Search
- Page Path
- HOME > Search
- Calcium & Bone Metabolism
Big Data Articles (National Health Insurance Service Database) - 10-Year Fracture Risk in Postmenopausal Women with Osteopenia and Osteoporosis in South Korea
- Yeon-Hee Baek, Sun Wook Cho, Han Eol Jeong, Ju Hwan Kim, Yunji Hwang, Jeffrey L. Lange, Ju-Young Shin
- Endocrinol Metab. 2021;36(6):1178-1188. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1215
- 5,336 View
- 249 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
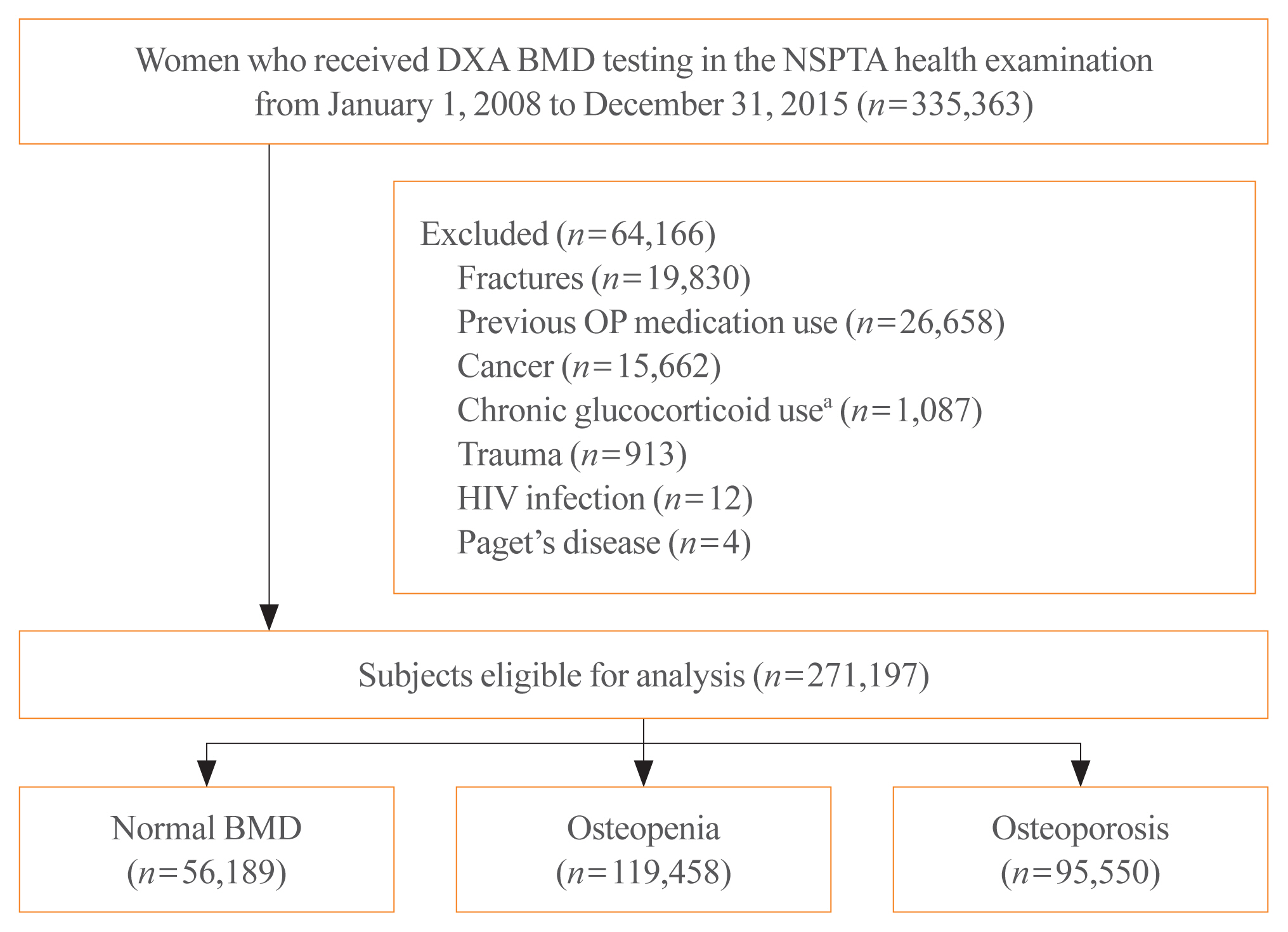
In South Korea, women aged 66 years are eligible for complimentary bone mineral density (BMD) screening via the National Screening Program for Transitional Ages. We aimed to evaluate the 10-year fracture risk in women receiving BMD screening between January 2008 and December 2015.
