Search
- Page Path
- HOME > Search
- Calcium & Bone Metabolism
Big Data Articles (National Health Insurance Service Database) - 10-Year Fracture Risk in Postmenopausal Women with Osteopenia and Osteoporosis in South Korea
- Yeon-Hee Baek, Sun Wook Cho, Han Eol Jeong, Ju Hwan Kim, Yunji Hwang, Jeffrey L. Lange, Ju-Young Shin
- Endocrinol Metab. 2021;36(6):1178-1188. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1215
- 5,353 View
- 249 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
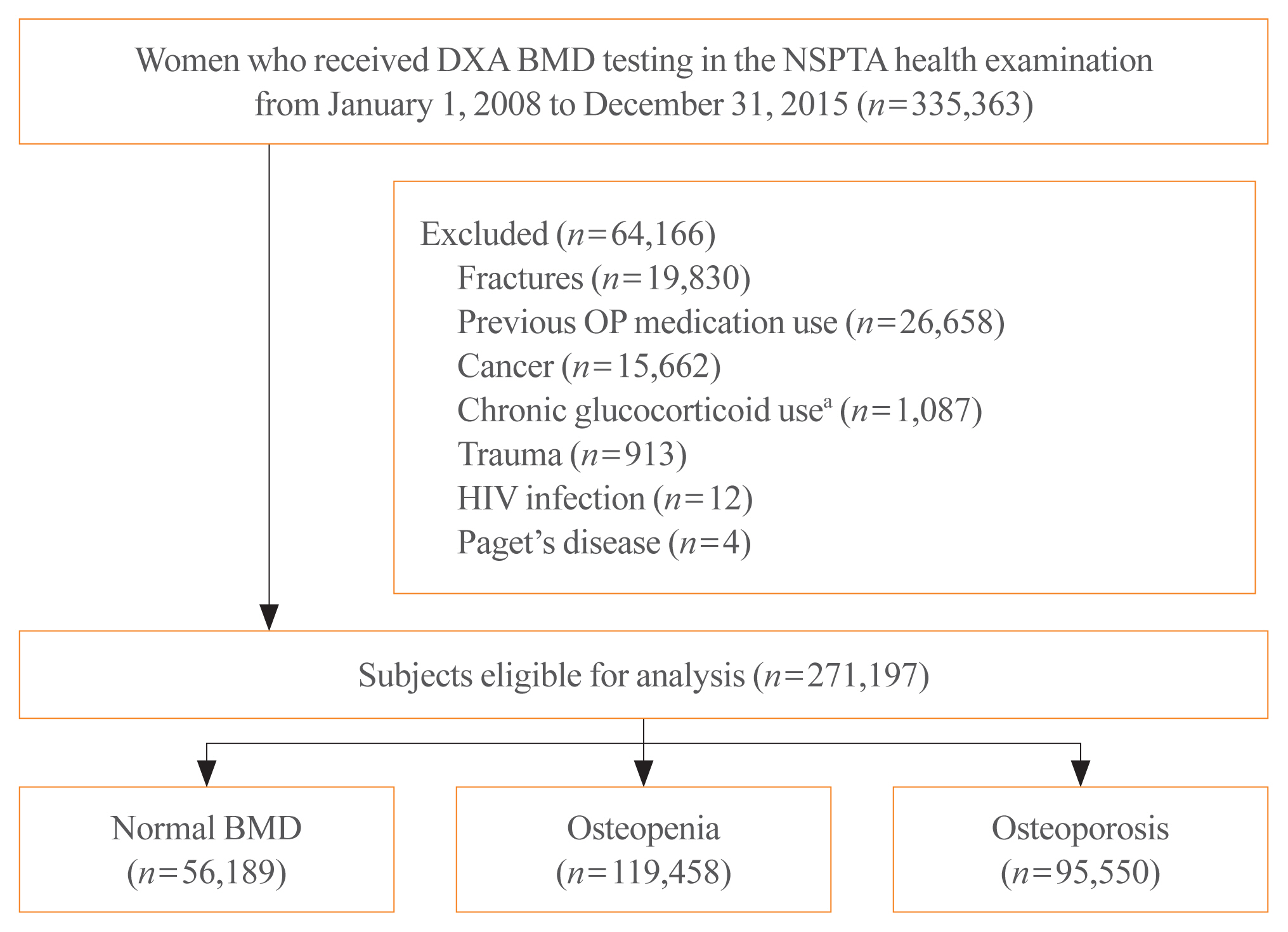
In South Korea, women aged 66 years are eligible for complimentary bone mineral density (BMD) screening via the National Screening Program for Transitional Ages. We aimed to evaluate the 10-year fracture risk in women receiving BMD screening between January 2008 and December 2015.
Methods
BMD was classified as normal (T-score ≥–1.0 standard deviation [SD]), osteopenia (T-score <–1.0 SD and >–2.5 SD), and osteoporosis (T score ≤–2.5 SD) from dual-energy X-ray absorptiometry. Follow-up continued from the screening date until a diagnosis for clinical fragility fracture (including sites of the vertebrae, hip, pelvis, clavicle, humerus, forearm, wrist, lower leg, and ankle), censored at the earliest date of trauma, death, or December 2017; fracture was ascertained using diagnostic codes from the National Health Insurance Service database. A multivariable Cox proportional hazard model was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of fracture in women with osteopenia or osteoporosis relative to women with normal BMD.
Results
Among the 271,197 women screened, 44.0% had osteopenia and 35.2% had osteoporosis. The 10 year cumulative incidence of fragility fractures was 31.1%, 37.5%, and 44.3% in women with normal BMD, osteopenia, and osteoporosis, respectively. Fracture risk was higher in women with osteopenia (HR, 1.31; 95% CI, 1.28 to 1.34) and osteoporosis (HR, 1.68; 95% CI, 1.64 to 1.72) than in women with normal BMD.
