Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
- Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
- Endocrinol Metab. 2023;38(6):679-689. Published online December 6, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1760
- 1,176 View
- 66 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
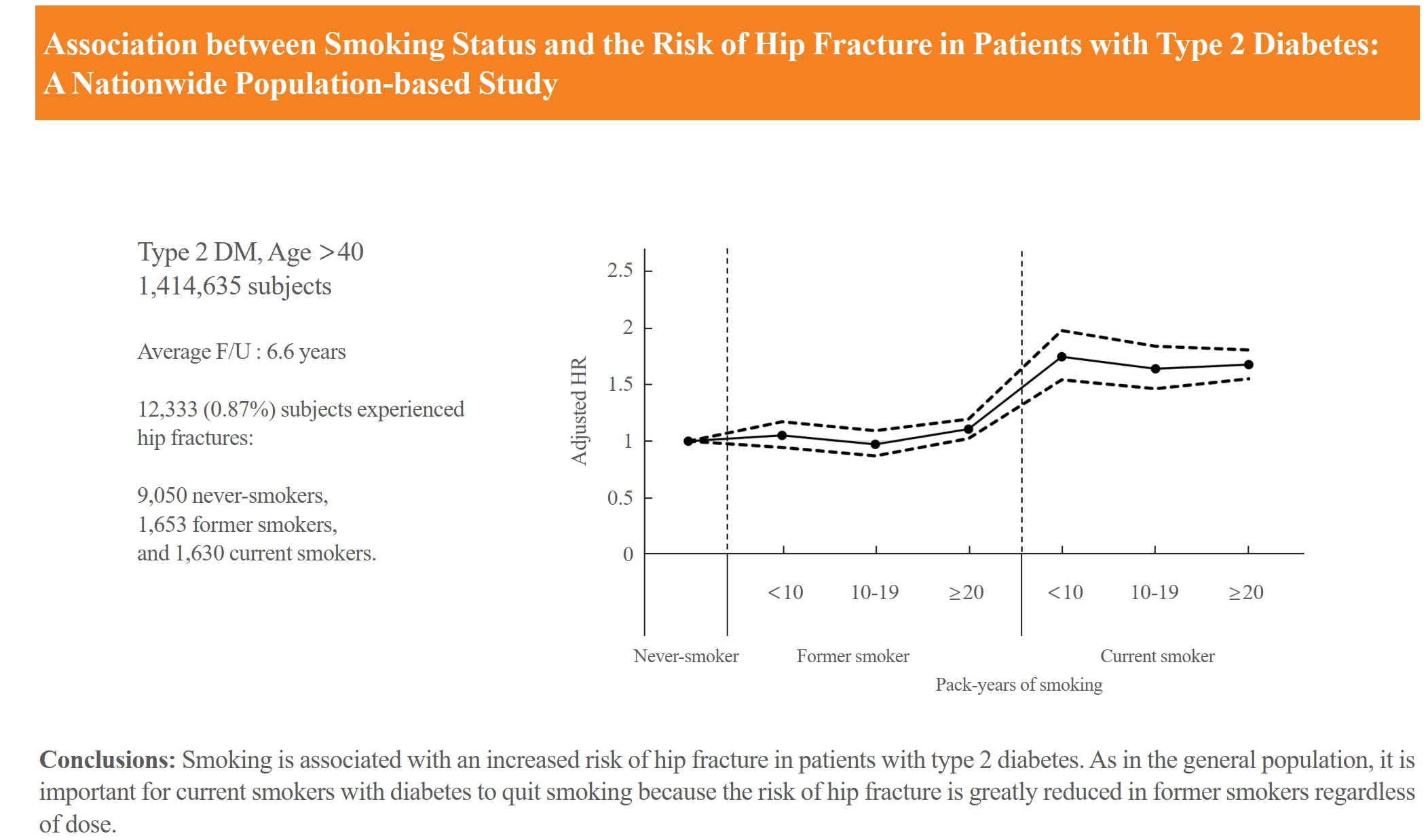
Limited longitudinal evidence exists regarding the potential association between smoking status and hip fracture among individuals with type 2 diabetes. We investigated this association using large-scale, nationwide cohort data for the Korean population.
Methods
This nationwide cohort study included 1,414,635 adults aged 40 and older who received Korean National Health Insurance Service health examinations between 2009 and 2012. Subjects with type 2 diabetes were categorized according to their smoking status, amount smoked (pack-years), number of cigarettes smoked per day, and duration of smoking. The results are presented as hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between smoking status parameters and risk of hip fracture in multivariable Cox proportional hazard regression analysis.
Results
Compared with never-smokers, an increased adjusted HR (aHR) for hip fracture was observed in current smokers (1.681; 95% CI, 1.578 to 1.791), and a comparable aHR for hip fracture was found in former smokers (1.065; 95% CI, 0.999 to 1.136). For former smokers who had smoked 20 pack-years or more, the risk was slightly higher than that for never-smokers (aHR, 1.107; 95% CI, 1.024 to 1.196). The hip fracture risk of female former smokers was similar to that of female current smokers, but the hip fracture risk in male former smokers was similar to that of male never-smokers.
Conclusion
Smoking is associated with an increased risk of hip fracture in patients with type 2 diabetes. Current smokers with diabetes should be encouraged to quit smoking because the risk of hip fracture is greatly reduced in former smokers.

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Association among Current Smoking, Alcohol Consumption, Regular Exercise, and Lower Extremity Amputation in Patients with Diabetic Foot: Nationwide Population-Based Study
- Yoon Jae Lee, Kyung-Do Han, Jun Hyeok Kim
- Endocrinol Metab. 2022;37(5):770-780. Published online October 12, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1519
- 3,272 View
- 202 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
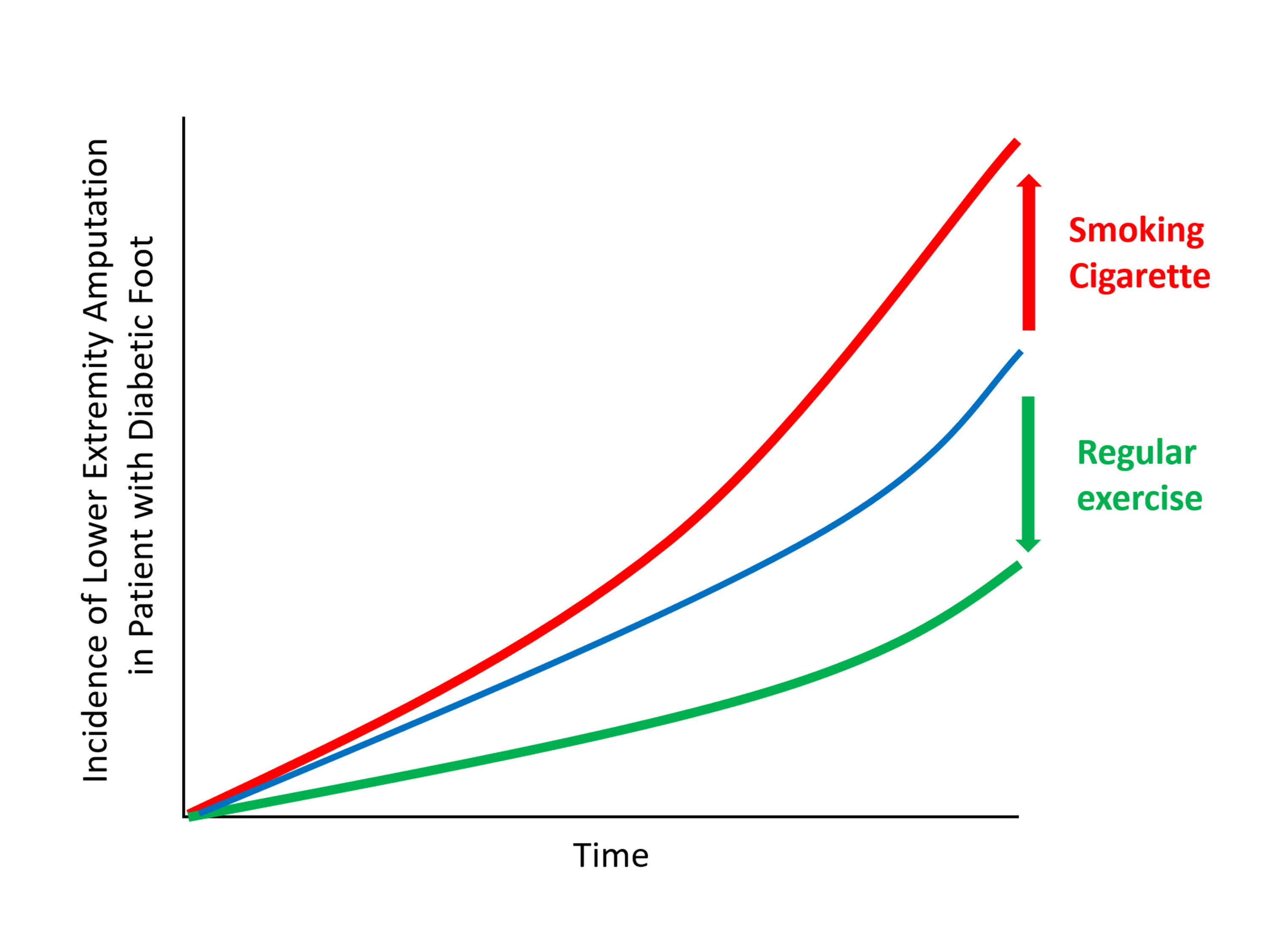
The present study investigates whether modifiable behavioral factors of current cigarette smoking, heavy alcohol consumption, and regular exercise are associated with risk of lower extremity amputation (LEA) in diabetic patients.
