Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
- Association of Shift Work with Normal-Weight Obesity in Community-Dwelling Adults
- Chul Woo Ahn, Sungjae Shin, Seunghyun Lee, Hye-Sun Park, Namki Hong, Yumie Rhee
- Endocrinol Metab. 2022;37(5):781-790. Published online October 25, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1532
- 3,272 View
- 189 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Shift work is associated with obesity and metabolic syndrome. However, this association in the normal-weight population remains unclear. This study aimed to investigate whether shift work is associated with normal-weight obesity (NWO).
Methods
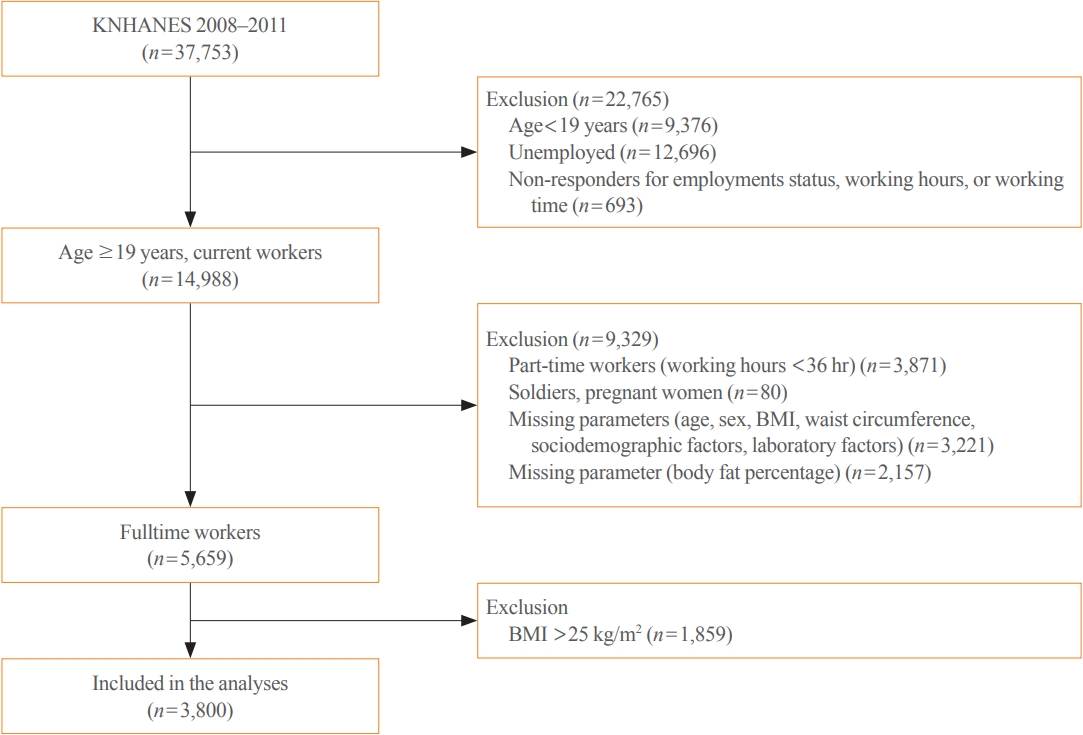
From the nationally representative Korea National Health and Nutrition Examination Survey (KNHANES) dataset (2008 to 2011), 3,800 full-time workers aged ≥19 years with a body mass index (BMI) ≤25 kg/m2 were analysed. We defined NWO as BMI ≤25 kg/m2 and body fat percentage ≥25% in men and ≥37% in women. Working patterns were classified into “daytime,” “other than daytime,” and “shift.” Multivariable logistic regression analysis was performed to evaluate the relationship between shift work and NWO.
Results
Shift work was associated with higher odds of NWO than daytime work (adjusted odds ratio [aOR], 1.47; 95% confidence interval [CI], 1.04 to 2.09) and night/evening work (aOR, 1.87; 95% CI, 1.11 to 3.14) after adjustment for type of work, working hours, age, sex, BMI, 25-hydroxyvitamin D levels, homeostatic model assessment for insulin resistance, and other sociodemographic factors. In subgroup analyses, the association between shift work and NWO was more robust in those aged ≥60 years and those working ≥56 hours/week.
Conclusion
Shift work was associated with NWO in community-dwelling Korean adults, independent of age, sex, BMI, and other covariates. -
Citations
Citations to this article as recorded by- Impaired Melatonin Secretion, Oxidative Stress and Metabolic Syndrome in Night Shift Work
Sorina Hohor, Cristina Mandanach, Andreea Maftei, Corina Aurelia Zugravu, Marina Ruxandra Oțelea
Antioxidants.2023; 12(4): 959. CrossRef - Normal-Weight Obesity and Metabolic Syndrome in Korean Adults: A Population-Based Cross-Sectional Study
Jeonghyeon Kim, Seamon Kang, Hyunsik Kang
Healthcare.2023; 11(16): 2303. CrossRef - You Can’t Avoid Shift Work? Then Focus on Body Fat Rather than Weight
Eun Kyung Lee
Endocrinology and Metabolism.2022; 37(5): 756. CrossRef
- Impaired Melatonin Secretion, Oxidative Stress and Metabolic Syndrome in Night Shift Work

- Diabetes, Obesity and Metabolism
- Musclin Is Related to Insulin Resistance and Body Composition, but Not to Body Mass Index or Cardiorespiratory Capacity in Adults
- Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis Valbuena, Andrés F. Milán, María C. Trillos-Almanza, Sergio Granados, Miguel Peña, Mauricio Estrada-Castrillón, Juan C. Aristizábal, Raúl Narvez-Sanchez, Jaime Gallo-Villegas, Juan C. Calderón
- Endocrinol Metab. 2021;36(5):1055-1068. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1104
- 5,064 View
- 137 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We studied whether musclin function in humans is related to glycemic control, body composition, and cardiorespiratory capacity.