Methods
BMD was classified as normal (T-score ≥–1.0 standard deviation [SD]), osteopenia (T-score <–1.0 SD and >–2.5 SD), and osteoporosis (T score ≤–2.5 SD) from dual-energy X-ray absorptiometry. Follow-up continued from the screening date until a diagnosis for clinical fragility fracture (including sites of the vertebrae, hip, pelvis, clavicle, humerus, forearm, wrist, lower leg, and ankle), censored at the earliest date of trauma, death, or December 2017; fracture was ascertained using diagnostic codes from the National Health Insurance Service database. A multivariable Cox proportional hazard model was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of fracture in women with osteopenia or osteoporosis relative to women with normal BMD.
Results
Among the 271,197 women screened, 44.0% had osteopenia and 35.2% had osteoporosis. The 10 year cumulative incidence of fragility fractures was 31.1%, 37.5%, and 44.3% in women with normal BMD, osteopenia, and osteoporosis, respectively. Fracture risk was higher in women with osteopenia (HR, 1.31; 95% CI, 1.28 to 1.34) and osteoporosis (HR, 1.68; 95% CI, 1.64 to 1.72) than in women with normal BMD.
Conclusion
Women with osteopenia and women with osteoporosis, identified by the national BMD screening program, demonstrated a substantially elevated risk of fracture. -
Citations
Citations to this article as recorded by- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women
S. Han, S. Kim, E.J. Yeh, H.S. Suh
Osteoporosis International.2024; 35(2): 339. CrossRef - Duration of osteoporosis treatment to reduce the risk of subsequent osteoporotic fracture and all-cause mortality in elderly hip fracture patients in a Korean real-world study
Soong Joon Lee, Minjoon Cho, Hojoon Lee, Hyuna Lim, Jae Hyup Lee
Archives of Osteoporosis.2024;[Epub] CrossRef - Do Patients with Benign Paroxysmal Positional Vertigo Have a Higher Prevalence of Osteoporosis? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Keunho Kim, Yeonjoo Choi
Journal of Personalized Medicine.2024; 14(3): 303. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Chronic airway disease as a major risk factor for fractures in osteopenic women: Nationwide cohort study
Sung Hye Kong, Ae Jeong Jo, Chan Mi Park, Kyun Ik Park, Ji Eun Yun, Jung Hee Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biomimetic Porous Magnesium Alloy Scaffolds Promote the Repair of Osteoporotic Bone Defects in Rats through Activating the Wnt/β-Catenin Signaling Pathway
Yuanchao Zhu, Gaozhi Jia, Yifei Yang, Jian Weng, Su Liu, Mengwei Zhang, Geng Zhang, Haotian Qin, Yixiao Chen, Qi Yang, Guangyin Yuan, Fei Yu, Hui Zeng
ACS Biomaterials Science & Engineering.2023; 9(6): 3435. CrossRef - Correlation between bone mineral density and bone metabolic markers in postmenopausal women with osteoporotic fractures at different C-terminal telopeptide of type 1 collagen levels: a retrospective analysis study
Xiaonan Zhu, Lin Chen, Ling Pan, Yuexi Zeng, Qiang Fu, Yanbin Liu, Yongde Peng, Yufan Wang, Li You
Menopause.2023; 30(11): 1139. CrossRef - Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
Endocrinology and Metabolism.2023; 38(6): 669. CrossRef - A Meaningful Journey to Predict Fractures with Deep Learning
Jeonghoon Ha
Endocrinology and Metabolism.2022; 37(4): 617. CrossRef - The Efficacy of Selective Estrogen Receptor Modulators Monotherapies in Postmenopausal Women with Osteopenia
Kyung Wook Kim, Young Il Kim, Ki-Choul Kim
Journal of Bone Metabolism.2022; 29(3): 185. CrossRef - Correlation of Psoas Muscle Index with Fragility Vertebral Fracture: A Retrospective Cross-Sectional Study of Middle-Aged and Elderly Women
Yihui Zhang, Yilihamu Dilixiati, Wei Jiang, Xiufeng Cao, Yuanyuan Chen, Hui Guo, Christian-Heinz Anderwald
International Journal of Endocrinology.2022; 2022: 1. CrossRef
- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women

- Clinical Study
- Urinary Albumin Excretion Reflects Cardiovascular Risk in Postmenopausal Women without Diabetes: The 2011 to 2013 Korean National Health and Nutrition Examination Survey
- Hee Jung Ahn, Do Sik Moon, Da Yeong Kang, Jung In Lee, Da Young Kim, Jin Hwa Kim, Sang Yong Kim, Hak Yeon Bae
- Endocrinol Metab. 2016;31(4):537-546. Published online November 3, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.537
- 3,565 View
- 31 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The objective of the current study was to determine whether there was an association between urinary albumin excretion and cardiovascular disease (CVD) risk by estimating the Framingham Risk Score (FRS) in postmenopausal women without diabetes.
Methods This study was based on data from the Korea National Health and Nutrition Examination Survey, which was conducted by the Korean Ministry of Health and Welfare in 2011 to 2013. Data on 2,316 postmenopausal women from a total of 24,594 participants was included in the analysis.
Results The mean FRS was significantly different in each of the urinary albumin to creatinine ratio (UACR) subgroups, and it increased with UACR. The FRS was 12.69±0.12 in the optimal group, 14.30±0.19 in the intermediate normal group, 14.62±0.26 in the high normal group, and 15.86±0.36 in the microalbuminuria group. After fully adjusting for potential confounding factors, high normal levels and microalbuminuria were significantly associated with the highest tertile of FRS ([odds ratio (OR), 1.642; 95% confidence interval (CI), 1.124 to 2.400] and [OR, 3.385; 95% CI, 2.088 to 5.488], respectively) compared with the optimal subgroup. High normal levels and microalbuminuria were also significantly associated with a ≥10% 10-year risk of CVD ([OR, 1.853; 95% CI, 1.122 to 3.060] and [OR, 2.831; 95% CI, 1.327 to 6.037], respectively) after adjusting for potential confounding covariates.
Conclusion Urinary albumin excretion reflects CVD risk in postmenopausal women without diabetes, and high normal levels and microalbuminuria were independently associated with a higher risk of CVD.
-
Citations
Citations to this article as recorded by- Association between urinary albumin creatinine ratio and cardiovascular disease
Yoo Jin Kim, Sang Won Hwang, Taesic Lee, Jun Young Lee, Young Uh, Gulali Aktas
PLOS ONE.2023; 18(3): e0283083. CrossRef - Relationship between Hypertension and the Declining Renal Function in Korean Adults
Jun Ho Lee
The Korean Journal of Clinical Laboratory Science.2021; 53(1): 32. CrossRef - Significance of Obstetrical History with Future Cardiovascular Disease Risk
Emmanuel Bassily, Cameron Bell, Sean Verma, Nidhi Patel, Aarti Patel
The American Journal of Medicine.2019; 132(5): 567. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Association between urinary albumin creatinine ratio and cardiovascular disease

- Clinical Study
- High Levels of Serum DPP-4 Activity Are Associated with Low Bone Mineral Density in Obese Postmenopausal Women
- Sang-Wook Kim, Eun-Hee Cho
- Endocrinol Metab. 2016;31(1):93-99. Published online March 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.1.93
- 3,493 View
- 39 Download
- 11 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase 4/CD26 (DPP-4) is a widely expressed cell surface serine protease. DPP-4 inhibitors, one of common anti-diabetic agents play a protective role in bone metabolism in recent studies. A soluble form of DPP-4 is found in serum, and exhibits DPP-4 enzymatic activity. However, the physiological role of serum or soluble DPP-4 and its relationship with DPP-4 enzymatic function remain poorly understood. The aims of current study were to determine the association between serum DPP-4 activity and bone mineral density (BMD) in postmenopausal women.
