Articles
- Page Path
- HOME > Endocrinol Metab > Volume 37(2); 2022 > Article
-
Original ArticleThyroid Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
 Keypoint
Keypoint
Microvascular ultrasonography (MVUS) is a third-generation Doppler technique developed to increase sensitivity compared to conventional Doppler. The purpose of this study was to compare MVUS with conventional color Doppler (CD) and power Doppler (PD) imaging to distinguish Graves’ disease from destructive thyroiditis. MVUS showed non-inferiority in diagnostic accuracy compared to conventional CD or PD images, with less inter-observer variability. -
Han-Sang Baek1
 , Ji-Yeon Park1, Chai-Ho Jeong2, Jeonghoon Ha1, Moo Il Kang1, Dong-Jun Lim1
, Ji-Yeon Park1, Chai-Ho Jeong2, Jeonghoon Ha1, Moo Il Kang1, Dong-Jun Lim1
-
Endocrinology and Metabolism 2022;37(2):323-332.
DOI: https://doi.org/10.3803/EnM.2022.1413
Published online: April 13, 2022
1Division of Endocrinology and Metabolism, Department of Internal Medicine Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
2Division of Endocrinology and Metabolism, Department of Internal Medicine, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- Corresponding author: Dong-Jun Lim. Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-gu, Seoul 06591, Korea Tel: +82-2-2258-6009, Fax: +82-2-599-3589, E-mail: ldj6026@catholic.ac.kr
Copyright © 2022 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Microvascular ultrasonography (MVUS) is a third-generation Doppler technique that was developed to increase sensitivity compared to conventional Doppler. The purpose of this study was to compare MVUS with conventional color Doppler (CD) and power Doppler (PD) imaging to distinguish Graves’ disease (GD) from destructive thyroiditis (DT).
-
Methods
- This prospective study included 101 subjects (46 GDs, 47 DTs, and eight normal controls) from October 2020 to November 2021. All ultrasonography examinations were performed using microvascular flow technology (MV-Flow). The CD, PD, and MVUS images were semi-quantitatively graded according to blood flow patterns. On the MVUS images, vascularity indices (VIs), which were the ratio (%) of color pixels in the total grayscale pixels in a defined region of interest, were obtained automatically. Receiver operating characteristic curve analysis was performed to verify the diagnostic performance of MVUS. The interclass correlation coefficient and Cohen’s kappa analysis were used to analyze the reliability of MVUS (ClinicalTrials.gov:NCT04879173).
-
Results
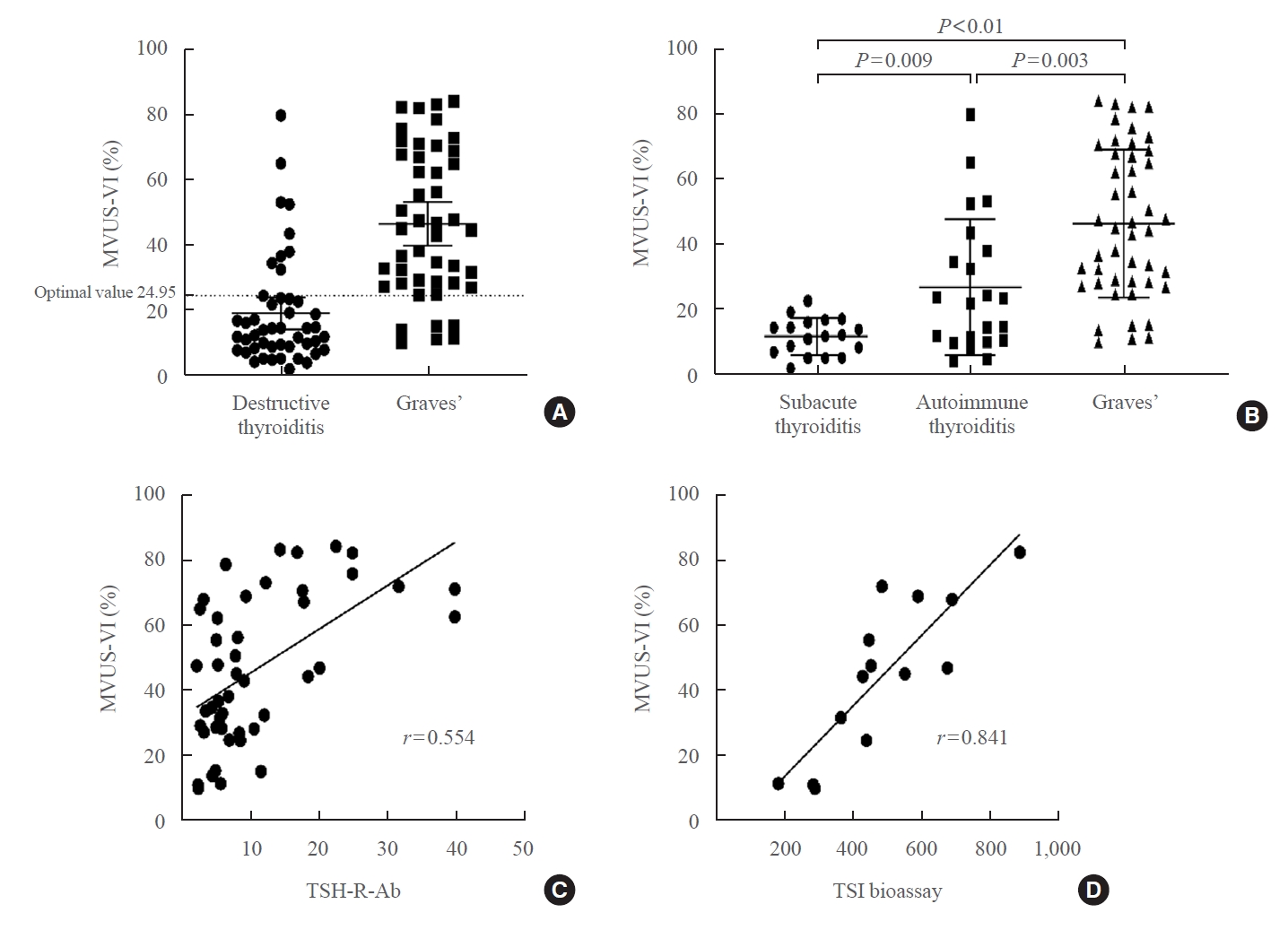
- The area under the curve (AUC) for CD, PD, MVUS, and MVUS-VI was 0.822, 0.844, 0.808, and 0.852 respectively. The optimal cutoff value of the MVUS-VI was 24.95% for distinguishing GD and DT with 87% sensitivity and 80.9% specificity. We found a significant positive correlation of MVUS-VI with thyrotropin receptor antibody (r=0.554) and with thyroid stimulating immunoglobulin bioassay (r=0.841). MVUS showed high intra- and inter-observer reliability from various statistical method.