Conclusion
Women with osteopenia and women with osteoporosis, identified by the national BMD screening program, demonstrated a substantially elevated risk of fracture. -
Citations
Citations to this article as recorded by- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women
S. Han, S. Kim, E.J. Yeh, H.S. Suh
Osteoporosis International.2024; 35(2): 339. CrossRef - Duration of osteoporosis treatment to reduce the risk of subsequent osteoporotic fracture and all-cause mortality in elderly hip fracture patients in a Korean real-world study
Soong Joon Lee, Minjoon Cho, Hojoon Lee, Hyuna Lim, Jae Hyup Lee
Archives of Osteoporosis.2024;[Epub] CrossRef - Do Patients with Benign Paroxysmal Positional Vertigo Have a Higher Prevalence of Osteoporosis? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Keunho Kim, Yeonjoo Choi
Journal of Personalized Medicine.2024; 14(3): 303. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Chronic airway disease as a major risk factor for fractures in osteopenic women: Nationwide cohort study
Sung Hye Kong, Ae Jeong Jo, Chan Mi Park, Kyun Ik Park, Ji Eun Yun, Jung Hee Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biomimetic Porous Magnesium Alloy Scaffolds Promote the Repair of Osteoporotic Bone Defects in Rats through Activating the Wnt/β-Catenin Signaling Pathway
Yuanchao Zhu, Gaozhi Jia, Yifei Yang, Jian Weng, Su Liu, Mengwei Zhang, Geng Zhang, Haotian Qin, Yixiao Chen, Qi Yang, Guangyin Yuan, Fei Yu, Hui Zeng
ACS Biomaterials Science & Engineering.2023; 9(6): 3435. CrossRef - Correlation between bone mineral density and bone metabolic markers in postmenopausal women with osteoporotic fractures at different C-terminal telopeptide of type 1 collagen levels: a retrospective analysis study
Xiaonan Zhu, Lin Chen, Ling Pan, Yuexi Zeng, Qiang Fu, Yanbin Liu, Yongde Peng, Yufan Wang, Li You
Menopause.2023; 30(11): 1139. CrossRef - Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
Endocrinology and Metabolism.2023; 38(6): 669. CrossRef - A Meaningful Journey to Predict Fractures with Deep Learning
Jeonghoon Ha
Endocrinology and Metabolism.2022; 37(4): 617. CrossRef - The Efficacy of Selective Estrogen Receptor Modulators Monotherapies in Postmenopausal Women with Osteopenia
Kyung Wook Kim, Young Il Kim, Ki-Choul Kim
Journal of Bone Metabolism.2022; 29(3): 185. CrossRef - Correlation of Psoas Muscle Index with Fragility Vertebral Fracture: A Retrospective Cross-Sectional Study of Middle-Aged and Elderly Women
Yihui Zhang, Yilihamu Dilixiati, Wei Jiang, Xiufeng Cao, Yuanyuan Chen, Hui Guo, Christian-Heinz Anderwald
International Journal of Endocrinology.2022; 2022: 1. CrossRef
- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women

- Clinical Study
- Association between Obesity and Bone Mineral Density by Gender and Menopausal Status
- Mohammad Reza Salamat, Amir Hossein Salamat, Mohsen Janghorbani
- Endocrinol Metab. 2016;31(4):547-558. Published online November 4, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.547
- 5,545 View
- 65 Download
- 62 Web of Science
- 62 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated whether there were gender differences in the effect of obesity on bone mineral density (BMD) based on menopausal status.
Methods We assessed 5,892 consecutive patients 20 to 91 years old who were referred for dual-energy X-ray absorptiometry (DXA) scans. All subjects underwent a standard BMD scan of the hip (total hip and femoral neck) and lumbar spine (L1 to L4) using a DXA scan and body size assessment. Body mass index was used to categorize the subjects as normal weight, overweight, and obese.
Results BMD was higher in obese and overweight versus normal weight men, premenopausal women, and postmenopausal women. Compared to men ≥50 years and postmenopausal women with normal weight, the age-adjusted odds ratio of osteopenia was 0.19 (95% confidence interval [CI], 0.07 to 0.56) and 0.38 (95% CI, 0.29 to 0.51) for obese men ≥50 years and postmenopausal women. Corresponding summaries for osteoporosis were 0.26 (95% CI, 0.11 to 0.64) and 0.15 (95% CI, 0.11 to 0.20), respectively. Compared to men <50 years and premenopausal women with normal weight, the age-adjusted odds ratio of low bone mass was 0.22 (95% CI, 0.11 to 0.45) and 0.16 (95% CI, 0.10 to 0.26) for obese men <50 years and premenopausal women, respectively.
Conclusion Obesity is associated with BMD of the hip and lumbar spine and overweight and obese individuals have similar degrees of osteoporosis. This result was not significantly different based on gender and menopausal status, which could be an important issue for further investigation.
-
Citations
Citations to this article as recorded by- The inter-relationship of the triad: osteoporosis, fracture risk, and obesity—a longitudinal multicenter analysis by the Egyptian Academy of Bone Health
Yasser El Miedany, Maha El Gaafary, Safaa Mahran, Naglaa Gadallah, Atef Abdel Azim, Waleed Hassan, Mohammed Hassan Abu-Zaid, Radwa H. Shalaby, Samar abd Alhamed Tabra, Walaa Elwakil
Egyptian Rheumatology and Rehabilitation.2024;[Epub] CrossRef - Relationships between obesity markers and bone parameters in community-dwelling older adults
L. Lemoine, F. Buckinx, A. Aidoud, V. Leroy, B. Fougère, M. Aubertin-Leheudre
Aging Clinical and Experimental Research.2024;[Epub] CrossRef - The Influence of Obesity on Bone Health in Post-COVID-19 Recovery- Single-Center Experience
Bhumi Chaturvedi, Sourav Debnath, Hemant Bareth, Preeti Raj, Pratima Singh, Mahaveer Singh, Deepak Nathiya, Balvir Tomar
International Journal of General Medicine.2024; Volume 17: 29. CrossRef - Can routine MRI spine T1 sequences be used for prediction of decreased bone density?