Methods
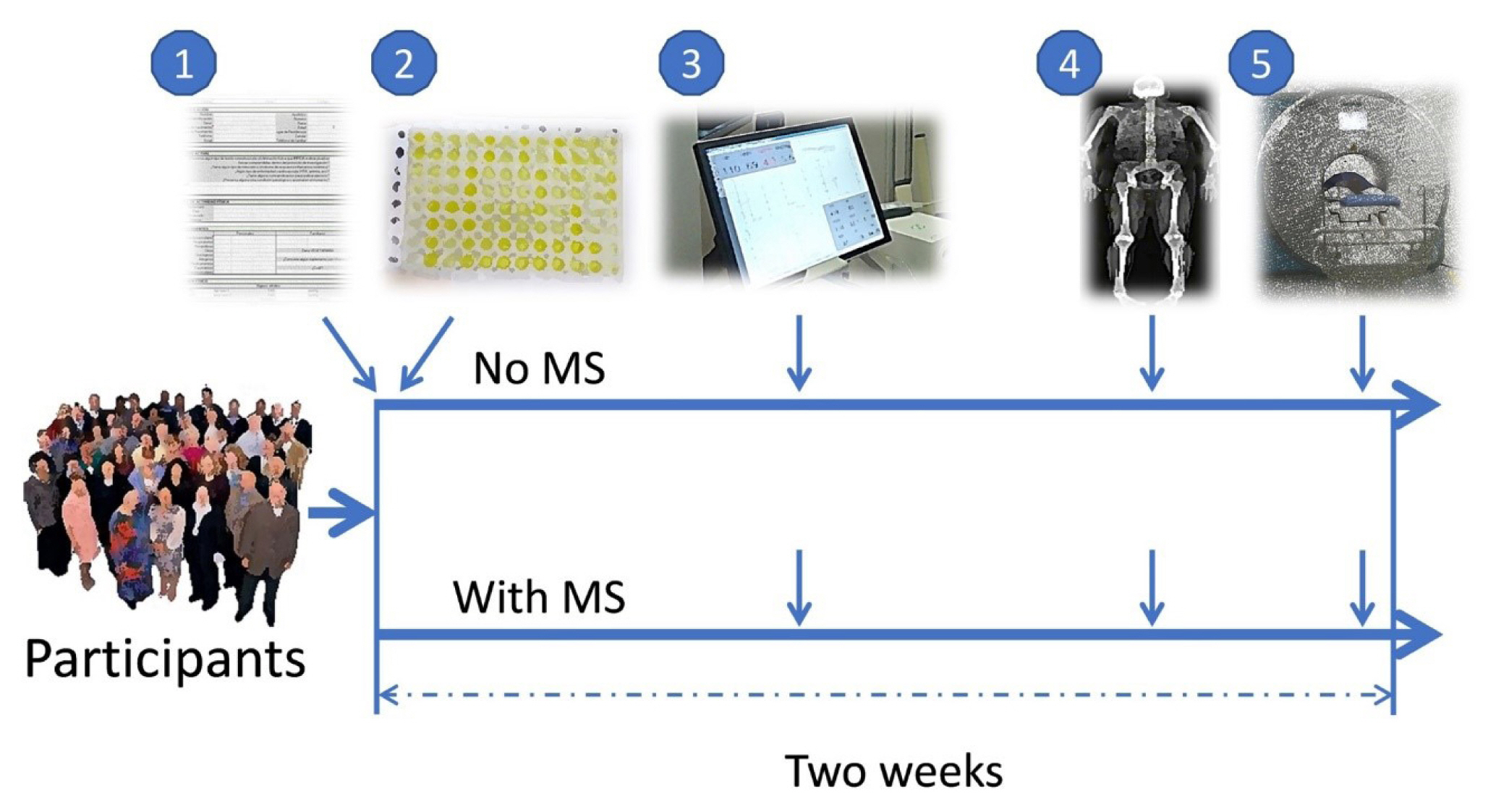
A cross-sectional study was performed in sedentary adults with or without metabolic syndrome (MS). Serum musclin was measured by enzyme-linked immunosorbent assay. Insulin resistance (IR) was evaluated by the homeostatic model assessment (HOMA-IR). Body composition was determined by dual-energy X-ray absorptiometry and muscle composition by measuring carnosine in the thigh, a surrogate of fiber types, through proton magnetic resonance spectroscopy. Cardiorespiratory capacity was assessed through direct ergospirometry.
Results
The control (n=29) and MS (n=61) groups were comparable in age (51.5±6.5 years old vs. 50.7±6.1 years old), sex (72.4% vs. 70.5% women), total lean mass (58.5%±7.4% vs. 57.3%±6.8%), and peak oxygen consumption (VOpeak) (31.0±5.8 mL O2./kg.min vs. 29.2±6.3 mL O2/kg.min). Individuals with MS had higher body mass index (BMI) (30.6±4.0 kg/m2 vs. 27.4± 3.6 kg/m2), HOMA-IR (3.5 [95% confidence interval, CI, 2.9 to 4.6] vs. 1.7 [95% CI, 1.1 to 2.0]), and musclin (206.7 pg/mL [95% CI, 122.7 to 387.8] vs. 111.1 pg/mL [95% CI, 63.2 to 218.5]) values than controls (P˂0.05). Musclin showed a significant relationship with HOMA-IR (β=0.23; 95% CI, 0.12 to 0.33; P˂0.01), but not with VOpeak, in multiple linear regression models adjusted for age, sex, fat mass, lean mass, and physical activity. Musclin was significantly associated with insulin, glycemia, visceral fat, and regional muscle mass, but not with BMI, VCO2peak, maximum heart rate, maximum time of work, or carnosine.
Conclusion
In humans, musclin positively correlates with insulinemia, IR, and a body composition profile with high visceral adiposity and lean mass, but low body fat percentage. Musclin is not related to BMI or cardiorespiratory capacity. -
Citations
Citations to this article as recorded by- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation
Wonjun Cho, Heeseung Oh, Sung Woo Choi, A. M. Abd El-Aty, Fatma Yeşilyurt, Ji Hoon Jeong, Tae Woo Jung
Inflammation.2024; 47(1): 1. CrossRef - Glucose restriction enhances oxidative fiber formation: A multi-omic signal network involving AMPK and CaMK2
Kaiyi Zhang, Ning Xie, Huaqiong Ye, Jiakun Miao, Boce Xia, Yu Yang, Huanqi Peng, Shuang Xu, Tianwen Wu, Cong Tao, Jinxue Ruan, Yanfang Wang, Shulin Yang
iScience.2024; 27(1): 108590. CrossRef - Myokines: metabolic regulation in obesity and type 2 diabetes
Zhi-Tian Chen, Zhi-Xuan Weng, Jiandie D Lin, Zhuo-Xian Meng
Life Metabolism.2024;[Epub] CrossRef - Epidemiological, mechanistic, and practical bases for assessment of cardiorespiratory fitness and muscle status in adults in healthcare settings
Jaime A. Gallo-Villegas, Juan C. Calderón
European Journal of Applied Physiology.2023; 123(5): 945. CrossRef - Serum Levels of Myonectin Are Lower in Adults with Metabolic Syndrome and Are Negatively Correlated with Android Fat Mass
Jorge L. Petro, María Carolina Fragozo-Ramos, Andrés F. Milán, Juan C. Aristizabal, Jaime A. Gallo-Villegas, Juan C. Calderón
International Journal of Molecular Sciences.2023; 24(8): 6874. CrossRef - The correlation of serum musclin with diabetic nephropathy
Jie Zhang, Jing Shi, Zengguang Cheng, Wenchao Hu
Cytokine.2023; 167: 156211. CrossRef - Efficacy of high-intensity interval- or continuous aerobic-training on insulin resistance and muscle function in adults with metabolic syndrome: a clinical trial
Jaime Gallo-Villegas, Leonardo A. Castro-Valencia, Laura Pérez, Daniel Restrepo, Oscar Guerrero, Sergio Cardona, Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis H. Valbuena, Miguel Peña, Andrés F. Milán, Maria C. Trillos-Almanza, Sergio Granados, Juan C.