Methods We recruited data and serum samples from 124 consecutive healthy postmenopausal women aged >50 years. We divided study subjects into obese (body mass index [BMI] ≥25 kg/m2) and non-obese (BMI <25 kg/m2) postmenopausal women and examined the correlation between serum DPP-4 activity and clinical variables in each groups.
Results A total of 124 postmenopausal women was enrolled, with a mean age of 59.9±7.1 years. The mean BMI of the study patients was 24.4±2.8 kg/m2. Regarding bone turnover markers, serum DPP-4 activity was positively correlated with serum calcium concentrations, intact parathyroid hormone, and serum C-telopeptide levels in all of the study subjects. However, there was no association between serum DPP-4 activity and BMD in the spine or femoral neck in all of the study subjects. Serum DPP-4 activity was negatively correlated (
R =−0.288,P =0.038) with BMD of the spine in obese postmenopausal women.Conclusion This study demonstrated for the first time that serum soluble DPP-4 activity was negatively correlated with BMD in obese postmenopausal women.
-
Citations
Citations to this article as recorded by- A novel mechanism of Vildagliptin in regulating bone metabolism and mitigating osteoporosis
Jinwen He, Dacheng Zhao, Bo Peng, Xingwen Wang, Shenghong Wang, Xiaobing Zhao, Peng Xu, Bin Geng, Yayi Xia
International Immunopharmacology.2024; 130: 111671. CrossRef - Comparative evaluation of Sodium-glucose co-transporter-2 inhibitors and dipeptidyl peptidase-4 inhibitors influence on bone turnover markers in rats with experimental type 2 diabetes mellitus
N. V. Timkina, A. V. Simanenkova, T. L. Karonova, T. D. Vlasov, N. Yu. Semenova, А. A. Bairamov, V. A. Timofeeva, A. A. Shimshilashvili, E. V. Shlyakhto
Osteoporosis and Bone Diseases.2022; 24(4): 27. CrossRef - The relationship between bone marrow adipose tissue and bone metabolism in postmenopausal osteoporosis
Jiao Li, Xiang Chen, Lingyun Lu, Xijie Yu
Cytokine & Growth Factor Reviews.2020; 52: 88. CrossRef - Update on: effects of anti-diabetic drugs on bone metabolism
Guillaume Mabilleau, Béatrice Bouvard
Expert Review of Endocrinology & Metabolism.2020; 15(6): 415. CrossRef - Soluble Dipeptidyl Peptidase-4 Levels Are Associated with Decreased Renal Function in Patients with Type 2 Diabetes Mellitus
Eun-Hee Cho, Sang-Wook Kim
Diabetes & Metabolism Journal.2019; 43(1): 97. CrossRef - Marrow Adipose Tissue: Its Origin, Function, and Regulation in Bone Remodeling and Regeneration
Qiwen Li, Yunshu Wu, Ning Kang
Stem Cells International.2018; 2018: 1. CrossRef - Association between Serum Dipeptidyl Peptidase-4 Concentration and Obesity-related Factors in Health Screen Examinees
Ji Yeon Lee, Byoung Kuk Jang, Min Kyung Song, Hye Soon Kim, Mi-Kyung Kim
Journal of Obesity & Metabolic Syndrome.2017; 26(3): 188. CrossRef - Association of DPP-4 activity with BMD, body composition, and incident hip fracture: the Cardiovascular Health Study
L. D. Carbone, P. Bůžková, H. A. Fink, J. A. Robbins, M. Bethel, C. M. Isales, W. D. Hill
Osteoporosis International.2017; 28(5): 1631. CrossRef - Adipocyte Accumulation in the Bone Marrow during Obesity and Aging Impairs Stem Cell-Based Hematopoietic and Bone Regeneration
Thomas H. Ambrosi, Antonio Scialdone, Antonia Graja, Sabrina Gohlke, Anne-Marie Jank, Carla Bocian, Lena Woelk, Hua Fan, Darren W. Logan, Annette Schürmann, Luis R. Saraiva, Tim J. Schulz
Cell Stem Cell.2017; 20(6): 771. CrossRef - The emerging role of bone marrow adipose tissue in bone health and dysfunction
Thomas H. Ambrosi, Tim J. Schulz
Journal of Molecular Medicine.2017; 95(12): 1291. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Dipeptidyl Peptidase-4 and Adolescent Idiopathic Scoliosis: Expression in Osteoblasts
Emilie Normand, Anita Franco, Alain Moreau, Valérie Marcil
Scientific Reports.2017;[Epub] CrossRef - Effect of Dipeptidyl Peptidase-4 Inhibitors on Bone Metabolism and the Possible Underlying Mechanisms
Yinqiu Yang, Chenhe Zhao, Jing Liang, Mingxiang Yu, Xinhua Qu
Frontiers in Pharmacology.2017;[Epub] CrossRef
- A novel mechanism of Vildagliptin in regulating bone metabolism and mitigating osteoporosis

- The Effect of Hormone Replacement Therapy on Carotid Intima-Media Thickness in Healthy Postmenopausal Women.
