Articles
- Page Path
- HOME > Endocrinol Metab > Volume 35(1); 2020 > Article
-
Original ArticleClinical Study Epidemiology and Prognosis of Pheochromocytoma/Paraganglioma in Korea: A Nationwide Study Based on the National Health Insurance Service
-
Jung Hee Kim1*
 , Hyemi Moon2*
, Hyemi Moon2* , Junghyun Noh3, Juneyoung Lee2, Sin Gon Kim4
, Junghyun Noh3, Juneyoung Lee2, Sin Gon Kim4
-
Endocrinology and Metabolism 2020;35(1):157-164.
DOI: https://doi.org/10.3803/EnM.2020.35.1.157
Published online: March 19, 2020
1Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
2Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
3Division of Endocrinology and Metabolism, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
4Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- Corresponding author: Sin Gon Kim. Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, 73 Inchon-ro, Seongbuk-gu, Seoul 02841, Korea. Tel: +82-2-920-5890, Fax: +82-2-922-5974, k50367@korea.ac.kr
- *These authors contributed equally to this work.
Copyright © 2020 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Pheochromocytomas and paragangliomas (PPGLs) are rare endocrine tumors originating from chromaffin cells. PPGLs are associated with a high mortality rate and several complications. To date, no epidemiological studies have been conducted on PPGLs in Asia. This study aimed to investigate the epidemiology and prognosis of PPGLs in Korea using nationwide data.
-
Methods
- Using the National Health Insurance Service Database, subjects with a principal diagnosis of PPGLs on two or more occasions between 2003 and 2014 who satisfied the operational definition of PPGLs were included. Incidence, prevalence, complications, metastasis, and mortality were investigated.
-
Results
- In total, 1048 subjects with a mean age of 47.6±16.1 years were included. There was no sex preponderance. The overall prevalence of PPGLs was 2.13 per 100,000 persons, and the overall age-standardized incidence rate was 0.18 per 100,000 person-years. Malignant PPGLs accounted for 17.7% (185 of 1,048) of cases, and 94 subjects exhibited metastasis at the time of diagnosis. Among initially non-metastatic PPGLs, 9.5% (nine of 954) eventually metastasized after a mean duration of 78.1±41.4 months. The 5-year survival rates for non-metastatic and metastatic PPGLs at diagnosis were 97% and 84%, respectively. Multivariable Cox regression models adjusted for covariates showed that metastatic PPGLs were associated with a 2.40-fold higher risk of mortality than non-metastatic PPGLs (95% confidence interval, 1.38 to 4.17; P=0.002).
-
Conclusion
- PPGLs are rare in Korea, and the prognosis of these endocrine tumors varies depending on whether they are benign or malignant. This epidemiological study paves the way for further research on PPGLs.
- Pheochromocytomas and paragangliomas (PPGLs) are rare endocrine tumors that originate from chromaffin cells of the sympathetic and parasympathetic nervous systems. Pheochromocytomas (PCCs) most often arise from the adrenal medulla, while paragangliomas (PGLs) tend to arise from the sympathetic or parasympathetic ganglia outside of the adrenal medulla, such as those in the retroperitoneum, pelvis, thorax, head, and neck [1]. While PCCs are commonly functional, in which case they produce one or more catecholamines, PGLs derived from the parasympathetic ganglia are often non-functional. Typical PPGL symptoms that occur due to excess catecholamines include headaches, palpitations, paroxysmal hypertension, and sweating. In addition to these symptoms, cardiovascular and metabolic-related morbidity and mortality also increase due to catecholamine excess [2345]. Furthermore, some PPGLs have metastatic potential. Metastatic PPGLs are defined by the presence of chromaffin cell-derived tumors in non-chromaffin organs at diagnosis or during follow-up. In the past, metastatic PPGLs have accounted for 10% to 20% of all PPGLs [67].
- Among patients with hypertension, the prevalence of PPGLs varies between 0.2% and 0.6%. Approximately 5% to 7% of patients with adrenal incidentalomas are diagnosed with PCCs [89]. In autopsy cases, PCC was recognized in one tumor among 2031 autopsies (0.05%) [10]. However, epidemiological studies are rarely conducted on the level of a national population. A national pathology study conducted in the Netherlands between 1995 and 2015 identified 1,493 patients with PCC or sympathetic PGL, corresponding to an age-standardized incidence rate of 0.57 per 100,000 person-years [11]. The overall incidence of PPGLs has been reported to be gradually increasing over time [11].
- Moreover, to date, no epidemiological studies on PPGLs have been conducted in Korea. Therefore, the aim of this study was to investigate and identify the epidemiology of PPGLs in Korea and to explore related complications and prognoses using nationwide data based on the National Health Insurance Service (NHIS).
