Previous issues
- Page Path
- HOME > BROWSE ARTICLES > Previous issues
- Obesity and Metabolism
- Impact of Skeletal Muscle Mass on Metabolic Health
- Gyuri Kim, Jae Hyeon Kim
- Endocrinol Metab. 2020;35(1):1-6. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.1
- 10,676 View
- 293 Download
- 64 Web of Science
- 68 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Skeletal muscle is regarded as an endocrine and paracrine organ. Muscle-derived secretory proteins, referred to as myokines, mediate interactions between skeletal muscle mass and other organs such as the liver, adipose tissue, pancreas, bone, and the cardiovascular system. As individuals age, reduced levels of physical activity and sarcopenia (loss of skeletal muscle mass and strength) are associated with physical frailty and disability. Recently, several studies have suggested that the loss of skeletal muscle mass may contribute to metabolic disease. Therefore, herein, we focus on the relationships between skeletal muscle mass and metabolic diseases, including metabolic syndrome and non-alcoholic fatty liver disease.
-
Citations
Citations to this article as recorded by- Sex differences in the association between dual‐energy x‐ray absorptiometry‐measured body composition and periodontitis
Peijun Zhu, An Li, Qingqing Cai, Yuntao Chen, Yang Liu, Harriët Jager‐Wittenaar, Geerten‐Has E. Tjakkes, Shulan Xu
Journal of Periodontology.2024; 95(3): 219. CrossRef - Advances in the treatment of functional male hypogonadism
Giovanni Corona, Giulia Rastrelli, Clotilde Sparano, Linda Vignozzi, Alessandra Sforza, Mario Maggi
Expert Review of Endocrinology & Metabolism.2024; 19(2): 163. CrossRef - Heterogeneously elevated branched-chain/aromatic amino acids among new-onset type-2 diabetes mellitus patients are potentially skewed diabetes predictors
Min Wang, Yang Ou, Xiang-Lian Yuan, Xiu-Fang Zhu, Ben Niu, Zhuang Kang, Bing Zhang, Anwar Ahmed, Guo-Qiang Xing, Heng Su
World Journal of Diabetes.2024; 15(1): 53. CrossRef - The Vicious Cycle of Type 2 Diabetes Mellitus and Skeletal Muscle Atrophy: Clinical, Biochemical, and Nutritional Bases
Jose M. Lopez-Pedrosa, Maria Camprubi-Robles, German Guzman-Rolo, Andres Lopez-Gonzalez, Jose Manuel Garcia-Almeida, Alejandro Sanz-Paris, Ricardo Rueda
Nutrients.2024; 16(1): 172. CrossRef - FGF21 Induces Skeletal Muscle Atrophy and Increases Amino Acids in Female Mice: A Potential Role for Glucocorticoids
Karlton R Larson, Devi Jayakrishnan, Karla A Soto Sauza, Michael L Goodson, Aki T Chaffin, Arik Davidyan, Suraj Pathak, Yanbin Fang, Diego Gonzalez Magaña, Benjamin F Miller, Karen K Ryan
Endocrinology.2024;[Epub] CrossRef - Mortality risk relationship using standard categorized BMI or knee-height based BMI – does the overweight/lower mortality paradox hold true?
Nivetha Natarajan Gavriilidou, Mats Pihlsgård, Sölve Elmståhl, Henrik Ekström
Aging Clinical and Experimental Research.2024;[Epub] CrossRef - Gromwell (Lithospermum erythrorhizon) Attenuates High-Fat-Induced Skeletal Muscle Wasting by Increasing Protein Synthesis and Mitochondrial Biogenesis
Ji-Sun Kim, Hyunjung Lee, Ahyoung Yoo, Hang Yeon Jeong, Chang Hwa Jung, Jiyun Ahn, Tae-Youl Ha
Journal of Microbiology and Biotechnology.2024; 34(3): 495. CrossRef - L-shaped association between lean body mass to visceral fat mass ratio with hyperuricemia: a cross-sectional study
Longti Li, Ya Shao, Huiqin Zhong, Yu Wang, Rong Zhang, Boxiong Gong, Xiaoxv Yin
Lipids in Health and Disease.2024;[Epub] CrossRef - Prevalence of adiposity-based chronic disease and its association with anthropometric and clinical indices: a cross-sectional study
Luis E González-Salazar, Aurora E Serralde-Zúñiga, Adriana Flores-López, Juan P Díaz-Sánchez, Isabel Medina-Vera, Edgar Pichardo-Ontiveros, Rocío Guizar-Heredia, Karla G Hernández-Gómez, Ana Vigil-Martínez, Liliana Arteaga-Sánchez, Azalia Avila-Nava, Nata
British Journal of Nutrition.2023; 130(1): 93. CrossRef - Skeletal Muscle Myokine Expression in Critical Illness, Association With Outcome and Impact of Therapeutic Interventions
Ilse Vanhorebeek, Jan Gunst, Michaël P Casaer, Inge Derese, Sarah Derde, Lies Pauwels, Johan Segers, Greet Hermans, Rik Gosselink, Greet Van den Berghe
Journal of the Endocrine Society.2023;[Epub] CrossRef - Effect of Circadian Rhythm Disturbance on the Human Musculoskeletal System and the Importance of Nutritional Strategies
Norsham Juliana, Liyana Azmi, Nadia Mohd Effendy, Nur Islami Mohd Fahmi Teng, Izuddin Fahmy Abu, Nur Nabilah Abu Bakar, Sahar Azmani, Noor Anisah Abu Yazit, Suhaini Kadiman, Srijit Das
Nutrients.2023; 15(3): 734. CrossRef - Molecular mechanisms of post‐burn muscle wasting and the therapeutic potential of physical exercise
Dorien Dombrecht, Ulrike Van Daele, Birgit Van Asbroeck, David Schieffelers, Pieter‐Jan Guns, Nick Gebruers, Jill Meirte, Eric van Breda
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(2): 758. CrossRef - Metabolic Impact of Frailty Changes Diabetes Trajectory
Alan J. Sinclair, Ahmed H. Abdelhafiz
Metabolites.2023; 13(2): 295. CrossRef - From Single- to Multi-organ-on-a-Chip System for Studying Metabolic Diseases
Minjeong Jang, Hong Nam Kim
BioChip Journal.2023; 17(2): 133. CrossRef - INFLUENCE OF SARCOPENIA ON THE COURSE AND PROGNOSIS IN PATIENTS WITH CHRONIC HEART FAILURE
Gulyaev N.I., Adamov A.A., Akhmetshin I.M.