-
Conclusion
- In a real time and quantitative manner, MVUS-VI could be helpful to differentiate GD from thyroiditis in thyrotoxic patients, with less inter-observer variability.
- Thyrotoxicosis is a condition in which various clinical symptoms and signs occur due to an excess of thyroid hormone. Thyrotoxicosis can occur with hyperthyroidism and the major cause is Graves’ disease (GD). Destructive thyroiditis (DT), in contrast, is typically one of the causes of thyrotoxicosis without hyperthyroidism, referring to any disease conditions induced by inflammation of the thyroid tissue.
- Precise discrimination between GD and DT is clinically very important in determining treatment methods. For the treatment of GD, thioamide anti-thyroid drugs (ATDs) have been commonly used [1,2]. The use of ATDs is contraindicated in DT because of the fear of inducing hypothyroidism. However, it seems to be difficult to effectively differentiate GD from DT within a short time of clinical practice.
- Serum thyrotropin receptor antibody (TSH-R-Ab) and thyroid scans have been used for the differential diagnosis of GD from DT in a conventional manner. Measuring serum TSH-R-Ab shows high sensitivity and specificity, but the results take several days, especially at primary physician clinics. And thyroid scans can only be performed in a small number of equipped hospitals and cannot be used for pregnant women.
- For the differential diagnosis of thyrotoxic patients, thyroid ultrasound (US) has been infrequently used as a noninvasive and rapid clinical tool [3]. Considering the potential real-time diagnostic ability of US, one may make the decision to use ATD before getting the serum TSH-R-Ab results. Although previous studies showed that thyroid US using color Doppler (CD) or power Doppler (PD) [1] have potential ability to differentiate the GD from other thyroiditis, major difficulty in objectively quantifying the results [4-6] were inevitable problems to be solved.
- Microvascular ultrasonography (MVUS) is a third-generation Doppler technique, which was developed to increase sensitivity compared to conventional Doppler. MVUS uses an advanced filter with spatiotemporal coherence information that can differentiate tissue artifacts from low-velocity blood flow. In contrast, conventional CD uses a conventional clutter filter, so true low-velocity blood flow can be eliminated because of overlapping frequency with low-frequency components resulting from patients’ motion, pulsation, and respiration [7]. MVUS has been tested for the differential diagnosis of many diseases in various organs [8-10]. However, to date, in thyroid disease, MVUS has been evaluated for its ability to distinguish malignant thyroid nodules from benign ones and has been limitedly used for the differential diagnosis of thyrotoxic patients [11-13].
- In this study, we tried to differentiate GD and DT among thyrotoxic patients using MVUS.
INTRODUCTION
- Study subjects
- We prospectively enrolled patients who visited our clinic between October 2020 and November 2021 (https://clinicaltrials.gov/ct2/show/NCT04879173). This study was approved by the Institutional Review Board of the Seoul St. Mary’s Hospital (Seoul, Korea) (KC19DCSI0744), and written informed consent was received from all patients. The thyrotoxic status of the enrolled subjects was confirmed with biochemical laboratory data of increased free thyroxine (fT4) above the reference range and decreased thyrotropin (TSH) below the reference range. Patients who are taking ATD within 3 months before ultrasonography or who received any surgical procedure to their thyroid were excluded. The blood tests for each study subject included TSH, fT4, triiodothyronine (T3), anti-microsomal-antibody (thyroid peroxidase antibody [TPO-Ab]), thyroglobulin antibody (Tg-Ab), TSH-R-Ab, and thyroid stimulating immunoglobulin (TSI) bioassay, if clinically needed. The normal ranges were as follows: TSH (0.55 to 4.78 μIU/mL), fT4 (0.89 to 1.76 ng/mL), T3 (0.6 to 1.81 ng/mL), TPO-Ab (<60 U/mL), Tg-Ab (<60 U/mL), TSH-R-Ab (<1.75 IU/L), and TSI bioassay (<140%).
- GD was confirmed by TSH-R-Abs. The clinical history and thyroid scan results were also considered in the diagnosis of GD. Autoimmune thyroiditis was diagnosed by positive TPO-Ab or Tg-Ab levels and the unique US findings of Hashimoto’s thyroiditis [3,14]. The diagnosis of subacute thyroiditis was made based on painful goiter, systemic inflammatory signs (erythrocyte sedimentation rate and C-reactive protein), and irregular hypoechoic tender lesions on US [15]. Drug-induced thyroiditis or postpartum thyroiditis was diagnosed based on the patient’s clinical history. All patients were followed up at least 3 months to observe the clinical course.
- For the generally healthy group, we included volunteers who had no history of thyroid disease. They visited the hospital for a general health checkup and a euthyroid state was confirmed by normal TSH and free T4 levels. Blood pressure and heart rate were measured with an autonomic blood pressure meter after sufficient rest before the sonography exam.