INTRODUCTION
- Data source
- The Korean National Health Insurance Program, which is operated by the Ministry for Health, Welfare and Family Affairs, covers nearly the entire Korean population (specifically, around 97%) [12]. All medical institutions submit healthcare utilization-related data to ensure reimbursements, and these data are stored in the NHIS database. Therefore, the NHIS database contains all forms of healthcare data, including data on demographic characteristics, diagnoses, comorbidities (as defined by the International Classification of Diseases, 10th revision [ICD-10]), prescriptions, diagnostic or surgical procedures, and the medical costs of claims. The data used for the present study comprised all NHIS claim records between 2002 and 2014.
- Study subjects
- First, a 1-year window (from January 1, 2002 to December 31, 2002) was set. Subjects with their first claim record in 2002 (n=71), which might have included those diagnosed before 2002, were excluded from this study. Subjects with PPGLs who satisfied the following criteria from January 1, 2003 to December 31, 2014 were included: (1) having the following ICD-10 diagnostic codes as the principal diagnosis on two or more—occasions: D350 (benign neoplasm of adrenal gland), D441 (neoplasm of uncertain behavior, adrenal), I1522 (hypertension due to PCC), C741 (malignant neoplasm, adrenal medulla), or C749 (malignant neoplasm, adrenal nonspecified) for adrenal tumors; D356 (benign neoplasm, aortic body, and PGL), D446 (neoplasm of uncertain behavior, carotid), D447 (neoplasm of uncertain behavior, aortic body, and PGL), D487 (neoplasm of uncertain behavior, unspecific sites), or C755 (malignant neoplasm, aortic body, and PGL) for PGLs. Subjects with one of the above-mentioned diagnoses as the primary diagnosis on two or more occasions were included (n=36,956). The first date of PPGL registration in the NHIS database was assumed to be the date of diagnosis. (2) Identified subjects were further limited to those who were undergoing the following types of surgery after the first date of PPGL registration (n=8,945): P4571 (adrenalectomy, unilateral), P4572 (adrenalectomy, bilateral), P4581 (carotid body tumor resection, unilateral), P4582 (carotid body tumor resection, bilateral), Q2501 (retroperitoneal tumor resection, unilateral), Q2502 (retroperitoneal tumor resection, bilateral), R3512 (transurethral resection of bladder tumor), O1591 (mediastinal tumor resection, unilateral), or O1592 (mediastinal tumor resection, bilateral). (3) Among these, subjects who underwent biochemical tests for catecholamine excess, such as tests for vanillylmandelic acid (C3211, C3212, C3213), epinephrine (C3231), norepinephrine (C3232), dopamine (C3233), normetanephrine (C3234), metanephrine (C3235), or total catecholamines (C3239) at least twice, including at least one preoperative biochemical test, were included (n=1,428). (4) Of the identified cases, patients with primary aldosteronism (E260, I1520, I1521), Cushing syndrome (E240, E248, E249), or adrenal cortical carcinoma (C740) as the principal or secondary diagnosis were excluded (n=380). A total of 1,048 subjects who satisfied all inclusion and exclusion criteria were included (Fig. 1). Among them, metastatic PPGLs were defined as being present in cases with the diagnostic codes of C741, C749, and C755 at least once. Subjects with the diagnostic codes of C741, C749, or C755 at diagnosis were considered to have metastasis at diagnosis. Subjects who had no metastasis at the time of first diagnosis, but in whom metastasis was detected during the follow-up period, were classified as having experienced metastasis during follow-up. Subjects with parasympathetic head and neck PGLs were not included, since these tumors are nonfunctional and may not show a response on biochemical tests.
- Comorbidities were defined if the following diagnostic codes were present as at least two principal or secondary diagnoses, regardless of the date of diagnosis: cerebrovascular disease (I60, I61, I62, I63, I64, I67), cardiovascular disease (I11, I20, I21, I25.1, I50), aortic disease (I71), diabetes mellitus (E10, E11, E12, E13, E14), osteoporosis (M80, M81), and fractures (M48.4, S42.2, S52.0, S52.1, S52.2, S72.0, S72.1, S72.2, S32.0, S32.1, S32.2, S32.5, S22.0).
- Statistical analysis
- The subjects' baseline demographic and clinical characteristics were summarized as mean±standard deviation for interval variables and as numbers (%) for categorical variables. Age-specific incidence rates of PPGLs were calculated by dividing the number of cases in the specific age group by the corresponding age-specific national population. Mortality data obtained from the National Statistical Office were used to determine the survival status of study subjects after PPGL diagnosis. Cox proportional hazard regression models were applied to compare the mortality risk between metastatic and non-metastatic PPGLs. Multivariable Cox proportional hazard regression models were adjusted for age, sex, cerebrovascular disease, cardiovascular disease, diabetes mellitus, and fractures. The proportionality of hazards assumption between metastatic and non-metastatic PPGL groups was examined using a logarithm plot of cumulative hazards, and the assumption was found to be met. Hazard ratios (HRs) and 95% confidence intervals (CI) were calculated. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA) and STATA version 15.0 (Stata Corp., College Station, TX, USA). All P values provided were two-sided, and P values <0.05 were considered to indicate statistical significance.