Methods
A total of 2,644,440 diabetic patients (aged ≥20 years) was analyzed using the database of the Korean National Health Insurance Service. Cox proportional hazard regression was used to assess adjusted hazard ratios (HRs) for the behavioral factors with risk of LEA under adjustment for potential confounders.
Results
The risk of LEA was significantly increased by current cigarette smoking and heavy alcohol consumption (HR, 1.436; 95% confidence interval [CI], 1.367 to 1.508 and HR, 1.082; 95% CI, 1.011 to 1.158) but significantly decreased with regular exercise (HR, 0.745; 95% CI, 0.706 to 0.786) after adjusting for age, sex, smoking, alcohol consumption, exercise, low income, hypertension, dyslipidemia, body mass index, using insulin or oral antidiabetic drugs, and diabetic duration. A synergistically increased risk of LEA was observed with larger number of risky behaviors.
Conclusion
Modification of behaviors of current smoking, heavy alcohol intake, and exercise prevents LEA and can improve physical, emotional, and social quality of life in diabetic patients. -
Citations
Citations to this article as recorded by- Adjuvant effect of antimicrobial photodynamic therapy (aPDT) in the treatment of diabetic foot ulcers: A case series
Rita de Cassia Ferreira, Rebeca Boltes Cecatto, Silvana Torres Perez, Raquel Agnelli Mesquita‐Ferrari, Sandra Kalil Bussadori, Cinthya Cosme Duran, Anna Carolina Tempestini Horliana, Kristianne Porta Santos Fernandes
Journal of Biophotonics.2024;[Epub] CrossRef - Factors associated with diabetic foot ulcers and lower limb amputations in type 1 and type 2 diabetes supported by real‐world data from the German/Austrian DPV registry
Alexander J. Eckert, Stefan Zimny, Marcus Altmeier, Ana Dugic, Anton Gillessen, Latife Bozkurt, Gabriele Götz, Wolfram Karges, Frank J. Wosch, Stephan Kress, Reinhard W. Holl
Journal of Diabetes.2024;[Epub] CrossRef - Investigating Diabetic Foot Pathophysiology and Amputation Prevention Strategies through Behavioral Modification
Jun Hyeok Kim
Journal of Wound Management and Research.2023; 19(3): 167. CrossRef
- Adjuvant effect of antimicrobial photodynamic therapy (aPDT) in the treatment of diabetic foot ulcers: A case series

- Thyroid
- Effect of Cigarette Smoking on Thyroid Cancer: Meta-Analysis
- Joon-Hyop Lee, Young Jun Chai, Ka Hee Yi
- Endocrinol Metab. 2021;36(3):590-598. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.954
- 12,483 View
- 190 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
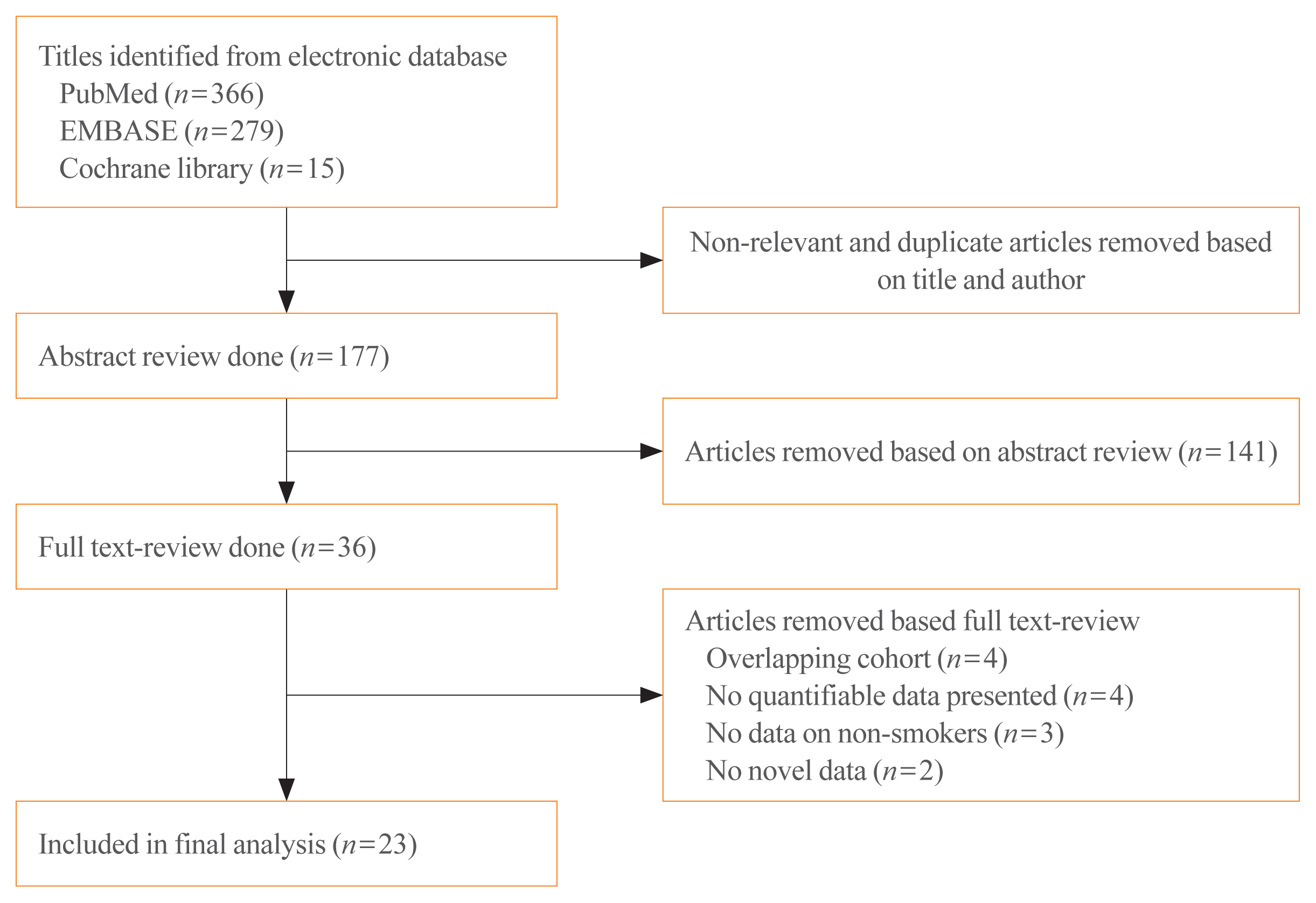
Although smoking is generally carcinogenic, its effect on thyroid cancers is still subject to controversy. The purpose of this study was to summarize the role of smoking in relation to thyroid cancer occurrence.
Methods
We performed a meta-analysis of 24 eligible studies: 21 case-control studies and three prospective cohort studies. The summary odds ratio (OR) and 95% confidence interval (CI) of all studies were acquired based on random effect model. Further subgroup analyses were conducted according to gender, histological type of thyroid cancer, and smoking status of patients for the case-control studies.
