Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
- Renal Protection of Mineralocorticoid Receptor Antagonist, Finerenone, in Diabetic Kidney Disease
- Dong-Lim Kim, Seung-Eun Lee, Nan Hee Kim
- Endocrinol Metab. 2023;38(1):43-55. Published online February 27, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1629
- 5,540 View
- 763 Download
- 5 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
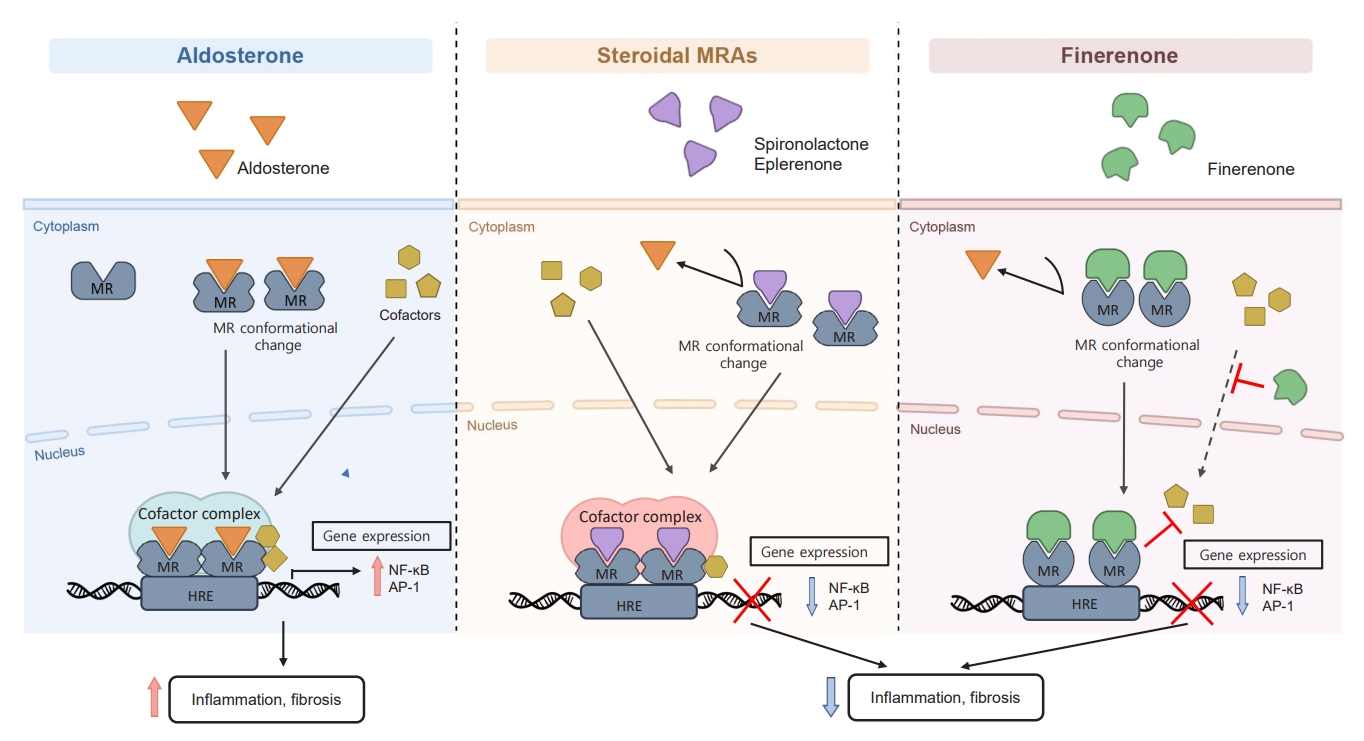
ePub - Chronic kidney disease (CKD) is the most common cause of end-stage renal disease in patients with type 2 diabetes mellitus (T2DM). CKD increases the risk of cardiovascular diseases; therefore, its prevention and treatment are important. The prevention of diabetic kidney disease (DKD) can be achieved through intensive glycemic control and blood pressure management. Additionally, DKD treatment aims to reduce albuminuria and improve kidney function. In patients with T2DM, renin-angiotensin-aldosterone system inhibitors, sodium glucose cotransporter 2 inhibitors, and glucagon-like peptide-1 receptor agonists can delay the progression of DKD. Hence, there is a need for novel treatments that can effectively suppress DKD progression. Finerenone is a first-in-class nonsteroidal mineralocorticoid receptor antagonist with clinically proven efficacy in improving albuminuria, estimated glomerular filtration rate, and risk of cardiovascular events in early and advanced DKD. Therefore, finerenone is a promising treatment option to delay DKD progression. This article reviews the mechanism of renal effects and major clinical outcomes of finerenone in DKD.
-
Citations
Citations to this article as recorded by- Neue Antihypertensiva im Renin-Angiotensin-Aldosteron-System
Markus van der Giet
CardioVasc.2024; 24(1): 33. CrossRef -
Chicoric acid
advanced PAQR3 ubiquitination to ameliorate ferroptosis in diabetes nephropathy through the relieving of the interaction between PAQR3 and P110α pathway
Weiwei Zhang, Yong Liu, Jiajun Zhou, Teng Qiu, Haitang Xie, Zhichen Pu
Clinical and Experimental Hypertension.2024;[Epub] CrossRef - Endothelial CXCR2 deficiency attenuates renal inflammation and glycocalyx shedding through NF-κB signaling in diabetic kidney disease
Siyuan Cui, Xin Chen, Jiayu Li, Wei Wang, Deqi Meng, Shenglong Zhu, Shiwei Shen
Cell Communication and Signaling.2024;[Epub] CrossRef - Molecular Targets of Novel Therapeutics for Diabetic Kidney Disease: A New Era of Nephroprotection
Alessio Mazzieri, Francesca Porcellati, Francesca Timio, Gianpaolo Reboldi
International Journal of Molecular Sciences.2024; 25(7): 3969. CrossRef - Epigenetic modification in diabetic kidney disease
Zhe Liu, Jiahui Liu, Wanning Wang, Xingna An, Ling Luo, Dehai Yu, Weixia Sun
Frontiers in Endocrinology.2023;[Epub] CrossRef - Novel Approaches in Chronic Renal Failure without Renal Replacement Therapy: A Review
Sandra Martínez-Hernández, Martín Muñoz-Ortega, Manuel Ávila-Blanco, Mariana Medina-Pizaño, Javier Ventura-Juárez
Biomedicines.2023; 11(10): 2828. CrossRef - Finerenone and other future therapeutic options for Alport syndrome
Helen Pearce, Holly Mabillard
Journal of Rare Diseases.2023;[Epub] CrossRef
- Neue Antihypertensiva im Renin-Angiotensin-Aldosteron-System

- Diabetes, Obesity and Metabolism
- Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
- Eun-Jung Rhee
- Endocrinol Metab. 2022;37(3):415-429. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.304

- 4,492 View
- 261 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The world is suffering from a rapid increase in the number of people with diabetes due to the increased prevalence of obesity and lengthened life span. Since the development of insulin thanks to the efforts of Prof. Banting and Dr. Best in 1922, for which they won the Nobel Prize, remarkable developments in anti-diabetic medications have dramatically lengthened the lifespan of patients with diabetes. However, the control rate of hyperglycemia in patients with diabetes remains unsatisfactory, since glycemic control requires both medication and lifestyle modifications to slow the deterioration of pancreatic beta-cell function and prevent diabetic complications. From the initial “triumvirate” to the “ominous octet,” and now the “egregious eleven,” the number of organs recognized as being involved in hyperglycemia and diabetes has increased with the development of anti-diabetic medications. Recent unexpected results from outcome trials of anti-diabetic medications have enabled anti-diabetic medications to be indicated for the prevention of chronic kidney disease and heart failure, even in patients without diabetes. In this review, I would like to summarize the extra-glycemic effects of anti-diabetic medications.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Glucagon-Like Peptide Receptor Agonist Inhibits Angiotensin II-Induced Proliferation and Migration in Vascular Smooth Muscle Cells and Ameliorates Phosphate-Induced Vascular Smooth Muscle Cells Calcification
Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2024; 48(1): 83. CrossRef - To do one and to get more: Part I. Diabetes and bone
Wen-Ling Lee, Peng-Hui Wang, Szu-Ting Yang, Chia-Hao Liu, Wen-Hsun Chang, Fa-Kung Lee
Journal of the Chinese Medical Association.2022; 85(10): 965. CrossRef
- Association between underweight and risk of heart failure in diabetes patients

