Search
- Page Path
- HOME > Search
Original Article
- Diabetes, obesity and metabolism
- Effects of an Electronic Medical Records-Linked Diabetes Self-Management System on Treatment Targets in Real Clinical Practice: Retrospective, Observational Cohort Study
- So Jung Yang, Sun-Young Lim, Yoon Hee Choi, Jin Hee Lee, Kun-Ho Yoon
- Endocrinol Metab. 2024;39(2):364-374. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1878

- 404 View
- 8 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study evaluated the effects of a mobile diabetes management program called “iCareD” (College of Medicine, The Catholic University of Korea) which was integrated into the hospital’s electronic medical records system to minimize the workload of the healthcare team in the real clinical practice setting.
Methods
In this retrospective observational study, we recruited 308 patients. We categorized these patients based on their compliance regarding their use of the iCareD program at home; compliance was determined through self-monitored blood glucose inputs and message subscription rates. We analyzed changes in the ABC (hemoglobin A1c, blood pressure, and low-density lipoprotein cholesterol) levels from the baseline to 12 months thereafter, based on the patients’ iCareD usage patterns.
Results
The patients comprised 92 (30%) non-users, 170 (55%) poor-compliance users, and 46 (15%) good-compliance users; the ABC target achievement rate showed prominent changes in good-compliance groups from baseline to 12 months (10.9% vs. 23.9%, P<0.05), whereas no significant changes were observed for poor-compliance users and non-users (13.5% vs. 18.8%, P=0.106; 20.7% vs. 14.1%, P=0.201; respectively).
Conclusion
Implementing the iCareD can improve the ABC levels of patients with diabetes with minimal efforts of the healthcare team in real clinical settings. However, the improvement of patients’ compliance concerning the use of the system without the vigorous intervention of the healthcare team needs to be solved in the future.

Review Article
- Diabetes, obesity and metabolism
- Initial Combination Therapy in Type 2 Diabetes
- Ji Yoon Kim, Nam Hoon Kim
- Endocrinol Metab. 2024;39(1):23-32. Published online November 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1816
- 2,041 View
- 245 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
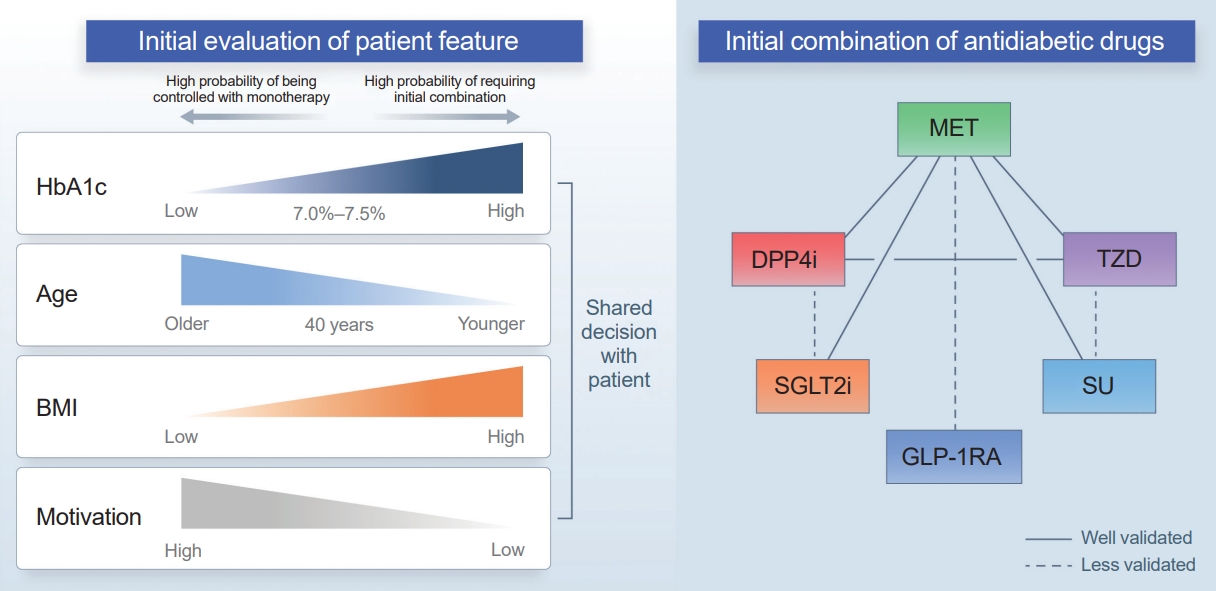
ePub - Type 2 diabetes (T2D) is a progressive disease in which it is challenging to achieve long-term durable glycemic control. However, intensive glycemic control is crucial for preventing diabetes-related complications. Previous studies showed that monotherapy with a stepwise add-on approach was seldom effective for long-term durable glycemic control. Combination therapy, which refers to the use of two or more drugs to control hyperglycemia, has multiple benefits, including the ability to target a variety of pathophysiological processes underlying hyperglycemia. In clinical trials, initial combination therapy showed better glycemic control than monotherapy or a stepwise approach. Emerging evidence indicates that initial combination therapy is associated with preserved β-cell function and fewer complications in T2D. However, cost-effectiveness and adverse events with combination therapy are issues that should be considered. Therefore, initial combination therapy is an important option for patients with T2D that clinicians should consider with a view toward balancing benefits and potential harms. In this review, we summarize the literature addressing initial combination therapy in T2D, and we suggest optimal strategies based on clinical situations and patient characteristics.

