Most view
- Page Path
- HOME > BROWSE ARTICLES > Most view
Most-read articles are from the articles published in 2022 during the last three month.
Original Article
- Diabetes, Obesity and Metabolism
- Effect of the Concomitant Use of Subcutaneous Basal Insulin and Intravenous Insulin Infusion in the Treatment of Severe Hyperglycemic Patients
- Yejee Lim, Jung Hun Ohn, Joo Jeong, Jiwon Ryu, Sun-wook Kim, Jae Ho Cho, Hee-Sun Park, Hye Won Kim, Jongchan Lee, Eun Sun Kim, Nak-Hyun Kim, You Hwan Jo, Hak Chul Jang
- Endocrinol Metab. 2022;37(3):444-454. Published online June 3, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1341
- 59,025 View
- 240 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
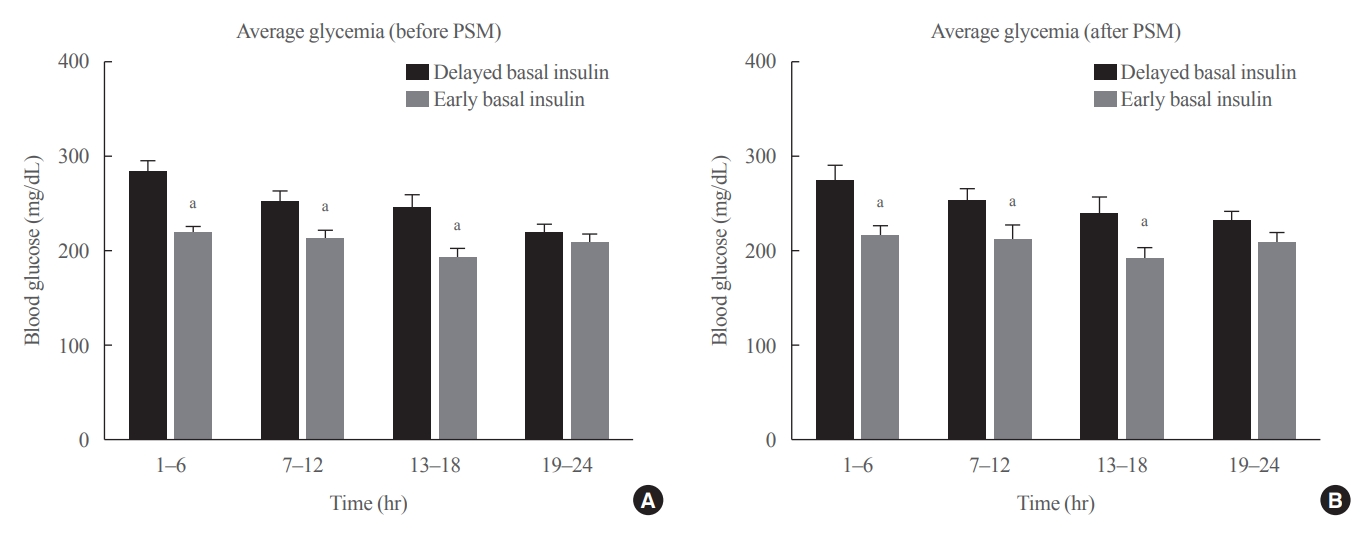
No consensus exists regarding the early use of subcutaneous (SC) basal insulin facilitating the transition from continuous intravenous insulin infusion (CIII) to multiple SC insulin injections in patients with severe hyperglycemia other than diabetic ketoacidosis. This study evaluated the effect of early co-administration of SC basal insulin with CIII on glucose control in patients with severe hyperglycemia.
Methods
Patients who received CIII for the management of severe hyperglycemia were divided into two groups: the early basal insulin group (n=86) if they received the first SC basal insulin 0.25 U/kg body weight within 24 hours of CIII initiation and ≥4 hours before discontinuation, and the delayed basal insulin group (n=79) if they were not classified as the early basal insulin group. Rebound hyperglycemia was defined as blood glucose level of >250 mg/dL in 24 hours following CIII discontinuation. Propensity score matching (PSM) methods were additionally employed for adjusting the confounding factors (n=108).
Results
The rebound hyperglycemia incidence was significantly lower in the early basal insulin group than in the delayed basal insulin group (54.7% vs. 86.1%), despite using PSM methods (51.9%, 85.2%). The length of hospital stay was shorter in the early basal insulin group than in the delayed basal insulin group (8.5 days vs. 9.6 days, P=0.027). The hypoglycemia incidence did not differ between the groups.
Conclusion
Early co-administration of basal insulin with CIII prevents rebound hyperglycemia and shorten hospital stay without increasing the hypoglycemic events in patients with severe hyperglycemia. -
Citations
Citations to this article as recorded by- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024
Nuha A. ElSayed, Grazia Aleppo, Raveendhara R. Bannuru, Dennis Bruemmer, Billy S. Collins, Laya Ekhlaspour, Rodolfo J. Galindo, Marisa E. Hilliard, Eric L. Johnson, Kamlesh Khunti, Ildiko Lingvay, Glenn Matfin, Rozalina G. McCoy, Mary Lou Perry, Scott J.
Diabetes Care.2024; 47(Supplement): S295. CrossRef - 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2023
Nuha A. ElSayed, Grazia Aleppo, Vanita R. Aroda, Raveendhara R. Bannuru, Florence M. Brown, Dennis Bruemmer, Billy S. Collins, Marisa E. Hilliard, Diana Isaacs, Eric L. Johnson, Scott Kahan, Kamlesh Khunti, Jose Leon, Sarah K. Lyons, Mary Lou Perry, Priya
Diabetes Care.2023; 46(Supplement): S267. CrossRef - Effectiveness and safety of early insulin glargine administration in combination with continuous intravenous insulin infusion in the management of diabetic ketoacidosis: A randomized controlled trial
Kitti Thammakosol, Chutintorn Sriphrapradang
Diabetes, Obesity and Metabolism.2023; 25(3): 815. CrossRef
- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024