- Diabetes, Obesity and Metabolism
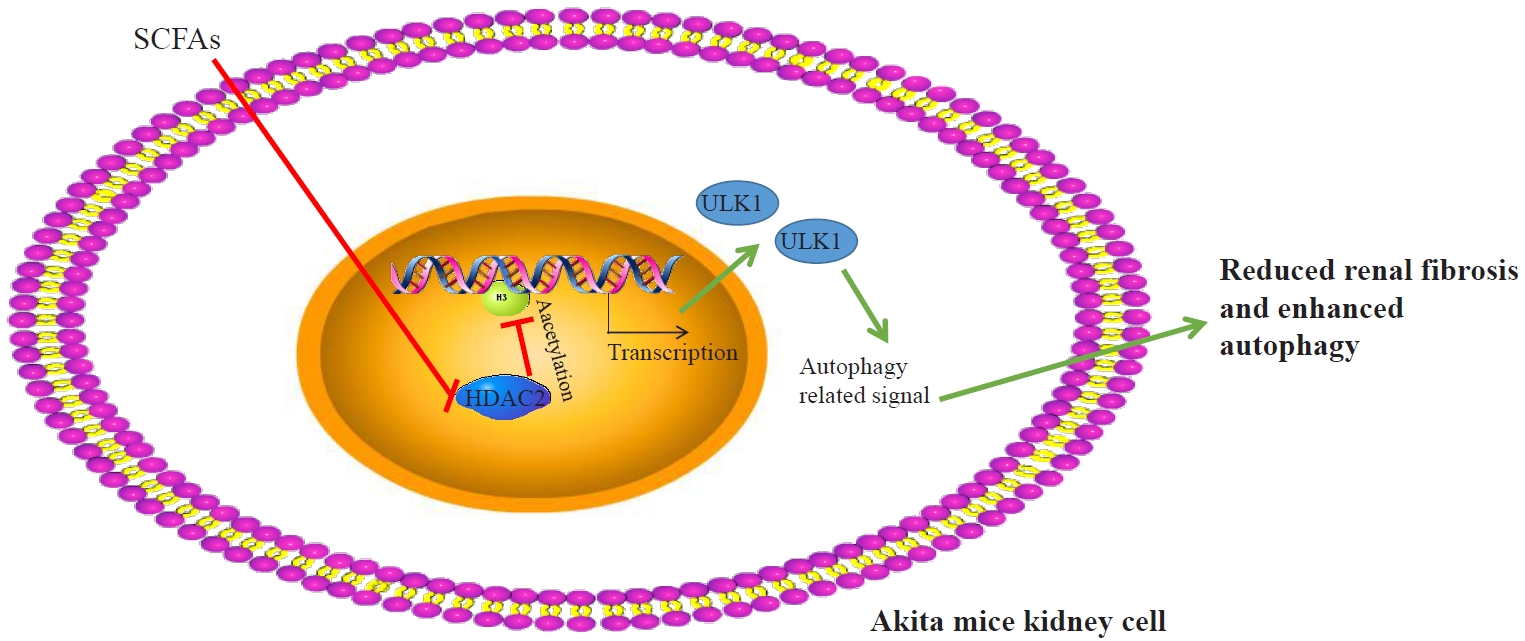
- Short-Chain Fatty Acids Attenuate Renal Fibrosis and Enhance Autophagy of Renal Tubular Cells in Diabetic Mice Through the HDAC2/ULK1 Axis
- Xiaoying Ma, Qiong Wang
- Endocrinol Metab. 2022;37(3):432-443. Published online May 16, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1336
- 7,038 View
- 151 Download
- 10 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study investigated the effect of short-chain fatty acids (SCFAs) on diabetes in a mouse model.
Methods
Autophagy in Akita mice and streptozocin (STZ)-induced diabetic C57BL/6 mice was determined by Western blots and immunohistochemistry (IHC). Western blots, IHC, hematoxylin and eosin staining, Masson staining, periodic acid-Schiff staining, and picrosirius red staining were conducted to detect whether autophagy and renal function improved in Akita mice and STZ-induced diabetic C57BL/6 mice after treatment of SCFAs. Western blots, IHC, and chromatin immunoprecipitation were performed to determine whether SCFAs affected diabetic mice via the histone deacetylase (HDAC2)/unc-51 like autophagy activating kinase 1 (ULK1) axis. Diabetic mice with kidney-specific knockout of HDAC2 were constructed, and IHC, Masson staining, and Western blots were carried out to detect whether the deletion of endogenous HDAC2 contributed to the improvement of autophagy and renal fibrosis in diabetic mice.
Results
Reduced autophagy and severe fibrosis were observed in Akita mice and STZ-induced diabetic C57BL/6 mice. Increased autophagy and reduced renal cell fibrosis were found in SCFA-treated Akita diabetic mice and STZ-induced diabetic C57BL/6 mice. Diabetic mice treated with SCFAs had lower HDAC2 expression and more enriched binding of ULK1 promoter sequences to H3K27Ac. Endogenous knockout of HDAC2 caused enhanced autophagy and decreased renal fibrosis in diabetic mice treated with SCFAs.
Conclusion
SCFAs enhanced autophagy of renal tubular cells and attenuated renal fibrosis in diabetic mice through the HDAC2/ULK1 axis. -
Citations
Citations to this article as recorded by- NSD1 supports cell growth and regulates autophagy in HPV-negative head and neck squamous cell carcinoma
Iuliia Topchu, Igor Bychkov, Demirkan Gursel, Petr Makhov, Yanis Boumber
Cell Death Discovery.2024;[Epub] CrossRef - Dietary fiber intake and its association with diabetic kidney disease in American adults with diabetes: A cross-sectional study
Xin-Hua Jia, Sheng-Yan Wang, Ai-Qin Sun
World Journal of Diabetes.2024; 15(3): 475. CrossRef - Epigenetic and post-translational modifications in autophagy: biological functions and therapeutic targets
Feng Shu, Han Xiao, Qiu-Nuo Li, Xiao-Shuai Ren, Zhi-Gang Liu, Bo-Wen Hu, Hong-Sheng Wang, Hao Wang, Guan-Min Jiang
Signal Transduction and Targeted Therapy.2023;[Epub] CrossRef - Mechanisms of Blood–Brain Barrier Protection by Microbiota-Derived Short-Chain Fatty Acids
Ekaterina Fock, Rimma Parnova
Cells.2023; 12(4): 657. CrossRef - The Role of Histone Modifications in the Pathogenesis of Diabetic Kidney Disease
Christodoula Kourtidou, Konstantinos Tziomalos
International Journal of Molecular Sciences.2023; 24(6): 6007. CrossRef - Mechanism of histone deacetylase HDAC2 in FOXO3-mediated trophoblast pyroptosis in preeclampsia
Jia Liu, Weihui Yang
Functional & Integrative Genomics.2023;[Epub] CrossRef - Macrophage polarization induces endothelium-to-myofibroblast transition in chronic allograft dysfunction
Zeping Gui, Xiang Zhang, Qianguang Han, Zhou Hang, Ruoyun Tan, Min Gu, Zijie Wang
Renal Failure.2023;[Epub] CrossRef - Periodic acid–Schiff staining in oral exfoliative cytology of diabetic patients: The odyssey for noninvasive screening – A systematic review and meta-analysis
KYesoda Aniyan, KrithikaChandrasekar Lakshmi, Anuradha Ganesan
Dental Research Journal.2023; 20(1): 73. CrossRef - Luteolin alleviates renal ischemia-reperfusion injury in streptozotocin induced diabetic rats by inhibiting metalloenzymes expression
Rakesh B. Daude, Jigna S. Shah
Current Issues in Pharmacy and Medical Sciences.2023; 36(4): 199. CrossRef - Molecular mechanisms of histone deacetylases and inhibitors in renal fibrosis progression
Jiayu Wang, Jiaxing Li, Xin Zhang, Min Zhang, Xiaopeng Hu, Hang Yin
Frontiers in Molecular Biosciences.2022;[Epub] CrossRef - Sacubitril/Valsartan contributes to improving the diabetic kidney disease and regulating the gut microbiota in mice
Peipei Wang, Ruixue Guo, Xiwen Bai, Wen Cui, Yiding Zhang, Huangmin Li, Jin Shang, Zhanzheng Zhao
Frontiers in Endocrinology.2022;[Epub] CrossRef - Recent advances and potentiality of postbiotics in the food industry: Composition, inactivation methods, current applications in metabolic syndrome, and future trends
Yujie Zhong, Tao Wang, Ruilin Luo, Jiayu Liu, Ruyi Jin, Xiaoli Peng
Critical Reviews in Food Science and Nutrition.2022; : 1. CrossRef
- NSD1 supports cell growth and regulates autophagy in HPV-negative head and neck squamous cell carcinoma

- Calcium & Bone Metabolism
Big Data Articles (National Health Insurance Service Database) - Hip Fracture Risk According to Diabetic Kidney Disease Phenotype in a Korean Population
- Seung Eun Lee, Juhwan Yoo, Kyoung-Ah Kim, Kyungdo Han, Han Seok Choi
- Endocrinol Metab. 2022;37(1):148-158. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1315
- 3,522 View
- 117 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
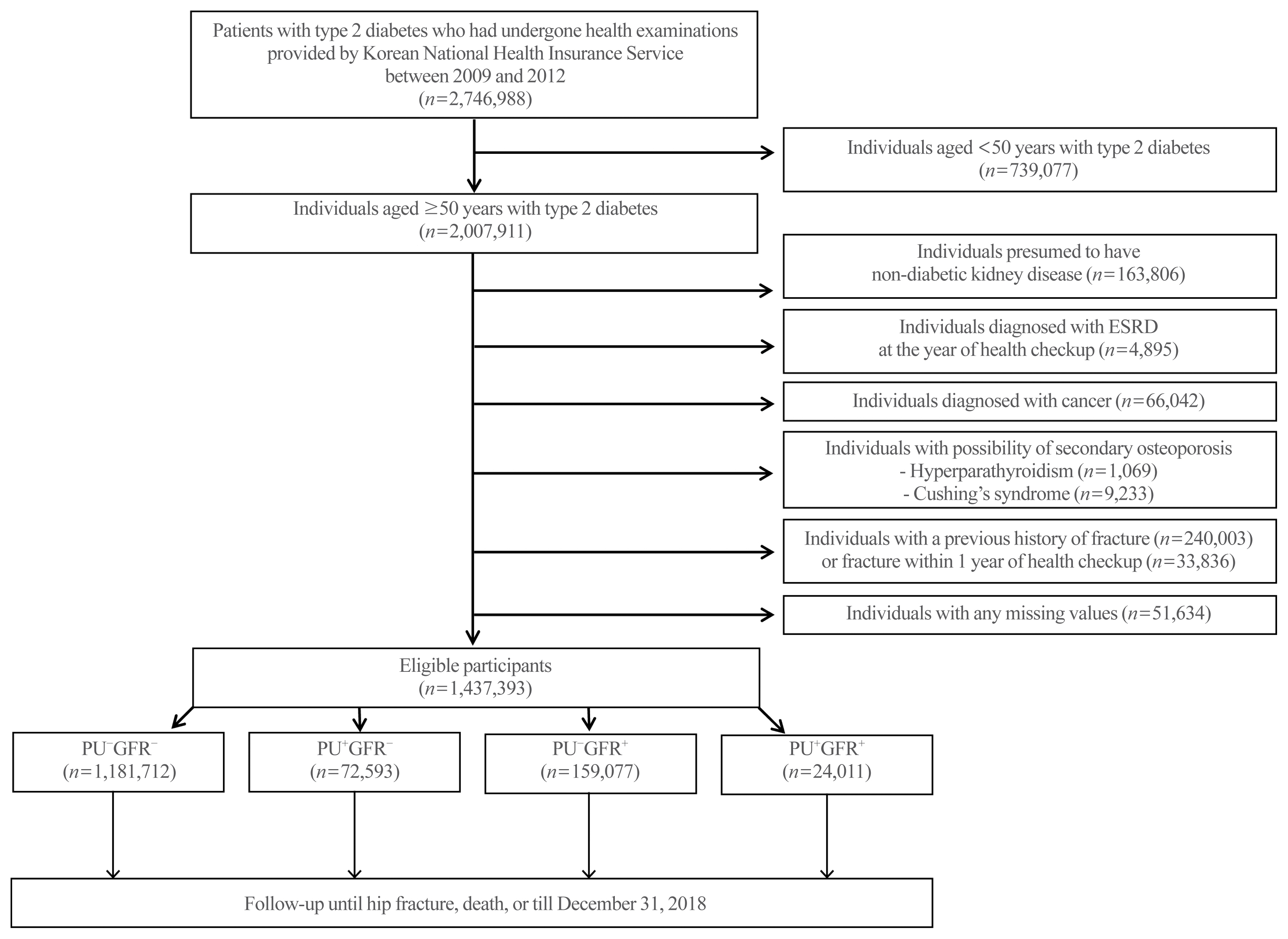
ePub - Background
Diabetic kidney disease (DKD) is associated with an elevated risk of fractures. However, little is known about the association between proteinuric or non-proteinuric DKD and the risk of hip fracture. Thus, we investigated the incidence of hip fractures among Korean adults with type 2 diabetes mellitus (T2DM) stratified by DKD phenotype.
Methods
In this retrospective cohort study using the Korean National Health Insurance Service database, patients with T2DM who received at least one general health checkup between 2009 and 2012 were followed until the date of hip fracture, death, or December 31, 2018. We classified the DKD phenotype by proteinuria and estimated glomerular filtration rate (eGFR), as follows: no DKD (PU−GFR−), proteinuric DKD with normal eGFR (PU+GFR−), non-proteinuric DKD with reduced eGFR (PU−GFR+), and proteinuric DKD with reduced eGFR (PU+GFR+)
Results
The cumulative incidence of hip fractures was highest in the PU+GFR+ group, followed by the PU−GFR+ group and the PU+GFR− group. After adjustment for confounding factors, the hazard ratio (HR) for hip fracture was still highest in the PU+GFR+ group. However, the PU+GFR− group had a higher HR for hip fracture than the PU−GFR+ group (PU+GFR+ : HR, 1.69; 95% confidence interval [CI], 1.57 to 1.81; PU+GFR− : HR, 1.37; 95% CI, 1.30 to 1.46; PU−GFR+ : HR, 1.20; 95% CI, 1.16 to 1.24 using the PU−GFR− group as the reference category).
Conclusion
The present study demonstrated that DKD was significantly associated with a higher risk of hip fracture, with proteinuria as a major determinant. -
Citations
Citations to this article as recorded by- Proteinuria screening and risk of bone fracture: a retrospective cohort study using a nationwide population-based database
Akira Okada, Akira Honda, Hideaki Watanabe, Yusuke Sasabuchi, Shotaro Aso, Kayo Ikeda Kurakawa, Masaomi Nangaku, Toshimasa Yamauchi, Hideo Yasunaga, Hirotaka Chikuda, Takashi Kadowaki, Satoko Yamaguchi
Clinical Kidney Journal.2024;[Epub] CrossRef - Fracture risks associated with sodium-glucose cotransporter-2 inhibitors in type 2 diabetes patients across eGFR and albuminuria categories: A population-based study in Hong Kong
David Tak Wai Lui, Tingting Wu, Eric Ho Man Tang, Ivan Chi Ho Au, Chi Ho Lee, Yu Cho Woo, Kathryn Choon Beng Tan, Carlos King Ho Wong
Diabetes Research and Clinical Practice.2023; 197: 110576. CrossRef - Diagnose und Management der Osteoporose bei Diabetes mellitus (Update 2023)
Christian Muschitz, Alexandra Kautzky-Willer, Yvonne Winhofer, Martina Rauner, Judith Haschka, Daniel Cejka, Robert Wakolbinger-Habel, Peter Pietschmann
Wiener klinische Wochenschrift.2023; 135(S1): 207. CrossRef - Association between exercise and risk of fractures in new-onset type 2 diabetes: a retrospective cohort study
Seung Eun Lee, Juhwan Yoo, Bong-Seong Kim, Kyoung-Ah Kim, Kyungdo Han, Han Seok Choi
Archives of Osteoporosis.2023;[Epub] CrossRef - Two-Year Changes in Diabetic Kidney Disease Phenotype and the Risk of Heart Failure: A Nationwide Population-Based Study in Korea
Seung Eun Lee, Juhwan Yoo, Han Seok Choi, Kyungdo Han, Kyoung-Ah Kim
Diabetes & Metabolism Journal.2023; 47(4): 523. CrossRef
- Proteinuria screening and risk of bone fracture: a retrospective cohort study using a nationwide population-based database