- Ethical considerations
- Personal information in the Health Insurance Review and Assessment Service database was anonymously encrypted. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 1803-033-926). Informed consent was waived by the IRB.
METHODS
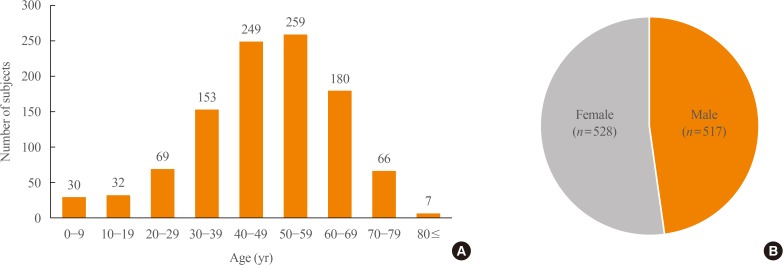
- Between 2003 and 2014, there were a total of 1,048 subjects with PPGLs, with a mean age of 47.6±16.1 years. The peak age of onset varied between 40 and 59 years. There was no sex preponderance (men, n=517 [49.5%]; women, n=528 [50.5%]) (Fig. 2). The overall prevalence of PPGLs was 2.13 per 100,000 persons, while the overall age-standardized incidence rate was 0.18 per 100,000 person-years. The number of subjects with PPGLs was lowest in 2004 (n=54) and highest in 2011 (n=123), and the crude incidence rate showed a similar tendency (Fig. 3).
- PPGLs were accompanied by a variety of comorbidities. When all complications were included regardless of the date of diagnosis, the prevalence rates of cerebrovascular disease, cardiovascular disease, aortic disease, diabetes mellitus, osteoporosis, and fractures were 15.5%, 39.1%, 0.7%, 56.8%, 25.3%, and 6.2%, respectively (Table 1). The overall rate of cardiovascular-related morbidity was approximately 55%.
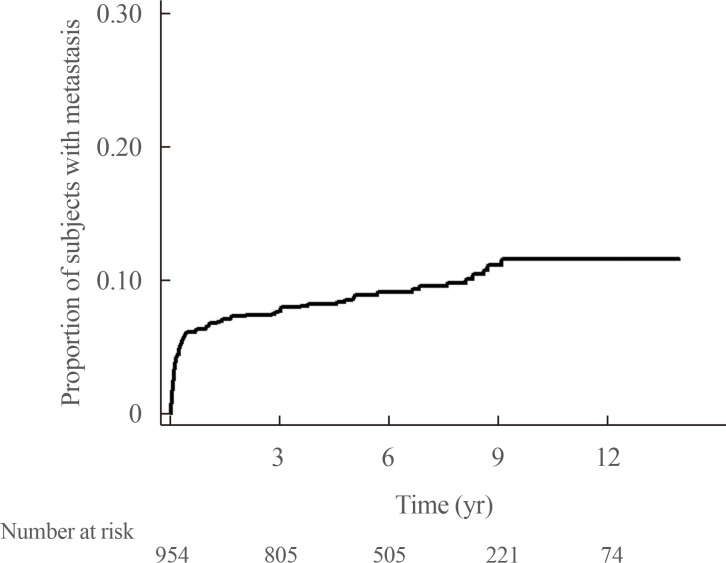
- Further analysis was performed with regard to patients' prognosis. At the time of diagnosis, 9.0% (94/1,048) of PPGLs had already metastasized to other organs. Among initially benign PPGLs (n=954), 9.5% (n=91) eventually metastasized to other organs. The mean duration to progression into metastatic lesions was 78.1±41.4 months (Fig. 4). The overall rate of PPGLs showing malignancy at initial diagnosis or during the follow-up period was 17.7% (185 of 1,048).