Results
The summary effect size indicated a negative association of smoking for thyroid cancer (OR, 0.798; 95% CI, 0.681 to 0.935). From the subgroup analyses for the case-control studies, reduced risk of thyroid cancer was observed in both men (OR, 0.734; 95% CI, 0.553 to 0.974) and women (OR, 0.792; 95% CI, 0.700 to 0.897). The protective effect of smoking was observed in studies in which thyroid cancer was limited to differentiated thyroid cancers (DTCs) (OR, 0.798; 95% CI, 0.706 to 0.902).
Conclusion
Our results suggests that smoking may have a protective effect on thyroid cancer, especially on DTCs. Further studies with larger sample sizes should be conducted in elucidating the dose and time dependent effect of smoking on thyroid cancer with specific focus on the types of thyroid cancers. -
Citations
Citations to this article as recorded by- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders
I. M. Belovalova, E. S. Shugurova, M. O. Korchagina, T. N. Borkhoeva, M. S. Sheremeta
Clinical and experimental thyroidology.2024; 19(2): 11. CrossRef - Relationship between Serum Levels of Selenium and Thyroid Cancer: A Systematic Review and Meta-Analysis
Runhua Hao, Ping Yu, Lanlan Gui, Niannian Wang, Da Pan, Shaokang Wang
Nutrition and Cancer.2023; 75(1): 14. CrossRef - Potentially inappropriate medication and frailty in older adults: A systematic review and meta-analysis
Wenlian Ma, Hongyan Wang, Zhifei Wen, Linfeng Liu, Xiangeng Zhang
Archives of Gerontology and Geriatrics.2023; 114: 105087. CrossRef - Inflammation biomarkers are associated with the incidence of cardiovascular disease: a meta-analysis
Yifei Liu, Suzhen Guan, Haiming Xu, Na Zhang, Min Huang, Zhihong Liu
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Maternal gestational weight gain and offspring’s neurodevelopmental outcomes: A systematic review and meta-analysis
Dan Wu, Yicheng Li, Lingyan Chen, Marieke Klein, Barbara Franke, Jinjin Chen, Jan Buitelaar
Neuroscience & Biobehavioral Reviews.2023; 153: 105360. CrossRef - Association of preoperative hypoprotein malnutrition with spinal postoperative complications and other conditions: A systematic review and meta-analysis
Yongrong Hu, Liping Wang, Hao Liu, Kunhai Yang, Song Wang, Xiang Zhang, Bo Qu, Hongsheng Yang
Clinical Nutrition ESPEN.2023; 57: 448. CrossRef - Metabolic syndrome and risk of ovarian cancer: a systematic review and meta-analysis
Ziyu Chen, Zesi Liu, Hongxia Yang, Chaosheng Liu, Fandou Kong
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cigarette smoking and thyroid cancer risk: A Mendelian randomization study
Hongzhan Jiang, Yi Li, Jiali Shen, Huihui Lin, Siyue Fan, Rongliang Qiu, Jiaxi He, Ende Lin, Lijuan Chen
Cancer Medicine.2023; 12(19): 19866. CrossRef - Longitudinal Changes in Smoking Habits in Women and Subsequent Risk of Cancer
Thi Xuan Mai Tran, Soyeoun Kim, Huiyeon Song, Boyoung Park
American Journal of Preventive Medicine.2022; 63(6): 894. CrossRef
- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders

- Clinical Study
- Gender-Dependent Reference Range of Serum Calcitonin Levels in Healthy Korean Adults
- Eyun Song, Min Ji Jeon, Hye Jin Yoo, Sung Jin Bae, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Hong-Kyu Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(2):365-373. Published online April 7, 2021
- DOI: https://doi.org/10.3803/EnM.2020.939

- 4,991 View
- 152 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Serum calcitonin measurement contains various clinical and methodological aspects. Its reference level is wide and unclear despite sensitive calcitonin kits are available. This study aimed to identify the specific reference range in the healthy Korean adults.
Methods
Subjects were ≥20 years with available calcitonin (measured by a two-site immunoradiometric assay) data by a routine health checkup. Three groups were defined as all eligible subjects (group 1, n=10,566); subjects without self or family history of thyroid disease (group 2, n=5,152); and subjects without chronic kidney disease, autoimmune thyroid disease, medication of proton pump inhibitor/H2 blocker/steroid, or other malignancies (group 3, n=4,638).
Results
This study included 6,341 male and 4,225 female subjects. Males had higher mean calcitonin than females (2.3 pg/mL vs. 1.9 pg/mL, P<0.001) in group 1. This gender difference remained similar in groups 2 and 3. Calcitonin according to age or body mass index was not significant in both genders. Higher calcitonin in smoking than nonsmoking men was observed but not in women. Sixty-nine subjects had calcitonin higher than the upper reference limit (10 pg/mL) and 64 of them had factors associated with hypercalcitoninemia besides medullary thyroid cancer. Our study suggests the reference intervals for men who were non, ex-, current smokers, and women (irrespective of smoking status) as <5.7, <7.1, <7.9, and <3.6 pg/mL, respectively.
Conclusion
Specific calcitonin reference range should be provided considering for sex and smoking status. Taking account for several factors known to induce hypercalcitoninemia can help interpret the gray zone of moderately elevated calcitonin. -
Citations
Citations to this article as recorded by- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma
Pierpaolo Trimboli, Giuseppe Peloni, Dorotea Confalonieri, Elena Gamarra, Tommaso Piticchio, Francesco Frasca, Petra Makovac, Arnoldo Piccardo, Lorenzo Ruinelli
Frontiers in Oncology.2024;[Epub] CrossRef - Surgical treatment of solid variant of papillary thyroid carcinoma: Fifteen-year experience of a tertiary center
Katarina Tausanović, Marina Stojanović, Milan Jovanović, Boban Stepanović, Jovan Ilić, Sara Ivaniš, Vladan Živaljević
Medicinska istrazivanja.2024; 57(1): 121. CrossRef - Some genetic differences in patients with rheumatoid arthritis
Hosam M. Ahmad, Zaki M. Zaki, Asmaa S. Mohamed, Amr E. Ahmed
BMC Research Notes.2023;[Epub] CrossRef - Presence or severity of Hashimoto’s thyroiditis does not influence basal calcitonin levels: observations from CROHT biobank
M. Cvek, A. Punda, M. Brekalo, M. Plosnić, A. Barić, D. Kaličanin, L. Brčić, M. Vuletić, I. Gunjača, V. Torlak Lovrić, V. Škrabić, V. Boraska Perica
Journal of Endocrinological Investigation.2022; 45(3): 597. CrossRef - Environmental Factors That Affect Parathyroid Hormone and Calcitonin Levels
Mirjana Babić Leko, Nikolina Pleić, Ivana Gunjača, Tatijana Zemunik
International Journal of Molecular Sciences.2021; 23(1): 44. CrossRef
- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma

- Clinical Study
- Association between Secondhand Smoke Exposure and Metabolic Syndrome in 118,609 Korean Never Smokers Verified by Self-Reported Questionnaire and Urine Cotinine
- Ji Hye Kim, Byung Jin Kim, Young Youl Hyun, Jin Ho Kang
- Endocrinol Metab. 2020;35(4):892-900. Published online December 23, 2020
- DOI: https://doi.org/10.3803/EnM.2020.847
- 4,252 View
- 100 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
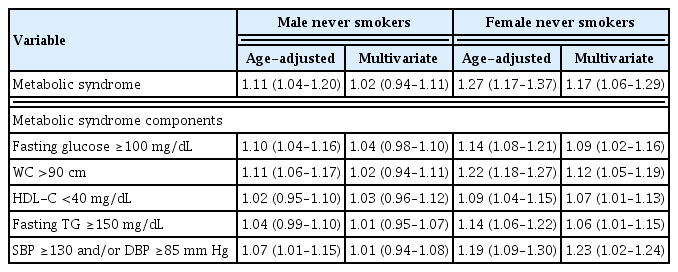
No study has reported the association between secondhand smoke (SHS) exposure and metabolic syndrome (MetS) in self-reported never smokers verified by both self-reported questionnaire and urine cotinine.
Methods
A total of 118,609 self-reported and cotinine-verified never smokers (38,385 male; age 34.8±7.1 years) who participated in the Kangbuk Samsung Health Study between 2011 and 2016 were included. Cotinine-verified never smokers were defined as individuals with urinary cotinine <50 ng/mL. SHS exposure was defined as current exposure to passive smoking indoors at home or workplace.