European Journal of Applied Physiology.2022; 122(2): 331. CrossRef - Reactive Oxygen and Nitrogen Species (RONS) and Cytokines—Myokines Involved in Glucose Uptake and Insulin Resistance in Skeletal Muscle
Paola Llanos, Jesus Palomero
Cells.2022; 11(24): 4008. CrossRef
- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation

- Diabetes
- A Review of the Effects of Glucagon-Like Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors on Lean Body Mass in Humans
- Jack Alistair Sargeant, Joseph Henson, James Adam King, Thomas Yates, Kamlesh Khunti, Melanie Jane Davies
- Endocrinol Metab. 2019;34(3):247-262. Published online September 26, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.3.247
- 11,420 View
- 419 Download
- 57 Web of Science
- 59 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Weight loss is an important goal in the management of several chronic conditions, including type 2 diabetes mellitus, and pharmacological therapies that aid weight loss are appealing. Glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose cotransporter 2 inhibitors (SGLT2is) are novel glucose-lowering therapies that have been shown to induce clinically significant reductions in body weight. However, this weight loss may not be attributed solely to fat mass (FM). Given the importance of skeletal muscle and lean body mass (LBM) on cardio-metabolic health and physical function, we reviewed the available literature reporting the effects of GLP-1RAs and SGLT2is on body composition. Results demonstrate that, in most circumstances, the weight loss associated with both therapies predominantly comprises a reduction in FM, although significant heterogeneity exists between studies. In over half of the studies identified, the proportion of LBM reduction ranged between 20% and 50% of total weight lost, which is consistent with diet-induced weight loss and bariatric surgery. No clear differences existed between GLP-1RAs and SGLT2is. Consequently, the loss of LBM and skeletal muscle associated with weight loss induced by GLP-1RAs and SGLT2is warrants attention. Strategies to preserve skeletal muscle and improve physical function, for example through structured exercise, are of great importance.
-
Citations
Citations to this article as recorded by- Drug‐related sarcopenia as a secondary sarcopenia
Masafumi Kuzuya
Geriatrics & Gerontology International.2024; 24(2): 195. CrossRef - Exercise induces tissue-specific adaptations to enhance cardiometabolic health
Stephen P. Ashcroft, Ben Stocks, Brendan Egan, Juleen R. Zierath
Cell Metabolism.2024; 36(2): 278. CrossRef - Once-weekly semaglutide administered after laparoscopic sleeve gastrectomy: Effects on body weight, glycemic control, and measured nutritional metrics in Japanese patients having both obesity and type 2 diabetes
Rieko Kanai, Sachiho Kinoshita, Izumi Kanbe, Mariko Sameda, Shuhei Yamaoka, Osamu Horikawa, Yasuhiro Watanabe, Ichiro Tatsuno, Kohji Shirai, Takashi Oshiro, Atsuhito Saiki
Obesity Pillars.2024; 9: 100098. CrossRef - Twenty‐four‐hour physical behaviour profiles across type 2 diabetes mellitus subtypes
Joseph Henson, Aikaterina Tziannou, Alex V. Rowlands, Charlotte L. Edwardson, Andrew P. Hall, Melanie J. Davies, Thomas Yates
Diabetes, Obesity and Metabolism.2024; 26(4): 1355. CrossRef - The Current Landscape of Pharmacotherapies for Sarcopenia
Gulistan Bahat, Serdar Ozkok
Drugs & Aging.2024; 41(2): 83. CrossRef - Malnutrition and Sarcopenia as Reasons for Caution with GLP-1 Receptor Agonist Use in HFpEF
ELISSA DRIGGIN, PARAG GOYAL
Journal of Cardiac Failure.2024; 30(4): 610. CrossRef - Is the GLP-1 receptor agonist, semaglutide, a good option for weight loss in persons with HIV?
Daniel Lee, Jacqueline Capeau
AIDS.2024; 38(4): 603. CrossRef - Efficacy and safety of tirzepatide, GLP‐1 receptor agonists, and other weight loss drugs in overweight and obesity: a network meta‐analysis
Xin‐Hui Pan, Bryan Tan, Yip Han Chin, Ethan Cheng Zhe Lee, Gwyneth Kong, Bryan Chong, Martin Kueh, Chin Meng Khoo, Anurag Mehta, Priyanka Majety, Gowtham R. Grandhi, Georgios K. Dimitriadis, Roger Foo, Nicholas W. S. Chew, Carel W. Le Roux, Mamas A. Mamas
Obesity.2024; 32(5): 840. CrossRef - Dual and Triple Incretin-Based Co-agonists: Novel Therapeutics for Obesity and Diabetes
Robert M. Gutgesell, Rubén Nogueiras, Matthias H. Tschöp, Timo D. Müller
Diabetes Therapy.2024; 15(5): 1069. CrossRef - Malnutrition in real-world patients hospitalized for heart failure with preserved ejection fraction and its potential impact on generalizability of EMPEROR-Preserved trial
Shinsuke Takeuchi, Takashi Kohno, Ayumi Goda, Yasuyuki Shiraishi, Mike Saji, Yuji Nagatomo, Toshikazu D. Tanaka, Makoto Takei, Shintaro Nakano, Kyoko Soejima, Shun Kohsaka, Tsutomu Yoshikawa
International Journal of Cardiology.2023; 370: 263. CrossRef - Marked weight loss on liraglutide 3.0 mg: Real‐life experience of a Swiss cohort with obesity
Sara Santini, Nathalie Vionnet, Jérôme Pasquier, Elena Gonzalez‐Rodriguez, Montserrat Fraga, Nelly Pitteloud, Lucie Favre
Obesity.2023; 31(1): 74. CrossRef - Early type 2 diabetes treatment intensification with glucagon‐like peptide‐1 receptor agonists in primary care: An Australian perspective on guidelines and the global evidence
Roy Rasalam, Sarah Abdo, Gary Deed, Richard O'Brien, Jane Overland
Diabetes, Obesity and Metabolism.2023; 25(4): 901. CrossRef - The effects of weight‐lowering pharmacotherapies on physical activity, function and fitness: A systematic review and meta‐analysis of randomized controlled trials
Rishi Jobanputra, Jack A. Sargeant, Abdullah Almaqhawi, Ehtasham Ahmad, Franciskos Arsenyadis, David R. Webb, Louisa Y. Herring, Kamlesh Khunti, Melanie J. Davies, Thomas Yates
