Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- Glucagon-Like Peptide-1 Based Therapies: A New Horizon in Obesity Management
- Jang Won Son, Soo Lim
- Endocrinol Metab. 2024;39(2):206-221. Published online April 16, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1940
- 1,345 View
- 101 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
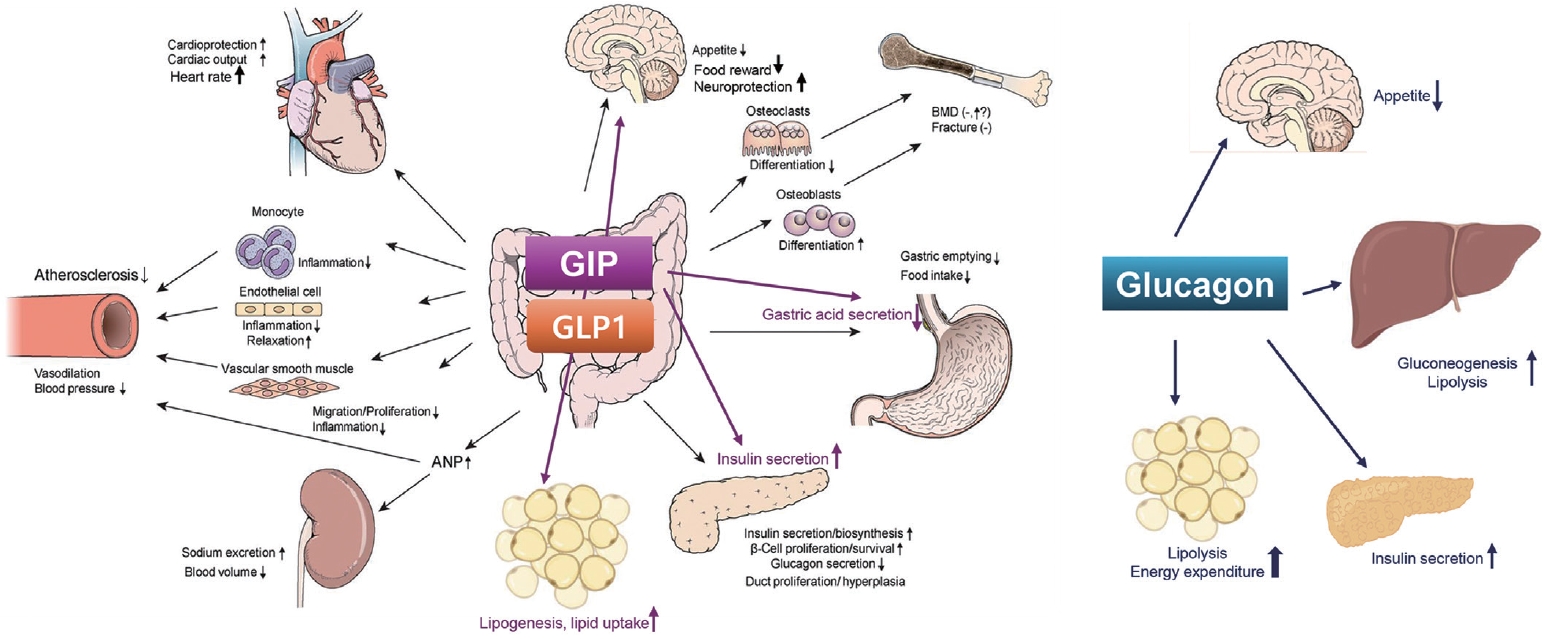
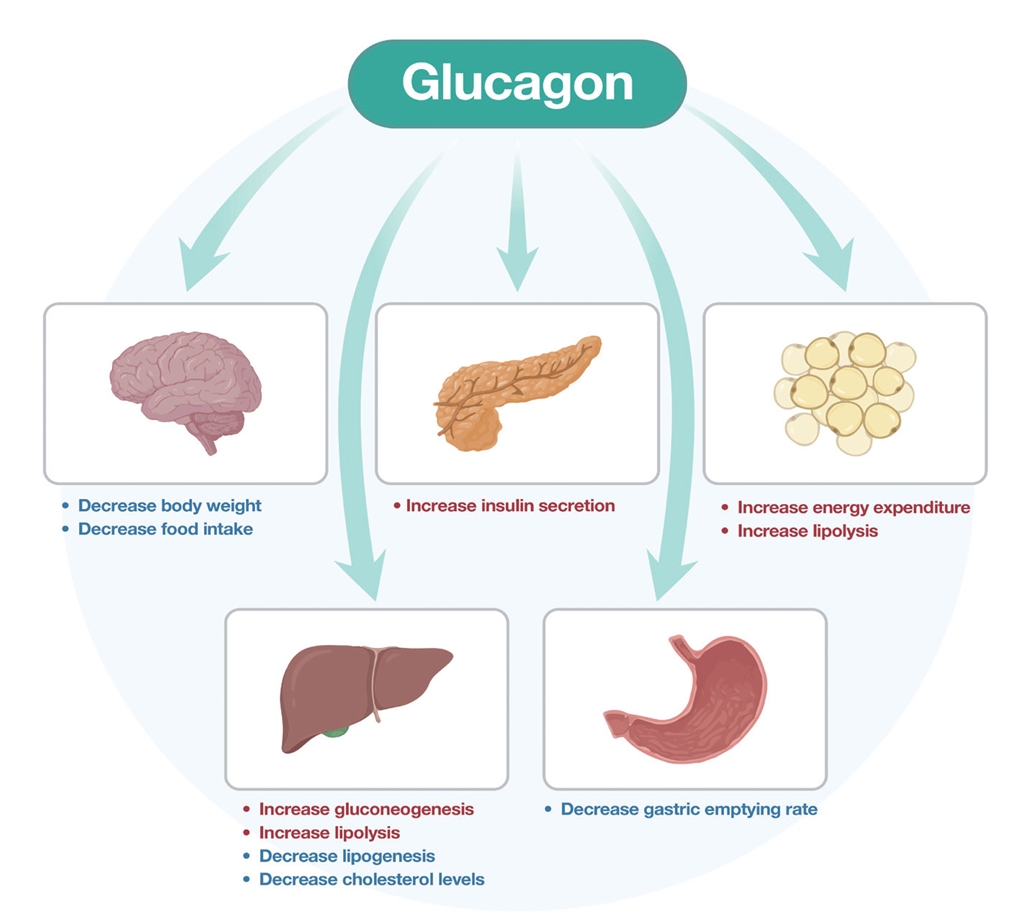
ePub - Obesity is a significant risk factor for health issues like type 2 diabetes and cardiovascular disease. It often proves resistant to traditional lifestyle interventions, prompting a need for more precise therapeutic strategies. This has led to a focus on signaling pathways and neuroendocrine mechanisms to develop targeted obesity treatments. Recent developments in obesity management have been revolutionized by introducing novel glucagon-like peptide-1 (GLP-1) based drugs, such as semaglutide and tirzepatide. These drugs are part of an emerging class of nutrient-stimulated hormone-based therapeutics, acting as incretin mimetics to target G-protein–coupled receptors like GLP-1, glucose-dependent insulinotropic polypeptide (GIP), and glucagon. These receptors are vital in regulating body fat and energy balance. The development of multiagonists, including GLP-1–glucagon and GIP–GLP-1–glucagon receptor agonists, especially with the potential for glucagon receptor activation, marks a significant advancement in the field. This review covers the development and clinical efficacy of various GLP-1-based therapeutics, exploring the challenges and future directions in obesity management.

- Diabetes, obesity and metabolism
- Glucagon: Physiological and Pharmacological Functions and Pathophysiological Significance in Type 2 Diabetes
- Tadahiro Kitamura
- Endocrinol Metab. 2024;39(1):33-39. Published online February 22, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1911
- 1,536 View
- 129 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
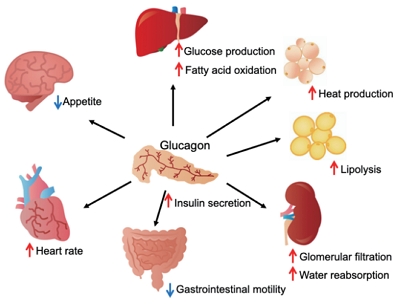
ePub - Glucagon has many functions, including the promotion of hepatic glucose production, fatty acid oxidation, thermogenesis, energy consumption, lipolysis, and myocardial contraction, as well as the suppression of lipogenesis, appetite, and gastrointestinal motility. However, it remains unclear which of these functions are physiological and which are pharmacological. Research on glucagon has lagged behind research on insulin because cross-reactivity with glucagon-related peptides in plasma has hindered the development of an accurate measurement system for glucagon. We recently developed a new glucagon sandwich enzyme-linked immunosorbent assay (ELISA) that is more specific and more sensitive to glucagon than the currently used measurement systems. The new sandwich ELISA is expected to contribute to personalized medicine for diabetes through its use in clinical examinations, the diagnosis of the pathophysiological condition of individual diabetes patients, and the choice of a treatment strategy. Efforts are continuing to develop glucagon/glucagon-like peptide-1 receptor dual agonists to improve obesity and fatty liver by enhancing glucagon’s appetite-suppressing and lipolysis- and thermogenesis-promoting effects. Thus, glucagon is expected to be applied to new diagnostic and therapeutic strategies based on a more accurate understanding of its functions.

- Diabetes, obesity and metabolism
- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update
- Agnieszka Jakubowska, Carel W. le Roux, Adie Viljoen
- Endocrinol Metab. 2024;39(1):12-22. Published online February 14, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1942
- 2,775 View
- 217 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Obesity is the fifth leading risk factor for global deaths with numbers continuing to increase worldwide. In the last 20 years, the emergence of pharmacological treatments for obesity based on gastrointestinal hormones has transformed the therapeutic landscape. The successful development of glucagon-like peptide-1 (GLP-1) receptor agonists, followed by the synergistic combined effect of glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists achieved remarkable weight loss and glycemic control in those with the diseases of obesity and type 2 diabetes. The multiple cardiometabolic benefits include improving glycemic control, lipid profiles, blood pressure, inflammation, and hepatic steatosis. The 2023 phase 2 double-blind, randomized controlled trial evaluating a GLP-1/GIP/glucagon receptor triagonist (retatrutide) in patients with the disease of obesity reported 24.2% weight loss at 48 weeks with 12 mg retatrutide. This review evaluates the current available evidence for GLP-1 receptor agonists, dual GLP-1/GIP receptor co-agonists with a focus on GLP-1/GIP/glucagon receptor triagonists and discusses the potential future benefits and research directions.
-
Citations
Citations to this article as recorded by- New Mechanisms to Prevent Heart Failure with Preserved Ejection Fraction Using Glucagon-like Peptide-1 Receptor Agonism (GLP-1 RA) in Metabolic Syndrome and in Type 2 Diabetes: A Review
Jorge E. Jalil, Luigi Gabrielli, María Paz Ocaranza, Paul MacNab, Rodrigo Fernández, Bruno Grassi, Paulina Jofré, Hugo Verdejo, Monica Acevedo, Samuel Cordova, Luis Sanhueza, Douglas Greig
International Journal of Molecular Sciences.2024; 25(8): 4407. CrossRef
- New Mechanisms to Prevent Heart Failure with Preserved Ejection Fraction Using Glucagon-like Peptide-1 Receptor Agonism (GLP-1 RA) in Metabolic Syndrome and in Type 2 Diabetes: A Review

