Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Treatment of Hypoparathyroidism by Re-Establishing the Effects of Parathyroid Hormone
- Lars Rejnmark
- Endocrinol Metab. 2024;39(2):262-266. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1916
- 1,292 View
- 77 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
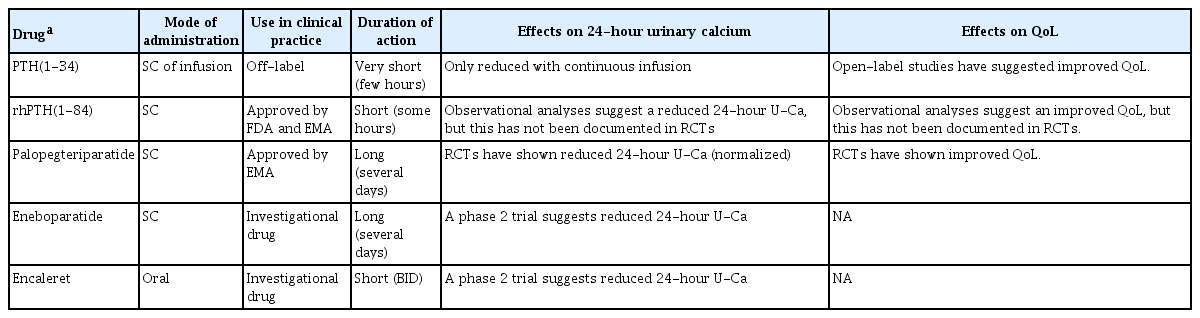
ePub - The conventional treatment of hypoparathyroidism (HypoPT) includes active vitamin D and calcium. Despite normalization of calcium levels, the conventional treatment is associated with fluctuations in calcium levels, hypercalciuria, renal impairment, and decreased quality of life (QoL). Replacement therapy with parathyroid hormone (PTH)(1-84) is an option in some countries. However, convincing beneficial effects have not been demonstrated, which may be due to the short duration of action of this treatment. Recently, palopegteriparatide (also known as TransCon PTH) has been marketed in Europe and is expected also to be approved in other countries. Palopegteriparatide is a prodrug with sustained release of PTH(1-34) designed to provide stable physiological PTH levels for 24 hours/day. A phase 3 study demonstrated maintenance of normocalcemia in patients with chronic HypoPT, with no need for conventional therapy. Furthermore, this treatment lowers urinary calcium and improves QoL. Another long-acting PTH analog with effects on the parathyroid hormone receptor (eneboparatide) is currently being tested in a phase 3 trial. Furthermore, the treatment of autosomal dominant hypocalcemia type 1 with a calcilytic (encaleret) is also being tested. All in all, improved treatment options are on the way that will likely take the treatment of HypoPT to the next level.

- Calcium & bone metabolism
- Protein Signatures of Parathyroid Adenoma according to Tumor Volume and Functionality
- Sung Hye Kong, Jeong Mo Bae, Jung Hee Kim, Sang Wan Kim, Dohyun Han, Chan Soo Shin
- Endocrinol Metab. 2024;39(2):375-386. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1827
- 1,056 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
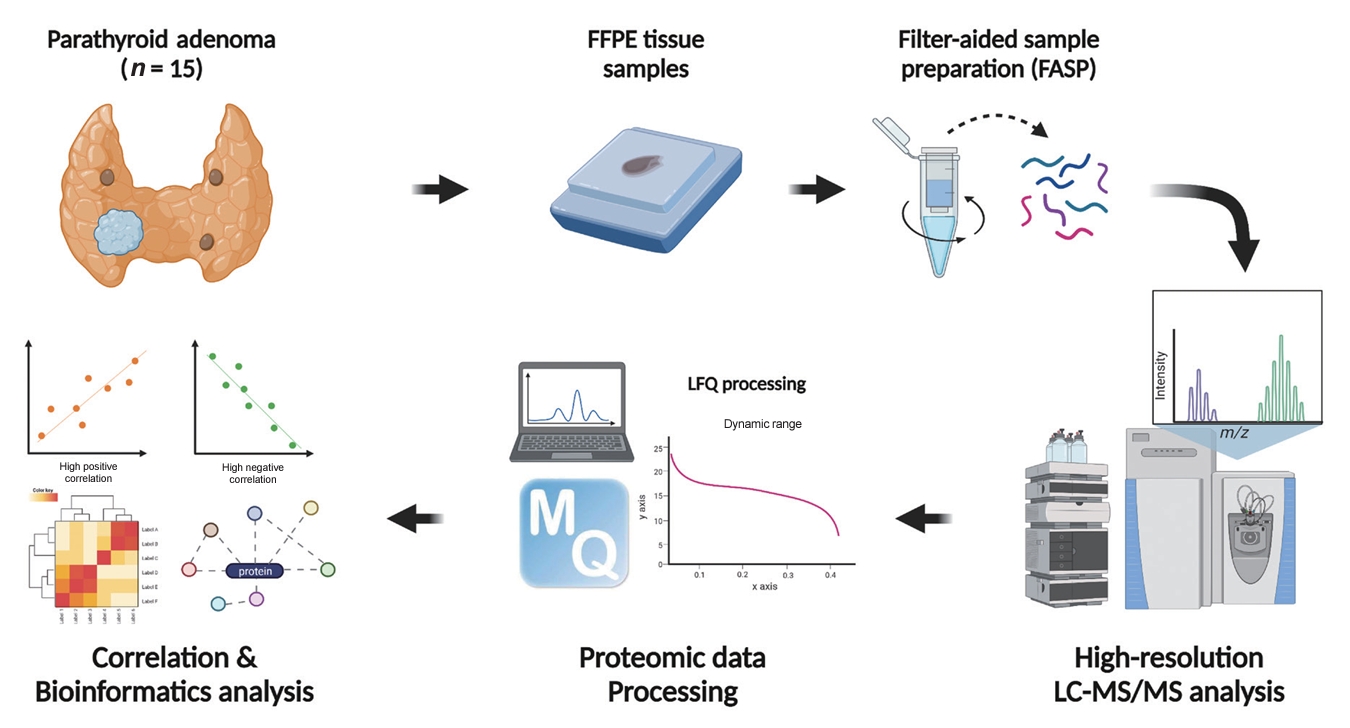
Parathyroid adenoma (PA) is a common endocrine disease linked to multiple complications, but the pathophysiology of the disease remains incompletely understood. The study aimed to identify the key regulator proteins and pathways of PA according to functionality and volume through quantitative proteomic analyses.
Methods
We conducted a retrospective study of 15 formalin-fixed, paraffin-embedded PA samples from tertiary hospitals in South Korea. Proteins were extracted, digested, and the resulting peptides were analyzed using liquid chromatography-tandem mass spectrometry. Pearson correlation analysis was employed to identify proteins significantly correlated with clinical variables. Canonical pathways and transcription factors were analyzed using Ingenuity Pathway Analysis.
Results
The median age of the participants was 52 years, and 60.0% were female. Among the 8,153 protein groups analyzed, 496 showed significant positive correlations with adenoma volume, while 431 proteins were significantly correlated with parathyroid hormone (PTH) levels. The proteins SLC12A9, LGALS3, and CARM1 were positively correlated with adenoma volume, while HSP90AB2P, HLA-DRA, and SCD5 showed negative correlations. DCPS, IRF2BPL, and FAM98A were the main proteins that exhibited positive correlations with PTH levels, and SLITRK4, LAP3, and AP4E1 had negative correlations. Canonical pathway analysis demonstrated that the RAN and sirtuin signaling pathways were positively correlated with both PTH levels and adenoma volume, while epithelial adherence junction pathways had negative correlations.
Conclusion
Our study identified pivotal proteins and pathways associated with PA, offering potential therapeutic targets. These findings accentuate the importance of proteomics in understanding disease pathophysiology and the need for further research.