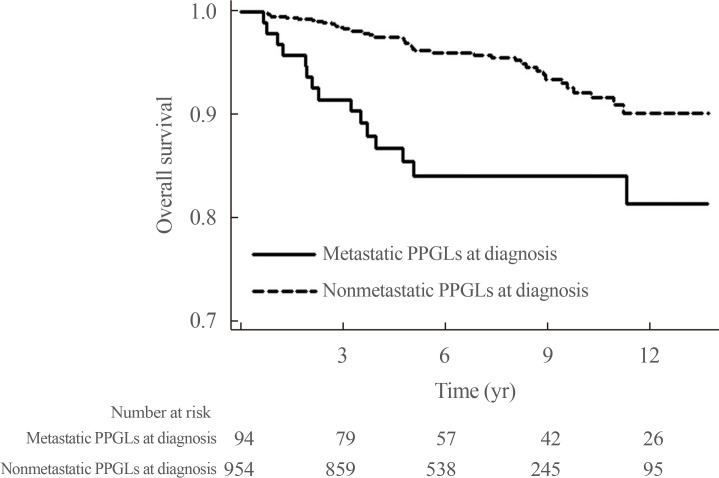
- A total of 61 deaths among 1,048 subjects were reported during a median follow-up duration of 78.8 months (range, 7.9 to 168). Among the 94 subjects who had metastatic PPGLs at diagnosis, 15 died, whereas among the 954 subjects with non-metastatic PPGLs at diagnosis, 46 died. Among the 91 subjects who had initially benign PPGLs, but experienced metastasis during the follow-up period, nine subjects died. The 5-year survival rates for non-metastatic and metastatic PPGLs at diagnosis were 97% and 84%, respectively. The HR for mortality was 2.86 (95% CI, 1.59 to 5.15) for metastatic PPGLs at diagnosis when compared with non-metastatic PPGLs at diagnosis (n=954), with the latter group including 91 patients who experienced metastasis during follow-up (Fig. 5). The HR for mortality was not significantly different between subjects with non-metastatic PPGLs (n=863) and those who had initially benign PPGLs, but experienced metastasis during the follow-up period (n=91) (data not shown, HR, 1.25; 95% CI, 0.59 to 2.65). Table 2 shows that the HR for subjects with metastatic PPGLs at diagnosis or during the follow-up period (n=185) was 2.04 (95% CI, 1.20 to 3.48) when compared with those with non-metastatic PPGLs (n=863). The mean survival time of subjects with metastatic PPGLs at diagnosis was 97.4±51.0 months. In multivariable Cox regression models adjusted for age, sex, cerebrovascular disease, cardiovascular disease, diabetes mellitus, and fractures, metastatic PPGLs at diagnosis or during the follow-up period were associated with a 2.40-fold higher risk of mortality than non-metastatic PPGLs (95% CI, 1.38 to 4.17; P=0.002) (Table 2). Male subjects and those with cerebrovascular disease had particularly high risk of mortality.
RESULTS
- This was the first nationwide population-based epidemiological study of PPGLs to be conducted in Asia, using NHIS data from Korea. In this study, PPGLs were found to have a prevalence of 2.13 per 100,000 persons and an age-standardized incidence of 0.18 per 100,000 person-years. Past studies have reported the prevalence of PPGLs to range from 0.2% to 0.6% in hypertensive patients [13141516]. The incidence rate of PCCs was estimated to be 0.8 per 100,000 person-years (11 cases for 30 years in 45,800 people) in Rochester, Minnesota [17]. However, only a few epidemiological studies have been conducted using a nationwide registry. A recent nationwide pathology registry study conducted in the Netherlands identified a total of 1,493 patients with either PCC or sympathetic PGL between 1995 and 2015 [11]. The researchers reported overall age-standardized incidence rates of 0.37 and 0.57 per 100,000 person-years in 1995–1999 and 2011–2015, respectively [11]. These incidence rates were higher than that reported in the present study (0.18 per 100,000 person-years). The Dutch group reported an increased incidence of PPGLs over the past two decades, in contrast with the present study, which did not demonstrate any increasing trend with time. This difference is most likely due to the shorter study period in the present study than in the Dutch study. The mean age at diagnosis was 47.6 years in Korean PPGL patients, which is similar to or lower than that in previous studies [1118]. Similar to the present study, some studies reported no significant difference in prevalence between the sexes, while findings from another study demonstrated a slight female preponderance (55% vs. 45%) [1118].
- Cardiovascular diseases such as arrhythmia, myocardial ischemia, heart failure, stress-induced cardiomyopathy, and stroke are major complications related to excessive circulating catecholamines [4]. In the present study, the approximate rate of cardiovascular and cerebrovascular disease was 55%, which is higher than the rate reported in a previous study [5]. Hyperglycemia and diabetes mellitus, observed in around 23% to 50% of patients, are some of the potential complications of catecholamine excess [1920]. Similar rates of diabetes mellitus (52.9%) were found in our PPGL subjects. Successful tumor resection resolved diabetes mellitus in 78.6% of patients [20]. Hyperglycemia in PPGL patients results from inhibited insulin secretion, stimulated glucagon secretion, and increased peripheral insulin resistance [19]. The present study revealed osteoporosis and fracture prevalence rates of 25.3% and 6.2%, respectively. With regards to bone health, trabecular bone loss and elevated bone resorption markers have been reported [21]. The apparent mechanism was sympathetic overactivation, which resulted in an uncoupling between excessive bone resorption and inadequate bone formation [22].