"Medical & pharmaceutical journal "Pulse".2023; : 124. CrossRef - Frailty and the Interactions between Skeletal Muscle, Bone, and Adipose Tissue-Impact on Cardiovascular Disease and Possible Therapeutic Measures
María Elena Soto, Israel Pérez-Torres, María Esther Rubio-Ruiz, Agustina Cano-Martínez, Linaloe Manzano-Pech, Verónica Guarner-Lans
International Journal of Molecular Sciences.2023; 24(5): 4534. CrossRef - Sarcoplasmic Reticulum Ca2+ Buffer Proteins: A Focus on the Yet-To-Be-Explored Role of Sarcalumenin in Skeletal Muscle Health and Disease
Elena Conte, Giorgia Dinoi, Paola Imbrici, Annamaria De Luca, Antonella Liantonio
Cells.2023; 12(5): 715. CrossRef - Antarctic krill extracts enhance muscle regeneration and muscle function via mammalian target of rapamycin regulation
Seongmin Lee, Mi-Ock Baek, Sana Abdul Khaliq, Amna Parveen, Sun Yeou Kim, Jin-Hyoung Kim, Il-Chan Kim, Mee-Sup Yoon
Journal of Functional Foods.2023; 103: 105483. CrossRef - Pharmacological and physiological roles of adipokines and myokines in metabolic-related dementia
Archana Arjunan, Juhyun Song
Biomedicine & Pharmacotherapy.2023; 163: 114847. CrossRef - PRMT5 links lipid metabolism to contractile function of skeletal muscles
Kun Ho Kim, Zhihao Jia, Madigan Snyder, Jingjuan Chen, Jiamin Qiu, Stephanie N Oprescu, Xiyue Chen, Sabriya A Syed, Feng Yue, Bruno T Roseguini, Anthony N Imbalzano, Changdeng Hu, Shihuan Kuang
EMBO reports.2023;[Epub] CrossRef - “Biqi” Bayberry Extract Promotes Skeletal Muscle Fiber Type Remodeling by Increasing Fast Myofiber Formation via the Akt/FoxO1 Pathway in Mice
Jinjie Li, Yi Li, Xiangying Suo, Jiangtao Li, Da Huang, Guangning Kou
Foods.2023; 12(13): 2471. CrossRef - Effects of high-intensity interval training (HIIT) on skeletal muscle atrophy, function, and myokine profile in diabetic myopathy
Yeşim Özçatal, Fırat Akat, Yakup Tatar, Hakan Fıçıcılar, Bilge Serdaroğlu, Ferda Topal Çelikkan, Metin Baştuğ
Cytokine.2023; 169: 156279. CrossRef - Impaired proteostatic mechanisms other than decreased protein synthesis limit old skeletal muscle recovery after disuse atrophy
Jordan D. Fuqua, Marcus M. Lawrence, Zachary R. Hettinger, Agnieszka K. Borowik, Parker L. Brecheen, Marcelina M. Szczygiel, Claire B. Abbott, Frederick F. Peelor, Amy L. Confides, Michael Kinter, Sue C. Bodine, Esther E. Dupont‐Versteegden, Benjamin F. M
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(5): 2076. CrossRef - Body physique rating as a factor to identify at-risk Mexicans for Metabolic Syndrome
Oscar Herrera-Fomperosa, Sergio K. Bustamante-Villagomez, Sarahí Vazquez-Álvarez, Gabriela Vázquez-Marroquín, Leonardo M. Porchia, Enrique Torres-Rasgado, Ricardo Pérez-Fuentes, M. Elba Gonzalez-Mejia
Human Nutrition & Metabolism.2023; 33: 200206. CrossRef - Association between Fractional Oxygen Extraction from Resting Quadriceps Muscle and Body Composition in Healthy Men
Rodrigo Yáñez-Sepúlveda, Jorge Olivares-Arancibia, Guillermo Cortés-Roco, Aldo Vasquez-Bonilla, Matías Monsalves-Álvarez, Ildefonso Alvear-Órdenes, Marcelo Tuesta
Journal of Functional Morphology and Kinesiology.2023; 8(4): 149. CrossRef - Correlations between Mental Health, Physical Activity, and Body Composition in American College Students after the COVID-19 Pandemic Lockdown
Luis Torres, Manuela C. Caciula, Alin S. Tomoiaga, Carmen Gugu-Gramatopol
International Journal of Environmental Research and Public Health.2023; 20(22): 7045. CrossRef - Association between total body muscle percentage and prevalence of non-alcoholic fatty liver disease in Korean adults findings from an 18-year follow-up: a prospective cohort study
Byoung Chan Ahn, Chul Yong Park, Jung Hee Hong, Ki Ook Baek
Journal of Yeungnam Medical Science.2023; 40(Suppl): S47. CrossRef - The independent and joint associations among muscle strength, abdominal obesity and cardiometabolic variables among adults
Tiago Rodrigues de Lima, David Alejandro González‐Chica, Xuemei Sui, Diego Augusto Santos Silva
European Journal of Sport Science.2022; 22(7): 1122. CrossRef - Mentale Gesundheit und physische Aktivität
Wolfgang Laube
Manuelle Medizin.2022; 60(1): 13. CrossRef - A new paradigm in sarcopenia: Cognitive impairment caused by imbalanced myokine secretion and vascular dysfunction
Danbi Jo, Gwangho Yoon, Oh Yoen Kim, Juhyun Song
Biomedicine & Pharmacotherapy.2022; 147: 112636. CrossRef - Sarcopenia Is a Cause and Consequence of Metabolic Dysregulation in Aging Humans: Effects of Gut Dysbiosis, Glucose Dysregulation, Diet and Lifestyle
James W. Daily, Sunmin Park
Cells.2022; 11(3): 338. CrossRef - Leveraging deep phenotyping from health check-up cohort with 10,000 Korean individuals for phenome-wide association study of 136 traits
Eun Kyung Choe, Manu Shivakumar, Anurag Verma, Shefali Setia Verma, Seung Ho Choi, Joo Sung Kim, Dokyoon Kim
Scientific Reports.2022;[Epub] CrossRef - Zika virus disrupts gene expression in human myoblasts and myotubes: Relationship with susceptibility to infection
Ingo Riederer, Daniella Arêas Mendes-da-Cruz, Guilherme Cordenonsi da Fonseca, Mariela Natacha González, Otavio Brustolini, Cássia Rocha, Guilherme Loss, Joseane Biso de Carvalho, Mariane Talon Menezes, Lidiane Menezes Souza Raphael, Alexandra Gerber, Myr
PLOS Neglected Tropical Diseases.2022; 16(2): e0010166. CrossRef - Teil 1: Muskeldysfunktionen – mit Training gegen Schmerz
Wolfgang Laube
Manuelle Medizin.2022; 60(2): 84. CrossRef - Transcription factors KLF15 and PPARδ cooperatively orchestrate genome-wide regulation of lipid metabolism in skeletal muscle
Liyan Fan, David R. Sweet, Erica K. Fan, Domenick A. Prosdocimo, Annmarie Madera, Zhen Jiang, Roshan Padmanabhan, Saptarsi M. Haldar, Vinesh Vinayachandran, Mukesh K. Jain