- Calcium & bone metabolism
- New Insights into Calorie Restriction Induced Bone Loss
- Linyi Liu, Clifford J. Rosen
- Endocrinol Metab. 2023;38(2):203-213. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1673

- 3,399 View
- 176 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Caloric restriction (CR) is now a popular lifestyle choice due to its ability in experimental animals to improve lifespan, reduce body weight, and lessen oxidative stress. However, more and more emerging evidence suggests this treatment requires careful consideration because of its detrimental effects on the skeletal system. Experimental and clinical studies show that CR can suppress bone growth and raise the risk of fracture, but the specific mechanisms are poorly understood. Reduced mechanical loading has long been thought to be the primary cause of weight loss-induced bone loss from calorie restriction. Despite fat loss in peripheral depots with calorie restriction, bone marrow adipose tissue (BMAT) increases, and this may play a significant role in this pathological process. Here, we update recent advances in our understanding of the effects of CR on the skeleton, the possible pathogenic role of BMAT in CR-induced bone loss, and some strategies to mitigate any potential side effects on the skeletal system.
-
Citations
Citations to this article as recorded by- Obesity, diabetes and risk of bone fragility: How BMAT behavior is affected by metabolic disturbances and its influence on bone health
Gregório Corrêa Guimarães, João Bosco Costa Coelho, João Gabriel Oliveira Silva, Ana Carolina Chalfun de Sant’Ana, Cássia Alves Carrilho de Sá, Júlia Marques Moreno, Lívia Marçal Reis, Camila Souza de Oliveira Guimarães
Osteoporosis International.2024; 35(4): 575. CrossRef - Bone Marrow Adipose Tissue Is Not Required for Reconstitution of the Immune System Following Irradiation in Male Mice
Jessica A. Keune, Carmen P. Wong, Adam J. Branscum, Scott A. Menn, Urszula T. Iwaniec, Russell T. Turner
International Journal of Molecular Sciences.2024; 25(4): 1980. CrossRef - Dietary restriction plus exercise change gene expression of Cxcl12 abundant reticular cells in female mice
Aoi Ikedo, Yuuki Imai
Journal of Bone and Mineral Metabolism.2024;[Epub] CrossRef - Once-weekly semaglutide versus placebo in adults with increased fracture risk: a randomised, double-blinded, two-centre, phase 2 trial
Morten S. Hansen, Eva M. Wölfel, Shakespeare Jeromdesella, Jens-Jakob K. Møller, Charlotte Ejersted, Niklas R. Jørgensen, Richard Eastell, Stinus G. Hansen, Morten Frost
eClinicalMedicine.2024; 72: 102624. CrossRef
- Obesity, diabetes and risk of bone fragility: How BMAT behavior is affected by metabolic disturbances and its influence on bone health

- Calcium & Bone Metabolism
- Update on Preoperative Parathyroid Localization in Primary Hyperparathyroidism
- Hye-Sun Park, Namki Hong, Jong Ju Jeong, Mijin Yun, Yumie Rhee
- Endocrinol Metab. 2022;37(5):744-755. Published online October 25, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1589

- 4,203 View
- 359 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Parathyroidectomy is the treatment of choice for primary hyperparathyroidism when the clinical criteria are met. Although bilateral neck exploration is traditionally the standard method for surgery, minimally invasive parathyroidectomy (MIP), or focused parathyroidectomy, has been widely accepted with comparable curative outcomes. For successful MIP, accurate preoperative localization of parathyroid lesions is essential. However, no consensus exists on the optimal approach for localization. Currently, ultrasonography and technetium-99m-sestamibi–single photon emission computed tomography/computed tomography are widely accepted in most cases. However, exact localization cannot always be achieved, especially in cases with multiglandular disease, ectopic glands, recurrent disease, and normocalcemic primary hyperparathyroidism. Therefore, new modalities for preoperative localization have been developed and evaluated. Positron emission tomography/computed tomography and parathyroid venous sampling have demonstrated improvements in sensitivity and accuracy. Both anatomical and functional information can be obtained by combining these methods. As each approach has its advantages and disadvantages, the localization study should be deliberately chosen based on each patient’s clinical profile, costs, radiation exposure, and the availability of experienced experts. In this review, we summarize various methods for the localization of hyperfunctioning parathyroid tissues in primary hyperparathyroidism.
-
Citations
Citations to this article as recorded by- Expression of the Calcium-Sensing Receptor on Normal and Abnormal Parathyroid and Thyroid Tissue
Anne L. Worth, Mesrop Ayrapetyan, Susan J. Maygarden, Zibo Li, Zhanhong Wu, Chris B. Agala, Lawrence T. Kim
Journal of Surgical Research.2024; 293: 618. CrossRef - Use of [18F]fluorocholine PET/CT in the detection of primary hyperparathyroidism in paediatrics: a case report
Helena Martínez Sánchez, Francisca Moreno Macián, Sara León Cariñena, Carmen de Mingo Alemany, Lidia Blasco González, Raquel Sánchez Vañó
Journal of Pediatric Endocrinology and Metabolism.2024;[Epub] CrossRef - A Rare Case of Hyperfunctioning Lipoadenoma Presenting as a Cystic Pararthyroid Lesion
Jinyoung Kim, Ohjoon Kwon, Tae-Jung Kim, So Lyung Jung, Eun Ji Han, Ki-Ho Song
Journal of Bone Metabolism.2023; 30(2): 201. CrossRef - Role of 18F-Fluorocholine Positron Emission Tomography (PET)/Computed Tomography (CT) in Diagnosis of Elusive Parathyroid Adenoma
Janan R Badier, Pokhraj P Suthar, Jagadeesh S Singh, Miral D Jhaveri
Cureus.2023;[Epub] CrossRef - Pitfalls of DualTracer 99m-Technetium (Tc) Pertechnetate and Sestamibi Scintigraphy before Parathyroidectomy: Between Primary-Hyperparathyroidism-Associated Parathyroid Tumour and Ectopic Thyroid Tissue
Mara Carsote, Mihaela Stanciu, Florina Ligia Popa, Oana-Claudia Sima, Eugenia Petrova, Anca-Pati Cucu, Claudiu Nistor
Medicina.2023; 60(1): 15. CrossRef - Diagnostic Performance of Magnetic Resonance Imaging for Parathyroid Localization of Primary Hyperparathyroidism: A Systematic Review
Max H. M. C. Scheepers, Zaid Al-Difaie, Lloyd Brandts, Andrea Peeters, Bjorn Winkens, Mahdi Al-Taher, Sanne M. E. Engelen, Tim Lubbers, Bas Havekes, Nicole D. Bouvy, Alida A. Postma
Diagnostics.2023; 14(1): 25. CrossRef
- Expression of the Calcium-Sensing Receptor on Normal and Abnormal Parathyroid and Thyroid Tissue