- Ultrasound evaluation
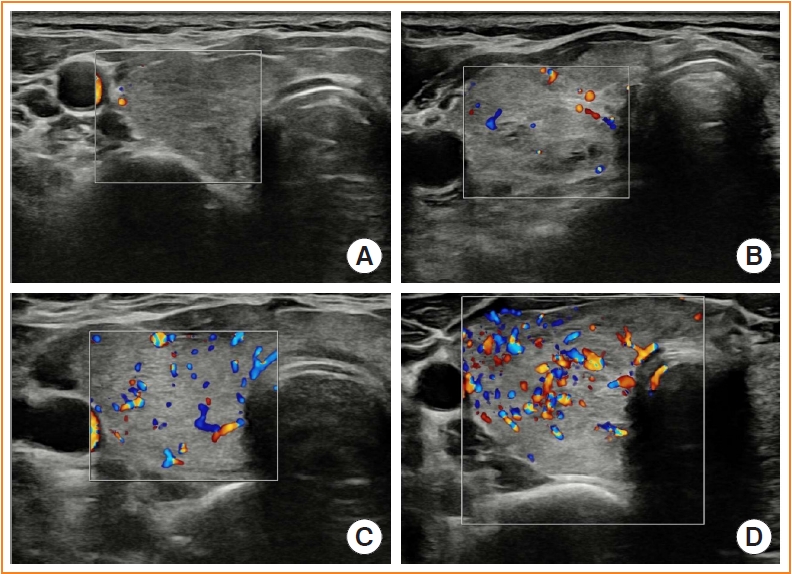
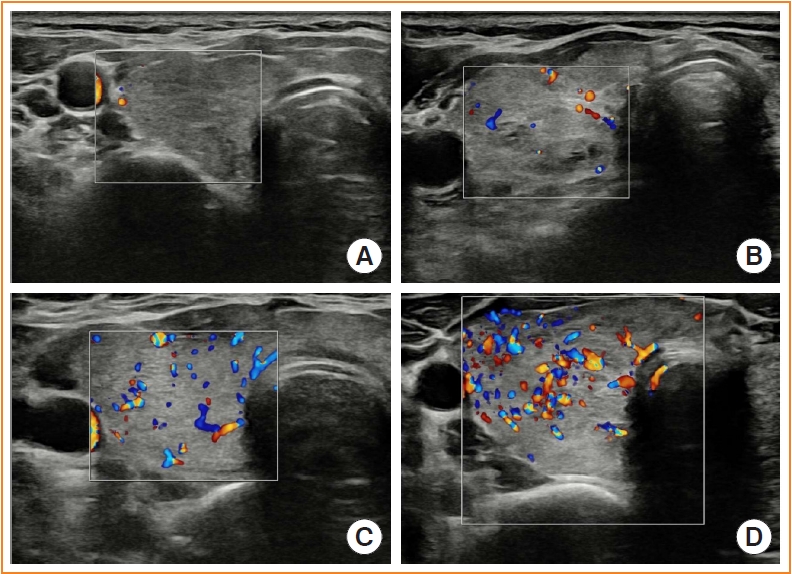
- All gray US, CD, PD, and MVUS were performed with an RS85 equipped with MV-Flow manufactured by Samsung Medison Co. Ltd. (Seoul, Korea). The volume of each lobe was measured on grayscale US as π/6×length×width×depth. Afterward, CD and PD images were obtained in the middle of the right and left thyroid in the transverse plane. We classified and scored those images into four groups according to the semi-quantitative (vascularity score) blood flow patterns suggested by a previous study [14,16-18]: pattern 0, blood flow limited to the peripheral thyroid arteries, while parenchymal flow is absent; pattern 1, the presence of mildly increased parenchymal flow; pattern 2, clearly increased blood flow with diffuse homogenous distribution; and pattern 3, markedly increased blood flow with a homogenous distribution, including the so-called “thyroid inferno” (Fig. 1). The vascularity score for CD and PD was obtained from the right and left lobe in all study subjects and final values for CD and PD indicated the mean values of them.
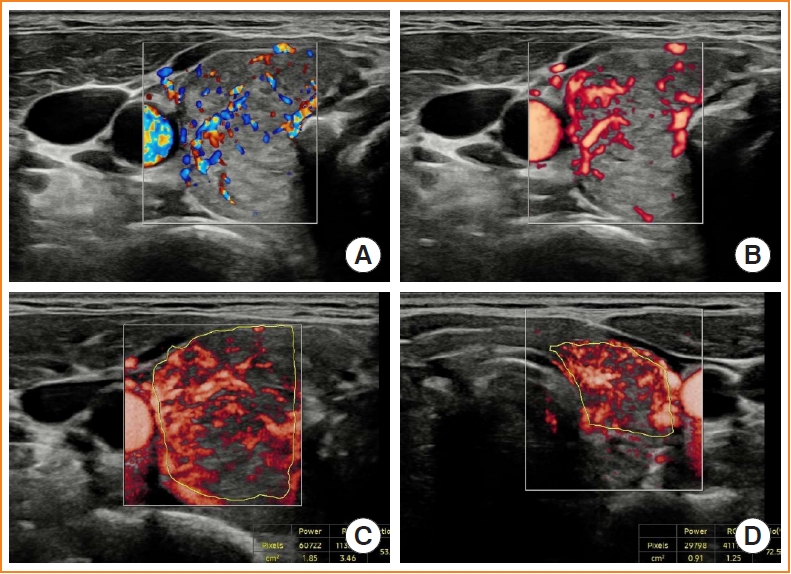
- MVUS was performed from the middle of each thyroid lobe in the transverse plane. Considering differences due to the cardiac cycle, the systolic cardiac phase in which the vascular codes were the brightest was caught in all cine images [19,20]. The vascularity index (VI) represents the percentage of color pixels in the total grayscale pixels in a defined region of interest (ROI). To identify the ROI, we traced the thyroid structure manually, excluding the peri-thyroidal vascular structures [19]. The VI automatically displays the number of pixels, area, and ratio (%) measurements within the ROI (Fig. 2). The VI was obtained twice from each lobe in all study subjects and finally MVUS-VI indicated the mean values of right and left VI. For the measurement of intra-observer variations, a second VI measurement was performed after completely removing the probe for at least 5 seconds and was made at almost the same plane as the first measurement. For the measurement of inter-observer variations, two observers performed VI measurements on the same patients sequentially (Fig. 3). Parameters for CD were Frequency; general, Gain 50, pulse-repetition frequency 0.21 kHz, and Power; 90. Parameters for PD or MVUS were same except pulse-repetition frequency (0.56 kHz for PD, 0.74 kHz for MVUS).