Results
Prevalence of SHS exposure in the overall population was 22.6% (27.4% for males and 20.3% for females (P<0.001). The overall prevalence of MetS was 6.8% and was higher in males than in females (10.7% vs. 4.9%, P<0.001). In both genders, MetS prevalence was higher in the SHS exposure group than the non-SHS exposure group (11.3% vs. 10.4%, P=0.010 for males; 5.8% vs. 4.6%, P<0.001 for females). However, there was significant gender interaction for the association between SHS exposure and MetS (P for interaction=0.010). In the multivariate regression analyses, SHS exposure was associated with increased MetS odds only in females (odds ratio [95% confidence interval], 1.02 [0.94 to 1.11] in male vs. 1.17 [1.06 to 1.29] in female). In particular, females with SHS exposure of ≥1 hour/day and ≥3 times showed increased odds of MetS compared with those without SHS exposure (1.22 [1.02 to 1.45], 1.30 [1.14 to 1.49]).
Conclusion
This cross-sectional study showed that SHS exposure was significantly associated with prevalence of MetS in self-reported and cotinine-verified female never smokers. -
Citations
Citations to this article as recorded by- Combined Influence of Eight Lifestyle Factors on Metabolic Syndrome Incidence: A Prospective Cohort Study from the MECH-HK Study
Yun-Yang Deng, Fei-Wan Ngai, Jing Qin, Lin Yang, Ka-Po Wong, Harry-Haoxiang Wang, Yao-Jie Xie
Nutrients.2024; 16(4): 547. CrossRef - Association of Zinc Intake, Tobacco Smoke Exposure, With Metabolic Syndrome: Evidence from NHANES 2007–2018
Shengxiang Yang, Qian Chen, Lin Wang
Biological Trace Element Research.2024;[Epub] CrossRef - The association between urinary cotinine level and metabolic syndrome profiles among adolescents: findings from the Ewha Birth and growth study
Hyunjin Park, Ui-Jeong Kim, Eun Jeong Choi, Seunghee Jun, Bomi Park, Hye Ah Lee, Hae Soon Kim, Hyesook Park
BMC Public Health.2023;[Epub] CrossRef - Association of environmental tobacco smoke exposure with metabolic syndrome: A longitudinal Cohort Study of 71,055 never smokers
Hyo-In Choi, Seung Jae Lee, Jeong Gyu Kang, Sung Ho Lee, Bum Soo Kim, Byung Jin Kim
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(11): 2534. CrossRef
- Combined Influence of Eight Lifestyle Factors on Metabolic Syndrome Incidence: A Prospective Cohort Study from the MECH-HK Study

- Thyroid
- Clinical Relevance of Environmental Factors in the Pathogenesis of Autoimmune Thyroid Disease
- Wilmar M. Wiersinga
- Endocrinol Metab. 2016;31(2):213-222. Published online May 13, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.213
- 9,083 View
- 210 Download
- 88 Web of Science
- 93 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Genetic factors contribute for about 70% to 80% and environmental factors for about 20% to 30% to the pathogenesis of autoimmune thyroid disease (AITD). Relatives of AITD patients carry a risk to contract AITD themselves. The 5-year risk can be quantified by the so-called Thyroid Events Amsterdam-score, based on serum thyroid-stimulating hormone, thyroid peroxidase (TPO)-antibodies and family history. Subjects at risk may ask what they can do to prevent development of AITD. This review summarizes what is known about modulation of exposure to environmental factors in terms of AITD prevention. To stop smoking decreases the risk on Graves disease but increases the risk on Hashimoto disease. Moderate alcohol intake provides some protection against both Graves and Hashimoto disease. Low selenium intake is associated with a higher prevalence of thyroid autoimmunity, but evidence that selenium supplementation may lower TPO antibodies and prevent subclinical hypothyroidism remains inconclusive. Low serum vitamin D levels are associated with a higher prevalence of TPO antibodies, but intervention studies with extra vitamin D have not been done yet. Stress may provoke Graves hyperthyroidism but not Hashimoto thyroiditis. Estrogen use have been linked to a lower prevalence of Graves disease. The postpartum period is associated with an increased risk of AITD. Taking together, preventive interventions to diminish the risk of AITD are few, not always feasible, and probably of limited efficacy.
-
Citations
Citations to this article as recorded by- Trends in Prevalence of Thyroid Dysfunction and its Associations With Mortality Among US Participants, 1988-2012
Xiaowen Zhang, Yong Wang, Hongwei Wang, Xinlin Zhang
The Journal of Clinical Endocrinology & Metabolism.2024; 109(2): e657. CrossRef - The role of medical and organizational measures in improving the quality of early detection and clinical examination of autoimmune thyroiditis among the population of the Republic of Belarus
L. I. Danilova, V. A. Rozhko, I. V. Veyalkin, S. N. Nikanovich, T. M. Sharshakova
Health and Ecology Issues.2024; 20(4): 129. CrossRef - Hyperthyroidism
Layal Chaker, David S Cooper, John P Walsh, Robin P Peeters
The Lancet.2024; 403(10428): 768. CrossRef - A Review of Thyroid Dysfunction Due to COVID-19
Alireza Arefzadeh
Mini-Reviews in Medicinal Chemistry.2024; 24(3): 265. CrossRef - Alteration in kynurenine pathway metabolites in young women with autoimmune thyroiditis
Anna Krupa, Agnieszka Łebkowska, Marcin Kondraciuk, Karol Adam Kaminski, Irina Kowalska
Scientific Reports.2024;[Epub] CrossRef - Association of autoimmune thyroid disease with type 1 diabetes mellitus and its ultrasonic diagnosis and management
Jin Wang, Ke Wan, Xin Chang, Rui-Feng Mao
World Journal of Diabetes.2024; 15(3): 348. CrossRef - Hashimoto’s thyroiditis and coexisting disorders in correlation with HLA status—an overview
Peter Mikosch, Adrian Aistleitner, Markus Oehrlein, Eva Trifina-Mikosch
Wiener Medizinische Wochenschrift.2023; 173(1-2): 41. CrossRef - The management and metabolic characterization: hyperthyroidism and hypothyroidism
Yangyang Wang, YanPing Sun, Bingyou Yang, Qiuhong Wang, Haixue Kuang
Neuropeptides.2023; 97: 102308. CrossRef - Zn and Se abrogate heavy metal mixture induced ovarian and thyroid oxido-inflammatory effects mediated by activation of NRF2-HMOX-1 in female albino rats
Boma F. Eddie-Amadi, Anthonet N. Ezejiofor, Chinna N. Orish, Orish E. Orisakwe
Current Research in Toxicology.2023; 4: 100098. CrossRef - Genetically predicted selenium concentrations and thyroid function: A two‐sample Mendelian randomization study
Hui‐Jun Huang, Shan‐Shan Wang, Ming‐Min Jin, Bin‐Wei Cheng, Yu Liu, Xiao‐Chen Liu, Qiu‐Yan Yu, Xin‐Jun Yang
Clinical Endocrinology.2023; 98(6): 813. CrossRef - Identification of Smoking-Associated Transcriptome Aberration in Blood with Machine Learning Methods
FeiMing Huang, QingLan Ma, JingXin Ren, JiaRui Li, Fen Wang, Tao Huang, Yu-Dong Cai, Bilal Alatas
BioMed Research International.2023; 2023: 1. CrossRef - COVID-induced thyroid autoimmunity
Alessandro Brancatella, Nicola Viola, Ferruccio Santini, Francesco Latrofa
Best Practice & Research Clinical Endocrinology & Metabolism.2023; 37(2): 101742. CrossRef - Associations between vitamin D levels and dietary patterns in patients with Hashimoto’s thyroiditis