Hrishikesh Kale, Saksham Yadav
Acta Radiologica.2023; 64(1): 164. CrossRef - Inverse association of serum osteocalcin and bone mineral density in renal transplant recipients
Wei-Chen Lin, Ming-Che Lee, Yen-Cheng Chen, Bang-Gee Hsu
Tzu Chi Medical Journal.2023; 35(2): 165. CrossRef - Understanding the confluence of injury and obesity in a Grade 2 obesity and above population
Richard C. Franklin, Janet L. Franklin, Jessica M. Swinbourne, Elisia Manson, Georgina Loughnan, Tania Markovic, Samantha Hocking
Australian and New Zealand Journal of Public Health.2023; 47(1): 100008. CrossRef - The association of dietary acid load (DAL) with estimated skeletal muscle mass and bone mineral content: a cross-sectional study
Fatemeh Gholami, Niki Bahrampour, Mahsa Samadi, Niloufar Rasaei, Habib Yarizadeh, Sina Naghshi, Khadijeh Mirzaei
BMC Nutrition.2023;[Epub] CrossRef - The Relationship between Bone Mineral Densitometry and Visceral Adiposity Index in Postmenopausal Women
Halis Elmas, Cevdet Duran, Mustafa Can, Ismet Tolu, Ibrahim Guney
Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics.2023; 45(02): 082. CrossRef - A Review of Potential Therapies to Attenuate Bone Mineral Density Loss in Obese Individuals Prior to Total Joint Replacement Surgery
Charlotte von Hoffmann, Kayla Penta, Amanpreet Singh
Cureus.2023;[Epub] CrossRef - Association between Adiposity and Bone Mineral Density in Adults: Insights from a National Survey Analysis
Yang Jiao, Juan Sun, Yuanmeng Li, Junduo Zhao, Jianxiong Shen
Nutrients.2023; 15(15): 3492. CrossRef - Extract of Artemisia dracunculus L. Modulates Osteoblast Proliferation and Mineralization
Matthew C. Scott, Aleah Bourgeois, Yongmei Yu, David H. Burk, Brenda J. Smith, Z. Elizabeth Floyd
International Journal of Molecular Sciences.2023; 24(17): 13423. CrossRef - Determinants of Bone Mineral Density in Iranian Women with Polycystic Ovary Syndrome
Fariba Karimi, Parisa Mardani
International Journal of Endocrinology and Metabolism.2023;[Epub] CrossRef - The effect of overweight or obesity on osteoporosis: A systematic review and meta-analysis
Yupeng Liu, Yi Liu, Yufeng Huang, Siyu Le, Huinan Jiang, Binye Ruan, Xuemei Ao, Xudong Shi, Xiaoyi Fu, Shuran Wang
Clinical Nutrition.2023; 42(12): 2457. CrossRef - Association of the visceral adiposity index with femur bone mineral density and osteoporosis among the U.S. older adults from NHANES 2005–2020: a cross-sectional study
Aochuan Sun, Jiayu Hu, Shushangzhi Wang, Fen Yin, Zhengtang Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - High fat diet causes inferior vertebral structure and function without disc degeneration in RAGE‐KO mice
Danielle N. D'Erminio, Divya Krishnamoorthy, Alon Lai, Robert C. Hoy, Devorah M. Natelson, Jashvant Poeran, Andrew Torres, Damien M. Laudier, Philip Nasser, Deepak Vashishth, Svenja Illien‐Jünger, James C. Iatridis
Journal of Orthopaedic Research.2022; 40(7): 1672. CrossRef - Dosing Therapeutic Radiopharmaceuticals in Obese Patients
Merel van Nuland, Tessa F. Ververs, Marnix G. E. H. Lam
International Journal of Molecular Sciences.2022; 23(2): 818. CrossRef - Bone Density and Structure in Overweight Men With and Without Diabetes
Jakob Starup-Linde, Marie Juul Ornstrup, Thomas Nordstrøm Kjær, Simon Lykkeboe, Aase Handberg, Søren Gregersen, Torben Harsløf, Steen Bønløkke Pedersen, Peter Vestergaard, Bente Lomholt Langdahl
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Relationship Between Bone Mineral Density and Body Composition Among Qatari Women With High Rate of Obesity: Qatar Biobank Data
Abdelhamid Kerkadi, Shalima Lathief, Yasmen Khial, Toka Teleb, Grace Attieh, Md Mizanur Rahman, Zumin Shi, Abdelali Agouni
Frontiers in Nutrition.2022;[Epub] CrossRef - Predicting Lumbar Vertebral Osteopenia Using LvOPI Scores and Logistic Regression Models in an Exploratory Study of Premenopausal Taiwanese Women
Chun-Wen Chen, Yi-Jui Liu, Shao-Chieh Lin, Chien-Yuan Wang, Wu-Chung Shen, Der-Yang Cho, Tung-Yang Lee, Cheng-Hsuan Juan, Cheng-En Juan, Kai-Yuan Cheng, Chun-Jung Juan
Journal of Medical and Biological Engineering.2022; 42(5): 722. CrossRef - Thirty Obesity Myths, Misunderstandings, and/or Oversimplifications: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022
Harold Edward Bays, Angela Golden, Justin Tondt
Obesity Pillars.2022; 3: 100034. CrossRef - Bone mass in Saudi women aged 20–40 years: the association with obesity and vitamin D deficiency
Mai Albaik, Jalaluddin A. Khan, Ikhlas Sindi, Kristina E. Akesson, Fiona E. A. McGuigan
Archives of Osteoporosis.2022;[Epub] CrossRef - The pathophysiology of osteoporosis in obesity and type 2 diabetes in aging women and men: The mechanisms and roles of increased bone marrow adiposity
Dalia Ali, Michaela Tencerova, Florence Figeac, Moustapha Kassem, Abbas Jafari
Frontiers in Endocrinology.2022;[Epub] CrossRef - Roles of Follicle-Stimulating Hormone on Bone Metabolism in Late Postmenopausal Women
Chaiho Jeong, Jinyoung Kim, Yejee Lim, Jeonghoon Ha, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Journal of Bone Metabolism.2022; 29(3): 175. CrossRef - Bone Health in Adults With Prader–Willi Syndrome: Clinical Recommendations Based on a Multicenter Cohort Study
Denise H van Abswoude, Karlijn Pellikaan, Anna G W Rosenberg, Kirsten Davidse, Muriel Coupaye, Charlotte Høybye, Tania P Markovic, Graziano Grugni, Antonino Crinò, Assumpta Caixàs, Christine Poitou, Helena Mosbah, Tessa Weir, Leo A van Vlimmeren, Joost P
The Journal of Clinical Endocrinology & Metabolism.2022; 108(1): 59. CrossRef - Does the Severity of Obesity Influence Bone Mineral Density Values in Premenopausal Women?
