly type E2 caused by a novelPTHLH mutation, which was confused with PPHP with unclassical genetic penetrance.-
Citations
Citations to this article as recorded by- A novel heterozygous mutation in PTHLH causing autosomal dominant brachydactyly type E complicated with short stature
Jian Sun, Nian Yang, Zhengquan Xu, Hongbo Cheng, Xiangxin Zhang
Molecular Genetics & Genomic Medicine.2024;[Epub] CrossRef - A novel mutation in PTHLH in a family with a variable phenotype with brachydactyly, short stature, oligodontia and developmental delay
Mirjam E.A. Scheffer-Rath, Hermine E. Veenstra-Knol, Annemieke M. Boot
Bone Reports.2023; 19: 101699. CrossRef - Bioactive phytoconstituents as potent inhibitors of casein kinase-2: dual implications in cancer and COVID-19 therapeutics
Farah Anjum, Md Nayab Sulaimani, Alaa Shafie, Taj Mohammad, Ghulam Md. Ashraf, Anwar L. Bilgrami, Fahad A. Alhumaydhi, Suliman A. Alsagaby, Dharmendra Kumar Yadav, Md. Imtaiyaz Hassan
RSC Advances.2022; 12(13): 7872. CrossRef - Characterization and expression profiling of G protein-coupled receptors (GPCRs) in Spodoptera litura (Lepidoptera: Noctuidae)
Yanxiao Li, Han Gao, Hui Zhang, Runnan Yu, Fan Feng, Jing Tang, Bin Li
Comparative Biochemistry and Physiology Part D: Genomics and Proteomics.2022; 44: 101018. CrossRef - Genes with specificity for expression in the round cell layer of the growth plate are enriched in genomewide association study (GWAS) of human height
Nora E. Renthal, Priyanka Nakka, John M. Baronas, Henry M. Kronenberg, Joel N. Hirschhorn
Journal of Bone and Mineral Research.2020; 36(12): 2300. CrossRef - Search for Novel Mutational Targets in Human Endocrine Diseases
So Young Park, Myeong Han Seo, Sihoon Lee
Endocrinology and Metabolism.2019; 34(1): 23. CrossRef - A Heterozygous Splice-Site Mutation in PTHLH Causes Autosomal Dominant Shortening of Metacarpals and Metatarsals
Monica Reyes, Bert Bravenboer, Harald Jüppner
Journal of Bone and Mineral Research.2019; 34(3): 482. CrossRef - A 3.06-Mb interstitial deletion on 12p11.22-12.1 caused brachydactyly type E combined with pectus carinatum
Jia Huang, Hong-Yan Liu, Rong-Rong Wang, Hai Xiao, Dong Wu, Tao Li, Ying-Hai Jiang, Xue Zhang
Chinese Medical Journal.2019; 132(14): 1681. CrossRef - Parathyroid Hormone-Related Protein in the Hand or Out of Hand?
Sang Wan Kim
Endocrinology and Metabolism.2018; 33(2): 202. CrossRef
- A novel heterozygous mutation in PTHLH causing autosomal dominant brachydactyly type E complicated with short stature