- Diabetes, Obesity and Metabolism
- Incretin and Pancreatic β-Cell Function in Patients with Type 2 Diabetes
- Chang Ho Ahn, Tae Jung Oh, Se Hee Min, Young Min Cho
- Endocrinol Metab. 2023;38(1):1-9. Published online February 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.103
- 3,386 View
- 362 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
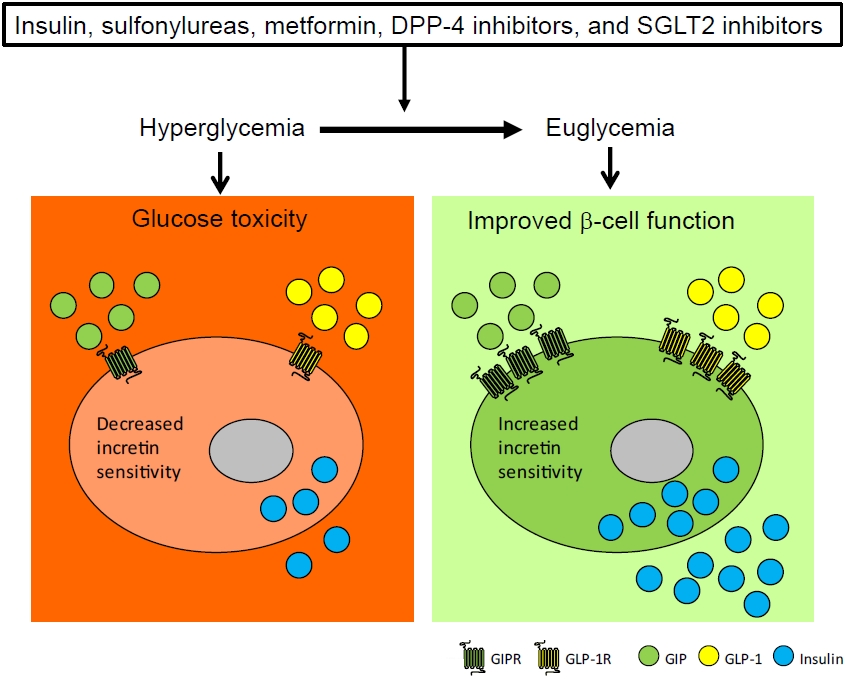
ePub - To maintain normal glucose homeostasis after a meal, it is essential to secrete an adequate amount of insulin from pancreatic β-cells. However, if pancreatic β-cells solely depended on the blood glucose level for insulin secretion, a surge in blood glucose levels would be inevitable after the ingestion of a large amount of carbohydrates. To avoid a deluge of glucose in the bloodstream after a large carbohydrate- rich meal, enteroendocrine cells detect the amount of nutrient absorption from the gut lumen and secrete incretin hormones at scale. Since insulin secretion in response to incretin hormones occurs only in a hyperglycemic milieu, pancreatic β-cells can secrete a “Goldilocks” amount of insulin (i.e., not too much and not too little) to keep the blood glucose level in the normal range. In this regard, pancreatic β-cell sensitivity to glucose and incretin hormones is crucial for maintaining normal glucose homeostasis. In this Namgok lecture 2022, we review the effects of current anti-diabetic medications on pancreatic β-cell sensitivity to glucose and incretin hormones.
-
Citations
Citations to this article as recorded by- Initial Combination Therapy in Type 2 Diabetes
Ji Yoon Kim, Nam Hoon Kim
Endocrinology and Metabolism.2024; 39(1): 23. CrossRef
- Initial Combination Therapy in Type 2 Diabetes

- Diabetes, Obesity and Metabolism
- Glucagon-Like Peptide 1 Therapy: From Discovery to Type 2 Diabetes and Beyond
- Adie Viljoen, Stephen C. Bain
- Endocrinol Metab. 2023;38(1):25-33. Published online February 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1642
- 2,833 View
- 309 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The therapeutic benefits of the incretin hormone, glucagon-like peptide 1 (GLP1), for people with type 2 diabetes and/or obesity, are now firmly established. The evidence-base arising from head-to-head comparative effectiveness studies in people with type 2 diabetes, as well as the recommendations by professional guidelines suggest that GLP1 receptor agonists should replace more traditional treatment options such as sulfonylureas and dipeptidyl-peptidase 4 (DPP4) inhibitors. Furthermore, their benefits in reducing cardiovascular events in people with type 2 diabetes beyond improvements in glycaemic control has led to numerous clinical trials seeking to translate this benefit beyond type 2 diabetes. Following early trial results their therapeutic benefit is currently being tested in other conditions including fatty liver disease, kidney disease, and Alzheimer’s disease.
-
Citations
Citations to this article as recorded by- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update
Agnieszka Jakubowska, Carel W. le Roux, Adie Viljoen
Endocrinology and Metabolism.2024; 39(1): 12. CrossRef - The Association of Circulating Glucagon-Like Peptide-1 with Cognitive Functions and Biomarkers in Alzheimer’s Disease
Mengqing Liu, Nenghong Ma, Xiao Yang, Miao Sun, Xiaowen Li, Yuhui Liu, Qing Chang, Changchun Hei, Jian-Hong Wang
Journal of Alzheimer's Disease.2024; : 1. CrossRef - Glucagon-like peptide 1 receptor agonists: cardiovascular benefits and mechanisms of action
John R. Ussher, Daniel J. Drucker
Nature Reviews Cardiology.2023; 20(7): 463. CrossRef - A new class of glucose-lowering therapy for type 2 diabetes: the latest development in the incretin arena
Stephen C Bain, Thinzar Min
The Lancet.2023; 402(10401): 504. CrossRef - Flattening the biological age curve by improving metabolic health: to taurine or not to taurine, that’ s the question
Kwok M. Ho, Anna Lee, William Wu, Matthew T.V. Chan, Lowell Ling, Jeffrey Lipman, Jason Roberts, Edward Litton, Gavin M. Joynt, Martin Wong
Journal of Geriatric Cardiology.2023; 20(11): 813. CrossRef
- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update

- Diabetes, Obesity and Metabolism
- Dulaglutide Ameliorates Palmitic Acid-Induced Hepatic Steatosis by Activating FAM3A Signaling Pathway
- Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2022;37(1):74-83. Published online February 9, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1293
- 4,949 View
- 235 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
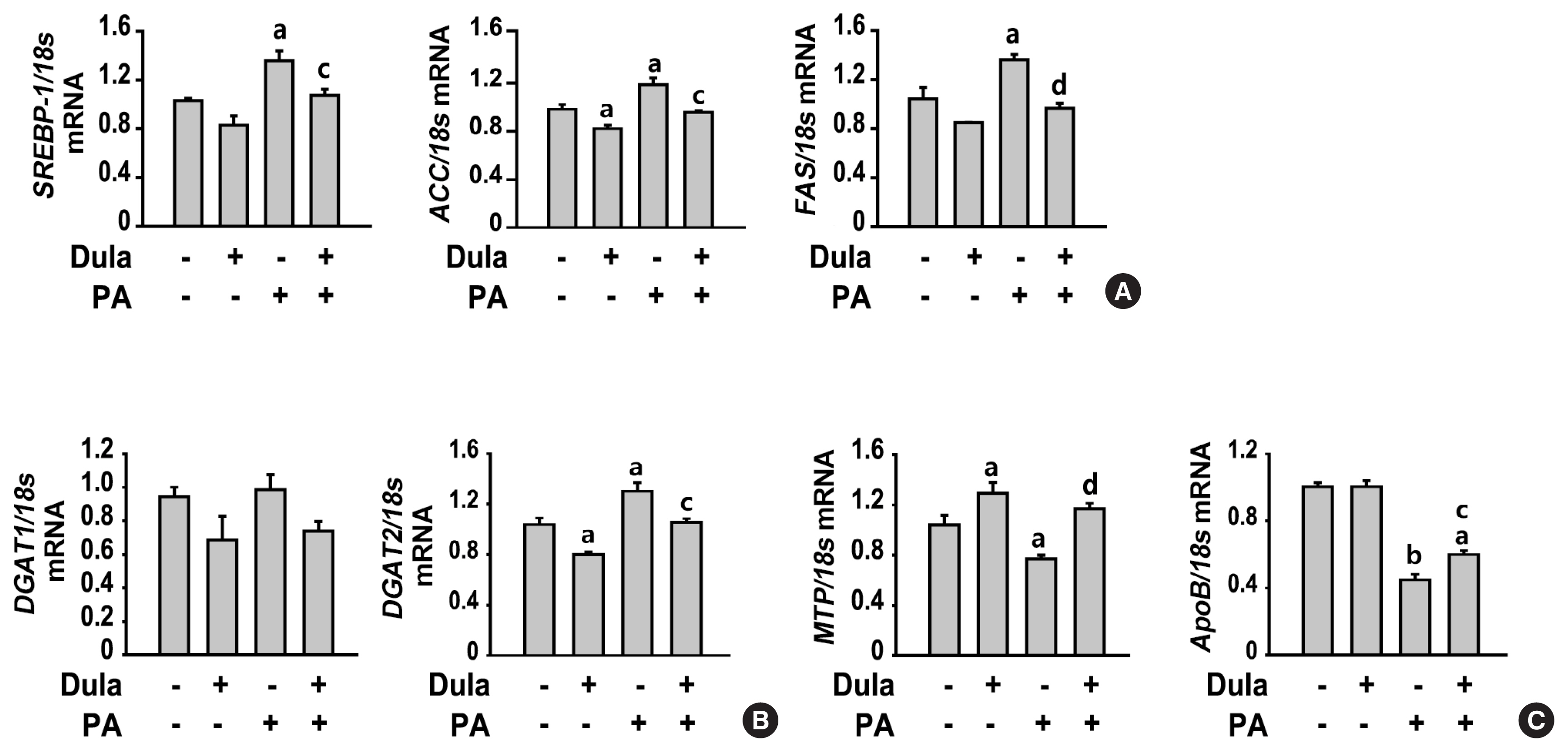
Dulaglutide, a long-acting glucagon-like peptide-1 receptor agonist (GLP-1RA), has been shown to reduce body weight and liver fat content in patients with type 2 diabetes. Family with sequence similarity 3 member A (FAM3A) plays a vital role in regulating glucose and lipid metabolism. The aim of this study was to determine the mechanisms by which dulaglutide protects against hepatic steatosis in HepG2 cells treated with palmitic acid (PA).
Methods
HepG2 cells were pretreated with 400 μM PA for 24 hours, followed by treatment with or without 100 nM dulaglutide for 24 hours. Hepatic lipid accumulation was determined using Oil red O staining and triglyceride (TG) assay, and the expression of lipid metabolism-associated factor was analyzed using quantitative real time polymerase chain reaction and Western blotting.
Results
Dulaglutide significantly decreased hepatic lipid accumulation and reduced the expression of genes associated with lipid droplet binding proteins, de novo lipogenesis, and TG synthesis in PA-treated HepG2 cells. Dulaglutide also increased the expression of proteins associated with lipolysis and fatty acid oxidation and FAM3A in PA-treated cells. However, exendin-(9-39), a GLP-1R antagonist, reversed the expression of FAM3A, and fatty acid oxidation-associated factors increased due to dulaglutide. In addition, inhibition of FAM3A by siRNA attenuated the reducing effect of dulaglutide on TG content and its increasing effect on regulation of fatty acid oxidation.
Conclusion
These results suggest that dulaglutide could be used therapeutically for improving nonalcoholic fatty liver disease, and its effect could be mediated in part via upregulation of FAM3A expression through a GLP-1R-dependent pathway. -
Citations
Citations to this article as recorded by- GLP-1/GLP-1RAs: New Options for the Drug Treatment of NAFLD
Haoran Jiang, Linquan Zang
Current Pharmaceutical Design.2024; 30(2): 100. CrossRef - GLP-1 Receptor Agonists in Non-Alcoholic Fatty Liver Disease: Current Evidence and Future Perspectives
Riccardo Nevola, Raffaella Epifani, Simona Imbriani, Giovanni Tortorella, Concetta Aprea, Raffaele Galiero, Luca Rinaldi, Raffaele Marfella, Ferdinando Carlo Sasso
International Journal of Molecular Sciences.2023; 24(2): 1703. CrossRef - FAM3A mediates the phenotypic switch of human aortic smooth muscle cells stimulated with oxidised low-density lipoprotein by influencing the PI3K-AKT pathway
Lei Yang, Baoshun Du, Shitao Zhang, Maode Wang
In Vitro Cellular & Developmental Biology - Animal.2023; 59(6): 431. CrossRef - ATP Secretion and Metabolism in Regulating Pancreatic Beta Cell Functions and Hepatic Glycolipid Metabolism
Jing Li, Han Yan, Rui Xiang, Weili Yang, Jingjing Ye, Ruili Yin, Jichun Yang, Yujing Chi
Frontiers in Physiology.2022;[Epub] CrossRef - Targeted therapeutics and novel signaling pathways in non-alcohol-associated fatty liver/steatohepatitis (NAFL/NASH)
Xiaohan Xu, Kyle L. Poulsen, Lijuan Wu, Shan Liu, Tatsunori Miyata, Qiaoling Song, Qingda Wei, Chenyang Zhao, Chunhua Lin, Jinbo Yang
Signal Transduction and Targeted Therapy.2022;[Epub] CrossRef
- GLP-1/GLP-1RAs: New Options for the Drug Treatment of NAFLD

