Articles
- Page Path
- HOME > Endocrinol Metab > Volume 29(4); 2014 > Article
-
Original ArticleClinical Study Sex Factors in the Metabolic Syndrome as a Predictor of Cardiovascular Disease
- Sunghwan Suh1*, Jongha Baek2*, Ji Cheol Bae3, Kyoung-Nyoun Kim1, Mi Kyoung Park1, Duk Kyu Kim1, Nam H. Cho4, Moon-Kyu Lee2
-
Endocrinology and Metabolism 2014;29(4):522-529.
DOI: https://doi.org/10.3803/EnM.2014.29.4.522
Published online: December 29, 2014
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Dong-A Medical Center, Dong-A University College of Medicine, Busan, Korea.
2Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
3Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
4Department of Preventive Medicine, Ajou University School of Medicine, Suwon, Korea.
- Corresponding author: Nam H. Cho. Department of Preventive Medicine, Ajou University School of Medicine, 206 World cup-ro, Yeongtong-gu, Suwon 443-721, Korea. Tel: +82-31-219-5083, Fax: +82-31-219-5084, chnaha@ajou.ac.kr
- Corresponding author: Moon-Kyu Lee. Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 135-710, Korea. Tel: +82-2-3410-3431, Fax: +82-2-3410-0393, leemk@skku.edu
- *These authors contributed equally to this work.
Copyright © 2014 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Metabolic syndrome (MetS) is a condition characterized by a cluster of metabolic disorders and is associated with increased risk of cardiovascular disease (CVD). This study analyzed data from the Korean Health and Genome Study to examine the impact of MetS on CVD.
-
Methods
- A total of 8,898 subjects (4,241 males and 4,657 females), 40 to 69 years of age, were enrolled and evaluated for the development of new onset CVD from 2001 to 2012 (median 8.1 years of follow-up).
-
Results
- The prevalence of MetS at baseline was 22.0% (932/4,241) and 29.7% (1,383/4,657) in males and females, respectively. MetS was associated with increased risk of coronary heart disease (CHD; hazard ratio [HR], 1.818; 95% confidence interval [CI], 1.312 to 2.520 in males; HR, 1.789; 95% CI, 1.332 to 2.404 in females) and CVD (HR, 1.689; 95% CI, 1.295 to 2.204 in males; HR, 1.686; 95% CI, 1.007 to 2.192 in females). Specifically, MetS was associated with risk of future stroke in females only (HR, 1.486; 95% CI, 1.007 to 2.192). Among MetS components, abdominal obesity and hypertension were independent predictors of both CHD and CVD. In addition, a higher number of MetS components correlated with higher CVD risk.
-
Conclusion
- MetS is a significant risk factor for the development of CVD although its impact varies between sexes.
- Metabolic syndrome (MetS) is a condition characterized by a cluster of metabolic disorders including abdominal obesity, insulin resistance/glucose intolerance, dyslipidemia and hypertension. The concept of MetS was introduced by Reaven [1] in 1988, as a clustering of cardiovascular risks, and MetS prevalence is increasing worldwide. The significance of MetS has unraveled gradually in recent years. According to data from the National Health and Nutrition Examination Survey (NHANES) III and NHANESs 1999 to 2006, the age-adjusted prevalence of MetS increased from 29.2% to 34.2% in the United States [2], and a similar trend has been observed in Asian countries [3]. The age-adjusted prevalence of MetS in Korea increased rapidly from 24.9% in 1998 to 31.3% in 2007 [4]. MetS also increases the risk of developing diabetes mellitus (DM) because its components represent major risk factors for impaired glucose metabolism [5]. Accordingly, the prevalence of DM and obesity in Korea has steadily increased [6,7] becoming one of the main targets of public health intervention as well as a social and economic problem in the near future. It is well documented that MetS is associated with increased risk of all-cause mortality and cardiovascular disease (CVD) [8,9,10]. However, the role of MetS in the development of CVD in Korea has only been shown in studies with small sample sizes or cross-sectional designs [11,12,13]. Therefore, this study analyzed data from the largest-scale Korean community based prospective cohort study to examine the impact of MetS on CVD over a 10-year follow-up period.