- Statistical analyses
- SPSS version 24 (IBM Co., Armonk, NY, USA) was used for almost statistical analyses. Receiver operating characteristic (ROC) curve analysis was performed to compare the diagnostic performance of MVUS for differentiating GD from DT. Through the ROC curve, the area under the curve (AUC), and optimal cutoff values for CD, PD, and VI were calculated and compared. The optimal cutoff value was defined as the number where the sum of sensitivity and 1-specificity was maximized. To compare each ROC curve to other ROC curve, we did non-inferiority test based on web-site based on R package (plotROC, pROC, rocNIT, R Project for Statistical Computing, Vienna, Austria) [21]. A P value of <0.05 was considered statistically significant.
- For intra and inter-observer variation analysis, we did two statistical methods; Interclass correlation coefficient (ICC) and Cohen’s kappa method. ICC was used to analyze the reliability of MVUS. Cohen’s kappa analysis was used to concordance of final diagnosis according to VI between intra- and inter-observer. The degree of correlation of two methods was expected based on previous study [22,23].
METHODS
- Baseline characteristics
- During the study period, 109 patients were screened and examined by the MVUS. Among them, eight were excluded because of inadequate medication status (n=5), previous isthmectomy surgery (n=1), and hyperfunctioning nodules (n=2) (Fig. 3). Therefore, MVUS was examined for 93 thyrotoxicosis patients and eight normal healthy volunteers. Finally, 46 GD (10 males, 36 females) and 47 DT (10 males, 37 females) patients were enrolled in this study. Among 47 DT patients, 18 with subacute thyroiditis, 22 with autoimmune thyroiditis, two with postpartum thyroiditis, and five with drug-induced thyroiditis were included.
- There were no significant differences in the age at diagnosis, gender distribution and body mass index between the GD and DT groups. However, the fT4, T3 and TSH-R-Ab levels were significantly higher in the GD patients. T3/fT4 was not different statistically between two groups (Table 1).
- The semi-quantitative CD, PD, and MVUS scores were all significantly higher in GD patients than in DT, indicating the hypervascular status of GD. The mean value of the right and left VI of the GD patients was higher than that of the DT patients (46.90%±22.65% vs. 19.46%±16.83%, P<0.001).
- Eight normal controls were included in the healthy group and there were no statistical differences in age (P=0.322) or sex (P=0.584) between the three groups. The mean age was 40.75±14.08 years, and three males and five females were included. The normal controls showed lower thyroid vascularity compared to the GD and DT groups (right 11.79%±6.40%, left 8.09%±7.72%, and mean 9.94%±6.11%; P<0.001).
- Diagnostic accuracy of MVUS through ROC curve analysis
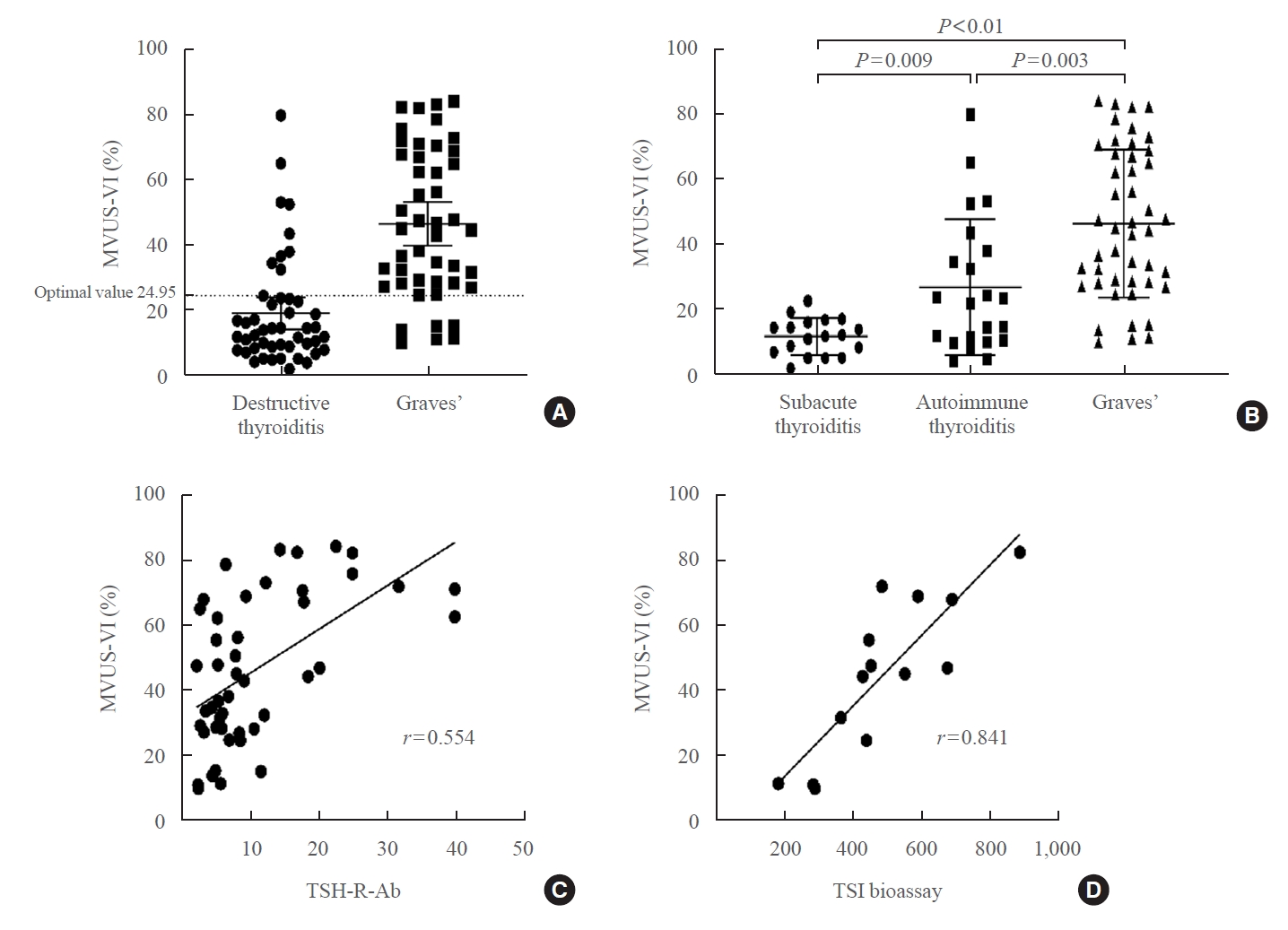
- The AUC for the mean of right and left CD, PD, MVUS, and MVUS-VI was 0.822, 0.844, 0.808, and 0.852 respectively. VIs of MVUS showed greater AUC values than the semi-quantitative MVUS scores. MVUS showed non-inferiority to CD (P=0.03) and PD (P=0.004). MVUS-VI also showed non-inferiority to CD (P=0.05) and PD (P=0.02). With an optimal cutoff VI of 24.95% for distinguishing GD and DT, the sensitivity and specificity of MVUS-VI were 87.0% and 80.9% respectively. The VI showed the highest negative predictive value (86.4%) compared to other Doppler tools (Table 2, Supplemental Fig. S1).