- Diabetes, Obesity and Metabolism
- EW-7197 Attenuates the Progression of Diabetic Nephropathy in db/db Mice through Suppression of Fibrogenesis and Inflammation
- Kyung Bong Ha, Weerapon Sangartit, Ah Reum Jeong, Eun Soo Lee, Hong Min Kim, Soyeon Shim, Upa Kukongviriyapan, Dae-Kee Kim, Eun Young Lee, Choon Hee Chung
- Endocrinol Metab. 2022;37(1):96-111. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1305
- 3,981 View
- 180 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
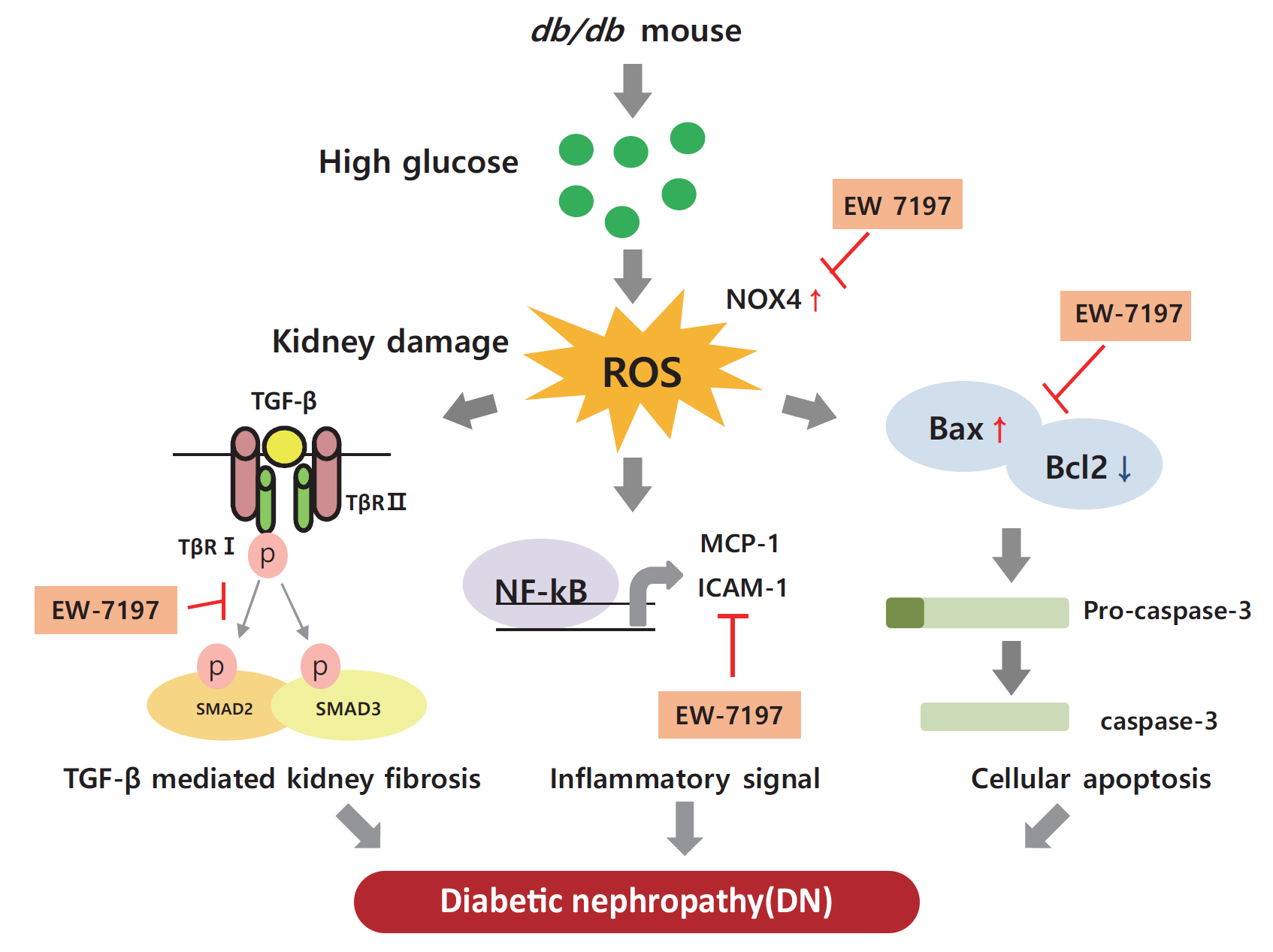
ePub - Background
Diabetic nephropathy (DN) is characterized by albuminuria and accumulation of extracellular matrix (ECM) in kidney. Transforming growth factor-β (TGF-β) plays a central role in promoting ECM accumulation. We aimed to examine the effects of EW-7197, an inhibitor of TGF-β type 1 receptor kinase (ALK5), in retarding the progression of DN, both in vivo, using a diabetic mouse model (db/db mice), and in vitro, in podocytes and mesangial cells.
Methods
In vivo study: 8-week-old db/db mice were orally administered EW-7197 at a dose of 5 or 20 mg/kg/day for 10 weeks. Metabolic parameters and renal function were monitored. Glomerular histomorphology and renal protein expression were evaluated by histochemical staining and Western blot analyses, respectively. In vitro study: DN was induced by high glucose (30 mM) in podocytes and TGF-β (2 ng/mL) in mesangial cells. Cells were treated with EW-7197 (500 nM) for 24 hours and the mechanism associated with the attenuation of DN was investigated.
Results
Enhanced albuminuria and glomerular morphohistological changes were observed in db/db compared to that of the nondiabetic (db/m) mice. These alterations were associated with the activation of the TGF-β signaling pathway. Treatment with EW-7197 significantly inhibited TGF-β signaling, inflammation, apoptosis, reactive oxygen species, and endoplasmic reticulum stress in diabetic mice and renal cells.
Conclusion
EW-7197 exhibits renoprotective effect in DN. EW-7197 alleviates renal fibrosis and inflammation in diabetes by inhibiting downstream TGF-β signaling, thereby retarding the progression of DN. Our study supports EW-7197 as a therapeutically beneficial compound to treat DN. -
Citations
Citations to this article as recorded by- TGF-β signaling in health, disease, and therapeutics
Ziqin Deng, Tao Fan, Chu Xiao, He Tian, Yujia Zheng, Chunxiang Li, Jie He
Signal Transduction and Targeted Therapy.2024;[Epub] CrossRef - Oxidative stress and inflammation in diabetic nephropathy: role of polyphenols
Qi Jin, Tongtong Liu, Yuan Qiao, Donghai Liu, Liping Yang, Huimin Mao, Fang Ma, Yuyang Wang, Liang Peng, Yongli Zhan
Frontiers in Immunology.2023;[Epub] CrossRef - Beneficial Effects of a Curcumin Derivative and Transforming Growth Factor-β Receptor I Inhibitor Combination on Nonalcoholic Steatohepatitis
Kyung Bong Ha, Eun Soo Lee, Na Won Park, Su Ho Jo, Soyeon Shim, Dae-Kee Kim, Chan Mug Ahn, Choon Hee Chung
Diabetes & Metabolism Journal.2023; 47(4): 500. CrossRef
- TGF-β signaling in health, disease, and therapeutics

- Diabetes, Obesity and Metabolism
- Tetrahydrocurcumin Ameliorates Kidney Injury and High Systolic Blood Pressure in High-Fat Diet-Induced Type 2 Diabetic Mice
- Weerapon Sangartit, Kyung Bong Ha, Eun Soo Lee, Hong Min Kim, Upa Kukongviriyapan, Eun Young Lee, Choon Hee Chung
- Endocrinol Metab. 2021;36(4):810-822. Published online August 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.988
- 4,040 View
- 163 Download
- 7 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
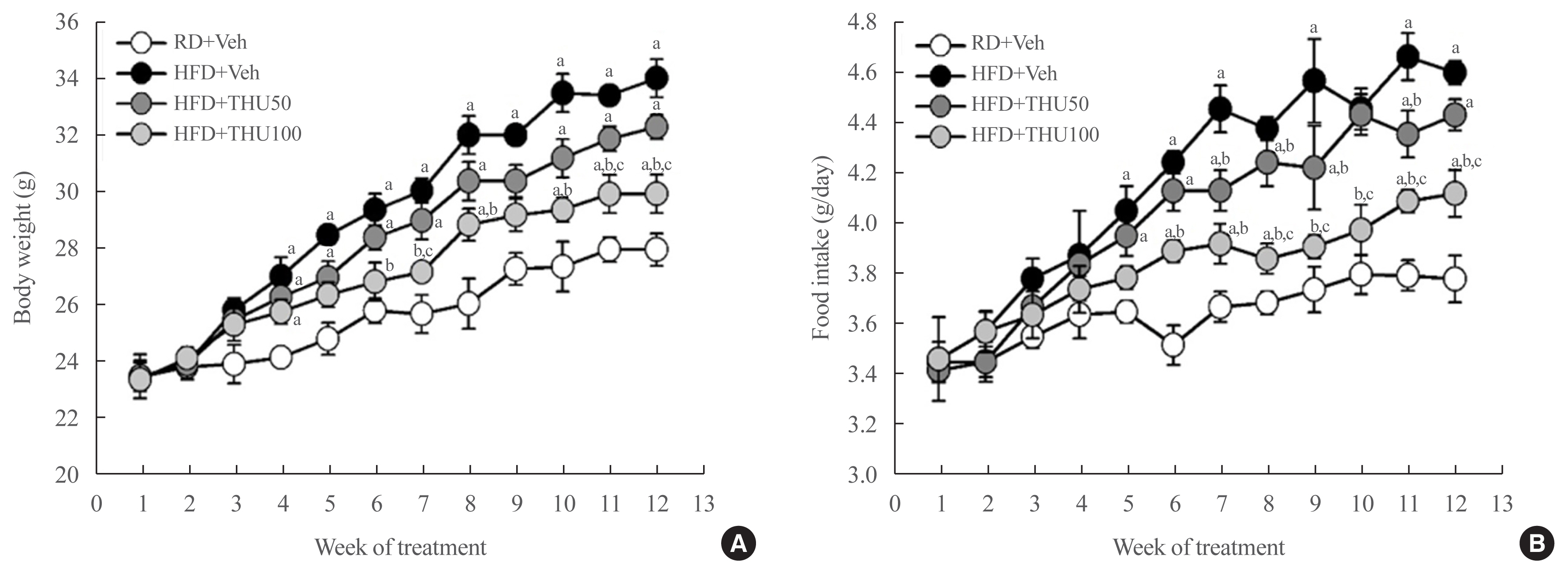
Activation of the intrarenal renin-angiotensin system (RAS) is implicated in the pathogenesis of kidney injury and hypertension. We aimed to investigate the protective effect of tetrahydrocurcumin (THU) on intrarenal RAS expression, kidney injury, and systolic blood pressure (SBP) in high-fat diet (HFD)-induced type 2 diabetic mice.
Methods
Eight-week-old male mice were fed a regular diet (RD) or HFD for 12 weeks, and THU (50 or 100 mg/kg/day) was intragastrically administered with HFD. Physiological and metabolic changes were monitored and the expression of RAS components and markers of kidney injury were assessed.
Results
HFD-fed mice exhibited hyperglycemia, insulin resistance, and dyslipidemia compared to those in the RD group (P<0.05). Kidney injury in these mice was indicated by an increase in the ratio of albumin to creatinine, glomerular hypertrophy, and the effacement of podocyte foot processes. Expression of intrarenal angiotensin-converting enzyme, angiotensin II type I receptor, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase-4, and monocyte chemoattractant protein-1 was also markedly increased in HFD-fed mice. HFD-fed mice exhibited elevated SBP that was accompanied by an increase in the wall thickness and vascular cross-sectional area (P<0.05), 12 weeks post-HFD consumption. Treatment with THU (100 mg/kg/day) suppressed intrarenal RAS activation, improved insulin sensitivity, and reduced SBP, thus, attenuating kidney injury in these mice.
Conclusion
THU alleviated kidney injury in mice with HFD-induced type 2 diabetes, possibly by blunting the activation of the intrarenal RAS/nicotinamide adenine dinucleotide phosphate oxidase IV (NOX4)/monocyte chemoattractant protein 1 (MCP-1) axis and by lowering the high SBP. -
Citations
Citations to this article as recorded by- The Development of Dyslipidemia in Chronic Kidney Disease and Associated Cardiovascular Damage, and the Protective Effects of Curcuminoids
Zeltzin Alejandra Ceja-Galicia, Ana Karina Aranda-Rivera, Isabel Amador-Martínez, Omar Emiliano Aparicio-Trejo, Edilia Tapia, Joyce Trujillo, Victoria Ramírez, José Pedraza-Chaverri
Foods.2023; 12(5): 921. CrossRef - Translation Animal Models of Diabetic Kidney Disease: Biochemical and Histological Phenotypes, Advantages and Limitations
Wenting Luo, Shiyun Tang, Xiang Xiao, Simin Luo, Zixuan Yang, Wei Huang, Songqi Tang
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1297. CrossRef - Curcumin ameliorates focal segmental glomerulosclerosis by inhibiting apoptosis and oxidative stress in podocytes
Hui Zhang, Qing-Qing Dong, Hua-Pan Shu, Yu-Chi Tu, Qian-Qian Liao, Li-Jun Yao
Archives of Biochemistry and Biophysics.2023; 746: 109728. CrossRef - An examination of the protective effects and molecular mechanisms of curcumin, a polyphenol curcuminoid in diabetic nephropathy
Xiaoyu Zhu, Xingli Xu, Chigang Du, Yanping Su, Lixue Yin, Xiaoqiu Tan, Hui Liu, Yiru Wang, Lei Xu, Xinghua Xu
Biomedicine & Pharmacotherapy.2022; 153: 113438. CrossRef - An integrated bioinformatics analysis and experimental study identified key biomarkers CD300A or CXCL1, pathways and immune infiltration in diabetic nephropathy mice
WEI LIANG, QIANG LUO, ZONGWEI ZHANG, KEJU YANG, ANKANG YANG, QINGJIA CHI, HUAN HU
BIOCELL.2022; 46(8): 1989. CrossRef
- The Development of Dyslipidemia in Chronic Kidney Disease and Associated Cardiovascular Damage, and the Protective Effects of Curcuminoids