Emneh Hammoud, Hechmi Toumi, Christophe Jacob, Antonio Pinti, Eric Lespessailles, Rawad El Hage
Journal of Clinical Densitometry.2021; 24(2): 225. CrossRef - Serum resistin levels as predictor of low bone mineral density in postmenopausal women
Sundus Tariq, Saba Tariq, Saba Khaliq, Khalid Parvez Lone
Health Care for Women International.2021; 42(1): 82. CrossRef - Changes in bone mass associated with obesity and weight loss in humans: Applicability of animal models
Vivi F.H. Jensen, Anne-Marie Mølck, Majken Dalgaard, Fiona E. McGuigan, Kristina E. Akesson
Bone.2021; 145: 115781. CrossRef - Association of some dietary ingredients, vitamin D, estrogen, and obesity polymorphic receptor genes with bone mineral density in a sample of obese Egyptian women
Nayera E. Hassan, Salwa M. El Shebini, Sahar A. El-Masry, Nihad H. Ahmed, Ghada Nour Eldeen, Enas A. Rasheed, Manal M. Aly, Khhadija M. Alian, Mahmoud AS. Afify, Aya Khalil
Journal of Genetic Engineering and Biotechnology.2021; 19(1): 28. CrossRef - The obesity indices mediate the relationships of blood lipids and bone mineral density in Chinese elders
Bing Ge, Si-Qi Lu, Shu-Feng Lei
Molecular and Cellular Probes.2021; 56: 101705. CrossRef - Neurogenic Obesity and Skeletal Pathology in Spinal Cord Injury
David W. McMillan, Mark S. Nash, David R. Gater, Rodrigo J. Valderrábano
Topics in Spinal Cord Injury Rehabilitation.2021; 27(1): 57. CrossRef - The Influence of Stochastic Resonance Whole-Body Vibration on Women over 50 Years of Age—Preliminary Studies Based on Patients’ Own Experiences
Magdalena Hartman-Petrycka, Agata Lebiedowska, Anna Stolecka-Warzecha, Andrzej Szumski, Barbara Błońska-Fajfrowska
Applied Sciences.2021; 11(9): 3980. CrossRef - Growth hormone treatment and bone mineral density in pediatric patients with Prader–Willi syndrome
Yuji Oto, Nobuyuki Murakami, Takeshi Inoue, Keiko Matsubara, Sohei Saima, Hiroyuki Ogata, Hiroshi Ihara, Toshiro Nagai, Tomoyo Matsubara
Journal of Pediatric Endocrinology and Metabolism.2021; 34(9): 1181. CrossRef - Bone Mineral Density Changes during Weight Regain following Weight Loss with and without Exercise
Monica C. Serra, Alice S. Ryan
Nutrients.2021; 13(8): 2848. CrossRef - Obesity and Bone: A Complex Relationship
Giuseppe Rinonapoli, Valerio Pace, Carmelinda Ruggiero, Paolo Ceccarini, Michele Bisaccia, Luigi Meccariello, Auro Caraffa
International Journal of Molecular Sciences.2021; 22(24): 13662. CrossRef - A study on bone mass density using dual energy X-ray absorptiometry: Does high body mass index have protective effect on bone density in obese patients?
Azin Shayganfar, Shadi Ebrahimian, Mahsa Masjedi, Sadaf Daryaei
Journal of Research in Medical Sciences.2020; 25(1): 4. CrossRef - Relationship Between Metabolic Syndrome and Bone Fracture Risk in Mid-Aged Korean Women Using FRAX Scoring System
Hyun Joo Lee, Seo Yoon Hwang, Seung Chul Kim, Jong Kil Joo, Dong Soo Suh, Ki Hyung Kim
Metabolic Syndrome and Related Disorders.2020; 18(4): 219. CrossRef - The Skeletal Consequences of Bariatric Surgery
Alexandra N. Krez, Emily M. Stein
Current Osteoporosis Reports.2020; 18(3): 262. CrossRef - Association of obesity with bone mineral density and osteoporosis in adults: a systematic review and meta-analysis
D. Qiao, Y. Li, X. Liu, X. Zhang, X. Qian, H. Zhang, G. Zhang, C. Wang
Public Health.2020; 180: 22. CrossRef - Obesity and leptin influence vitamin D metabolism and action in human marrow stromal cells
Jing Li, Yuan Gao, Tao Yu, Jeffrey K. Lange, Meryl S. LeBoff, Anna Gorska, Simon Luu, Shuanhu Zhou, Julie Glowacki
The Journal of Steroid Biochemistry and Molecular Biology.2020; 198: 105564. CrossRef - Gender-specific prevalence and influencing factors of osteopenia and osteoporosis in Chinese rural population: the Henan Rural Cohort Study
Dou Qiao, Xiaotian Liu, Runqi Tu, Xia Zhang, Xinling Qian, Haiqing Zhang, Jingjing Jiang, zhongyan Tian, Yan Wang, Xiaokang Dong, Zhicheng Luo, Xue Liu, Huiling Tian, Gongyuan Zhang, Jun Pan, Chongjian Wang
BMJ Open.2020; 10(1): e028593. CrossRef - Association between Visceral Fat and Bone Mineral Density in Both Male and Female Patients with Adult Growth Hormone Deficiency
Linman Li, Li Zhong, Xiaoya Zheng, Wenyi You, Yunting Wang, Jihui Yu, Xun Wu, Wei Ren, Gangyi Yang
Biochemistry Research International.2020; 2020: 1. CrossRef - Association between non-Caucasian-specific ASCC1 gene polymorphism and osteoporosis and obesity in Korean postmenopausal women
Hye-Won Cho, Hyun-Seok Jin, Yong-Bin Eom
Journal of Bone and Mineral Metabolism.2020; 38(6): 868. CrossRef - BONE MINERAL DENSITY AND TRABECULAR BONE SCORE IN POSTMENOPAUSAL WOMEN WITH KNEE OSTEOARTHRITIS AND OBESITY
Vladyslav V. Povoroznyuk, Nataliia V. Zaverukha, Anna S. Musiienko
Wiadomości Lekarskie.2020; 73(3): 529. CrossRef - Obesity in Qatar: A Case-Control Study on the Identification of Associated Risk Factors
Md. Tawkat Islam Khondaker, Junaed Younus Khan, Mahmoud Ahmed Refaee, Nady El Hajj, M. Sohel Rahman, Tanvir Alam
Diagnostics.2020; 10(11): 883. CrossRef - Effect of Weight Loss via Severe vs Moderate Energy Restriction on Lean Mass and Body Composition Among Postmenopausal Women With Obesity
Radhika V. Seimon, Anthony L. Wild-Taylor, Shelley E. Keating, Sally McClintock, Claudia Harper, Alice A. Gibson, Nathan A. Johnson, Hamish A. Fernando, Tania P. Markovic, Jacqueline R. Center, Janet Franklin, Peter Y. Liu, Stuart M. Grieve, Jim Lagopoulo