- The present study demonstrated a high incidence of metastatic PPGLs in all study subjects (17.8%), which is similar to the rates reported in previous studies (8% to 20%) [672324]. However, a single-center study in Korea reported that among 223 PPGL patients, 12 (5.3%) presented with metastasis at diagnosis, whereas 17 (7.6%) developed metastasis during follow-up [6]. In another Korean study, the prevalence of metastatic PPGLs was 11.0% (n=33) among 299 PPGL patients [24]. The difference between these studies and the present study is most likely due to the different characteristics of the subjects. In the present study, due to the use of claims data, subjects were identified only based on diagnostic codes without pathological confirmation. Thus, pheochromocytomatosis—tumor spillage after adrenalectomy of benign PCCs—may have contributed to the high rate of metastasis [2526]. Nevertheless, subjects of the present study could not be lost to follow-up since the whole national population was included. This study also reported that 10.5% of subjects with non-metastatic PPGLs at the time of initial diagnosis developed metastatic lesions within a median duration of 6 years. Similarly, Hamidi et al. [23] also demonstrated the development of metastases within a median duration of 5.5 years (range, 0.3 to 53.4) from initial diagnosis [23]. This finding emphasized the importance of long-term follow-up, even in patients who initially present with non-metastatic PPGLs.
- Previous reports on the 5-year survival rates for metastatic PPGLs have been widely inconsistent, ranging from 12% to 84% [272829]. A recent study reported a 5-year survival rate of 85.4% in 272 subjects with metastatic PPGLs [23]. In the present study, the 5-year survival rate for metastatic PPGLs was 84%. Individualized treatment for malignant PPGLs is therefore required, and the heterogeneity of metastatic PPGLs must be emphasized.
- The present study had several strengths. First, it explored nationwide data representative of the Korean population and demonstrated the overall prevalence and incidence of PPGLs in Korea. Additionally, enrolled subjects could not be lost to follow-up, since health insurance is mandatory in the Korean population. The use of complete and long-term follow-up data helped in the evaluation of real-world mortality risk.
- However, several inevitable limitations should be mentioned. First, the NHIS database does not include biochemical, imaging, or pathological information. Therefore, due to these pitfalls in the database characteristics, the operational definitions based on the diagnostic code, the number of laboratory tests, and surgery may not reflect the true diagnosis. Definitions based on the diagnostic code, surgery, or prescription code had to be assumed. The prevalence or incidence could therefore have been overestimated or underestimated. To overcome this limitation, the prevalence of PPGLs in a specific region was compared with that of PPGLs at the associated local hospital, which revealed a similar number of PPGL patients. Parasympathetic PGLs can be non-functional, and these may have not been included in the present study. Finally, only patients who underwent surgery were included, so some patients who did not undergo surgery may have been missed. The causes of death could not be investigated since, due to an anonymity protocol, they were not accessible.
- Collectively, the prevalence and annual incidence rates of PPGLs in Korea are 0.18 and 2.13 per 100,000 persons, respectively. Metastatic PPGLs accounted for 17.7% of all PPGLs, including 9.0% with metastasis at the time of diagnosis. PPGLs are accompanied by high rates of mortality and complications. This epidemiological study may pave the way for further research on PPGLs.
DISCUSSION
-
Acknowledgements
- This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KNIDI), funded by the Ministry of Health and Welfare of the Republic of Korea (grant number: HI17C1926). We would like to thank the Committee of Clinical Practice Guidelines of the Korean Endocrine Society.
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS:
Article information
- 1. Lenders JWM, Eisenhofer G. Update on modern management of pheochromocytoma and paraganglioma. Endocrinol Metab (Seoul) 2017;32:152–161. ArticlePubMedPMC
- 2. Plouin PF, Duclos JM, Soppelsa F, Boublil G, Chatellier G. Factors associated with perioperative morbidity and mortality in patients with pheochromocytoma: analysis of 165 operations at a single center. J Clin Endocrinol Metab 2001;86:1480–1486. ArticlePubMed
- 3. Khorram-Manesh A, Ahlman H, Nilsson O, Oden A, Jansson S. Mortality associated with pheochromocytoma in a large Swedish cohort. Eur J Surg Oncol 2004;30:556–559. ArticlePubMed
- 4. Prejbisz A, Lenders JW, Eisenhofer G, Januszewicz A. Cardiovascular manifestations of phaeochromocytoma. J Hypertens 2011;29:2049–2060. ArticlePubMed