- Diabetes
- Cardiorenal Protection in Diabetic Kidney Disease
- Jason F. Lee, Ecaterina Berzan, Vikas S. Sridhar, Ayodele Odutayo, David Z.I. Cherney
- Endocrinol Metab. 2021;36(2):256-269. Published online April 19, 2021
- DOI: https://doi.org/10.3803/EnM.2021.987
- 5,711 View
- 299 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
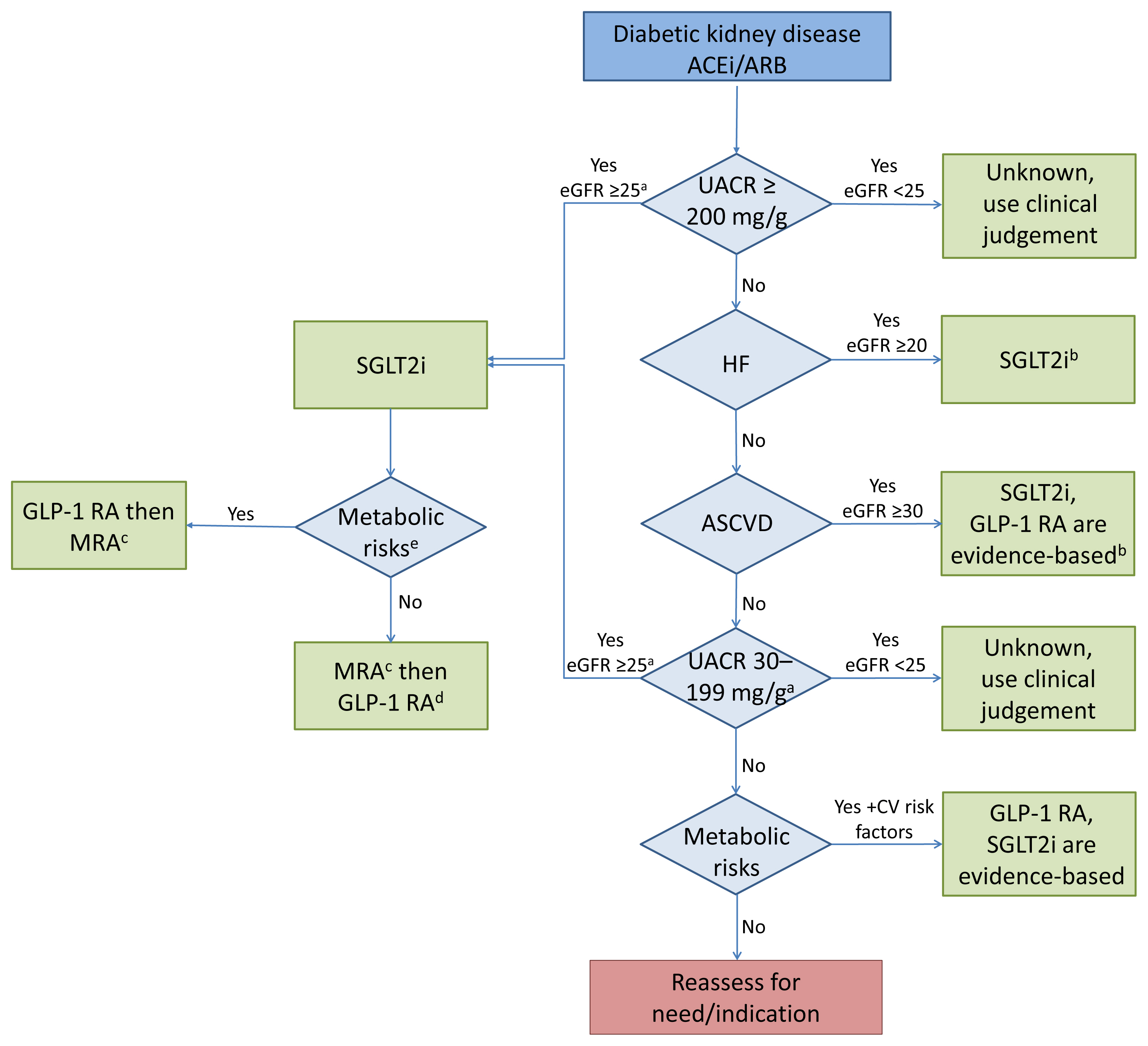
ePub - Over the last 5 years there have been many new developments in the management of diabetic kidney disease. Glucagon-like peptide-1 receptor agonists (GLP-1 RA) and sodium-glucose cotransporter-2 (SGLT2) inhibitors were initially used for glycemic control, but more recent studies have now shown that their benefits extend to cardiovascular and kidney outcomes. The recent addition of data on the novel mineralocorticoid receptor antagonist (MRA) gives us another approach to further decrease the residual risk of diabetic kidney disease progression. In this review we describe the mechanism of action, key studies, and possible adverse effects related to these three classes of medications. The management of type 2 diabetes now includes an increasing number of medications for the management of comorbidities in a patient population at significant risk of cardiovascular disease and progression of chronic kidney disease. It is from this perspective that we seek to outline the rationale for the sequential and/or combined use of SGLT2 inhibitors, GLP-1 RA and MRAs in patients with type 2 diabetes for heart and kidney protection.
-
Citations
Citations to this article as recorded by- Relative and Absolute Risks of Adverse Events with Real-World Use of SGLT2 Inhibitors in CKD
Ayodele Odutayo, Adeera Levin
Clinical Journal of the American Society of Nephrology.2023; 18(5): 557. CrossRef - Renal Protection of Mineralocorticoid Receptor Antagonist, Finerenone, in Diabetic Kidney Disease
Dong-Lim Kim, Seung-Eun Lee, Nan Hee Kim
Endocrinology and Metabolism.2023; 38(1): 43. CrossRef - Intrarenal Mechanisms of Sodium-Glucose Cotransporter-2 Inhibitors on Tubuloglomerular Feedback and Natriuresis
Eun Sil Koh, Gheun-Ho Kim, Sungjin Chung
Endocrinology and Metabolism.2023; 38(4): 359. CrossRef - SGLT2 and DPP4 inhibitors improve Alzheimer’s disease–like pathology and cognitive function through distinct mechanisms in a T2D–AD mouse model
A Young Sim, Da Hyun Choi, Jong Youl Kim, Eun Ran Kim, A-ra Goh, Yong-ho Lee, Jong Eun Lee
Biomedicine & Pharmacotherapy.2023; 168: 115755. CrossRef - Narrative review investigating the nephroprotective mechanisms of sodium glucose cotransporter type 2 inhibitors in diabetic and nondiabetic patients with chronic kidney disease
Emma S. Speedtsberg, Martin Tepel
Frontiers in Endocrinology.2023;[Epub] CrossRef - Management of CKD
Nimrit Goraya, Jennifer D. Moran
Nephrology Self-Assessment Program.2022; 21(2): 146. CrossRef - Nonsteroidal mineralocorticoid receptor antagonism for cardiovascular and renal disorders − New perspectives for combination therapy
Peter Kolkhof, Amer Joseph, Ulrich Kintscher
Pharmacological Research.2021; 172: 105859. CrossRef - Sodium‐Glucose Cotransporter 2 Inhibitors, All‐Cause Mortality, and Cardiovascular Outcomes in Adults with Type 2 Diabetes: A Bayesian Meta‐Analysis and Meta‐Regression
Ayodele Odutayo, Bruno R. da Costa, Tiago V. Pereira, Vinay Garg, Samir Iskander, Fatimah Roble, Rahim Lalji, Cesar A. Hincapié, Aquila Akingbade, Myanca Rodrigues, Arnav Agarwal, Bishoy Lawendy, Pakeezah Saadat, Jacob A. Udell, Francesco Cosentino, Peter
Journal of the American Heart Association.2021;[Epub] CrossRef - Finerenone: A Potential Treatment for Patients with Chronic Kidney Disease and Type 2 Diabetes Mellitus
Luis D’Marco, María Jesús Puchades, Lorena Gandía, Claudia Forquet, Elena Giménez-Civera, Nayara Panizo, Javier Reque, Isabel Juan-García, Valmore Bermúdez, José Luis Gorriz
touchREVIEWS in Endocrinology.2021; 17(2): 84. CrossRef - Sodium-Glucose Cotransporter 2 Inhibitors Mechanisms of Action: A Review
Jorge I. Fonseca-Correa, Ricardo Correa-Rotter
Frontiers in Medicine.2021;[Epub] CrossRef
- Relative and Absolute Risks of Adverse Events with Real-World Use of SGLT2 Inhibitors in CKD