INTRODUCTION
- Study population
- The design and baseline characteristics of the Ansung-Ansan cohort study have been published previously [14]. Briefly, it is an ongoing prospective, community-based cohort study that is part of the Korean Health and Genome Study (KHGS), a community-based epidemiological survey to investigate trends in DM and associated risk factors. The baseline examination was performed in 2001 to 2002, and biennial follow-up examinations were continued through 2012. To be eligible, subjects must be 40 to 69 years old, have resided within the borders of the survey area for at least 6 months before testing, and be mentally and physically able to participate. Participants were recruited from two Korean communities within 60 km of Seoul. Ansung is a representative rural farming community that had a population of 132,906 in 2000 [15]. Ansan is a representative urban community that had a population of 554,998 in 2000 [15]. A total of 10,038 subjects (5,018 from Ansung and 5,020 from Ansan, respectively) were enrolled in KHGS. Throughout the study, the same trained researchers and instruments were used to collect data. Anthropometric parameters and blood pressure were measured by standard methods. Fasting plasma glucose, lipid profiles, insulin and proteinuria were measured in a central laboratory. Social factors (smoking, exercise, and alcohol intake) were assessed by questionnaire. Current smokers were defined as those who smoked at least one cigarette per day for at least the prior year. Excessive alcohol intake was defined as consumption of ≥30 g of alcohol per day. Informed written consent was obtained from all participants. The study protocol was approved by the ethics committee of the Korean Center for Disease Control and the Institutional Review Board of Ajou University School of Medicine.
- Definition of the MetS
- Subjects were diagnosed with MetS if they met at least three of the following revised National Cholesterol Education Program Adult Treatment Panel III criteria [16]: (1) abdominal obesity; (2) triglycerides 150 mg/dL or greater; (3) high density lipoprotein cholesterol (HDL-C) less than 40 mg/dL in males or less than 50 mg/dL in females; (4) blood pressure 130/85 mm Hg or greater, or current use of antihypertensive medications; or (5) fasting plasma glucose 100 mg/dL or greater, or previously diagnosed type 2 DM or on oral antidiabetic agents or insulin. Abdominal obesity was defined as a waist circumference ≥90 cm for males and ≥85 cm for females, which are the proposed ethnically appropriate abdominal obesity criteria for Korean people by the Korean Society for the Study of Obesity [17].
- Determination of incident CVD
- Coronary heart disease (CHD) was defined as definite myocardial infarction confirmed by electrocardiogram and/or enzyme changes or any angina diagnosis that required intervention after confirmation of coronary artery stenosis by coronary angiography. Stroke included cerebral infarction, hemorrhagic stroke, transient ischemic attack, and vertebrobasilar insufficiency as demonstrated by diagnostic work-ups, such as, computed tomography, magnetic resonance imaging studies and accompanying neurologic symptoms and/or signs. CVD was defined as the occurrence of CHD and/or stroke. Persons with medical events reported by the patient himself or found during routine follow-up were asked to bring their medical records. Each event was confirmed and documented by the relevant clinical information (death certificates, postmortem reports, medical records, hospital discharge summaries, laboratory results, etc.). Initial data were obtained from 10,038 subjects who participated in KHGS. Among these subjects, 1,140 were excluded for the following reasons: (1) previous history of CVD (n=230); (2) lack of follow-up examinations after baseline examination (n=908); and (3) missing data (n=2). After applying the above exclusion criteria, a total of 8,898 subjects were eligible for the study. Among them, 692 developed CVD events during the 10-year follow-up period (mean follow-up of 96.8 months). The CVD group comprised all those who developed CVD during the follow-up period.
- Statistical analyses
- Statistical analyses were carried out using PASW version 21.0 (IBM Co., Armonk, NY, USA). Descriptive statistics for continuous data are expressed as the mean±standard deviation if normally distributed. Discrete data were summarized as numbers with percentages. Independent t test and Mann-Whitney U test were used to compare differences in continuous variables between the two groups. Chi-squared tests were used to analyze dichotomous variables between the groups. Age- and multivariate-adjusted hazard ratios (HR) and 95% confidence intervals (CIs) were estimated with the use of the Cox proportional hazards model to examine MetS baseline status and determine whether the variables played a role in the prediction of incident CHD, stroke, or CVD. For all statistical analyses, a two-sided P<0.05 was considered statistically significant.