- Bone Metabolism
- Normocalcemic Primary Hyperparathyroidism: Need for a Standardized Clinical Approach
- Guido Zavatta, Bart L. Clarke
- Endocrinol Metab. 2021;36(3):525-535. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1061

- 6,456 View
- 381 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since normocalcemic primary hyperparathyroidism (NHPT) was first defined at the Third International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism in 2008, many papers have been published describing its prevalence and possible complications. Guidelines for the management of this condition are still lacking, and making the diagnosis requires fulfillment of strict criteria. Recent studies have shown that intermittent oscillations of serum calcium just below and slightly above the normal limits are very frequent, therefore challenging the assumption that serum calcium must be consistently normal to make the diagnosis. There is debate if these variations in serum calcium outside the normal range should be included under the rubric of NHPT or, rather, a milder form of classical primary hyperparathyroidism. Innovative approaches to define NHPT have been proposed that still need to be validated in prospective studies. Non-classical complications, especially cardiovascular complications, have been associated with NHPT, indicating that hyperparathyroidism may be a cardiovascular risk factor. New associations between parathyroid hormone (PTH) and several other comorbidities have also been reported from observational studies, suggesting that excessive PTH secretion might cause tissue dysfunction independent of serum calcium. Heterogeneous studies using different definitions of NHPT, however, make it difficult to draw definitive conclusions regarding the role of PTH excess when complications other than osteoporosis or kidney stones are described. This review will focus on clinical aspects and suggest an approach to NHPT.
-
Citations
Citations to this article as recorded by- Surgery for Normocalcemic Hyperparathyroidism
Pallavi Kulkarni, David Goldenberg
Otolaryngologic Clinics of North America.2024; 57(1): 111. CrossRef - Linea guida sulla gestione terapeutica dell’iperparatiroidismo primario sporadico nell’adulto
Fabio Vescini, Marco Boniardi, Marina Carotti, Elena Castellano, Cristiana Cipriani, Cristina Eller-Vainicher, Sandro Giannini, Maurizio Iacobone, Francesca Pace, Antonio Stefano Salcuni, Federica Saponaro, Stefano Spiezia, Annibale Versari, Guido Zavatta
L'Endocrinologo.2024; 25(2): 222. CrossRef - Evaluation of the Thiazide Challenge Test to Differentiate Primary From Hypercalciuria-Related Hyperparathyroidism
Ewout Verly, Bruno Lapauw, Charlotte Verroken
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - DXA-based bone strain index in normocalcemic primary hyperparathyroidism
Gaia Tabacco, Anda Mihaela Naciu, Carmelo Messina, Gianfranco Sanson, Luca Rinaudo, Roberto Cesareo, Stefania Falcone, Nicola Napoli, Fabio Massimo Ulivieri, Andrea Palermo
Osteoporosis International.2023; 34(5): 999. CrossRef - Iperparatiroidismo primario normocalcemico
Silvia Egiddi, Luigi Bonifazi Meffe, Anda Mihaela Naciu, Gaia Tabacco, Nicola Napoli, Andrea Palermo
L'Endocrinologo.2023; 24(3): 249. CrossRef - The Russian registry of primary hyperparathyroidism, latest update
Natalia G. Mokrysheva, Anna K. Eremkina, Alina R. Elfimova, Elena V. Kovaleva, Anastasiia P. Miliutina, Ekaterina E. Bibik, Anna M. Gorbacheva, Ekaterina A. Dobreva, Irina S. Maganeva, Julia A. Krupinova, Rustam H. Salimkhanov, Lizaveta A. Aboishava, Elen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Incidental Normocalcemic Primary Hyperparathyroidism Presenting With Symptomatic Hypophosphatemia: A Case Report
Omar Tabbikha, Joanne Chamy, Michael El Khoury
Cureus.2023;[Epub] CrossRef - Long-term effects of hypercalcemia in kidney transplant recipients with persistent hyperparathyroidism
Juan Carlos Ramirez-Sandoval, Lluvia Marino, Gabriel Cojuc-Konigsberg, Estefania Reul-Linares, Nathalie Desire Pichardo-Cabrera, Cristino Cruz, Elisa Naomi Hernández-Paredes, Nathan Berman-Parks, Vanessa Vidal-Ruíz, Jonathan Mauricio Estrada-Linares, Alfr
Journal of Nephrology.2023;[Epub] CrossRef - Evaluating Patients for Secondary Causes of Osteoporosis
E. Michael Lewiecki
Current Osteoporosis Reports.2022; 20(1): 1. CrossRef - Preoperative Thoracic Muscle Mass Predicts Bone Density Change After Parathyroidectomy in Primary Hyperparathyroidism
Seung Won Burm, Namki Hong, Seunghyun Lee, Gi Jeong Kim, Sang Hyun Hwang, Jongju Jeong, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2474. CrossRef - Applications of Metabolomics in Calcium Metabolism Disorders in Humans
Beata Podgórska, Marta Wielogórska-Partyka, Joanna Godzień, Julia Siemińska, Michał Ciborowski, Małgorzata Szelachowska, Adam Krętowski, Katarzyna Siewko
International Journal of Molecular Sciences.2022; 23(18): 10407. CrossRef - Serum Calcium/Phosphorus Ratio in Biochemical Screening of Primary Hyperparathyroidism
Nagihan Bestepe, Fatma Neslihan Cuhaci, Burcak Polat, Berna Evranos Ogmen, Didem Ozdemir, Reyhan Ersoy, Bekir Cakir
Revista da Associação Médica Brasileira.2022; 68(12): 1668. CrossRef
- Surgery for Normocalcemic Hyperparathyroidism