- Clinical Study
- Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
- Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
- Endocrinol Metab. 2021;36(2):388-400. Published online March 31, 2021
- DOI: https://doi.org/10.3803/EnM.2020.912
- 6,347 View
- 360 Download
- 13 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
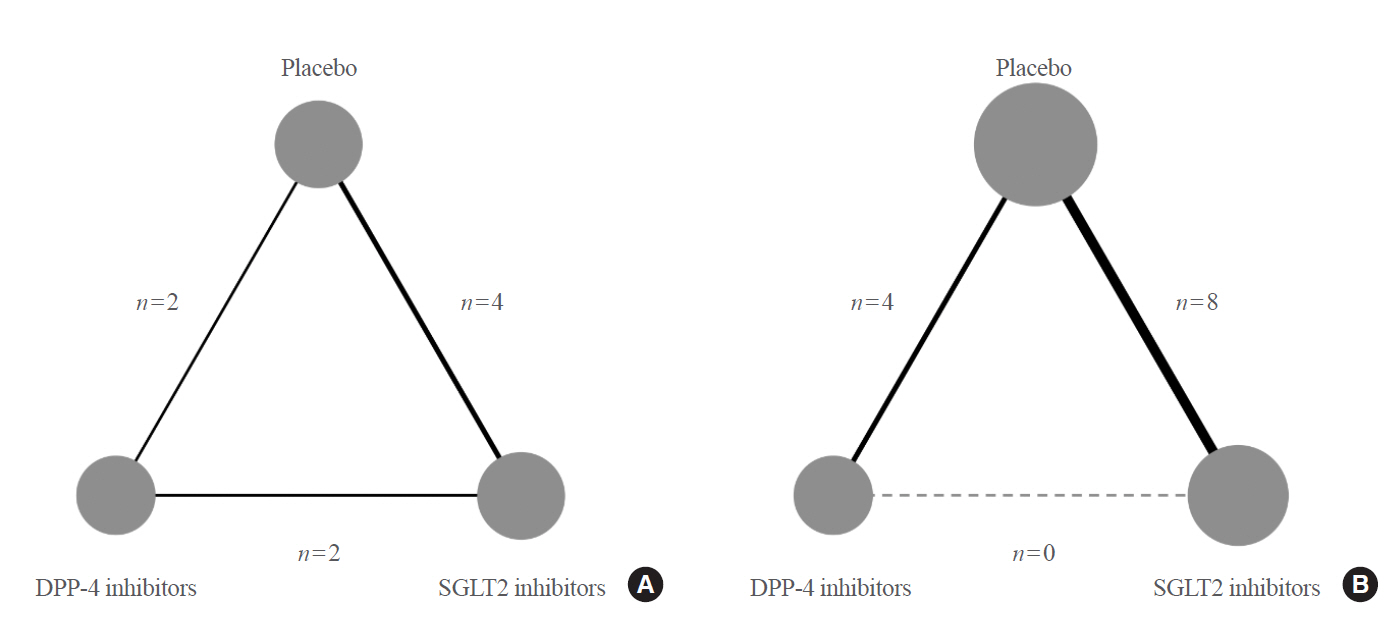
To compare the renal effects of dipeptidyl peptidase-4 (DPP-4) inhibitors and sodium-glucose cotransporter 2 (SGLT2) inhibitors on individual outcomes in patients with type 2 diabetes.
Methods
We searched electronic databases (MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials) from inception to June 2019 to identity eligible randomized controlled trials of DPP-4 inhibitors or SGLT2 inhibitors that reported at least one kidney outcome in patients with type 2 diabetes. Outcomes of interest were microalbuminuria, macroalbuminuria, worsening nephropathy, and end-stage kidney disease (ESKD). We performed an arm-based network meta-analysis using Bayesian methods and calculated absolute risks and rank probabilities of each treatment for the outcomes.
Results
Seventeen studies with 87,263 patients were included. SGLT2 inhibitors significantly lowered the risks of individual kidney outcomes, including microalbuminuria (odds ratio [OR], 0.64; 95% credible interval [CrI], 0.41 to 0.93), macroalbuminuria (OR, 0.48; 95% CrI, 0.24 to 0.72), worsening nephropathy (OR, 0.65; 95% CrI, 0.44 to 0.91), and ESKD (OR, 0.65; 95% CrI, 0.46 to 0.98) as compared with placebo. However, DPP-4 inhibitors did not lower the risks. SGLT2 inhibitors were considerably associated with higher absolute risk reductions in all kidney outcomes than DPP-4 inhibitors, although the benefits were statistically insignificant. The rank probabilities showed that SGLT2 inhibitors were better treatments for lowering the risk of albuminuria and ESKD than placebo or DPP-4 inhibitors.
Conclusion
SGLT2 inhibitors were superior to DPP-4 inhibitors in reducing the risk of albuminuria and ESKD in patients with type 2 diabetes. -
Citations
Citations to this article as recorded by- Therapie des Typ-2-Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Die Diabetologie.2024; 20(2): 212. CrossRef - Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study
Mototsugu Nagao, Jun Sasaki, Kyoko Tanimura-Inagaki, Ichiro Sakuma, Hitoshi Sugihara, Shinichi Oikawa
Cardiovascular Diabetology.2024;[Epub] CrossRef - Comparative Effect of Glucose-Lowering Drugs for Type 2 Diabetes Mellitus on Stroke Prevention: A Systematic Review and Network Meta-Analysis
Ji Soo Kim, Gyeongsil Lee, Kyung-Il Park, Seung-Won Oh
Diabetes & Metabolism Journal.2024; 48(2): 312. CrossRef - Therapy of Type 2 Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Experimental and Clinical Endocrinology & Diabetes.2024;[Epub] CrossRef - Therapie des Typ-2-Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Die Diabetologie.2023; 19(5): 658. CrossRef - Renoprotective Effect of Thai Patients with Type 2 Diabetes Mellitus Treated with SGLT-2 Inhibitors versus DPP-4 Inhibitors: A Real-World Observational Study
Apichaya Chanawong, Suriyon Uitrakul, Supatcha Incomenoy, Natnicha Poonchuay, Rizky Abdulah
Advances in Pharmacological and Pharmaceutical Sciences.2023; 2023: 1. CrossRef - Different nursing interventions on sleep quality among critically ill patients: A systematic review and network meta-analysis
Daijin Huang, Yumei Li, Jing Ye, Chang Liu, Dongyan Shen, Yunhui Lv
Medicine.2023; 102(52): e36298. CrossRef - New trends in the approach to the treatment of type 2 diabetes - observations and benefits in the outpatient practice of a diabetologist
Pavel Weber, Hana Meluzínová, Dana Weberová
Klinická farmakologie a farmacie.2022; 35(4): 118. CrossRef - Comparative efficacy of novel antidiabetic drugs on cardiovascular and renal outcomes in patients with diabetic kidney disease: A systematic review and network meta‐analysis
Hongwei Cao, Tao Liu, Li Wang, Qiuhe Ji
Diabetes, Obesity and Metabolism.2022; 24(8): 1448. CrossRef - Therapie des Typ-2-Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald H. Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Die Diabetologie.2022; 18(5): 623. CrossRef - Significant reduction in chronic kidney disease progression with sodium‐glucose cotransporter‐2 inhibitors compared to dipeptidyl peptidase‐4 inhibitors in adults with type 2 diabetes in a UK clinical setting: An observational outcomes study based on inte
Iskandar Idris, Ruiqi Zhang, Jil B. Mamza, Mike Ford, Tamsin Morris, Amitava Banerjee, Kamlesh Khunti
Diabetes, Obesity and Metabolism.2022; 24(11): 2138. CrossRef - Therapy of Type 2 Diabetes
Rüdiger Landgraf, Jens Aberle, Andreas L. Birkenfeld, Baptist Gallwitz, Monika Kellerer, Harald Klein, Dirk Müller-Wieland, Michael A. Nauck, Tobias Wiesner, Erhard Siegel
Experimental and Clinical Endocrinology & Diabetes.2022; 130(S 01): S80. CrossRef - Molecular Mechanistic Pathways Targeted by Natural Compounds in the Prevention and Treatment of Diabetic Kidney Disease
Kaixuan Zhou, Xue Zi, Jiayu Song, Qiulu Zhao, Jia Liu, Huiwei Bao, Lijing Li
Molecules.2022; 27(19): 6221. CrossRef - Lower risk of gout in sodium glucose cotransporter 2 (SGLT2) inhibitors versus dipeptidyl peptidase-4 (DPP4) inhibitors in type-2 diabetes
Jiandong Zhou, Xuejin Liu, Oscar Hou-In Chou, Lifang Li, Sharen Lee, Wing Tak Wong, Qingpeng Zhang, Carlin Chang, Tong Liu, Gary Tse, Fengshi Jing, Bernard Man Yung Cheung
Rheumatology.2022;[Epub] CrossRef - New Era for Renal-Protective Therapy in Type 2 Diabetes: Better Renal Outcomes in Patients with Type 2 Diabetes Taking Sodium-Glucose Cotransporter 2 Inhibitors versus Dipeptidyl Peptidase-4 Inhibitors
Chan-Hee Jung
Endocrinology and Metabolism.2021; 36(2): 339. CrossRef - Efficacy / safety balance of DPP-4 inhibitors versus SGLT2 inhibitors in elderly patients with type 2 diabetes
André J. Scheen
Diabetes & Metabolism.2021; 47(6): 101275. CrossRef
- Therapie des Typ-2-Diabetes

- Clinical Study
- Association of Vitamin D Deficiency with Diabetic Nephropathy
- So-hyeon Hong, Young Bin Kim, Hoon Sung Choi, Tae-Dong Jeong, Jin Taek Kim, Yeon Ah Sung
- Endocrinol Metab. 2021;36(1):106-113. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.826

- 8,462 View
- 225 Download
- 21 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Low 25-hydroxyvitamin D (25OHD) levels are associated with the incidence of type 2 diabetes mellitus (T2DM). However, the association between 25OHD and metabolic health status or diabetic complications is inconclusive. We evaluated this relationship between vitamin D status and metabolic parameters and complications of T2DM.
Methods
This study included 1,392 patients with T2DM who visited Eulji and Ewha Diabetes Center between January 2011 and August 2016. Anthropometric parameters and laboratory tests including glycated hemoglobin (HbA1c), lipid profile, liver and kidney function, and urinary albumin-to-creatinine ratio (UACR) were evaluated. Diabetic macro- and microvascular complications were determined through a medical record review. Serum 25OHD concentrations were measured by chemiluminescent immunoassay.
Results
The mean 25OHD level was 16.8±9.6 ng/mL. Vitamin D deficiency (<20 ng/mL) and severe deficiency (<10 ng/mL) were observed in 990 (71.1%) and 351 (25.2%) participants, respectively. 25OHD level was positively correlated with age and highdensity lipoprotein cholesterol (HDL-C) level and negatively correlated with HbA1c, triglyceride level, and UACR. HDL-C and UACR were significantly associated with 25OHD after adjusting for other variables. Vitamin D deficiency was independently related to nephropathy after adjusting for confounding variables.
Conclusion
Vitamin D deficiency was common among Korean T2DM patients; it was independently associated with microalbuminuria and HDL level, and positively related to diabetic nephropathy. -
Citations
Citations to this article as recorded by- ED-71 ameliorates bone regeneration in type 2 diabetes by reducing ferroptosis in osteoblasts via the HIF1α pathway
Maoshan Wang, Yingxue Liu, Houda Gui, Gaoqiang Ma, Binyang Li, Zhanwei Zhang, Gyeonghwi Yu, Ailin Wu, Xin Xu, Dongjiao Zhang
European Journal of Pharmacology.2024; 969: 176303. CrossRef - Vitamin D metabolism in diabetic nephropathy
Z. V. Abilov, R. Kh. Salimkhanov, A. A. Povaliaeva, A. Yu. Zhukov, E. A. Pigarova, L. K. Dzeranova, L. Ya. Rozhinskaya
Obesity and metabolism.2024; 20(4): 283. CrossRef - COVID-19 infection and metabolic comorbidities: Mitigating role of nutritional sufficiency and drug – nutraceutical combinations of vitamin D
Sumit Kumar Mandal, Meghana Tare, P.R. Deepa
Human Nutrition & Metabolism.2023; 31: 200179. CrossRef - Effects of Vitamin D Supplementation in Diabetic Kidney Disease: A Systematic Review
Thais de Oliveira e Silva Ullmann, Beatrys Juliani Ramalho, Lucas Fornari Laurindo, Ricardo José Tofano, Claudio José Rubira, Elen Landgraf Guiguer, Sandra Maria Barbalho, Uri Adrian Prync Flato, Katia Portero Sloan, Adriano Cressoni Araujo
Journal of Renal Nutrition.2023; 33(5): 618. CrossRef - Diabetic Nephropathy: Significance of Determining Oxidative Stress and Opportunities for Antioxidant Therapies
Marina Darenskaya, Sergey Kolesnikov, Natalya Semenova, Lyubov Kolesnikova
International Journal of Molecular Sciences.2023; 24(15): 12378. CrossRef - Association between serum 25- hydroxyvitamin D and albuminuiria in middle-aged and older Chinese patients with type 2 diabetes
Luyan Zhang, Qian Guo, Yanjia Xu, Wenzhen Wei, Yu Wang
BMC Endocrine Disorders.2023;[Epub] CrossRef - Vitamin D deficiency and its associated factors among patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Mitku Mammo Taderegew, Gashaw Garedew Woldeamanuel, Alemayehu Wondie, Atsede Getawey, Abera Nesiru Abegaz, Fentahun Adane
BMJ Open.2023; 13(10): e075607. CrossRef - Progression of diabetic nephropathy and vitamin D serum levels: A pooled analysis of 7722 patients
Yomna E. Dean, Sameh Samir Elawady, Wangpan Shi, Ahmed A. Salem, Arinnan Chotwatanapong, Haya Ashraf, Tharun Reddi, Prashant Obed Reddy Dundi, Waleed Yasser Habash, Mohamed Yasser Habash, Safaa Ahmed, Hana M. Samir, Ahmed Elsayed, Aryan Arora, Abhinav Aro
Endocrinology, Diabetes & Metabolism.2023;[Epub] CrossRef - Incidence of Vitamin D Deficiency and Its Association With Microalbuminuria in Patients With Type 2 Diabetes Mellitus
Muhammad Hamza Riaz, Ammar Jamil, Hira Yousaf, Muhammad Hassan, Muhammad Ahmer Sohaib, Sharjeel Babar, Muhammad Hassan Ahmad, Ibtesam Allahi, Muhammad Zeshan Mehmood, Tayyab Mumtaz Khan
Cureus.2023;[Epub] CrossRef - The Role of Vitamin D in Diabetic Nephropathy: A Translational Approach
Charlotte Delrue, Reinhart Speeckaert, Joris R. Delanghe, Marijn M. Speeckaert
International Journal of Molecular Sciences.2022; 23(2): 807. CrossRef - Associations of serum amyloid A and 25‐hydroxyvitamin D with diabetic nephropathy: A cross‐sectional study
Qian Liu, Jin Sun, Tongdao Xu, Guangrong Bian, Fumeng Yang
Journal of Clinical Laboratory Analysis.2022;[Epub] CrossRef - Formulation Strategies for Improving the Stability and Bioavailability of Vitamin D-Fortified Beverages: A Review
Elsa F. Vieira, Suene Souza
Foods.2022; 11(6): 847. CrossRef - Association between Vitamin D Status and Mortality among Adults with Diabetic Kidney Disease
Feng Xu, Hongyu Lu, Tianwen Lai, Ling Lin, Yongsong Chen, Pratibha V. Nerurkar
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Assessment of the relationship between 25-hydroxyvitamin D and albuminuria in type 2 diabetes mellitus
Seyed Alireza Zomorodian, Maryam Shafiee, Zeinab Karimi, Fatemeh Masjedi, Amirhossein Roshanshad
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association of Serum 25 (OH) Vitamin D With Chronic Kidney Disease Progression in Type 2 Diabetes
Suyan Duan, Fang Lu, Buyun Wu, Chengning Zhang, Guangyan Nie, Lianqin Sun, Zhimin Huang, Honglei Guo, Bo Zhang, Changying Xing, Yanggang Yuan
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Influence of Dietary Supplementations on Neuropathic Pain
Francesco D’Egidio, Giorgia Lombardozzi, Housem E. Kacem Ben Haj M’Barek, Giada Mastroiacovo, Margherita Alfonsetti, Annamaria Cimini
Life.2022; 12(8): 1125. CrossRef - Emergence of Ectopic Adrenal Tissues-What are the Probable Mechanisms?
Gürkan Tarçın, Oya Ercan
Journal of Clinical Research in Pediatric Endocrinology.2022; 14(3): 258. CrossRef - Nutritional Supplements for the Treatment of Neuropathic Pain
Khaled M. Abdelrahman, Kevin V. Hackshaw
Biomedicines.2021; 9(6): 674. CrossRef - Vitamin D Deficiency as a Predictor of a High Prevalence of Coronary Artery Disease in Pancreas Transplant Candidates With Type 1 Diabetes
Małgorzata Buksińska-Lisik, Przemysław J. Kwasiborski, Robert Ryczek, Wojciech Lisik, Artur Mamcarz
Frontiers in Endocrinology.2021;[Epub] CrossRef - Serum 25-hydroxyvitamin D and Metabolic Parameters in Healthy Korean Adults: Korean National Health and Nutrition Examination Survey VI
Jeonghoon Ha, Hansang Baek, Chaiho Jeong, Hyunsam Kim, Ki-Hyun Baek, Moo Il Kang, Dong-Jun Lim
International Journal of General Medicine.2021; Volume 14: 5233. CrossRef - Association Between 25(OH)Vitamin D, HbA1c and Albuminuria in Diabetes Mellitus: Data From a Population-Based Study (VIDAMAZON)
João Soares Felício, Hana Andrade de Rider Britto, Pedro Celeira Cortez, Fabrício de Souza Resende, Manuela Nascimento de Lemos, Lorena Vilhena de Moraes, Vitória Teixeira de Aquino, Fernanda de Souza Parente, Natércia Neves Marques de Queiroz, João Felíc
Frontiers in Endocrinology.2021;[Epub] CrossRef - Vitamin D Analogs Can Retard the Onset or Progression of Diabetic Kidney Disease: A Systematic Review
Samuel N. Uwaezuoke
Frontiers in Clinical Diabetes and Healthcare.2021;[Epub] CrossRef
- ED-71 ameliorates bone regeneration in type 2 diabetes by reducing ferroptosis in osteoblasts via the HIF1α pathway