- 5. Zelinka T, Petrak O, Turkova H, Holaj R, Strauch B, Krsek M, et al. High incidence of cardiovascular complications in pheochromocytoma. Horm Metab Res 2012;44:379–384. ArticlePubMedPDF
- 6. Kim KY, Kim JH, Hong AR, Seong MW, Lee KE, Kim SJ, et al. Disentangling of malignancy from benign pheochromocytomas/paragangliomas. PLoS One 2016;11:e0168413. ArticlePubMedPMC
- 7. Plouin PF, Fitzgerald P, Rich T, Ayala-Ramirez M, Perrier ND, Baudin E, et al. Metastatic pheochromocytoma and paraganglioma: focus on therapeutics. Horm Metab Res 2012;44:390–399. ArticlePubMedPDF
- 8. Hong AR, Kim JH, Park KS, Kim KY, Lee JH, Kong SH, et al. Optimal follow-up strategies for adrenal incidentalomas: reappraisal of the 2016 ESE-ENSAT guidelines in real clinical practice. Eur J Endocrinol 2017;177:475–483. ArticlePubMed
- 9. Mantero F, Terzolo M, Arnaldi G, Osella G, Masini AM, Ali A, et al. A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. J Clin Endocrinol Metab 2000;85:637–644. PubMed
- 10. McNeil AR, Blok BH, Koelmeyer TD, Burke MP, Hilton JM. Phaeochromocytomas discovered during coronial autopsies in Sydney, Melbourne and Auckland. Aust N Z J Med 2000;30:648–652. ArticlePubMed
- 11. Berends AMA, Buitenwerf E, de Krijger RR, Veeger NJGM, van der Horst-Schrivers ANA, Links TP, et al. Incidence of pheochromocytoma and sympathetic paraganglioma in the Netherlands: a nationwide study and systematic review. Eur J Intern Med 2018;51:68–73. ArticlePubMed
- 12. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol 2017;46:799–800. ArticlePubMedPDF
- 13. Sinclair AM, Isles CG, Brown I, Cameron H, Murray GD, Robertson JW. Secondary hypertension in a blood pressure clinic. Arch Intern Med 1987;147:1289–1293. ArticlePubMed
- 14. Anderson GH Jr, Blakeman N, Streeten DH. The effect of age on prevalence of secondary forms of hypertension in 4429 consecutively referred patients. J Hypertens 1994;12:609–615. ArticlePubMed
- 15. Ariton M, Juan CS, AvRuskin TW. Pheochromocytoma: clinical observations from a Brooklyn tertiary hospital. Endocr Pract 2000;6:249–252. ArticlePubMedPDF
- 16. Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T. Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res 2004;27:193–202. ArticlePubMed
- 17. Beard CM, Sheps SG, Kurland LT, Carney JA, Lie JT. Occurrence of pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin Proc 1983;58:802–804. PubMed
- 18. Guerrero MA, Schreinemakers JM, Vriens MR, Suh I, Hwang J, Shen WT, et al. Clinical spectrum of pheochromocytoma. J Am Coll Surg 2009;209:727–732. ArticlePubMed
- 19. Mesmar B, Poola-Kella S, Malek R. The physiology behind diabetes mellitus in patients with pheochromocytoma: a review of the literature. Endocr Pract 2017;23:999–1005. ArticlePubMed
- 20. Beninato T, Kluijfhout WP, Drake FT, Lim J, Kwon JS, Xiong M, et al. Resection of pheochromocytoma improves diabetes mellitus in the majority of patients. Ann Surg Oncol 2017;24:1208–1213. ArticlePubMedPDF
- 21. Kim BJ, Kwak MK, Ahn SH, Kim H, Lee SH, Song KH, et al. Lower bone mass and higher bone resorption in pheochromocytoma: importance of sympathetic activity on human bone. J Clin Endocrinol Metab 2017;102:2711–2718. ArticlePubMedPDF
- 22. Kim BJ, Lee SH, Koh JM. Bone health in adrenal disorders. Endocrinol Metab (Seoul) 2018;33:1–8. ArticlePubMedPMC
- 23. Hamidi O, Young WF Jr, Iniguez-Ariza NM, Kittah NE, Gruber L, Bancos C, et al. Malignant pheochromocytoma and paraganglioma: 272 patients over 55 years. J Clin Endocrinol Metab 2017;102:3296–3305. ArticlePubMedPMCPDF
- 24. Choi YM, Sung TY, Kim WG, Lee JJ, Ryu JS, Kim TY, et al. Clinical course and prognostic factors in patients with malignant heochromocytoma and paraganglioma: a single institution experience. J Surg Oncol 2015;112:815–821. ArticlePubMed
- 25. Li ML, Fitzgerald PA, Price DC, Norton JA. Iatrogenic pheochromocytomatosis: a previously unreported result of laparoscopic adrenalectomy. Surgery 2001;130:1072–1077. ArticlePubMed
- 26. Bosca Robledo A, Ponce Marco JL, Belda Ibanez T, Meseguer Anastasio MF, Gomez Gavara C. Pheochromocytomatosis: a risk after pheochromocytoma surgery. Am Surg 2010;76:E122–E124. PubMed
- 27. Hamidi O, Young WF Jr, Gruber L, Smestad J, Yan Q, Ponce OJ, et al. Outcomes of patients with metastatic phaeochromocytoma and paraganglioma: a systematic review and meta-analysis. Clin Endocrinol (Oxf) 2017;87:440–450. ArticlePubMedPMC
- 28. Ayala-Ramirez M, Feng L, Johnson MM, Ejaz S, Habra MA, Rich T, et al. Clinical risk factors for malignancy and overall survival in patients with pheochromocytomas and sympathetic paragangliomas: primary tumor size and primary tumor location as prognostic indicators. J Clin Endocrinol Metab 2011;96:717–725. ArticlePubMedPDF
- 29. Goffredo P, Sosa JA, Roman SA. Malignant pheochromocytoma and paraganglioma: a population level analysis of long-term survival over two decades. J Surg Oncol 2013;107:659–664. ArticlePubMed
References
(A) Age and (B) sex distributions of study subjects with pheochromocytomas and paragangliomas. The sex of three subjects was not identified.