- Six GD patients were in the false negative range (low VI values with GD) and nine DT patients in the false positive range (high VI values without GD) according to the designated cutoff value (24.95%) obtained by AUC analysis (Fig. 4A). Among the patients who showed false-negative results, two were older than 68, and one received steroid treatment for a neurology problem. All patients who showed false-positive results were TPO or Tg antibody-positive. One patient received an immune checkpoint inhibitor for progressive cervical cancer.
- We further investigated the difference in the MVUS-VI between Graves’ patients, subacute thyroiditis patients, and autoimmune thyroiditis patients. The mean VI value in GD patients was 46.90±22.65 and the MVUS-VI among autoimmune thyroiditis and subacute thyroiditis patients was 27.34±20.87 and 12.14±5.64, respectively, indicating that GD patients showed the highest MVUS-VI, followed by autoimmune thyroiditis and subacute thyroiditis in that order (Fig. 4B).
- Correlation between the vascularity index of MVUS-VI and clinical parameters
- To determine whether the MVUS-VI was closely associated with other clinical parameters, a correlation analysis was performed only in GD patients. From the correlation coefficients, we found a positive correlation between the MVUS-VI and TSH-R-Ab (r=0.554) (Fig. 4C). Despite of small number (n=14), the MVUS-VI also showed the best positive correlation with TSI bioassay value (r=0.841) (Fig. 4D). The MVUS-VI also showed a positive correlation with fT4 and T3 levels. But it was rarely associated with the age at diagnosis, T3/fT4 or heart rate (Table 3).
- Intra- and inter-observer reliability of MVUS-VI
- Between the intra-observers or inter-observer, there were no significant differences in reliability as assessed by ICC (0.98 in intra-observer, 0.93 in inter-observer). The kappa value was 0.821 in the intra-observer and 0.883 in the inter-observer. It means the concordance of two operators would be almost perfect (Table 4) [23].
RESULTS
- MVUS showed non-inferiority in diagnostic accuracy compared to conventional CD or PD images. Especially, AUC values of the MVUS-VI (mean 0.852) were significantly larger than those of CD (mean 0.822) and PD (mean 0.844). In one previous study using CD for the diagnosis of GD, the diagnostic accuracy was 76.6% [24], which was similar to that of CD in our study.
- Although many previous studies showed that CD had successfully differentiated GD and thyroiditis in thyrotoxic patients, most of them used saved images, not real-time images [15,16,18-20]. And blood flow velocity measurement was used to diagnose GD, but it is a sophisticated technique especially for beginners to thyroid US [3]. Even though serum TSH-R-Ab measurements show high diagnostic accuracy, it takes several days to acquire the result in the real clinical field. Using MVUS, physicians could get clues for the diagnosis immediately after the physical examination, before getting the TSH-R-Ab or thyroid scan results.
- In addition, MVUS images can be numerically quantified. Many previous studies showed increased vascularization in Graves’ patients but they used vascularization scores subjectively scored by the operators [16-18]. To quantify thyroid vascularity, some investigators used the VI or similar concepts [4,15,20]. However, most studies used a computer program to calculate the VI on saved images, not in a real-time manner. The VI could be automatically obtained with MVUS in a real-time manner. From this process, the numerically quantified VI showed better diagnostic accuracy than even semi-quantitative MVUS. In addition, it could be helpful, especially, for the inexperienced operator of thyroid ultrasonography. When the blood flow within the thyroid is obviously increased due to severe GD, even inexperienced operators are able to make a proper diagnosis in a qualitative manner. However, if the thyroid vascularity is vaguely increased, inexperienced operators cannot reach a definite diagnosis by conventional methods such as CD or PD due to no cutoff values [3].
- To our knowledge, the optimal cutoff VI value to differentiate GD from thyroiditis has not been confirmed in previous study. In our study, through ROC curve analysis, an optimal value of 24.95% was determined for distinguishing GD and DT. The sensitivity was higher but the specificity was nearly the same or lower than that of conventional Doppler images because MVUS can detect even the smallest increase in vascular flow. This means that MVUS can sensitively capture these hypervascular states, accordingly, including autoimmune thyroiditis as a false positive.
- A few subjects showed high MVUS-VI scores close to the mean MVUS-VI score of the GD patients and the patients were finally found not to have GD, but autoimmune thyroiditis. This could be reason for the lower AUC and specificity of MVUS compared to that of CD or PD; MVUS detect the smallest vascular increase even in autoimmune thyroiditis. In a previous study with pediatric subjects, the MVUS-VI of GD patients was significantly higher than that of the autoimmune thyroiditis and healthy control groups [19]. Despite the fact that the study also included euthyroid GD patients under ATD treatment, considering the false positives in our study, there might be a gray zone with overlapping values between GD and autoimmune thyroiditis (Fig. 4B).
- Corona et al. [17] showed that interferon-γ-inducible chemokine levels were increased in autoimmune thyroid disease. The chemokine levels were highest in GD patients but were higher in autoimmune thyroiditis patients than in healthy controls [17]. Bogazzi et al. [18] showed an increase in intrathyroidal vascularity in patients with spontaneous hyperthyroidism but not in thyrotoxicosis due to DT. Although they all used semi-quantitative methods for thyroid vascularity scoring, thyroid vascularity might be associated with TSH or TSH-R-Ab levels. Accordingly, GD and autoimmune thyroiditis might induce a different pathway to increase thyroid vascularity.