- Diabetes, Obesity and Metabolism
- Efficacy and Safety of the New Appetite Suppressant, Liraglutide: A Meta-Analysis of Randomized Controlled Trials
- Shinje Moon, Jibeom Lee, Hye Soo Chung, Yoon Jung Kim, Jae Myung Yu, Sung Hoon Yu, Chang-Myung Oh
- Endocrinol Metab. 2021;36(3):647-660. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2020.934

- 6,221 View
- 302 Download
- 13 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity is a chronic disease associated with metabolic diseases such as diabetes and cardiovascular disease. Since the U.S. Food and Drug Administration approved liraglutide as an anti-obesity drug for nondiabetic patients in 2014, it has been widely used for weight control in overweight and obese people. This study aimed to systematically analyze the effects of liraglutide on body weight and other cardiometabolic parameters.
Methods
We investigated articles from PubMed, EMBASE, and the Cochrane Library to search randomized clinical trials that examined body weight changes with liraglutide treatment.
Results
We included 31 studies with 8,060 participants for this meta-analysis. The mean difference (MD) between the liraglutide group and the placebo group was −4.19 kg (95% confidence interval [CI], −4.84 to −3.55), with a −4.16% change from the baseline (95% CI, −4.90 to −3.43). Liraglutide treatment correlated with a significantly reduced body mass index (MD: −1.55; 95% CI, −1.76 to −1.34) and waist circumference (MD: −3.11 cm; 95% CI, −3.59 to −2.62) and significantly decreased blood pressure (systolic blood pressure, MD: −2.85 mm Hg; 95% CI, −3.36 to −2.35; diastolic blood pressure, MD: −0.66 mm Hg; 95% CI, −1.02 to −0.30), glycated hemoglobin (MD: −0.40%; 95% CI, −0.49 to −0.31), and low-density lipoprotein cholesterol (MD: –2.91 mg/dL; 95% CI, −5.28 to −0.53; MD: −0.87% change from baseline; 95% CI, −1.17 to −0.56).
Conclusion
Liraglutide is effective for weight control and can be a promising drug for cardiovascular protection in overweight and obese people. -
Citations
Citations to this article as recorded by- Pharmacotherapy for obesity: moving towards efficacy improvement
Walmir Coutinho, Bruno Halpern
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Physiopathology and Treatment of Obesity and Overweight: A Proposal for a New Anorectic
Bruno Silvestrini, Mauro Silvestrini, Mayank Choubey
Journal of Obesity.2024; 2024: 1. CrossRef - Side effect profile of pharmacologic therapies for liver fibrosis in nonalcoholic fatty liver disease: a systematic review and network meta-analysis
Yilin Li, Rong Lei, Honglin Lei, Qin Xiong, Fengjiao Xie, Chengjiao Yao, Peimin Feng
European Journal of Gastroenterology & Hepatology.2023; 35(1): 1. CrossRef - Recommendations for the prevention and management of obesity in the Iraqi population
Hussein Ali Nwayyir, Esraa Majid Mutasher, Osama Mohammed Alabid, Muthana Abdulrazzaq Jabbar, Wefak Hasan Abdulraheem Al-Kawaz, Haider Ayad Alidrisi, Majid Alabbood, Muhammed Chabek, Munib AlZubaidi, Lujain Anwar Al-khazrajy, Ibtihal Shukri Abd Alhaleem,
Postgraduate Medicine.2023; 135(5): 425. CrossRef - A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Fatma Haddad, Ghadeer Dokmak, Maryam Bader, Rafik Karaman
Life.2023; 13(4): 1012. CrossRef - Liraglutide, a glucagon-like peptide-1 analog, in individuals with obesity in clinical practice
Juyoung Shin, Raeun Kim, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 49. CrossRef - The effects of subcutaneous Tirzepatide on obesity and overweight: a systematic review and meta‐regression analysis of randomized controlled trials
Pejman Rohani, Nasser Malekpour Alamdari, Seyedeh Elaheh Bagheri, Azita Hekmatdoost, Mohammad Hassan Sohouli
Frontiers in Endocrinology.2023;[Epub] CrossRef - Efficacy and safety of liraglutide for weight management in children and adolescents: a systematic review and meta-analysis of randomized controlled trials
Hao Gou, Yiman Zhai, Junjun Guo
European Journal of Pediatrics.2023; 182(11): 5095. CrossRef - Efficacy and safety of once-weekly semaglutide in adults with overweight or obesity: a meta-analysis
Ping Zhong, Hai Zeng, Miaochun Huang, Wenbin Fu, Zhixia Chen
Endocrine.2022; 75(3): 718. CrossRef - Pharmacological profile of once-weekly injectable semaglutide for chronic weight management
David C. W. Lau, Rachel L Batterham, Carel W. le Roux
Expert Review of Clinical Pharmacology.2022; 15(3): 251. CrossRef - Pharmacological Management of Obesity: A Century of Expert Opinions in Cecil Textbook of Medicine
Peter Manu, Cristina-Mihaela Lăcătuşu, Liliana M. Rogozea, Simona Cernea
American Journal of Therapeutics.2022; 29(4): e410. CrossRef - GLP-1 agonists: superior for mind and body in antipsychotic-treated patients?
Katerina Horska, Jana Ruda-Kucerova, Silje Skrede
Trends in Endocrinology & Metabolism.2022; 33(9): 628. CrossRef - Targeting skeletal muscle mitochondrial health in obesity
Chantal A. Pileggi, Breana G. Hooks, Ruth McPherson, Robert R.M. Dent, Mary-Ellen Harper
Clinical Science.2022; 136(14): 1081. CrossRef - A Study on Weight Loss Cause as per the Side Effect of Liraglutide
Jin Yu, Jeongmin Lee, Seung-Hwan Lee, Jae-Hyung Cho, Hun-Sung Kim, Heng Zhou
Cardiovascular Therapeutics.2022; 2022: 1. CrossRef
- Pharmacotherapy for obesity: moving towards efficacy improvement

- Diabetes
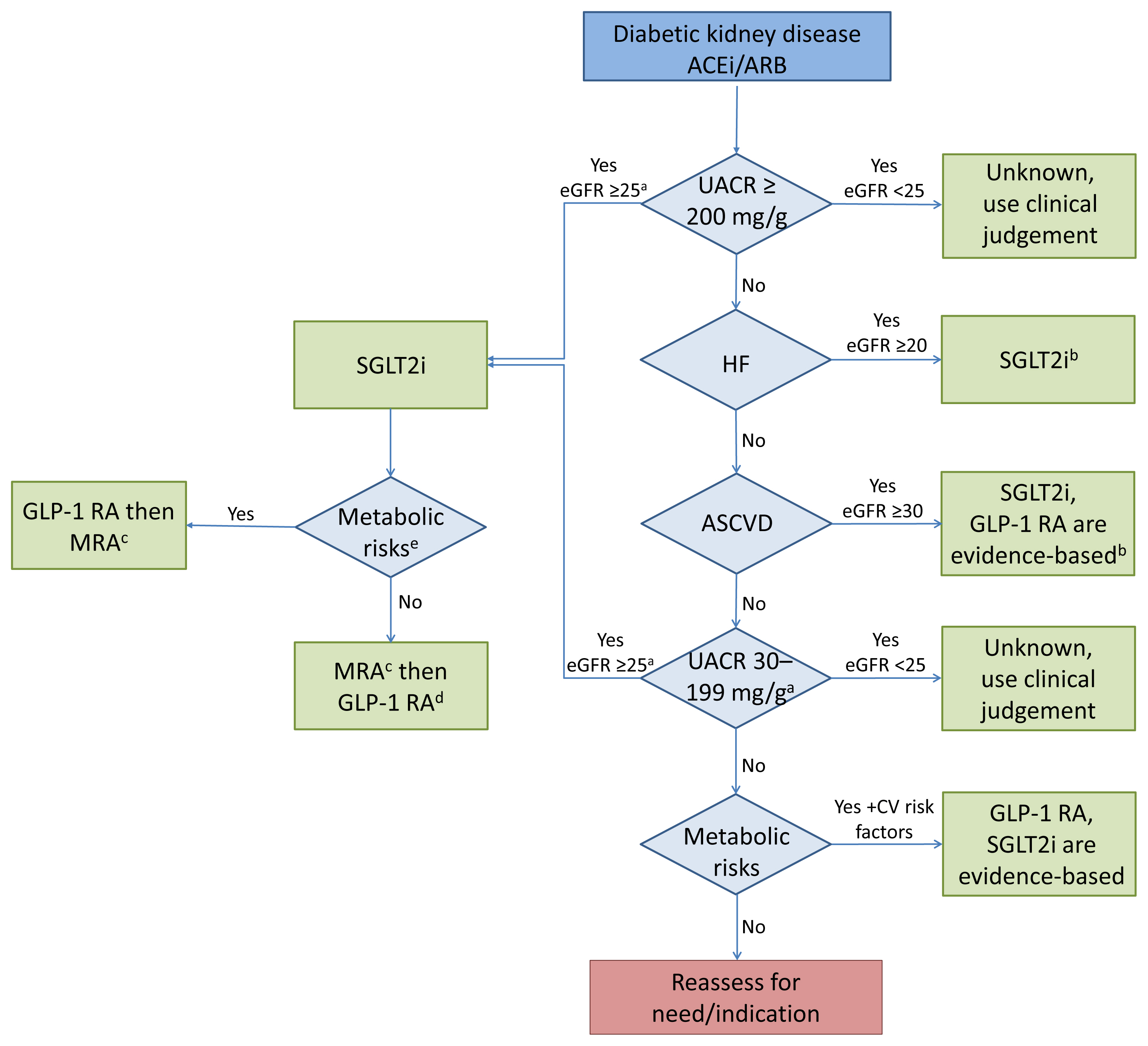
- Cardiorenal Protection in Diabetic Kidney Disease
- Jason F. Lee, Ecaterina Berzan, Vikas S. Sridhar, Ayodele Odutayo, David Z.I. Cherney
- Endocrinol Metab. 2021;36(2):256-269. Published online April 19, 2021
- DOI: https://doi.org/10.3803/EnM.2021.987
- 5,808 View
- 300 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Over the last 5 years there have been many new developments in the management of diabetic kidney disease. Glucagon-like peptide-1 receptor agonists (GLP-1 RA) and sodium-glucose cotransporter-2 (SGLT2) inhibitors were initially used for glycemic control, but more recent studies have now shown that their benefits extend to cardiovascular and kidney outcomes. The recent addition of data on the novel mineralocorticoid receptor antagonist (MRA) gives us another approach to further decrease the residual risk of diabetic kidney disease progression. In this review we describe the mechanism of action, key studies, and possible adverse effects related to these three classes of medications. The management of type 2 diabetes now includes an increasing number of medications for the management of comorbidities in a patient population at significant risk of cardiovascular disease and progression of chronic kidney disease. It is from this perspective that we seek to outline the rationale for the sequential and/or combined use of SGLT2 inhibitors, GLP-1 RA and MRAs in patients with type 2 diabetes for heart and kidney protection.
-
Citations
Citations to this article as recorded by- Relative and Absolute Risks of Adverse Events with Real-World Use of SGLT2 Inhibitors in CKD
Ayodele Odutayo, Adeera Levin
Clinical Journal of the American Society of Nephrology.2023; 18(5): 557. CrossRef - Renal Protection of Mineralocorticoid Receptor Antagonist, Finerenone, in Diabetic Kidney Disease
Dong-Lim Kim, Seung-Eun Lee, Nan Hee Kim
Endocrinology and Metabolism.2023; 38(1): 43. CrossRef - Intrarenal Mechanisms of Sodium-Glucose Cotransporter-2 Inhibitors on Tubuloglomerular Feedback and Natriuresis
Eun Sil Koh, Gheun-Ho Kim, Sungjin Chung
Endocrinology and Metabolism.2023; 38(4): 359. CrossRef - SGLT2 and DPP4 inhibitors improve Alzheimer’s disease–like pathology and cognitive function through distinct mechanisms in a T2D–AD mouse model
A Young Sim, Da Hyun Choi, Jong Youl Kim, Eun Ran Kim, A-ra Goh, Yong-ho Lee, Jong Eun Lee
Biomedicine & Pharmacotherapy.2023; 168: 115755. CrossRef - Narrative review investigating the nephroprotective mechanisms of sodium glucose cotransporter type 2 inhibitors in diabetic and nondiabetic patients with chronic kidney disease
Emma S. Speedtsberg, Martin Tepel
Frontiers in Endocrinology.2023;[Epub] CrossRef - Management of CKD
Nimrit Goraya, Jennifer D. Moran
Nephrology Self-Assessment Program.2022; 21(2): 146. CrossRef - Nonsteroidal mineralocorticoid receptor antagonism for cardiovascular and renal disorders − New perspectives for combination therapy
Peter Kolkhof, Amer Joseph, Ulrich Kintscher
Pharmacological Research.2021; 172: 105859. CrossRef - Sodium‐Glucose Cotransporter 2 Inhibitors, All‐Cause Mortality, and Cardiovascular Outcomes in Adults with Type 2 Diabetes: A Bayesian Meta‐Analysis and Meta‐Regression
Ayodele Odutayo, Bruno R. da Costa, Tiago V. Pereira, Vinay Garg, Samir Iskander, Fatimah Roble, Rahim Lalji, Cesar A. Hincapié, Aquila Akingbade, Myanca Rodrigues, Arnav Agarwal, Bishoy Lawendy, Pakeezah Saadat, Jacob A. Udell, Francesco Cosentino, Peter
Journal of the American Heart Association.2021;[Epub] CrossRef - Finerenone: A Potential Treatment for Patients with Chronic Kidney Disease and Type 2 Diabetes Mellitus
Luis D’Marco, María Jesús Puchades, Lorena Gandía, Claudia Forquet, Elena Giménez-Civera, Nayara Panizo, Javier Reque, Isabel Juan-García, Valmore Bermúdez, José Luis Gorriz
touchREVIEWS in Endocrinology.2021; 17(2): 84. CrossRef - Sodium-Glucose Cotransporter 2 Inhibitors Mechanisms of Action: A Review
Jorge I. Fonseca-Correa, Ricardo Correa-Rotter
Frontiers in Medicine.2021;[Epub] CrossRef
- Relative and Absolute Risks of Adverse Events with Real-World Use of SGLT2 Inhibitors in CKD