JAMA Network Open.2019; 2(10): e1913733. CrossRef - Lipid profiles as potential mediators linking body mass index to osteoporosis among Chinese adults: the Henan Rural Cohort Study
D. Y. Wu, D. Qiao, X. Zhang, H. Q. Zhang, Z. C. Luo, Y. Wang, J. Pan, C. Wang
Osteoporosis International.2019; 30(7): 1413. CrossRef - ALVEOLAR BONE PATTERN AND SALIVARY LEPTIN LEVELS AMONG PREMENOPAUSAL OBESE WOMEN
Silvia Helena de Carvalho SALES-PERES, Francisco Carlos GROPPO, Rafaela Carolina Soares BONATO, Matheus de Carvalho SALES-PERES, Francisco HAITER-NETO, Elinton Adami CHAIM
ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo).2019;[Epub] CrossRef - Associations of obesity with osteoporosis and metabolic syndrome in Korean postmenopausal women: a cross-sectional study using national survey data
Hyun-Young Kim, Yunmi Kim
Archives of Osteoporosis.2019;[Epub] CrossRef - Analysis of bone mass and its relationship with body composition in school-aged children and adolescents based on stage of puberty and site specificity
Cui Song, Min Zhu, Rongfei Zheng, Yujuan Hu, Rong Li, Gaohui Zhu, Long Chen, Feng Xiong
Medicine.2019; 98(8): e14005. CrossRef - Influence of increased body mass index on orthodontic tooth movement and related parameters in children and adolescents: A systematic review of longitudinal controlled clinical studies
Dimitrios Michelogiannakis, P Emile Rossouw, Junad Khan, Zohaib Akram, Evangelos Menenakos, Fawad Javed
Journal of Orthodontics.2019; 46(4): 323. CrossRef - Metabolic Syndrome in Arab Adults with Low Bone Mineral Density
Kaiser Wani, Sobhy M. Yakout, Mohammed Ghouse Ahmed Ansari, Shaun Sabico, Syed Danish Hussain, Majed S. Alokail, Eman Sheshah, Naji J. Aljohani, Yousef Al-Saleh, Jean-Yves Reginster, Nasser M. Al-Daghri
Nutrients.2019; 11(6): 1405. CrossRef - The osteogenic effect of liraglutide involves enhanced mitochondrial biogenesis in osteoblasts
Subhashis Pal, Shailendra K. Maurya, Sourav Chattopadhyay, Shyamsundar Pal China, Konica Porwal, Chirag Kulkarni, Sabyasachi Sanyal, Rohit A. Sinha, Naibedya Chattopadhyay
Biochemical Pharmacology.2019; 164: 34. CrossRef - Lean Body Mass in the Prediction of Bone Mineral Density in Postmenopausal Women
Bolaji Lilian Ilesanmi-Oyelere, Jane Coad, Nicole Roy, Marlena Cathorina Kruger
BioResearch Open Access.2018; 7(1): 150. CrossRef - Postmenopausal osteoporosis and breast cancer: The biochemical links and beneficial effects of functional foods
Aliyu Muhammad, Sanusi Bello Mada, Ibrahim Malami, Gilead E. Forcados, Ochuko L. Erukainure, Hadiza Sani, Ibrahim Babangida Abubakar
Biomedicine & Pharmacotherapy.2018; 107: 571. CrossRef - Bone mineral density in midlife long-term users of hormonal contraception in South Africa: relationship with obesity and menopausal status
Mags E. Beksinska, Immo Kleinschmidt, Jenni A. Smit
Women's Midlife Health.2018;[Epub] CrossRef - Body fat has stronger associations with bone mass density than body mass index in metabolically healthy obesity
Yuan-Yuei Chen, Wen-Hui Fang, Chung-Ching Wang, Tung-Wei Kao, Yaw-Wen Chang, Chen-Jung Wu, Yi-Chao Zhou, Yu-Shan Sun, Wei-Liang Chen, Manlio Vinciguerra
PLOS ONE.2018; 13(11): e0206812. CrossRef - Prevalence and risk factors for osteoporosis and fractures in axial spondyloarthritis: A systematic review and meta-analysis
Julio Ramírez, Juan Carlos Nieto-González, Rafael Curbelo Rodríguez, Santos Castañeda, Loreto Carmona
Seminars in Arthritis and Rheumatism.2018; 48(1): 44. CrossRef - Prevalence of osteoporosis and osteopenia in an apparently healthy Indian population - a cross-sectional retrospective study
Neelam Kaushal, Divya Vohora, Rajinder K. Jalali, Sujeet Jha
Osteoporosis and Sarcopenia.2018; 4(2): 53. CrossRef - Metabolically healthy/unhealthy components may modify bone mineral density in obese people
Atieh Mirzababaei, Khadijeh Mirzaei, Leila Khorrami-nezhad, Zhila Maghbooli, Seyed Ali Keshavarz
Archives of Osteoporosis.2017;[Epub] CrossRef - Obesity and orthodontic treatment: is there any direct relationship?
Alberto Consolaro
Dental Press Journal of Orthodontics.2017; 22(3): 21. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Impact of Obesity on Orthodontic Tooth Movement in Adolescents: A Prospective Clinical Cohort Study
H.F. Saloom, S.N. Papageorgiou, G.H. Carpenter, M.T. Cobourne
Journal of Dental Research.2017; 96(5): 547. CrossRef
- The inter-relationship of the triad: osteoporosis, fracture risk, and obesity—a longitudinal multicenter analysis by the Egyptian Academy of Bone Health

- Clinical Study
- Urinary Albumin Excretion Reflects Cardiovascular Risk in Postmenopausal Women without Diabetes: The 2011 to 2013 Korean National Health and Nutrition Examination Survey
- Hee Jung Ahn, Do Sik Moon, Da Yeong Kang, Jung In Lee, Da Young Kim, Jin Hwa Kim, Sang Yong Kim, Hak Yeon Bae
- Endocrinol Metab. 2016;31(4):537-546. Published online November 3, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.537
- 3,571 View
- 31 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The objective of the current study was to determine whether there was an association between urinary albumin excretion and cardiovascular disease (CVD) risk by estimating the Framingham Risk Score (FRS) in postmenopausal women without diabetes.
Methods This study was based on data from the Korea National Health and Nutrition Examination Survey, which was conducted by the Korean Ministry of Health and Welfare in 2011 to 2013. Data on 2,316 postmenopausal women from a total of 24,594 participants was included in the analysis.