Original Articles
- Diabetes, obesity and metabolism
- Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
- Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
- Endocrinol Metab. 2023;38(5):538-544. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1730
- 1,920 View
- 109 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
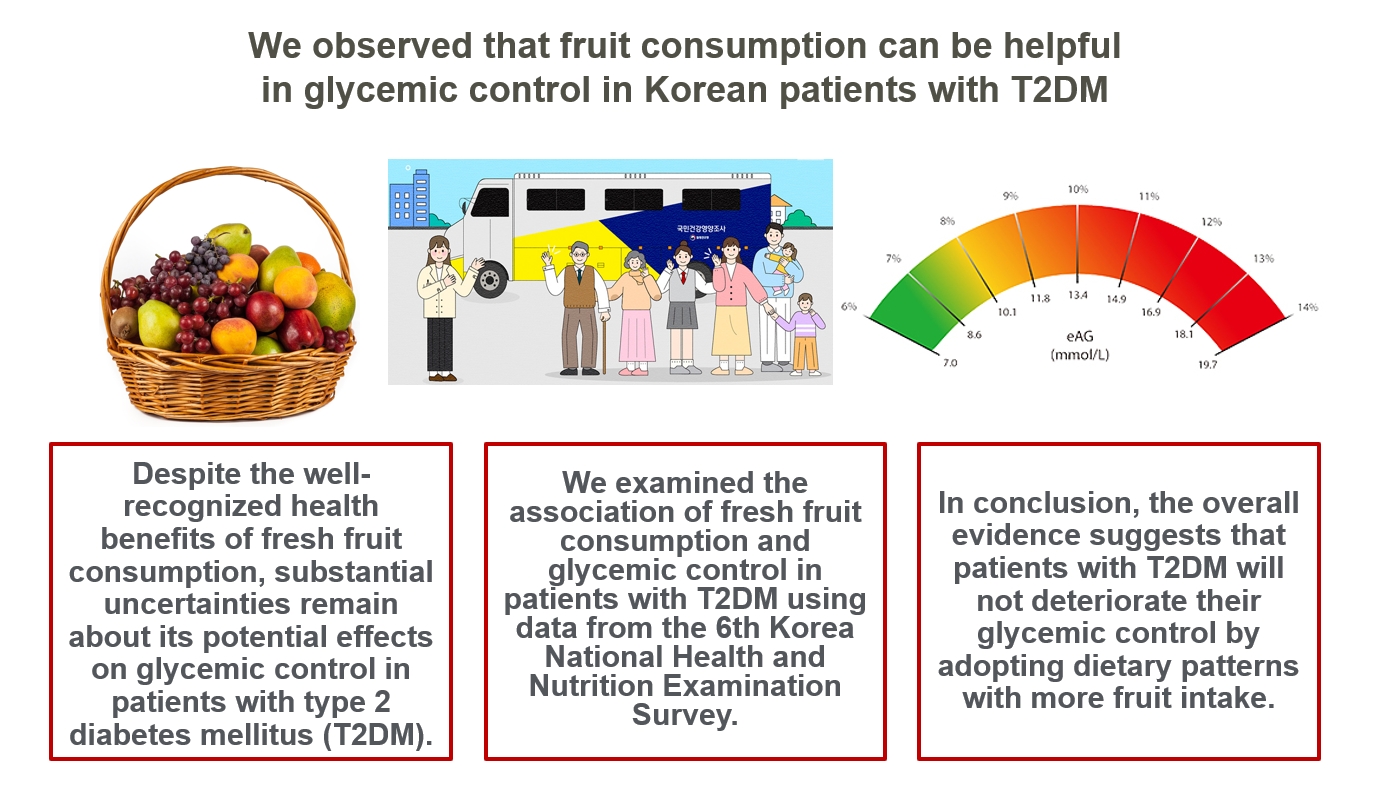
Despite the well-recognized health benefits of fresh fruit consumption, there is still substantial uncertainty about its potential effects on glycemic control in patients with type 2 diabetes mellitus (T2DM).
Methods
We examined the association of fresh fruit consumption and glycemic control in patients with T2DM using data from the 6th Korea National Health and Nutrition Examination Survey. The study sample was divided into three groups based on weekly fruit consumption frequency for the analysis.
Results
Patients with the highest fruit intake were older than those in the other two groups, and women were more likely to consume fruits in general. Being a current smoker and weekly alcohol intake also showed negative correlations according to the fruit intake tertiles. Fruit consumption was positively correlated with better hemoglobin A1c (HbA1c) levels. Moreover, patients in the highest tertile of fruit intake were 3.48 times more likely to be in good glycemic control defined as HbA1c <7%.
Conclusion
We observed that fruit consumption can be helpful in glycemic control in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- The Relationship between Alcohol Consumption and Diabetes in Korean Adults
Gi Tae Kim, Jae Woong Sull
Biomedical Science Letters.2023; 29(3): 159. CrossRef
- The Relationship between Alcohol Consumption and Diabetes in Korean Adults

- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes
- Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
- Endocrinol Metab. 2022;37(4):641-651. Published online August 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1501
- 6,162 View
- 165 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The prevalence of young-onset diabetes (YOD) has been increasing worldwide. As the incidence of YOD increases, it is necessary to determine the characteristics of YOD and the factors that influence its development and associated complications.
Methods
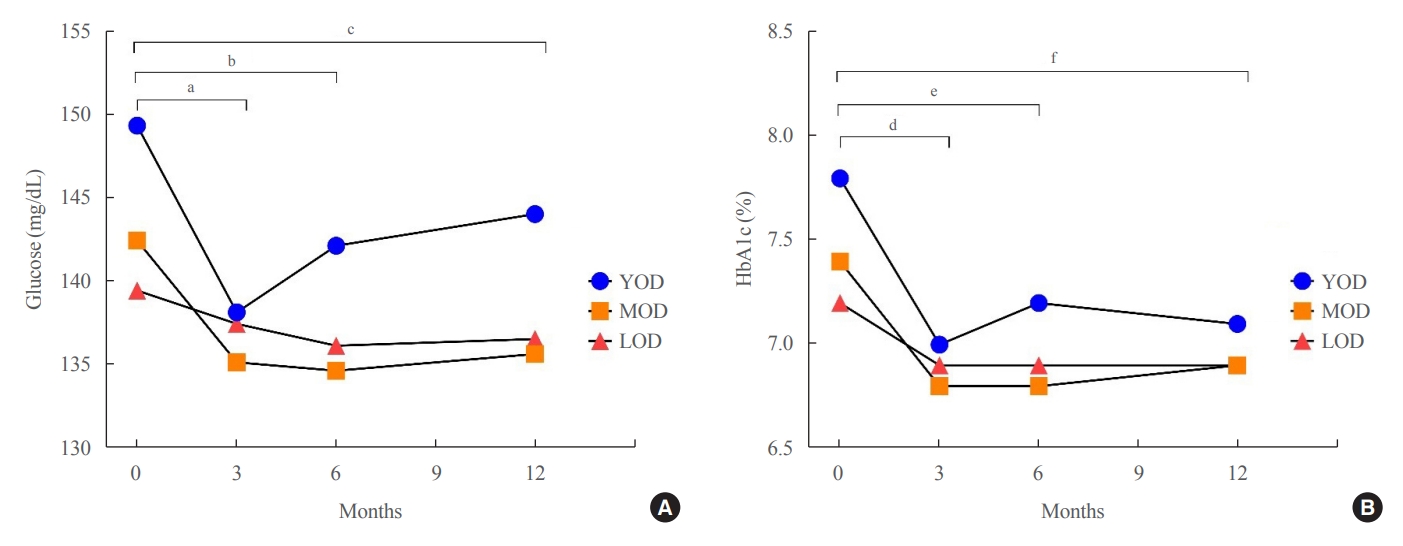
In this retrospective study, we recruited patients who were diagnosed with type 2 diabetes mellitus between June 2001 and December 2021 at a tertiary hospital. The study population was categorized according to age: YOD (age <40 years), middle-age-onset diabetes (MOD, 40≤ age <65 years), and late-onset diabetes (LOD, age ≥65 years). We examined trends in glycemic control by analyzing fasting glucose levels during the first year in each age group. A Cox proportional-hazards model was used to determine the relative risk of developing complications according to glycemic control trends.
Results
The fasting glucose level at the time of diagnosis was highest in the YOD group (YOD 149±65 mg/dL; MOD 143±54 mg/dL; and LOD 140±55 mg/dL; p=0.009). In the YOD group, glucose levels decreased at 3 months, but increased by 12 months. YOD patients and those with poor glycemic control in the first year were at a higher risk of developing complications, whereas the risk in patients with LOD was not statistically significant.
Conclusion
YOD patients had higher glucose levels at diagnosis, and their glycemic control was poorly maintained. As poor glycemic control can influence the development of complications, especially in young patients, intensive treatment is necessary for patients with YOD. -