Review Articles
- Thyroid
- Update from the 2022 World Health Organization Classification of Thyroid Tumors: A Standardized Diagnostic Approach
- Chan Kwon Jung, Andrey Bychkov, Kennichi Kakudo
- Endocrinol Metab. 2022;37(5):703-718. Published online October 4, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1553
- 16,408 View
- 2,112 Download
- 48 Web of Science
- 65 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
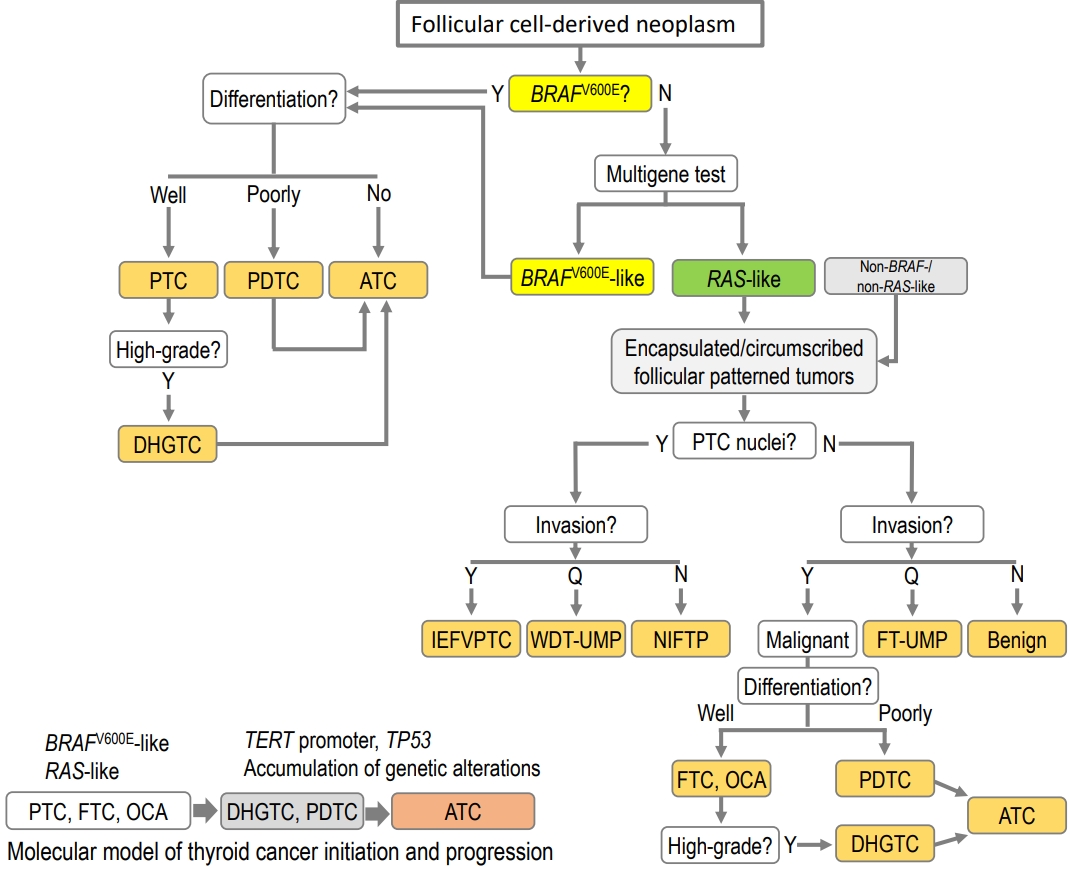
ePub - The fifth edition of the World Health Organization (WHO) histologic classification of thyroid neoplasms released in 2022 includes newly recognized tumor types, subtypes, and a grading system. Follicular cell-derived neoplasms are categorized into three families (classes): benign tumors, low-risk neoplasms, and malignant neoplasms. The terms “follicular nodular disease” and “differentiated high-grade thyroid carcinoma” are introduced to account for multifocal hyperplastic/neoplastic lesions and differentiated thyroid carcinomas with high-grade features, respectively. The term “Hürthle cells” is replaced with “oncocytic cells.” Invasive encapsulated follicular and cribriform morular variants of papillary thyroid carcinoma (PTC) are now redefined as distinct tumor types, given their different genetic alterations and clinicopathologic characteristics from other PTC subtypes. The term “variant” to describe a subclass of tumor has been replaced with the term “subtype.” Instead, the term “variant” is reserved to describe genetic alterations. A histologic grading system based on the mitotic count, necrosis, and/or the Ki67 index is used to identify high-grade follicular-cell derived carcinomas and medullary thyroid carcinomas. The 2022 WHO classification introduces the following new categories: “salivary gland-type carcinomas of the thyroid” and “thyroid tumors of uncertain histogenesis.” This review summarizes the major changes in the 2022 WHO classification and their clinical relevance.
-
Citations
Citations to this article as recorded by- Tumeurs de la thyroïde : nouveautés de la classification OMS 2022
Serge Guyétant, Myriam Decaussin Petrucci, Emmanuelle Leteurtre
Annales de Pathologie.2024; 44(1): 5. CrossRef - Diagnostic Performance of [18F]TFB PET/CT Compared with Therapeutic Activity [131I]Iodine SPECT/CT and [18F]FDG PET/CT in Recurrent Differentiated Thyroid Carcinoma
David Ventura, Matthias Dittmann, Florian Büther, Michael Schäfers, Kambiz Rahbar, Daniel Hescheler, Michael Claesener, Philipp Schindler, Burkhard Riemann, Robert Seifert, Wolfgang Roll
Journal of Nuclear Medicine.2024; 65(2): 192. CrossRef - Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy
Wen Liu, Beibei Jiang, Jingli Xue, Ruijing Liu, Yuqing Wei, Peifeng Li
Annals of Diagnostic Pathology.2024; 69: 152243. CrossRef - Management of aggressive variants of papillary thyroid cancer
Ying Ki Lee, Aleix Rovira, Paul V. Carroll, Ricard Simo
Current Opinion in Otolaryngology & Head & Neck Surgery.2024; 32(2): 125. CrossRef - Artificial Intelligence Detected the Relationship Between Nuclear Morphological Features and Molecular Abnormalities of Papillary Thyroid Carcinoma
Toui Nishikawa, Ibu Matsuzaki, Ayata Takahashi, Iwamoto Ryuta, Fidele Yambayamba Musangile, Kanako Sagan, Mizuki Nishikawa, Yurina Mikasa, Yuichi Takahashi, Fumiyoshi Kojima, Shin-ichi Murata
Endocrine Pathology.2024; 35(1): 40. CrossRef - Review of the 2023 World Congress on Thyroid Cancer (WCTC 2023, London): is there light at the end of the tunnel for patients with neglected cancer?
S.M. Cherenko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2024; 19(8): 609. CrossRef - Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma
Lindsay A. Bischoff, Ian Ganly, Laura Fugazzola, Erin Buczek, William C. Faquin, Bryan R. Haugen, Bryan McIver, Caitlin P. McMullen, Kate Newbold, Daniel J. Rocke, Marika D. Russell, Mabel Ryder, Peter M. Sadow, Eric Sherman, Maisie Shindo, David C. Shonk
JAMA Otolaryngology–Head & Neck Surgery.2024; 150(3): 265. CrossRef - Malignancy in a Solitary Thyroid Nodule: A Retrospective Histopathological Evaluation
Hassan Alzahrani
International Journal of General Medicine.2024; Volume 17: 135. CrossRef - Pathologie thyroïdienne. Actualités et problèmes pratiques. Introduction
Serge Guyétant
Annales de Pathologie.2024; 44(2): 90. CrossRef - Diagnostic implication of thyroid spherules for cytological diagnosis of thyroid nodules
Heeseung Sohn, Kennichi Kakudo, Chan Kwon Jung
Cytopathology.2024; 35(3): 383. CrossRef - Aggressive Primary Thyroid Mucoepidermoid Carcinoma with Extensive Pulmonary Involvement
Marius Mitrache, Dana Terzea, Anca Sirbu, Simona Fica
Biomedicines.2024; 12(2): 285. CrossRef - Unravelling the role of long non-coding RNAs in modulating the Hedgehog pathway in cancer
Shailendra Singh Chandel, Anurag Mishra, Gaurav Dubey, Ravindra Pal Singh, Mithilesh Singh, Mohit Agarwal, Himmat Singh Chawra, Neelima Kukreti
Pathology - Research and Practice.2024; 254: 155156. CrossRef - Hürthle cell (Oncocytic) carcinoma – Is hemithyroidectomy enough?
Taylor O. Julsrud, Trenton R. Foster, Robert A. Vierkant, Melanie L. Lyden, Travis J. McKenzie, Mabel Ryder, Benzon M. Dy
Surgical Oncology Insight.2024; 1(1): 100010. CrossRef - Échographie des carcinomes thyroïdiens différenciés de souche folliculaire
P.Y. Marcy, M. Tassart, J.G. Marchand, J. Sanglier, A. Bizeau, E. Ghanassia
Journal d'imagerie diagnostique et interventionnelle.2024; 7(2): 54. CrossRef - Differentiating BRAF V600E- and RAS-like alterations in encapsulated follicular patterned tumors through histologic features: a validation study
Chankyung Kim, Shipra Agarwal, Andrey Bychkov, Jen-Fan Hang, Agnes Stephanie Harahap, Mitsuyoshi Hirokawa, Kennichi Kakudo, Somboon Keelawat, Chih-Yi Liu, Zhiyan Liu, Truong Phan-Xuan Nguyen, Chanchal Rana, Huy Gia Vuong, Yun Zhu, Chan Kwon Jung
Virchows Archiv.2024;[Epub] CrossRef - Cas no5. High-grade Tall cell papillary carcinoma
Myriam Decaussin-Petrucci
Annales de Pathologie.2024; 44(2): 114. CrossRef - Current and future of immunotherapy for thyroid cancer based on bibliometrics and clinical trials
Ke Wang, Ying Zhang, Yang Xing, Hong Wang, Minghua He, Rui Guo
Discover Oncology.2024;[Epub] CrossRef - Cas no6. Anaplastic thyroid carcinoma, epidermoid subtype
Myriam Decaussin-Petrucci
Annales de Pathologie.2024; 44(2): 120. CrossRef - Papillary Thyroid Carcinoma With Lymphoepithelial Features and Lacking Association With Epstein-Barr Virus (EBV): A Rare Case
Ahmed Bendari, Saroja Devi Geetha, Reham Al-Refai, Xuelin Zhong, Sunder Sham, Manju Harshan
Cureus.2024;[Epub] CrossRef - Clinical and morphological features and unsolved issues in diagnosis of aggressive forms of papillary thyroid carcinoma
Denis V. Korotovsky, Sergey V. Sergiiko, Sergey A. Lukyanov
Perm Medical Journal.2024; 41(1): 90. CrossRef - Finding possible diagnostic markers for differentiating benign and malignant thyroid tumors on example investigate of rheological properties1
I. Javakhishvili, T. Sanikidze, K. Mardaleishvili, N. Momtselidze, T. Urdulashvili, M. Mantskava, L. Prantl, F. Jung
Clinical Hemorheology and Microcirculation.2024; : 1. CrossRef - Unraveling the Significance of DGCR8 and miRNAs in Thyroid Carcinoma
Lia Rodrigues, Arnaud Da Cruz Paula, Paula Soares, João Vinagre
Cells.2024; 13(7): 561. CrossRef - Management of Poorly Differentiated Thyroid Cancer and Differentiated High-Grade Thyroid Carcinoma
Iram S. Alam, Kepal N. Patel
Surgical Clinics of North America.2024;[Epub] CrossRef - What’s new in thyroid pathology 2024: updates from the new WHO classification and bethesda system
Andrey Bychkov, Chan Kwon Jung
Journal of Pathology and Translational Medicine.2024; 58(2): 98. CrossRef - Ultrasound–Histopathological Presentation of Thyroid and Ovary Lesions in Adolescent Patients with DICER1 Syndrome: Case Reports and Literature Overview
Dominika Januś, Monika Kujdowicz, Konrad Kaleta, Kamil Możdżeń, Jan Radliński, Anna Taczanowska-Niemczuk, Aleksandra Kiszka-Wiłkojć, Marcin Maślanka, Wojciech Górecki, Jerzy B. Starzyk
Children.2024; 11(4): 403. CrossRef - Surgical treatment of solid variant of papillary thyroid carcinoma: Fifteen-year experience of a tertiary center
Katarina Tausanović, Marina Stojanović, Milan Jovanović, Boban Stepanović, Jovan Ilić, Sara Ivaniš, Vladan Živaljević
Medicinska istrazivanja.2024; 57(1): 121. CrossRef - Critical appraisal of the WHO 2022 classification of thyroid cancer
Mithraa Devi Sekar, Debasis Gochhait, Sadishkumar Kamalanathan
Thyroid Research and Practice.2024; 20(1): 8. CrossRef - Patterns in the Reporting of Aggressive Histologic Subtypes in Papillary Thyroid Cancer
Yeon J. Lee, Caitlin E. Egan, Jacques A. Greenberg, Teagan Marshall, Abhinay Tumati, Brendan M. Finnerty, Toni Beninato, Rasa Zarnegar, Thomas J. Fahey, Minerva A. Romero Arenas
Journal of Surgical Research.2024; 298: 325. CrossRef - Update on C-Cell Neuroendocrine Neoplasm: Prognostic and Predictive Histopathologic and Molecular Features of Medullary Thyroid Carcinoma
Chan Kwon Jung, Shipra Agarwal, Jen-Fan Hang, Dong-Jun Lim, Andrey Bychkov, Ozgur Mete
Endocrine Pathology.2023; 34(1): 1. CrossRef - The 5th edition of WHO classification of tumors of endocrine organs: changes in the diagnosis of follicular-derived thyroid carcinoma
Fulvio Basolo, Elisabetta Macerola, Anello Marcello Poma, Liborio Torregrossa
Endocrine.2023; 80(3): 470. CrossRef - Preoperative Risk Stratification of Follicular-patterned Thyroid Lesions on Core Needle Biopsy by Histologic Subtyping and RAS Variant-specific Immunohistochemistry
Meejeong Kim, Sora Jeon, Chan Kwon Jung
Endocrine Pathology.2023; 34(2): 247. CrossRef - Ultrasound evolution of parenchymal changes in the thyroid gland with autoimmune thyroiditis in children prior to the development of papillary thyroid carcinoma – a follow-up study
Dominika Januś, Monika Kujdowicz, Małgorzata Wójcik, Anna Taczanowska-Niemczuk, Aleksandra Kiszka-Wiłkojć, Wojciech Górecki, Jerzy B. Starzyk
Frontiers in Endocrinology.2023;[Epub] CrossRef - Papillary thyroid carcinoma with aggressive fused follicular and solid growth pattern: A unique histological subtype with high‐grade malignancy?
Shin‐ichi Murata, Ibu Matsuzaki, Mitsuo Kishimoto, Naomi Katsuki, Toshinori Onishi, Mitsuyoshi Hirokawa, Fumiyoshi Kojima
Pathology International.2023; 73(5): 207. CrossRef - Multi-Omics and Management of Follicular Carcinoma of the Thyroid
Thifhelimbilu Emmanuel Luvhengo, Ifongo Bombil, Arian Mokhtari, Maeyane Stephens Moeng, Demetra Demetriou, Claire Sanders, Zodwa Dlamini
Biomedicines.2023; 11(4): 1217. CrossRef - Molecular Genetics of Diffuse Sclerosing Papillary Thyroid Cancer
Meshael Alswailem, Balgees Alghamdi, Anwar Alotaibi, Abeer Aljomiah, Hindi Al-Hindi, Avaniyapuram Kannan Murugan, Mohamed Abouelhoda, Yufei Shi, Ali S Alzahrani
The Journal of Clinical Endocrinology & Metabolism.2023; 108(9): e704. CrossRef - Multifunctional Phase-Transition Nanoparticles for Effective Targeted Sonodynamic-Gene Therapy Against Thyroid Papillary Carcinoma
Shihui Guan, Dengke Teng, Hui Wang, Qimeihui Wang, Xi Zhen, Guoqing Sui, Yang Wang, Lingyu Zhu, Yuanqiang Lin, Dan Jiao, Feng Guo
International Journal of Nanomedicine.2023; Volume 18: 2275. CrossRef - Utilizing Dynamic Risk Stratification in Patients With Tall Cell Variant Papillary Thyroid Cancer
David Zimmer, Gilman Plitt, Brandon Prendes, Jamie Ku, Natalie Silver, Eric Lamarre, Emrullah Yilmaz, Jessica Geiger, Christian Nasr, Lea El Hage, Mario Skugor, Shauna Cambpell, Shlomo Koyfman, Jacob Miller, Neil Woody, Katherine Heiden, Nikhil Joshi, Tar
The Laryngoscope.2023; 133(9): 2430. CrossRef - Ultrasound, laboratory and histopathological insights in diagnosing papillary thyroid carcinoma in a paediatric population: a single centre follow-up study between 2000-2022
Dominika Januś, Małgorzata Wójcik, Anna Taczanowska-Niemczuk, Aleksandra Kiszka-Wiłkojć, Monika Kujdowicz, Małgorzata Czogała, Wojciech Górecki, Jerzy B. Starzyk
Frontiers in Endocrinology.2023;[Epub] CrossRef - Medullary Thyroid Carcinoma: A Single Institute Experience
Sonal Trivedi, T. Salahuddin, Mohamed Taher Mithi, Priyank Rathod, Arpit Bandi, Shashank J. Pandya, Mohit Sharma, Shailesh Patel, Vikas Warikoo, Ketul Puj, Abhijeet Salunkhe, Keval Patel, Shivam Pandya
Indian Journal of Otolaryngology and Head & Neck Surgery.2023; 75(4): 2884. CrossRef - FNAC (Fine needle aspiration cytology) and histopathological correlation and reclassification of thyroid neoplasm in accordance with WHO classification 2022
Fareeda Joshi, Shreya Hegde
Indian Journal of Pathology and Oncology.2023; 10(2): 132. CrossRef - Papillary thyroid carcinoma associated with non‑functioning parathyroid carcinoma with Warthin's tumor of the parotid gland: A case report and brief literature review
Ari Abdullah, Aras Qaradakhy, Yadgar Saeed, Abdulwahid Salih, Seema Karim, Osama Ali, Shko Hassan, Shalaw Nasraldeen, Shvan Mohammed, Fahmi Kakamad
Medicine International.2023;[Epub] CrossRef - Warthin-like papillary thyroid carcinoma: a case report and comprehensive review of the literature
Abdel Mouhaymen Missaoui, Fatma Hamza, Wafa Belabed, Manel Mellouli, Mohamed Maaloul, Slim Charfi, Issam Jardak, Tahya Sellami-Boudawara, Nabila Rekik, Mohamed Abid
Frontiers in Endocrinology.2023;[Epub] CrossRef - Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
Chan Kwon Jung
Journal of Pathology and Translational Medicine.2023; 57(4): 208. CrossRef - Cancer Predisposition Syndromes and Thyroid Cancer: Keys for a Short Two-Way Street
Ioana Balinisteanu, Monica-Cristina Panzaru, Lavinia Caba, Maria-Christina Ungureanu, Andreea Florea, Ana Maria Grigore, Eusebiu Vlad Gorduza
Biomedicines.2023; 11(8): 2143. CrossRef - Deep learning prediction model for central lymph node metastasis in papillary thyroid microcarcinoma based on cytology
Wenhao Ren, Yanli Zhu, Qian Wang, Yuntao Song, Zhihui Fan, Yanhua Bai, Dongmei Lin
Cancer Science.2023; 114(10): 4114. CrossRef - Cytology and Histology of Thyroid Nodules: Exploring Novel Insights in the Molecular Era for Enhanced Patient Management
Beatrix Cochand-Priollet, Zahra Maleki
Current Oncology.2023; 30(8): 7753. CrossRef - Agrin is a novel oncogenic protein in thyroid cancer
Anna Adamiok‑Ostrowska, Małgorzata Grzanka, Barbara Czarnocka
Oncology Letters.2023;[Epub] CrossRef - Analysis of Pathological Features of Thyroid Carcinoma in the Western Yunnan
身吾 王
Advances in Clinical Medicine.2023; 13(10): 15820. CrossRef - Insight of novel biomarkers for papillary thyroid carcinoma through multiomics
Wei Liu, Junkan Zhu, Zhen Wu, Yongxiang Yin, Qiao Wu, Yiming Wu, Jiaojiao Zheng, Cong Wang, Hongyan Chen, Talal Jamil Qazi, Jun Wu, Yuqing Zhang, Houbao Liu, Jingmin Yang, Daru Lu, Xumin Zhang, Zhilong Ai
Frontiers in Oncology.2023;[Epub] CrossRef - Identification of NIFTP-Specific mRNA Markers for Reliable Molecular Diagnosis of Thyroid Tumors
So-Yeon Lee, Jong-Lyul Park, Kwangsoon Kim, Ja Seong Bae, Jae-Yoon Kim, Seon-Young Kim, Chan Kwon Jung
Endocrine Pathology.2023; 34(3): 311. CrossRef - Somatostatin Receptor Type 2 and Thyroid-Stimulating Hormone Receptor Expression in Oncocytic Thyroid Neoplasms: Implications for Prognosis and Treatment
Andrea Gillis, Rui Zheng-Pywell, Chandler McLeod, Dezhi Wang, John M. Ness, Rachael Guenter, Jason Whitt, Tomas A. Prolla, Herbert Chen, Manuel Lora Gonzalez, Bart Rose, Ricardo V. Lloyd, Renata Jaskula-Sztul, Diana Lin
Modern Pathology.2023; 36(12): 100332. CrossRef - Comparison of Treatment and Prognosis Between Follicular Variant
Papillary Thyroid Carcinoma and Classical Papillary Thyroid
Carcinoma
Bing Zhang, Wenming Wu, Jinjing Liu, Zhou Liang, Liang Zong
Hormone and Metabolic Research.2023; 55(12): 855. CrossRef - Sentinel lymph node mapping: current applications and future perspectives in thyroid carcinoma
Isabella Merante Boschin, Loris Bertazza, Carla Scaroni, Caterina Mian, Maria Rosa Pelizzo
Frontiers in Medicine.2023;[Epub] CrossRef - Utility of the Growth Differentiation Factor-15 in the Differential Diagnosis of Follicular-Patterned Lesions of the Thyroid on Cytopathologic and Histopathologic Samples
Prasanna V Perumal, Neelaiah Siddaraju, Sunil K Saxena, Soundravally Rajendiran, Ramachandra V Bhat
Cureus.2023;[Epub] CrossRef - Investigation of pre‐operative demographic, biochemical, sonographic and cytopathological findings in low‐risk thyroid neoplasms
Muzaffer Serdar Deniz, Didem Özdemir, Narin Nasıroğlu İmga, Hüsniye Başer, Fatma Neslihan Çuhacı Seyrek, Ayşegül Aksoy Altınboğa, Oya Topaloğlu, Reyhan Ersoy, Bekir Çakır
Clinical Endocrinology.2023; 99(5): 502. CrossRef - Applications of machine and deep learning to thyroid cytology and histopathology: a review
Greg Slabaugh, Luis Beltran, Hasan Rizvi, Panos Deloukas, Eirini Marouli
Frontiers in Oncology.2023;[Epub] CrossRef - The Asian Thyroid Working Group, from 2017 to 2023
Kennichi Kakudo, Chan Kwon Jung, Zhiyan Liu, Mitsuyoshi Hirokawa, Andrey Bychkov, Huy Gia Vuong, Somboon Keelawat, Radhika Srinivasan, Jen-Fan Hang, Chiung-Ru Lai
Journal of Pathology and Translational Medicine.2023; 57(6): 289. CrossRef - Anaplastic thyroid cancer: Pathogenesis, prognostic factors and genetic landscape (Review)
Abdul-Mohsen Alhejaily, Omar Alhuzim, Yazeed Alwelaie
Molecular and Clinical Oncology.2023;[Epub] CrossRef - Simultaneous Occurrence of Medullary Thyroid Carcinoma and Papillary Thyroid Carcinoma: A Case Series with Literature Review
Poupak Fallahi, Armando Patrizio, Giulio Stoppini, Giusy Elia, Francesca Ragusa, Sabrina Rosaria Paparo, Eugenia Balestri, Valeria Mazzi, Chiara Botrini, Gilda Varricchi, Salvatore Ulisse, Marco Ghionzoli, Alessandro Antonelli, Silvia Martina Ferrari
Current Oncology.2023; 30(12): 10237. CrossRef - Construction and validation of a nomogram for predicting cervical lymph node metastasis in diffuse sclerosing variant of papillary thyroid carcinoma
Xunyi Lin, Jiaxing Huo, Huan Zhang, Hang Su, Fenghua Zhang
Langenbeck's Archives of Surgery.2023;[Epub] CrossRef - Canine follicular cell and medullary thyroid carcinomas: Immunohistochemical characterization
Jana Jankovic, Eve Tièche, Martina Dettwiler, Kerstin Hahn, Stephanie Scheemaeker, Martin Kessler, Sylvie Daminet, Sven Rottenberg, Miguel Campos
Veterinary Pathology.2023;[Epub] CrossRef - A 16-Year Single-Center Series of Trachea Resections for Locally Advanced Thyroid Carcinoma
Julia I. Staubitz-Vernazza, Sina Schwind, Oana Lozan, Thomas J. Musholt
Cancers.2023; 16(1): 163. CrossRef - Reprogramming of Cellular Metabolism and Its Therapeutic Applications in Thyroid Cancer
Yuji Nagayama, Koichiro Hamada
Metabolites.2022; 12(12): 1214. CrossRef - Developments to improve outcomes in thyroid surgery
Thomas J. Musholt
Innovative Surgical Sciences.2022; 7(3-4): 77. CrossRef - The relationship of the clinicopathological characteristics and treatment results of post-Chornobyl papillary thyroid microcarcinomas with the latency period and radiation exposure
Tetiana Bogdanova, Serhii Chernyshov, Liudmyla Zurnadzhy, Tatiana I. Rogounovitch, Norisato Mitsutake, Mykola Tronko, Masahiro Ito, Michael Bolgov, Sergii Masiuk, Shunichi Yamashita, Vladimir A. Saenko
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Tumeurs de la thyroïde : nouveautés de la classification OMS 2022