Results The mean FRS was significantly different in each of the urinary albumin to creatinine ratio (UACR) subgroups, and it increased with UACR. The FRS was 12.69±0.12 in the optimal group, 14.30±0.19 in the intermediate normal group, 14.62±0.26 in the high normal group, and 15.86±0.36 in the microalbuminuria group. After fully adjusting for potential confounding factors, high normal levels and microalbuminuria were significantly associated with the highest tertile of FRS ([odds ratio (OR), 1.642; 95% confidence interval (CI), 1.124 to 2.400] and [OR, 3.385; 95% CI, 2.088 to 5.488], respectively) compared with the optimal subgroup. High normal levels and microalbuminuria were also significantly associated with a ≥10% 10-year risk of CVD ([OR, 1.853; 95% CI, 1.122 to 3.060] and [OR, 2.831; 95% CI, 1.327 to 6.037], respectively) after adjusting for potential confounding covariates.
Conclusion Urinary albumin excretion reflects CVD risk in postmenopausal women without diabetes, and high normal levels and microalbuminuria were independently associated with a higher risk of CVD.
-
Citations
Citations to this article as recorded by- Association between urinary albumin creatinine ratio and cardiovascular disease
Yoo Jin Kim, Sang Won Hwang, Taesic Lee, Jun Young Lee, Young Uh, Gulali Aktas
PLOS ONE.2023; 18(3): e0283083. CrossRef - Relationship between Hypertension and the Declining Renal Function in Korean Adults
Jun Ho Lee
The Korean Journal of Clinical Laboratory Science.2021; 53(1): 32. CrossRef - Significance of Obstetrical History with Future Cardiovascular Disease Risk
Emmanuel Bassily, Cameron Bell, Sean Verma, Nidhi Patel, Aarti Patel
The American Journal of Medicine.2019; 132(5): 567. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Association between urinary albumin creatinine ratio and cardiovascular disease

- Clinical Study
- High Levels of Serum DPP-4 Activity Are Associated with Low Bone Mineral Density in Obese Postmenopausal Women
- Sang-Wook Kim, Eun-Hee Cho
- Endocrinol Metab. 2016;31(1):93-99. Published online March 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.1.93
- 3,495 View
- 39 Download
- 11 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase 4/CD26 (DPP-4) is a widely expressed cell surface serine protease. DPP-4 inhibitors, one of common anti-diabetic agents play a protective role in bone metabolism in recent studies. A soluble form of DPP-4 is found in serum, and exhibits DPP-4 enzymatic activity. However, the physiological role of serum or soluble DPP-4 and its relationship with DPP-4 enzymatic function remain poorly understood. The aims of current study were to determine the association between serum DPP-4 activity and bone mineral density (BMD) in postmenopausal women.
Methods We recruited data and serum samples from 124 consecutive healthy postmenopausal women aged >50 years. We divided study subjects into obese (body mass index [BMI] ≥25 kg/m2) and non-obese (BMI <25 kg/m2) postmenopausal women and examined the correlation between serum DPP-4 activity and clinical variables in each groups.
Results A total of 124 postmenopausal women was enrolled, with a mean age of 59.9±7.1 years. The mean BMI of the study patients was 24.4±2.8 kg/m2. Regarding bone turnover markers, serum DPP-4 activity was positively correlated with serum calcium concentrations, intact parathyroid hormone, and serum C-telopeptide levels in all of the study subjects. However, there was no association between serum DPP-4 activity and BMD in the spine or femoral neck in all of the study subjects. Serum DPP-4 activity was negatively correlated (
R =−0.288,P =0.038) with BMD of the spine in obese postmenopausal women.Conclusion This study demonstrated for the first time that serum soluble DPP-4 activity was negatively correlated with BMD in obese postmenopausal women.
-
Citations
Citations to this article as recorded by- A novel mechanism of Vildagliptin in regulating bone metabolism and mitigating osteoporosis
Jinwen He, Dacheng Zhao, Bo Peng, Xingwen Wang, Shenghong Wang, Xiaobing Zhao, Peng Xu, Bin Geng, Yayi Xia
International Immunopharmacology.2024; 130: 111671. CrossRef - Comparative evaluation of Sodium-glucose co-transporter-2 inhibitors and dipeptidyl peptidase-4 inhibitors influence on bone turnover markers in rats with experimental type 2 diabetes mellitus
N. V. Timkina, A. V. Simanenkova, T. L. Karonova, T. D. Vlasov, N. Yu. Semenova, А. A. Bairamov, V. A. Timofeeva, A. A. Shimshilashvili, E. V. Shlyakhto
Osteoporosis and Bone Diseases.2022; 24(4): 27. CrossRef - The relationship between bone marrow adipose tissue and bone metabolism in postmenopausal osteoporosis
Jiao Li, Xiang Chen, Lingyun Lu, Xijie Yu
Cytokine & Growth Factor Reviews.2020; 52: 88. CrossRef - Update on: effects of anti-diabetic drugs on bone metabolism
Guillaume Mabilleau, Béatrice Bouvard
Expert Review of Endocrinology & Metabolism.2020; 15(6): 415. CrossRef - Soluble Dipeptidyl Peptidase-4 Levels Are Associated with Decreased Renal Function in Patients with Type 2 Diabetes Mellitus
Eun-Hee Cho, Sang-Wook Kim
Diabetes & Metabolism Journal.2019; 43(1): 97. CrossRef - Marrow Adipose Tissue: Its Origin, Function, and Regulation in Bone Remodeling and Regeneration
Qiwen Li, Yunshu Wu, Ning Kang
Stem Cells International.2018; 2018: 1. CrossRef - Association between Serum Dipeptidyl Peptidase-4 Concentration and Obesity-related Factors in Health Screen Examinees
Ji Yeon Lee, Byoung Kuk Jang, Min Kyung Song, Hye Soon Kim, Mi-Kyung Kim
Journal of Obesity & Metabolic Syndrome.2017; 26(3): 188. CrossRef - Association of DPP-4 activity with BMD, body composition, and incident hip fracture: the Cardiovascular Health Study
L. D. Carbone, P. Bůžková, H. A. Fink, J. A. Robbins, M. Bethel, C. M. Isales, W. D. Hill
Osteoporosis International.2017; 28(5): 1631. CrossRef - Adipocyte Accumulation in the Bone Marrow during Obesity and Aging Impairs Stem Cell-Based Hematopoietic and Bone Regeneration
Thomas H. Ambrosi, Antonio Scialdone, Antonia Graja, Sabrina Gohlke, Anne-Marie Jank, Carla Bocian, Lena Woelk, Hua Fan, Darren W. Logan, Annette Schürmann, Luis R. Saraiva, Tim J. Schulz
Cell Stem Cell.2017; 20(6): 771. CrossRef - The emerging role of bone marrow adipose tissue in bone health and dysfunction
Thomas H. Ambrosi, Tim J. Schulz
Journal of Molecular Medicine.2017; 95(12): 1291. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Dipeptidyl Peptidase-4 and Adolescent Idiopathic Scoliosis: Expression in Osteoblasts
Emilie Normand, Anita Franco, Alain Moreau, Valérie Marcil
Scientific Reports.2017;[Epub] CrossRef - Effect of Dipeptidyl Peptidase-4 Inhibitors on Bone Metabolism and the Possible Underlying Mechanisms
Yinqiu Yang, Chenhe Zhao, Jing Liang, Mingxiang Yu, Xinhua Qu
Frontiers in Pharmacology.2017;[Epub] CrossRef
- A novel mechanism of Vildagliptin in regulating bone metabolism and mitigating osteoporosis

- The Effect of Hormone Replacement Therapy on Carotid Intima-Media Thickness in Healthy Postmenopausal Women.