- Clinical Study
- Short-Term Effects of Beraprost Sodium on the Markers for Cardiovascular Risk Prediction in Type 2 Diabetic Patients with Microalbuminuria
- Yun Mi Choi, Hyuk-Sang Kwon, Kyung Mook Choi, Won-Young Lee, Eun-Gyoung Hong
- Endocrinol Metab. 2019;34(4):398-405. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.398
- 5,290 View
- 60 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background To evaluate the changes in cardiovascular risk markers including pulse wave velocity (PWV), microalbuminuria, inflammatory cytokines, and adhesion molecules after treatment with beraprost sodium (BPS) in patients with diabetic nephropathy.
Methods This was a multicenter, prospective, randomized, double-blind, placebo-controlled trial. Type 2 diabetes mellitus patients with microalbuminuria were included. The primary endpoints were changes in microalbuminuria in spot urine and PWV after BPS or placebo (PCB) treatment for 24 weeks. The secondary endpoints were changes in clinical and metabolic parameters.
Results A total of 52 patients completed the 24-week trial. Changes in PWV were not different significantly in the BPS and PCB groups (right,
P =0.16; left,P =0.11). Changes in microalbuminuria were 14.2±157.0 and 34.5±146.6 (µg/mg Cr) in the BPS and PCB groups, respectively (P =0.63). Subgroup analysis in the high blood pressure (BP) group (baseline systolic BP >120 mm Hg and diastolic BP >80 mm Hg), showed that microalbuminuria decreased by −47.6 in the BPS group compared with an increase by 116.4 (µg/mg Cr) in the PCB group (P =0.04). Also, in the large waist circumference group (>95 cm), microalbuminuria decreased significantly in the BPS group (P =0.04).Conclusion Short-term treatment of BPS for patients with diabetic nephropathy did not show significant improvement in various cardiovascular risk factors. However, BPS significantly decreased microalbuminuria in study subjects with higher cardiovascular risk such as high BP or large waist circumference.
-
Citations
Citations to this article as recorded by- Clinical efficacy of beraprost sodium in treating chronic kidney disease: A six-month prospective study
Chen Sun, Xin Wu, Xin Zhang, Shulin Li, Ruoyu Jia, Dong Sun
Heliyon.2024; 10(2): e24156. CrossRef - Clinical efficacy and safety of beraprost sodium in the treatment of nephrotic syndrome: A meta-analysis
Peng Yan, Ben Ke, Xiangdong Fang
Medicine.2023; 102(42): e34958. CrossRef - Dysregulated coagulation system links to inflammation in diabetic kidney disease
Mengyun Xiao, Donge Tang, Shaodong Luan, Bo Hu, Wenyu Gong, Wolfgang Pommer, Yong Dai, Lianghong Yin
Frontiers in Clinical Diabetes and Healthcare.2023;[Epub] CrossRef - The effects of beraprost sodium on renal function and cardiometabolic profile in patients with diabetes mellitus: a systematic review and meta-analysis of clinical trials
Peyman Nowrouzi-Sohrabi, Reza Tabrizi, Kamran Hessami, Mojtaba Shabani-Borujeni, Mahnaz Hosseini-Bensenjan, Shahla Rezaei, Mohammad Jalali, Pedram Keshavarz, Fariba Ahmadizar
International Urology and Nephrology.2022; 54(1): 111. CrossRef - Thrombocytopenia in COVID‑19 and vaccine‑induced thrombotic thrombocytopenia
Styliani Geronikolou, Işil Takan, Athanasia Pavlopoulou, Marina Mantzourani, George Chrousos
International Journal of Molecular Medicine.2022;[Epub] CrossRef - The Role of Platelets in Diabetic Kidney Disease
Ukhti Jamil Rustiasari, Joris J. Roelofs
International Journal of Molecular Sciences.2022; 23(15): 8270. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef
- Clinical efficacy of beraprost sodium in treating chronic kidney disease: A six-month prospective study