- Miscellaneous
- Clinical Characteristics, Management, and Potential Biomarkers of Endocrine Dysfunction Induced by Immune Checkpoint Inhibitors
- Shintaro Iwama, Tomoko Kobayashi, Hiroshi Arima
- Endocrinol Metab. 2021;36(2):312-321. Published online April 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1007
- 5,595 View
- 268 Download
- 15 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
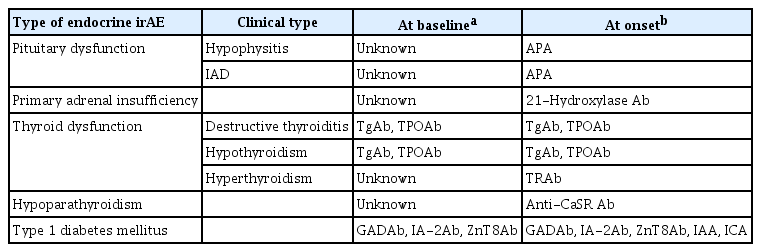
ePub - Immune-related adverse events (irAEs) affecting the endocrine glands are among the most frequent irAEs induced by immune checkpoint inhibitors (ICIs) and include hypopituitarism, primary adrenal insufficiency, thyrotoxicosis, hypothyroidism, hypoparathyroidism, and type 1 diabetes mellitus. Since the incidence and clinical features of endocrine irAEs vary according to the ICI used, it is important to understand the characteristics of these irAEs and to manage each one appropriately. Since some endocrine irAEs, including adrenal crisis and diabetic ketoacidosis, are potentially life-threatening, predicting the risk of endocrine irAEs before their onset is critical. Several autoantibodies have been detected in patients who develop endocrine irAEs, among which anti-thyroid antibodies may be predictive biomarkers of thyroid dysfunction. In this review, we describe the clinical features of each endocrine irAE induced by ICIs and discuss their potential biomarkers, including autoantibodies.
-
Citations
Citations to this article as recorded by- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events
Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima
Endocrine Journal.2024; 71(1): 23. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - Endocrinopathies Associated With Immune Checkpoint Inhibitor Use
Anupam Kotwal, Randol Kennedy, Nupur Kikani, Sonali Thosani, Whitney Goldner, Afreen Shariff
Endocrine Practice.2024;[Epub] CrossRef - Recovery from insulin dependence in immune checkpoint inhibitor‐associated diabetes mellitus: A case report
Marie Okubo, Yuji Hataya, Kanta Fujimoto, Toshio Iwakura, Naoki Matsuoka
Journal of Diabetes Investigation.2023; 14(1): 147. CrossRef - Case Report: A Rising Cause of New-Onset Endocrinopathies After Immunotherapy
Charity Tan, Sarah Hendricks, Kristina Hernandez, Martha Benavides, Rupinderjit Samra
The Journal for Nurse Practitioners.2023; 19(5): 104582. CrossRef - Risk of Thyroid Dysfunction in PD-1 Blockade Is Stratified by the Pattern of TgAb and TPOAb Positivity at Baseline
Xin Zhou, Shintaro Iwama, Tomoko Kobayashi, Masahiko Ando, Hiroshi Arima
The Journal of Clinical Endocrinology & Metabolism.2023; 108(10): e1056. CrossRef - Severe thyrotoxicosis induced by tislelizumab: a case report and literature review
Liman Huo, Chao Wang, Haixia Ding, Xuelian Shi, Bin Shan, Ruoying Zhou, Ping Liang, Juan Hou
Frontiers in Oncology.2023;[Epub] CrossRef - Life-Threatening Endocrinological Immune-Related Adverse Events of Immune Checkpoint Inhibitor Therapy
Aleksandra Basek, Grzegorz K. Jakubiak, Grzegorz Cieślar, Agata Stanek
Cancers.2023; 15(24): 5786. CrossRef - Increased Risk of Thyroid Dysfunction by PD-1 and CTLA-4 Blockade in Patients Without Thyroid Autoantibodies at Baseline
Shintaro Iwama, Tomoko Kobayashi, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Masahiko Ando, Xin Zhou, Ayana Yamagami, Takeshi Onoue, Yohei Kawaguchi, Takashi Miyata, Mariko Sugiyama, Hiroshi Takagi, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tets
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): e1620. CrossRef - Biomarkers and risk factors for the early prediction of immune-related adverse events: a review
Ying Zhang, Xiaoling Zhang, Weiling Li, Yunyi Du, Wenqing Hu, Jun Zhao
Human Vaccines & Immunotherapeutics.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors as a Threat to the Hypothalamus–Pituitary Axis: A Completed Puzzle
Agnese Barnabei, Andrea Corsello, Rosa Maria Paragliola, Giovanni Maria Iannantuono, Luca Falzone, Salvatore Maria Corsello, Francesco Torino
Cancers.2022; 14(4): 1057. CrossRef - Elevated TSH Level, TgAb, and Prior Use of Ramucirumab or TKIs as Risk Factors for Thyroid Dysfunction in PD-L1 Blockade
Tomoko Kobayashi, Shintaro Iwama, Ayana Yamagami, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Xin Zhou, Masahiko Ando, Takeshi Onoue, Takashi Miyata, Mariko Sugiyama, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tetsunari Hase, Masahiro Morise, Taka
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4115. CrossRef - Preconditioning of the immune system modulates the response of papillary thyroid cancer to immune checkpoint inhibitors
Fabiana Pani, Yoshinori Yasuda, Sylvie T Rousseau, Kevin C Bermea, Solmaz Roshanmehr, Rulin Wang, Srinivasan Yegnasubramanian, Patrizio Caturegli, Luigi Adamo
Journal for ImmunoTherapy of Cancer.2022; 10(12): e005538. CrossRef - Survival benefit of endocrine dysfunction following immune checkpoint inhibitors for nonthyroidal cancers
Anupam Kotwal, Mabel Ryder
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 517. CrossRef
- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events

- Clinical Study
- Radioactive Parathyroid Adenomas on Sestamibi Scans: Low Parathyroid Hormone Secretory Potential and Large Volume
- Sung Hye Kong, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
- Endocrinol Metab. 2021;36(2):351-358. Published online April 6, 2021
- DOI: https://doi.org/10.3803/EnM.2020.823