- Site-Specific Difference of Bone Geometry Indices in Hypoparathyroid Patients
- Hye-Sun Park, Da Hea Seo, Yumie Rhee, Sung-Kil Lim
- Endocrinol Metab. 2017;32(1):68-76. Published online February 6, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.68
- 3,317 View
- 32 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypoparathyroid patients often have a higher bone mineral density (BMD) than the general population. However, an increase in BMD does not necessarily correlate with a solid bone microstructure. This study aimed to evaluate the bone microstructure of hypoparathyroid patients by using hip structure analysis (HSA).
Methods Ninety-five hypoparathyroid patients >20 years old were enrolled and 31 of them had eligible data for analyzing bone geometry parameters using HSA. And among the control data, we extracted sex-, age-, and body mass index-matched three control subjects to each patient. The BMD data were reviewed retrospectively and the bone geometry parameters of the patients were analyzed by HSA.
Results The mean Z-scores of hypoparathyroid patients at the lumbar spine, femoral neck, and total hip were above zero (0.63±1.17, 0.48±1.13, and 0.62±1.10, respectively). The differences in bone geometric parameters were site specific. At the femoral neck and intertrochanter, the cross-sectional area (CSA) and cortical thickness (C.th) were higher, whereas the buckling ratio (BR) was lower than in controls. However, those trends were opposite at the femoral shaft; that is, the CSA and C.th were low and the BR was high.
Conclusion Our study shows the site-specific effects of hypoparathyroidism on the bone. Differences in bone components, marrow composition, or modeling based bone formation may explain these findings. However, further studies are warranted to investigate the mechanism, and its relation to fracture risk.
-
Citations
Citations to this article as recorded by- Vertebral fractures, trabecular bone score and their determinants in chronic hypoparathyroidism
S. Saha, V. Mannar, D. Kandasamy, V. Sreenivas, R. Goswami
Journal of Endocrinological Investigation.2022; 45(9): 1777. CrossRef - Epidemiology and Financial Burden of Adult Chronic Hypoparathyroidism
Sigridur Bjornsdottir, Steven Ing, Deborah M Mitchell, Tanja Sikjaer, Line Underbjerg, Zaki Hassan-Smith, Jad Sfeir, Neil J Gittoes, Bart L Clarke L
Journal of Bone and Mineral Research.2020; 37(12): 2602. CrossRef - Effect of Endogenous Parathyroid Hormone on Bone Geometry and Skeletal Microarchitecture
A Ram Hong, Ji Hyun Lee, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
Calcified Tissue International.2019; 104(4): 382. CrossRef - Bone responses to chronic treatment of adult hypoparathyroid patients with PTH peptides
Sofie Malmstroem, Lars Rejnmark, Dolores M. Shoback
Current Opinion in Endocrine and Metabolic Research.2018; 3: 51. CrossRef
- Vertebral fractures, trabecular bone score and their determinants in chronic hypoparathyroidism