- Jang Yel Shin, Bong Soo Cha, Choon Hee Chung, Won Heum Shim, Hyun Chul Lee
- J Korean Endocr Soc. 2006;21(1):14-21. Published online February 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.1.14
- 1,702 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cardiovascular disease is the leading cause of death in postmenopausal women. The use of hormone replacement therapy (HRT) preventing for cardiovascular disease in postmenopausal women remains controversial. We investigated the effect of HRT on carotid intima-media thickness (IMT) according to the HRT duration in healthy postmenopausal women. METHODS: One hundred and twenty postmenopausal women (mean age: 55.4 +/- 3.3 years) were classified into never users, short-term, and long-term users according to the HRT duration. Carotid IMT was measured, and the clinical and biochemical cardiovascular risk factors were examined. RESULTS: The mean IMT was significantly thinner in the long-term users than that in the never users (0.62 +/- 0.11 vs. 0.71 +/- 0.14 mm, P < 0.01). Also, the maximal IMT was significantly thinner in the short-term and the long-term users. However, there is no significant difference in the mean and maximal IMTs between the estrogen alone and estrogen plus progestins used group. The period exposed to menopause was significantly shorter in the long-term users than that in the never users (1.8 +/- 2.3 vs. 4.3 +/- 3.3 years, P < 0.001). CONCLUSION: Our findings suggest that if HRT is initiated during early postmenopausal period before the onset of atherosclerosis, HRT may have a beneficial effect on the prevention of carotid atherosclerosis.

- Association between Serum Leptin Concentration and Bone Mineral Density in Healthy Korean Women.
- Yumie Rhee, Dae Jung Kim, Se Hwa Kim, Chul Woo Ahn, Bong Soo Cha, Kyung Rae Kim, Hyun Chul Lee, Sung Kil Lim
- J Korean Endocr Soc. 2003;18(2):177-183. Published online April 1, 2003
- 1,107 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Leptin is known to affect bone metabolism both centrally and peripherally. This study was performed to investigate the relationship between leptin and bone mineral density(BMD) in healthy premenopausal and postmenopausal Korean women. METHODS: 140 women were recruited for a routine health check-up. Anthro-pometric and biochemical data were checked as usual. BMDs were measured by dual x-ray absorptiometry of the spine and femur in 67 premenopausal women and 73 postmenopausal women, in addition to their serum leptin levels. RESULTS: Serum leptin level showed no correlation with BMD in premenopausal women, but there was a positive correlation betwen serum leptin and spinal BMD in postmenopausal women(r=0.468, p<0.001). After the correcting for age, body mass index, and duration of menopause, the serum leptin level and BMD still showed a positive correlation(r=0.217, p=0.088) although weak. The women in the lowest quartile of serum leptin level showed significantly lower lumbar and femoral neck BMD. CONCLUSION: Leptin level seems to have a weak relationship with BMD showing different features in premenopausal and postmenopausal women.