Citations
Citations to this article as recorded by- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes & Metabolism.2024; 50(1): 101505. CrossRef - Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study
Da Hea Seo, Mina Kim, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes Research and Clinical Practice.2024; 208: 111098. CrossRef - Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus
Hye-Sun Park, Yongin Cho, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, Suk Chon, Jeong-Taek Woo, Sei Hyun Baik, Kwan Woo Lee, So Hun Kim
Scientific Reports.2024;[Epub] CrossRef - Early onset type 2 diabetes mellitus: an update
Myrsini Strati, Melpomeni Moustaki, Theodora Psaltopoulou, Andromachi Vryonidou, Stavroula A. Paschou
Endocrine.2024;[Epub] CrossRef - Complications and Treatment of Early-Onset Type 2 Diabetes
Fahimeh Soheilipour, Naghmeh Abbasi Kasbi, Mahshid Imankhan, Delaram Eskandari
International Journal of Endocrinology and Metabolism.2023;[Epub] CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
Endocrinology and Metabolism.2022; 37(6): 945. CrossRef -
ISPAD
Clinical Practice Consensus Guidelines 2022: Management of the child, adolescent, and young adult with diabetes in limited resource settings
Anju Virmani, Stuart J. Brink, Angela Middlehurst, Fauzia Mohsin, Franco Giraudo, Archana Sarda, Sana Ajmal, Julia E. von Oettingen, Kuben Pillay, Supawadee Likitmaskul, Luis Eduardo Calliari, Maria E. Craig
Pediatric Diabetes.2022; 23(8): 1529. CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
May Thu Hla Aye, Sajid Adhi Raja, Vui Heng Chong
Endocrinology and Metabolism.2022; 37(6): 943. CrossRef
- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study