- Adrenal gland
- Hypoparathyroidism: Replacement Therapy with Parathyroid Hormone
- Lars Rejnmark, Line Underbjerg, Tanja Sikjaer
- Endocrinol Metab. 2015;30(4):436-442. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.436
- 3,517 View
- 39 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hypoparathyroidism (HypoPT) is characterized by low serum calcium levels caused by an insufficient secretion of parathyroid hormone (PTH). Despite normalization of serum calcium levels by treatment with activated vitamin D analogues and calcium supplementation, patients are suffering from impaired quality of life (QoL) and are at increased risk of a number of comorbidities. Thus, despite normalization of calcium levels in response to conventional therapy, this should only be considered as an apparent normalization, as patients are suffering from a number of complications and calcium-phosphate homeostasis is not normalized in a physiological manner. In a number of recent studies, replacement therapy with recombinant human PTH (rhPTH(1-84)) as well as therapy with the N-terminal PTH fragment (rhPTH(1-34)) have been investigated. Both drugs have been shown to normalize serum calcium while reducing needs for activated vitamin D and calcium supplements. However, once a day injections cause large fluctuations in serum calcium. Twice a day injections diminish fluctuations, but don't restore the normal physiology of calcium homeostasis. Recent studies using pump-delivery have shown promising results on maintaining normocalcemia with minimal fluctuations in calcium levels. Further studies are needed to determine whether this may improve QoL and lower risk of complications. Such data are needed before replacement with the missing hormone can be recommended as standard therapy.
-
Citations
Citations to this article as recorded by- Point-of-Care Peptide Hormone Production Enabled by Cell-Free Protein Synthesis
Madison A. DeWinter, Ariel Helms Thames, Laura Guerrero, Weston Kightlinger, Ashty S. Karim, Michael C. Jewett
ACS Synthetic Biology.2023; 12(4): 1216. CrossRef - Comparing laser speckle contrast imaging and indocyanine green angiography for assessment of parathyroid perfusion
Emmanuel A. Mannoh, Naira Baregamian, Giju Thomas, Carmen C. Solόrzano, Anita Mahadevan-Jansen
Scientific Reports.2023;[Epub] CrossRef - Effects of Multi-stage Procurement on the Viability and Function of Human Donor Parathyroid Glands
Yvonne M. Kelly, Casey Ward, Run Zhang, Shareef Syed, Peter G. Stock, Quan-Yang Duh, Julie A. Sosa, James Koh
Journal of Surgical Research.2022; 276: 404. CrossRef - Kidney Complications and Hospitalization in Patients With Chronic Hypoparathyroidism: A Cohort Study in Sweden
Oskar Swartling, Marie Evans, Tim Spelman, Wafa Kamal, Olle Kämpe, Michael Mannstadt, Ylva Trolle Lagerros, Sigridur Björnsdottir
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4098. CrossRef - Hypocalcaemia
Zaki Hassan-Smith, Neil Gittoes
Medicine.2021; 49(9): 562. CrossRef - Safety and Efficacy of 5 Years of Treatment With Recombinant Human Parathyroid Hormone in Adults With Hypoparathyroidism
Michael Mannstadt, Bart L Clarke, John P Bilezikian, Henry Bone, Douglas Denham, Michael A Levine, Munro Peacock, Jeffrey Rothman, Dolores M Shoback, Mark L Warren, Nelson B Watts, Hak-Myung Lee, Nicole Sherry, Tamara J Vokes
The Journal of Clinical Endocrinology & Metabolism.2019; 104(11): 5136. CrossRef - Management of Endocrine Emergencies in the ICU
Judith Jacobi
Journal of Pharmacy Practice.2019; 32(3): 314. CrossRef - Microencapsulated parathyroid allotransplantation in the omental tissue
Emrah Yucesan, Harun Basoglu, Beyza Goncu, Fahri Akbas, Yeliz Emine Ersoy, Erhan Aysan
Artificial Organs.2019; 43(10): 1022. CrossRef - Die HypAus-Studie
Maximilian Zach, Adelina Tmava-Berisha, Stefan Schatzl, Michael Lehner, Greisa Vila, Karin Amrein
Journal für Klinische Endokrinologie und Stoffwechsel.2018; 11(2): 45. CrossRef -
Sustained release of parathyroid hormone via
in situ
cross‐linking gelatin hydrogels improves the therapeutic potential of tonsil‐derived mesenchymal stem cells for hypoparathyroidism
Yoon Shin Park, Yunki Lee, Yoon Mi Jin, Gyungah Kim, Sung Chul Jung, Yoon Jeong Park, Ki Dong Park, Inho Jo
Journal of Tissue Engineering and Regenerative Medicine.2018;[Epub] CrossRef - Hypocalcaemia
Zaki Hassan-Smith, Neil Gittoes
Medicine.2017; 45(9): 555. CrossRef
- Point-of-Care Peptide Hormone Production Enabled by Cell-Free Protein Synthesis