Obesity Reviews.2023;[Epub] CrossRef - Combination of exercise and GLP-1 receptor agonist treatment reduces severity of metabolic syndrome, abdominal obesity, and inflammation: a randomized controlled trial
Rasmus M. Sandsdal, Christian R. Juhl, Simon B. K. Jensen, Julie R. Lundgren, Charlotte Janus, Martin B. Blond, Mads Rosenkilde, Adrian F. Bogh, Lasse Gliemann, Jens-Erik B. Jensen, Charalambos Antoniades, Bente M. Stallknecht, Jens J. Holst, Sten Madsbad
Cardiovascular Diabetology.2023;[Epub] CrossRef - Impact of novel glucose‐lowering therapies on physical function in people with type 2 diabetes: A systematic review and meta‐analysis of randomised placebo‐controlled trials
Ehtasham Ahmad, Franciskos Arsenyadis, Abdullah Almaqhawi, Mary Barker, Rishi Jobanputra, Jack A. Sargeant, David R. Webb, Thomas Yates, Melanie J. Davies
Diabetic Medicine.2023;[Epub] CrossRef - Cancer cachexia as a blueprint for treating obesity
Nikolai P. Jaschke, Tilman D. Rachner
Trends in Endocrinology & Metabolism.2023; 34(7): 395. CrossRef - The sun is rising on a new era of pharmacotherapy for obesity: some words of caution
Peter N. Benotti, Bruce R. Bistrian
Surgery for Obesity and Related Diseases.2023; 19(9): 1075. CrossRef - Liraglutide Protects Against Diastolic Dysfunction and Improves Ventricular Protein Translation
Cody Rutledge, Angela Enriquez, Kevin Redding, Mabel Lopez, Steven Mullett, Stacy L. Gelhaus, Michael Jurczak, Eric Goetzman, Brett A. Kaufman
Cardiovascular Drugs and Therapy.2023;[Epub] CrossRef - Effect of sodium-glucose transporter 2 inhibitors on sarcopenia in patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Sha Zhang, Zhan Qi, Yidong Wang, Danfei Song, Deqiu Zhu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cysteine‐lowering treatment with mesna against obesity: Proof of concept and results from a human phase I, dose‐finding study
Kathrine J. Vinknes, Thomas Olsen, Hasse Khiabani Zaré, Nasser E. Bastani, Emma Stolt, Anja F. Dahl, Roger D. Cox, Helga Refsum, Kjetil Retterstøl, Anders Åsberg, Amany Elshorbagy
Diabetes, Obesity and Metabolism.2023; 25(11): 3161. CrossRef - Repurposing Drugs for Diabetes Mellitus as Potential Pharmacological Treatments for Sarcopenia – A Narrative Review
Miles D. Witham, Antoneta Granic, Ewan Pearson, Sian M. Robinson, Avan A. Sayer
Drugs & Aging.2023; 40(8): 703. CrossRef - Introduction to the dietary management of obesity in adults
Vivian Lee
Clinical Medicine.2023; 23(4): 304. CrossRef - Efficacy and safety of the sodium‐glucose co‐transporter‐2 inhibitor empagliflozin in elderly Japanese adults (≥65 years) with type 2 diabetes: A randomized, double‐blind, placebo‐controlled, 52‐week clinical trial (EMPA‐ELDERLY)
Daisuke Yabe, Kosuke Shiki, Gosuke Homma, Thomas Meinicke, Yuji Ogura, Yutaka Seino
Diabetes, Obesity and Metabolism.2023; 25(12): 3538. CrossRef - Independent Link Between Use of Mineralocorticoid Receptor Antagonists and Muscle Wasting in Heart Failure Patients Not Receiving Renin-Angiotensin System Inhibitors
Ryo Numazawa, Satoshi Katano, Toshiyuki Yano, Ryohei Nagaoka, Katsuhiko Ohori, Hidemichi Kouzu, Suguru Honma, Yusuke Fujisawa, Kotaro Yamano, Arata Osanami, Masayuki Koyama, Akiyoshi Hashimoto, Masato Furuhashi
Circulation Journal.2023; 88(1): 10. CrossRef - Sodium-glucose co-transporter 2 inhibitors and Sarcopenia: A controversy that must be solved
Baris Afsar, Rengin Elsurer Afsar
Clinical Nutrition.2023; 42(12): 2338. CrossRef - Oral semaglutide improves body composition and preserves lean mass in patients with type 2 diabetes: a 26-week prospective real-life study
Sara Volpe, Giuseppe Lisco, Margherita Fanelli, Davide Racaniello, Valentina Colaianni, Valentina Lavarra, Domenico Triggiani, Lucilla Crudele, Vincenzo Triggiani, Carlo Sabbà, Giovanni De Pergola, Giuseppina Piazzolla
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Effects of Sodium–Glucose Cotransporter 2 Inhibitors on Body Composition in Type 2 Diabetes Mellitus: A Narrative Review
Soodeh Jahangiri, Mojtaba Malek, Sanjay Kalra, Mohammad E. Khamseh
Diabetes Therapy.2023; 14(12): 2015. CrossRef - Relationship between sodium–glucose cotransporter-2 inhibitors and muscle atrophy in patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Chengdong Xia, Yufeng Han, Chunhui Yin, Ruyue Geng, Zhenfei Liu, Yongle Du, Mingkun Yu
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Role of Lifestyle Modification with Second-Generation Anti-obesity Medications: Comparisons, Questions, and Clinical Opportunities
Thomas A. Wadden, Ariana M. Chao, Molly Moore, Jena S. Tronieri, Adam Gilden, Anastassia Amaro, Sharon Leonard, John M. Jakicic
Current Obesity Reports.2023; 12(4): 453. CrossRef - Sarcopenia and Diabetes: A Detrimental Liaison of Advancing Age
Giuseppe Lisco, Olga Eugenia Disoteo, Anna De Tullio, Vincenzo De Geronimo, Vito Angelo Giagulli, Fabio Monzani, Emilio Jirillo, Renato Cozzi, Edoardo Guastamacchia, Giovanni De Pergola, Vincenzo Triggiani
Nutrients.2023; 16(1): 63. CrossRef - Novel Antidiabetic Strategies and Diabetologists' Views in Nonalcoholic Steatohepatitis
Sabine Kahl, Jennifer Pützer, Michael Roden
Seminars in Liver Disease.2022; 42(01): 048. CrossRef - Effect of Empagliflozin Versus Placebo on Body Fluid Balance in Patients With Acute Myocardial Infarction and Type 2 Diabetes Mellitus: Subgroup Analysis of the EMBODY Trial
Yu Hoshika, Yoshiaki Kubota, Kosuke Mozawa, Shuhei Tara, Yukichi Tokita, Kenji Yodogawa, Yu-Ki Iwasaki, Takeshi Yamamoto, Hitoshi Takano, Yayoi Tsukada, Kuniya Asai, Masaaki Miyamoto, Yasushi Miyauchi, Eitaro Kodani, Mitsunori Maruyama, Jun Tanabe, Wataru
Journal of Cardiac Failure.2022; 28(1): 56. CrossRef - Effect of GLP-1 receptor agonist, liraglutide, on muscle in spontaneously diabetic torii fatty rats