- Diabetes
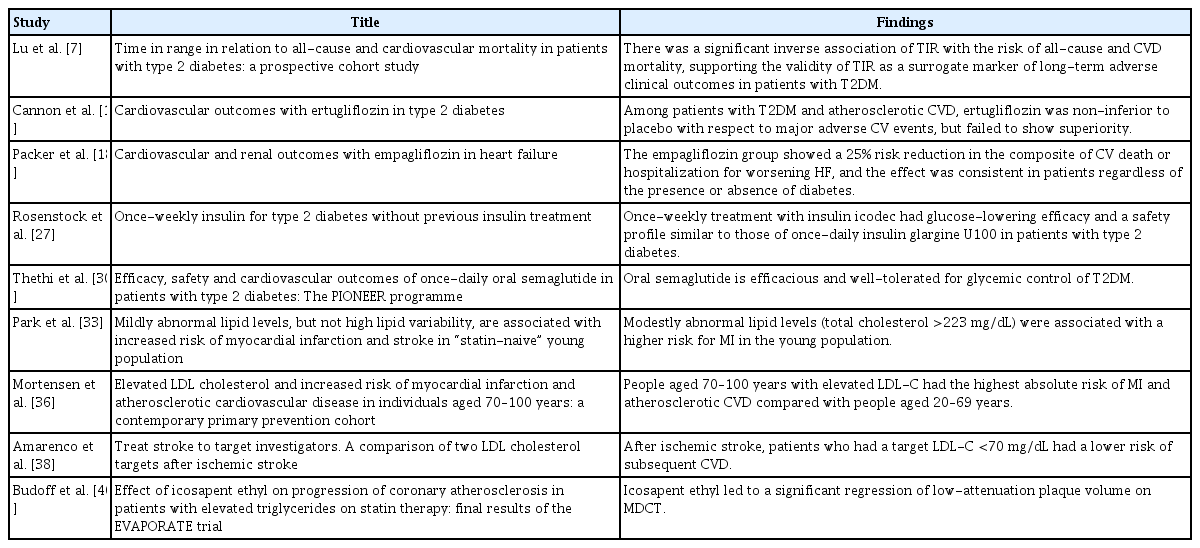
- Best Achievements in Clinical Medicine in Diabetes and Dyslipidemia in 2020
- Eun-Jung Rhee, Mee-Kyung Kim, Won-Young Lee
- Endocrinol Metab. 2021;36(1):41-50. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2021.106
- 4,348 View
- 178 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Over the last two decades, our understanding of diabetes and treatment strategies have evolved tremendously, from scientific, mechanistic, and human perspectives. The categories of anti-diabetic medications expanded from a few to numerous, enabling clinicians to personalize diabetes care and treatment. Thanks to rapid growth in the field of science and medical engineering, newer treatment options are coming to the market with various advantages and disadvantages to be aware of. Therefore, clinicians should rapidly adopt new trends based on guidelines and data from many clinical trials in the field of diabetes. In the treatment of dyslipidemia, trends and guidelines are changing every year, and novel therapies are being developed. In this review, we would like to summarize the major achievements in clinical medicine in 2020 in the field of diabetes mellitus and dyslipidemia.
-
Citations
Citations to this article as recorded by- Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Combined Effects of Obesity and Dyslipidaemia on the Prevalence of Diabetes Amongst Adults Aged ≥45 Years: Evidence from a Nationally Representative Cross-Sectional Study
Simin Zhang, Donghan Sun, Xiaoyi Qian, Li Li, Wenwen Wu
International Journal of Environmental Research and Public Health.2022; 19(13): 8036. CrossRef - Low-Density Lipoprotein Cholesterol Level, Statin Use and Myocardial Infarction Risk in Young Adults
Heekyoung Jeong, Kyungdo Han, Soon Jib Yoo, Mee Kyoung Kim
Journal of Lipid and Atherosclerosis.2022; 11(3): 288. CrossRef
- Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study

- Diabetes
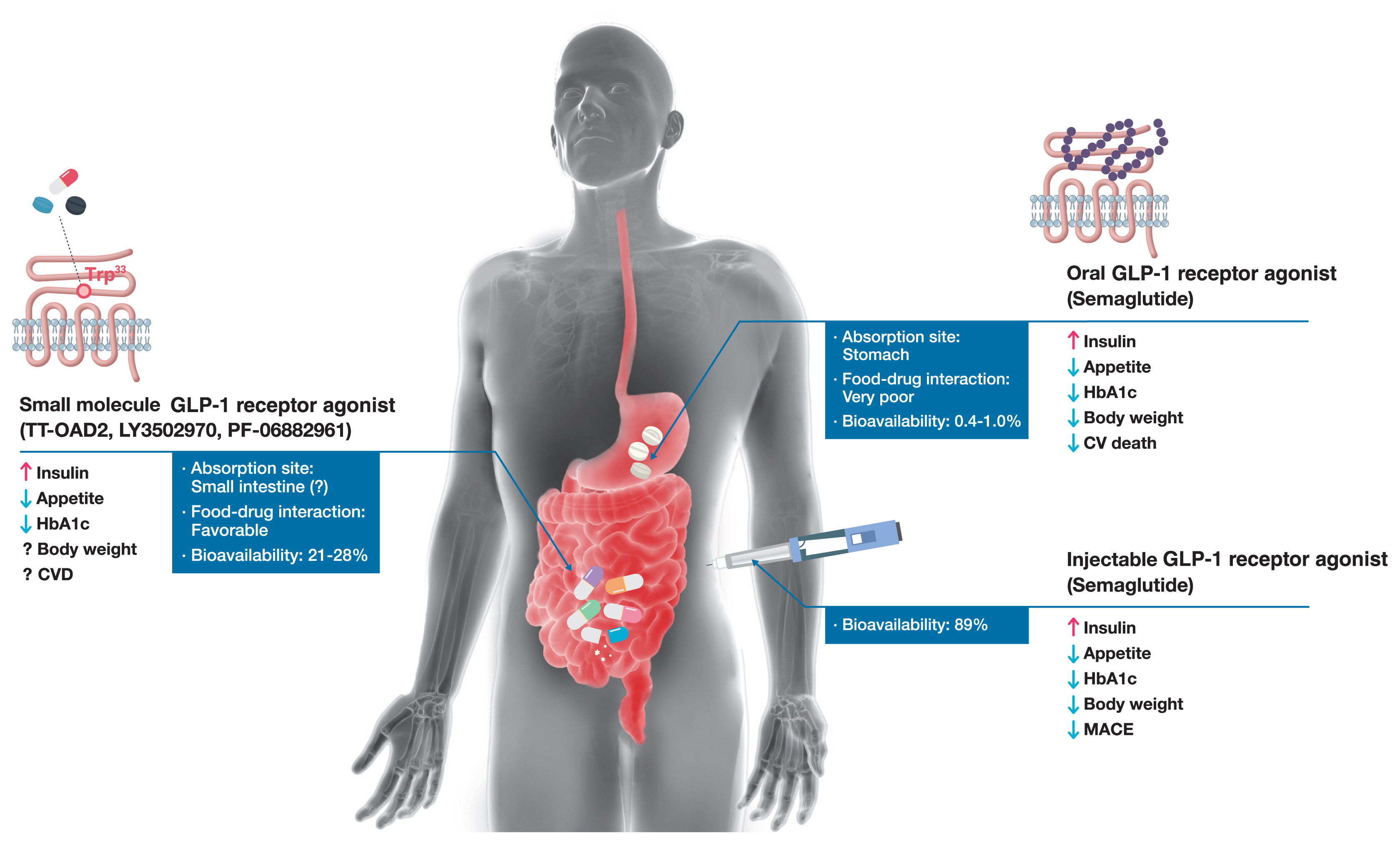
- Peptidyl and Non-Peptidyl Oral Glucagon-Like Peptide-1 Receptor Agonists
- Hun Jee Choe, Young Min Cho
- Endocrinol Metab. 2021;36(1):22-29. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2021.102
- 27,999 View
- 656 Download
- 11 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Glucagon-like peptide-1 (GLP-1) receptor agonists are efficacious glucose-lowering medications with salient benefits for body weight and cardiovascular events. This class of medications is now recommended as the top priority for patients with established cardiovascular disease or indicators of high risk. Until the advent of oral semaglutide, however, GLP-1 receptor agonists were available only in the form of subcutaneous injections. Aversion to needles, discomfort with self-injection, or skin problems at the injection site are commonly voiced problems in people with diabetes, and thus, attempts for non-invasive delivery strategies have continued. Herein, we review the evolution of GLP-1 therapy from its discovery and the development of currently approved drugs to the unprecedented endeavor to administer GLP-1 receptor agonists via the oral route. We focus on the pharmacokinetic and pharmacodynamic properties of the recently approved oral GLP-1 receptor agonist, oral semaglutide. Small molecule oral GLP-1 receptor agonists are currently in development, and we introduce how these chemicals have addressed the challenge posed by interactions with the large extracellular ligand binding domain of the GLP-1 receptor. We specifically discuss the structure and pharmacological properties of TT-OAD2, LY3502970, and PF-06882961, and envision an era where more patients could benefit from oral GLP-1 receptor agonist therapy.
-
Citations
Citations to this article as recorded by- Sulfobetaine modification of poly (D, L-lactide-co-glycolic acid) nanoparticles enhances mucus permeability and improves bioavailability of orally delivered liraglutide
Zhenyu Zhao, Ruihuan Ding, Yumei Wang, Ranran Yuan, Houqian Zhang, Tianyang Li, Wei Zheng, Entao Chen, Aiping Wang, Yanan Shi
Journal of Drug Delivery Science and Technology.2024; 93: 105437. CrossRef - Physiology and pharmacology of glucagon-like peptide-1 receptor
D. V. Kurkin, D. A. Bakulin, E. I. Morkovin, V. I. Petrov, A. V. Strygin, K. N. Koryanova, Yu. V. Gorbunova, Yu. A. Kolosov, O. V. Ivanova, E. V. Pavlova, M. A. Dzhavakhyan, A. V. Zaborovsky, V. B. Saparova, I. E. Makarenko, R. I. Drai, A. N. Chumachenko
Pharmacy & Pharmacology.2024; 11(4): 347. CrossRef - G protein-coupled receptors driven intestinal glucagon-like peptide-1 reprogramming for obesity: Hope or hype?
Mohan Patil, Ilaria Casari, Leon N. Warne, Marco Falasca
Biomedicine & Pharmacotherapy.2024; 172: 116245. CrossRef - Glucagon-like peptide-1 analogs: Miracle drugs are blooming?
Binbin Gong, Zhihong Yao, Chenxu Zhou, Wenxi Wang, Lidan Sun, Jing Han
European Journal of Medicinal Chemistry.2024; 269: 116342. CrossRef - Opportunities and challenges of incretin-based hypoglycemic agents treating type 2 diabetes mellitus from the perspective of physiological disposition
Yaochen Xie, Qian Zhou, Qiaojun He, Xiaoyi Wang, Jincheng Wang
Acta Pharmaceutica Sinica B.2023; 13(6): 2383. CrossRef - Advances in GLP-1 receptor agonists for the treatment of type 2 diabetes
Shurui Hong, J. Xiao, Y. He
BIO Web of Conferences.2023; 61: 01006. CrossRef - Safety and efficacy of the new, oral, small-molecule, GLP-1 receptor agonists orforglipron and danuglipron for the treatment of type 2 diabetes and obesity: systematic review and meta-analysis of randomized controlled trials
Paschalis Karakasis, Dimitrios Patoulias, Konstantinos Pamporis, Panagiotis Stachteas, Konstantinos I. Bougioukas, Aleksandra Klisic, Nikolaos Fragakis, Manfredi Rizzo
Metabolism.2023; 149: 155710. CrossRef - A review of glucoregulatory hormones potentially applicable to the treatment of Alzheimer’s disease: mechanism and brain delivery
Reeju Amatya, Kyoung Ah Min, Meong Cheol Shin
Journal of Pharmaceutical Investigation.2022; 52(2): 195. CrossRef - Anti-Obesity Medications and Investigational Agents: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022
Harold E. Bays, Angela Fitch, Sandra Christensen, Karli Burridge, Justin Tondt
Obesity Pillars.2022; 2: 100018. CrossRef - Structural basis of peptidomimetic agonism revealed by small-molecule GLP-1R agonists Boc5 and WB4-24
Zhaotong Cong, Qingtong Zhou, Yang Li, Li-Nan Chen, Zi-Chen Zhang, Anyi Liang, Qing Liu, Xiaoyan Wu, Antao Dai, Tian Xia, Wei Wu, Yan Zhang, Dehua Yang, Ming-Wei Wang
Proceedings of the National Academy of Sciences.2022;[Epub] CrossRef - Improved Split TEV GPCR β-arrestin-2 Recruitment Assays via Systematic Analysis of Signal Peptide and β-arrestin Binding Motif Variants
Yuxin Wu, Isabelle von Hauff, Niels Jensen, Moritz Rossner, Michael Wehr
Biosensors.2022; 13(1): 48. CrossRef - GLP-1 Receptor Agonists: Beyond Their Pancreatic Effects
Xin Zhao, Minghe Wang, Zhitong Wen, Zhihong Lu, Lijuan Cui, Chao Fu, Huan Xue, Yunfeng Liu, Yi Zhang
Frontiers in Endocrinology.2021;[Epub] CrossRef - Recent developments in GLP‐1RA therapy: A review of the latest evidence of efficacy and safety and differences within the class
Evie K. Bain, Stephen C. Bain
Diabetes, Obesity and Metabolism.2021; 23(S3): 30. CrossRef
- Sulfobetaine modification of poly (D, L-lactide-co-glycolic acid) nanoparticles enhances mucus permeability and improves bioavailability of orally delivered liraglutide