- Thyroid
- Hypoparathyroidism and Subclinical Hypothyroidism with Secondary Hemochromatosis
- Hyung Ki Jeong, Joon Hwan An, Hyoung Sang Kim, Eun Ae Cho, Min Gui Han, Jung Sik Moon, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2014;29(1):91-95. Published online March 14, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.1.91
- 4,453 View
- 46 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hemochromatosis is an inherited genetic disorder of iron metabolism which can also occur as a secondary result of iron-overload. It leads to organ damage such as cardiomyopathy, liver cirrhosis, hypogonadism, and diabetes. This paper discusses a case of secondary hemochromatosis associated with repeated transfusions, presenting as asymptomatic hypoparathyroidism and subclinical hypothyroidism with multiple organ involvement. The 29-year-old female, who had severe aplastic anemia, received multiple transfusions totaling approximately 1,400 units of red blood cells over 15 years. During her routine laboratory examination, hypocalcemia was detected with decreased intact parathyroid hormone and increased thyroid stimulating hormone. Serum ferritin, iron, and total iron binding capacity had increased to 27,583.03 ng/mL, 291 µg/dL, and 389 µg/dL, respectively. She had unusually bronze skin and computed tomography revealed iron deposition in the thyroid, liver, and heart. Multiorgan involvement as seen in this case is rare in hemochromatosis associated with secondary transfusions. To the best of the author's knowledge, this is the first case report in Korea of hypoparathyroidism and subclinical hypothyroidism due to iron deposition in the parathyroid and thyroid gland.
-
Citations
Citations to this article as recorded by- Hypocalcaemic cardiomyopathy: a description of two cases and a literature review
Martin Válek, Lenka Roblová, Ivan Raška, Dita Schaffelhoferová, Tomáš Paleček
ESC Heart Failure.2020; 7(3): 1291. CrossRef - Differential effects of Fe2+ and Fe3+ on osteoblasts and the effects of 1,25(OH)2D3, deferiprone and extracellular calcium on osteoblast viability under iron-overloaded conditions
Kornkamon Lertsuwan, Ketsaraporn Nammultriputtar, Supanan Nanthawuttiphan, Natnicha Tannop, Jarinthorn Teerapornpuntakit, Jirawan Thongbunchoo, Narattaphol Charoenphandhu, Gianpaolo Papaccio
PLOS ONE.2020; 15(5): e0234009. CrossRef - Apparent Resolution of Canine Primary Hypoparathyroidism with Immunosuppressive Treatment
J. Warland, B. Skelly, C. Knudsen, M. Herrtage
Journal of Veterinary Internal Medicine.2015; 29(1): 400. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Hypocalcaemic cardiomyopathy: a description of two cases and a literature review

- Polyglandular Autoimmune Syndrome Type III with Primary Hypoparathyroidism
- Sang Jin Kim, Sang-Yoon Kim, Han-Byul Kim, Hyukwon Chang, Ho-Chan Cho
- Endocrinol Metab. 2013;28(3):236-240. Published online September 13, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.3.236
- 4,008 View
- 34 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Polyglandular autoimmune syndrome is defined as multiple endocrine gland insufficiencies accompanied by autoimmune diseases of the endocrine and nonendocrine system. After Schmidt introduced a case of nontuberculosis adrenal gland dysfunction with thyroiditis in 1926, Neufeld defined polyglandular autoimmune syndrome by I, II, and III subtypes in 1980 by their presentation of occurrence age, heredity methods, relationship with human leukocyte antigen, and accompanying diseases. We report a case of a 32-year-old female with polyglandular autoimmune syndrome III accompanied by type 1 diabetes mellitus that was treated with insulin (36 units per day) for 11 years. She had insulin deficiency and Hashimoto thyroiditis as an autoimmune disorder. In addition, she had several features similar to Albright's hereditary osteodystrophy including short stature, truncal obesity, round face, short neck, low intelligence (full IQ 84), and decreased memory. Although Albright's hereditary osteodystrophy is morphological evidence of pseudohypoparathyroidism or pseudopseudohypoparathyroidism, she had primary hypoparathyroidism on laboratory results. Here, we report a case of polyglandular autoimmune syndrome III with type 1 diabetes mellitus, autoimmune thyroiditis, and primary hypoparathyroidism, accompanied by clinical features similar to Albright's hereditary osteodystrophy.
-
Citations
Citations to this article as recorded by- Autoimmune polyglandular syndrome type III associated with antineutrophil cytoplasmic autoantibody-mediated crescentic glomerulonephritis
Shiyuan Tian, Baofeng Xu, Ziwei Liu, Rui Liu
Medicine.2020; 99(7): e19179. CrossRef - Hypoparathyroidism: Genetics and Diagnosis
Michael Mannstadt, Luisella Cianferotti, Rachel I Gafni, Francesca Giusti, Elizabeth Helen Kemp, Christian A Koch, Kelly L Roszko, Liam Yao, Gordon H Guyatt, Rajesh V Thakker, Weibo Xia, Maria-Luisa Brandi
Journal of Bone and Mineral Research.2020; 37(12): 2615. CrossRef - A rare case of polyglandular autoimmune syndrome type IIIc with primary antibody failure
Adina Elena Stanciu, Florentina Sava, Gergely Toldi
Gynecological Endocrinology.2018; 34(4): 283. CrossRef - Autoimmune Polyendocrine Syndrome Type IIIC and Ankylosing Spondylitis; a Case Report
Ali Javinani, Hamid Reza Aghaei Meybodi, Ahmad Reza Jamshidi, Farhad Gharibdoost, Hoda Kavosi
Rheumatology Research.2016;[Epub] CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Autoimmune polyglandular syndrome type III associated with antineutrophil cytoplasmic autoantibody-mediated crescentic glomerulonephritis