METHODS
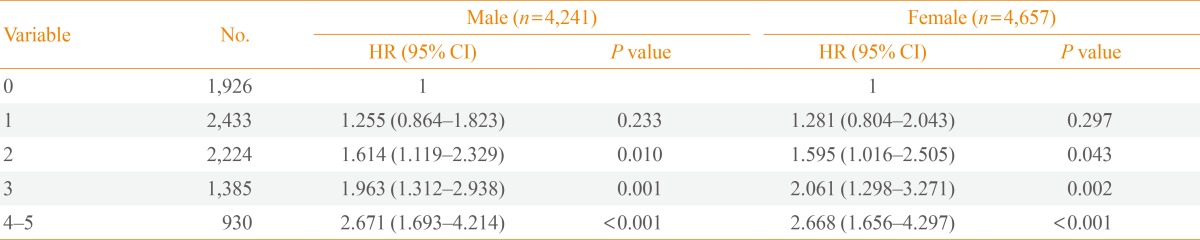
- Baseline characteristics of the study subjects are shown in Table 1. Mean follow-up duration was 8.1 years. The overall prevalence of MetS at baseline was 26.0% (22.0% in males and 29.7% in females). Males had significantly higher waist circumference, fasting plasma glucose, diastolic blood pressure, and triglycerides. A greater proportion of males were also current smokers and reported excessive alcohol intake. Compared to males, females were older and had higher body mass index, HDL-C level and homeostasis model of assessment-insulin resistance (HOMA-IR). Females also had a greater number of MetS components (1.8 vs. 1.5) compared to males. MetS was associated with CVD in both males and females despite controlling for other well-documented cardiovascular risk factors. Specifically, MetS was found to be associated with an increased risk of future CHD (HR, 1.818; 95% CI, 1.312 to 2.520; P<0.001) and CVD (HR, 1.689; 95% CI, 1.295 to 2.204; P<0.001) in males. In females, MetS was significantly correlated with the development of CHD (HR, 1.789; 95% CI, 1.332 to 2.404; P<0.001), stroke (HR, 1.486; 95% CI, 1.007 to 2.192; P=0.046), and CVD (HR, 1.686; 95% CI, 1.319 to 2.154; P<0.001) after a mean follow-up of 8.1 years (Table 2). In addition to MetS itself, some individual components of the MetS were also significantly associated with the risk of developing CHD, stroke or CVD. This was independent of known cardiovascular risk factors such as age, current smoking, low density lipoprotein cholesterol (LDL-C), and HOMA-IR (Table 3). Abdominal obesity was an independent predictor of both CHD and CVD in both sexes. Hypertension was a significant risk factor in all outcome parameters including CHD, stroke, and CVD in both males and females. Hyperglycemia was significantly associated with CHD and CVD only in males. However, lipid parameters (i.e., triglycerides and HDL-C) were not significantly correlated with the development of CVD. The HR for developing CVD increased with increasing numbers of MetS components, after adjusting for confounding factors (Table 4).
RESULTS
- In the present study, MetS was a significant risk factor for the development of CVD although its impact varies between sexes. More specifically, MetS was correlated with the development of stroke only in females. In addition, the number of MetS components was linearly associated with risk of CVD or CHD.
- The overall prevalence rate of CVD in KHGS during the 10-year follow-up period was 7.7% (692/8,898). Overall, MetS prevalence was 26.0% (2,315/8,898) and a higher proportion of females had MetS compared to men, which is similar to previously reported values [4]. A meta-analysis by Gami et al. [18] that included 36 different prospective studies found that the overall relative risk for incident CVD for individuals with MetS was 1.78 (95% CI, 1.58 to 2.00). In this study, the HR for development of CVD was 1.689 (95% CI, 1.295 to 2.204) in males and 1.686 (95% CI, 1.319 to 2.154) in females. This HR is also close to the estimate obtained from Asia Pacific Cohort Study Collaboration, which gathered individual data from 35 cohorts from the Republic of Korea, China, Hong Kong, Japan, Taiwan, Thailand, and Singapore [19]. In the present study, MetS was associated with risk of stroke in females, which has been reported previously [11,20]. Northern Manhattan Study [21] and The Atherosclerosis Risk in Communities data [22] also found that the effect of MetS on stroke risk was greater among women. They suggested that there may be risk differentials according to sex for the MetS due to disparities in the prevalence and potency of vascular risk factors. Sex differences in MetS components (higher proportion of abdominal obesity and lower HDL-C levels in females; data not shown) in this study could explain this phenomenon. Alternative explanations for possible sex differences include a greater impact of the MetS among postmenopausal women. CVD development rate was much higher in females age ≥50 compared to the others (data not shown). However, we do not have data on menopause and hormone use in KHGS. Longitudinal studies based on stroke registries suggested that women are more likely than men to have a stroke and the natural course of stroke is worse in women having a higher probability to be functionally dependent and institutionalized [23]. Recently, meta-analysis found that the excess risk of stroke associated with DM is significantly higher in women than men [24]. These data support the idea that that women's metabolic and vascular risk factor profile has to deteriorate to a greater extent than men to transition from normal to a deranged metabolic state. Moreover, it has been suggested that gender difference in arterial structure and function may lead to gender difference in the relationship of risk factors with stroke [25].