Shohei Yamada, Yuji Ogura, Kazuho Inoue, Jun Tanabe, Takeshi Sugaya, Keiichi Ohata, Yoshio Nagai, Yasunori Natsuki, Seiko Hoshino, Shiika Watanabe, Daisuke Ichikawa, Kenjiro Kimura, Yugo Shibagaki, Atsuko Kamijo-Ikemori
Molecular and Cellular Endocrinology.2022; 539: 111472. CrossRef - Exendin-4 alleviates steatosis in an in vitro cell model by lowering FABP1 and FOXA1 expression via the Wnt/-catenin signaling pathway
Olfa Khalifa, Neyla S. AL-Akl, Khaoula Errafii, Abdelilah Arredouani
Scientific Reports.2022;[Epub] CrossRef - Body composition changes at 12 months following different surgical weight loss interventions in adults with obesity: A systematic review and meta‐analysis of randomized control trials
Amy Sylivris, Jakub Mesinovic, David Scott, Paul Jansons
Obesity Reviews.2022;[Epub] CrossRef - Safety and effectiveness of empagliflozin in Japanese patients with type 2 diabetes: final results of a 3-year post-marketing surveillance study
Kohei Kaku, Kazuhiro Yamamoto, Yumiko Fukushima, Hristo Lliev, Atsutaka Yasui
Expert Opinion on Drug Safety.2022; 21(10): 1315. CrossRef - Safety and effectiveness of empagliflozin according to body mass index in Japanese patients with type 2 diabetes: a subgroup analysis of a 3-year post-marketing surveillance study
Kohei Kaku, Kazuhiro Yamamoto, Yumiko Fukushima, Seiko Mizuno, Daisuke Nitta
Expert Opinion on Drug Safety.2022; 21(11): 1411. CrossRef - Le risque de dénutrition chez le sujet âgé diabétique : une limite à l’utilisation des « nouvelles » classes thérapeutiques ?
Lyse Bordier, Jean Doucet, Bernard Bauduceau
Médecine des Maladies Métaboliques.2022; 16(5): 422. CrossRef - Emerging evidence of the relationship between fat-free mass and ghrelin, glucagon-like peptide-1, and peptide-YY
Austin J. Graybeal, Jada L. Willis, Elisa Morales-Marroquin, Grant M. Tinsley, Sarah E. Messiah, Meena Shah
Nutrition.2022; 103-104: 111815. CrossRef - The Effectiveness of GLP-1 Receptor Agonist Semaglutide on Body Composition in Elderly Obese Diabetic Patients: A Pilot Study
Yoshinori Ozeki, Takayuki Masaki, Akari Kamata, Shotaro Miyamoto, Yuichi Yoshida, Mitsuhiro Okamoto, Koro Gotoh, Hirotaka Shibata
Medicines.2022; 9(9): 47. CrossRef - Distribution of lean mass and mortality risk in patients with type 2 diabetes
Li Ding, Yuxin Fan, Jingting Qiao, Jing He, Ruodan Wang, Qing He, Jingqiu Cui, Zhongshu Ma, Fangqiu Zheng, Hua Gao, Chenlin Dai, Hongyan Wei, Jun Li, Yuming Cao, Gang Hu, Ming Liu
Primary Care Diabetes.2022; 16(6): 824. CrossRef - Cardio-sarcopenia: A syndrome of concern in aging
De Rong Loh, Ru-San Tan, Wee Shiong Lim, Angela S. Koh
Frontiers in Medicine.2022;[Epub] CrossRef - Type 2 diabetes
Ehtasham Ahmad, Soo Lim, Roberta Lamptey, David R Webb, Melanie J Davies
The Lancet.2022; 400(10365): 1803. CrossRef - Elevated circulating level of β-aminoisobutyric acid (BAIBA) in heart failure patients with type 2 diabetes receiving sodium-glucose cotransporter 2 inhibitors
Satoshi Katano, Toshiyuki Yano, Hidemichi Kouzu, Ryohei Nagaoka, Ryo Numazawa, Kotaro Yamano, Yusuke Fujisawa, Katsuhiko Ohori, Nobutaka Nagano, Takefumi Fujito, Ryo Nishikawa, Wataru Ohwada, Masaki Katayose, Tatsuya Sato, Atsushi Kuno, Masato Furuhashi
Cardiovascular Diabetology.2022;[Epub] CrossRef - An overview of anamorelin as a treatment option for cancer-associated anorexia and cachexia
Guilherme Wesley Peixoto Da Fonseca, Stephan von Haehling
Expert Opinion on Pharmacotherapy.2021; 22(7): 889. CrossRef - Liraglutide Does Not Adversely Impact Fat‐Free Mass Loss
Andrew Grannell, William P. Martin, Babak Dehestani, Werd Al‐Najim, John C. Murphy, Carel W. le Roux
Obesity.2021; 29(3): 529. CrossRef - Rationale and design of the EMPA-ELDERLY trial: a randomised, double-blind, placebo-controlled, 52-week clinical trial of the efficacy and safety of the sodium–glucose cotransporter-2 inhibitor empagliflozin in elderly Japanese patients with type 2 diabet
Daisuke Yabe, Kosuke Shiki, Keiko Suzaki, Thomas Meinicke, Yutaro Kotobuki, Kenichiro Nishida, Douglas Clark, Atsutaka Yasui, Yutaka Seino
BMJ Open.2021; 11(4): e045844. CrossRef - Cancer Risk in Normal Weight Individuals with Metabolic Obesity: A Narrative Review
Bethina Liu, Hugh E. Giffney, Rhonda S. Arthur, Thomas E. Rohan, Andrew J. Dannenberg
Cancer Prevention Research.2021; 14(5): 509. CrossRef - Comprehensive analysis of LncRNAs expression profiles in an in vitro model of steatosis treated with Exendin-4
Khaoula Errafii, Neyla S. Al-Akl, Olfa Khalifa, Abdelilah Arredouani
Journal of Translational Medicine.2021;[Epub] CrossRef - Dapagliflozin increases the lean-to total mass ratio in type 2 diabetes mellitus
Vaneza Lira W. Wolf, Ikaro Breder, Luiz Sérgio F. de Carvalho, Alexandre A. S. Soares, Riobaldo M. Cintra, Joaquim Barreto, Daniel B. Munhoz, Sheila T. Kimura-Medorima, Wilson Nadruz, Gil Guerra-Júnior, Thiago Quinaglia, Elza Muscelli, Andrei C. Sposito
Nutrition & Diabetes.2021;[Epub] CrossRef - Optimising the Heart Failure Treatment Pathway: The Role of SGLT2 Inhibitors
Marc Evans, Angharad R. Morgan, Zaheer Yousef, Gethin Ellis, Umesh Dashora, Dipesh C. Patel, Pam Brown, Wasim Hanif, Johnathan N. Townend, Naresh Kanumilli, Jim Moore, John P. H. Wilding, Stephen C. Bain
Drugs.2021; 81(11): 1243. CrossRef - Glucose-lowering Drugs and Hospitalization for Heart Failure: A Systematic Review and Additive-effects Network Meta-analysis With More Than 500 000 Patient-years
Riobaldo M Cintra, Ana Claudia Nogueira, Isabella Bonilha, Beatriz M Luchiari, Otavio R Coelho-Filho, Otavio R Coelho, Pedro Schwartzmann, Elza Muscellie, Wilson Nadruz, Luiz Sergio F Carvalho, Andrei C Sposito
The Journal of Clinical Endocrinology & Metabolism.2021; 106(10): 3060. CrossRef - Physical activity and exercise in the management of type 2 diabetes: where to start?