Dean Kaličanin, Maja Cvek, Ana Barić, Veselin Škrabić, Ante Punda, Vesna Boraska Perica
Frontiers in Nutrition.2023;[Epub] CrossRef - COMPARATIVE MORPHOLOGY OF THE THYROID GLAND
L. O. Sviatotska
Bulletin of Problems Biology and Medicine.2023; 1(2): 386. CrossRef - Evaluation and epigenetic impact of B12, vitamin D, folic acid and anemia in Hashimoto's thyroiditis: a clinical and molecular docking study
Elif Sibel ASLAN, Savaş GÜR
Journal of Health Sciences and Medicine.2023; 6(4): 705. CrossRef - Interactions between Polygenetic Variants and Lifestyle Factors in Hypothyroidism: A Hospital-Based Cohort Study
Da Sol Kim, Sunmin Park
Nutrients.2023; 15(17): 3850. CrossRef - Do Dietary Supplements Affect Inflammation, Oxidative Stress, and Antioxidant Status in Adults with Hypothyroidism or Hashimoto’s Disease?—A Systematic Review of Controlled Trials
Katarzyna Kubiak, Maria Karolina Szmidt, Joanna Kaluza, Agnieszka Zylka, Ewa Sicinska
Antioxidants.2023; 12(10): 1798. CrossRef - Identification and Preliminary Clinical Validation of Key Extracellular Proteins as the Potential Biomarkers in Hashimoto’s Thyroiditis by Comprehensive Analysis
Zihan Xi, Tinglin Yang, Tao Huang, Jun Zhou, Peng Yang
Biomedicines.2023; 11(12): 3127. CrossRef - An examination of retinal findings with optical coherence tomography in hypothyroidism patients with vitamin D deficiency: A comparative study
Samet Sayılan, Dila Kırağı, Mehmet Tayfun Arslan
Journal of Clinical Medicine of Kazakhstan.2023; 20(6): 36. CrossRef - The role of IL-4 −590 (C>T) Gene as diagnostic biomarker of Hashimoto thyroiditis disease patients in AL-Najaf provenance /Iraq
Sarah Hasan Kadhum AL-Huchaimi, Mahdi Hussain AL-Ammar, Sabah N. AL-Fatlawi
Al-Kufa University Journal for Biology.2023; 15(3): 14. CrossRef - Early life stress in women with autoimmune thyroid disorders
Alessia Corso, Hermann Engel, Fabienne Müller, Serena Fiacco, Laura Mernone, Elena Gardini, Ulrike Ehlert, Susanne Fischer
Scientific Reports.2023;[Epub] CrossRef - Protective Effects of Selenium and Zinc Against Nickel Chloride–Induced Hormonal Changes and Oxidative Damage in Thyroid of Pregnant Rats
Imane Salah, Ounassa Adjroud, Awatef Elwej
Biological Trace Element Research.2022; 200(5): 2183. CrossRef - Effects of animal protein intake during pregnancy on autoimmune thyroiditis in pregnant women with mild iodine deficiency
Zhengyuan Wang, Jiaying Shen, Qi Song, Xueying Cui, Zehuan Shi, Jin Su, Jiajie Zang
Journal of Human Nutrition and Dietetics.2022; 35(3): 542. CrossRef - Positive antithyroid antibody predicts severity of neuromyelitis optica spectrum disorder in children
Liang Huo, Hua Wang, Yujun Yuan, Jian Gao, Xueyan Liu
Multiple Sclerosis and Related Disorders.2022; 57: 103425. CrossRef - Seasonality of month of birth in patients with autoimmune endocrine diseases: A systematic review
Ana M. Ramos-Leví, Gloria Collado, Monica Marazuela
Endocrinología, Diabetes y Nutrición.2022; 69(10): 779. CrossRef - Are ethnic differences, urinary iodine status, lead and cadmium exposure associated with thyroid autoimmunity and hypothyroid status? A cross-sectional study
Yi Chen, Qian Xiang, Ningjian Wang, Wen Zhang, Chunfang Zhu, Yuying Wang, Heng Wan, Jing Cheng, Kun Zhang, Yan Cai, Yingli Lu
BMJ Open.2022; 12(2): e056909. CrossRef - The Association of Thyroid Nodules With Blood Trace Elements Identified in a Cross-Section Study
Huixian Zeng, Yuanyuan Hu, Yaosheng Luo, Yanshi Ye, Cheng Song, Genfeng Yu, Zhi Chen, Siyang Liu, Yongqian Liang, Lingling Liu, Heng Wan, Jie Shen
Frontiers in Nutrition.2022;[Epub] CrossRef - Nutritional Management of Thyroiditis of Hashimoto
Yana Danailova, Tsvetelina Velikova, Georgi Nikolaev, Zorka Mitova, Alexander Shinkov, Hristo Gagov, Rossitza Konakchieva
International Journal of Molecular Sciences.2022; 23(9): 5144. CrossRef - Association Between Vitamin D Deficiency and Autoimmune Thyroid Disorder: A Systematic Review
Sabah A Khozam, Abdulhadi M Sumaili, Mohammed A Alflan, Rawan As'ad Salameh Shawabkeh
Cureus.2022;[Epub] CrossRef - Metabolic Characteristics of Hashimoto’s Thyroiditis Patients and the Role of Microelements and Diet in the Disease Management—An Overview
Aniceta A. Mikulska, Marta Karaźniewicz-Łada, Dorota Filipowicz, Marek Ruchała, Franciszek K. Główka
International Journal of Molecular Sciences.2022; 23(12): 6580. CrossRef - Predictors of autoimmune thyroid disease
Carol Cardona Attard, W. C. Candy Sze, Sandro Vella
Baylor University Medical Center Proceedings.2022; 35(5): 608. CrossRef - Selenium Status and Supplementation Effects in Pregnancy—A Study on Mother–Child Pairs from a Single-Center Cohort
Dorota Filipowicz, Ewelina Szczepanek-Parulska, Małgorzata Kłobus, Krzysztof Szymanowski, Thilo Samson Chillon, Sabrina Asaad, Qian Sun, Aniceta A. Mikulska-Sauermann, Marta Karaźniewicz-Łada, Franciszek K. Główka, Dominika Wietrzyk, Lutz Schomburg, Marek
Nutrients.2022; 14(15): 3082. CrossRef - Inflammasome activation as a link between obesity and thyroid disorders: Implications for an integrated clinical management
Rosario Le Moli, Veronica Vella, Dario Tumino, Tommaso Piticchio, Adriano Naselli, Antonino Belfiore, Francesco Frasca
Frontiers in Endocrinology.2022;[Epub] CrossRef - Seasonality of month of birth in patients with autoimmune endocrine diseases: A systematic review
Ana M. Ramos-Leví, Gloria Collado, Monica Marazuela
Endocrinología, Diabetes y Nutrición (English ed.).2022; 69(10): 779. CrossRef - Impact of iodine intake on the pathogenesis of autoimmune thyroid disease in children and adults
Iyshwarya Bhaskar Kalarani, Ramakrishnan Veerabathiran
Annals of Pediatric Endocrinology & Metabolism.2022; 27(4): 256. CrossRef - Morphological features of thyroid benign focal neoplasms in Graves’ disease
Yu.V. Buldygina, A.V. Zelinskaya, L.Yu. Zurnadzhy, Yu.M. Tarashchenko, S.L. Shlyakhtych, M.D. Tronko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(4): 213. CrossRef - Onset of Marine-Lenhart syndrome and Graves’ ophthalmopathy in a female patient treated with alemtuzumab for multiple sclerosis
Rosario Le Moli, Marco Russo, Pasqualino Malandrino, Veronica Vella, Antonino Belfiore, Francesco Frasca
Hormones.2021; 20(1): 161. CrossRef - Limited Genetic Overlap Between Overt Hashimoto’s Thyroiditis and Graves’ Disease in Twins: A Population-based Study
Jakob Skov, Jan Calissendorff, Daniel Eriksson, Patrik Magnusson, Olle Kämpe, Sophie Bensing, Ralf Kuja-Halkola
The Journal of Clinical Endocrinology & Metabolism.2021; 106(4): e1101. CrossRef - DNA Methylation Patterns in the HLA-DPB1 and PDCD1LG2 Gene Regions in Patients with Autoimmune Thyroiditis from Different Water Iodine Areas
Siyuan Wan, Lixiang Liu, Bingxuan Ren, Mengying Qu, Huaiyong Wu, Wen Jiang, Xiaoming Wang, Hongmei Shen
Thyroid.2021; 31(11): 1741. CrossRef - Персоналізація лікування хвороби Грейвса на підставі клініко- імунологічних характеристик перебігу захворювання
Yu.V. Buldygina, S.L. Shlyakhtych, H.M. Terekhova, T.V. Fed’ko, V.M. Klochkova, L.S. Strafun, Z.H. Lysova, I.I. Savos’ko