- Diabetes, Obesity and Metabolism
- Recent Updates to Clinical Practice Guidelines for Diabetes Mellitus
- Jin Yu, Seung-Hwan Lee, Mee Kyoung Kim
- Endocrinol Metab. 2022;37(1):26-37. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.105
- 17,070 View
- 1,147 Download
- 22 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
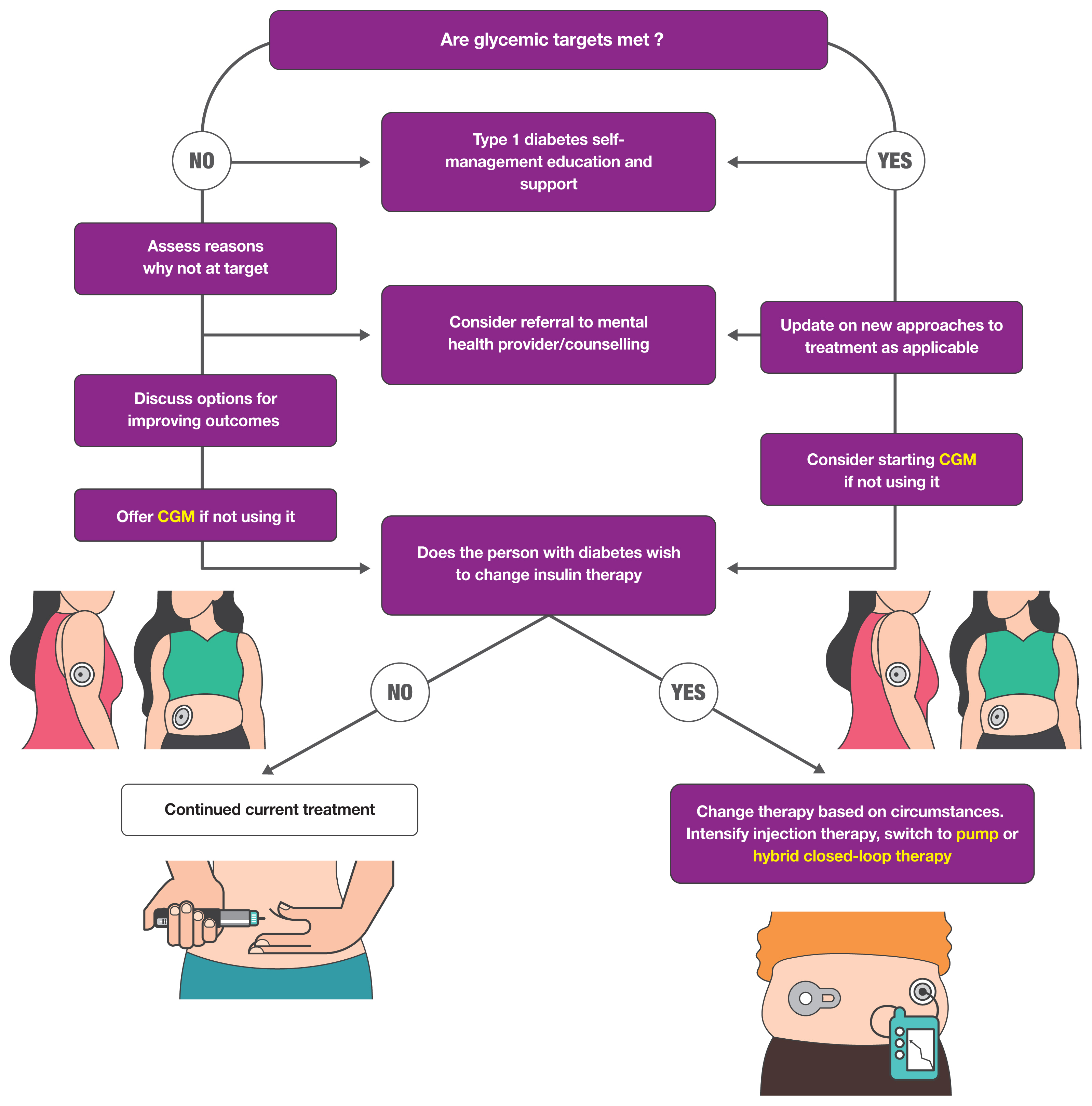
ePub - Guidelines for the management of patients with diabetes have become an important part of clinical practice that improve the quality of care and help establish evidence-based medicine in this field. With rapidly accumulating evidence on various aspects of diabetes care, including landmark clinical trials of treatment agents and newer technologies, timely updates of the guidelines capture the most current state of the field and present a consensus. As a leading academic society, the Korean Diabetes Association publishes practice guidelines biennially and the American Diabetes Association does so annually. In this review, we summarize the key changes suggested in the most recent guidelines. Some of the important updates include treatment algorithms emphasizing comorbid conditions such as atherosclerotic cardiovascular disease, heart failure, and chronic kidney disease in the selection of anti-diabetic agents; wider application of continuous glucose monitoring (CGM), insulin pump technologies and indices derived from CGM such as time in range; more active screening of subjects at high-risk of diabetes; and more detailed individualization in diabetes care. Although there are both similarities and differences among guidelines and some uncertainty remains, these updates provide a good approach for many clinical practitioners who are battling with diabetes.
-
Citations
Citations to this article as recorded by- Finerenone: Efficacy of a New Nonsteroidal Mineralocorticoid Receptor Antagonist in Treatment of Patients With Chronic Kidney Disease and Type 2 Diabetes
Subo Dey, Jasmine Garg, Andy Wang, Eva Holzner, William H. Frishman, Wilbert S. Aronow
Cardiology in Review.2024; 32(3): 285. CrossRef - Use of Diabetes Medications before and after a Heart Failure–Related Hospitalization among Nursing Home Residents
Tingting Zhang, Andrew R. Zullo, Kaleen (Kaley) N. Hayes, Dae Hyun Kim, Yoojin Lee, Lori A. Daiello, Douglas P. Kiel, Sarah D. Berry
Journal of the American Medical Directors Association.2024; 25(3): 454. CrossRef - Accuracy and Safety of the 15-Day CareSens Air Continuous Glucose Monitoring System
Kyung-Soo Kim, Seung-Hwan Lee, Won Sang Yoo, Cheol-Young Park
Diabetes Technology & Therapeutics.2024; 26(4): 222. CrossRef - Body composition and metabolic syndrome in patients with type 1 diabetes
Qiong Zeng, Xiao-Jing Chen, Yi-Ting He, Ze-Ming Ma, Yi-Xi Wu, Kun Lin
World Journal of Diabetes.2024; 15(1): 81. CrossRef - The best internal structure of the Diabetes Quality of Life Measure (DQOL) in Brazilian patients
Denilson Menezes Almeida, Aldair Darlan Santos-de-Araújo, José Mário Costa Brito Júnior, Marcela Cacere, André Pontes-Silva, Cyrene Piazera Costa, Maria Cláudia Gonçalves, José Márcio Soares Leite, Almir Vieira Dibai-Filho, Daniela Bassi-Dibai
BMC Public Health.2024;[Epub] CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - SGLT2 inhibitors and their possible use in prevention and treatment of neurological diseases
Mateusz Sobczyk, Daria Żuraw, Paulina Oleksa, Kacper Jasiński, Mikołaj Porzak, Michał Dacka
Prospects in Pharmaceutical Sciences.2024; 22(1): 16. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - Innovative Therapeutic Approaches in Non-Alcoholic Fatty Liver Disease: When Knowing Your Patient Is Key
Marta Alonso-Peña, Maria Del Barrio, Ana Peleteiro-Vigil, Carolina Jimenez-Gonzalez, Alvaro Santos-Laso, Maria Teresa Arias-Loste, Paula Iruzubieta, Javier Crespo
International Journal of Molecular Sciences.2023; 24(13): 10718. CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Access to novel anti-diabetic agents in resource limited settings: A brief commentary
Poobalan Naidoo, Kiolan Naidoo, Sumanth Karamchand, Rory F Leisegang
World Journal of Diabetes.2023; 14(7): 939. CrossRef - Comparative efficacy and safety profile of once-weekly Semaglutide versus once-daily Sitagliptin as an add-on to metformin in patients with type 2 diabetes: a systematic review and meta-analysis
Tirath Patel, Fnu Nageeta, Rohab Sohail, Tooba Shaukat Butt, Shyamala Ganesan, Fnu Madhurita, Muhammad Ahmed, Mahrukh Zafar, Wirda Zafar, Mohammad Uzair Zaman, Giustino Varrassi, Mahima Khatri, Satesh Kumar
Annals of Medicine.2023;[Epub] CrossRef - Bexagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, for improvement of glycemia in type 2 diabetes mellitus: a systematic review and meta-analysis
Sagar Dholariya, Siddhartha Dutta, Ragini Singh, Deepak Parchwani, Amit Sonagra, Mehul Kaliya
Expert Opinion on Pharmacotherapy.2023; 24(18): 2187. CrossRef - Analysis of the management and therapeutic performance of diabetes mellitus employing special target
Hong-Yan Sun, Xiao-Yan Lin
World Journal of Diabetes.2023; 14(12): 1721. CrossRef - Zinc Chloride Enhances the Antioxidant Status, Improving the Functional and Structural Organic Disturbances in Streptozotocin-Induced Diabetes in Rats
Irina Claudia Anton, Liliana Mititelu-Tartau, Eliza Gratiela Popa, Mihaela Poroch, Vladimir Poroch, Ana-Maria Pelin, Liliana Lacramioara Pavel, Ilie Cristian Drochioi, Gina Eosefina Botnariu
Medicina.2022; 58(11): 1620. CrossRef
- Finerenone: Efficacy of a New Nonsteroidal Mineralocorticoid Receptor Antagonist in Treatment of Patients With Chronic Kidney Disease and Type 2 Diabetes