Journal of Biological Chemistry.2022; 298(6): 101926. CrossRef - An Overview of the TRP-Oxidative Stress Axis in Metabolic Syndrome: Insights for Novel Therapeutic Approaches
Mizael C. Araújo, Suzany H. S. Soczek, Jaqueline P. Pontes, Leonardo A. C. Marques, Gabriela S. Santos, Gisele Simão, Laryssa R. Bueno, Daniele Maria-Ferreira, Marcelo N. Muscará, Elizabeth S. Fernandes
Cells.2022; 11(8): 1292. CrossRef - Effects of a 10-Week Physical Activity Intervention on Asylum Seekers’ Physiological Health
Matheus Guerra, Danilo Garcia, Maryam Kazemitabar, Erik Lindskär, Erica Schütz, Daniel Berglind
Brain Sciences.2022; 12(7): 822. CrossRef - Low muscle mass and mortality risk later in life: A 10-year follow-up study
Cristina Camargo Pereira, Valéria Pagotto, Cesar de Oliveira, Erika Aparecida Silveira, Kiyoshi Sanada
PLOS ONE.2022; 17(7): e0271579. CrossRef - Independent and joint associations of weightlifting and aerobic activity with all-cause, cardiovascular disease and cancer mortality in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial
Jessica Gorzelitz, Britton Trabert, Hormuzd A Katki, Steven C Moore, Eleanor L Watts, Charles E Matthews
British Journal of Sports Medicine.2022; 56(22): 1277. CrossRef - Handgrip Strength Cutoff Value Among Korean Adolescents with Metabolic Syndrome Components: Korean National Health and Nutrition Examination Survey Data 2014–2017
Chang Hoon Lee, Jun Hyeok Lee, Yong Whi Jeong, Hong Koh, Yunkoo Kang
Metabolic Syndrome and Related Disorders.2022; 20(10): 584. CrossRef - Physical activity level, sitting time, and skeletal muscle mass between esports players and non-esports players
Zhi H. SEE, Mohamad S. ABDUL HAMID
Gazzetta Medica Italiana Archivio per le Scienze Mediche.2022;[Epub] CrossRef - Impact of the Nutrition–Inflammation Status on the Functionality of Patients with Chronic Kidney Disease
Ángel Nogueira, Graciela Álvarez, Guillermina Barril
Nutrients.2022; 14(22): 4745. CrossRef - Does Timing Matter? A Narrative Review of Intermittent Fasting Variants and Their Effects on Bodyweight and Body Composition
Alan A. Aragon, Brad J. Schoenfeld
Nutrients.2022; 14(23): 5022. CrossRef - Sex- and region-specific associations of skeletal muscle mass with metabolic dysfunction-associated fatty liver disease
Pei Xiao, Pu Liang, Panjun Gao, Jinyi Wu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Donor Skeletal Muscle Quality Affects Graft Mortality After Living Donor Liver Transplantation- A Single Center, Retrospective Study
Takahiro Tomiyama, Noboru Harada, Takeo Toshima, Yuki Nakayama, Katsuya Toshida, Akinari Morinaga, Yukiko Kosai-Fujimoto, Takahiro Tomino, Takeshi Kurihara, Kazuki Takeishi, Yoshihiro Nagao, Kazutoyo Morita, Shinji Itoh, Tomoharu Yoshizumi
Transplant International.2022;[Epub] CrossRef - Handgrip Strength Is Associated with Metabolic Syndrome and Insulin Resistance in Children and Adolescents: Analysis of Korea National Health and Nutrition Examination Survey 2014–2018
Hae Woon Jung, Jieun Lee, Jaehyun Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(4): 334. CrossRef - Diet quality and a traditional dietary pattern predict lean mass in Australian women: Longitudinal data from the Geelong Osteoporosis Study
Jessica A. Davis, Mohammadreza Mohebbi, Fiona Collier, Amy Loughman, Nitin Shivappa, James R. Hébert, Julie A. Pasco, Felice N. Jacka
Preventive Medicine Reports.2021; 21: 101316. CrossRef - Association between serum FGF21 level and sarcopenia in older adults
Hee-Won Jung, Jin Hoon Park, Da Ae Kim, Il-Young Jang, So Jeong Park, Jin Young Lee, Seungjoo Lee, Jeoung Hee Kim, Hyon-Seung Yi, Eunju Lee, Beom-Jun Kim
Bone.2021; 145: 115877. CrossRef - Benchside to the bedside of frailty and cardiovascular aging: Main shared cellular and molecular mechanisms
Sandra Maria Barbalho, Ricardo José Tofano, Eduardo Federigui Baisi Chagas, Cláudia Rucco Penteado Detregiachi, Ricardo de Alvares Goulart, Uri Arian Princ Flato
Experimental Gerontology.2021; 148: 111302. CrossRef - Effect of CCL11 on In Vitro Myogenesis and Its Clinical Relevance for Sarcopenia in Older Adults
Da Ae Kim, So Jeong Park, Jin Young Lee, Jeoung Hee Kim, Seungjoo Lee, Eunju Lee, Il-Young Jang, Hee-Won Jung, Jin Hoon Park, Beom-Jun Kim
Endocrinology and Metabolism.2021; 36(2): 455. CrossRef - Sarcopenic obesity as a determinant of cardiovascular disease risk in older people: a systematic review
Katherine Evans, Dima Abdelhafiz, Ahmed H Abdelhafiz
Postgraduate Medicine.2021; 133(8): 831. CrossRef - Decreased continuous sitting time increases heart rate variability in patients with cardiovascular risk factors
Natsuki Nakayama, Masahiko Miyachi, Koji Tamakoshi, Toshio Hayashi, Koji Negi, Koji Watanabe, Makoto Hirai, Sharon Mary Brownie
PLOS ONE.2021; 16(6): e0253399. CrossRef - Muskeltraining – ein universelles Medikament
Wolfgang Laube
Manuelle Medizin.2021; 59(3): 179. CrossRef - The Effects of Oxytocin on Appetite Regulation, Food Intake and Metabolism in Humans
Liya Kerem, Elizabeth A. Lawson
International Journal of Molecular Sciences.2021; 22(14): 7737. CrossRef - Weight Loss Strategies and the Risk of Skeletal Muscle Mass Loss
David McCarthy, Aloys Berg
Nutrients.2021; 13(7): 2473. CrossRef - Association of FGF‐19 and FGF‐21 levels with primary sarcopenia
Rabia Bag Soytas, Veysel Suzan, Pinar Arman, Tugce Emiroglu Gedik, Damla Unal, Mahir Cengiz, Ibrahim Murat Bolayirli, Deniz Suna Erdincler, Alper Doventas, Hakan Yavuzer
Geriatrics & Gerontology International.2021; 21(10): 959. CrossRef - Der Muskulatur mehr Aufmerksamkeit schenken!
