Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Treatment of Hypoparathyroidism by Re-Establishing the Effects of Parathyroid Hormone
- Lars Rejnmark
- Endocrinol Metab. 2024;39(2):262-266. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1916
- 1,174 View
- 63 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
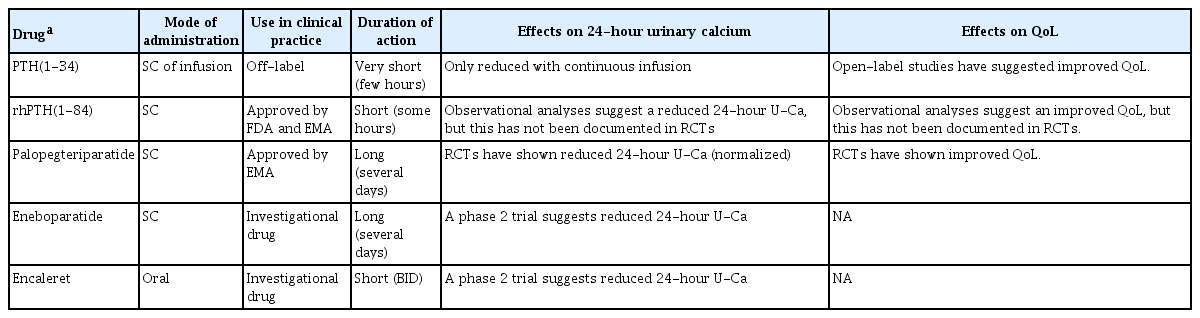
ePub - The conventional treatment of hypoparathyroidism (HypoPT) includes active vitamin D and calcium. Despite normalization of calcium levels, the conventional treatment is associated with fluctuations in calcium levels, hypercalciuria, renal impairment, and decreased quality of life (QoL). Replacement therapy with parathyroid hormone (PTH)(1-84) is an option in some countries. However, convincing beneficial effects have not been demonstrated, which may be due to the short duration of action of this treatment. Recently, palopegteriparatide (also known as TransCon PTH) has been marketed in Europe and is expected also to be approved in other countries. Palopegteriparatide is a prodrug with sustained release of PTH(1-34) designed to provide stable physiological PTH levels for 24 hours/day. A phase 3 study demonstrated maintenance of normocalcemia in patients with chronic HypoPT, with no need for conventional therapy. Furthermore, this treatment lowers urinary calcium and improves QoL. Another long-acting PTH analog with effects on the parathyroid hormone receptor (eneboparatide) is currently being tested in a phase 3 trial. Furthermore, the treatment of autosomal dominant hypocalcemia type 1 with a calcilytic (encaleret) is also being tested. All in all, improved treatment options are on the way that will likely take the treatment of HypoPT to the next level.

- Adrenal gland
- Effects of Altered Calcium Metabolism on Cardiac Parameters in Primary Aldosteronism
- Jung Soo Lim, Namki Hong, Sungha Park, Sung Il Park, Young Taik Oh, Min Heui Yu, Pil Yong Lim, Yumie Rhee
- Endocrinol Metab. 2018;33(4):485-492. Published online November 30, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.4.485
- 4,096 View
- 43 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Increasing evidence supports interplay between aldosterone and parathyroid hormone (PTH), which may aggravate cardiovascular complications in various heart diseases. Negative structural cardiovascular remodeling by primary aldosteronism (PA) is also suspected to be associated with changes in calcium levels. However, to date, few clinical studies have examined how changes in calcium and PTH levels influence cardiovascular outcomes in PA patients. Therefore, we investigated the impact of altered calcium homeostasis caused by excessive aldosterone on cardiovascular parameters in patients with PA.
Methods Forty-two patients (mean age 48.8±10.9 years; 1:1, male:female) whose plasma aldosterone concentration/plasma renin activity ratio was more than 30 were selected among those who had visited Severance Hospital from 2010 to 2014. All patients underwent adrenal venous sampling with complete access to both adrenal veins.
Results The prevalence of unilateral adrenal adenoma (54.8%) was similar to that of bilateral adrenal hyperplasia. Mean serum corrected calcium level was 8.9±0.3 mg/dL (range, 8.3 to 9.9). The corrected calcium level had a negative linear correlation with left ventricular end-diastolic diameter (LVEDD, ρ=−0.424,
P =0.031). Moreover, multivariable regression analysis showed that the corrected calcium level was marginally associated with the LVEDD and corrected QT (QTc) interval (β=−0.366,P =0.068 and β=−0.252,P =0.070, respectively).Conclusion Aldosterone-mediated hypercalciuria and subsequent hypocalcemia may be partly involved in the development of cardiac remodeling as well as a prolonged QTc interval, in subjects with PA, thereby triggering deleterious effects on target organs additively.
-
Citations
Citations to this article as recorded by- Bone and mineral metabolism in patients with primary aldosteronism: A systematic review and meta-analysis
Anning Wang, Yuhan Wang, Hongzhou Liu, Xiaodong Hu, Jiefei Li, Huaijin Xu, Zhimei Nie, Lingjing Zhang, Zhaohui Lyu
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Bone and mineral metabolism in patients with primary aldosteronism: A systematic review and meta-analysis

- A Case of Parathyroid Apoplexy of Primary Hyperparathyroidism Presenting as Auditory Hallucinations Accompanied with Hypocalcemia.
- Eon Ju Jeon, Ji Yun Jeong, Jung Guk Kim
- Endocrinol Metab. 2012;27(2):163-168. Published online June 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.2.163
- 22,402 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - The natural history of primary hyperparathyroidism, due to parathyroid adenoma, is unknown. Furthermore, spontaneous resolution of parathyroid necrosis or hemorrhage is rare and usually asymptomatic. Here, we report a case of parathyroid apoplexy of primary hyperparathyroidism, presenting as auditory hallucinations, accompanied with hypocalcemia. A 39-year-old man who was incidentally diagnosed with primary hyperparathyroidism, and waiting surgery for parathyroidectomy presented to psychiatric service with auditory hallucinations. He developed tetany, while taking psychiatric drugs. On a follow-up investigation, his serum calcium level fell from 11.8 to 5.8 mg/dL. His intact parathyroid hormone level also decreased from 1,017 pg/mL to 71.1 pg/mL. The parathyroid apoplexy was confirmed after a surgical removal of the infarcted adenoma. The auditory hallucinations disappeared, and serum calcium level was returned to within the normal range.