- Diabetes
- Effects of Dipeptidyl Peptidase-4 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
- Jae Hyun Bae, Sunhee Kim, Eun-Gee Park, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
- Endocrinol Metab. 2019;34(1):80-92. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.80
- 7,601 View
- 267 Download
- 36 Web of Science
- 38 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background To investigate the effects of dipeptidyl peptidase-4 (DPP-4) inhibitors on renal outcomes in patients with type 2 diabetes.
Methods MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials were searched to identify randomized controlled trials (RCTs) of DPP-4 inhibitors from inception to September 2017. We selected eligible RCTs comparing DPP-4 inhibitors with placebo or other antidiabetic agents and reporting at least one renal outcome. A meta-analysis was conducted to calculate standardized mean differences, weighted mean differences (WMDs), relative risks (RRs), and 95% confidence intervals (CIs) for each renal outcome.
Results We included 23 RCTs with 19 publications involving 41,359 patients. Overall changes in urine albumin-to-creatinine ratio were comparable between DPP-4 inhibitors and controls (
P =0.150). However, DPP-4 inhibitors were associated with significantly lower risk of incident microalbuminuria (RR, 0.89; 95% CI, 0.80 to 0.98;P =0.022) and macroalbuminuria (RR, 0.77; 95% CI, 0.61 to 0.97;P =0.027), as well as higher rates of regression of albuminuria (RR, 1.22; 95% CI, 1.10 to 1.35;P <0.001) compared with controls. Although DPP-4 inhibitors were associated with small but significantly lower estimated glomerular filtration rate (WMD, −1.11 mL/min/1.73 m2; 95% CI, −1.78 to −0.44;P =0.001), there was no difference in the risk of end-stage renal disease between two groups (RR, 0.93; 95% CI, 0.76 to 1.14;P =0.475).Conclusion DPP-4 inhibitors had beneficial renal effects mainly by reducing the risk of development or progression of albuminuria compared with placebo or other antidiabetic agents.
-
Citations
Citations to this article as recorded by- Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study
Mototsugu Nagao, Jun Sasaki, Kyoko Tanimura-Inagaki, Ichiro Sakuma, Hitoshi Sugihara, Shinichi Oikawa
Cardiovascular Diabetology.2024;[Epub] CrossRef - Effects of glucose‐lowering agents on cardiovascular and renal outcomes in subjects with type 2 diabetes: An updated meta‐analysis of randomized controlled trials with external adjudication of events
Edoardo Mannucci, Marco Gallo, Andrea Giaccari, Riccardo Candido, Basilio Pintaudi, Giovanni Targher, Matteo Monami
Diabetes, Obesity and Metabolism.2023; 25(2): 444. CrossRef - Sitagliptin Mitigates Diabetic Nephropathy in a Rat Model of Streptozotocin-Induced Type 2 Diabetes: Possible Role of PTP1B/JAK-STAT Pathway
Sarah M. AL-Qabbaa, Samaher I. Qaboli, Tahani K. Alshammari, Maha A. Alamin, Haya M. Alrajeh, Lama A. Almuthnabi, Rana R. Alotaibi, Asma S. Alonazi, Anfal F. Bin Dayel, Nawal M. Alrasheed, Nouf M. Alrasheed
International Journal of Molecular Sciences.2023; 24(7): 6532. CrossRef - Take an individualized and multipronged approach when managing older adults with type 2 diabetes
Sheridan M. Hoy
Drugs & Therapy Perspectives.2023; 39(5): 171. CrossRef - Cardiovascular and Renal Outcomes With Sodium-Glucose Cotransporter-2 Inhibitors and Dipeptidyl Peptidase-4 Inhibitors Combination Therapy: A Meta-Analysis of Randomized Cardiovascular Outcome Trials
Awadhesh Kumar Singh, Akriti Singh, Ritu Singh
Endocrine Practice.2023; 29(7): 509. CrossRef - Sodium‐glucose cotransporter 2 inhibitors versus dipeptidyl peptidase 4 inhibitors on new‐onset overall cancer in Type 2 diabetes mellitus: A population‐based study
Cheuk To Chung, Ishan Lakhani, Oscar Hou In Chou, Teddy Tai Loy Lee, Edward Christopher Dee, Kenrick Ng, Wing Tak Wong, Tong Liu, Sharen Lee, Qingpeng Zhang, Bernard Man Yung Cheung, Gary Tse, Jiandong Zhou
Cancer Medicine.2023; 12(11): 12299. CrossRef - Comparative Effects of Glucose-Lowering Medications on Kidney Outcomes in Type 2 Diabetes
Deborah J. Wexler, Ian H. de Boer, Alokananda Ghosh, Naji Younes, Ionut Bebu, Silvio E. Inzucchi, Janet B. McGill, Sunder Mudaliar, David Schade, Michael W. Steffes, William V. Tamborlane, Meng H. Tan, Faramarz Ismail-Beigi, Jill P. Crandall, Melissa Dian
JAMA Internal Medicine.2023; 183(7): 705. CrossRef - SAFETY PROFILE OF DIPEPTIDYL PEPTIDASE-4 INHIBITORS
M. Ganeva
Trakia Journal of Sciences.2023; 21(1): 54. CrossRef - Chronic Kidney Disease and SGLT2 Inhibitors: A Review of the Evolving Treatment Landscape
Christian W. Mende
Advances in Therapy.2022; 39(1): 148. CrossRef - Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Gunjan Y. Gandhi, Arshag D. Mooradian
Drugs & Aging.2022; 39(1): 39. CrossRef - Pharmacoeconomic evaluation of dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes mellitus: a systematic literature review
Zhen Ruan, Huimin Zou, Qing Lei, Carolina Oi Lam Ung, Honghao Shi, Hao Hu
Expert Review of Pharmacoeconomics & Outcomes Research.2022; 22(4): 555. CrossRef - Effect of Anagliptin versus Sitagliptin on Renal Function: Subanalyzes from the REASON Trial
Hiroki Teragawa, Takeshi Morimoto, Yuichi Fujii, Tomohiro Ueda, Mio Sakuma, Michio Shimabukuro, Osamu Arasaki, Koichi Node, Takashi Nomiyama, Shinichiro Ueda
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 685. CrossRef - Glomerular filtration rate as a kidney outcome of diabetic kidney disease: a focus on new antidiabetic drugs
Hyo Jin Kim, Sang Soo Kim, Sang Heon Song
The Korean Journal of Internal Medicine.2022; 37(3): 502. CrossRef - The Effects of Dipeptidyl Peptidase 4 Inhibitors on Renal Function in Patients with Type 2 Diabetes Mellitus
Wan-Chia Hsu, Chun-Sheng Lin, Jung-Fu Chen, Chih-Min Chang
Journal of Clinical Medicine.2022; 11(9): 2653. CrossRef - Treatment of diabetes mellitus has borne much fruit in the prevention of cardiovascular disease
Hiroaki Yagyu, Hitoshi Shimano
Journal of Diabetes Investigation.2022; 13(9): 1472. CrossRef - Finerenone, a Novel and Safer Approach toward Management of Diabetic Kidney Disease with Heart Failure
Ayesha Abdul Qadir Memon, Sarmad Iqbal
Global Journal of Medical, Pharmaceutical, and Biomedical Update.2022; 17: 12. CrossRef - The effects of dipeptidyl peptidase‐4 inhibitors on kidney outcomes
Daniel V. O'Hara, Thomas R. Parkhill, Sunil V. Badve, Min Jun, Meg J. Jardine, Vlado Perkovic
Diabetes, Obesity and Metabolism.2021; 23(3): 763. CrossRef - Urinary DPP4 correlates with renal dysfunction, and DPP4 inhibition protects against the reduction in megalin and podocin expression in experimental CKD
Acaris Benetti, Flavia Letícia Martins, Letícia Barros Sene, Maria Heloisa M. Shimizu, Antonio C. Seguro, Weverton M. Luchi, Adriana C. C. Girardi
American Journal of Physiology-Renal Physiology.2021; 320(3): F285. CrossRef - Incretin-based drugs and the kidney in type 2 diabetes: choosing between DPP-4 inhibitors and GLP-1 receptor agonists
Johannes F.E. Mann, Marcel H.A. Muskiet
Kidney International.2021; 99(2): 314. CrossRef - Renoprotective Effects of DPP-4 Inhibitors
Daiji Kawanami, Yuichi Takashi, Hiroyuki Takahashi, Ryoko Motonaga, Makito Tanabe
Antioxidants.2021; 10(2): 246. CrossRef - Danegaptide Prevents TGFβ1-Induced Damage in Human Proximal Tubule Epithelial Cells of the Kidney
Paul E. Squires, Gareth W. Price, Ulrik Mouritzen, Joe A. Potter, Bethany M. Williams, Claire E. Hills
International Journal of Molecular Sciences.2021; 22(6): 2809. CrossRef - Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2021; 36(2): 388. CrossRef - Consensus Recommendations by the Asian Pacific Society of Cardiology: Optimising Cardiovascular Outcomes in Patients with Type 2 Diabetes
Jack Wei Chieh Tan, David Sim, Junya Ako, Wael Almahmeed, Mark E Cooper, Jamshed J Dalal, Chaicharn Deerochanawong, David Wei Chun Huang, Sofian Johar, Upendra Kaul, Sin Gon Kim, Natalie Koh, Alice Pik-Shan Kong, Rungroj Krittayaphong, Bernard Kwok, Bien
European Cardiology Review.2021;[Epub] CrossRef - Diabetes and kidney disease: emphasis on treatment with SGLT-2 inhibitors and GLP-1 receptor agonists
Francesco Prattichizzo, Paola de Candia, Antonio Ceriello
Metabolism.2021; 120: 154799. CrossRef - SGLT2 Inhibitors and Other Novel Therapeutics in the Management of Diabetic Kidney Disease
Robert C. Stanton
Seminars in Nephrology.2021; 41(2): 85. CrossRef - Mineralocorticoid Receptor Antagonists in Diabetic Kidney Disease
Nina Vodošek Hojs, Sebastjan Bevc, Robert Ekart, Nejc Piko, Tadej Petreski, Radovan Hojs
Pharmaceuticals.2021; 14(6): 561. CrossRef - Podocyte Glucocorticoid Receptors Are Essential for Glomerular Endothelial Cell Homeostasis in Diabetes Mellitus
Swayam Prakash Srivastava, Han Zhou, Ocean Setia, Alan Dardik, Carlos Fernandez‐Hernando, Julie Goodwin
Journal of the American Heart Association.2021;[Epub] CrossRef - Coronavirus Disease (COVID)-19 and Diabetic Kidney Disease
Swayam Prakash Srivastava, Rohit Srivastava, Subhash Chand, Julie E. Goodwin
Pharmaceuticals.2021; 14(8): 751. CrossRef - Effects of DPP4 inhibitors on renal outcomes in diabetes mellitus: A systematic review and meta-analysis
SaikatK Dalui, Raja Chakraverty, Nafisha Yasmin, Smita Pattanaik, Kaushik Pandit, Suparna Chatterjee
Indian Journal of Endocrinology and Metabolism.2021; 25(4): 283. CrossRef - Comparison of Adverse Kidney Outcomes With Empagliflozin and Linagliptin Use in Patients With Type 2 Diabetic Patients in a Real-World Setting
Yueh-Ting Lee, Chien-Ning Hsu, Chung-Ming Fu, Shih-Wei Wang, Chiang-Chi Huang, Lung-Chih Li
Frontiers in Pharmacology.2021;[Epub] CrossRef - The Role of DPP-4 Inhibitors in Type-2 Diabetes Patients with Chronic Kidney Disease
Mishal Yousef Alqurashi, Khalid Faisal Alharthi, Abdulaziz Abdulrahman Alshehri, Yazeed Khalid Alharbi, Mohammad Abdulmunem Sanousi, Anas Abdullah Almazyed, Khulud Saeed Alghamdi, Sarah Musaad Alrashidi, Waad Abdullah Qaeed, Amjad Aedh Alasmari
Pharmacophore.2021; 12(3): 91. CrossRef - Type 2 diabetes mellitus management in patients with chronic kidney disease: an update
Zoi Kleinaki, Stella Kapnisi, Sofia-Andriani Theodorelou-Charitou, Ilias P. Nikas, Stavroula A. Paschou
Hormones.2020; 19(4): 467. CrossRef - Renal Outcomes in Type 2 Diabetes: A Review of Cardiovascular and Renal Outcome Trials
David M. Williams, Asif Nawaz, Marc Evans
Diabetes Therapy.2020; 11(2): 369. CrossRef - Favorable pleiotropic effects of sodium glucose cotransporter 2 inhibitors: head-to-head comparisons with dipeptidyl peptidase-4 inhibitors in type 2 diabetes patients
Shih-Chieh Shao, Kai-Cheng Chang, Swu-Jane Lin, Rong-Nan Chien, Ming-Jui Hung, Yuk-Ying Chan, Yea-Huei Kao Yang, Edward Chia-Cheng Lai
Cardiovascular Diabetology.2020;[Epub] CrossRef - Novel therapeutic agents for the treatment of diabetic kidney disease
Rachel E. Hartman, P.S.S. Rao, Mariann D. Churchwell, Susan J. Lewis
Expert Opinion on Investigational Drugs.2020; 29(11): 1277. CrossRef - Renal protection with glucagon-like peptide-1 receptor agonists
Martina Vitale, Jonida Haxhi, Tiziana Cirrito, Giuseppe Pugliese
Current Opinion in Pharmacology.2020; 54: 91. CrossRef - Loss of Mitochondrial Control Impacts Renal Health
Swayam Prakash Srivastava, Keizo Kanasaki, Julie E. Goodwin
Frontiers in Pharmacology.2020;[Epub] CrossRef - Effects of Sodium-Glucose Cotransporter 2 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Scientific Reports.2019;[Epub] CrossRef
- Ipragliflozin and sitagliptin differentially affect lipid and apolipoprotein profiles in type 2 diabetes: the SUCRE study