- According to previous studies, once TSH receptors are stimulated by Graves’ immunoglobulin G, placenta growth factor (PIGF) and vascular endothelial growth factor (VEGF) are upregulated, leading to angiogenesis [25-27]. This association between TSH receptor stimulation and thyroid vascularity was also shown by using ultrasonography in various studies although the thyroid vascularization was scored by the semiquantitative method [15,16,20]. In our results, the MVUS-VI and TSH-R-Ab or TSI bioassay showed positive correlations with statistical significance. Based on our results, measuring the MVUS-VI could be helpful to predict antibody activity in realtime practice as Shih et al. [20] predicted that the VI could be measured directly in their study. In addition, because TSI bioassay is known to provide information about GD activity [28], VI could also be used to measure the disease activity. So, the usage of the MVUS-VI to predict the prognosis or activity of GD might be investigated in the future.
- The close correlation between the MVUS-VI and TSH-R-Ab has important clinical implication for managing false negative results in case that the VI was low despite of GD. Because TSH-R-Abs mirror severity of GD [29,30], low VI could imply the severity of the disease is relative low so the beginning of ATD is not so urgent.
- One essential point in the acquisition of US images is intra-and inter-observer issues. We measured the MVUS-VI at a time point when the colored area was the brightest. There might be differences according to when the operator captured the images. We measured the VI twice for each lobe in almost all study subjects. Two operators performed MVUS on the same patient sequentially in a limited number of subjects. From these intra- and inter-observer variability examinations, we confirmed MVUS reliably by high concordance rates. In addition, with kappa analysis, the diagnosis from two measurements was expected to almost same. However, there could be some disagreement of actual values between two measurements. For overcoming the aspect of agreement of MVUS, MVUS using VI should be computerized in the future for convenient data acquisition with minimum inter-observer variability [20].
- The present study had some limitations. First, we did not perform the quantitative analysis with the calculation of the VI on CD and PD. So, it is unclear whether a better performance of the MVUS is caused by the US technique per se or by addition of quantified VI. Second, we did not check the patients’ symptomatic severity, so it was impossible to identify a relationship between MVUS and symptom severity.
- In a real time and quantitative manner, MVUS-VI could be helpful to differentiate GD from thyroiditis in thyrotoxic patients. MVUS showed low intra- or inter-observer variability and the VI of MVUS showed a strong positive correlation with TSH-R-Ab, suggesting that MVUS could predict TSH-R-Ab levels in real practice.
DISCUSSION
Supplementary Information
Supplemental Fig. S1.
-
CONFLICTS OF INTEREST
This research was supported by research equipment from Samsung Medison Co., Ltd. (Seoul, Korea). The sponsor had no role in the writing of the manuscript or in the decision to submit the manuscript for publication.
-
AUTHOR CONTRIBUTIONS
Conception or design: H.S.B., C.H.J., D.J.L. Acquisition, analysis, or interpretation of data: H.S.B., J.Y.P., C.H.J., J.H., M.I.K., D.J.L. Drafting the work or revising: H.S.B., D.J.L. Final approval of the manuscript: H.S.B., J.Y.P., C.H.J., J.H., M.I.K., D.J.L.
Article information
-
Acknowledgements
- Parts of this work were presented as an abstract at the 90th Annual Meeting of the American Thyroid Association, September 30 to October 3, 2021, virtual event.

| Characteristic | GD (n=46) | DT (n=47) | P value |
|---|---|---|---|
| Age, yr | 47.54±16.61 | 48.74±12.81 | 0.697 |
| Sex, male/female | 10/36 | 10/37 | 1.000 |
| BMI, kg/m2 | 22.25±3.24 | 22.20±2.99 | 0.943 |
| TFT | |||
| fT4, ng/dL | 4.03±2.07 | 3.14±1.97 | 0.029 |
| T3, ng/mL | 3.79±1.74 | 2.70±1.29 | 0.001 |
| T3/fT4 | 1.09±0.31 | 1.14±0.35 | 0.502 |
| TSH, µIU/mL | 0.01±0.01 | 0.07±0.33 | 0.203 |
| TSH-R-Ab, IU/L | 10.90±9.39 | 0.92±0.33 | <0.001 |
| US finding | |||
| Volume, Rt., mL | 10.59±6.22 | 9.89±5.36 | 0.253 |
| Volume, Lt., mL | 8.16±5.05 | 7.37±4.28 | 0.203 |
| CD, Rt.a | 1.98±0.77 | 0.91±0.72 | <0.001 |
| CD, Lt.a | 1.72±0.75 | 0.85±0.78 | <0.001 |
| CD, mean | 1.85±0.72 | 0.88±0.71 | <0.001 |
| PD, Rt.a | 2.17±0.74 | 1.06±0.70 | <0.001 |
| PD, Lt.a | 1.98±0.75 | 1.02±0.79 | <0.001 |
| PD, mean | 2.08±0.71 | 1.04±0.70 | <0.001 |
| MVUS, Rt.a | 2.57±0.69 | 1.47±0.91 | <0.001 |
| MVUS, Lt.a | 2.48±0.69 | 1.55±0.85 | <0.001 |
| MVUS, mean | 2.52±0.67 | 1.51±0.86 | <0.001 |
| MVUS-VI Rt., % | 47.70±24.50 | 18.95±17.12 | <0.001 |
| MVUS-VI Lt., % | 46.10±22.73 | 19.97±17.76 | <0.001 |
| MVUS-VI mean, % | 46.90±22.65 | 19.46±16.83 | <0.001 |
Values are expressed as mean±standard deviation.