- Reversible Heart Failure and Rhabdomyolysis Caused by Primary Hypoparathyroidism during Lactation.
- Kyongyeun Jung, Jeong Hyun Choi, Hee Jin Kim, Hyun Kyung Chung, Dohee Kim
- Endocrinol Metab. 2011;26(3):268-271. Published online September 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.3.268
- 1,684 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Hypocalcemia can be complicated, on rare occasions, by congestive heart failure and may also be associated with labor and lactation in some cases. Herein, we report a 30-year-old woman with hypocalcemia-induced heart failure secondary to primary idiopathic hypoparathyroidism precipitated by lactation. The patient presented with chest pain and paresthesia in both arms and legs during breast-feeding after her second delivery. She had severe hypocalcemia and low parathyroid hormone levels. Hypocalcemia-induced rhabdomyolysis further aggravated her hypocalcemia symptoms. The echocardiogram showed global hypokinesia with an ejection fraction of 47%. After calcium and vitamin D replacement, her symptoms and ventricular function improved. Hypocalcemia needs to be considered in patients with heart failure, because it is readily reversible. To the best of our knowledge, this is the first report of a patient with heart failure and rhabdomyolysis induced by primary hypoparathyroidism during lactation.

- A Case of Pseudohypoparathyroidism with Graves' Disease.
- Gil Woo Lee, Jae Hoon Kim, Kang Won Lee, Sa Il Kim, Sang Mo Hong, Dong Sun Kim, Woong Hwan Choi, You Hern Ahn, Tae Wha Kim
- Endocrinol Metab. 2010;25(3):221-225. Published online September 1, 2010
- DOI: https://doi.org/10.3803/EnM.2010.25.3.221
- 1,648 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Pseudohypoparathyroidism is a rare disease that is characterized by target cell resistance to the effects of parathyroid hormone and this disease is classified into various types depending on the phenotypic and biochemical findings. The patients with pseudohypoparathyroidism present with the clinical and biochemical features of hypoparathyroidism, but they have an increased serum level of parathyroid hormone. We experienced a case of pseudohypoparathyroidism in a 24 years old woman who had Graves' disease at that time. She had hypocalcemia, hyperphosphatemia, an elevated serum parathyroid hormone level and a normal urinary basal cyclic AMP(adenosine monophosphate) level. She also had a normal phenotypic appearance. Therefore, she was classified as suffering with pseudohypoparathyroidism type II. The clinical and laboratory abnormalities were improved by calcium supplementation in addition to vitamin D. To the best of our knowledge, this is the first case of pseudohypoparathyroidism combined with Graves' disease in Korea.