Deirdre Harrington, Joe Henson
Practical Diabetes.2021; 38(5): 35. CrossRef - Efpeglenatide and Heart and Kidney Outcomes in Type 2 Diabetes
New England Journal of Medicine.2021; 385(22): 2105. CrossRef - Effects of Antidiabetic Drugs on Muscle Mass in Type 2 Diabetes Mellitus
Satoshi Ida, Ryutaro Kaneko, Kanako Imataka, Kaoru Okubo, Yoshitaka Shirakura, Kentaro Azuma, Ryoko Fujiwara, Kazuya Murata
Current Diabetes Reviews.2021; 17(3): 293. CrossRef - Effects of liraglutide and empagliflozin added to insulin therapy in patients with type 2 diabetes: A randomized controlled study
Hirotatsu Nakaguchi, Yoshinobu Kondo, Mayu Kyohara, Hiromi Konishi, Koji Oiwa, Yasuo Terauchi
Journal of Diabetes Investigation.2020; 11(6): 1542. CrossRef - Sodium Glucose Co-Transporter 2 Inhibition Does Not Favorably Modify the Physiological Responses to Dietary Counselling in Diabetes-Free, Sedentary Overweight and Obese Adult Humans
Shane P.P. Ryan, Alissa A. Newman, Jessie R. Wilburn, Lauren D. Rhoades, S. Raj J. Trikha, Ellen C. Godwin, Hayden M. Schoenberg, Micah L. Battson, Taylor R. Ewell, Gary J. Luckasen, Laurie M. Biela, Christopher L. Melby, Christopher Bell
Nutrients.2020; 12(2): 510. CrossRef - GLP-1 Receptor Agonist Treatment in Morbid Obesity and Type 2 Diabetes Due to Pathogenic Homozygous Melanocortin-4 Receptor Mutation: A Case Report
Eva W. Iepsen, Christian T. Have, Simon Veedfald, Sten Madsbad, Jens J. Holst, Niels Grarup, Oluf Pedersen, Ivan Brandslund, Jens-Christian Holm, Torben Hansen, Signe S. Torekov
Cell Reports Medicine.2020; 1(1): 100006. CrossRef - Glucagon‐like peptide 1 infusions overcome anabolic resistance to feeding in older human muscle
Haitham Abdulla, Bethan E. Phillips, Daniel J. Wilkinson, Marie Limb, Tereza Jandova, Joseph J. Bass, Debbie Rankin, Jessica Cegielski, Mariwan Sayda, Hannah Crossland, John P. Williams, Kenneth Smith, Iskandar Idris, Philip J. Atherton
Aging Cell.2020;[Epub] CrossRef
- Drug‐related sarcopenia as a secondary sarcopenia

- Clinical Study
- Effects of Short-Term Exenatide Treatment on Regional Fat Distribution, Glycated Hemoglobin Levels, and Aortic Pulse Wave Velocity of Obese Type 2 Diabetes Mellitus Patients
- Ju-Young Hong, Keun-Young Park, Byung-Joon Kim, Won-Min Hwang, Dong-Ho Kim, Dong-Mee Lim
- Endocrinol Metab. 2016;31(1):80-85. Published online March 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.1.80
- 4,962 View
- 49 Download
- 26 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Most type 2 diabetes mellitus patients are obese and have obesity related vascular complications. Exenatide treatment is well known for both decreasing glycated hemoglobin levels and reduction in body weight. So, this study aimed to determine the effects of exenatide on body composition, glycated hemoglobin levels, and vascular stiffness in obese type 2 diabetes mellitus patients.
Methods For 1 month, 32 obese type 2 diabetes mellitus patients were administered 5 µg of exenatide twice daily. The dosage was then increased to 10 µg. Patients' height, body weight, glycated hemoglobin levels, lipid profile, pulse wave velocity (PWV), body mass index, fat mass, and muscle mass were measured by using Inbody at baseline and after 3 months of treatment.
Results After 3 months of treatment, glycated hemoglobin levels decreased significantly (
P =0.007). Triglyceride, total cholesterol, and low density lipoprotein levels decreased, while aspartate aminotransferase and alanine aminotransferase levels were no change. Body weight, and fat mass decreased significantly (P =0.002 andP =0.001, respectively), while interestingly, muscle mass did not decrease (P =0.289). In addition to, Waist-to-hip ratio and aortic PWV decreased significantly (P =0.006 andP =0.001, respectively).Conclusion Effects of short term exenatide use in obese type 2 diabetes mellitus with cardiometabolic high risk patients not only reduced body weight without muscle mass loss, body fat mass, and glycated hemoglobin levels but also improved aortic PWV in accordance with waist to hip ratio.