- Among the five MetS components, blood pressure and abdominal obesity components were the key predictors of CVD in this study. Hypertension itself is a known cardiovascular risk factor [26,27] and data from 57,237 subjects who came to regular health examinations at a single center in Korea also confirmed this association [28]. Moreover, abdominal obesity is significantly associated with risk of CHD [29] and insulin resistance, which is the underlying etiology of MetS [1]. Abdominal obesity is a major factor in the increased prevalence of MetS in Koreans over the past 10 years [4]. It was previously reported that MetS is associated with abnormal left ventricular structure and function [30,31]. This cardiac dysfunction induced by insulin resistance and MetS could explain the development of CVD [32]. Hyperglycemia was associated with CHD and CVD only in males, although components of hyperglycemia were predictors of CHD and CVD in total subjects including both males and females (data not shown). Lipid parameters did not predict the development of CVD, though previous reports are inconsistent regarding which MetS components predict CVD [10,11,13,28]. These discrepancies may be explained in part by the different study populations and different follow-up periods of each study. Aside from MetS components, age, smoking status, LDL-C, and HOMA-IR are independent risk factors of CVD (data not shown) which are well-known risk factors of CVD [27].
- The present study showed that the risk of incident CVD was found to increase with the number of MetS components, and increased by 2.6-fold in those with four or more MetS components compared to those without any MetS components. This synergistic association is noteworthy because some individual components such as hypertriglyceridemia and low HDL-C levels were not significant predictors of CVD. Frequency of CHD, stroke, and CVD were significantly correlated with an increasing number of MetS components (data not shown). This linear synergistic correlation has been reported previously [13,20] and increases the likelihood of CVD to an extent greater than the likelihood conferred by any individual MetS component [33]. This study also found that the risk of CVD increased incrementally as the number of MetS components increased. A similar relationship was found when CVD was sub-classified as CHD or stroke (data not shown). Two or more MetS components were predictive of CVD. This suggests that subjects with two MetS components (especially those with abdominal obesity and hypertension) who do not yet have MetS, should be alert for the development of CVD. Furthermore, it is important to determine ethnicity-specific cutoff points for individual components of MetS based on cardiovascular outcomes.
- To the best of the authors' knowledge, this study is the largest prospective cohort study of a Korean population with a long follow-up period that reports the association of MetS with incident CVD. The strengths of this study include its longitudinal population-based study design, long duration of follow-up and sufficient number of CVD events, data analysis according to sex and exclusion of patients with CVD at baseline. One limitation of this study is that MetS diagnosis was based on a single measurement of MetS components at baseline. During follow-up, risk factors may have changed due to medication or lifestyle modifications, and thus MetS diagnosis may have changed during the course of the study. This would weaken the associations found in this study, biasing the results toward the null hypothesis. Therefore, the associations reported here may be stronger than the results indicate.