Wolfgang Laube
Manuelle Medizin.2021; 59(4): 302. CrossRef - Methodology, clinical applications, and future directions of body composition analysis using computed tomography (CT) images: A review
Antti Tolonen, Tomppa Pakarinen, Antti Sassi, Jere Kyttä, William Cancino, Irina Rinta-Kiikka, Said Pertuz, Otso Arponen
European Journal of Radiology.2021; 145: 109943. CrossRef - Waist and hip circumference are independently associated with the risk of liver disease in population‐based studies
Oscar Danielsson, Markku J. Nissinen, Antti Jula, Veikko Salomaa, Satu Männistö, Annamari Lundqvist, Markus Perola, Fredrik Åberg
Liver International.2021; 41(12): 2903. CrossRef - Understanding of sarcopenia: from definition to therapeutic strategies
Jee Won Kim, Ryuni Kim, Hyerim Choi, Sang-Jin Lee, Gyu-Un Bae
Archives of Pharmacal Research.2021; 44(9-10): 876. CrossRef - Muscle strength and its association with cardiometabolic variables in adolescents: does the expression of muscle strength values matter?
Tiago Rodrigues de Lima, Xuemei Sui, Luiz Rodrigo Augustemak de Lima, Diego Augusto Santos Silva
World Journal of Pediatrics.2021; 17(6): 597. CrossRef - Musclin Is Related to Insulin Resistance and Body Composition, but Not to Body Mass Index or Cardiorespiratory Capacity in Adults
Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis Valbuena, Andrés F. Milán, María C. Trillos-Almanza, Sergio Granados, Miguel Peña, Mauricio Estrada-Castrillón, Juan C. Aristizábal, Raúl Narvez-Sanchez, Jaime Gallo-Villegas, Juan C. Calderón
Endocrinology and Metabolism.2021; 36(5): 1055. CrossRef - Physical Exercise and Myokines: Relationships with Sarcopenia and Cardiovascular Complications
Sandra Maria Barbalho, Uri Adrian Prync Flato, Ricardo José Tofano, Ricardo de Alvares Goulart, Elen Landgraf Guiguer, Cláudia Rucco P. Detregiachi, Daniela Vieira Buchaim, Adriano Cressoni Araújo, Rogério Leone Buchaim, Fábio Tadeu Rodrigues Reina, Piero
International Journal of Molecular Sciences.2020; 21(10): 3607. CrossRef Prevalence of Metabolic Syndrome and Association with Grip Strength in Older Adults: Findings from the HOPE Study
Reshma Aziz Merchant, Yiong Huak Chan, Jia Yi Lim, John E Morley
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 2677. CrossRef- Lower Serum n-3 Fatty Acid Level in Older Adults with Sarcopenia
Il-Young Jang, Hee-Won Jung, Jin Hoon Park, Jeoung Hee Kim, Seungjoo Lee, Eunju Lee, Jin Young Lee, So Jeong Park, Da Ae Kim, Su Jung Kim, Hyun Ju Yoo, Beom-Jun Kim
Nutrients.2020; 12(10): 2959. CrossRef - Advances in understanding of health‐promoting benefits of medicine and food homology using analysis of gut microbiota and metabolomics
Minmin Yang, Tao Yan, Meng Yu, Jie Kang, Ruoxi Gao, Peng Wang, Yuhuan Zhang, Huafeng Zhang, Lin Shi
Food Frontiers.2020; 1(4): 398. CrossRef - The association of circulating kynurenine, a tryptophan metabolite, with frailty in older adults
Il-Young Jang, Jin Hoon Park, Jeoung Hee Kim, Seungjoo Lee, Eunju Lee, Jin Young Lee, So Jeong Park, Da Ae Kim, Mark W. Hamrick, Beom-Jun Kim
Aging.2020; 12(21): 22253. CrossRef - Sarcopenia and Muscle Aging: A Brief Overview
Tam Dao, Alexander E. Green, Yun A Kim, Sung-Jin Bae, Ki-Tae Ha, Karim Gariani, Mi-ra Lee, Keir J. Menzies, Dongryeol Ryu
Endocrinology and Metabolism.2020; 35(4): 716. CrossRef
- Sex differences in the association between dual‐energy x‐ray absorptiometry‐measured body composition and periodontitis

- Thyroid
- Update on Thyroid Hormone Levels and Thyroid Dysfunction in the Korean Population Based on Data from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
- Jae Hoon Chung
- Endocrinol Metab. 2020;35(1):7-13. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.7
- 6,951 View
- 150 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
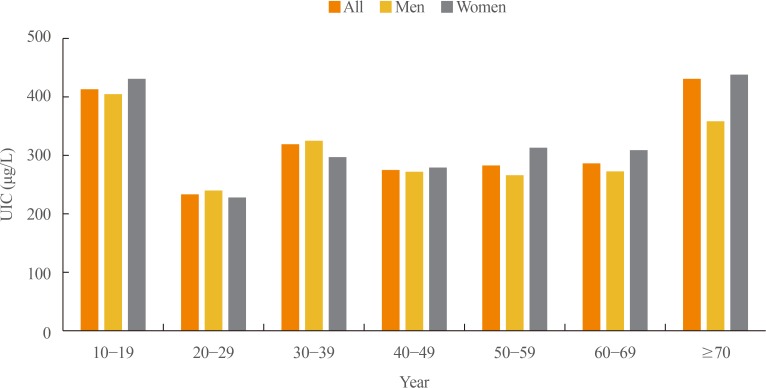
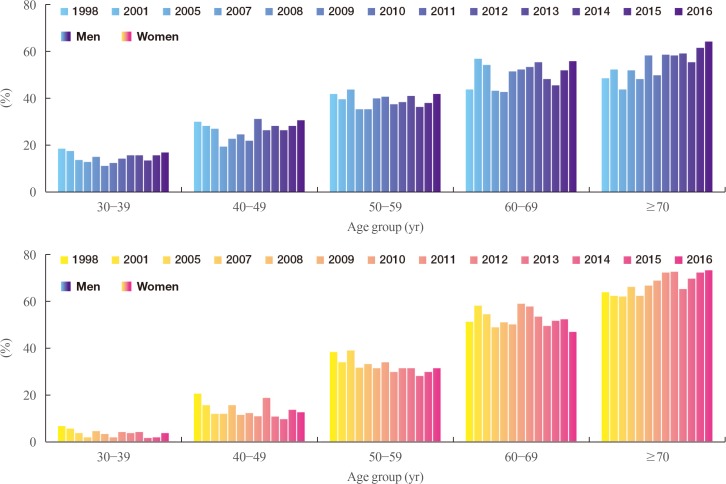