- Adrenal Gland
- Recent Updates on the Management of Adrenal Incidentalomas
- Seung Shin Park, Jung Hee Kim
- Endocrinol Metab. 2023;38(4):373-380. Published online August 16, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1779
- 7,248 View
- 1,450 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
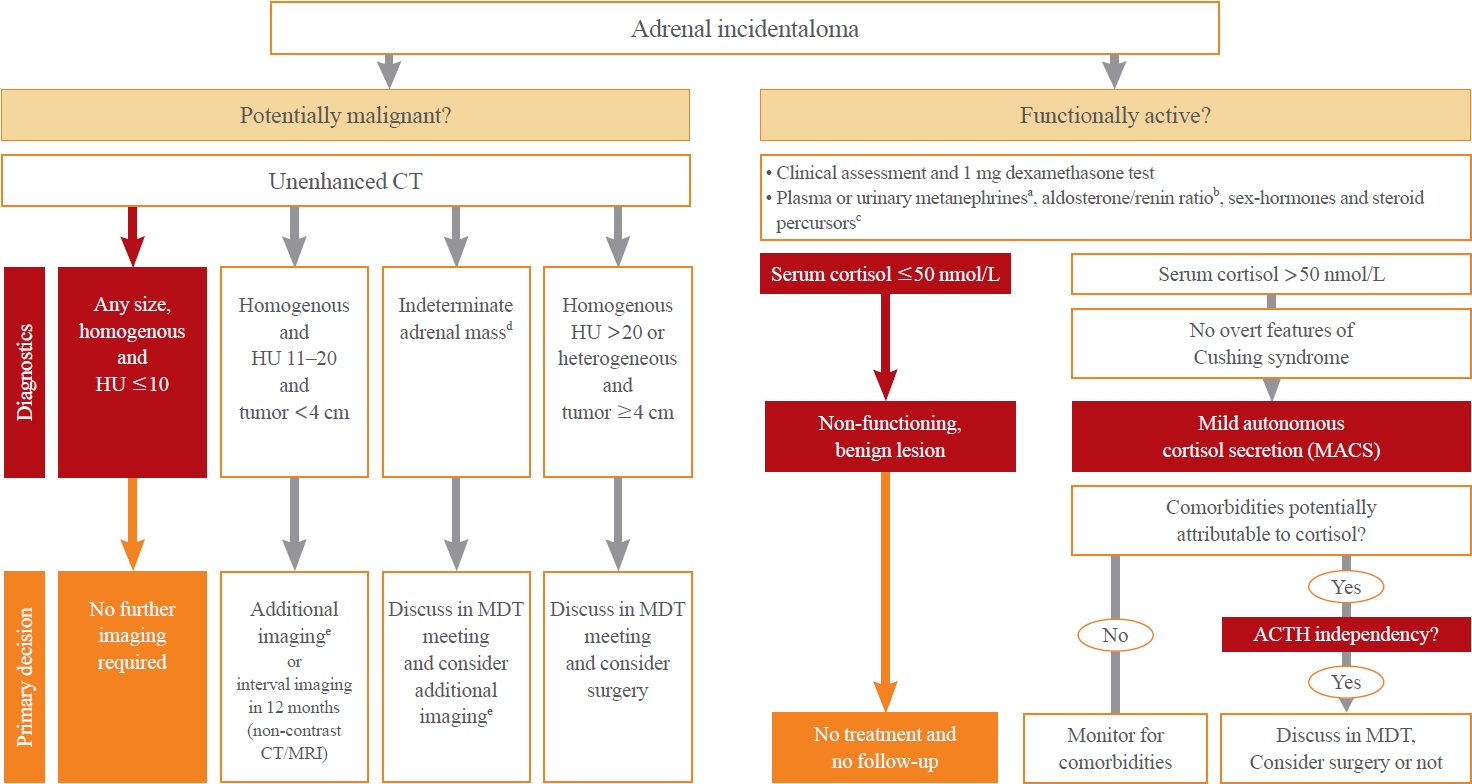
ePub - Adrenal incidentalomas represent an increasingly common clinical conundrum with significant implications for patients. The revised 2023 European Society of Endocrinology (ESE) guideline incorporates cutting-edge evidence for managing adrenal incidentalomas. This paper provides a concise review of the updated contents of the revised guideline. In the 2023 guideline, in patients without signs and symptoms of overt Cushing’s syndrome, a post-dexamethasone cortisol level above 50 nmol/L (>1.8 μg/dL) should be considered as mild autonomous cortisol secretion. Regarding the criteria of benign adrenal adenomas, a homogeneous adrenal mass with ≤10 Hounsfield units on non-contrast computed tomography requires no further follow-up, irrespective of its size. The updated guideline also discusses steroid metabolomics using tandem mass spectrometry to discriminate malignancy. It underscores the importance of high-volume surgeons performing adrenalectomy and emphasizes the pivotal role of a multidisciplinary team approach in deciding the treatment plan for indeterminate adrenal masses. The guideline advocates for more proactive surgical treatment for indeterminate adrenal masses in young patients (<40 years) and pregnant women. This review of the 2023 ESE guideline underscores the ongoing evolution of the adrenal incidentaloma management landscape, emphasizing the need for further research and adaptation of diagnostic and therapeutic strategies.