- In summary, MetS was found to be associated with future risk of CHD and CVD in a prospective study with 10 years of follow-up. More specifically, MetS predicted stroke in females and CHD/CVD in both sexes. Risk of incident CVD increased with the number of MetS components. Therefore, individualized lifestyle modifications according to sex and number of MetS components, with or without pharmacological interventions, should be conducted to reduce the burden and negative consequences of MetS.
DISCUSSION
-
Acknowledgements
- The authors are grateful to Bong Deok Kim and Hyun Kyu Kim, staff of the Center for Clinical Epidemiology, Ajou University School of Medicine, for their effort in managing the Korean Health and Genome Study. The epidemiological study was supported by the National Genome Research Institute, the Korean Center for Disease Control and Prevention (contract #2001~2003-348-6111-221, 2004-347-6111-213 and 2005-347-2400-2440-215). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
ACKNOWLEDGMENTS
- 1. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988;37:1595–1607. ArticlePubMed
- 2. Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999-2006. Diabetes Care 2011;34:216–219. ArticlePubMed
- 3. Pan WH, Yeh WT, Weng LC. Epidemiology of metabolic syndrome in Asia. Asia Pac J Clin Nutr 2008;17(Suppl 1):37–42. PubMed
- 4. Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, Choi SH, Cho SI, Park KS, Lee HK, Jang HC, Koh KK. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care 2011;34:1323–1328. ArticlePubMedPMC
- 5. Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA, Stern MP. Prospective analysis of the insulin-resistance syndrome (syndrome X). Diabetes 1992;41:715–722. ArticlePubMed
- 6. Oh SW. Obesity and metabolic syndrome in Korea. Diabetes Metab J 2011;35:561–566. ArticlePubMedPMC
- 7. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J 2011;35:303–308. ArticlePubMedPMC
- 8. Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med 2006;119:812–819. ArticlePubMed
- 9. Alexander CM, Landsman PB, Teutsch SM, Haffner SM. Third National Health and Nutrition Examination Survey (NHANES III). National Cholesterol Education Program (NCEP). NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 2003;52:1210–1214. ArticlePubMed
- 10. Chien KL, Hsu HC, Sung FC, Su TC, Chen MF, Lee YT. Metabolic syndrome as a risk factor for coronary heart disease and stroke: an 11-year prospective cohort in Taiwan community. Atherosclerosis 2007;194:214–221. ArticlePubMed
- 11. Hwang YC, Jee JH, Oh EY, Choi YH, Lee MS, Kim KW, Lee MK. Metabolic syndrome as a predictor of cardiovascular diseases and type 2 diabetes in Koreans. Int J Cardiol 2009;134:313–321. ArticlePubMed
- 12. Kim MH, Kim MK, Choi BY, Shin YJ. Prevalence of the metabolic syndrome and its association with cardiovascular diseases in Korea. J Korean Med Sci 2004;19:195–201. ArticlePubMedPMC
- 13. Khang YH, Cho SI, Kim HR. Risks for cardiovascular disease, stroke, ischaemic heart disease, and diabetes mellitus associated with the metabolic syndrome using the new harmonised definition: findings from nationally representative longitudinal data from an Asian population. Atherosclerosis 2010;213:579–585. ArticlePubMed
- 14. Kim BG, Park JT, Ahn Y, Kimm K, Shin C. Geographical difference in the prevalence of isolated systolic hypertension in middle-aged men and women in Korea: the Korean Health and Genome Study. J Hum Hypertens 2005;19:877–883. ArticlePubMedPDF
- 15. Choi SH, Kim TH, Lim S, Park KS, Jang HC, Cho NH. Hemoglobin A1c as a diagnostic tool for diabetes screening and new-onset diabetes prediction: a 6-year community-based prospective study. Diabetes Care 2011;34:944–949. ArticlePubMedPMC
- 16. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–2752. ArticlePubMed