The number of study subjects and the incidence rate of pheochromocytomas and paragangliomas by year.

Kaplan-Meier survival curve for metastasis in non-metastatic pheochromocytomas and paragangliomas at diagnosis.
Kaplan-Meier survival curve according to metastasis at diagnosis. PPGL, pheochromocytomas and paraganglioma.
Prevalence of Comorbidities among Study Subjects (n=1,048)
| Comorbidity | No. (%) |
|---|---|
| Cerebrovascular disease | 162 (15.5) |
| Cardiovascular disease | 410 (39.1) |
| Aortic disease | 7 (0.7) |
| Diabetes mellitus | 595 (56.8) |
| Osteoporosis | 265 (25.3) |
| Fracture | 65 (6.2) |
HRs for Mortality in Subjects with Metastatic PPGLs at Any Time (n=185) Compared to Those with Nonmetastatic PPGLs (n=863)
HR, hazard ratio; PPGL, pheochromocytomas and paraganglioma; CI, confidence interval.
aAdjusted for age, sex, cerebrovascular disease, cardiovascular disease, diabetes mellitus, and fractures; bMetastasis at initial diagnosis or during follow-up. HRs compared with subjects with non-metastatic PPGLs are shown.
Figure & Data
References
Citations

- Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Diagnosis and Management of Pheochromocytomas and Paragangliomas: A Guide for the Clinician
Sona Sharma, Lauren Fishbein
Endocrine Practice.2023; 29(12): 999. CrossRef - Pheochromocytoma: a changing perspective and current concepts
Andreas Kiriakopoulos, Periklis Giannakis, Evangelos Menenakos
Therapeutic Advances in Endocrinology and Metabolism.2023;[Epub] CrossRef - Image-Guided Precision Medicine in the Diagnosis and Treatment of Pheochromocytomas and Paragangliomas
Gildas Gabiache, Charline Zadro, Laura Rozenblum, Delphine Vezzosi, Céline Mouly, Matthieu Thoulouzan, Rosine Guimbaud, Philippe Otal, Lawrence Dierickx, Hervé Rousseau, Christopher Trepanier, Laurent Dercle, Fatima-Zohra Mokrane
Cancers.2023; 15(18): 4666. CrossRef - Trends in the incidence of adrenocortical carcinoma and pheochromocytoma/paraganglioma in Taiwan
Chung-Hsin Tsai, Tun-Sung Huang, Shih-Ping Cheng
Formosan Journal of Surgery.2023; 56(5): 147. CrossRef - An open-label, single-arm, multi-center, phase II clinical trial of single-dose [131I]meta-iodobenzylguanidine therapy for patients with refractory pheochromocytoma and paraganglioma
Anri Inaki, Tohru Shiga, Yoshito Tsushima, Megumi Jinguji, Hiroshi Wakabayashi, Daiki Kayano, Norihito Akatani, Takafumi Yamase, Yuji Kunita, Satoru Watanabe, Tomo Hiromasa, Hiroshi Mori, Kenji Hirata, Shiro Watanabe, Tetsuya Higuchi, Hiroyasu Tomonaga, S
Annals of Nuclear Medicine.2022; 36(3): 267. CrossRef - Pheochromocytomas and Abdominal Paragangliomas: A Practical Guidance
Jan Calissendorff, Carl Christofer Juhlin, Irina Bancos, Henrik Falhammar
Cancers.2022; 14(4): 917. CrossRef - Characteristics of Intraoperative Hemodynamic Instability in Postoperatively Diagnosed Pheochromocytoma and Sympathetic Paraganglioma Patients
Jung Hee Kim, Hyung-Chul Lee, Su-jin Kim, Kyu Eun Lee, Kyeong Cheon Jung
Frontiers in Endocrinology.2022;[Epub] CrossRef - Change of Computed Tomography-Based Body Composition after Adrenalectomy in Patients with Pheochromocytoma
Yousun Ko, Heeryoel Jeong, Seungwoo Khang, Jeongjin Lee, Kyung Won Kim, Beom-Jun Kim
Cancers.2022; 14(8): 1967. CrossRef - Systematic Review: Incidence of Pheochromocytoma and Paraganglioma Over 70 Years
Abdul Rahman Al Subhi, Veronica Boyle, Marianne S Elston
Journal of the Endocrine Society.2022;[Epub] CrossRef - Incidence and risk factors for myocardial injury after laparoscopic adrenalectomy for pheochromocytoma: A retrospective cohort study