- Obesity and Metabolism
- Current Challenges in Diabetic Nephropathy: Early Diagnosis and Ways to Improve Outcomes
- Sang Soo Kim, Jong Ho Kim, In Joo Kim
- Endocrinol Metab. 2016;31(2):245-253. Published online May 27, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.245
- 6,135 View
- 93 Download
- 51 Web of Science
- 45 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetes is often associated with chronic kidney disease (CKD) and is the primary cause of kidney failure in half of patients who receive dialysis therapy. Given the increasing prevalence of diabetes and its high morbidity and mortality, diabetic nephropathy is a serious drawback in individual patients and a tremendous socioeconomic burden on society. Despite growing concern for the management of diabetic nephropathy, the prevalence of CKD with diabetes is the same today as it was 20 years ago. The current strategy to manage diabetic nephropathy, including the control of hyperglycemia, dyslipidemia, and blood pressure and the wide-spread use of renin-angiotensin-aldosterone system inhibitors, is well established to be beneficial in the early stages of diabetic nephropathy. However, the effects are uncertain in patients with relatively progressed CKD. Therefore, early diagnosis or risk verification is extremely important in order to reduce the individual and socioeconomic burdens associated with diabetic nephropathy by providing appropriate management to prevent the development and progression of this condition. This review focuses on recent research and guidelines regarding risk assessment, advances in medical treatment, and challenges of and future treatments for diabetic nephropathy.
-
Citations
Citations to this article as recorded by- The Role of Angiotensin-Converting Enzyme (ACE) Polymorphisms in the Risk of Development and Treatment of Diabetic Nephropathy
Magdalena Król-Kulikowska, Nikita Abramenko, Milan Jakubek, Mirosław Banasik, Marta Kepinska
Journal of Clinical Medicine.2024; 13(4): 995. CrossRef - Diagnostic utility of renal shear wave elastography and renal Doppler findings in diabetic nephropathy: a case–control study
Ahmed Abdelrahman Baz, Eman Muhammad Abdeen, Mona Yousry Helmy, Abo El-Magd Al-Bohy
Egyptian Journal of Radiology and Nuclear Medicine.2024;[Epub] CrossRef - Gestione perioperatoria del paziente diabetico adulto
M. Raucoules-Aimé, T. Thierry Nessan Ouattara
EMC - Anestesia-Rianimazione.2023; 28(1): 1. CrossRef - Pyruvate Kinase M2: A New Biomarker for the Early Detection of Diabetes-Induced Nephropathy
Yeon Su Park, Joo Hee Han, Jae Hyeon Park, Ji Soo Choi, Seung Hyeon Kim, Hyung Sik Kim
International Journal of Molecular Sciences.2023; 24(3): 2683. CrossRef - Tratamiento perioperatorio del paciente diabético adulto
M. Raucoules-Aimé, T. Thierry Nessan Ouattara
EMC - Anestesia-Reanimación.2023; 49(1): 1. CrossRef - Renal Protection of Mineralocorticoid Receptor Antagonist, Finerenone, in Diabetic Kidney Disease
Dong-Lim Kim, Seung-Eun Lee, Nan Hee Kim
Endocrinology and Metabolism.2023; 38(1): 43. CrossRef - The role of tubulointerstitial markers in differential diagnosis and prognosis in patients with type 2 diabetes and biopsy proven diabetic kidney disease
Xijian Wang, Liang Ren, Ying Huang, Zhengang Feng, Guangdi Zhang, Houyong Dai
Clinica Chimica Acta.2023; 547: 117448. CrossRef - Network pharmacology and molecular docking technology-based predictive study of the active ingredients and potential targets of rhubarb for the treatment of diabetic nephropathy
Shaojie Fu, Yena Zhou, Cong Hu, Zhonggao Xu, Jie Hou
BMC Complementary Medicine and Therapies.2022;[Epub] CrossRef - Acrolein plays a culprit role in the pathogenesis of diabetic nephropathy in vitro and in vivo
Zhen-Jie Tong, Chin-Wei Kuo, Po-Cheng Yen, Chih-Ching Lin, Ming-Tsun Tsai, Shing-Hwa Lu, Yi-Ping Chang, Wen-Sheng Liu, Han-Hsing Tsou, Hsiao-Wei Cheng, Hsiang-Tsui Wang
European Journal of Endocrinology.2022; 187(4): 579. CrossRef - Probiotics ameliorates glycemic control of patients with diabetic nephropathy: A randomized clinical study
Hongyang Jiang, Yan Zhang, Dongyan Xu, Qing Wang
Journal of Clinical Laboratory Analysis.2021;[Epub] CrossRef - Blood Oxygen Level-Dependent (BOLD) MRI in Glomerular Disease
Daniel R. Nemirovsky, Puneet Gupta, Sophia Hu, Raymond Wong, Avnesh S. Thakor
Transplantology.2021; 2(2): 109. CrossRef - Amelioration of STZ-induced nephropathy in diabetic rats by saffron hydro alcoholic extract
Jamal Amri, Mona Alaee, Seyed Amirhossein Latifi, Abbas Alimoradian, Mehdi Salehi
Hormone Molecular Biology and Clinical Investigation.2021; 42(4): 411. CrossRef - Exosomes: Biomarkers and Therapeutic Targets of Diabetic Vascular Complications
Anqi Chen, Hailing Wang, Ying Su, Chunlin Zhang, Yanmei Qiu, Yifan Zhou, Yan Wan, Bo Hu, Yanan Li
Frontiers in Endocrinology.2021;[Epub] CrossRef - Sodium-glucose cotransporter 2 inhibitors benefit to kidney and cardiovascular outcomes for patients with type 2 diabetes mellitus and chronic kidney disease 3b-4: A systematic review and meta-analysis of randomized clinical trials
Haiyan Cao, Youxia Liu, Zhixia Tian, Yuhang Lian, Junya Jia, Ming Liu, Dong Li
Diabetes Research and Clinical Practice.2021; 180: 109033. CrossRef - Proteinuria as a significant predictive factor for the progression of carotid artery atherosclerosis in non-albuminuric type 2 diabetes
Young-eun Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes Research and Clinical Practice.2021; 181: 109082. CrossRef - The Role of Mesenchymal Stromal Cells-Derived Small Extracellular Vesicles in Diabetes and Its Chronic Complications
Fu-Xing-Zi Li, Xiao Lin, Feng Xu, Su-Kang Shan, Bei Guo, Li-Min Lei, Ming-Hui Zheng, Yi Wang, Qiu-Shuang Xu, Ling-Qing Yuan
Frontiers in Endocrinology.2021;[Epub] CrossRef - Preparation of Ergosterol-Loaded Nanostructured Lipid Carriers for Enhancing Oral Bioavailability and Antidiabetic Nephropathy Effects
Zhonghua Dong, Sajid Iqbal, Zhongxi Zhao
AAPS PharmSciTech.2020;[Epub] CrossRef - Carbon dots as fluorescent nanoprobe for the determination of N-acetyl-β-d-glucosaminidase activity
Jimei Ma, Heng Zhang, Fangfang Peng, Xiaoqing Yang, Zi-Long Li, Linhao Sun, Hong Jiang
Analytica Chimica Acta.2020; 1101: 129. CrossRef - Coffee Consumption is Associated with a Decreased Risk of Incident Chronic Kidney Disease: A Systematic Review and Meta-analysis of Cohort Studies
Thatsaphan Srithongkul, Patompong Ungprasert
European Journal of Internal Medicine.2020; 77: 111. CrossRef - Understanding molecular upsets in diabetic nephropathy to identify novel targets and treatment opportunities
Nidhi Raval, Akshant Kumawat, Dnyaneshwar Kalyane, Kiran Kalia, Rakesh K. Tekade
Drug Discovery Today.2020; 25(5): 862. CrossRef - A meta-analysis of serum Hcy in diagnosis of diabetic nephropathy
Xiaoling Zhou, Aijie Shi, Xiao Zhou
Pteridines.2020; 31(1): 1. CrossRef - Link between ACE I/D gene polymorphism and dyslipidemia in diabetic nephropathy: A case-control study from Hyderabad, India
UmmeNajiya Mahwish, KamakshiChaithri Ponnaluri, Babi Heera, SatishReddy Alavala, KRudrama Devi, SreeBhushan Raju, GSuman Latha, Parveen Jahan
Indian Journal of Nephrology.2020; 30(2): 77. CrossRef - Assessment of urinary NGAL for differential diagnosis and progression of diabetic kidney disease
Suyan Duan, Jiajia Chen, Lin Wu, Guangyan Nie, Lianqin Sun, Chengning Zhang, Zhimin Huang, Changying Xing, Bo Zhang, Yanggang Yuan
Journal of Diabetes and its Complications.2020; 34(10): 107665. CrossRef - Urinary proteins detected using modern proteomics intervene in early type 2 diabetic kidney disease – a pilot study
Alina Golea-Secara, Cristian Munteanu, Mirela Sarbu, Octavian M Cretu, Silvia Velciov, Adrian Vlad, Flaviu Bob, Florica Gadalean, Cristina Gluhovschi, Oana Milas, Anca Simulescu, Maria Mogos-Stefan, Mihaela Patruica, Ligia Petrica, Alina D Zamfir
Biomarkers in Medicine.2020; 14(16): 1521. CrossRef - Efficacy and safety of Shenkang injection as adjuvant therapy in patients with diabetic nephropathy
Yanping Wang, Mingzhu Li, Chenyun Li, Sheng Xu, Jiangfeng Wu, Gaochuan Zhang, Yuanyuan Cai
Medicine.2020; 99(52): e23821. CrossRef - A Nucleoside/Nucleobase-Rich Extract from Cordyceps Sinensis Inhibits the Epithelial–Mesenchymal Transition and Protects against Renal Fibrosis in Diabetic Nephropathy
Zhonghua Dong, Yueyue Sun, Guangwei Wei, Siying Li, Zhongxi Zhao
Molecules.2019; 24(22): 4119. CrossRef - Lack of Association between Past Helicobacter pylori Infection and Diabetes: A Two-Cohort Study
Jeung Hui Pyo, Hyuk Lee, Sung Chul Choi, Soo Jin Cho, Yoon-Ho Choi, Yang Won Min, Byung-Hoon Min, Jun Haeng Lee, Heejin Yoo, Kyunga Kim, Jae J. Kim
Nutrients.2019; 11(8): 1874. CrossRef - Serum Homocysteine, cystatin C as Biomarkers for Progression of Diabetic Nephropathy
Weihai Xu, Suhua Tang, Meijuan Xiang, Jianyun Peng
Pteridines.2019; 30(1): 183. CrossRef - Serum leptin in diabetic nephropathy male patients from Gaza Strip
Maged M. Yassin, Ayman M. AbuMustafa, Mohamed M. Yassin
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 1245. CrossRef - Effects of Sodium-Glucose Cotransporter 2 Inhibitors on Renal Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Scientific Reports.2019;[Epub] CrossRef - Association between nonalbumin proteinuria and renal tubular damage of N-acetyl-β-d-glucosaminidase and its clinical relevance in patients with type 2 diabetes without albuminuria
Eugene Han, Mi-Kyung Kim, Yong-ho Lee, Hye Soon Kim, Byung-Wan Lee
Journal of Diabetes and its Complications.2019; 33(3): 255. CrossRef - Supplementation of Abelmoschus manihot Ameliorates Diabetic Nephropathy and Hepatic Steatosis by Activating Autophagy in Mice
Hwajin Kim, Theodomir Dusabimana, So Kim, Jihyun Je, Kyuho Jeong, Min Kang, Kye Cho, Hye Kim, Sang Park
Nutrients.2018; 10(11): 1703. CrossRef - Perioperative management of adult diabetic patients. Preoperative period
Gaëlle Cheisson, Sophie Jacqueminet, Emmanuel Cosson, Carole Ichai, Anne-Marie Leguerrier, Bogdan Nicolescu-Catargi, Alexandre Ouattara, Igor Tauveron, Paul Valensi, Dan Benhamou
Anaesthesia Critical Care & Pain Medicine.2018; 37: S9. CrossRef - Practical management of diabetes patients before, during and after surgery: A joint French diabetology and anaesthesiology position statement
E. Cosson, B. Catargi, G. Cheisson, S. Jacqueminet, C. Ichai, A.-M. Leguerrier, A. Ouattara, I. Tauveron, E. Bismuth, D. Benhamou, P. Valensi
Diabetes & Metabolism.2018; 44(3): 200. CrossRef - MicroRNA‐326‐3p ameliorates high glucose and ox‐LDL‐IC‐ induced fibrotic injury in renal mesangial cells by targeting FcγRIII
Yiting Wang, Rui Zhang, Junlin Zhang, Fang Liu
Nephrology.2018; 23(11): 1031. CrossRef - Urinary Extracellular Vesicle
Wei-Cheng Xu, Ge Qian, Ai-Qun Liu, Yong-Qiang Li, He-Qun Zou
Chinese Medical Journal.2018; 131(11): 1357. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Comparison between Atorvastatin and Rosuvastatin in Renal Function Decline among Patients with Diabetes
Eugene Han, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Beom Seok Kim, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Endocrinology and Metabolism.2017; 32(2): 274. CrossRef - WITHDRAWN: Salvianolate attenuates renal fibrosis in rat models of diabetic nephropathy by inhibiting inflammation and oxidative stress mechanisms
Chongxiang Xiong, Jianrao Lu, Xinhua Wang, Monica V. Masucci
Biochemical and Biophysical Research Communications.2017;[Epub] CrossRef - Diffusion tensor imaging of the renal cortex in diabetic patients: correlation with urinary and serum biomarkers
Ahmed Abdel Khalek Abdel Razek, Mohammad Alsayed Abd Alhamid Al-Adlany, Alhadidy Mohammed Alhadidy, Mohammed Ali Atwa, Naglaa Elsayed Abass Abdou
Abdominal Radiology.2017; 42(5): 1493. CrossRef - Texte 2 : période préopératoire
Gaëlle Cheisson, Sophie Jacqueminet, Emmanuel Cosson, Carole Ichai, Anne-Marie Leguerrier, Bogdan Nicolescu-Catargi, Alexandre Ouattara, Igor Tauveron, Paul Valensi, Dan Benhamou
Anesthésie & Réanimation.2017; 3(3): 218. CrossRef - Global Cardiovascular and Renal Outcomes of Reduced GFR
Bernadette Thomas, Kunihiro Matsushita, Kalkidan Hassen Abate, Ziyad Al-Aly, Johan Ärnlöv, Kei Asayama, Robert Atkins, Alaa Badawi, Shoshana H. Ballew, Amitava Banerjee, Lars Barregård, Elizabeth Barrett-Connor, Sanjay Basu, Aminu K. Bello, Isabela Bensen
Journal of the American Society of Nephrology.2017; 28(7): 2167. CrossRef - Salvia miltiorrhiza Lipophilic Fraction Attenuates Oxidative Stress in Diabetic Nephropathy through Activation of Nuclear Factor Erythroid 2-Related Factor 2
Lin An, Mei Zhou, Faiz M. M. T. Marikar, Xue-Wen Hu, Qiu-Yun Miao, Ping Li, Jun Chen
The American Journal of Chinese Medicine.2017; 45(07): 1441. CrossRef - Addition of nonalbumin proteinuria to albuminuria improves prediction of type 2 diabetic nephropathy progression
Jong Ho Kim, Seo Young Oh, Eun Heui Kim, Min Jin Lee, Yun Kyung Jeon, Bo Hyun Kim, Jin Mi Kim, Yong Ki Kim, Sang Soo Kim, In Joo Kim
Diabetology & Metabolic Syndrome.2017;[Epub] CrossRef - Reversal of Early Diabetic Nephropathy by Islet Transplantation under the Kidney Capsule in a Rat Model
Yunqiang He, Ziqiang Xu, Mingshi Zhou, Minmin Wu, Xuehai Chen, Silu Wang, Kaiyan Qiu, Yong Cai, Hongxing Fu, Bicheng Chen, Mengtao Zhou
Journal of Diabetes Research.2016; 2016: 1. CrossRef
- The Role of Angiotensin-Converting Enzyme (ACE) Polymorphisms in the Risk of Development and Treatment of Diabetic Nephropathy


 KES
KES

 First
First Prev
Prev