- 17. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, Kim DY, Kwon HS, Kim SR, Lee CB, Oh SJ, Park CY, Yoo HJ. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract 2007;75:72–80. ArticlePubMed
- 18. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol 2007;49:403–414. ArticlePubMed
- 19. Asia Pacific Cohort Studies Collaboration. Patel A, Barzi F, Woodard M, Ni Mhurchu C, Ohkubo T, Lam TH, Welborn T. An evaluation of metabolic risks for coronary death in the Asia Pacific region. Diabetes Res Clin Pract 2006;74:274–281. ArticlePubMed
- 20. Ninomiya T, Kubo M, Doi Y, Yonemoto K, Tanizaki Y, Rahman M, Arima H, Tsuryuya K, Iida M, Kiyohara Y. Impact of metabolic syndrome on the development of cardiovascular disease in a general Japanese population: the Hisayama study. Stroke 2007;38:2063–2069. ArticlePubMed
- 21. Boden-Albala B, Sacco RL, Lee HS, Grahame-Clarke C, Rundek T, Elkind MV, Wright C, Giardina EG, DiTullio MR, Homma S, Paik MC. Metabolic syndrome and ischemic stroke risk: Northern Manhattan Study. Stroke 2008;39:30–35. ArticlePubMed
- 22. McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care 2005;28:385–390. ArticlePubMed
- 23. Lorenzano S, Ahmed N, Falcou A, Mikulik R, Tatlisumak T, Roffe C, Wahlgren N, Toni D. SITS Investigators. Does sex influence the response to intravenous thrombolysis in ischemic stroke?: answers from safe implementation of treatments in Stroke-International Stroke Thrombolysis Register. Stroke 2013;44:3401–3406. ArticlePubMed
- 24. Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet 2014;383:1973–1980. ArticlePubMed
- 25. Walsh T, Donnelly T, Lyons D. Why a sex difference in age-adjusted relationship between height and stroke mortality? Stroke 2007;38:e92ArticlePubMed
- 26. Kannel WB. Elevated systolic blood pressure as a cardiovascular risk factor. Am J Cardiol 2000;85:251–255. ArticlePubMed
- 27. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2013 update: a report from the American Heart Association. Circulation 2013;127:e6–e245. ArticlePubMed
- 28. Shin CY, Yun KE, Park HS. Blood pressure has a greater impact on cardiovascular mortality than other components of metabolic syndrome in Koreans. Atherosclerosis 2009;205:614–619. ArticlePubMed
- 29. Felix-Redondo FJ, Grau M, Baena-Diez JM, Degano IR, de Leon AC, Guembe MJ, Alzamora MT, Vega-Alonso T, Robles NR, Ortiz H, Rigo F, Mayoral-Sanchez E, Tormo MJ, Segura-Fragoso A, Fernandez-Berges D. Prevalence of obesity and associated cardiovascular risk: the DARIOS study. BMC Public Health 2013;13:542ArticlePubMedPMC
- 30. Gong HP, Tan HW, Fang NN, Song T, Li SH, Zhong M, Zhang W, Zhang Y. Impaired left ventricular systolic and diastolic function in patients with metabolic syndrome as assessed by strain and strain rate imaging. Diabetes Res Clin Pract 2009;83:300–307. ArticlePubMed
- 31. Aijaz B, Ammar KA, Lopez-Jimenez F, Redfield MM, Jacobsen SJ, Rodeheffer RJ. Abnormal cardiac structure and function in the metabolic syndrome: a population-based study. Mayo Clin Proc 2008;83:1350–1357. ArticlePubMedPMC
- 32. Sundstrom J, Arnlov J, Stolare K, Lind L. Blood pressure-independent relations of left ventricular geometry to the metabolic syndrome and insulin resistance: a population-based study. Heart 2008;94:874–878. ArticlePubMed
- 33. Hutcheson R, Rocic P. The metabolic syndrome, oxidative stress, environment, and cardiovascular disease: the great exploration. Exp Diabetes Res 2012;2012:271028ArticlePubMedPMCPDF
References
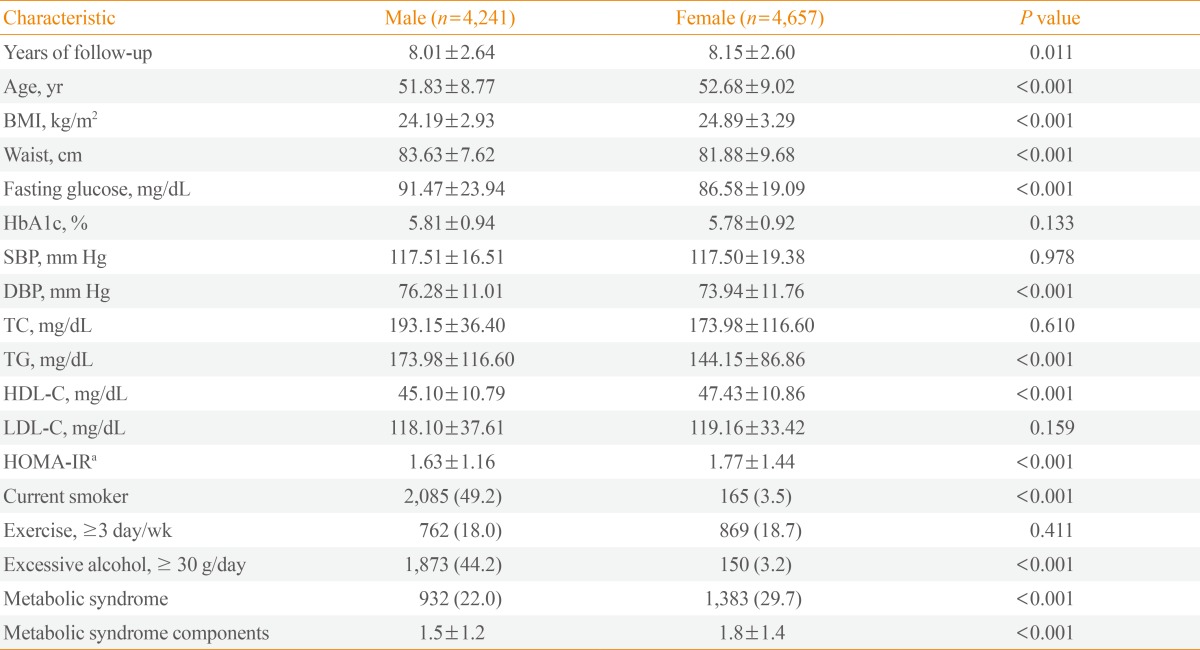
Values are expressed as mean±SD or number (%).
BMI, body mass index; HbA1c, glycated hemoglobin; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; TG, triglycerides; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; HOMA-IR, homeostasis model of assessment-insulin resistance.
aHOMA-IR=[fasting plasma glucose (mmol/L)×fasting plasma insulin]/22.5.