-
Citations
Citations to this article as recorded by- Adipose tissue inflammation linked to obesity: A review of current understanding, therapies and relevance of phyto-therapeutics
Christiana Eleojo Aruwa, Saheed Sabiu
Heliyon.2024; 10(1): e23114. CrossRef - Separate and combined effects of empagliflozin and semaglutide on vascular function: A 32‐week randomized trial
Liv Vernstrøm, Søren Gullaksen, Steffen S. Sørensen, Kristian L. Funck, Esben Laugesen, Per L. Poulsen
Diabetes, Obesity and Metabolism.2024; 26(5): 1624. CrossRef - Diabetic Sarcopenia. A proposed muscle screening protocol in people with diabetes
Daniel de Luis Román, Juana Carretero Gómez, José Manuel García-Almeida, Fernando Garrachón Vallo, German Guzmán Rolo, Juan José López Gómez, Francisco José Tarazona-Santabalbina, Alejandro Sanz-Paris
Reviews in Endocrine and Metabolic Disorders.2024;[Epub] CrossRef - The Current Landscape of Pharmacotherapies for Sarcopenia
Gulistan Bahat, Serdar Ozkok
Drugs & Aging.2024; 41(2): 83. CrossRef - Vascular Aging: Assessment and Intervention
Ao Li, Jinhua Yan, Ya Zhao, Zhenping Yu, Shane Tian, Abdul Haseeb Khan, Yuanzheng Zhu, Andong Wu, Cuntai Zhang, Xiao-Li Tian
Clinical Interventions in Aging.2023; Volume 18: 1373. CrossRef - The Effect of Additional Treatment with Empagliflozin or Semaglutide on Endothelial Function and Arterial Stiffness in Subjects with Type 1 Diabetes Mellitus—ENDIS Study
Maja Preložnik Navodnik, Andrej Janež, Ivan Žuran
Pharmaceutics.2023; 15(7): 1945. CrossRef - Sarcopenia as a Little-Recognized Comorbidity of Type II Diabetes Mellitus: A Review of the Diagnosis and Treatment
Christian Salom Vendrell, Elisa García Tercero, Juan Bautista Moro Hernández, Bernardo Abel Cedeno-Veloz
Nutrients.2023; 15(19): 4149. CrossRef - Oral semaglutide improves body composition and preserves lean mass in patients with type 2 diabetes: a 26-week prospective real-life study
Sara Volpe, Giuseppe Lisco, Margherita Fanelli, Davide Racaniello, Valentina Colaianni, Valentina Lavarra, Domenico Triggiani, Lucilla Crudele, Vincenzo Triggiani, Carlo Sabbà, Giovanni De Pergola, Giuseppina Piazzolla
Frontiers in Endocrinology.2023;[Epub] CrossRef - GLP1 Receptor Agonists—Effects beyond Obesity and Diabetes
Sydney S. Wilbon, Mikhail G. Kolonin
Cells.2023; 13(1): 65. CrossRef - The Effectiveness of GLP-1 Receptor Agonist Semaglutide on Body Composition in Elderly Obese Diabetic Patients: A Pilot Study
Yoshinori Ozeki, Takayuki Masaki, Akari Kamata, Shotaro Miyamoto, Yuichi Yoshida, Mitsuhiro Okamoto, Koro Gotoh, Hirotaka Shibata
Medicines.2022; 9(9): 47. CrossRef - Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus
Juan J. Gorgojo-Martínez, Pedro Mezquita-Raya, Juana Carretero-Gómez, Almudena Castro, Ana Cebrián-Cuenca, Alejandra de Torres-Sánchez, María Dolores García-de-Lucas, Julio Núñez, Juan Carlos Obaya, María José Soler, José Luis Górriz, Miguel Ángel Rubio-H
Journal of Clinical Medicine.2022; 12(1): 145. CrossRef - The Impact of Glucose-Lowering Drugs on Sarcopenia in Type 2 Diabetes: Current Evidence and Underlying Mechanisms
Elena Massimino, Anna Izzo, Gabriele Riccardi, Giuseppe Della Pepa
Cells.2021; 10(8): 1958. CrossRef - Anti‐diabetic drugs and sarcopenia: emerging links, mechanistic insights, and clinical implications
Xueli Zhang, Yi Zhao, Shuobing Chen, Hua Shao
Journal of Cachexia, Sarcopenia and Muscle.2021; 12(6): 1368. CrossRef - Effect of glycemic control on markers of subclinical atherosclerosis in patients with type 2 diabetes mellitus: A review
Sofia Antoniou, Katerina K K Naka, Marios Papadakis, Aris Bechlioulis, Agathocles Tsatsoulis, Lampros K Michalis, Stelios Tigas
World Journal of Diabetes.2021; 12(11): 1856. CrossRef - A Review of the Effects of Glucagon-Like Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors on Lean Body Mass in Humans
Jack Alistair Sargeant, Joseph Henson, James Adam King, Thomas Yates, Kamlesh Khunti, Melanie Jane Davies
Endocrinology and Metabolism.2019; 34(3): 247. CrossRef - The effect of dulaglutide on body composition in type 2 diabetes mellitus patients on hemodialysis
Takahiro Yajima, Kumiko Yajima, Hiroshi Takahashi, Keigo Yasuda
Journal of Diabetes and its Complications.2018; 32(8): 759. CrossRef - Effects of Newer Antidiabetic Drugs on Endothelial Function and Arterial Stiffness: A Systematic Review and Meta-Analysis
Konstantinos Batzias, Alexios S. Antonopoulos, Evangelos Oikonomou, Gerasimos Siasos, Evanthia Bletsa, Panagiota K. Stampouloglou, Chara-Vasiliki Mistakidi, Marina Noutsou, Niki Katsiki, Periklis Karopoulos, Georgios Charalambous, Anastasia Thanopoulou, N
Journal of Diabetes Research.2018; 2018: 1. CrossRef - Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes
N. González, Z. Moreno-Villegas, A. González-Bris, J. Egido, Ó. Lorenzo
Cardiovascular Diabetology.2017;[Epub] CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Difference in protective effects of GIP and GLP-1 on endothelial cells according to cyclic adenosine monophosphate response
Dong-Mee Lim, Keun-Young Park, Won-Min Hwang, Ju-Young Kim, Byung-Joon Kim
Experimental and Therapeutic Medicine.2017; 13(5): 2558. CrossRef - Treatment Strategy for Type 2 Diabetes with Obesity: Focus on Glucagon-like Peptide-1 Receptor Agonists
Qiuhe Ji
Clinical Therapeutics.2017; 39(6): 1244. CrossRef - Differential Role of Adipose Tissues in Obesity and Related Metabolic and Vascular Complications
Almudena Gómez-Hernández, Nuria Beneit, Sabela Díaz-Castroverde, Óscar Escribano
International Journal of Endocrinology.2016; 2016: 1. CrossRef
- Adipose tissue inflammation linked to obesity: A review of current understanding, therapies and relevance of phyto-therapeutics

- Clinical Study
- Characteristics of Body Composition and Muscle Strength of North Korean Refugees during South Korean Stay
- Sun Wook Cho, So Hee Lee, Eun Sil Koh, Si Eun Kim, Seok Joong Kim
- Endocrinol Metab. 2015;30(4):551-556. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.551
- 3,621 View
- 39 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the changes of body composition and muscle strength of North Korean refugees (NKRs) according to their duration of stay in South Korea.
Methods NKRs who volunteered and were living in South Korea, aged 20 to 75 years were recruited. Body compositions were analyzed by bioelectrical impedance analysis. Muscle strength was measured with the hand grip test. Demographic and migration information was obtained with a questionnaire.
Results A total of 158 volunteers were recruited at a mean age of 48.3±11.4 years. The mean time from when they escaped from North Korea and arrived in South Korea was 5.8±4.3 years. Height, weight, and body surface area were significantly smaller in all NKRs compared to South Korean controls, except for women aged over 50 years. In females of younger ages (<50 years), NKRs with more than a 4-year stay in South Korea had a higher weight and fat mass than that of those who had a shorter stay (less than 4 years) in South Korea. All NKRs had a weaker grip strength than that of the age-matched controls from South Korea.