- Diabetes, obesity and metabolism
- The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update
- Agnieszka Jakubowska, Carel W. le Roux, Adie Viljoen
- Endocrinol Metab. 2024;39(1):12-22. Published online February 14, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1942
- 2,592 View
- 207 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
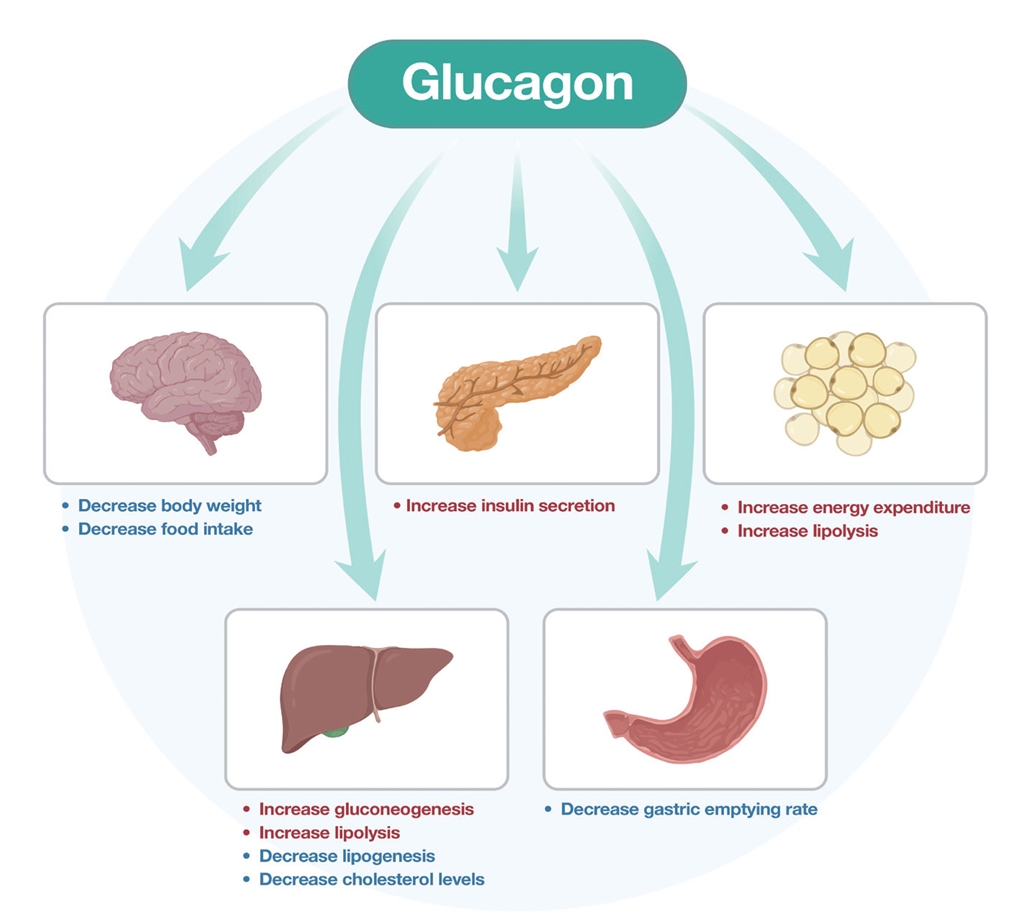
ePub - Obesity is the fifth leading risk factor for global deaths with numbers continuing to increase worldwide. In the last 20 years, the emergence of pharmacological treatments for obesity based on gastrointestinal hormones has transformed the therapeutic landscape. The successful development of glucagon-like peptide-1 (GLP-1) receptor agonists, followed by the synergistic combined effect of glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists achieved remarkable weight loss and glycemic control in those with the diseases of obesity and type 2 diabetes. The multiple cardiometabolic benefits include improving glycemic control, lipid profiles, blood pressure, inflammation, and hepatic steatosis. The 2023 phase 2 double-blind, randomized controlled trial evaluating a GLP-1/GIP/glucagon receptor triagonist (retatrutide) in patients with the disease of obesity reported 24.2% weight loss at 48 weeks with 12 mg retatrutide. This review evaluates the current available evidence for GLP-1 receptor agonists, dual GLP-1/GIP receptor co-agonists with a focus on GLP-1/GIP/glucagon receptor triagonists and discusses the potential future benefits and research directions.
-
Citations
Citations to this article as recorded by- New Mechanisms to Prevent Heart Failure with Preserved Ejection Fraction Using Glucagon-like Peptide-1 Receptor Agonism (GLP-1 RA) in Metabolic Syndrome and in Type 2 Diabetes: A Review
Jorge E. Jalil, Luigi Gabrielli, María Paz Ocaranza, Paul MacNab, Rodrigo Fernández, Bruno Grassi, Paulina Jofré, Hugo Verdejo, Monica Acevedo, Samuel Cordova, Luis Sanhueza, Douglas Greig
International Journal of Molecular Sciences.2024; 25(8): 4407. CrossRef
- New Mechanisms to Prevent Heart Failure with Preserved Ejection Fraction Using Glucagon-like Peptide-1 Receptor Agonism (GLP-1 RA) in Metabolic Syndrome and in Type 2 Diabetes: A Review