ePub In 2017, the first Korean nationwide data on serum thyroid stimulating hormone (TSH) levels, serum free thyroxine (fT4) levels, and urinary iodine concentration (UIC) were published based on a population of 7,061 Koreans who participated in the Korea National Health and Nutrition Examination Survey VI. The mean TSH level was 2.16 mIU/L, with a reference interval of 0.59 to 7.03 mIU/L (men 2.09 mIU/L, women 2.24 mIU/L,
P <0.001). A U-shaped association was found between serum TSH levels and age. The mean fT4 level was 1.25 ng/dL, and its reference interval was 0.92 to 1.60 ng/dL (men 1.29 ng/dL, women 1.20 ng/dL,P <0.0001). Serum fT4 levels decreased with age (P for trend <0.0001). Serum thyroid peroxidase antibody (TPOAb) was detected in 7.30% of participants (men 4.33%, women 10.62%). TPOAb titers tended to increase with age, and were higher in women than in men. The median UIC was 294 µg/L, and UIC showed a U-shaped relationship with age. According to the World Health Organization recommendations, only 23% of participants were in the adequate range of iodine intake, while 65% were in the above requirements or excessive, and 12% in insufficient. The prevalence of overt hyperthyroidism and hypothyroidism in Koreans was 0.34% to 0.54% and 0.73% to 1.43%, respectively.-
Citations
Citations to this article as recorded by- Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey
Eunji Mun, Hye Ah Lee, Jung Eun Choi, Rosie Lee, Kyung Hee Kim, Hyesook Park, Hae Soon Kim
Children.2024; 11(3): 370. CrossRef - Diagnostic Value of Carotid Plaque Assessment with AIS Based on Quantitative Parameters of Dual-Layer Detector Spectral CT
Xiaoying Meng, Fei Li, Wenpei Wu, Juncang Wu
International Journal of General Medicine.2024; Volume 17: 1263. CrossRef - Hyperthyroidism
Sun Y. Lee, Elizabeth N. Pearce
JAMA.2023; 330(15): 1472. CrossRef - Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
Endocrinology and Metabolism.2023; 38(6): 729. CrossRef - Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2021; 36(3): 500. CrossRef - Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study
Kyungsik Kim, Sun Wook Cho, Young Joo Park, Kyu Eun Lee, Dong-Wook Lee, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 790. CrossRef
- Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey

- Thyroid
- Unmet Clinical Needs in the Treatment of Patients with Thyroid Cancer
- Won Bae Kim, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong
- Endocrinol Metab. 2020;35(1):14-25. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.14
- 7,061 View
- 135 Download
- 14 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
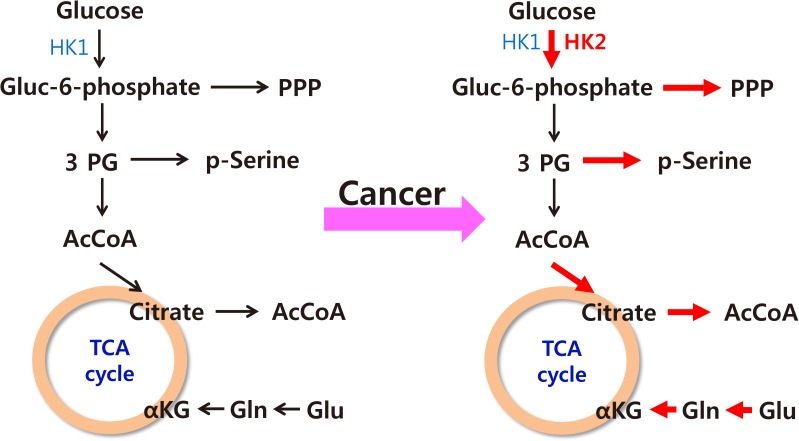
ePub The increased incidence of thyroid cancer is a worldwide phenomenon; however, the issue of overdiagnosis has been most prominent in South Korea. The age-standardized mortality rate of thyroid cancer in Korea steeply increased from 1985 to 2004 (from 0.17 per 100,000 to 0.85 per 100,000), and then decreased until 2015 to 0.42 per 100,000, suggesting that early detection reduced mortality. However, early detection of thyroid cancer may be cost-ineffective, considering its very high prevalence and indolent course. Therefore, risk stratification and tailored management are vitally important, but many prognostic markers can only be evaluated postoperatively. Discovery of preoperative marker(s), especially for small cancers, is the most important unmet clinical need for thyroid cancer. Herein, we discuss some such factors that we recently discovered. Another unmet clinical need is better treatment of radioiodine-refractory (RAIR) differentiated thyroid cancer (DTC) and undifferentiated cancers. Although sorafenib and lenvatinib are available, better drugs are needed. We found that phosphoglycerate dehydrogenase, a critical enzyme for serine biosynthesis, could be a novel therapeutic target, and that the lymphocyte-to-monocyte ratio is a prognostic marker of survival in patients with anaplastic thyroid carcinoma or RAIR DTC. Deeper insights are needed into tumor-host interactions in thyroid cancer to improve treatment.