- Jang Yel Shin, Bong Soo Cha, Choon Hee Chung, Won Heum Shim, Hyun Chul Lee
- J Korean Endocr Soc. 2006;21(1):14-21. Published online February 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.1.14
- 1,703 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cardiovascular disease is the leading cause of death in postmenopausal women. The use of hormone replacement therapy (HRT) preventing for cardiovascular disease in postmenopausal women remains controversial. We investigated the effect of HRT on carotid intima-media thickness (IMT) according to the HRT duration in healthy postmenopausal women. METHODS: One hundred and twenty postmenopausal women (mean age: 55.4 +/- 3.3 years) were classified into never users, short-term, and long-term users according to the HRT duration. Carotid IMT was measured, and the clinical and biochemical cardiovascular risk factors were examined. RESULTS: The mean IMT was significantly thinner in the long-term users than that in the never users (0.62 +/- 0.11 vs. 0.71 +/- 0.14 mm, P < 0.01). Also, the maximal IMT was significantly thinner in the short-term and the long-term users. However, there is no significant difference in the mean and maximal IMTs between the estrogen alone and estrogen plus progestins used group. The period exposed to menopause was significantly shorter in the long-term users than that in the never users (1.8 +/- 2.3 vs. 4.3 +/- 3.3 years, P < 0.001). CONCLUSION: Our findings suggest that if HRT is initiated during early postmenopausal period before the onset of atherosclerosis, HRT may have a beneficial effect on the prevention of carotid atherosclerosis.

- Association between Serum Leptin Concentration and Bone Mineral Density in Healthy Korean Women.
- Yumie Rhee, Dae Jung Kim, Se Hwa Kim, Chul Woo Ahn, Bong Soo Cha, Kyung Rae Kim, Hyun Chul Lee, Sung Kil Lim
- J Korean Endocr Soc. 2003;18(2):177-183. Published online April 1, 2003
- 1,107 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Leptin is known to affect bone metabolism both centrally and peripherally. This study was performed to investigate the relationship between leptin and bone mineral density(BMD) in healthy premenopausal and postmenopausal Korean women. METHODS: 140 women were recruited for a routine health check-up. Anthro-pometric and biochemical data were checked as usual. BMDs were measured by dual x-ray absorptiometry of the spine and femur in 67 premenopausal women and 73 postmenopausal women, in addition to their serum leptin levels. RESULTS: Serum leptin level showed no correlation with BMD in premenopausal women, but there was a positive correlation betwen serum leptin and spinal BMD in postmenopausal women(r=0.468, p<0.001). After the correcting for age, body mass index, and duration of menopause, the serum leptin level and BMD still showed a positive correlation(r=0.217, p=0.088) although weak. The women in the lowest quartile of serum leptin level showed significantly lower lumbar and femoral neck BMD. CONCLUSION: Leptin level seems to have a weak relationship with BMD showing different features in premenopausal and postmenopausal women.

- Changes of Biochemical Bone Markers and Bone Mineral Density after Hormone Replacement Therapy in Korean Women.
- Kyong Soo Park, Do Joon Park, Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee, Jae Hyeon Kim, Jeong Goo Kim
- J Korean Endocr Soc. 2000;15(2):226-236. Published online January 1, 2001
- 934 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Biochemical bone markers have been suggested to reflect postmenopausal high bone turnover. These markers could be useful in following response to hormone replacement therapy (HRT). But we have few studies about the sequential changes of biochemical bone markers and bone mass after HRT in Korean women, and it is unclear whether women with early menopause have different response to HRT from women with normal menopause. The aims of the present study were to see the sequential changes of biochemical bone markers and bone mass after HRT in Korean women, to examine whether a single baseline biochemical bone marker or a change in biochemical bone marker could predict subsequent bone mass, and to determine the difference of response to HRT between women with early menopause and women with normal menopause. METHODS: Postmenopausal women (n=21) were divided with into three groups according to their age at menopause (AAM): the first group with AAM < or = 43 years (early menopause group, n=7), the second group with 43 years < or = AAM < or = 50 years (n=4), and the third group with AAM > or = 50 years (normal menopause group, n=10). For the HRT, conjugated estrogen (0.625mg per day) and continuous or cyclic medroxyprogesterone (2.5-10mg per day) were administered. Bone mineral density (BMD) was measured at baseline and 12 months and biochemical bone markers were measured at baseline and 3, 6, and 12 months during HRT. RESULTS: Deoxypyridinoline, type 1 collagen N-telopeptide, bone alkaline phosphatase, and osteocalcin were significantly decreased at 3 months, and mean percent changes from baseline of bone resorption markers were larger than those of bone formation markers. At 12 months, BMD was significantly increased at lumbar spine and Ward's triangle. But BMD was not significantly increased at femur neck and femur trochanter. Two baseline bone markers (bone alkaline phosphatase and type 1 collagen N-telopeptide) correlated with changes of BMD but any changes of bone markers at 3, 6 months didn't correlate with changes of BMD. In early menopause group, changes of bone markers and BMD were larger than those in normal menopause group, but the difference between the two groups was not significant. CONCLUSION: All four bone markers showed significant reduction at 3 months, but bone resorption markers were decreased more markedly and rapidly, and some baseline bone markers can predict the change of BMD after HRT. The difference of response to HRT between early menopause group and normal menopause group was not significant.