- Diabetes, Obesity and Metabolism
- Lipoprotein Lipase: Is It a Magic Target for the Treatment of Hypertriglyceridemia
- Joon Ho Moon, Kyuho Kim, Sung Hee Choi
- Endocrinol Metab. 2022;37(4):575-586. Published online August 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.402
- 7,830 View
- 439 Download
- 11 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
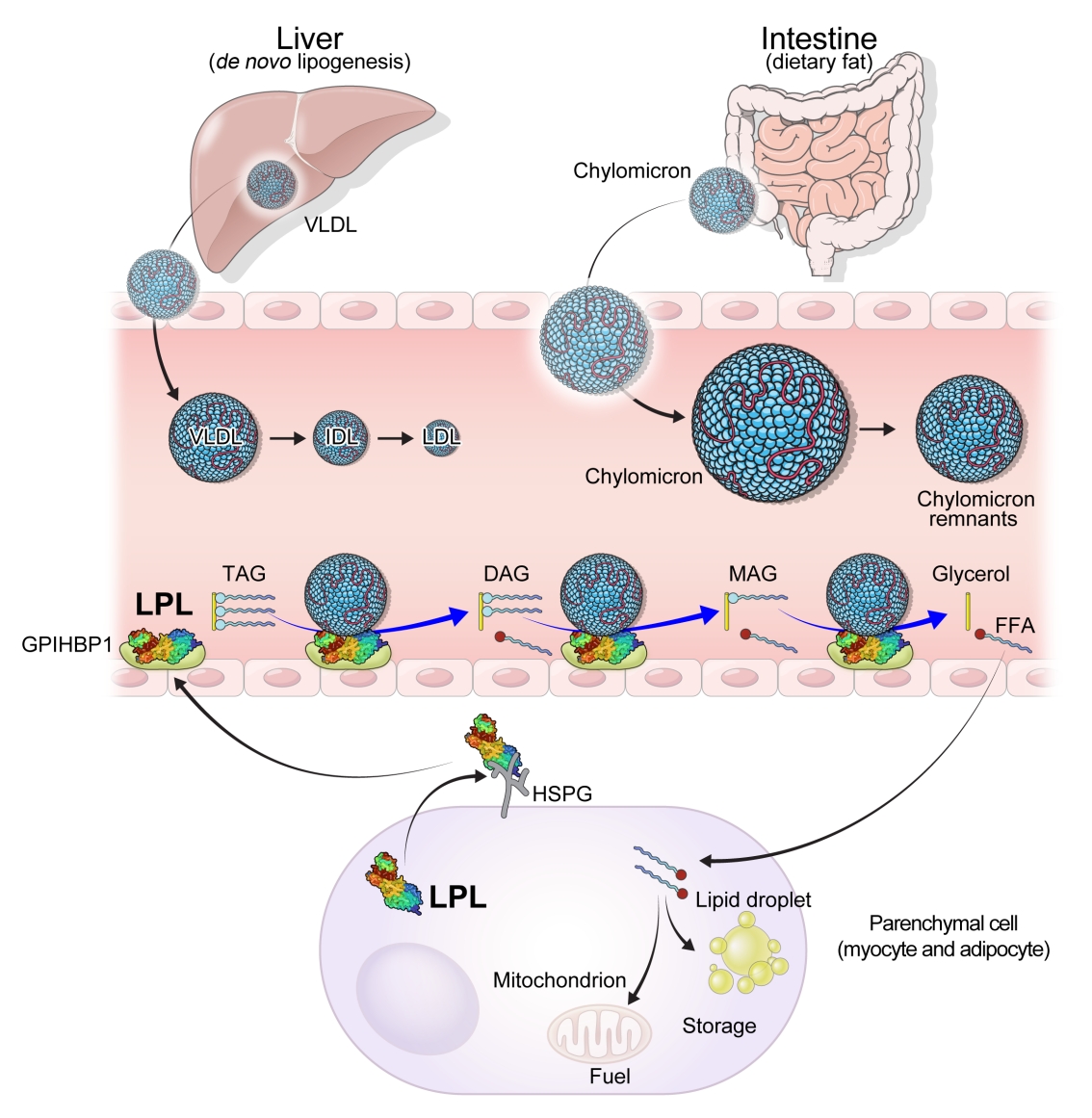
ePub - High levels of triglycerides (TG) and triglyceride-rich lipoproteins (TGRLs) confer a residual risk of cardiovascular disease after optimal low-density lipoprotein cholesterol (LDL-C)–lowering therapy. Consensus has been made that LDL-C is a non-arguable primary target for lipid lowering treatment, but the optimization of TGRL for reducing the remnant risk of cardiovascular diseases is urged. Omega-3 fatty acids and fibrates are used to reduce TG levels, but many patients still have high TG and TGRL levels combined with low high-density lipoprotein concentration that need to be ideally treated. Lipoprotein lipase (LPL) is a key regulator for TGs that hydrolyzes TGs to glycerol and free fatty acids in lipoprotein particles for lipid storage and consumption in peripheral organs. A deeper understanding of human genetics has enabled the identification of proteins regulating the LPL activity, which include the apolipoproteins and angiopoietin-like families. Novel therapeutic approach such as antisense oligonucleotides and monoclonal antibodies that regulate TGs have been developed in recent decades. In this article, we focus on the biology of LPL and its modulators and review recent clinical application, including genetic studies and clinical trials of novel therapeutics. Optimization of LPL activity to lower TG levels could eventually reduce incident atherosclerotic cardiovascular disease in conjunction with successful LDL-C reduction.
-
Citations
Citations to this article as recorded by- The chylomicron saga: time to focus on postprandial metabolism
Alejandro Gugliucci
Frontiers in Endocrinology.2024;[Epub] CrossRef - Sanghuangporus vaninii extract ameliorates hyperlipidemia in rats by mechanisms identified with transcriptome analysis
Ning Gao, Yuanzhen Liu, Guangjie Liu, Bo Liu, Yupeng Cheng
Food Science & Nutrition.2024;[Epub] CrossRef - Targeting host-specific metabolic pathways—opportunities and challenges for anti-infective therapy
Monika I. Konaklieva, Balbina J. Plotkin
Frontiers in Molecular Biosciences.2024;[Epub] CrossRef - Obesity, dyslipidemia, and cardiovascular disease: A joint expert review from the obesity medicine association and the National Lipid Association 2024
Harold Edward Bays, Carol Kirkpatrick, Kevin C. Maki, Peter P. Toth, Ryan T. Morgan, Justin Tondt, Sandra Michelle Christensen, Dave Dixon, Terry A. Jacobson
Obesity Pillars.2024; : 100108. CrossRef - Role of Fenofibrate Use in Dyslipidemia and Related Comorbidities in the Asian Population: A Narrative Review
Chaicharn Deerochanawong, Sin Gon Kim, Yu-Cheng Chang
Diabetes & Metabolism Journal.2024; 48(2): 184. CrossRef - Xanthohumol, a prenylated chalcone, regulates lipid metabolism by modulating the LXRα/RXR-ANGPTL3-LPL axis in hepatic cell lines and high-fat diet-fed zebrafish models
Wan-Yun Gao, Pei-Yi Chen, Hao-Jen Hsu, Je-Wen Liou, Chia-Ling Wu, Ming-Jiuan Wu, Jui-Hung Yen
Biomedicine & Pharmacotherapy.2024; 174: 116598. CrossRef - Obesity, dyslipidemia, and cardiovascular disease: A joint expert review from the Obesity Medicine Association and the National Lipid Association 2024
Harold Edward Bays, Carol Kirkpatrick, Kevin C. Maki, Peter P. Toth, Ryan T. Morgan, Justin Tondt, Sandra Michelle Christensen, Dave Dixon, Terry A. Jacobson
Journal of Clinical Lipidology.2024;[Epub] CrossRef - High producer variant of lipoprotein lipase may protect from hepatocellular carcinoma in alcohol-associated cirrhosis
Franziska Schmalz, Janett Fischer, Hamish Innes, Stephan Buch, Christine Möller, Madlen Matz-Soja, Witigo von Schönfels, Benjamin Krämer, Bettina Langhans, Alexandra Klüners, Michael Soyka, Felix Stickel, Jacob Nattermann, Christian P. Strassburg, Thomas
JHEP Reports.2023; 5(4): 100684. CrossRef - Measurement of Serum Low Density Lipoprotein Cholesterol and Triglyceride-Rich Remnant Cholesterol as Independent Predictors of Atherosclerotic Cardiovascular Disease: Possibilities and Limitations
Dieter Lütjohann, Hans-Ulrich Klör, Frans Stellaard
Nutrients.2023; 15(9): 2202. CrossRef - Influence of antipsychotic medications on hyperlipidemia risk in patients with schizophrenia: evidence from a population-based cohort study and in vitro hepatic lipid homeostasis gene expression
Tien-Yuan Wu, Ni Tien, Cheng-Li Lin, Yu-Cun Cheah, Chung Y. Hsu, Fuu-Jen Tsai, Yi-Jen Fang, Yun-Ping Lim
Frontiers in Medicine.2023;[Epub] CrossRef - Triglyceride-Rich Lipoprotein Metabolism: Key Regulators of Their Flux
Alejandro Gugliucci
Journal of Clinical Medicine.2023; 12(13): 4399. CrossRef - Sugar and Dyslipidemia: A Double-Hit, Perfect Storm
Alejandro Gugliucci
Journal of Clinical Medicine.2023; 12(17): 5660. CrossRef - Dyslipidemia in Patients with Chronic Kidney Disease: An Updated Overview
Sang Heon Suh, Soo Wan Kim
Diabetes & Metabolism Journal.2023; 47(5): 612. CrossRef - Peroxisome Proliferator-Activated Receptor α in Lipoprotein Metabolism and Atherosclerotic Cardiovascular Disease
Elena Valeria Fuior, Evangelia Zvintzou, Theodosios Filippatos, Katerina Giannatou, Victoria Mparnia, Maya Simionescu, Anca Violeta Gafencu, Kyriakos E. Kypreos
Biomedicines.2023; 11(10): 2696. CrossRef - Developing a model to predict the early risk of hypertriglyceridemia based on inhibiting lipoprotein lipase (LPL): a translational study
Julia Hernandez-Baixauli, Gertruda Chomiciute, Juan María Alcaide-Hidalgo, Anna Crescenti, Laura Baselga-Escudero, Hector Palacios-Jordan, Elisabet Foguet-Romero, Anna Pedret, Rosa M. Valls, Rosa Solà, Miquel Mulero, Josep M. Del Bas
Scientific Reports.2023;[Epub] CrossRef
- The chylomicron saga: time to focus on postprandial metabolism

- Adrenal gland
- A Contemporary Approach to the Diagnosis and Management of Adrenal Insufficiency
- Suranut Charoensri, Richard J. Auchus
- Endocrinol Metab. 2024;39(1):73-82. Published online January 22, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1894
- 2,484 View
- 244 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
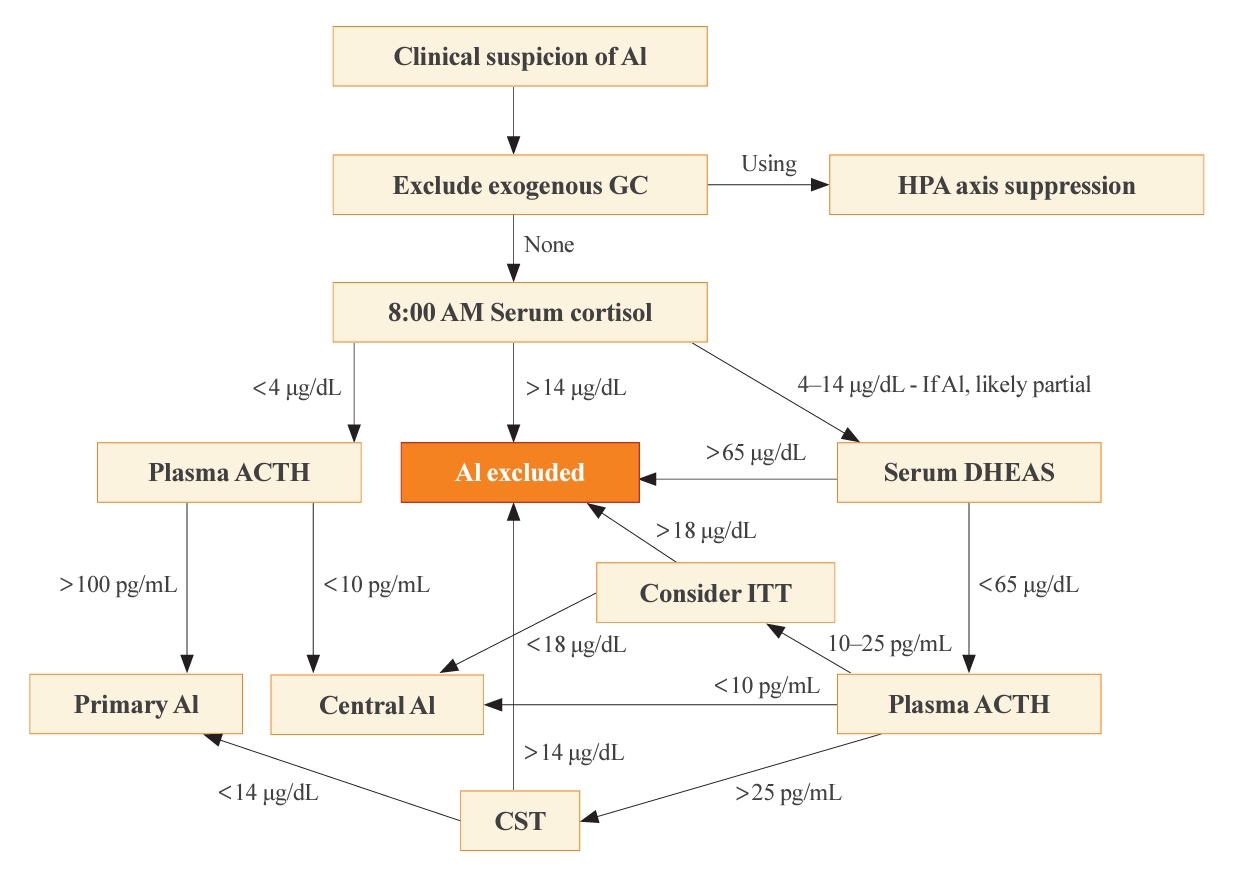
ePub - Adrenal insufficiency (AI) can be classified into three distinct categories based on its underlying causes: primary adrenal disorders, secondary deficiencies in adrenocorticotropin, or hypothalamic suppression from external factors, most commonly glucocorticoid medications used for anti-inflammatory therapy. The hallmark clinical features of AI include fatigue, appetite loss, unintentional weight loss, low blood pressure, and hyponatremia. Individuals with primary AI additionally manifest skin hyperpigmentation, hyperkalemia, and salt craving. The diagnosis of AI is frequently delayed due to the non-specific symptoms and signs early in the disease course, which poses a significant challenge to its early detection prior to an adrenal crisis. Despite the widespread availability of lifesaving glucocorticoid medications for decades, notable challenges persist, particularly in the domains of timely diagnosis while simultaneously avoiding misdiagnosis, patient education for averting adrenal crises, and the determination of optimal replacement therapies. This article reviews recent advancements in the contemporary diagnostic strategy and approaches to optimal treatment for AI.