- Endocrine Research
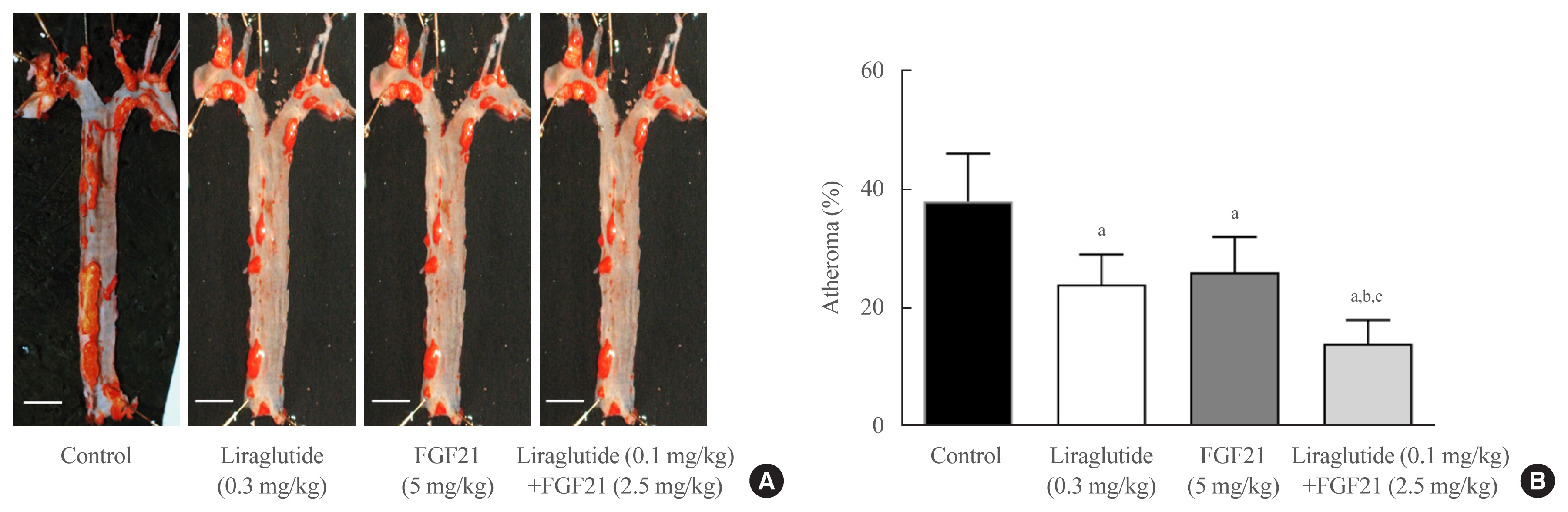
- Effects of Glucagon-Like Peptide-1 Analogue and Fibroblast Growth Factor 21 Combination on the Atherosclerosis-Related Process in a Type 2 Diabetes Mouse Model
- Jin Hee Kim, Gha Young Lee, Hyo Jin Maeng, Hoyoun Kim, Jae Hyun Bae, Kyoung Min Kim, Soo Lim
- Endocrinol Metab. 2021;36(1):157-170. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.781
- 6,923 View
- 176 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Glucagon-like peptide-1 (GLP-1) analogues regulate glucose homeostasis and have anti-inflammatory properties, but cause gastrointestinal side effects. The fibroblast growth factor 21 (FGF21) is a hormonal regulator of lipid and glucose metabolism that has poor pharmacokinetic properties, including a short half-life. To overcome these limitations, we investigated the effect of a low-dose combination of a GLP-1 analogue and FGF21 on atherosclerosis-related molecular pathways.
Methods
C57BL/6J mice were fed a high-fat diet for 30 weeks followed by an atherogenic diet for 10 weeks and were divided into four groups: control (saline), liraglutide (0.3 mg/kg/day), FGF21 (5 mg/kg/day), and low-dose combination treatment with liraglutide (0.1 mg/kg/day) and FGF21 (2.5 mg/kg/day) (n=6/group) for 6 weeks. The effects of each treatment on various atherogenesisrelated pathways were assessed.
Results
Liraglutide, FGF21, and their low-dose combination significantly reduced atheromatous plaque in aorta, decreased weight, glucose, and leptin levels, and increased adiponectin levels. The combination treatment upregulated the hepatic uncoupling protein-1 (UCP1) and Akt1 mRNAs compared with controls. Matric mentalloproteinase-9 (MMP-9), monocyte chemoattractant protein-1 (MCP-1), and intercellular adhesion molecule-1 (ICAM-1) were downregulated and phosphorylated Akt (p-Akt) and phosphorylated extracellular signal-regulated kinase (p-ERK) were upregulated in liver of the liraglutide-alone and combination-treatment groups. The combination therapy also significantly decreased the proliferation of vascular smooth muscle cells. Caspase-3 was increased, whereas MMP-9, ICAM-1, p-Akt, and p-ERK1/2 were downregulated in the liraglutide-alone and combination-treatment groups.
Conclusion
Administration of a low-dose GLP-1 analogue and FGF21 combination exerts beneficial effects on critical pathways related to atherosclerosis, suggesting the synergism of the two compounds. -
Citations
Citations to this article as recorded by- Current status and future perspectives of FGF21 analogues in clinical trials
Zara Siu Wa Chui, Qing Shen, Aimin Xu
Trends in Endocrinology & Metabolism.2024;[Epub] CrossRef - Design and pharmaceutical evaluation of bifunctional fusion protein of FGF21 and GLP-1 in the treatment of nonalcoholic steatohepatitis
Xianlong Ye, Yingli Chen, Jianying Qi, Shenglong Zhu, Yuanyuan Wu, Jingjing Xiong, Fei Hu, Zhimou Guo, Xinmiao Liang
European Journal of Pharmacology.2023; 952: 175811. CrossRef - Use of FGF21 analogs for the treatment of metabolic disorders: a systematic review and meta-analysis
Maria Paula Carbonetti, Fernanda Almeida-Oliveira, David Majerowicz
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Exploring the potential mechanism of Simiao Yongan decoction in the treatment of diabetic peripheral vascular disease based on network pharmacology and molecular docking technology
Fang Cao, Yongkang Zhang, Yuan Zong, Xia Feng, Junlin Deng, Yuzhen Wang, Yemin Cao
Medicine.2023; 102(52): e36762. CrossRef - The Healing Capability of Clove Flower Extract (CFE) in Streptozotocin-Induced (STZ-Induced) Diabetic Rat Wounds Infected with Multidrug Resistant Bacteria
Rewaa Ali, Tarek Khamis, Gamal Enan, Gamal El-Didamony, Basel Sitohy, Gamal Abdel-Fattah
Molecules.2022; 27(7): 2270. CrossRef - Nonalcoholic Steatohepatitis (NASH) and Atherosclerosis: Explaining Their Pathophysiology, Association and the Role of Incretin-Based Drugs
Eleftheria Galatou, Elena Mourelatou, Sophia Hatziantoniou, Ioannis S. Vizirianakis
Antioxidants.2022; 11(6): 1060. CrossRef - Unlocking the Therapeutic Potential of Glucagon-Like Peptide-1 Analogue and Fibroblast Growth Factor 21 Combination for the Pathogenesis of Atherosclerosis in Type 2 Diabetes
Jang Won Son
Endocrinology and Metabolism.2021; 36(1): 57. CrossRef - Effects of fasting on skeletal muscles and body fat of adult and old C57BL/6J mice
Mindaugas Kvedaras, Petras Minderis, Leonardo Cesanelli, Agne Cekanauskaite, Aivaras Ratkevicius
Experimental Gerontology.2021; 152: 111474. CrossRef - The Role of Fibroblast Growth Factor 21 in Diabetic Cardiovascular Complications and Related Epigenetic Mechanisms
Mengjie Xiao, Yufeng Tang, Shudong Wang, Jie Wang, Jie Wang, Yuanfang Guo, Jingjing Zhang, Junlian Gu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Liraglutide Decreases Liver Fat Content and Serum Fibroblast Growth Factor 21 Levels in Newly Diagnosed Overweight Patients with Type 2 Diabetes and Nonalcoholic Fatty Liver Disease
Xinyue Li, Xiaojuan Wu, Yumei Jia, Jing Fu, Lin Zhang, Tao Jiang, Jia Liu, Guang Wang, Claudia Cardoso
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Differential importance of endothelial and hematopoietic cell GLP-1Rs for cardiometabolic versus hepatic actions of semaglutide
Brent A. McLean, Chi Kin Wong, Kiran Deep Kaur, Randy J. Seeley, Daniel J. Drucker
JCI Insight.2021;[Epub] CrossRef
- Current status and future perspectives of FGF21 analogues in clinical trials