Brief Report
- Diabetes, Obesity and Metabolism
- Identification of Healthy and Unhealthy Lifestyles by a Wearable Activity Tracker in Type 2 Diabetes: A Machine Learning-Based Analysis
- Kyoung Jin Kim, Jung-Been Lee, Jimi Choi, Ju Yeon Seo, Ji Won Yeom, Chul-Hyun Cho, Jae Hyun Bae, Sin Gon Kim, Heon-Jeong Lee, Nam Hoon Kim
- Endocrinol Metab. 2022;37(3):547-551. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1479

- 2,950 View
- 124 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Lifestyle is a critical aspect of diabetes management. We aimed to define a healthy lifestyle using objectively measured parameters obtained from a wearable activity tracker (Fitbit) in patients with type 2 diabetes. This prospective observational study included 24 patients (mean age, 46.8 years) with type 2 diabetes. Expectation–maximization clustering analysis produced two groups: A (n=9) and B (n=15). Group A had a higher daily step count, lower resting heart rate, longer sleep duration, and lower mean time differences in going to sleep and waking up than group B. A Shapley additive explanation summary analysis indicated that sleep-related factors were key elements for clustering. The mean hemoglobin A1c level was 0.3 percentage points lower at the end of follow-up in group A than in group B. Factors related to regular sleep patterns could be possible determinants of lifestyle clustering in patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Rethink nutritional management in chronic kidney disease care
Fangyue Chen, Krit Pongpirul
Frontiers in Nephrology.2023;[Epub] CrossRef - Effect of a Wearable Device–Based Physical Activity Intervention in North Korean Refugees: Pilot Randomized Controlled Trial
Ji Yoon Kim, Kyoung Jin Kim, Kyeong Jin Kim, Jimi Choi, Jinhee Seo, Jung-Been Lee, Jae Hyun Bae, Nam Hoon Kim, Hee Young Kim, Soo-Kyung Lee, Sin Gon Kim
Journal of Medical Internet Research.2023; 25: e45975. CrossRef
- Rethink nutritional management in chronic kidney disease care

Original Article
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Risk and Risk Factors for Postpartum Type 2 Diabetes Mellitus in Women with Gestational Diabetes: A Korean Nationwide Cohort Study
- Mi Jin Choi, Jimi Choi, Chae Weon Chung
- Endocrinol Metab. 2022;37(1):112-123. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1276

- 4,089 View
- 171 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are differences in risk and risk factor findings of postpartum type 2 diabetes mellitus (T2DM) after gestational diabetes depending on study design and subjects of previous studies. This study aimed to assess these risk and risk factors more accurately through a population-based study to provide basic data for prevention strategies.
Methods
This open retrospective cohort included data of 419,101 women with gestational diabetes and matched 1,228,802 control women who delivered between 2004 and 2016 from the South Korea National Health Information Database of the National Health Insurance Service. Following 14 (median 5.9) years of follow-up, the incidence and hazard ratio (HR) of postpartum T2DM were evaluated using Kaplan-Meier curves and Cox proportional regression models.
Results
The incidence and HR of postpartum T2DM in women with gestational diabetes (compared to women without gestational diabetes) after the 14-year follow-up was 21.3% and 2.78 (95% confidence interval [CI], 2.74 to 2.82), respectively. Comorbid obesity (body mass index [BMI] ≥25 kg/m2) increased postpartum T2DM risk 7.59 times (95% CI, 7.33 to 7.86). Significant risk factors for postpartum T2DM were fasting glucose level, BMI, age, family history of diabetes, hypertension, and insulin use during pregnancy.
Conclusion
This population-based study showed higher postpartum T2DM risk in women with gestational diabetes than in those without, which was further increased by comorbid obesity. BMI and fasting glucose level were important postpartum risk factors. The management of obesity and glycemic control may be important strategies to prevent the incidence of diabetes after delivery. -
Citations
Citations to this article as recorded by- Antenatal factors and risk of postpartum hyperglycemia in women with gestational diabetes mellitus: A central India prospective cohort study
Nilajkumar Bagde, Madhuri Bagde, Vijayalakshmi Shanbhag, Pragati Trigunait, Nagma Sheikh, Sarita Agrawal
Journal of Family Medicine and Primary Care.2024; 13(1): 59. CrossRef - Integration of nutrigenomics, melatonin, serotonin and inflammatory cytokines in the pathophysiology of pregnancy-specific urinary incontinence in women with gestational diabetes mellitus
Danielle Cristina Honorio França, Eduardo Luzía França, Luis Sobrevia, Angélica Mércia Pascon Barbosa, Adenilda Cristina Honorio-França, Marilza Vieira Cunha Rudge
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2023; 1869(6): 166737. CrossRef - Risk factors associated with early postpartum glucose intolerance in women with a history of gestational diabetes mellitus: a systematic review and meta-analysis
Zhe Liu, Qianghuizi Zhang, Leyang Liu, Weiwei Liu
Endocrine.2023; 82(3): 498. CrossRef
- Antenatal factors and risk of postpartum hyperglycemia in women with gestational diabetes mellitus: A central India prospective cohort study