- Thyroid
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
- Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
- Endocrinol Metab. 2024;39(1):47-60. Published online February 15, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1937

- 1,896 View
- 173 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The indolent nature and favorable outcomes associated with papillary thyroid microcarcinoma have prompted numerous prospective studies on active surveillance (AS) and its adoption as an alternative to immediate surgery in managing low-risk thyroid cancer. This article reviews the current status of AS, as outlined in various international practice guidelines. AS is typically recommended for tumors that measure 1 cm or less in diameter and do not exhibit aggressive subtypes on cytology, extrathyroidal extension, lymph node metastasis, or distant metastasis. To determine the most appropriate candidates for AS, factors such as tumor size, location, multiplicity, and ultrasound findings are considered, along with patient characteristics like medical condition, age, and family history. Moreover, shared decision-making, which includes patient-reported outcomes such as quality of life and cost-effectiveness, is essential. During AS, patients undergo regular ultrasound examinations to monitor for signs of disease progression, including tumor growth, extrathyroidal extension, or lymph node metastasis. In conclusion, while AS is a feasible and reliable approach for managing lowrisk thyroid cancer, it requires careful patient selection, effective communication for shared decision-making, standardized follow-up protocols, and a clear definition of disease progression.

Namgok Lecture 2023
- Diabetes, obesity and metabolism
- Hypothalamic AMP-Activated Protein Kinase as a Whole-Body Energy Sensor and Regulator
- Se Hee Min, Do Kyeong Song, Chan Hee Lee, Eun Roh, Min-Seon Kim
- Endocrinol Metab. 2024;39(1):1-11. Published online February 14, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1922
- 1,882 View
- 74 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
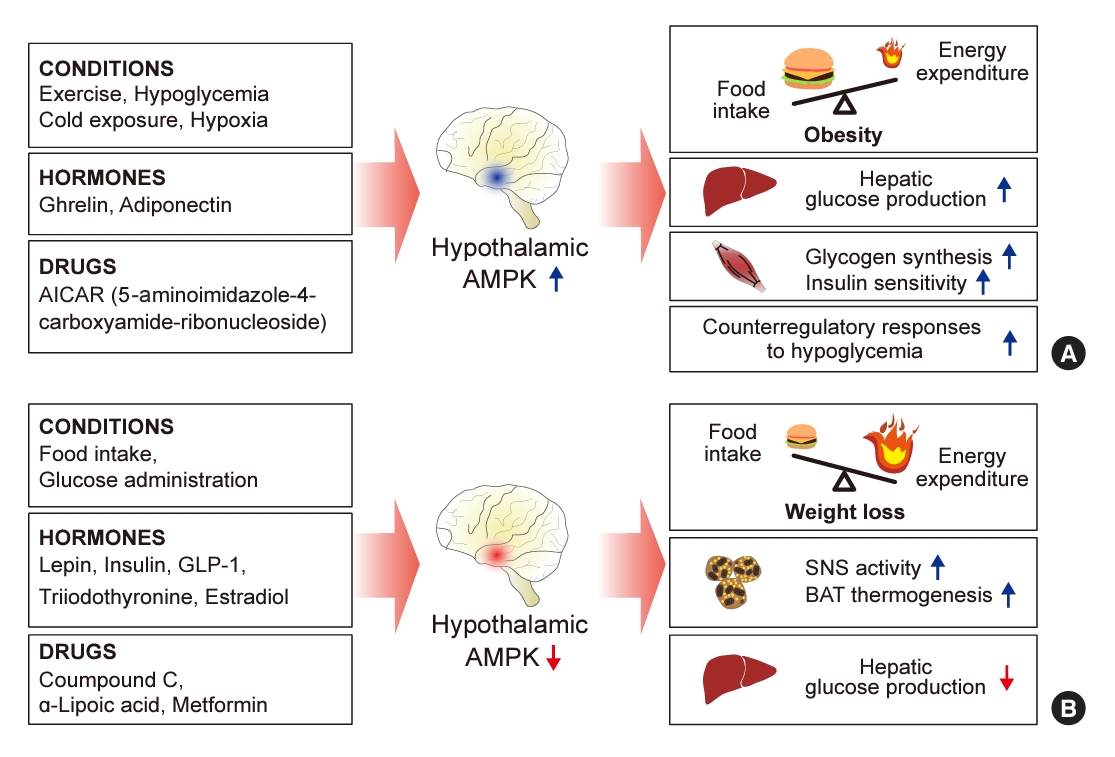
ePub - 5´-Adenosine monophosphate (AMP)-activated protein kinase (AMPK), a cellular energy sensor, is an essential enzyme that helps cells maintain stable energy levels during metabolic stress. The hypothalamus is pivotal in regulating energy balance within the body. Certain neurons in the hypothalamus are sensitive to fluctuations in food availability and energy stores, triggering adaptive responses to preserve systemic energy equilibrium. AMPK, expressed in these hypothalamic neurons, is instrumental in these regulatory processes. Hypothalamic AMPK activity is modulated by key metabolic hormones. Anorexigenic hormones, including leptin, insulin, and glucagon-like peptide 1, suppress hypothalamic AMPK activity, whereas the hunger hormone ghrelin activates it. These hormonal influences on hypothalamic AMPK activity are central to their roles in controlling food consumption and energy expenditure. Additionally, hypothalamic AMPK activity responds to variations in glucose concentrations. It becomes active during hypoglycemia but is deactivated when glucose is introduced directly into the hypothalamus. These shifts in AMPK activity within hypothalamic neurons are critical for maintaining glucose balance. Considering the vital function of hypothalamic AMPK in the regulation of overall energy and glucose balance, developing chemical agents that target the hypothalamus to modulate AMPK activity presents a promising therapeutic approach for metabolic conditions such as obesity and type 2 diabetes mellitus.

Original Article
- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes
- Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
- Endocrinol Metab. 2022;37(4):641-651. Published online August 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1501
- 6,167 View
- 166 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The prevalence of young-onset diabetes (YOD) has been increasing worldwide. As the incidence of YOD increases, it is necessary to determine the characteristics of YOD and the factors that influence its development and associated complications.
Methods
In this retrospective study, we recruited patients who were diagnosed with type 2 diabetes mellitus between June 2001 and December 2021 at a tertiary hospital. The study population was categorized according to age: YOD (age <40 years), middle-age-onset diabetes (MOD, 40≤ age <65 years), and late-onset diabetes (LOD, age ≥65 years). We examined trends in glycemic control by analyzing fasting glucose levels during the first year in each age group. A Cox proportional-hazards model was used to determine the relative risk of developing complications according to glycemic control trends.
Results
The fasting glucose level at the time of diagnosis was highest in the YOD group (YOD 149±65 mg/dL; MOD 143±54 mg/dL; and LOD 140±55 mg/dL; p=0.009). In the YOD group, glucose levels decreased at 3 months, but increased by 12 months. YOD patients and those with poor glycemic control in the first year were at a higher risk of developing complications, whereas the risk in patients with LOD was not statistically significant.
Conclusion
YOD patients had higher glucose levels at diagnosis, and their glycemic control was poorly maintained. As poor glycemic control can influence the development of complications, especially in young patients, intensive treatment is necessary for patients with YOD. -
Citations
Citations to this article as recorded by- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes & Metabolism.2024; 50(1): 101505. CrossRef - Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study
Da Hea Seo, Mina Kim, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes Research and Clinical Practice.2024; 208: 111098. CrossRef - Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus
Hye-Sun Park, Yongin Cho, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, Suk Chon, Jeong-Taek Woo, Sei Hyun Baik, Kwan Woo Lee, So Hun Kim
Scientific Reports.2024;[Epub] CrossRef - Early onset type 2 diabetes mellitus: an update
Myrsini Strati, Melpomeni Moustaki, Theodora Psaltopoulou, Andromachi Vryonidou, Stavroula A. Paschou
Endocrine.2024;[Epub] CrossRef - Complications and Treatment of Early-Onset Type 2 Diabetes
Fahimeh Soheilipour, Naghmeh Abbasi Kasbi, Mahshid Imankhan, Delaram Eskandari
International Journal of Endocrinology and Metabolism.2023;[Epub] CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
Endocrinology and Metabolism.2022; 37(6): 945. CrossRef -
ISPAD
Clinical Practice Consensus Guidelines 2022: Management of the child, adolescent, and young adult with diabetes in limited resource settings
Anju Virmani, Stuart J. Brink, Angela Middlehurst, Fauzia Mohsin, Franco Giraudo, Archana Sarda, Sana Ajmal, Julia E. von Oettingen, Kuben Pillay, Supawadee Likitmaskul, Luis Eduardo Calliari, Maria E. Craig
Pediatric Diabetes.2022; 23(8): 1529. CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
May Thu Hla Aye, Sajid Adhi Raja, Vui Heng Chong
Endocrinology and Metabolism.2022; 37(6): 943. CrossRef
- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study

Review Articles
- Calcium & Bone Metabolism
- Discontinuing Denosumab: Can It Be Done Safely? A Review of the Literature
- Wei Lin Tay, Donovan Tay
- Endocrinol Metab. 2022;37(2):183-194. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1369

- 16,179 View
- 898 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Denosumab, which has been approved for the treatment of osteoporosis since 2010, is a fully humanised monoclonal antibody against a cytokine, receptor activator of nuclear factor kappa B ligand (RANKL), involved in bone resorption. Continued use of denosumab results in a potent and sustained decrease in bone turnover, an increase in bone mineral density (BMD), and a reduction in vertebral and hip fractures. The anti-resorptive effects of denosumab are reversible upon cessation, and this reversal is accompanied by a transient marked increase in bone turnover that is associated with bone loss, and of concern, an increased risk of multiple vertebral fractures. In this review, we outline the effects of denosumab withdrawal on bone turnover markers, BMD, histomorphometry, and fracture risk. We provide an update on recent clinical trials that sought to answer how clinicians can transition away from denosumab safely with follow-on therapy to mitigate bone loss and summarise the recommendations of various international guidelines.
-
Citations
Citations to this article as recorded by- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury
Christopher M. Cirnigliaro, Michael F. La Fountaine, J. Scott Parrott, Steven C. Kirshblum, Susan J. Sauer, Sue A. Shapses, Isa A. McClure, William A. Bauman
Osteoporosis International.2023; 34(4): 741. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef
- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury

- Diabetes, obesity and metabolism
- Initial Combination Therapy in Type 2 Diabetes
- Ji Yoon Kim, Nam Hoon Kim
- Endocrinol Metab. 2024;39(1):23-32. Published online November 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1816
- 2,058 View
- 249 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Type 2 diabetes (T2D) is a progressive disease in which it is challenging to achieve long-term durable glycemic control. However, intensive glycemic control is crucial for preventing diabetes-related complications. Previous studies showed that monotherapy with a stepwise add-on approach was seldom effective for long-term durable glycemic control. Combination therapy, which refers to the use of two or more drugs to control hyperglycemia, has multiple benefits, including the ability to target a variety of pathophysiological processes underlying hyperglycemia. In clinical trials, initial combination therapy showed better glycemic control than monotherapy or a stepwise approach. Emerging evidence indicates that initial combination therapy is associated with preserved β-cell function and fewer complications in T2D. However, cost-effectiveness and adverse events with combination therapy are issues that should be considered. Therefore, initial combination therapy is an important option for patients with T2D that clinicians should consider with a view toward balancing benefits and potential harms. In this review, we summarize the literature addressing initial combination therapy in T2D, and we suggest optimal strategies based on clinical situations and patient characteristics.