- 3,404 View
- 124 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We investigated the clinical characteristics of parathyroid adenomas according to radioactivity on 99mTc-methoxyisobutylisonitrile (99mTc-MIBI) single-photon emission computed tomography/computed tomography (SPECT/CT) in primary hyperparathyroidism (PHPT) patients.
Methods
The study included 217 patients diagnosed with PHPT from 2000 to 2019 at Seoul National University Hospital who underwent 99mTc-MIBI SPECT/CT scans. On SPECT/CT, the radioactivity of parathyroid adenomas was measured as the ratio of the mean radioactivity count of the parathyroid adenoma to that of the contralateral thyroid.
Results
Tumors were localized by MIBI scans in 190 patients (MIBI [+] group) and by ultrasound or parathyroid four-dimensional CT in 27 patients (MIBI [–] group). The mean age was 55 years, and mean body mass index was 23.4 kg/m2. Patients in the MIBI (+) group had higher parathyroid hormone (iPTH) and lower 25-hydroxy vitamin D levels than those in the MIBI (–) group (168.0 pg/mL [interquartile range, IQR, 111.0 to 250.7] vs. 134.7 pg/mL [IQR, 98.2 to 191.2], P=0.049; 15.4 ng/mL [IQR, 11.1 to 20.8] vs. 21.2 ng/mL [IQR, 13.9 to 24.8], P=0.012, respectively). Patients in the MIBI (+) group had larger tumor volumes, but lower iPTH/volume ratios than those in the MIBI (–) group (1,216.66 [IQR, 513.40 to 2,663.02], 499.82 mm3 [IQR, 167.77 to 1,229.80], P=0.002; 0.18 [IQR, 0.08 to 0.46], 0.40 pg/mL/mm3 [IQR, 0.16 to 1.29], P=0.016, respectively). Adenoma radioactivity was positively correlated with calcium, iPTH, and volume (r=0.180, P=0.020; r=0.208, P=0.006; r=0.288, P<0.001, respectively), but not with iPTH/volume.
Conclusion
Parathyroid adenomas with positive MIBI scans had larger volumes and higher iPTH than adenomas with negative scans, but lower iPTH per unit volume. -
Citations
Citations to this article as recorded by- Protein Signatures of Parathyroid Adenoma according to Tumor Volume and Functionality
Sung Hye Kong, Jeong Mo Bae, Jung Hee Kim, Sang Wan Kim, Dohyun Han, Chan Soo Shin
Endocrinology and Metabolism.2024; 39(2): 375. CrossRef - Incidentally detected follicular thyroid carcinoma mimicking parathyroid adenoma on Tc-99m MIBI scan: A case report
Yeon-Hee Han, Hwan-Jeong Jeong, Sun Young Lee, Seok Tae Lim
Medicine.2024; 103(18): e38107. CrossRef - Atypical parathyroid tumor: clinical and parathyroid hormone response to surgical treatment
Antonio Giulio Napolitano, Massimo Monacelli, Valeria Liparulo, Eleonora Coviello, Domenico Pourmolkara, Stefano Avenia, Andrea Polistena
Annals of Surgical Treatment and Research.2023; 105(2): 76. CrossRef - The Relationship between Planar and SPECT/CT Parameters and Functional Markers in Primary Hyperparathyroidism
Guler Silov, Serpil Erdogan Ozbodur
Diagnostics.2023; 13(20): 3182. CrossRef
- Protein Signatures of Parathyroid Adenoma according to Tumor Volume and Functionality

- Clinical Study
- Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study
- Chaiho Jeong, Hye In Kwon, Hansang Baek, Hun-Sung Kim, Dong-Jun Lim, Ki-Hyun Baek, Jeonghoon Ha, Moo Il Kang
- Endocrinol Metab. 2020;35(4):925-932. Published online December 10, 2020
- DOI: https://doi.org/10.3803/EnM.2020.725

- 5,451 View
- 184 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Concomitant papillary thyroid cancer (PTC) and hyperparathyroidism (HPT) have been reported in several studies. Our study aimed to investigate the incidence of concomitant PTC in HPT patients upon preoperative diagnosis and present a clinical opinion on detecting thyroid malignancy in case of parathyroidectomy.
Methods
Patients who underwent parathyroidectomy between January 2009 and December 2019 in two medical centers were included. Of the 279 participants 154 were diagnosed as primary hyperparathyroidism (pHPT) and 125 as secondary hyperparathyroidism (sHPT). The incidence of concomitant PTC and its clinical characteristics were compared with 98 patients who underwent thyroidectomy and were diagnosed with classical PTC during the same period.
Results
Concurrent PTC was detected in 14 patients (9.1%) with pHPT and in nine patients (7.2%) with sHPT. Ten (71.4%) and seven (77.8%) PTCs were microcarcinomas in the pHPT and sHPT cases respectively. In the pHPT patients, vitamin D was lower in the pHPT+PTC group (13.0±3.7 ng/mL) than in the pHPT-only group (18.5±10.4 ng/mL; P=0.01). Vitamin D levels were also lower in the sHPT+PTC group (12.3±5.6 ng/mL) than in the sHPT-only group (18.0±10.2 ng/mL; P=0.12). In the concomitant PTC group, lymph node ratio was higher than in the classical PTC group (P=0.00).
Conclusion
A high prevalence of concomitant PTC was seen in patients with pHPT and sHPT. Those concomitant PTCs were mostly microcarcinomas and had more aggressive features, suggesting that efforts should be made to detect concomitant malignancies in the preoperative parathyroidectomy evaluation. -
Citations
Citations to this article as recorded by- The unexpected effect of parathyroid adenoma on inflammation
Ahmet Tarik Harmantepe, Belma Kocer, Zulfu Bayhan, Emre Gonullu, Ugur Can Dulger
Updates in Surgery.2024; 76(2): 589. CrossRef - Evaluation of Nodular Goiter and Papillary Thyroid Cancer Coincidence in Patients with Primary Hyperparathyroidism
Mustafa ÇALIŞKAN, Hasret CENGİZ, Taner DEMİRCİ
Düzce Tıp Fakültesi Dergisi.2023; 25(2): 200. CrossRef - Papillary thyroid carcinoma coexisting with benign thyroid and parathyroid pathology: clinical and pathomorphological features
A. Dinets, M. Gorobeiko, V. Hoperia, A. Lovin, S. Tarasenko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2023; 19(4): 274. CrossRef - The Nexus of Hyperparathyroidism and Thyroid Carcinoma: Insights into Pathogenesis and Diagnostic Challenges—A Narrative Review
Gregorio Scerrino, Nunzia Cinzia Paladino, Giuseppina Orlando, Giuseppe Salamone, Pierina Richiusa, Stefano Radellini, Giuseppina Melfa, Giuseppa Graceffa
Journal of Clinical Medicine.2023; 13(1): 147. CrossRef - Is preoperative parathyroid localization necessary for tertiary hyperparathyroidism?
Rongzhi Wang, Peter Abraham, Brenessa Lindeman, Herbert Chen, Jessica Fazendin
The American Journal of Surgery.2022; 224(3): 918. CrossRef - Papillary thyroid carcinoma prevalence and its predictors in patients with primary hyperparathyroidism
Elif Tutku DURMUŞ, Ayşegül ATMACA, Mehmet KEFELİ, Ramis ÇOLAK, Buğra DURMUŞ, Cafer POLAT
Journal of Health Sciences and Medicine.2022; 5(5): 1499. CrossRef - Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (Endocrinol Metab 2020;35:925-32, Chaiho Jeong et al.)
Chaiho Jeong, Jeonghoon Ha, Moo Il Kang
Endocrinology and Metabolism.2021; 36(1): 205. CrossRef - Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (Endocrinol Metab 2020;35:925-32, Chaiho Jeong et al.)
Burcu Candemir, Coşkun Meriç
Endocrinology and Metabolism.2021; 36(1): 203. CrossRef
- The unexpected effect of parathyroid adenoma on inflammation