- Diabetes
- A Review of the Effects of Glucagon-Like Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors on Lean Body Mass in Humans
- Jack Alistair Sargeant, Joseph Henson, James Adam King, Thomas Yates, Kamlesh Khunti, Melanie Jane Davies
- Endocrinol Metab. 2019;34(3):247-262. Published online September 26, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.3.247
- 11,663 View
- 422 Download
- 57 Web of Science
- 60 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Weight loss is an important goal in the management of several chronic conditions, including type 2 diabetes mellitus, and pharmacological therapies that aid weight loss are appealing. Glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose cotransporter 2 inhibitors (SGLT2is) are novel glucose-lowering therapies that have been shown to induce clinically significant reductions in body weight. However, this weight loss may not be attributed solely to fat mass (FM). Given the importance of skeletal muscle and lean body mass (LBM) on cardio-metabolic health and physical function, we reviewed the available literature reporting the effects of GLP-1RAs and SGLT2is on body composition. Results demonstrate that, in most circumstances, the weight loss associated with both therapies predominantly comprises a reduction in FM, although significant heterogeneity exists between studies. In over half of the studies identified, the proportion of LBM reduction ranged between 20% and 50% of total weight lost, which is consistent with diet-induced weight loss and bariatric surgery. No clear differences existed between GLP-1RAs and SGLT2is. Consequently, the loss of LBM and skeletal muscle associated with weight loss induced by GLP-1RAs and SGLT2is warrants attention. Strategies to preserve skeletal muscle and improve physical function, for example through structured exercise, are of great importance.
-
Citations
Citations to this article as recorded by- Drug‐related sarcopenia as a secondary sarcopenia
Masafumi Kuzuya
Geriatrics & Gerontology International.2024; 24(2): 195. CrossRef - Exercise induces tissue-specific adaptations to enhance cardiometabolic health
Stephen P. Ashcroft, Ben Stocks, Brendan Egan, Juleen R. Zierath
Cell Metabolism.2024; 36(2): 278. CrossRef - Once-weekly semaglutide administered after laparoscopic sleeve gastrectomy: Effects on body weight, glycemic control, and measured nutritional metrics in Japanese patients having both obesity and type 2 diabetes
Rieko Kanai, Sachiho Kinoshita, Izumi Kanbe, Mariko Sameda, Shuhei Yamaoka, Osamu Horikawa, Yasuhiro Watanabe, Ichiro Tatsuno, Kohji Shirai, Takashi Oshiro, Atsuhito Saiki
Obesity Pillars.2024; 9: 100098. CrossRef - Twenty‐four‐hour physical behaviour profiles across type 2 diabetes mellitus subtypes
Joseph Henson, Aikaterina Tziannou, Alex V. Rowlands, Charlotte L. Edwardson, Andrew P. Hall, Melanie J. Davies, Thomas Yates
Diabetes, Obesity and Metabolism.2024; 26(4): 1355. CrossRef - The Current Landscape of Pharmacotherapies for Sarcopenia
Gulistan Bahat, Serdar Ozkok
Drugs & Aging.2024; 41(2): 83. CrossRef - Malnutrition and Sarcopenia as Reasons for Caution with GLP-1 Receptor Agonist Use in HFpEF
ELISSA DRIGGIN, PARAG GOYAL
Journal of Cardiac Failure.2024; 30(4): 610. CrossRef - Is the GLP-1 receptor agonist, semaglutide, a good option for weight loss in persons with HIV?
Daniel Lee, Jacqueline Capeau
AIDS.2024; 38(4): 603. CrossRef - Efficacy and safety of tirzepatide, GLP‐1 receptor agonists, and other weight loss drugs in overweight and obesity: a network meta‐analysis
Xin‐Hui Pan, Bryan Tan, Yip Han Chin, Ethan Cheng Zhe Lee, Gwyneth Kong, Bryan Chong, Martin Kueh, Chin Meng Khoo, Anurag Mehta, Priyanka Majety, Gowtham R. Grandhi, Georgios K. Dimitriadis, Roger Foo, Nicholas W. S. Chew, Carel W. Le Roux, Mamas A. Mamas
Obesity.2024; 32(5): 840. CrossRef - Dual and Triple Incretin-Based Co-agonists: Novel Therapeutics for Obesity and Diabetes
Robert M. Gutgesell, Rubén Nogueiras, Matthias H. Tschöp, Timo D. Müller
Diabetes Therapy.2024; 15(5): 1069. CrossRef - GPR75: A Newly Identified Receptor for Targeted Intervention in the Treatment of Obesity and Metabolic Syndrome
Michael L. Fragner, Manish A. Parikh, Kaedrea A. Jackson, Michal Laniado Schwartzman, William H. Frishman, Stephen J. Peterson
Cardiology in Review.2024;[Epub] CrossRef - Malnutrition in real-world patients hospitalized for heart failure with preserved ejection fraction and its potential impact on generalizability of EMPEROR-Preserved trial
Shinsuke Takeuchi, Takashi Kohno, Ayumi Goda, Yasuyuki Shiraishi, Mike Saji, Yuji Nagatomo, Toshikazu D. Tanaka, Makoto Takei, Shintaro Nakano, Kyoko Soejima, Shun Kohsaka, Tsutomu Yoshikawa
International Journal of Cardiology.2023; 370: 263. CrossRef - Marked weight loss on liraglutide 3.0 mg: Real‐life experience of a Swiss cohort with obesity
Sara Santini, Nathalie Vionnet, Jérôme Pasquier, Elena Gonzalez‐Rodriguez, Montserrat Fraga, Nelly Pitteloud, Lucie Favre
Obesity.2023; 31(1): 74. CrossRef - Early type 2 diabetes treatment intensification with glucagon‐like peptide‐1 receptor agonists in primary care: An Australian perspective on guidelines and the global evidence
Roy Rasalam, Sarah Abdo, Gary Deed, Richard O'Brien, Jane Overland
Diabetes, Obesity and Metabolism.2023; 25(4): 901. CrossRef - The effects of weight‐lowering pharmacotherapies on physical activity, function and fitness: A systematic review and meta‐analysis of randomized controlled trials
Rishi Jobanputra, Jack A. Sargeant, Abdullah Almaqhawi, Ehtasham Ahmad, Franciskos Arsenyadis, David R. Webb, Louisa Y. Herring, Kamlesh Khunti, Melanie J. Davies, Thomas Yates
Obesity Reviews.2023;[Epub] CrossRef - Combination of exercise and GLP-1 receptor agonist treatment reduces severity of metabolic syndrome, abdominal obesity, and inflammation: a randomized controlled trial
Rasmus M. Sandsdal, Christian R. Juhl, Simon B. K. Jensen, Julie R. Lundgren, Charlotte Janus, Martin B. Blond, Mads Rosenkilde, Adrian F. Bogh, Lasse Gliemann, Jens-Erik B. Jensen, Charalambos Antoniades, Bente M. Stallknecht, Jens J. Holst, Sten Madsbad
Cardiovascular Diabetology.2023;[Epub] CrossRef - Impact of novel glucose‐lowering therapies on physical function in people with type 2 diabetes: A systematic review and meta‐analysis of randomised placebo‐controlled trials
Ehtasham Ahmad, Franciskos Arsenyadis, Abdullah Almaqhawi, Mary Barker, Rishi Jobanputra, Jack A. Sargeant, David R. Webb, Thomas Yates, Melanie J. Davies
Diabetic Medicine.2023;[Epub] CrossRef - Cancer cachexia as a blueprint for treating obesity
Nikolai P. Jaschke, Tilman D. Rachner
Trends in Endocrinology & Metabolism.2023; 34(7): 395. CrossRef - The sun is rising on a new era of pharmacotherapy for obesity: some words of caution
Peter N. Benotti, Bruce R. Bistrian
Surgery for Obesity and Related Diseases.2023; 19(9): 1075. CrossRef - Liraglutide Protects Against Diastolic Dysfunction and Improves Ventricular Protein Translation
Cody Rutledge, Angela Enriquez, Kevin Redding, Mabel Lopez, Steven Mullett, Stacy L. Gelhaus, Michael Jurczak, Eric Goetzman, Brett A. Kaufman
Cardiovascular Drugs and Therapy.2023;[Epub] CrossRef - Effect of sodium-glucose transporter 2 inhibitors on sarcopenia in patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Sha Zhang, Zhan Qi, Yidong Wang, Danfei Song, Deqiu Zhu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cysteine‐lowering treatment with mesna against obesity: Proof of concept and results from a human phase I, dose‐finding study
Kathrine J. Vinknes, Thomas Olsen, Hasse Khiabani Zaré, Nasser E. Bastani, Emma Stolt, Anja F. Dahl, Roger D. Cox, Helga Refsum, Kjetil Retterstøl, Anders Åsberg, Amany Elshorbagy
Diabetes, Obesity and Metabolism.2023; 25(11): 3161. CrossRef - Repurposing Drugs for Diabetes Mellitus as Potential Pharmacological Treatments for Sarcopenia – A Narrative Review
Miles D. Witham, Antoneta Granic, Ewan Pearson, Sian M. Robinson, Avan A. Sayer
Drugs & Aging.2023; 40(8): 703. CrossRef - Introduction to the dietary management of obesity in adults
Vivian Lee
Clinical Medicine.2023; 23(4): 304. CrossRef - Efficacy and safety of the sodium‐glucose co‐transporter‐2 inhibitor empagliflozin in elderly Japanese adults (≥65 years) with type 2 diabetes: A randomized, double‐blind, placebo‐controlled, 52‐week clinical trial (EMPA‐ELDERLY)
Daisuke Yabe, Kosuke Shiki, Gosuke Homma, Thomas Meinicke, Yuji Ogura, Yutaka Seino
Diabetes, Obesity and Metabolism.2023; 25(12): 3538. CrossRef - Independent Link Between Use of Mineralocorticoid Receptor Antagonists and Muscle Wasting in Heart Failure Patients Not Receiving Renin-Angiotensin System Inhibitors
Ryo Numazawa, Satoshi Katano, Toshiyuki Yano, Ryohei Nagaoka, Katsuhiko Ohori, Hidemichi Kouzu, Suguru Honma, Yusuke Fujisawa, Kotaro Yamano, Arata Osanami, Masayuki Koyama, Akiyoshi Hashimoto, Masato Furuhashi
Circulation Journal.2023; 88(1): 10. CrossRef - Sodium-glucose co-transporter 2 inhibitors and Sarcopenia: A controversy that must be solved
Baris Afsar, Rengin Elsurer Afsar
Clinical Nutrition.2023; 42(12): 2338. CrossRef - Oral semaglutide improves body composition and preserves lean mass in patients with type 2 diabetes: a 26-week prospective real-life study
Sara Volpe, Giuseppe Lisco, Margherita Fanelli, Davide Racaniello, Valentina Colaianni, Valentina Lavarra, Domenico Triggiani, Lucilla Crudele, Vincenzo Triggiani, Carlo Sabbà, Giovanni De Pergola, Giuseppina Piazzolla
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Effects of Sodium–Glucose Cotransporter 2 Inhibitors on Body Composition in Type 2 Diabetes Mellitus: A Narrative Review
Soodeh Jahangiri, Mojtaba Malek, Sanjay Kalra, Mohammad E. Khamseh
Diabetes Therapy.2023; 14(12): 2015. CrossRef - Relationship between sodium–glucose cotransporter-2 inhibitors and muscle atrophy in patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Chengdong Xia, Yufeng Han, Chunhui Yin, Ruyue Geng, Zhenfei Liu, Yongle Du, Mingkun Yu
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Role of Lifestyle Modification with Second-Generation Anti-obesity Medications: Comparisons, Questions, and Clinical Opportunities
Thomas A. Wadden, Ariana M. Chao, Molly Moore, Jena S. Tronieri, Adam Gilden, Anastassia Amaro, Sharon Leonard, John M. Jakicic
Current Obesity Reports.2023; 12(4): 453. CrossRef - Sarcopenia and Diabetes: A Detrimental Liaison of Advancing Age
Giuseppe Lisco, Olga Eugenia Disoteo, Anna De Tullio, Vincenzo De Geronimo, Vito Angelo Giagulli, Fabio Monzani, Emilio Jirillo, Renato Cozzi, Edoardo Guastamacchia, Giovanni De Pergola, Vincenzo Triggiani
Nutrients.2023; 16(1): 63. CrossRef - Novel Antidiabetic Strategies and Diabetologists' Views in Nonalcoholic Steatohepatitis
Sabine Kahl, Jennifer Pützer, Michael Roden
Seminars in Liver Disease.2022; 42(01): 048. CrossRef - Effect of Empagliflozin Versus Placebo on Body Fluid Balance in Patients With Acute Myocardial Infarction and Type 2 Diabetes Mellitus: Subgroup Analysis of the EMBODY Trial
Yu Hoshika, Yoshiaki Kubota, Kosuke Mozawa, Shuhei Tara, Yukichi Tokita, Kenji Yodogawa, Yu-Ki Iwasaki, Takeshi Yamamoto, Hitoshi Takano, Yayoi Tsukada, Kuniya Asai, Masaaki Miyamoto, Yasushi Miyauchi, Eitaro Kodani, Mitsunori Maruyama, Jun Tanabe, Wataru
Journal of Cardiac Failure.2022; 28(1): 56. CrossRef - Effect of GLP-1 receptor agonist, liraglutide, on muscle in spontaneously diabetic torii fatty rats
Shohei Yamada, Yuji Ogura, Kazuho Inoue, Jun Tanabe, Takeshi Sugaya, Keiichi Ohata, Yoshio Nagai, Yasunori Natsuki, Seiko Hoshino, Shiika Watanabe, Daisuke Ichikawa, Kenjiro Kimura, Yugo Shibagaki, Atsuko Kamijo-Ikemori
Molecular and Cellular Endocrinology.2022; 539: 111472. CrossRef - Exendin-4 alleviates steatosis in an in vitro cell model by lowering FABP1 and FOXA1 expression via the Wnt/-catenin signaling pathway
Olfa Khalifa, Neyla S. AL-Akl, Khaoula Errafii, Abdelilah Arredouani
Scientific Reports.2022;[Epub] CrossRef - Body composition changes at 12 months following different surgical weight loss interventions in adults with obesity: A systematic review and meta‐analysis of randomized control trials
Amy Sylivris, Jakub Mesinovic, David Scott, Paul Jansons
Obesity Reviews.2022;[Epub] CrossRef - Safety and effectiveness of empagliflozin in Japanese patients with type 2 diabetes: final results of a 3-year post-marketing surveillance study
Kohei Kaku, Kazuhiro Yamamoto, Yumiko Fukushima, Hristo Lliev, Atsutaka Yasui
Expert Opinion on Drug Safety.2022; 21(10): 1315. CrossRef - Safety and effectiveness of empagliflozin according to body mass index in Japanese patients with type 2 diabetes: a subgroup analysis of a 3-year post-marketing surveillance study
Kohei Kaku, Kazuhiro Yamamoto, Yumiko Fukushima, Seiko Mizuno, Daisuke Nitta
Expert Opinion on Drug Safety.2022; 21(11): 1411. CrossRef - Le risque de dénutrition chez le sujet âgé diabétique : une limite à l’utilisation des « nouvelles » classes thérapeutiques ?
Lyse Bordier, Jean Doucet, Bernard Bauduceau
Médecine des Maladies Métaboliques.2022; 16(5): 422. CrossRef - Emerging evidence of the relationship between fat-free mass and ghrelin, glucagon-like peptide-1, and peptide-YY
Austin J. Graybeal, Jada L. Willis, Elisa Morales-Marroquin, Grant M. Tinsley, Sarah E. Messiah, Meena Shah
Nutrition.2022; 103-104: 111815. CrossRef - The Effectiveness of GLP-1 Receptor Agonist Semaglutide on Body Composition in Elderly Obese Diabetic Patients: A Pilot Study
Yoshinori Ozeki, Takayuki Masaki, Akari Kamata, Shotaro Miyamoto, Yuichi Yoshida, Mitsuhiro Okamoto, Koro Gotoh, Hirotaka Shibata
Medicines.2022; 9(9): 47. CrossRef - Distribution of lean mass and mortality risk in patients with type 2 diabetes
Li Ding, Yuxin Fan, Jingting Qiao, Jing He, Ruodan Wang, Qing He, Jingqiu Cui, Zhongshu Ma, Fangqiu Zheng, Hua Gao, Chenlin Dai, Hongyan Wei, Jun Li, Yuming Cao, Gang Hu, Ming Liu
Primary Care Diabetes.2022; 16(6): 824. CrossRef - Cardio-sarcopenia: A syndrome of concern in aging
De Rong Loh, Ru-San Tan, Wee Shiong Lim, Angela S. Koh
Frontiers in Medicine.2022;[Epub] CrossRef - Type 2 diabetes
Ehtasham Ahmad, Soo Lim, Roberta Lamptey, David R Webb, Melanie J Davies
The Lancet.2022; 400(10365): 1803. CrossRef - Elevated circulating level of β-aminoisobutyric acid (BAIBA) in heart failure patients with type 2 diabetes receiving sodium-glucose cotransporter 2 inhibitors
Satoshi Katano, Toshiyuki Yano, Hidemichi Kouzu, Ryohei Nagaoka, Ryo Numazawa, Kotaro Yamano, Yusuke Fujisawa, Katsuhiko Ohori, Nobutaka Nagano, Takefumi Fujito, Ryo Nishikawa, Wataru Ohwada, Masaki Katayose, Tatsuya Sato, Atsushi Kuno, Masato Furuhashi
Cardiovascular Diabetology.2022;[Epub] CrossRef - An overview of anamorelin as a treatment option for cancer-associated anorexia and cachexia
Guilherme Wesley Peixoto Da Fonseca, Stephan von Haehling
Expert Opinion on Pharmacotherapy.2021; 22(7): 889. CrossRef - Liraglutide Does Not Adversely Impact Fat‐Free Mass Loss
Andrew Grannell, William P. Martin, Babak Dehestani, Werd Al‐Najim, John C. Murphy, Carel W. le Roux
Obesity.2021; 29(3): 529. CrossRef - Rationale and design of the EMPA-ELDERLY trial: a randomised, double-blind, placebo-controlled, 52-week clinical trial of the efficacy and safety of the sodium–glucose cotransporter-2 inhibitor empagliflozin in elderly Japanese patients with type 2 diabet
Daisuke Yabe, Kosuke Shiki, Keiko Suzaki, Thomas Meinicke, Yutaro Kotobuki, Kenichiro Nishida, Douglas Clark, Atsutaka Yasui, Yutaka Seino
BMJ Open.2021; 11(4): e045844. CrossRef - Cancer Risk in Normal Weight Individuals with Metabolic Obesity: A Narrative Review
Bethina Liu, Hugh E. Giffney, Rhonda S. Arthur, Thomas E. Rohan, Andrew J. Dannenberg
Cancer Prevention Research.2021; 14(5): 509. CrossRef - Comprehensive analysis of LncRNAs expression profiles in an in vitro model of steatosis treated with Exendin-4
Khaoula Errafii, Neyla S. Al-Akl, Olfa Khalifa, Abdelilah Arredouani
Journal of Translational Medicine.2021;[Epub] CrossRef - Dapagliflozin increases the lean-to total mass ratio in type 2 diabetes mellitus
Vaneza Lira W. Wolf, Ikaro Breder, Luiz Sérgio F. de Carvalho, Alexandre A. S. Soares, Riobaldo M. Cintra, Joaquim Barreto, Daniel B. Munhoz, Sheila T. Kimura-Medorima, Wilson Nadruz, Gil Guerra-Júnior, Thiago Quinaglia, Elza Muscelli, Andrei C. Sposito
Nutrition & Diabetes.2021;[Epub] CrossRef - Optimising the Heart Failure Treatment Pathway: The Role of SGLT2 Inhibitors
Marc Evans, Angharad R. Morgan, Zaheer Yousef, Gethin Ellis, Umesh Dashora, Dipesh C. Patel, Pam Brown, Wasim Hanif, Johnathan N. Townend, Naresh Kanumilli, Jim Moore, John P. H. Wilding, Stephen C. Bain
Drugs.2021; 81(11): 1243. CrossRef - Glucose-lowering Drugs and Hospitalization for Heart Failure: A Systematic Review and Additive-effects Network Meta-analysis With More Than 500 000 Patient-years
Riobaldo M Cintra, Ana Claudia Nogueira, Isabella Bonilha, Beatriz M Luchiari, Otavio R Coelho-Filho, Otavio R Coelho, Pedro Schwartzmann, Elza Muscellie, Wilson Nadruz, Luiz Sergio F Carvalho, Andrei C Sposito
The Journal of Clinical Endocrinology & Metabolism.2021; 106(10): 3060. CrossRef - Physical activity and exercise in the management of type 2 diabetes: where to start?
Deirdre Harrington, Joe Henson
Practical Diabetes.2021; 38(5): 35. CrossRef - Efpeglenatide and Heart and Kidney Outcomes in Type 2 Diabetes
New England Journal of Medicine.2021; 385(22): 2105. CrossRef - Effects of Antidiabetic Drugs on Muscle Mass in Type 2 Diabetes Mellitus
Satoshi Ida, Ryutaro Kaneko, Kanako Imataka, Kaoru Okubo, Yoshitaka Shirakura, Kentaro Azuma, Ryoko Fujiwara, Kazuya Murata
Current Diabetes Reviews.2021; 17(3): 293. CrossRef - Effects of liraglutide and empagliflozin added to insulin therapy in patients with type 2 diabetes: A randomized controlled study
Hirotatsu Nakaguchi, Yoshinobu Kondo, Mayu Kyohara, Hiromi Konishi, Koji Oiwa, Yasuo Terauchi
Journal of Diabetes Investigation.2020; 11(6): 1542. CrossRef - Sodium Glucose Co-Transporter 2 Inhibition Does Not Favorably Modify the Physiological Responses to Dietary Counselling in Diabetes-Free, Sedentary Overweight and Obese Adult Humans
Shane P.P. Ryan, Alissa A. Newman, Jessie R. Wilburn, Lauren D. Rhoades, S. Raj J. Trikha, Ellen C. Godwin, Hayden M. Schoenberg, Micah L. Battson, Taylor R. Ewell, Gary J. Luckasen, Laurie M. Biela, Christopher L. Melby, Christopher Bell
Nutrients.2020; 12(2): 510. CrossRef - GLP-1 Receptor Agonist Treatment in Morbid Obesity and Type 2 Diabetes Due to Pathogenic Homozygous Melanocortin-4 Receptor Mutation: A Case Report
Eva W. Iepsen, Christian T. Have, Simon Veedfald, Sten Madsbad, Jens J. Holst, Niels Grarup, Oluf Pedersen, Ivan Brandslund, Jens-Christian Holm, Torben Hansen, Signe S. Torekov
Cell Reports Medicine.2020; 1(1): 100006. CrossRef - Glucagon‐like peptide 1 infusions overcome anabolic resistance to feeding in older human muscle
Haitham Abdulla, Bethan E. Phillips, Daniel J. Wilkinson, Marie Limb, Tereza Jandova, Joseph J. Bass, Debbie Rankin, Jessica Cegielski, Mariwan Sayda, Hannah Crossland, John P. Williams, Kenneth Smith, Iskandar Idris, Philip J. Atherton
Aging Cell.2020;[Epub] CrossRef
- Drug‐related sarcopenia as a secondary sarcopenia