Conclusion The NKRs showed relatively smaller physiques and weaker muscle strength than that of the South Korean controls. In younger female NKRs, shorter South Korean stay group showed small body weight and fat mass than that of longer South Korean stay group. Specific health support programs might be needed.
-
Citations
Citations to this article as recorded by- Assessment of diet quality of adults from North Korea: using nutrition quotient (NQ) for Korean adults
SaeByeol Kwon, Kyoung-Nam Kim, Moon-Kyung Shin
Journal of Nutrition and Health.2023; 56(2): 217. CrossRef - Associations between grip strength, cardiorespiratory fitness, cardiovascular risk and mental health in forcibly displaced people from a Greek refugee camp
Markus Gerber, Konstantinia Filippou, Florian Knappe, Ioannis D. Morres, Emmanouil Tzormpatzakis, Elsa Havas, Harald Seelig, Flora Colledge, Sebastian Ludyga, Marianne Meier, Yannis Theodorakis, Roland von Känel, Uwe Pühse, Antonis Hatzigeorgiadis
Scientific Reports.2023;[Epub] CrossRef - Weight Gain Predicts Metabolic Syndrome among North Korean Refugees in South Korea
Yoon Jung Kim, Yo Han Lee, Yun Jeong Lee, Kyeong Jin Kim, Sin Gon Kim
International Journal of Environmental Research and Public Health.2021; 18(16): 8479. CrossRef - Prevalence of General and Central Obesity and Associated Factors among North Korean Refugees in South Korea by Duration after Defection from North Korea: A Cross-Sectional Study
Yoon Kim, Sin Kim, Yo Lee
International Journal of Environmental Research and Public Health.2018; 15(4): 811. CrossRef
- Assessment of diet quality of adults from North Korea: using nutrition quotient (NQ) for Korean adults

- The One Year Effects of Growth Hormone Replacement on the Body Composition in the Normal Adults.
- Eui Hyun Kim, Suk Chon, Kwan Pyo Koh, Seong Joon Oh, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
- J Korean Endocr Soc. 2004;19(4):303-319. Published online August 1, 2004
- 1,018 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The secretion of growth hormone [GH] declines by 14.4% every decade, leading to the suggestion that the elderly are functionally GH deficient, which may increase adipose tissue and decrease the bone mass and density, as well as other negative changes in body composition. Recently, many studies have shown that GH replacement therapy may restore the changes that occur in the body composition with aging. AIM: The GH and insulin like growth factor-I[IGF-I] profiles were identified during GH replacement therapy in the elderly and compared with those of GH deficient[GHD] patients. The metabolic effects of GH replacement on the body composition of the elderly was also investigated, especially the body fat, muscle and bone parameters. Subjects and METHODS: 98 healthy normal out-patients and 13 GHD patients, who had peak GH concentrations less than 5 ng/mL after an insulin tolerance test [ITT] or growth hormone releasing hormone [GHRH] stimulation test, were the subjects of this study. All were receiving appropriate thyroid, adrenal and gonadal hormone replacements. The dose of recombinant human GH [rhGH] was 0.02~0.04 mg [0.06~0.12 IU]/kg of body weight.per week, given nightly by a subcutaneous injection, six times a week, over a 52 week period. The GH was measures after the ITT and GHRH stimulation tests, and the IGF-1, lipid parameters [total cholesterol, triglyceride, HDL-, and LDL cholesterol], visceral adipose tissue [VAT], subcutaneous adipose tissue [SAT], VAT/SAT ratio, quadriceps muscle area, total body fat, total bone mineral density [BMD], alkaline phosphatase [ALP], osteocalcin and urine deoxypyridinoline [DYP], as well as anthropometry, were also assessed. RESULTS: All the anthropometry features between the normal and GHD subjects were very similar. The hormonal profiles were checked; the GH peaks of the ITT and GHRH stimulation tests were significantly higher in the normal compared to the GHD patients, but the GHRH test showed lower GH peaks in than those of the ITT test in the normal subjects. The IGF-I levels after GH replacement were constantly maintained in the normal and GHD groups after 3 week and until the 52nd week. According to the lipid profiles, the GHD group showed significantly decreased total cholesterol and LDL-cholesterol after 12 weeks of GH replacement. The normal male group revealed constantly increased triglyceride levels during the entire 52 weeks of GH replacement, but thr other lipid parameters remained completely unchanged. The normal female group showed no change in any of their lipid parameters. Although the amounts of VAT at the baseline were the same in all groups, only the normal males showed effective visceral fat removal, with significantly reduced VAT after 52 weeks of GH treatment. In the normal female and GHD groups the bone mineral density had a V shaped curve after GH replacement, and the ALP and osteocalcin levels were significantly increased after 26 weeks of GH therapy in the GHD group. CONCLUSION: The body compositions in the normal male, female and GHD groups were similar before the GH replacement therapy, and the serum IGF-I levels were well maintained in all these groups during GH replacement. Although the majority of aging symptoms were improved, the body compositions tended to return to their original stati in the normal groups. GH replacement is recommended in the elderly for better health and well-being

- The Effects of Growth Hormone Tretment on Body Composition and Glucose Metabolism in Adult Hypophysectomized Rats.
- Kwan Woo Lee, Hyun Chul Lee, Kap Bum Huh, Yoon Sok Chung, Deok Bae Park, Yup Kang, Hyeon Man Kim, Seoung Oh Yang
- J Korean Endocr Soc. 1997;12(1):53-60. Published online January 1, 2001
- 980 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It is well known that growth hormone (GH) stimulates animal growth, but studies on metabolic effects of growth hormone have recently been increasing. The purpose of this study was to clarify the effects of growth hormone treatment on body composition and glucose metabolism in hypophysectomized growth hormone-deficient rats. METHODS: The 20-week-old rnale Sprague-Dawley rats were hypophysectomized and replaced with cortisol and thyroxine for 8 weeks, then administered with recombinant human growth hormone for 2 weeks. Group 1 consisted of intact controls (n 15), while group 2 consisted of hypophysectomized controls (n 12), and group three consisted of those with GH treatment (n 13). The body weights, body composition, blood glucose levels, plasma insulin-like growth factor-I (IGF-I) levels, euglycemic hyperinsulinemic clamp test, and glycogen synthase activities in gastrocnemius muscle were measured before and after growth hormone treatment. RESULTS: Plasma IGF-I levels in GH-treated group increased to intact control group levels after 2 weeks of GH treatment. There were significant changes in body composition after the treatment (fat mass significantly decreased and lean body mass significantly increased). There were no changes in glucose metabolism in peripheral tissue after 2 weeks of GH treatment. CONCLUSION: Human GH treatment (4 IU/kg/day) in adult hypophysectomized GH-deficient rats changed the body composition, but did not alter the glucose metabolism in peripheral tissue.


 KES
KES

 First
First Prev
Prev