Endokrynologia.2021; 26(4): 409. CrossRef - Parity and Incidence of Thyroid Autoimmunity: A Population-Based Tehran Thyroid Study
Miralireza Takyar, Maryam Rahmani, Atieh Amouzegar, Elham Madreseh, Maryam Tohidi, Ladan Mehran, Fereidoun Azizi
Thyroid.2020; 30(8): 1186. CrossRef - Immunomodulatory effect of vitamin D and its potential role in the prevention and treatment of thyroid autoimmunity: a narrative review
D. Gallo, L. Mortara, M. B. Gariboldi, S. A. M. Cattaneo, S. Rosetti, L. Gentile, D. M. Noonan, P. Premoli, C. Cusini, M. L. Tanda, L. Bartalena, E. Piantanida
Journal of Endocrinological Investigation.2020; 43(4): 413. CrossRef - Hashimoto Thyreoiditis, therapeutische Optionen und extrathyreoidale Assoziationen – ein aktueller Überblick
Eva Petnehazy, Wolfgang Buchinger
Wiener Medizinische Wochenschrift.2020; 170(1-2): 26. CrossRef - Pathophysiological Role and Therapeutic Implications of Vitamin D in Autoimmunity: Focus on Chronic Autoimmune Diseases
Mattia Bellan, Laura Andreoli, Chiara Mele, Pier Paolo Sainaghi, Cristina Rigamonti, Silvia Piantoni, Carla De Benedittis, Gianluca Aimaretti, Mario Pirisi, Paolo Marzullo
Nutrients.2020; 12(3): 789. CrossRef - Thyroxine-binding globulin, peripheral deiodinase activity, and thyroid autoantibody status in association of phthalates and phenolic compounds with thyroid hormones in adult population
Sohyeon Choi, Min Joo Kim, Young Joo Park, Sunmi Kim, Kyungho Choi, Gi Jeong Cheon, Yoon Hee Cho, Hye Li Jeon, Jiyoung Yoo, Jeongim Park
Environment International.2020; 140: 105783. CrossRef - Immunomodulatory Effects of Vitamin D in Thyroid Diseases
Chiara Mele, Marina Caputo, Alessandro Bisceglia, Maria Teresa Samà, Marco Zavattaro, Gianluca Aimaretti, Loredana Pagano, Flavia Prodam, Paolo Marzullo
Nutrients.2020; 12(5): 1444. CrossRef - Significance of arsenic and lead in Hashimoto's thyroiditis demonstrated on thyroid tissue, blood, and urine samples
Aleksandar Stojsavljević, Branislav Rovčanin, Jovana Jagodić, Danijela Drašković Radojković, Ivan Paunović, Marija Gavrović-Jankulović, Dragan Manojlović
Environmental Research.2020; 186: 109538. CrossRef - Graves’ disease: Epidemiology, genetic and environmental risk factors and viruses
Alessandro Antonelli, Silvia Martina Ferrari, Francesca Ragusa, Giusy Elia, Sabrina Rosaria Paparo, Ilaria Ruffilli, Armando Patrizio, Claudia Giusti, Debora Gonnella, Alfonso Cristaudo, Rudy Foddis, Yehuda Shoenfeld, Poupak Fallahi
Best Practice & Research Clinical Endocrinology & Metabolism.2020; 34(1): 101387. CrossRef - Vitamin D deficiency and thyroid autoantibody fluctuations in patients with Graves’ disease – A mere coincidence or a real relationship?
Maria Teresa Płazińska, Agata Czarnywojtek, Nadia Sawicka-Gutaj, Małgorzata Zgorzalewicz-Stachowiak, Barbara Czarnocka, Paweł Gut, Maria Karlinska, Marta Fichna, Adam Stachowski, Marek Ruchała, Iwona Krela-Kaźmierczak, Leszek Królicki
Advances in Medical Sciences.2020; 65(1): 39. CrossRef - An eight-year-old girl with autoimmune polyglandular syndrome type3A that developed during the course of primary Epstein–Barr virus (EBV) infection: clinical implication of EBV in autoimmune thyroid disease
Shizuka Kirino, Hisae Nakatani, Aoi Honma, Asami Shinbo, Keiko Onda, Mari Okada, Masako Imai, Natsuko Suzuki, Akihiro Oshiba, Masayuki Nagasawa
Immunological Medicine.2020; 43(1): 57. CrossRef - Exploring the role of copper and selenium in the maintenance of normal thyroid function among healthy Koreans
Min Joo Kim, Soo Chin Kim, Soie Chung, Serim Kim, Ji Won Yoon, Young Joo Park
Journal of Trace Elements in Medicine and Biology.2020; 61: 126558. CrossRef - A comparison of serum zinc levels in melasma and non-melasma patients: a preliminary study of thyroid dysfunction
Indina Sastrini Sekarnesia, Irma Bernadette S. Sitohang, Triana Agustin, Wismandari Wisnu, Aida S. D. Hoemardani
Acta Dermatovenerologica Alpina Pannonica et Adriatica.2020;[Epub] CrossRef - Hashimoto's thyroiditis: An update on pathogenic mechanisms, diagnostic protocols, therapeutic strategies, and potential malignant transformation
Massimo Ralli, Diletta Angeletti, Marco Fiore, Vittorio D'Aguanno, Alessandro Lambiase, Marco Artico, Marco de Vincentiis, Antonio Greco
Autoimmunity Reviews.2020; 19(10): 102649. CrossRef - Vitamin D and Autoimmune Thyroid Disease—Cause, Consequence, or a Vicious Cycle?
Inês Henriques Vieira, Dírcea Rodrigues, Isabel Paiva
Nutrients.2020; 12(9): 2791. CrossRef - New Insights into Mechanisms of Endocrine-Disrupting Chemicals in Thyroid Diseases: The Epigenetic Way
Letizia Pitto, Francesca Gorini, Fabrizio Bianchi, Elena Guzzolino
International Journal of Environmental Research and Public Health.2020; 17(21): 7787. CrossRef - Genotype association of IP6K3 gene with Hashimoto’s thyroiditis in Algerian population (Aures region)
Warda Kherrour, Dean Kalicanin, Luka Brčić, Leila Hambaba, Mouloud Yahia, Souheyla Benbia, Vesna Boraska Perica
Egyptian Journal of Medical Human Genetics.2020;[Epub] CrossRef - TOTAL ANTIOXIDANT ACTIVITY AND MANGANESE SUPEROXIDE DISMUTASE IN COMORBIDITY OF GASTROESOPHAGEAL REFLUX DISEASE AND AUTOIMMUNE THYROIDITIS IN STUDENT POPULATION
Tamara M. Pasiieshvili, Natalia M. Zhelezniakova, Lyudmila M. Pasiyeshvili, Olga M. Kovalyova
Wiadomości Lekarskie.2020; 73(12): 2644. CrossRef - Vitamin B12 and Vitamin D Levels in Patients with Autoimmune Hypothyroidism and Their Correlation with Anti-Thyroid Peroxidase Antibodies
Hanife Şerife Aktaş
Medical Principles and Practice.2020; 29(4): 364. CrossRef - Increased Risk of Thyroid Dysfunction Among Patients With Rheumatoid Arthritis
Qian Li, Bin Wang, Kaida Mu, Jing Zhang, Yanping Yang, Wei Yao, Jie Zhu, Jin-an Zhang
Frontiers in Endocrinology.2019;[Epub] CrossRef - Association between thyroglobulin polymorphisms and autoimmune thyroid disease: a systematic review and meta-analysis of case–control studies
Ming-Liang Zhang, Dong-ming Zhang, Cai-E. Wang, Xiao-Long Chen, Fang-Zhou Liu, Jian-Xue Yang
Genes & Immunity.2019; 20(6): 484. CrossRef - Changes in glucose‐lipid metabolism, insulin resistance, and inflammatory factors in patients with autoimmune thyroid disease
Yi Lei, Jun Yang, Hua Li, Haihua Zhong, Qin Wan
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Evaluation of Qualitative Dietary Protocol (Diet4Hashi) Application in Dietary Counseling in Hashimoto Thyroiditis: Study Protocol of a Randomized Controlled Trial
Natalia Wojtas, Lidia Wadolowska, Elżbieta Bandurska-Stankiewicz
International Journal of Environmental Research and Public Health.2019; 16(23): 4841. CrossRef - Sjögren’s Syndrome and Autoimmune Thyroid Disease: Two Sides of the Same Coin
Juan-Manuel Anaya, Paula Restrepo-Jiménez, Yhojan Rodríguez, Mónica Rodríguez-Jiménez, Yeny Acosta-Ampudia, Diana M. Monsalve, Yovana Pacheco, Carolina Ramírez-Santana, Nicolás Molano-González, Rubén D. Mantilla
Clinical Reviews in Allergy & Immunology.2019; 56(3): 362. CrossRef - Disease Presentation and Remission Rate in Graves Disease Treated With Antithyroid Drugs: is Gender Really A Factor?