- Reversible Heart Failure and Rhabdomyolysis Caused by Primary Hypoparathyroidism during Lactation.
- Kyongyeun Jung, Jeong Hyun Choi, Hee Jin Kim, Hyun Kyung Chung, Dohee Kim
- Endocrinol Metab. 2011;26(3):268-271. Published online September 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.3.268
- 1,686 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Hypocalcemia can be complicated, on rare occasions, by congestive heart failure and may also be associated with labor and lactation in some cases. Herein, we report a 30-year-old woman with hypocalcemia-induced heart failure secondary to primary idiopathic hypoparathyroidism precipitated by lactation. The patient presented with chest pain and paresthesia in both arms and legs during breast-feeding after her second delivery. She had severe hypocalcemia and low parathyroid hormone levels. Hypocalcemia-induced rhabdomyolysis further aggravated her hypocalcemia symptoms. The echocardiogram showed global hypokinesia with an ejection fraction of 47%. After calcium and vitamin D replacement, her symptoms and ventricular function improved. Hypocalcemia needs to be considered in patients with heart failure, because it is readily reversible. To the best of our knowledge, this is the first report of a patient with heart failure and rhabdomyolysis induced by primary hypoparathyroidism during lactation.

- A Case of Pseudohypoparathyroidism Worsened by Rhabdomyolysis.
- Won Jun Kim, Sin Je Moon, Hye Young Kim, Chang Beom Lee
- J Korean Endocr Soc. 2009;24(3):195-200. Published online September 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.3.195
- 1,985 View
- 25 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - The term pseudohypoparathyroidism describes a rare disorder characterized by resistance to the action of immunoreactive parathyroid hormone (PTH) in peripheral tissue rather than a deficiency of PTH. Patients present with tetany, spasm, hypocalcemia, hyperphosphatemia, and Albright's hereditary osteodystrophy (AHO). We present a case of symptomatic hypocalcemia due to pseudohypoparathyroidism aggravated by rhabdomyolysis. A 21-year-old man presented with tetany, AHO phenotypes and an ankle infection. Rhabdomyolysis was confirmed by marked elevation of serum creatine phosphokinase, more than 10 times above normal. Spasm was observed and the serum value of total calcium was as low as 3.7 mg/dL and that of phosphate was as high as 7.0 mg/dL, and the peak level of PTH was at 80.4 pg/mL. Although not surveyed by Ellsworth-Howard test and molecular study, it was classified as pseudohypoparathyroidism type 1a or 1c. The clinical and laboratory abnormalities were corrected by vitamin D in addition to calcium. The patient's mother, sister, and grandmother had AHO phenotypes without clinical and biochemical manifestations. To the best of our knowledge, this is the first case by maternal inheritance that AHO phenotypes appear for three generations of a family in Korea.
-
Citations
Citations to this article as recorded by- A Case of Pseudohypoparathyroidism with Graves' Disease
Gil Woo Lee, Jae Hoon Kim, Kang Won Lee, Sa Il Kim, Sang Mo Hong, Dong Sun Kim, Woong Hwan Choi, You Hern Ahn, Tae Wha Kim
Endocrinology and Metabolism.2010; 25(3): 221. CrossRef
- A Case of Pseudohypoparathyroidism with Graves' Disease

- A Case of Pseudohypoparathyroidism without Albright's Hereditary Osteodystrophy in an Adult.
- Yoonbum Lee, Jungmin Roh, Jeong seon Yoo, Jeongwoo Han, Jisun Nam, Minho Cho, Jongsuk Park, Chulwoo Ahn, Kyungrae Kim
- J Korean Endocr Soc. 2009;24(2):132-137. Published online June 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.2.132
- 1,785 View
- 25 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pseudohypoparathyroidism is a rare disease caused by resistance to parathyroid hormone, and is associated with typical clinical typical symptoms such as tetany and seizures, hypocalcemia, hyperphosphatemia and increased parathyroid hormone levels. Pseudohypoparathyroidism is classified to Type Ia, Ib, Ic and II according to the clinical and biochemical manifestations. Type Ia and Ic have morphological characteristics called Albright's hereditary osteodystrophy. Type Ib differs from type II for the pathogenesis. Type Ib may~receptors and type II may~ pathway, but the pathophysiology of type II is not clear yet. Administration of parathyroid hormone extract may help to distinguish between the two types. We report a case of a pseudohypoparathyroidism type Ib or II patient who had tetany, hypocalcemia and hyperphosphatemia with normal morphologic features.
-
Citations
Citations to this article as recorded by- A Case of Pseudohypoparathyroidism with Graves' Disease
Gil Woo Lee, Jae Hoon Kim, Kang Won Lee, Sa Il Kim, Sang Mo Hong, Dong Sun Kim, Woong Hwan Choi, You Hern Ahn, Tae Wha Kim
Endocrinology and Metabolism.2010; 25(3): 221. CrossRef
- A Case of Pseudohypoparathyroidism with Graves' Disease


 KES
KES

 First
First Prev
Prev