Ling Lan, Qian Shu, Chunhua Yu, Lijian Pei, Yuelun Zhang, Li Xu, Yuguang Huang
Frontiers in Oncology.2022;[Epub] CrossRef - The Clinical Characteristics of Pheochromocytomas and Paragangliomas with Negative Catecholamines
Lin Zhao, Xiaoran Zhang, Xu Meng, Ting Zhang, Hua Fan, Qiongyu Zhang, Yecheng Liu, Xianliang Zhou, Huadong Zhu
Journal of Clinical Medicine.2022; 11(19): 5583. CrossRef - A midline ectopic paraganglioma
Christina SANT FOURNIER, Matthias FARRUGIA, Kimberley PACE, Christian CAMENZULI, Alexander R. ATTARD
Chirurgia.2022;[Epub] CrossRef - Non-Selective Alpha-Blockers Provide More Stable Intraoperative Hemodynamic Control Compared with Selective Alpha1-Blockers in Patients with Pheochromocytoma and Paraganglioma: A Single-Center Retrospective Cohort Study with a Propensity Score-Matched Ana
Yang Yang, Jie Zhang, Liqun Fang, Xue Jia, Wensheng Zhang
Drug Design, Development and Therapy.2022; Volume 16: 3599. CrossRef - Incidence and Clinical Presentation of Pheochromocytoma and Sympathetic Paraganglioma: A Population-based Study
Andreas Ebbehoj, Kirstine Stochholm, Sarah Forslund Jacobsen, Christian Trolle, Peter Jepsen, Maciej Grzegorz Robaczyk, Åse Krogh Rasmussen, Ulla Feldt-Rasmussen, Reimar Wernich Thomsen, Esben Søndergaard, Per Løgstrup Poulsen
The Journal of Clinical Endocrinology & Metabolism.2021; 106(5): e2251. CrossRef - Determinants of anxiety and depression among pheochromocytoma patients
Siming Jia, Chengbai Li, Zhuqing Lei, Qiang Xia, Yuqing Jiang
Medicine.2021; 100(3): e24335. CrossRef - Pheochromocytoma and paraganglioma with negative results for urinary metanephrines show higher risks for metastatic diseases
Akiyuki Kawashima, Masakatsu Sone, Nobuya Inagaki, Kentaro Okamoto, Mika Tsuiki, Shoichiro Izawa, Michio Otsuki, Shintaro Okamura, Takamasa Ichijo, Takuyuki Katabami, Yoshiyu Takeda, Takanobu Yoshimoto, Mitsuhide Naruse, Akiyo Tanabe
Endocrine.2021; 74(1): 155. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Clinical Presentation and Perioperative Management of Pheochromocytomas and Paragangliomas: A 4-Decade Experience
Thomas Uslar, Ignacio F San Francisco, Roberto Olmos, Stefano Macchiavelo, Alvaro Zuñiga, Pablo Rojas, Marcelo Garrido, Alvaro Huete, Gonzalo P Mendez, Ignacio Cortinez, José Tomás Zemelman, Joaquín Cifuentes, Fernando Castro, Daniela Olivari, José Miguel
Journal of the Endocrine Society.2021;[Epub] CrossRef - Pheochromocytoma
Zhonghua Liu, Junsheng Ma, Camilo Jimenez, Miao Zhang
American Journal of Surgical Pathology.2021; 45(9): 1155. CrossRef - Perioperative hemodynamic instability in pheochromocytoma and sympathetic paraganglioma patients
Jung Hee Kim, Hyung-Chul Lee, Su-jin Kim, Soo Bin Yoon, Sung Hye Kong, Hyeong Won Yu, Young Jun Chai, June Young Choi, Kyu Eun Lee, Kwang-Woong Lee, Seung-Kee Min, Chan Soo Shin, Kyu Joo Park
Scientific Reports.2021;[Epub] CrossRef - Changes in the Nociception Level Index During Surgical Resection of Paragangliomas: A Case Report
Rita Saynhalath, Umar H. Khan, Gijo Alex, Joseph T. Murphy, Peter Szmuk
A&A Practice.2021; 15(11): e01542. CrossRef - Hypertension Cure and Reducing Pill Burden after Adrenalectomy for Endocrine Hypertension of Adrenal Origin: A Comparative Study from an Asian and UK Cohort
Kee Y Ngiam, Ciaran Durand, Titus C Vasciuc, Chia H Tai, Raluca Orpean, Fiona Eatock, Mehak Mahipal, Tan W Boon
World Journal of Endocrine Surgery.2021; 13(1): 9. CrossRef - A Brief Overview of the Epidemiology of Pheochromocytoma and Paraganglioma in Korea
Yun Mi Choi
Endocrinology and Metabolism.2020; 35(1): 95. CrossRef

 KES
KES

 PubReader
PubReader ePub Link
ePub Link Cite
Cite