- A Case of Pseudohypoparathyroidism Worsened by Rhabdomyolysis.
- Won Jun Kim, Sin Je Moon, Hye Young Kim, Chang Beom Lee
- J Korean Endocr Soc. 2009;24(3):195-200. Published online September 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.3.195
- 1,981 View
- 25 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - The term pseudohypoparathyroidism describes a rare disorder characterized by resistance to the action of immunoreactive parathyroid hormone (PTH) in peripheral tissue rather than a deficiency of PTH. Patients present with tetany, spasm, hypocalcemia, hyperphosphatemia, and Albright's hereditary osteodystrophy (AHO). We present a case of symptomatic hypocalcemia due to pseudohypoparathyroidism aggravated by rhabdomyolysis. A 21-year-old man presented with tetany, AHO phenotypes and an ankle infection. Rhabdomyolysis was confirmed by marked elevation of serum creatine phosphokinase, more than 10 times above normal. Spasm was observed and the serum value of total calcium was as low as 3.7 mg/dL and that of phosphate was as high as 7.0 mg/dL, and the peak level of PTH was at 80.4 pg/mL. Although not surveyed by Ellsworth-Howard test and molecular study, it was classified as pseudohypoparathyroidism type 1a or 1c. The clinical and laboratory abnormalities were corrected by vitamin D in addition to calcium. The patient's mother, sister, and grandmother had AHO phenotypes without clinical and biochemical manifestations. To the best of our knowledge, this is the first case by maternal inheritance that AHO phenotypes appear for three generations of a family in Korea.
-
Citations
Citations to this article as recorded by- A Case of Pseudohypoparathyroidism with Graves' Disease
Gil Woo Lee, Jae Hoon Kim, Kang Won Lee, Sa Il Kim, Sang Mo Hong, Dong Sun Kim, Woong Hwan Choi, You Hern Ahn, Tae Wha Kim
Endocrinology and Metabolism.2010; 25(3): 221. CrossRef
- A Case of Pseudohypoparathyroidism with Graves' Disease

- A Case of Pseudopseudohypoparathyroidism with Normal Stature.
- Sae Rom Kim, Yun Jeong Doh, Hee Kyung Kim, Seong Su Moon, Ju Young Lee, Jae Han Jeon, Soo Won Kim, Bo Wan Kim, In Kyu Lee, Jung Guk Kim
- J Korean Endocr Soc. 2009;24(2):138-143. Published online June 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.2.138
- 1,917 View
- 32 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pseudopseudohypoparathyroidism (PPHP) is characterized by the phenotype of Albright hereditary osteodystrophy (AHO) alone without biochemical evidence of multihormone resistance, which is unlike pseudohypoparathyroidism. AHO is associated with characteristic developmental abnormalities that include a short stocky stature, a short neck, brachydactyly, a round face, central obesity, mental retardation and subcutaneous ossifications. AHO is an autosomal dominant disease that's caused by heterozygous inactivating mutations in the Gsalpha gene (GNAS1). Melanocortin-4 receptor (MC4R) is a hypothalamic Gs-coupled receptor that is thought to mediate the central effect of leptin on satiety. MC4R mutations cause morbid obesity starting in infancy, as well as an elevated leptin level. A 62 year old man with a height of 171.5 cm, a round face, a short neck, central obesity and brachydactyly had normal ranges of serum calcium, phosphorus and PTH and a normal Ellsworth-Howard test. GNAS1 gene analysis revealed substitution of alanine to cysteine in the 165 codon of exon 6 and substitution of alanine to cysteine in the 231 codon of exon 9. Two known SNPs (Cyt-1042Thy, Gua-719Ade) in the MC4R were detected in the patient. We report here on a case of PPHP and the patient had normal stature. We propose that MC4R may have contributed to the obesity & normal stature of this patient.
-
Citations
Citations to this article as recorded by- Polyglandular Autoimmune Syndrome Type III with Primary Hypoparathyroidism
Sang Jin Kim, Sang-Yoon Kim, Han-Byul Kim, Hyukwon Chang, Ho-Chan Cho
Endocrinology and Metabolism.2013; 28(3): 236. CrossRef
- Polyglandular Autoimmune Syndrome Type III with Primary Hypoparathyroidism