Talia Diker-Cohen, Hadar Duskin-Bitan, Ilan Shimon, Dania Hirsch, Amit Akirov, Gloria Tsvetov, Eyal Robenshtok
Endocrine Practice.2019; 25(1): 43. CrossRef - IRAK2 and TLR10 confer risk of Hashimoto’s disease: a genetic association study based on the Han Chinese population
Miao Li, Wei Han, Li Zhu, Jue Jiang, Wei Qu, Lei Zhang, Liang Jia, Qi Zhou
Journal of Human Genetics.2019; 64(7): 617. CrossRef - Environmental exposure to pesticides and risk of thyroid diseases
Mar Requena, Antonia López-Villén, Antonio F. Hernández, Tesifón Parrón, Ángela Navarro, Raquel Alarcón
Toxicology Letters.2019; 315: 55. CrossRef - Determining the Level of Knowledge about Graves’ Disease: Single-Center Results
Hande Peynirci, Çiğdem Uzuntepe Aksu, Akif Doğan, Canan Ersoy
Ankara Medical Journal.2019;[Epub] CrossRef - Association between lifestyle and thyroid dysfunction: a cross-sectional epidemiologic study in the She ethnic minority group of Fujian Province in China
Yanling Huang, Liangchun Cai, Yuanyuan Zheng, Jinxing Pan, Liantao Li, Liyao Zong, Wei Lin, Jixing Liang, Huibin Huang, Junping Wen, Gang Chen
BMC Endocrine Disorders.2019;[Epub] CrossRef - Vitamin D Receptor Gene Polymorphisms and Autoimmune Thyroiditis: Are They Associated with Disease Occurrence and Its Features?
Adam Maciejewski, Michał J. Kowalczyk, Waldemar Herman, Adam Czyżyk, Marta Kowalska, Ryszard Żaba, Katarzyna Łącka
BioMed Research International.2019; 2019: 1. CrossRef - Diagnosis of Graves’ disease – laboratory tests and possible difficulties in interpretation
Agata Maria Kalicka
Diagnostyka Laboratoryjna.2019; 55(2): 121. CrossRef - The influence of single-nucleotide polymorphisms of interleukin-1β -511 and +3954 on the susceptibility to Hashimoto’s thyroiditis in Egyptian women: immune-endocrine interactions
Nearmeen M. Rashad, Manar H. Soliman, Mayada M. Mousa, Azza H. Abd El-Fatah
The Egyptian Journal of Internal Medicine.2019; 31(1): 14. CrossRef - Global epidemiology of hyperthyroidism and hypothyroidism
Peter N. Taylor, Diana Albrecht, Anna Scholz, Gala Gutierrez-Buey, John H. Lazarus, Colin M. Dayan, Onyebuchi E. Okosieme
Nature Reviews Endocrinology.2018; 14(5): 301. CrossRef - Selenoproteins in human body: focus on thyroid pathophysiology
Ana Valea, Carmen Emanuela Georgescu
Hormones.2018; 17(2): 183. CrossRef - Epidemiology of hyperthyroidism in Iran: a systematic review and meta-analysis
Sayed Mahmoud Sajjadi-Jazi, Farshad Sharifi, Mehdi Varmaghani, Hamidreza Aghaei Meybodi, Farshad Farzadfar, Bagher Larijani
Journal of Diabetes & Metabolic Disorders.2018; 17(2): 345. CrossRef - The effect of vitamin D supplementation on thyroid autoantibody levels in the treatment of autoimmune thyroiditis: a systematic review and a meta-analysis
Su Wang, Yaping Wu, Zhihua Zuo, Yijing Zhao, Kun Wang
Endocrine.2018; 59(3): 499. CrossRef - Thyroid disorders in alemtuzumab-treated multiple sclerosis patients: a Belgian consensus on diagnosis and management
Brigitte Decallonne, Emmanuel Bartholomé, Valérie Delvaux, Miguel D’haeseleer, Souraya El Sankari, Pierrette Seeldrayers, Bart Van Wijmeersch, Chantal Daumerie
Acta Neurologica Belgica.2018; 118(2): 153. CrossRef - Synergistic interactions of Angiotensin Converting Enzyme (ACE) gene and Apolipoprotein E (APOE) gene polymorphisms with T1DM susceptibility in south India
Padma-Malini Ravi, Rathika Chinniah, Ramgopal Sivanadham, Murali Vijayan, Dharmarajan Pannerselvam, S. Pushkala, Balakrishnan Karuppiah
Meta Gene.2018; 18: 39. CrossRef - The effect of obesity and dietary habits on oxidative stress in Hashimoto’s thyroiditis
Maria Giannakou, Katerina Saltiki, Emily Mantzou, Eleni Loukari, Georgios Philippou, Konstantinos Terzidis, Charalampos Stavrianos, Miltiades Kyprianou, Theodora Psaltopoulou, Kalliopi Karatzi, Maria Alevizaki
Endocrine Connections.2018; 7(9): 990. CrossRef - Interaction of HLA-DRB1* alleles and CTLA4 (+ 49 AG) gene polymorphism in Autoimmune Thyroid Disease
Sivanadham Ramgopal, Chinniah Rathika, Malini Ravi Padma, Vijayan Murali, Kannan Arun, Mohamed Nainar Kamaludeen, Karuppiah Balakrishnan
Gene.2018; 642: 430. CrossRef - New insights into the etiopathogenesis of Hashimoto's Thyroiditis: The role of genetics and epigenetics
Massimo Ralli, Armando De Virgilio, Marco Artico, Lucia Longo, Marco de Vincentiis, Antonio Greco
Autoimmunity Reviews.2018; 17(10): 1065. CrossRef - Comorbidity of autoimmune thyroid disorders and psychiatric disorders during the postpartum period: a Danish nationwide register-based cohort study
V. Bergink, V. J. M. Pop, P. R. Nielsen, E. Agerbo, T. Munk-Olsen, X. Liu
Psychological Medicine.2018; 48(8): 1291. CrossRef - Spontaneous conversion from Graves’ disease to Hashimoto’s thyroiditis: a case report
Muharrem Bayrak, Kenan Çadırcı, Emine Kartal Baykan, Ünsal Aydın, Ayşe Çarlıoğlu
Ortadoğu Tıp Dergisi.2018; 10(1): 81. CrossRef - Association of established hypothyroidism-associated genetic variants with Hashimoto’s thyroiditis
A. Barić, L. Brčić, S. Gračan, V. Torlak Lovrić, I. Gunjača, M. Šimunac, M. Brekalo, M. Boban, O. Polašek, M. Barbalić, T. Zemunik, A. Punda, V. Boraska Perica
Journal of Endocrinological Investigation.2017; 40(10): 1061. CrossRef - Immune Response of Laying Hens Exposed to 30 ppm Ammonia
for 25 Weeks
H. Chen, F.F. Yan, J.Y. Hu, Yanan Wu, C.M. Tucker, A.R. Green, H.W. Cheng
International Journal of Poultry Science.2017; 16(4): 139. CrossRef - Dietary Factors Associated with Plasma Thyroid Peroxidase and Thyroglobulin Antibodies
Antonela Matana, Vesela Torlak, Dubravka Brdar, Marijana Popović, Bernarda Lozić, Maja Barbalić, Vesna Boraska Perica, Ante Punda, Ozren Polašek, Caroline Hayward, Tatijana Zemunik
Nutrients.2017; 9(11): 1186. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Does vitamin D play a role in autoimmune endocrine disorders? A proof of concept
Barbara Altieri, Giovanna Muscogiuri, Luigi Barrea, Chantal Mathieu, Carla V. Vallone, Luca Mascitelli, Giorgia Bizzaro, Vincenzo M. Altieri, Giacomo Tirabassi, Giancarlo Balercia, Silvia Savastano, Nicola Bizzaro, Cristina L. Ronchi, Annamaria Colao, Alf
Reviews in Endocrine and Metabolic Disorders.2017; 18(3): 335. CrossRef - A case‐control study of the association between ulcerative colitis and hyperthyroidism in an Asian population
Ming‐Chieh Tsai, Herng‐Ching Lin, Cha‐Ze Lee
Clinical Endocrinology.2017; 86(6): 825. CrossRef - Hashimoto's thyroiditis: relative recurrence risk ratio and implications for screening of first‐degree relatives
Nikita Bothra, Nalini Shah, Manjunath Goroshi, Swati Jadhav, Sheetal Padalkar, Hemangini Thakkar, Gurudayal Singh Toteja, Vyankatesh Shivane, Anurag Lila, Tushar Bandgar
Clinical Endocrinology.2017; 87(2): 201. CrossRef - Serum 25-OH vitamin D levels in systemic sclerosis: analysis of 140 patients and review of the literature
Dilia Giuggioli, M. Colaci, G. Cassone, P. Fallahi, F. Lumetti, A. Spinella, F. Campomori, A. Manfredi, C. U. Manzini, A. Antonelli, C. Ferri
Clinical Rheumatology.2017; 36(3): 583. CrossRef - Are Perinatal Events Risk Factors for Childhood Thyroid Autoimmunity?