- Effects of Incretin-Based Therapies on Diabetic Microvascular Complications
- Yu Mi Kang, Chang Hee Jung
- Endocrinol Metab. 2017;32(3):316-325. Published online September 18, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.3.316
- 4,633 View
- 55 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The morbidity and mortality associated with diabetic complications impose a huge socioeconomic burden worldwide. Therefore, the ultimate goal of managing diabetes mellitus (DM) is to lower the risk of macrovascular complications and highly morbid microvascular complications such as diabetic nephropathy (DN) and diabetic retinopathy (DR). Potential benefits of incretin-based therapies such as glucagon-like peptide 1 receptor agonists (GLP-1 RAs) and dipeptidyl peptidase-4 (DPP-4) inhibitors on the diabetic macrovascular complications have been recently suggested, owing to their pleiotropic effects on multiple organ systems. However, studies primarily investigating the role of these therapies in diabetic microvascular complications are rare. Nevertheless, preclinical and limited clinical data suggest the potential protective effect of incretin-based agents against DN and DR via their anti-inflammatory, antioxidative, and antiapoptotic properties. Evidence also suggests that these incretin-dependent and independent beneficial effects are not necessarily associated with the glucose-lowering properties of GLP-1 RAs and DPP-4 inhibitors. Hence, in this review, we revisit the preclinical and clinical evidence of incretin-based therapy for DR and DN, the two most common, morbid complications in individuals with DM. In addition, the review discusses a few recent studies raising concerns of aggravating DR with the use of incretin-based therapies.
-
Citations
Citations to this article as recorded by- Efficacy and Safety of the Utilization of Dipeptidyl Peptidase IV Inhibitors in Diabetic Patients with Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical Trials
Moeber Mahzari, Muhannad Alqirnas, Moustafa Alhamadh, Faisal Alrasheed, Abdulrahman Alhabeeb, Wedad Al Madani, Hussain Aldera
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 1425. CrossRef - Anti-Inflammatory Effects of GLP-1R Activation in the Retina
Alessandra Puddu, Davide Maggi
International Journal of Molecular Sciences.2022; 23(20): 12428. CrossRef - Diabetes and Its Complications: Therapies Available, Anticipated and Aspired
Anu Grover, Komal Sharma, Suresh Gautam, Srishti Gautam, Monica Gulati, Sachin Kumar Singh
Current Diabetes Reviews.2021; 17(4): 397. CrossRef - SGLT2 Inhibitors, GLP-1 Agonists, and DPP-4 Inhibitors in Diabetes and Microvascular Complications: A Review
Christopher El Mouhayyar, Ruba Riachy, Abir Bou Khalil, Asaad Eid, Sami Azar
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Novel therapeutic agents for the treatment of diabetic kidney disease
Rachel E. Hartman, P.S.S. Rao, Mariann D. Churchwell, Susan J. Lewis
Expert Opinion on Investigational Drugs.2020; 29(11): 1277. CrossRef - Nationwide Trends in Pancreatitis and Pancreatic Cancer Risk Among Patients With Newly Diagnosed Type 2 Diabetes Receiving Dipeptidyl Peptidase 4 Inhibitors
Minyoung Lee, Jiyu Sun, Minkyung Han, Yongin Cho, Ji-Yeon Lee, Chung Mo Nam, Eun Seok Kang
Diabetes Care.2019; 42(11): 2057. CrossRef - Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2019; 34(1): 80. CrossRef - Serum adipocytokines are associated with microalbuminuria in patients with type 1 diabetes and incipient chronic complications
Tomislav Bulum, Marijana Vučić Lovrenčić, Martina Tomić, Sandra Vučković-Rebrina, Vinko Roso, Branko Kolarić, Vladimir Vuksan, Lea Duvnjak
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 496. CrossRef - Protective Effects of Incretin Against Age-Related Diseases
Di Zhang, Mingzhu Ma, Yueze Liu
Current Drug Delivery.2019; 16(9): 793. CrossRef - The role of dipeptidylpeptidase-4 inhibitors in management of cardiovascular disease in diabetes; focus on linagliptin
Annayya R. Aroor, Camila Manrique-Acevedo, Vincent G. DeMarco
Cardiovascular Diabetology.2018;[Epub] CrossRef
- Efficacy and Safety of the Utilization of Dipeptidyl Peptidase IV Inhibitors in Diabetic Patients with Chronic Kidney Disease: A Meta-Analysis of Randomized Clinical Trials