-
Citations
Citations to this article as recorded by- Lenvatinib Compared with Sorafenib as a First-Line Treatment for Radioactive Iodine-Refractory, Progressive, Differentiated Thyroid Carcinoma: Real-World Outcomes in a Multicenter Retrospective Cohort Study
Mijin Kim, Meihua Jin, Min Ji Jeon, Eui Young Kim, Dong Yeob Shin, Dong Jun Lim, Bo Hyun Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Hee Kyung Kim, Won Gu Kim
Thyroid.2023; 33(1): 91. CrossRef - Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Integration of ultrasound-based radiomics with clinical features for predicting cervical lymph node metastasis in postoperative patients with differentiated thyroid carcinoma
Fengjing Fan, Fei Li, Yixuan Wang, Zhengjun Dai, Yuyang Lin, Lin Liao, Bei Wang, Hongjun Sun
Endocrine.2023;[Epub] CrossRef - Transcriptomic Analysis of Papillary Thyroid Cancer: A Focus on Immune-Subtyping, Oncogenic Fusion, and Recurrence
Seung-Jin Park, Yea Eun Kang, Jeong-Hwan Kim, Jong-Lyul Park, Seon-Kyu Kim, Seung-Woo Baek, In Sun Chu, Shinae Yi, Seong Eun Lee, Young Joo Park, Eun-Jae Chung, Jin Man Kim, Hye Mi Ko, Je-Ryong Kim, Seung-Nam Jung, Ho-Ryun Won, Jae Won Chang, Bon Seok Koo
Clinical and Experimental Otorhinolaryngology.2022; 15(2): 183. CrossRef - Prognosis of Patients with 1–4 cm Papillary Thyroid Cancer Who Underwent Lobectomy: Focus on Gross Extrathyroidal Extension Invading Only the Strap Muscles
Ahreum Jang, Meihua Jin, Won Woong Kim, Min Ji Jeon, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Yu-Mi Lee, Won Gu Kim
Annals of Surgical Oncology.2022; 29(12): 7835. CrossRef - Carboxy terminus of HSP70‐interacting protein (CHIP) attenuates the stemness of thyroid cancer cells through decreasing OCT4 protein stability
Ying Xu, Gang Xu, Huimin Dang, Wei Qu, Dan Chang, Xin He, Minmin Li, Qian Wang
Environmental Toxicology.2021; 36(4): 686. CrossRef - Lactate Dehydrogenase A as a Potential New Biomarker for Thyroid Cancer
Eun Jeong Ban, Daham Kim, Jin Kyong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Kunhong Kim
Endocrinology and Metabolism.2021; 36(1): 96. CrossRef - Clinical implications of age and excellent response to therapy in patients with high‐risk differentiated thyroid carcinoma
Meihua Jin, Jonghwa Ahn, Yu‐Mi Lee, Tae‐Yon Sung, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jin‐Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Won Gu Kim
Clinical Endocrinology.2021; 95(6): 882. CrossRef - CD73 Overexpression Promotes Progression and Recurrence of Papillary Thyroid Carcinoma
Young Mun Jeong, Haejin Cho, Tae-Min Kim, Yourha Kim, Sora Jeon, Andrey Bychkov, Chan Kwon Jung
Cancers.2020; 12(10): 3042. CrossRef - The Role of Exosomes in Thyroid Cancer and Their Potential Clinical Application
Kaixiang Feng, Runsheng Ma, Lele Zhang, Hongqiang Li, Yifeng Tang, Gongbo Du, Dongpeng Niu, Detao Yin
Frontiers in Oncology.2020;[Epub] CrossRef
- Lenvatinib Compared with Sorafenib as a First-Line Treatment for Radioactive Iodine-Refractory, Progressive, Differentiated Thyroid Carcinoma: Real-World Outcomes in a Multicenter Retrospective Cohort Study

- Adrenal gland
- Is Follow-up of Adrenal Incidentalomas Always Mandatory?
- Giuseppe Reimondo, Alessandra Muller, Elisa Ingargiola, Soraya Puglisi, Massimo Terzolo
- Endocrinol Metab. 2020;35(1):26-35. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.26

- 6,473 View
- 250 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Adrenal masses are mainly detected unexpectedly by an imaging study performed for reasons unrelated to any suspect of adrenal diseases. Such masses are commonly defined as “adrenal incidentalomas” and represent a public health challenge because they are increasingly recognized in current medical practice. Management of adrenal incidentalomas is currently matter of debate. Although there is consensus on the need of a multidisciplinary expert team evaluation and surgical approach in patients with significant hormonal excess and/or radiological findings suspicious of malignancy demonstrated at the diagnosis or during follow-up, the inconsistency between official guidelines and the consequent diffuse uncertainty on management of small adrenal incidentalomas still represents a considerable problem in terms of clinical choices in real practice. The aim of the present work is to review the proposed strategies on how to manage patients with adrenal incidentalomas that are not candidates to immediate surgery. The recent European Society of Endocrinology/European Network for the Study of Adrenal Tumors guidelines have supported the view to avoid surveillance in patients with clear benign adrenal lesions <4 cm and/or without any hormonal secretion; however, newer prospective studies are needed to confirm safety of this strategy, in particular in younger patients.
-
Citations
Citations to this article as recorded by- Adrenal Incidentaloma—Innocent Bystander or Intruder?
Laurence Amar, Inga Harbuz-Miller, Adina F Turcu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1303. CrossRef - Diagnosing and managing adrenal incidentalomas
Justine Herndon, Irina Bancos
JAAPA.2023; 36(5): 12. CrossRef - Tumor enlargement in adrenal incidentaloma is related to glaucoma: a new prognostic feature?