- Thyroid
- Novel and Advanced Ultrasound Techniques for Thyroid Thermal Ablation
- Wai-Kin Chan, Jui-Hung Sun, Miaw-Jene Liou, Chia-Jung Hsu, Yu-Ling Lu, Wei-Yu Chou, Yan-Rong Li, Feng-Hsuan Liu
- Endocrinol Metab. 2024;39(1):40-46. Published online February 13, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1917
- 1,706 View
- 112 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thyroid radiofrequency ablation and microwave ablation are widely adopted minimally invasive treatments for diverse thyroid conditions worldwide. Fundamental skills such as the trans-isthmic approach and the moving shot technique are crucial for performing thyroid ablation, and advanced techniques, including hydrodissection and vascular ablation, improve safety and efficacy and reduce complications. Given the learning curve associated with ultrasound-guided therapeutic procedures, operators need training and experience. While training models exist, limited attention has been given to ultrasound maneuvers in ablation needle manipulation. This article introduces two essential maneuvers, the zigzag moving technique and the alienate maneuver, while also reviewing the latest ultrasound techniques in thyroid ablation, contributing valuable insights into this evolving field.

Namgok Lecture 2021
- Diabetes, Obesity and Metabolism
- The Influence of Obesity and Metabolic Health on Vascular Health
- Eun-Jung Rhee
- Endocrinol Metab. 2022;37(1):1-8. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.101

- 7,008 View
- 299 Download
- 15 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The prevalence of obesity is rapidly increasing worldwide. Obesity should not be understood only as the accumulation of fat in the body, but instead as a phenomenon that exerts different effects on our health according to the place of fat deposition and its stability. Obesity is the starting point of most metabolic diseases, such as diabetes, hypertension, metabolic syndrome, sleep apnea, and eventually cardiovascular disease. There are different kinds of obesity, ranging from simple obesity to sarcopenic obesity. The main purpose of intervening to address obesity is to decrease the ultimate consequence of obesity—namely, cardiovascular disease. The main mechanism through which obesity, especially abdominal obesity, increases cardiovascular risk is the obesity-induced derangement of metabolic health, leading to the development of metabolic diseases such as diabetes, non-alcoholic fatty liver disease, and metabolic syndrome, which are the main initiators of vascular damage. In this review, I discuss the influence of various types of obesity on the risk of metabolic diseases, and how these diseases increase cardiovascular disease risk.
-
Citations
Citations to this article as recorded by- Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study
Nam Hoon Kim, Ji Yoon Kim, Jimi Choi, Sin Gon Kim
European Heart Journal - Cardiovascular Pharmacotherapy.2024; 10(2): 118. CrossRef - Severity of abdominal obesity and cardiometabolic diseases in US adults
S. Wang, S. Shi, Y. Huang, H. Huang, V.W. Zhong
Public Health.2024; 227: 154. CrossRef - Anti-obesity effects of fucoidan from
Sargassum thunbergii in adipocytes and high fat diet induced obese mice through inhibiting adipogenic specific transcription factor
Hyo-Geun Lee, H.H.A.C.K. Jayawardhana, Fengqi Yang, D.P. Nagahawaththa, N.M. Liyanage, Kyung-Mo Song, Yun-Sang Choi, Seung-Hong Lee, You-Jin Jeon, Min-Cheol Kang
Food Science and Human Wellness.2024; 13(3): 1608. CrossRef - Association of a High Healthy Eating Index Diet with Long-Term Visceral Fat Loss in a Large Longitudinal Study
Sunmin Park
Nutrients.2024; 16(4): 534. CrossRef - Ancistrocladus tectorius Extract Inhibits Obesity by Promoting Thermogenesis and Mitochondrial Dynamics in High-Fat Diet-Fed Mice
Minju Kim, Jin Hyub Paik, Hwa Lee, Min Ji Kim, Sang Mi Eum, Soo Yong Kim, Sangho Choi, Ho-Yong Park, Hye Gwang Jeong, Tae-Sook Jeong
International Journal of Molecular Sciences.2024; 25(7): 3743. CrossRef - Biological Activity Evaluation of Olive, Grape, and Fig at Various Mixing Ratios
Chan-Hwi Lee, So-Young Lee, Ae-Jung Kim
Asian Journal of Beauty and Cosmetology.2024; 22(1): 91. CrossRef - Investigation and Comparison of Maternal Pre-Pregnancy Body Mass Index Coupled with Gestational Weight Gain on Maternal–Fetal Complications Based on US and Chinese Guidelines: A Retrospective Study
Wan-Ju Kung, Hsin-Yi Kuo, Ching-Feng Chang, Yeong-Hwa Zen, Ching-Chiang Lin
Reproductive Sciences.2024;[Epub] CrossRef - Mechanistic insights into dietary (poly)phenols and vascular dysfunction-related diseases using multi-omics and integrative approaches: Machine learning as a next challenge in nutrition research
Dragan Milenkovic, Tatjana Ruskovska
Molecular Aspects of Medicine.2023; 89: 101101. CrossRef - Pharmacological Support for the Treatment of Obesity—Present and Future
Marcin Kosmalski, Kacper Deska, Bartłomiej Bąk, Monika Różycka-Kosmalska, Tadeusz Pietras
Healthcare.2023; 11(3): 433. CrossRef - Prioritizing obesity treatment: expanding the role of cardiologists to improve cardiovascular health and outcomes
Donna H. Ryan, John E. Deanfield, Stephan Jacob
Cardiovascular Endocrinology & Metabolism.2023; 12(1): e0279. CrossRef - Adipopenia is associated with osteoporosis in community-dwelling non-underweight adults independent of sarcopenia
Seunghyun Lee, Kyoungmyoung Ko, Sungjae Shin, Hye Sun Park, Namki Hong, Yumie Rhee
Archives of Osteoporosis.2023;[Epub] CrossRef - Design, synthesis and evaluation of 2-pyrimidinylindole derivatives as anti-obesity agents by regulating lipid metabolism
Shi-Yao Guo, Li-Yuan Wei, Bing-Bing Song, Yu-Tao Hu, Zhi Jiang, Dan-Dan Zhao, Yao-Hao Xu, Yu-Wei Lin, Shu-Min Xu, Shuo-Bin Chen, Zhi-Shu Huang
European Journal of Medicinal Chemistry.2023; 260: 115729. CrossRef - Short-Term L-Citrulline Supplementation Does Not Affect Blood Pressure, Pulse Wave Reflection, or Arterial Stiffness at Rest and during Isometric Exercise in Older Males
Andrea Tryfonos, Filippos Christodoulou, George M. Pamboris, Stephanos Christodoulides, Anastasios A. Theodorou
Sports.2023; 11(9): 177. CrossRef - Skinfold Thickness as a Cardiometabolic Risk Predictor in Sedentary and Active Adult Populations
Sughey González-Torres, Luis Miguel Anaya-Esparza, Gabriel Fermín Trigueros del Valle, Edgar Alfonso Rivera-León, Zuamí Villagrán, Sergio Sánchez-Enríquez
Journal of Personalized Medicine.2023; 13(9): 1326. CrossRef - Impact of COVID-19 Lockdown on Non-Alcoholic Fatty Liver Disease and Insulin Resistance in Adults: A before and after Pandemic Lockdown Longitudinal Study
Ángel Arturo López-González, Bárbara Altisench Jané, Luis Masmiquel Comas, Sebastiana Arroyo Bote, Hilda María González San Miguel, José Ignacio Ramírez Manent
Nutrients.2022; 14(14): 2795. CrossRef - Fenofibrate enhances lipid deposition via modulating PPARγ, SREBP-1c, and gut microbiota in ob/ob mice fed a high-fat diet
Ying Zhang, Xiu-Bin Jia, Yun-Chao Liu, Wen-Qian Yu, Yan-Hong Si, Shou-Dong Guo
Frontiers in Nutrition.2022;[Epub] CrossRef - Predictive Roles of Basal Metabolic Rate and Body Water Distribution in Sarcopenia and Sarcopenic Obesity: The link to Carbohydrates
Lizheng Guan, Tiantian Li, Xuan Wang, Kang Yu, Rong Xiao, Yuandi Xi
Nutrients.2022; 14(19): 3911. CrossRef - Metabolic risk factors in patients with comorbidity in Ufa primary health care
O.V. Molchanova, A.V. Mamaeva, A.R. Dunayeva, Z.A. Lust, E.M. Faskhetdinova, R.N. Shepel, D.O. Orlov, L.M. Zhamalov, G.F. Andreeva, O.M. Drapkina
Profilakticheskaya meditsina.2022; 25(9): 39. CrossRef - Assessment of Vitamin D Levels in Relation to Statin Therapy in Elderly Hypertensive Patients with Comorbidities
Kinga-Ilona Nyulas, Zsuzsánna Simon-Szabó, Zoltán Preg, Sándor Pál, Arundhati Sharma, Tünde Pál, Márta Germán-Salló, Enikő Nemes-Nagy
Journal of Interdisciplinary Medicine.2022; 7(4): 88. CrossRef
- Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study

Review Article
- Calcium & Bone Metabolism
- A Key Metabolic Regulator of Bone and Cartilage Health
- Elizabeth Pérez-Hernández, Jesús Javier Pastrana-Carballo, Fernando Gómez-Chávez, Ramesh C. Gupta, Nury Pérez-Hernández
- Endocrinol Metab. 2022;37(4):559-574. Published online August 8, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1443
- 7,882 View
- 341 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Taurine, a cysteine-derived zwitterionic sulfonic acid, is a common ingredient in energy drinks and is naturally found in fish and other seafood. In humans, taurine is produced mainly in the liver, and it can also be obtained from food. In target tissues, such as the retina, heart, and skeletal muscle, it functions as an essential antioxidant, osmolyte, and antiapoptotic agent. Taurine is also involved in energy metabolism and calcium homeostasis. Taurine plays a considerable role in bone growth and development, and high-profile reports have demonstrated the importance of its metabolism for bone health. However, these reports have not been collated for more than 10 years. Therefore, this review focuses on taurine–bone interactions and covers recently discovered aspects of taurine’s effects on osteoblastogenesis, osteoclastogenesis, bone structure, and bone pathologies (e.g., osteoporosis and fracture healing), with due attention to the taurine–cartilage relationship.
-
Citations
Citations to this article as recorded by- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis
Mengxing Yin, Dezhi Zhou, Fu Jia, Xiaosan Su, Xiufang Li, Ruifen Sun, Junmin Li
Journal of Orthopaedic Surgery and Research.2023;[Epub] CrossRef - An in-silico approach to the potential modulatory effect of taurine on sclerostin (SOST) and its probable role during osteoporosis
Mazumder Adhish, I. Manjubala
Journal of Biomolecular Structure and Dynamics.2023; : 1. CrossRef - Flattening the biological age curve by improving metabolic health: to taurine or not to taurine, that’ s the question
Kwok M. Ho, Anna Lee, William Wu, Matthew T.V. Chan, Lowell Ling, Jeffrey Lipman, Jason Roberts, Edward Litton, Gavin M. Joynt, Martin Wong
Journal of Geriatric Cardiology.2023; 20(11): 813. CrossRef
- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis


 KES
KES

 First
First Prev
Prev