- New Potential Targets of Glucagon-Like Peptide 1 Receptor Agonists in Pancreatic β-Cells and Hepatocytes
- Won-Young Lee
- Endocrinol Metab. 2017;32(1):1-5. Published online February 6, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.1
- 4,224 View
- 43 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader It is well known that both insulin resistance and decreased insulin secretory capacity are important factors in the pathogenesis of type 2 diabetes mellitus (T2DM). In addition to genetic factors, obesity and lipotoxicity can increase the risk of T2DM. Glucagon-like peptide 1 (GLP-1) receptor agonists are novel antidiabetic drugs with multiple effects. They can stimulate glucose-dependent insulin secretion, inhibit postprandial glucagon release, delay gastric emptying, and induce pancreatic β-cell proliferation. They can also reduce the weight of patients with T2DM and relieve lipotoxicity at the cellular level. Many intracellular targets of GLP-1 have been found, but more remain to be identified. Elucidating these targets could be a basis for developing new potential drugs. My colleagues and I have investigated new targets of GLP-1, with a particular focus on pancreatic β-cell lines and hepatic cell lines. Herein, I summarize the recent work from my laboratory, with profound gratitude for receiving the prestigious 2016 Namgok Award.
-
Citations
Citations to this article as recorded by- Venom Peptides, Polyphenols and Alkaloids: Are They the Next Antidiabetics That Will Preserve β-Cell Mass and Function in Type 2 Diabetes?
Michele Lodato, Valérie Plaisance, Valérie Pawlowski, Maxime Kwapich, Alexandre Barras, Emeline Buissart, Stéphane Dalle, Sabine Szunerits, Jérôme Vicogne, Rabah Boukherroub, Amar Abderrahmani
Cells.2023; 12(6): 940. CrossRef - Diabetes, Incretin Therapy and Thoracic Aortic Aneurysm – What Does the Evidence Show?
Camilla Krizhanovskii , Anders Franco-Cereceda
Current Vascular Pharmacology.2019; 17(5): 432. CrossRef - Toll-like receptor 4 is necessary for glucose-dependent glucagon-like peptide-1 secretion in male mice
Lijuan Wang, Xiandong Zhan, Zhenhui Wang, Jing Ma, Xiaotong Chang, Xiaobo Zhu
Biochemical and Biophysical Research Communications.2019; 510(1): 104. CrossRef
- Venom Peptides, Polyphenols and Alkaloids: Are They the Next Antidiabetics That Will Preserve β-Cell Mass and Function in Type 2 Diabetes?

- Clinical Study
- Correlation of Glypican-4 Level with Basal Active Glucagon-Like Peptide 1 Level in Patients with Type 2 Diabetes Mellitus
- Sang Ah Lee, Gwanpyo Koh, Suk Ju Cho, So-Yeon Yoo, Sang Ouk Chin
- Endocrinol Metab. 2016;31(3):439-445. Published online September 26, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.439
- 4,078 View
- 41 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Previous studies have reported that glypican-4 (GPC4) regulates insulin signaling by interacting with insulin receptor and through adipocyte differentiation. However, GPC4 has not been studied with regard to its effects on clinical factors in patients with type 2 diabetes mellitus (T2DM). We aimed to identify factors associated with GPC4 level in T2DM.
Methods Between January 2010 and December 2013, we selected 152 subjects with T2DM and collected serum and plasma into tubes pretreated with aprotinin and dipeptidyl peptidase-4 inhibitor to preserve active gastric inhibitory polypeptide (GIP) and glucagon-like peptide 1 (GLP-1). GPC4, active GLP-1, active GIP, and other factors were measured in these plasma samples. We performed a linear regression analysis to identify factors associated with GPC4 level.
Results The subjects had a mean age of 58.1 years, were mildly obese (mean body mass index [BMI], 26.1 kg/m2), had T2DM of long-duration (mean, 101.3 months), glycated hemoglobin 7.5%, low insulin secretion, and low insulin resistance (mean homeostatic model assessment of insulin resistance [HOMA-IR], 1.2). Their mean GPC4 was 2.0±0.2 ng/mL. In multivariate analysis, GPC4 was independently associated with age (β=0.224,
P =0.009), and levels of active GLP-1 (β=0.171,P =0.049) and aspartate aminotransferase (AST; β=–0.176,P =0.043) after being adjusted for other clinical factors.Conclusion GPC4 was independently associated with age, active GLP-1, and AST in T2DM patients, but was not associated with HOMA-IR and BMI, which are well known factors related to GPC4. Further study is needed to identify the mechanisms of the association between GPC4 and basal active GLP-1 levels.
-
Citations
Citations to this article as recorded by- How Reliable are Commercially Available Glypican4 ELISA
Kits?
Joseph P. Buhl, Antje Garten, Jürgen Kratzsch, Wieland Kiess, Melanie Penke
Experimental and Clinical Endocrinology & Diabetes.2022; 130(02): 110. CrossRef - Serum glypican-4 is associated with the 10-year clinical outcome of patients with peripheral artery disease
Axel Muendlein, Christine Heinzle, Andreas Leiherer, Kathrin Geiger, Eva Maria Brandtner, Stella Gaenger, Peter Fraunberger, Christoph H. Saely, Heinz Drexel
International Journal of Cardiology.2022; 369: 54. CrossRef - Berberine activates the β-catenin/TCF4 signaling pathway by down-regulating miR-106b to promote GLP-1 production by intestinal L cells
Jiao Wang, Li-Rui Wei, Yan-Ling Liu, Cheng-Zhi Ding, Feng Guo, Jiao Wang, Qian Qin, Feng-Jiao Huang, Ying Xin, Sheng-Nan Ma, Qiu-Ran Zhai, Shou-Jun Wang, Gui-Jun Qin
European Journal of Pharmacology.2021; 911: 174482. CrossRef - Increased Glypican-4 Levels Are Associated with Obesity in Adolescents
Huseyin Dag, Nevin Cetin Dag, Okan Dikker
Iranian Journal of Pediatrics.2019;[Epub] CrossRef - Serum glypican 4 level in obese children and its relation to degree of obesity
Chutima Leelalertlauw, Manassawee Korwutthikulrangsri, Pat Mahachoklertwattana, Suwannee Chanprasertyothin, Patcharin Khlairit, Sarunyu Pongratanakul, Preamrudee Poomthavorn
Clinical Endocrinology.2017; 87(6): 689. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Efficacy and Safety of Single‐ or Double‐Drug Antidiabetic Regimens in the Treatment of Type 2 Diabetes Mellitus: A Network Meta‐Analysis
Xi‐Ling Yang, Mi‐Ma Duo‐Ji, Zi‐Wen Long
Journal of Cellular Biochemistry.2017; 118(12): 4536. CrossRef
- How Reliable are Commercially Available Glypican4 ELISA
Kits?


 KES
KES

 First
First Prev
Prev