M. Caputo, T. Daffara, A. Ferrero, M. Romanisio, E. Monti, C. Mele, M. Zavattaro, S. Tricca, A. Siani, A. Clemente, C. Palumbo, S. De Cillà, A. Carriero, A. Volpe, P. Marzullo, G. Aimaretti, F. Prodam
Journal of Endocrinological Investigation.2023; 47(2): 377. CrossRef - The Role of Biomarkers in Adrenocortical Carcinoma: A Review of Current Evidence and Future Perspectives
Maja Mizdrak, Tina Tičinović Kurir, Joško Božić
Biomedicines.2021; 9(2): 174. CrossRef - An Adrenocortical Carcinoma Evolving After Nine Years of Latency From a Small Adrenal Incidentaloma
Harpreet S Kohli, Sukesh Manthri, Shikha Jain, Rahul Kashyap, Sheng Chen, Thoyaja Koritala, Aysun Tekin, Ramesh Adhikari, Raghavendra Tirupathi, Aram Barbaryan, Simon Zec, Hanyin Wang, Stephanie Welle, Pavan Devulapally, Mack Sheraton, Manpreet Kaur, Vish
Cureus.2021;[Epub] CrossRef - Diagnostic algorithm of the subclinical forms of adrenal neoplasms
Sofya G. Blyumina, Pavel N. Romashchenko, Igor S. Zheleznyak
Bulletin of the Russian Military Medical Academy.2021; 23(3): 67. CrossRef
- Adrenal Incidentaloma—Innocent Bystander or Intruder?

- Miscellaneous
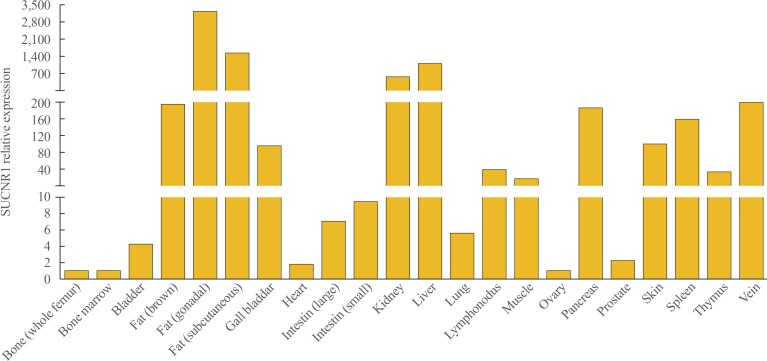
- Multifaceted Actions of Succinate as a Signaling Transmitter Vary with Its Cellular Locations
- Yuqi Guo, Sun Wook Cho, Deepak Saxena, Xin Li
- Endocrinol Metab. 2020;35(1):36-43. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.36
- 7,675 View
- 198 Download
- 25 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Since the identification of succinate's receptor in 2004, studies supporting the involvement of succinate signaling through its receptor in various diseases have accumulated and most of these investigations have highlighted succinate's pro-inflammatory role. Taken with the fact that succinate is an intermediate metabolite in the center of mitochondrial activity, and considering its potential regulation of protein succinylation through succinyl-coenzyme A, a review on the overall multifaceted actions of succinate to discuss whether and how these actions relate to the cellular locations of succinate is much warranted. Mechanistically, it is important to consider the sources of succinate, which include somatic cellular released succinate and those produced by the microbiome, especially the gut microbiota, which is an equivalent, if not greater contributor of succinate levels in the body. Continue learning the critical roles of succinate signaling, known and unknown, in many pathophysiological conditions is important. Furthermore, studies to delineate the regulation of succinate levels and to determine how succinate elicits various types of signaling in a temporal and spatial manner are also required.
-
Citations
Citations to this article as recorded by- Type 2 diabetes and succinate: unmasking an age-old molecule
Sonia Fernández-Veledo, Anna Marsal-Beltran, Joan Vendrell
Diabetologia.2024; 67(3): 430. CrossRef - Metabolism Serves as a Bridge Between Cardiomyocytes and Immune Cells in Cardiovascular Diseases
Lixiao Hang, Ying Zhang, Zheng Zhang, Haiqiang Jiang, Lin Xia
Cardiovascular Drugs and Therapy.2024;[Epub] CrossRef - The Tricarboxylic Acid Cycle as a Central Regulator of the Rate of Aging: Implications for Metabolic Interventions
Jonathan M. Borkum
Advanced Biology.2023;[Epub] CrossRef - Dysregulation of metabolic pathways in pulmonary fibrosis
Rishi Rajesh, Reham Atallah, Thomas Bärnthaler
Pharmacology & Therapeutics.2023; 246: 108436. CrossRef - Succinate metabolism and membrane reorganization drives the endotheliopathy and coagulopathy of traumatic hemorrhage
Sarah Abdullah, Michael Ghio, Aaron Cotton-Betteridge, Aditya Vinjamuri, Robert Drury, Jacob Packer, Oguz Aras, Jessica Friedman, Mardeen Karim, David Engelhardt, Emma Kosowski, Kelby Duong, Farhana Shaheen, Patrick R. McGrew, Charles T. Harris, Robert Re
Science Advances.2023;[Epub] CrossRef - Pharmacokinetics of Succinate in Rats after Intravenous Administration of Mexidol
A. V. Shchulkin, P. Yu. Mylnikov, I. V. Chernykh, A. S. Esenina, E. N. Yakusheva
Bulletin of Experimental Biology and Medicine.2023; 175(1): 54. CrossRef - Complex II Biology in Aging, Health, and Disease
Eric Goetzman, Zhenwei Gong, Bob Zhang, Radhika Muzumdar
Antioxidants.2023; 12(7): 1477. CrossRef - The Influence of the Microbiome on Urological Malignancies: A Systematic Review
Joao G. Porto, Maria Camila Suarez Arbelaez, Brandon Pena, Archan Khandekar, Ankur Malpani, Bruno Nahar, Sanoj Punnen, Chad R. Ritch, Mark L. Gonzalgo, Dipen J. Parekh, Robert Marcovich, Hemendra N. Shah
Cancers.2023; 15(20): 4984. CrossRef - The Gut Microbiome, Metformin, and Aging
Sri Nitya Reddy Induri, Payalben Kansara, Scott C. Thomas, Fangxi Xu, Deepak Saxena, Xin Li
Annual Review of Pharmacology and Toxicology.2022; 62(1): 85. CrossRef - Tissue- and substrate-dependent mitochondrial responses to acute hypoxia–reoxygenation stress in a marine bivalve (Crassostrea gigas
)
Linda Adzigbli, Eugene P. Sokolov, Siriluck Ponsuksili, Inna M. Sokolova
Journal of Experimental Biology.2022;[Epub] CrossRef - Acute Succinate Administration Increases Oxidative Phosphorylation and Skeletal Muscle Explosive Strength via SUCNR1
Guli Xu, Yexian Yuan, Pei Luo, Jinping Yang, Jingjing Zhou, Canjun Zhu, Qingyan Jiang, Gang Shu
Frontiers in Veterinary Science.2022;[Epub] CrossRef - Integrated bioinformatics analysis identifies established and novel TGFβ1-regulated genes modulated by anti-fibrotic drugs
Ava C. Wilson, Joe Chiles, Shah Ashish, Diptiman Chanda, Preeti L. Kumar, James A. Mobley, Enid R. Neptune, Victor J. Thannickal, Merry-Lynn N. McDonald
Scientific Reports.2022;[Epub] CrossRef - SUCNR1 Mediates the Priming Step of the Inflammasome in Intestinal Epithelial Cells: Relevance in Ulcerative Colitis
Cristina Bauset, Lluis Lis-Lopez, Sandra Coll, Laura Gisbert-Ferrándiz, Dulce C. Macias-Ceja, Marta Seco-Cervera, Francisco Navarro, Juan V. Esplugues, Sara Calatayud, Dolores Ortiz-Masia, Maria D. Barrachina, Jesús Cosín-Roger
Biomedicines.2022; 10(3): 532. CrossRef - Succinate as a New Actor in Pluripotency and Early Development?