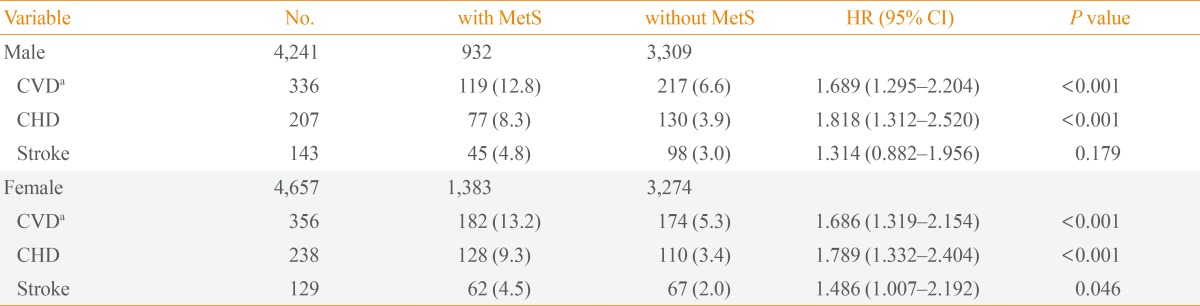
Values are expressed as number (%). Adjusted for age, smoking status, low density lipoprotein cholesterol, and homeostasis model of assessment-insulin resistance.
MetS, metabolic syndrome; HR, hazard ratio; CI, confidence interval; CVD, cardiovascular disease; CHD, coronary heart disease.
aCVD was defined as occurrence of CHD and/or stroke.
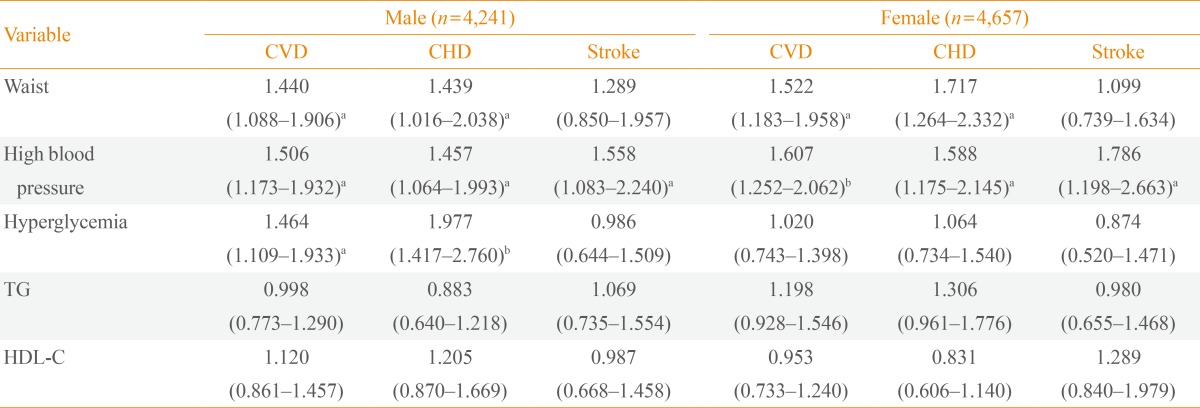
Values are expressed as hazard ratio (95% confidence interval). Adjusted for age, smoking status, low density lipoprotein cholesterol, homeostasis model of assessment-insulin resistance, and metabolic syndrome components.
CVD, cardiovascular disease; CHD, coronary heart disease; TG, triglycerides; HDL, high density lipoprotein cholesterol.
aP<0.05; bP<0.001.
Figure & Data
References
Citations

- Cardiovascular age of workers with different employment categories
Byung-Kook Lee, Jaeouk Ahn, Nam-Soo Kim, Jungsun Park, Yangho Kim
Archives of Environmental & Occupational Health.2022; 77(3): 243. CrossRef - Effects of Anthocyanin-rich Berries on the Risk of Metabolic Syndrome: A Systematic Review and Meta-analysis
Mikkel Roulund Wilken, Max Norman Tandrup Lambert, Christine Bodelund Christensen, Per Bendix Jeppesen
Review of Diabetic Studies.2022; 18(1): 42. CrossRef - Rate and risk factors of metabolic components and component combinations according to hypertension status in Tibetans in a cross-sectional study
Jihong Hu, Brian Thompson, Shuxia Wang, Minhao Guo, Chunjuan Yan, Fengfeng Ding, Peng Guo, Li Chen, Zhuoma Cao, Jianzong Wang
Medicine.2022; 101(43): e31320. CrossRef - Gender differences in changes in metabolic syndrome status and its components and risk of cardiovascular disease: a longitudinal cohort study
Azra Ramezankhani, Fereidoun Azizi, Farzad Hadaegh
Cardiovascular Diabetology.2022;[Epub] CrossRef - The Association of Metabolic Syndrome with the development of cardiovascular disease among Kazakhs in remote rural areas of Xinjiang, China: a cohort study
Wenwen Yang, Shuxia Guo, Haixia Wang, Yu Li, Xianghui Zhang, Yunhua Hu, Heng Guo, Kui Wang, Yizhong Yan, Jingyu Zhang, Jiaolong Ma, Lei Mao, Lati Mu, Jiaming Liu, Yanpeng Song, Changjing Li, Zhuo Ma, Rulin Ma, Jia He
BMC Public Health.2021;[Epub] CrossRef - Serum Arylsulfatase and Acid Phosphatase Activity in Patients with Metabolic Syndrome as a Result of Oxidative Damage to Lysosomes
Dorota M. Olszewska-Słonina
Protein & Peptide Letters.2021; 28(11): 1246. CrossRef - Validation of Risk Prediction Models for Atherosclerotic Cardiovascular Disease in a Prospective Korean Community-Based Cohort
Jae Hyun Bae, Min Kyong Moon, Sohee Oh, Bo Kyung Koo, Nam Han Cho, Moon-Kyu Lee