- Association of Estrogen Receptor Genotypes with Serum Lipids and Responsiveness of Serum Lipids to Hormonal Replacement Therapy in Korean Postmenopausal Women.
- So Ra Park, Jae Eun Park, Chung Kyu Hwang, Phil Ho Jung, Chang Hoon Yim, Ho Yeon Chung, Ki Ok Han, Hyun Ku Yoon, Hak Chul Jang, In Kwon Han
- J Korean Endocr Soc. 1999;14(3):553-561. Published online January 1, 2001
- 1,059 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Several biologically plausible mechanisms have been proposed for estrogen-mediated caridoprotection, including estrogen-assocaited changes in lipid metabolism and endothelial function of vessel walls. These effects are thought to be mediated via estrogen receptor (ER). Relationships between ER polymorphisms and serum lipid levels were not investigated enoughly. METHODS: Three restriction fragment length polymorphisms (RFLPs) at the ER gene locus, represented as B-variant, PvuII and XbaI, and their relationship to serum lipid levels were examined in 318 postmenopausal women. Their mean age was 54.5+/-6.5 years (mean+SD). An association between ER genotypes and changes in lipid levels after 1 year of estrogen replacement therapy was also investigated in follow-up 251 women. RESULTS: The B-variant was not found in Korean women. The distribution of the PvuII and XbaI polymorphisms was as follows: PP 109 (34%), Pp 166 (52%), pp 43 (14%), and XX 204 (64%), Xx 95 (30%), xx 19 (6%). Significant relationship was found between genotypes and changes in serum total cholesterol levels after lyr estrogen replacement therapy. There was no significant relationship between ER genotypes and changes in HDL cholesterol, LDL cholesterol and triglyceride levels after estrogen therapy. CONCLUSION: These data indicate that these polymorphisms are possible predictor on lipid response to estrogen replacement therapy.

- Influence of Early Age at Menopause on Bone Mineral Density and Biochemical Bone Marker.
- Young Joo Park, Chan Soo Shin, Do Joon Park, Jung Koo Kim, Sung Yeon Kim, Bo Yeon Cho, Hong Gyu Lee, Jae Hyun Kim, In Kyung Chung
- J Korean Endocr Soc. 1999;14(2):346-354. Published online January 1, 2001
- 1,163 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Among the various factors affecting bone mass and bone metabolism, aging and menopause play a major role. After the disappearance of the menstrual cycle, estrogen deficiency is the most important factor in bone loss. It is still unclear whether women with early menopause have a rate of bone loss different from women whose menopause has occurred later. Various biochemical bone markers are increased after menopause but it is still unclear whether women with early menopause have biochemical bone markers different from women whose menopause has occurred later. The aim of this study was to establish whether healthy women with early or normal menopause have different bone mass, biochemical bone markers and rates of bone loss. METHODS: Postmenopausal healthy women were divided into two groups according to their age at menopause(AAM): one group with AAM > 43 years, and the other group with AAM 50 years. Bone mass was measured using a dual energy X-ray absorptiometry(DEXA) in the lumbar, femur neck, femur trochanter, and Wards triangle. Serum levels of bone alkaline phosphatase and osteocalcin, and urine levels of calcium, deoxypyridinoline and type I collagen N-telopeptide were measured using a commercial kit. RESULTS: Age and body mass index in the early menopause group were different from those in the normal menopause group. All the bone mass and the biochemical bone markers in the early menopause group were not different from those in the normal menopause group. We selected 15 subjects from the two groups matched by age and BML Bone mass of femur neck in the early menopause group was lower than in the normal menopause group matched by age and BMI. Bone mass in lumbar, femur trochanter, and Wards triangle was lower in the early menopause group than in the normal menopause group, but the difference between the two groups was not significant. After adjusting years since menopause, we didnt find the difference of bone mass between the two groups. All the bone biochemical markers were not different in the two groups matched by age and BMI. CONCLUSION: Our data suggest that women with early menopause dont lose bone faster than women with normal menopause.

- The Repreducitve History and Other Potential Risk Factors as The Determinants of Bone Mineral Density at Postmenopause.
- Min Kyung Song, Young Jun Won, Suk Won Park, Young Duk Song, Sung Kil Lim, Jae Jun Oh, Hyun Chul Lee, Kap Bum Huh
- J Korean Endocr Soc. 1999;14(1):91-101. Published online January 1, 2001
- 1,006 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The purpose of this study was to determine the associations of the potential risk factors including reproductive history and lifestyle factors with bone mineral density at postmenopause. METHODS: The bone mineral density of the lumbar spine and proximal femur were measured by dual energy X-ray absorptiometry (DEXA), and physical and anthropometric data were obtained in 187 healthy postmenopausal women aged 45 to 73. Informations about risk factors were assessed by questionairres including medicosurgical and family history, reproductive history and lifestyle factors (dietary calcium intake, past use of oral contraceptives, consumption of alcohol and caffeine, smoking habits and exercise pattern). RESULTS: 1) Each prevalence of osteopenia and osteoporosis was 43.9% and 16.6% in postmenopausal women. 2) In simple correlation analysis between each risk factor and bone mineral density, factors associated with higher level in body mineral density (BMD) were body mass index (BMI)(p<0.01) and reproductive periods (p<0.05) in lumar spine and femur neck, and exerecise strength in femur neck (p<0.05). On the other hand, more aging and longer postmnopausal periods, lower BMD in lumbar spine and femur (p<0.01) and later menarche, lower BMD in lumbar spine (p<0.01) and femur neck (p<0.05) and higher frequencies of parity were influenced on lower BMD in lumbar spine and femur wards (p<0.01) and femur neck (p<0.05). But the other factors had no relation to BMD. 3) There was no significant difference in BMD according to the amount of diet calcium intake, gravity, lactation, the past use of oral contraceptives, the family history of osteoporosis, smoking habits and intake of caffeine and alcohol. 4) No reproductive history and other risk factors were significantly associated with BMD after the influences of age, postmenopausal periods and BMI were adjusted in multiple regression analysis. CONCLUSION: These results show there are no consistent effects on bone mineral density, after adjusting for age and BMI, of reproductive history and any other risk factors in postmenopausal women.


 KES
KES

 First
First Prev
Prev