- A Case of Pseudohypoparathyroidism without Albright's Hereditary Osteodystrophy in an Adult.
- Yoonbum Lee, Jungmin Roh, Jeong seon Yoo, Jeongwoo Han, Jisun Nam, Minho Cho, Jongsuk Park, Chulwoo Ahn, Kyungrae Kim
- J Korean Endocr Soc. 2009;24(2):132-137. Published online June 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.2.132
- 1,780 View
- 25 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pseudohypoparathyroidism is a rare disease caused by resistance to parathyroid hormone, and is associated with typical clinical typical symptoms such as tetany and seizures, hypocalcemia, hyperphosphatemia and increased parathyroid hormone levels. Pseudohypoparathyroidism is classified to Type Ia, Ib, Ic and II according to the clinical and biochemical manifestations. Type Ia and Ic have morphological characteristics called Albright's hereditary osteodystrophy. Type Ib differs from type II for the pathogenesis. Type Ib may~receptors and type II may~ pathway, but the pathophysiology of type II is not clear yet. Administration of parathyroid hormone extract may help to distinguish between the two types. We report a case of a pseudohypoparathyroidism type Ib or II patient who had tetany, hypocalcemia and hyperphosphatemia with normal morphologic features.
-
Citations
Citations to this article as recorded by- A Case of Pseudohypoparathyroidism with Graves' Disease
Gil Woo Lee, Jae Hoon Kim, Kang Won Lee, Sa Il Kim, Sang Mo Hong, Dong Sun Kim, Woong Hwan Choi, You Hern Ahn, Tae Wha Kim
Endocrinology and Metabolism.2010; 25(3): 221. CrossRef
- A Case of Pseudohypoparathyroidism with Graves' Disease

- A Case of the Milk-alkali Syndrome During Management of Idiopathic Hypoparathyroidism.
- Yong Wan Park, Sung Rae Kim, Jung Min Lee, Seong Hun Kim, Sang Woo Han, Soon Jib Yoo, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- J Korean Endocr Soc. 2004;19(4):439-445. Published online August 1, 2004
- 1,111 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Idiopathic hypoparathyroidism is a relatively rare disease characterized by hypocalcemia and hyperphosphatemia: this is due to a deficiency or a sereretory disorder of the parathyroid hormone without any prior operation nor underlying medical disoder. Calcium carbonate and vitamin D substitution are generally considered as the mainstay of therapy, but these treatments can cause hypercalcemia and hypercalciuria. Persistent ingestion of large amount of calcium carbonate can cause milk-alkali syndrome that is characterized by hypercalcemia, metabolic alkalosis and renal failure. Once a patient is diagnosed with milk-alkali syndrome, withdrawal of calcium carbonate and vitamin D is essential and treatment with saline diuresis and furosemide is the usually effective. In treatmenf of hypoparathyroidism with calcium carbonate and vitamin D substitution, evaluation of serum calcium and urinary calcium excretion is essential to avoid hypercalcemia and ypercalciuria. We concluded that during treatment with calcium carbonate and vitamin D substitution for patients with idiopathic hypoparathyroidism, they should have carefully laboratory monitoring, and they should be made aware of the circumstances influencing calcium metabolism

- A Case of Pseudopseudohypoparathyroidism with Partial Empty Sella.
- Jang Hyun Koh, Yeon Lee, Joung Wook Choi, Tae Won Hong, Mi Jin Kim, Young Goo Shin, Choon Hee Chung
- J Korean Endocr Soc. 2004;19(4):433-438. Published online August 1, 2004
- 1,048 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Pseudohypoparathyroidism (PHP) is a rare endocrine syndrome, which is characterized by Albright's hereditary osteodystrophy (AHO). Pseudopseudohypoparathyroidism (PPHP) presents with AHO features, but does not show clinical symptoms or the same laboratory finding as hypoparathyroidism. A 54 aged woman visited our department with lower abdominal pain. She had a history of a total hysterectomy due to persistent uterine bleeding 30 years previously. She showed abnormal physical findings, including a round face, short stature and brachydactyly. Her hormonal data were within normal limits, as follows: PTH 40.72 pg/mL, calcium 8.6 mg/dL, phosphorus 4.0 mg/dL and 24 hour urine cAMP 3.2 nmol/mg. On a pituitary challenge test, the basal levels and response rates of FSH and LH were low, and a sella CT scan showed partially empty sella. Herein is reported a case of PPHP, with partial empty sella, with a review of the literature


 KES
KES

 First
First Prev
Prev