- Miscellaneous
- Rare PTH Gene Mutations Causing Parathyroid Disorders: A Review
- Joon-Hyop Lee, Munkhtugs Davaatseren, Sihoon Lee
- Endocrinol Metab. 2020;35(1):64-70. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.64

- 5,127 View
- 109 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Since parathyroid hormone (PTH) was first isolated and its gene (
PTH ) was sequenced, only eightPTH mutations have been discovered. The C18R mutation inPTH , discovered in 1990, was the first to be reported. This autosomal dominant mutation induces endoplasmic reticulum stress and subsequent apoptosis in parathyroid cells. The next mutation, which was reported in 1992, is associated with exon skipping. The substitution of G with C in the first nucleotide of the second intron results in the exclusion of the second exon; since this exon includes the initiation codon, translation initiation is prevented. An S23P mutation and an S23X mutation at the same residue were reported in 1999 and 2012, respectively. Both mutations resulted in hypoparathyroidism. In 2008, a somatic R83X mutation was detected in a parathyroid adenoma tissue sample collected from a patient with hyperparathyroidism. In 2013, a heterozygous p.Met1_Asp6del mutation was incidentally discovered in a case-control study. Two years later, the R56C mutation was reported; this is the only reported hypoparathyroidism-causing mutation in the mature bioactive part ofPTH . In 2017, another heterozygous mutation, M14K, was detected. The discovery of these eight mutations in thePTH gene has provided insights into its function and broadened our understanding of the molecular mechanisms underlying mutation progression. Further attempts to detect other such mutations will help elucidate the functions of PTH in a more sophisticated manner.-
Citations
Citations to this article as recorded by- The Intricacies of Renal Phosphate Reabsorption—An Overview
Valerie Walker
International Journal of Molecular Sciences.2024; 25(9): 4684. CrossRef - Molecular and Clinical Spectrum of Primary Hyperparathyroidism
Smita Jha, William F Simonds
Endocrine Reviews.2023; 44(5): 779. CrossRef - Rare cause of persistent hypocalcaemia in infancy due to PTH gene mutation
Savita Khadse, Vrushali Satish Takalikar, Radha Ghildiyal, Nikhil Shah
BMJ Case Reports.2023; 16(9): e256358. CrossRef - Homozygous Ser-1 to Pro-1 mutation in parathyroid hormone identified in hypocalcemic patients results in secretion of a biologically inactive pro-hormone
Patrick Hanna, Ashok Khatri, Shawn Choi, Severine Brabant, Matti L. Gild, Marie L. Piketty, Bruno Francou, Dominique Prié, John T. Potts, Roderick J. Clifton-Bligh, Agnès Linglart, Thomas J. Gardella, Harald Jüppner
Proceedings of the National Academy of Sciences.2023;[Epub] CrossRef - Genetics of monogenic disorders of calcium and bone metabolism
Paul J. Newey, Fadil M. Hannan, Abbie Wilson, Rajesh V. Thakker
Clinical Endocrinology.2022; 97(4): 483. CrossRef - Homozygous missense variant of PTH (c.166C>T, p.(Arg56Cys)) as the cause of familial isolated hypoparathyroidism in a three-year-old child
Stine Linding Andersen, Anja Lisbeth Frederiksen, Astrid Bruun Rasmussen, Mette Madsen, Ann-Margrethe Rønholt Christensen
Journal of Pediatric Endocrinology and Metabolism.2022; 35(5): 691. CrossRef - Novel PTH Gene Mutations Causing Isolated Hypoparathyroidism
Colin P Hawkes, Jamal M Al Jubeh, Dong Li, Susan E Tucker, Tara Rajiyah, Michael A Levine
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2449. CrossRef
- The Intricacies of Renal Phosphate Reabsorption—An Overview

- Clinical Study
- Impact of Subtotal Parathyroidectomy on Clinical Parameters and Quality of Life in Hemodialysis Patients with Secondary Hyperparathyroidism
- Mohamed Mimi Abd Elgawwad El-kholey, Ghada El-said Ibrahim, Osama Ibrahim Elshahat, Ghada El-Kannishy
- Endocrinol Metab. 2019;34(4):367-373. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.367
- 4,481 View
- 81 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Impairment of quality of life (QOL) is a key clinical characteristic of patients with end-stage renal disease (ESRD), and can be especially severe in the presence of secondary hyperparathyroidism (SHPT). Despite the proven success of parathyroidectomy (PTX) in controlling biochemical parameters in patients with severe SHPT, evidence is lacking regarding the effects of PTX on various clinical outcomes, including QOL.
Methods Twenty ESRD patients on maintenance hemodialysis with SHPT who underwent subtotal PTX were included in an observational longitudinal study. All studied patients underwent history-taking, clinical examinations, and laboratory investigations, including a complete blood count and measurements of serum calcium, phosphorus, magnesium, parathyroid hormone (PTH), and albumin levels preoperatively and at 3 months postoperatively. QOL was assessed before surgery and at 3 months after surgery using the Kidney Disease Quality of Life 36-Item Short-Form instrument.
Results After PTX, significant decreases in serum PTH and phosphorus levels were observed, as well as a significant increase in serum magnesium levels. Significant weight gain and improvements of QOL were also detected postoperatively.
Conclusion Subtotal PTX seems to be an efficient alternative to medical management in uncontrolled cases of SHPT, as it is capable of controlling the biochemical derangements that occur in hyperparathyroidism. Furthermore, PTX had a beneficial effect on clinical outcomes, as shown by weight gain and improvements in all QOL scales.
-
Citations
Citations to this article as recorded by- Abnormalities of serum magnesium levels in dialysis patients undergoing parathyroidectomy
Chi-Yu Kuo, Chung-Hsin Tsai, Jie-Jen Lee, Shih-Ping Cheng
Updates in Surgery.2024;[Epub] CrossRef - Effect of Parathyroidectomy on Quality of Life Among Patients Undergoing Dialysis
Lin Wang, Ming-Hui Xin, Yan Ma, Yu Wang, Meng-Yuan Hu, Qiang-Qiang Liu, Jin-Bor Chen
International Journal of General Medicine.2022; Volume 15: 1185. CrossRef - Paricalcitol versus Calcitriol + Cinacalcet for the Treatment of Secondary Hyperparathyroidism in Chronic Kidney Disease in China: A Cost-Effectiveness Analysis
Zhuolin Zhang, Lele Cai, Hong Wu, Xinglu Xu, Wenqing Fang, Xuan He, Xiao Wang, Xin Li
Frontiers in Public Health.2021;[Epub] CrossRef
- Abnormalities of serum magnesium levels in dialysis patients undergoing parathyroidectomy