Randomized Controlled Trial
- The Effect of Intensive Education on Glycemic Control in Type 2 Diabetic Patients.
- Youn Wook Lee, Won Sun Hwang, Sun Jung Choe, Dong Hun Lee, Doh Hyun Kim, Eun Hee Lee, Eun Gyoung Hong, Hye Lim Noh, Yoon Sok Chung, Kwan Woo Lee, Hyeon Man Kim
- J Korean Endocr Soc. 2003;18(1):63-72. Published online February 1, 2003
- 1,313 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
To this date, efforts to develop effective methods for the education of diabetic patients have been limited. The important goal of self-management and weight control for diabetic treatment can not be attained without long and intensive period of education. This study was undertaken to assess the effectiveness of an intensive educational program, of behavior and diet control, which was carried out on subjects with type 2 diabetes, on an out-patient basis. We compared the effectiveness of an intensive education programme with that of a conventional education programme for the self-management of type 2 diabetic patients. METHODS: Subjects with type 2 diabetes were randomly selected, and allocated to one of two groups. One group received a conventional education programme of self-management(the CE group), and the second group received an intensive education programmes for three months, after which the effectiveness of the programmes were evaluated. RESULTS: 1) The levels of fasting blood sugar(FBS), postprandial 2 hour blood sugar(PP2h) and HbA1c were significantly lowered in both groups following the intervention(p<0.05). In the IE group, the FBS declined from 12.4nmol/L to 7.7nmol/L, PP2h declined from 20.3nmol/L to 10.9nmol/L, and the HbA1c showed a similar decline from 9.4 to 7.0% after intervention(p<0.05). In the CE group, the FBS declined from 10.9 to 9.4nmol/l, the PP2h decreased from 17.1 to 14.6 nmol/l, and the HbA1c also decreased from 8.5 to 7.3% after intervention(p<0.05). The decrease in the FBS and HbA1c following the educational intervention was more pronounced in the IE group than the CE group (p<0.05). 2) The effectiveness of the education programmes in promoting appropriate dietary behavior in the diabetic subjects was assessed by a scoring system in three parts: a regularity score, a balance score and an attitude score. From a comparative study of the three scores, the patients attitudes were observed to be much improved in both the groups following the intervention compared to before the programmes, but the balance and total scores were significantly higher in the IE group than the CE group(p<0.05). CONCLUSION: We can conclude that the intensive diabetic education programme is more effective than a conventional programme, not only in improving the patients' levels of glucose, HbAlc, and dietary score, but also the diabetic patients self-control abilities, promoting behavioral change, and prompting problem solving capabilities in respect to the everyday problems that they have to face throughout their lives.


 KES
KES

 First
First Prev
Prev