GD, Graves’ disease; DT, destructive thyroiditis; BMI, body mass index; TFT, thyroid function test; fT4, free thyroxine; T3, triiodothyronine; TSH, thyrotropin; TSH-R-Ab, thyrotropin receptor antibody; US, ultrasonography; Rt., right; Lt., left; CD, color Doppler; PD, power Doppler; MVUS, microvascular sonography; VI, vascularity index; Mean, the average of CD, PD, MVUS, and MVUS-VI of both thyroid lobes.
a Each Doppler image was classified and graded into four groups according to the blood flow pattern.
| Variable | Sensitivitya | Specificitya | PPVa | NPVa | AUC | 95% CI | P value for ROC curves power | P value for non-inferiority test |
|---|---|---|---|---|---|---|---|---|
| CDb | 71.7 | 80.9 | 78.6 | 74.5 | 0.822 | 0.737–0.907 | <0.001 | |
| PDb | 73.9 | 87.2 | 85.0 | 77.4 | 0.844 | 0.762–0.926 | <0.001 | |
| MVUSb | 67.4 | 85.1 | 81.6 | 72.7 | 0.808 | 0.718–0.898 | <0.001 | 0.03 (vs. CD) |
| 0.004 (vs. PD) | ||||||||
| MVUS-VIb, % | 87.0 | 80.9 | 81.6 | 86.4 | 0.852 | 0.774–0.930 | <0.001 | 0.05 (vs. CD) |
| 0.02 (vs. PD) |
CD, color Doppler; PD, power Doppler; MVUS, microvascular sonography; VI, vascularity index; PPV, positive predictive value; NPV, negative predictive value; AUC, area under the curve; CI, confidence interval; ROC, receiver operating characteristic.
a Value at the optimal cutoff value;
b Each values were driven from mean values of both thyroid lobe.
| Variable | TSH-R-Ab | TSI | fT4 | T3 | T3/T4 | TSHc | HR | Age | MVUS-VI |
|---|---|---|---|---|---|---|---|---|---|
| TSH-R-Ab | 1 | ||||||||
| TSI | 0.380 | 1 | |||||||
| fT4 | 0.330a | 0.300 | 1 | ||||||
| T3 | 0.389b | 0.504 | 0.841b | 1 | |||||
| T3/fT4 | –0.139 | –0.236 | 0.367a | –0.150 | 1 | ||||
| TSH | –0.049 | 0.333 | –0.079 | –0.094 | –0.069 | 1 | |||
| HR | –0.040 | 0.119 | 0.111 | 0.191 | –0.054 | –0.309 | 1 | ||
| Age | –0.023 | –0.509 | –0.119 | –0.157 | 0.069 | 0.188 | –0.273 | 1 | |
| MVUS-VI | 0.554b | 0.841b | 0.407b | 0.573b | –0.265 | 0.020 | 0.125 | –0.053 | 1 |
VI, vascular index; TSH-R-Ab, thyrotropin receptor antibody; TSI, thyroid stimulating immunoglobulin; fT4, free thyroxine; T3, triiodothyronine; TSH, thyrotropin; HR, heart rate; MVUS-VI, mean microvascular ultrasonography vascularity index of both thyroid lobes.
a P<0.05;
b P<0.01;
c Log TSH values.
| Statistical method | Intra-observer (n=67) | Inter-observer (n=19) | Interpretation |
|---|---|---|---|
| ICC | 0.98 | 0.93 | Excellent |
| Cohens’ kappa | 0.821 | 0.883 | Almost perfect |
- 1. Kahaly GJ. Management of Graves thyroidal and extrathyroidal disease: an update. J Clin Endocrinol Metab 2020;105:3704–20.ArticlePubMedPMC
- 2. Chung JH. Antithyroid drug treatment in Graves’ disease. Endocrinol Metab (Seoul) 2021;36:491–9.ArticlePubMedPMC
- 3. Alzahrani AS, Ceresini G, Aldasouqi SA. Role of ultrasonography in the differential diagnosis of thyrotoxicosis: a noninvasive, cost-effective, and widely available but underutilized diagnostic tool. Endocr Pract 2012;18:567–78.ArticlePubMed
- 4. Hiromatsu Y, Ishibashi M, Miyake I, Soyejima E, Yamashita K, Koike N, et al. Color Doppler ultrasonography in patients with subacute thyroiditis. Thyroid 1999;9:1189–93.ArticlePubMed
- 5. Donkol RH, Nada AM, Boughattas S. Role of color Doppler in differentiation of Graves’ disease and thyroiditis in thyrotoxicosis. World J Radiol 2013;5:178–83.ArticlePubMedPMC
- 6. Rosario PW, Santos JB, Nunes NS, da Silva AL, Calsolari MR. Color flow Doppler sonography for the etiologic diagnosis of thyrotoxicosis. Horm Metab Res 2014;46:505–9.ArticlePubMed
- 7. Yoo J, Je BK, Choo JY. Ultrasonographic demonstration of the tissue microvasculature in children: microvascular ultrasonography versus conventional color Doppler ultrasonography. Korean J Radiol 2020;21:146–58.ArticlePubMed
- 8. Xiao XY, Chen X, Guan XF, Wu H, Qin W, Luo BM. Superb microvascular imaging in diagnosis of breast lesions: a comparative study with contrast-enhanced ultrasonographic microvascular imaging. Br J Radiol 2016;89:20160546.ArticlePubMedPMC
- 9. Dubinsky TJ, Revels J, Wang S, Toia G, Sonneborn R, Hippe DS, et al. Comparison of superb microvascular imaging with color flow and power Doppler imaging of small hepatocellular carcinomas. J Ultrasound Med 2018;37:2915–24.ArticlePubMed
- 10. Durmaz MS, Sivri M. Comparison of superb micro-vascular imaging (SMI) and conventional Doppler imaging techniques for evaluating testicular blood flow. J Med Ultrason (2001) 2018;45:443–52.ArticlePubMed
- 11. Ahn HS, Lee JB, Seo M, Park SH, Choi BI. Distinguishing benign from malignant thyroid nodules using thyroid ultrasonography: utility of adding superb microvascular imaging and elastography. Radiol Med 2018;123:260–70.ArticlePubMed
- 12. Zhu YC, Zhang Y, Deng SH, Jiang Q. A prospective study to compare superb microvascular imaging with grayscale ultrasound and color Doppler flow imaging of vascular distribution and morphology in thyroid nodules. Med Sci Monit 2018;24:9223–31.ArticlePubMedPMC