- Miscellaneous
- Intraoperative Parathyroid Hormone Monitoring in the Surgical Management of Sporadic Primary Hyperparathyroidism
- Zahra F. Khan, John I. Lew
- Endocrinol Metab. 2019;34(4):327-339. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.327
- 5,499 View
- 122 Download
- 22 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Intraoperative parathyroid hormone monitoring (IPM) has been shown to be a useful adjunct during parathyroidectomy to ensure operative success at many specialized medical centers worldwide. Using the Miami or “>50% intraoperative PTH drop” criterion, IPM confirms the complete excision of all hyperfunctioning parathyroid tissue before the operation is finished, and helps guide the surgeon to identify additional hyperfunctioning parathyroid glands that may necessitate further extensive neck exploration when intraoperative parathyroid hormone (PTH) levels do not drop sufficiently. The intraoperative PTH assay is also used to differentiate parathyroid from non-parathyroid tissues during operations using fine needle aspiration samples and to lateralize the side of the neck harboring the hypersecreting parathyroid through differential jugular venous sampling when preoperative localization studies are negative or equivocal. The use of IPM underscores the recognition and understanding of sporadic primary hyperparathyroidism (SPHPT) as a disease of function rather than form, where the surgeon is better equipped to treat such patients with quantitative instead of qualitative information for durable long-term operative success. There has been a significant paradigm shift over the last 2 decades from conventional to focused parathyroidectomy guided by IPM. This approach has proven to be a safe and rapid operation requiring minimal dissection performed in an ambulatory setting for the treatment of SPHPT.
-
Citations
Citations to this article as recorded by- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy
Phillip Staibano, Kevin Um, Sheila Yu, Mohit Bhandari, Michael K. Gupta, Michael Au, JEM (Ted) Young, Han Zhang
Frontiers in Surgery.2024;[Epub] CrossRef - Primary Hyperparathyroidism
Saba Kurtom, Sally E. Carty
Surgical Clinics of North America.2024;[Epub] CrossRef - Characteristics, management and outcomes of primary hyperparathyroidism from 2009 to 2021: a single centre report from South Africa
Kamal Govind, Imran M. Paruk, Ayesha A. Motala
BMC Endocrine Disorders.2024;[Epub] CrossRef - Parathyroidectomy for primary hyperparathyroidism: A retrospective analysis of localization, surgical characteristics, and treatment outcomes
Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee, Jin Ho Sohn
Asian Journal of Surgery.2023; 46(2): 788. CrossRef - Magnitude of parathyroid hormone elevation in primary hyperparathyroidism: Does time of day matter?
C. Corbin Frye, Janessa Sullivan, Sai Anusha Sanka, Jingxia Liu, L. Michael Brunt, William Gillanders, Taylor C. Brown, T.K. Pandian
Surgery.2023; 173(3): 659. CrossRef - Analysis of intraoperative laboratory measurements and imaging techniques such as Tc-99 m-MIBI SPECT/CT, 18F-fluorocholine PET/CT and ultrasound in patients operated with prediagnosis of parathyroid adenoma
Nurullah Bilen, Mehmet Avni Gokalp, Latif Yilmaz, Alper Aytekin, Ilyas Baskonus
Irish Journal of Medical Science (1971 -).2023; 192(4): 1695. CrossRef - Intraoperative Parathyroid Hormone Monitoring Is of Limited Usefulness in Guiding Autotransplantation in Reoperative or Subtotal Parathyroidectomy for Primary Hyperparathyroidism
Bradley A. Richards, Robert A. Vierkant, Benzon M. Dy, Trenton R. Foster, Travis J. McKenzie, Melanie L. Lyden
The American Surgeon™.2023; 89(12): 5421. CrossRef - Does 18F-Fluorocholine PET/CT add value to positive parathyroid scintigraphy in the presurgical assessment of primary hyperparathyroidism?
Alessio Imperiale, Jacob Bani, Gianluca Bottoni, Adrien Latgé, Céline Heimburger, Ugo Catrambone, Michel Vix, Giorgio Treglia, Arnoldo Piccardo
Frontiers in Medicine.2023;[Epub] CrossRef - Intraoperative Identification of Thyroid and Parathyroid Tissues During Human Endocrine Surgery Using the MasSpec Pen
Rachel J. DeHoog, Mary E. King, Michael F. Keating, Jialing Zhang, Marta Sans, Clara L. Feider, Kyana Y. Garza, Alena Bensussan, Anna Krieger, John Q. Lin, Sunil Badal, Elizabeth Alore, Christopher Pirko, Kirtan Brahmbhatt, Wendong Yu, Raymon Grogan, Livi
JAMA Surgery.2023; 158(10): 1050. CrossRef - A Rare Case of Recurrent Parathyroid Adenomas After Initial Parathyroidectomy
Grant N Schalet, Luke Vincent, Carl Eguez, Gerardo Diaz, Mark S Shachner
Cureus.2023;[Epub] CrossRef - Surgical treatment of tertiary hyperparathyroidism: does one fit for all?
Claudio Casella, Claudio Guarneri, Manuela Campanile, Xavier Adhoute, Pier Paolo Gelera, Riccardo Morandi
Frontiers in Endocrinology.2023;[Epub] CrossRef - A >50% Intraoperative Parathyroid Hormone Decrease Into Normal Reference Range Predicts Complete Excision of Malignancy in Patients With Parathyroid Carcinoma
Valerie L. Armstrong, Tanaz M. Vaghaiwalla, Cima Saghira, Cheng-Bang Chen, Yujie Wang, Johan Anantharaj, Mehmet Ackin, John I. Lew
Journal of Surgical Research.2023;[Epub] CrossRef - Variation in parathyroid adenoma size in patients with sporadic, primary hyperparathyroidism: small gland size does not preclude single gland disease
Sophie Dream, Tina W. F. Yen, Kara Doffek, Douglas B. Evans, Tracy S. Wang
Langenbeck's Archives of Surgery.2022; 407(5): 2067. CrossRef - Role and Recent Trend of Intraoperative Parathyroid Hormone Monitoring During Parathyroidectomy in Patients With Primary Hyperparathyroidism
Dongbin Ahn, Ji Hye Kwak
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2022; 65(5): 253. CrossRef - Parathyroid Adenoma: Rare Cause of Acute Recurrent Pancreatitis
Shikha Mahajan, Alka Kumar, Vivek Aggarwal, Vikas Jain, Vipul Baweja, Ajay Ajmani, Diplomate CBNC, Fellow EBNM LNU
Annals of Pediatric Gastroenterology and Hepatology.2022; 2(3-4): 9. CrossRef - Long-term outcome of surgical techniques for sporadic primary hyperparathyroidism in a tertiary referral center in Belgium
Klaas Van Den Heede, Amélie Bonheure, Nele Brusselaers, Sam Van Slycke
Langenbeck's Archives of Surgery.2022; 407(7): 3045. CrossRef - Contribution of intraoperative parathyroid hormone monitoring to the surgical success in minimal invasive parathyroidectomy
Ismail Ethem Akgün, Mehmet Taner Ünlü, Nurcihan Aygun, Mehmet Kostek, Mehmet Uludag
Frontiers in Surgery.2022;[Epub] CrossRef - Surgery for primary hyperparathyroidism
Murilo Catafesta das Neves, Rodrigo Oliveira Santos, Monique Nakayama Ohe
Archives of Endocrinology and Metabolism.2022; 66(5): 678. CrossRef - Використання інтраопераційного моніторингу рівня паратиреоїдного гормону в мінімально інвазивній хірургії щитоподібної та паращитоподібних залоз
S.V. Chernyshov, A.V. Tymkiv, A.V. Vovkanych, I.I. Komisarenko
Endokrynologia.2022; 27(4): 311. CrossRef - Diagnostic Values of Intraoperative (1-84) Parathyroid Hormone Levels are Superior to Intact Parathyroid Hormone for Successful Parathyroidectomy in Patients With Chronic Kidney Disease
Fangyan Xu, Yaoyu Huang, Ming Zeng, Lina Zhang, Wenkai Ren, Hanyang Qian, Ying Cui, Guang Yang, Wenbin Zhou, Shui Wang, Hui Huang, Huimin Chen, Yujie Xiao, Xueyan Gao, Zhanhui Gao, Jing Wang, Cuiping Liu, Jing Zhang, Baiqiao Zhao, Anning Bian, Fan Li, Hui
Endocrine Practice.2021; 27(11): 1065. CrossRef - Delayed Calcium Normalization after Successful Parathyroidectomy in Primary Hyperparathyroidism
Iván Emilio de la Cruz Rodríguez, Elsy Sarahí García Montesinos, María Fernanda Rodríguez-Delgado, Guadalupe Vargas Ortega, Lourdes Balcázar Hernández, Victoria Mendoza Zubieta, Victor Hernández Avendaño, Baldomero González Virla, Micha�l R. Laurent
Case Reports in Endocrinology.2021; 2021: 1. CrossRef - Parathyroid Surgery
Aditya S. Shirali, Uriel Clemente-Gutierrez, Nancy D. Perrier
Neuroimaging Clinics of North America.2021; 31(3): 397. CrossRef - Focused parathyroidectomy without intraoperative parathyroid hormone measurement in primary hyperparathyroidism: Still a valid approach?
Shelby Holt
Surgery.2021; 170(6): 1860. CrossRef - Response to the Comment on “Risk Factors of Redo Surgery After Unilateral Focused Parathyroidectomy – Conclusions From a Comprehensive Nationwide Database of 13,247 Interventions Over 6 Years”
Robert Caiazzo, Camille Marciniak, Francois Pattou
Annals of Surgery.2021; 274(6): e861. CrossRef
- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy

- A Case of Mediastinal parathyroid adenoma localized by technetium-99m sestamibi scanning.
- Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang, Ki Ho Song, Sung Hee Lee, Won Hee Han, Hyung Sun Sohn
- J Korean Endocr Soc. 1996;11(2):227-232. Published online November 7, 2019
- 1,030 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - We present a patient with primary hyperparathyroidism in whom preoperative Tc-99m sestarnibi scanning cleary demonstrated mediastinal parathyroid adenoma. After resectian of tumor through median sternotomy, he was restored to the normocalcemia. This case suggests that Tc-99m sestamibi scanning may be a useful method in the preoperative localization of mediastinal parathyroid adenoma.

- A Case of Primary Parathyroid Carcinoma with full-brown Symptom.
- Chang Soo Ryu, Deok Ki Kim, Kee Hyun Park, Shi Gyeong Seong, Dong Ho Kim, Sang Min Woo, In Sung Cho
- J Korean Endocr Soc. 1996;11(2):221-226. Published online November 7, 2019
- 1,312 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Primary hyperparathyroicism is a state of hypersecretion of PTH by the parathyroid. The etiology has not been established. The three possible etiologies of piimary hyperparathyroidism and incidences are adencena(83%), hyperplasia(15%), and carcinoma(1~2%). Parathyroid carcinoma usually presents in the fourth decades. The hallmark preoperative signs are hypercalcemia(serum calcium 15mg/dl). Palpable neck mass and bane and renal disease. Patients may present with multiple signs and syrnptoms, including recurrent nephrolithiasis, peptic ulcers, mental change, less frequently, extensive bone resorption. However, with greater awareness of the disease and wider use of screening tests, including blood calcium determinations, the diagnosis is frequently made in patients who have no symptoms and minimal, if any, signs of the disease ather than hypercalcemia and elevated levels of parathyroid Hormone. An 38-years-old woman was admitted to the hospital due to pain on the left knee joint. We experienced full-brown symptom pertaining to hyperpara- thyroidism. Thus we report a case herein and also discuss clinical anifestation, histologic features and treatment.

- Primary Hyperparathyroidism in Children.
- Han Sang Cho, Sang Ook Park, Byung Mun Lee, Yung Tak Lim, Su Yung Kim
- J Korean Endocr Soc. 1994;9(3):251-257. Published online November 6, 2019
- 1,079 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF - Primary hyperparathyroidism is a rare endocrine disease in children. It involves bone and joint, urinary tract, gastrointestinal tract and cardiovascular system. The main cause of these involvement is high level of PTH in serum, resulting in hypercalcemia.An 11 years old male patient who had complained of limping gait since last 18 months, showed typical laboratory and radiological findings of primary hyperparathyroidism. At the ultrasonography, computed tomography and radionuclide scanning, a well defined mass(10 X 15mm) was found on the posterior aspect of the right thyroid lobe. The mass was confirmed histologically as adenoma of parathyroid gland. The patient was successfully treated with subtotal parathyroidectomy and temporal administration of calcium and vitamin D.We report this case of primary hyperparathyroidism with brief review of the literatures.

- A Case of Primary Hyperparathyroidism Associated with Hypercalcemic Crisis and Systemic Calcinosis.
- Young Duk Song, Sung Kil Lim, Hyun Chul Lee, Kap Bum Huh, Bong Sou Park
- J Korean Endocr Soc. 1994;10(2):148-152. Published online November 6, 2019
- 1,012 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Recent reports have fueled on interest in the prevalance and significance of metastatic calcium deposition in patients with chronic hyperparathyroidism. Nephrocarcinosis and cutaneous cacifications have been recognized in patients with chronic renal failure, but the hypercalcemic crisis and systemic calcinosis are extremely rare in patients with primary hyperparathyroidism. We experienced a patient with primary hyperparathyroidism, presented with hypercalcemic crisis and metastatic calcification in the lungs, stomach, liver, and disappeared by successful parathyroidectomy.


 KES
KES

 First
First Prev
Prev