Berglind Jonsdottir, Markus Lundgren, Sara Wallengren, Åke Lernmark, Ida Jönsson, Helena Elding Larsson
European Thyroid Journal.2017; 6(6): 298. CrossRef - Variants of Interleukin-22 Gene Confer Predisposition to Autoimmune Thyroid Disease
Rong-hua Song, Qian Li, Wen Wang, Qiu-ming Yao, Xiao-qing Shao, Jin-an Zhang
International Journal of Endocrinology.2017; 2017: 1. CrossRef - Environmental Issues in Thyroid Diseases
Silvia Martina Ferrari, Poupak Fallahi, Alessandro Antonelli, Salvatore Benvenga
Frontiers in Endocrinology.2017;[Epub] CrossRef
- Trends in Prevalence of Thyroid Dysfunction and its Associations With Mortality Among US Participants, 1988-2012

- Association between Cigarette Smoking and Thyroid Function in Adults without Previous History of Thyroid Disease.
- Bo Hyun Kim, Won Bae Kim, Tae Yong Kim, Hong Kyu Kim, Seong Hoon Jeon, Chang Won Lee, Young Kee Shong
- J Korean Endocr Soc. 2008;23(2):123-128. Published online April 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.2.123
- 2,156 View
- 31 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cigarette smoking has a significant impact on thyroid function. However, the association between smoking and thyroid function is incompletely understood. METHODS: We conducted a cross-sectional study that included 90,970 adults (age range: 20 to 79) who had visited the health promotion center at Asan Medical Center between January 1, 2001, and December 31, 2003. Those subjects with previous known thyroid disease, a history of thyroid operation, a history of thyroid function altering medication (herb, estrogen or digestive) or a family history of thyroid disease were excluded. Finally, 47,577 subjects (males: 30,726, females: 16,851) were included in this study. We calculated the age-adjusted geometric mean of the serum TSH and the age-adjusted mean of the serum free T4 among the current, former and never smokers. We also analyzed the age-adjusted prevalence of hypothyroidism and hyperthyroidism among each group. RESULTS: Among men, the geometric mean TSH level was significantly low in the current (1.40 mIU/L, 95% confidence interval [CI]: 1.38-1.41) and former smokers (1.59 mIU/L, 95% CI: 1.57-1.61) compared with the never smokers (1.65 mIU/L, 95% CI: 1.63-1.68). The mean free T4 level was high in the current smokers (1.236 ng/dL, 95% CI: 1.234-1.239) compared with the never smokers (1.234 ng/dL, 95% CI: 1.230-1.238). Similarly, among women, the geometric mean TSH level was low in the current smokers (1.75 mIU/L, 95% CI: 1.67-1.87) compared with the never smokers (1.85 mIU/L, 95% CI: 1.83-1.87). The mean free T4 level was high in the current smokers (1.149 ng/dL, 95% CI: 1.139-1.159) compared with the never smokers (1.138 ng/dL, 95% CI: 1.135-1.140). Among the current male smokers, heavy daily smoking (over 2 packs per day) was more associated with low TSH levels than moderate smoking (less than 1 pack per day). In men, the prevalence of subclinical hypothyroidism was low in the current smokers compared with the never smokers (odds ratio: 0.53, 95% CI: 0.43-0.66). CONCLUSION: We found that current smokers had lower TSH levels and higher free T4 levels than never smokers in both men and women and smoking was associated with a low prevalence of subclinical hypothyroidism in men, which may be of importance when evaluating subjects with subclinical hypothyroidism in Korea. -
Citations
Citations to this article as recorded by- Reference interval for thyrotropin in a ultrasonography screened Korean population
Mijin Kim, Tae Yong Kim, Soo Han Kim, Yunkyoung Lee, Su-yeon Park, Hyung-don Kim, Hyemi Kwon, Yun Mi Choi, Eun Kyung Jang, Min Ji Jeon, Won Gu Kim, Young Kee Shong, Won Bae Kim
The Korean Journal of Internal Medicine.2015; 30(3): 335. CrossRef - Clinical Review of Thyroid Dysfunction in the Subjects for Health Check-up
Ji Eun Park, Ho Chan Cho
Journal of Korean Thyroid Association.2012; 5(1): 52. CrossRef - Thyroid Dysfunction of North Korean Women Living in South Korea, Focusing on Subclinical Hypothyroidism
Joo Hyung Kim, Sol Ah Park, Nam Hoon Kim, Jae Hee Ahn, Yoon Jung Kim, Myongjin Cho, Yoon Jung Lee, Hye Jin Yoo, Hee Young Kim, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Sin Gon Kim
Endocrinology and Metabolism.2012; 27(3): 200. CrossRef
- Reference interval for thyrotropin in a ultrasonography screened Korean population

- Relationship between Plasma Leptin Levels and Carotid Intima-Medial Thickness in Korean Adults.
- Hyejin Lee, Eunsoon Hong, Youngsun Hong, Yeon Ah Sung
- J Korean Endocr Soc. 2002;17(1):87-94. Published online February 1, 2002
- 1,183 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Many studies have recently shown that leptin can promote angiogenesis via endothelial leptin receptors and induce oxidative stress in endothelial cells; These findings suggest the relationship between cardiovascular risk and blood leptin concentration. In the present study, we investigated the relationship between leptin concentration and carotid intima-medial thickness (CIMT) as an indicator of early atherosclerosis in adults. METHEODS: The study subjects comprised 138 (45 men and 93 women; mean age 42.4+/-7.5 years; mean BMI 24.0+/-2.7 kg/m2) without history of diabetes, hypertension or cardiovascular disease. We measured CIMT by high resolution ultrasonography and plasma leptin levels by radioimmunoassay. RESULTS: 1) No significant differences in age, BMI or CIMT between male and female subjects were noted, but the leptin levels in female were significantly higher than those in males. (8.42+/-5.90 ng/mL vs. 3.08+/-1.00 ng/mL, p<0.001) 2) CIMT showed a significant positive correlation with age (r=0.31, p< 0.001), BMI (r=0.25, p<0.01) and level (r=0.42, p<0.05) in simple regression analysis. 3) When male and female subjects were each divided into 3 groups by leptin concentration, no significant difference in CIMT among female subjects was found. In male subjects, CIMT was significantly higher in the highest tertile of leptin level than in the other 2 groups (0.65+/-0.03 mm vs. 0.56+/-0.07 mm and 0.53+/-0.07 mm, p<0.01) after adjustment for BMI and age. However, this difference was not significant after adjustment for smoking. 4) CIMT (0.61+/-0.05 mm vs. 0.53+/-0.07 mm, p<0.01) and leptin concentrations (3.57+/-2.13 ng/mL vs. 2.20+/-1.39 ng/mL, p<0.05) were significantly higher in male smokers than in male non-smokers. CONCLUSION: Our results demonstrated significant correlation of CIMT to plasma leptin level before adjustment for smoking. A possible explanation is the permissive action of smoking on the atherogenic effect of leptin. However, further studies to elucidate the relationships and interactions among smoking, leptin level and the development of atherosclerosis will be needed.


 KES
KES

 First
First Prev
Prev