- 13. Cappelli C, Pirola I, Gandossi E, Marini F, Cristiano A, Casella C, et al. Ultrasound microvascular blood flow evaluation: a new tool for the management of thyroid nodule? Int J Endocrinol 2019;2019:7874890.ArticlePubMedPMC
- 14. Sarikaya B, Demirbilek H, Akata D, Kandemir N. The role of the resistive index in Hashimoto’s thyroiditis: a sonographic pilot study in children. Clinics (Sao Paulo) 2012;67:1253–7.ArticlePubMedPMC
- 15. Ota H, Amino N, Morita S, Kobayashi K, Kubota S, Fukata S, et al. Quantitative measurement of thyroid blood flow for differentiation of painless thyroiditis from Graves’ disease. Clin Endocrinol (Oxf) 2007;67:41–5.ArticlePubMed
- 16. Vita R, Di Bari F, Perelli S, Capodicasa G, Benvenga S. Thyroid vascularization is an important ultrasonographic parameter in untreated Graves’ disease patients. J Clin Transl Endocrinol 2019;15:65–9.ArticlePubMedPMC
- 17. Corona G, Biagini C, Rotondi M, Bonamano A, Cremonini N, Petrone L, et al. Correlation between, clinical, biochemical, color Doppler ultrasound thyroid parameters, and CXCL-10 in autoimmune thyroid diseases. Endocr J 2008;55:345–50.ArticlePubMed
- 18. Bogazzi F, Bartalena L, Brogioni S, Burelli A, Manetti L, Tanda ML, et al. Thyroid vascularity and blood flow are not dependent on serum thyroid hormone levels: studies in vivo by color flow doppler sonography. Eur J Endocrinol 1999;140:452–6.ArticlePubMed
- 19. Bayramoglu Z, Kandemirli SG, Akyol Sari ZN, Kardelen AD, Poyrazoglu S, Bas F, et al. Superb microvascular imaging in the evaluation of pediatric Graves disease and Hashimoto thyroiditis. J Ultrasound Med 2020;39:901–9.ArticlePubMed
- 20. Shih SR, Chang JS, Lin LC, Chang YC, Li HY, Lee CY, et al. The relationship between thyrotropin receptor antibody levels and intrathyroid vascularity in patients with Graves’ disease. Exp Clin Endocrinol Diabetes 2013;121:1–5.ArticlePubMed
- 21. Kim J. ROC curves and sample size and inferiority [Internet]. Statistics4everyone; 2021 [cited 2022 Mar 25]. Available from: https://data-play3.shinyapps.io/ROC_pretty/.
- 22. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155–63.ArticlePubMedPMC
- 23. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74.ArticlePubMed
- 24. Scappaticcio L, Trimboli P, Keller F, Imperiali M, Piccardo A, Giovanella L. Diagnostic testing for Graves’ or non-Graves’ hyperthyroidism: a comparison of two thyrotropin receptor antibody immunoassays with thyroid scintigraphy and ultrasonography. Clin Endocrinol (Oxf) 2020;92:169–78.ArticlePubMed
- 25. Viglietto G, Romano A, Manzo G, Chiappetta G, Paoletti I, Califano D, et al. Upregulation of the angiogenic factors PlGF, VEGF and their receptors (Flt-1, Flk-1/KDR) by TSH in cultured thyrocytes and in the thyroid gland of thiouracilfed rats suggest a TSH-dependent paracrine mechanism for goiter hypervascularization. Oncogene 1997;15:2687–98.ArticlePubMed
- 26. Sato K, Yamazaki K, Shizume K, Kanaji Y, Obara T, Ohsumi K, et al. Stimulation by thyroid-stimulating hormone and Grave’s immunoglobulin G of vascular endothelial growth factor mRNA expression in human thyroid follicles in vitro and flt mRNA expression in the rat thyroid in vivo. J Clin Invest 1995;96:1295–302.ArticlePubMedPMC
- 27. Sato K. Vascular endothelial growth factors and thyroid disorders. Endocr J 2001;48:635–46.ArticlePubMed
- 28. Lytton SD, Kahaly GJ. Bioassays for TSH-receptor autoantibodies: an update. Autoimmun Rev 2010;10:116–22.ArticlePubMed
- 29. Kahaly GJ, Diana T, Kanitz M, Frommer L, Olivo PD. Prospective trial of functional thyrotropin receptor antibodies in Graves disease. J Clin Endocrinol Metab 2020;105:e1006–14.ArticlePubMed
- 30. Choi YM, Kwak MK, Hong SM, Hong EG. Changes in thyroid peroxidase and thyroglobulin antibodies might be associated with Graves’ disease relapse after antithyroid drug therapy. Endocrinol Metab (Seoul) 2019;34:268–74.ArticlePubMedPMC
References
Figure & Data
References
Citations

- Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management
Jin Wang, Ke Wan, Xin Chang, Rui-Feng Mao
World Journal of Diabetes.2024; 15(3): 348. CrossRef - The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Duplex Hemodynamic Parameters of Both Superior and Inferior Thyroid Arteries in Evaluation of Thyroid Hyperfunction Disorders
Maha Assem Hussein, Alaa Abdel Hamid, Rasha M Abdel Samie, Elshaymaa Hussein, Shereen Sadik Elsawy
International Journal of General Medicine.2022; Volume 15: 7131. CrossRef - Case 5: A 41-Year-Old Woman With Palpitation
Jiwon Yang, Kabsoo Shin, Jeongmin Lee, Jeonghoon Ha, Dong-Jun Lim, Han-Sang Baek
Journal of Korean Medical Science.2022;[Epub] CrossRef - Microvascular assessment of fascio-cutaneous flaps by ultrasound: A large animal study
Guillaume Goudot, Yanis Berkane, Eloi de Clermont-Tonnerre, Claire Guinier, Irina Filz von Reiterdank, Antonia van Kampen, Korkut Uygun, Curtis L. Cetrulo, Basak E. Uygun, Anahita Dua, Alexandre G. Lellouch
Frontiers in Physiology.2022;[Epub] CrossRef

 KES
KES
 PubReader
PubReader ePub Link
ePub Link Cite
Cite