- Association of Estrogen Receptor Genotypes with Serum Lipids and Responsiveness of Serum Lipids to Hormonal Replacement Therapy in Korean Postmenopausal Women.
- So Ra Park, Jae Eun Park, Chung Kyu Hwang, Phil Ho Jung, Chang Hoon Yim, Ho Yeon Chung, Ki Ok Han, Hyun Ku Yoon, Hak Chul Jang, In Kwon Han
- J Korean Endocr Soc. 1999;14(3):553-561. Published online January 1, 2001
- 1,058 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Several biologically plausible mechanisms have been proposed for estrogen-mediated caridoprotection, including estrogen-assocaited changes in lipid metabolism and endothelial function of vessel walls. These effects are thought to be mediated via estrogen receptor (ER). Relationships between ER polymorphisms and serum lipid levels were not investigated enoughly. METHODS: Three restriction fragment length polymorphisms (RFLPs) at the ER gene locus, represented as B-variant, PvuII and XbaI, and their relationship to serum lipid levels were examined in 318 postmenopausal women. Their mean age was 54.5+/-6.5 years (mean+SD). An association between ER genotypes and changes in lipid levels after 1 year of estrogen replacement therapy was also investigated in follow-up 251 women. RESULTS: The B-variant was not found in Korean women. The distribution of the PvuII and XbaI polymorphisms was as follows: PP 109 (34%), Pp 166 (52%), pp 43 (14%), and XX 204 (64%), Xx 95 (30%), xx 19 (6%). Significant relationship was found between genotypes and changes in serum total cholesterol levels after lyr estrogen replacement therapy. There was no significant relationship between ER genotypes and changes in HDL cholesterol, LDL cholesterol and triglyceride levels after estrogen therapy. CONCLUSION: These data indicate that these polymorphisms are possible predictor on lipid response to estrogen replacement therapy.

- The Repreducitve History and Other Potential Risk Factors as The Determinants of Bone Mineral Density at Postmenopause.
- Min Kyung Song, Young Jun Won, Suk Won Park, Young Duk Song, Sung Kil Lim, Jae Jun Oh, Hyun Chul Lee, Kap Bum Huh
- J Korean Endocr Soc. 1999;14(1):91-101. Published online January 1, 2001
- 1,006 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The purpose of this study was to determine the associations of the potential risk factors including reproductive history and lifestyle factors with bone mineral density at postmenopause. METHODS: The bone mineral density of the lumbar spine and proximal femur were measured by dual energy X-ray absorptiometry (DEXA), and physical and anthropometric data were obtained in 187 healthy postmenopausal women aged 45 to 73. Informations about risk factors were assessed by questionairres including medicosurgical and family history, reproductive history and lifestyle factors (dietary calcium intake, past use of oral contraceptives, consumption of alcohol and caffeine, smoking habits and exercise pattern). RESULTS: 1) Each prevalence of osteopenia and osteoporosis was 43.9% and 16.6% in postmenopausal women. 2) In simple correlation analysis between each risk factor and bone mineral density, factors associated with higher level in body mineral density (BMD) were body mass index (BMI)(p<0.01) and reproductive periods (p<0.05) in lumar spine and femur neck, and exerecise strength in femur neck (p<0.05). On the other hand, more aging and longer postmnopausal periods, lower BMD in lumbar spine and femur (p<0.01) and later menarche, lower BMD in lumbar spine (p<0.01) and femur neck (p<0.05) and higher frequencies of parity were influenced on lower BMD in lumbar spine and femur wards (p<0.01) and femur neck (p<0.05). But the other factors had no relation to BMD. 3) There was no significant difference in BMD according to the amount of diet calcium intake, gravity, lactation, the past use of oral contraceptives, the family history of osteoporosis, smoking habits and intake of caffeine and alcohol. 4) No reproductive history and other risk factors were significantly associated with BMD after the influences of age, postmenopausal periods and BMI were adjusted in multiple regression analysis. CONCLUSION: These results show there are no consistent effects on bone mineral density, after adjusting for age and BMI, of reproductive history and any other risk factors in postmenopausal women.


 KES
KES

 First
First Prev
Prev