Diabetes & Metabolism Journal.2020; 44(3): 458. CrossRef - The Prevalence of Obesity and Metabolic Syndrome in the Korean Military Compared with the General Population
Jung Hwan Lee, Da Hea Seo, Min Jung Nam, Geon Hui Lee, Dong Hee Yang, Min Joo Lee, Ung-Rim Choi, Seongbin Hong
Journal of Korean Medical Science.2018;[Epub] CrossRef - Relationship between serum bilirubin levels and cardiovascular disease
Sunghwan Suh, Young Rak Cho, Mi Kyoung Park, Duk Kyu Kim, Nam H. Cho, Moon-Kyu Lee, Christian Herder
PLOS ONE.2018; 13(2): e0193041. CrossRef - Comparison Between Metabolic Syndrome and the Framingham Risk Score as Predictors of Cardiovascular Diseases Among Kazakhs in Xinjiang
Wenwen Yang, Rulin Ma, Xianghui Zhang, Heng Guo, Jia He, Lei Mao, Lati Mu, Yunhua Hu, Yizhong Yan, Jiaming Liu, Jiaolong Ma, Shugang Li, Yusong Ding, Mei Zhang, Jingyu Zhang, Shuxia Guo
Scientific Reports.2018;[Epub] CrossRef - Impact of interactions among metabolic syndrome components on the development of cardiovascular disease among Kazakhs in Xinjiang
Wenwen Yang, Xiang Gao, Xianghui Zhang, Yunhua Hu, Heng Guo, Kui Wang, Yizhong Yan, Jia He, Jingyu Zhang, Jiaolong Ma, Lei Mao, Lati Mu, Jiaming Liu, Shugang Li, Yusong Ding, Mei Zhang, Rulin Ma, Shuxia Guo, Mahesh Narayan
PLOS ONE.2018; 13(10): e0205703. CrossRef - Prediction of cardiovascular disease in Korean population: based on health risk appraisal of national health screening program
Jae Moon Yun, Tae Gon Yoo, Seung-Won Oh, Be Long Cho, Eunyoung Kim, Insob Hwang
Journal of the Korean Medical Association.2017; 60(9): 746. CrossRef - Metabolic Syndrome Is a Strong Risk Factor for Minor Ischemic Stroke and Subsequent Vascular Events
Guang-Sheng Wang, Dao-Ming Tong, Xiao-Dong Chen, Tong-Hui Yang, Ye-Ting Zhou, Xiao-Bo Ma, Gianpaolo Reboldi
PLOS ONE.2016; 11(8): e0156243. CrossRef - Metabolic syndrome related to cardiovascular events in a 10-year prospective study
Laura Kazlauskienė, Jūratė Butnorienė, Antanas Norkus
Diabetology & Metabolic Syndrome.2015;[Epub] CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Impact of Cadmium Exposure on the Association between Lipopolysaccharide and Metabolic Syndrome
Seung Han, Kyoung Ha, Ja Jeon, Hae Kim, Kwan Lee, Dae Kim
International Journal of Environmental Research and Public Health.2015; 12(9): 11396. CrossRef - Heat Killed Lactobacillus reuteri GMNL-263 Reduces Fibrosis Effects on the Liver and Heart in High Fat Diet-Hamsters via TGF-β Suppression
Wei-Jen Ting, Wei-Wen Kuo, Dennis Hsieh, Yu-Lan Yeh, Cecilia-Hsuan Day, Ya-Hui Chen, Ray-Jade Chen, Viswanadha Padma, Yi-Hsing Chen, Chih-Yang Huang
International Journal of Molecular Sciences.2015; 16(10): 25881. CrossRef

 KES
KES
 PubReader
PubReader Cite
Cite