Damien Detraux, Patricia Renard
Metabolites.2022; 12(7): 651. CrossRef - Succinate Dehydrogenase, Succinate, and Superoxides: A Genetic, Epigenetic, Metabolic, Environmental Explosive Crossroad
Paule Bénit, Judith Goncalves, Riyad El Khoury, Malgorzata Rak, Judith Favier, Anne-Paule Gimenez-Roqueplo, Pierre Rustin
Biomedicines.2022; 10(8): 1788. CrossRef - Aqueous, Non-Polymer-Based Perovskite Quantum Dots for Bioimaging: Conserving Fluorescence and Long-Term Stability via Simple and Robust Synthesis
Sanjayan C G, Jyothi Mannekote Shivanna, Jessica D. Schiffman, Sakar Mohan, Srinivasa Budagumpi, R. Geetha Balakrishna
ACS Applied Materials & Interfaces.2022; 14(34): 38471. CrossRef - Targeting the succinate receptor effectively inhibits periodontitis
Yuqi Guo, Fangxi Xu, Scott C. Thomas, Yanli Zhang, Bidisha Paul, Satish Sakilam, Sungpil Chae, Patty Li, Caleb Almeter, Angela R. Kamer, Paramjit Arora, Dana T. Graves, Deepak Saxena, Xin Li
Cell Reports.2022; 40(12): 111389. CrossRef - Gemigliptin Alleviates Succinate-Induced Hepatic Stellate Cell Activation by Ameliorating Mitochondrial Dysfunction
Giang Nguyen, So Young Park, Dinh Vinh Do, Dae-Hee Choi, Eun-Hee Cho
Endocrinology and Metabolism.2022; 37(6): 918. CrossRef - Succinate at the Crossroad of Metabolism and Angiogenesis: Roles of SDH, HIF1α and SUCNR1
Reham Atallah, Andrea Olschewski, Akos Heinemann
Biomedicines.2022; 10(12): 3089. CrossRef - Divulging a Pleiotropic Role of Succinate Receptor SUCNR1 in Renal Cell Carcinoma Microenvironment
Rania Najm, Mahmood Yaseen Hachim, Richard K. Kandasamy
Cancers.2022; 14(24): 6064. CrossRef - Succinate dehydrogenase inhibitors: in silico flux analysis and in vivo metabolomics investigations show no severe metabolic consequences for rats and humans
H. Kamp, J. Wahrheit, S. Stinchcombe, T. Walk, F. Stauber, B.v. Ravenzwaay
Food and Chemical Toxicology.2021; 150: 112085. CrossRef - Can polarization of macrophage metabolism enhance cardiac regeneration?
Connor Lantz, Amanda Becker, Edward B. Thorp
Journal of Molecular and Cellular Cardiology.2021; 160: 87. CrossRef - Ethylmethylhydroxypyridine Succinate Induces Anti-inflammatory Polarization of Microglia in the Brain of Aging Rat
Y. I. Kirova, F. M. Shakova, T. A. Voronina
Biochemistry (Moscow), Supplement Series A: Membrane and Cell Biology.2021; 15(4): 356. CrossRef - Model systems in SDHx-related pheochromocytoma/paraganglioma
Krisztina Takács-Vellai, Zsolt Farkas, Fanni Ősz, Gordon W. Stewart
Cancer and Metastasis Reviews.2021; 40(4): 1177. CrossRef
- Type 2 diabetes and succinate: unmasking an age-old molecule

- Thyroid
- Recent Improvements in Genomic and Transcriptomic Understanding of Anaplastic and Poorly Differentiated Thyroid Cancers
- Seong-Keun Yoo, Young Shin Song, Young Joo Park, Jeong-Sun Seo
- Endocrinol Metab. 2020;35(1):44-54. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.44
- 7,235 View
- 242 Download
- 16 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
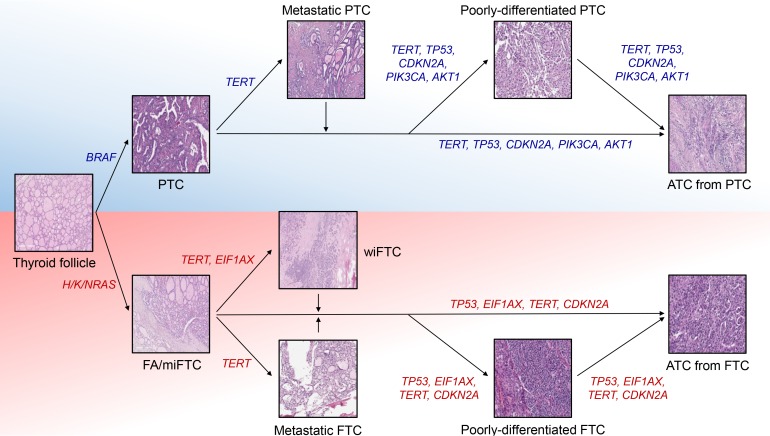
ePub Anaplastic thyroid cancer (ATC) is a lethal human cancer with a 5-year survival rate of less than 10%. Recently, its genomic and transcriptomic characteristics have been extensively elucidated over 5 years owing to advance in high throughput sequencing. These efforts have extended molecular understandings into the progression mechanisms and therapeutic vulnerabilities of aggressive thyroid cancers. In this review, we provide an overview of genomic and transcriptomic alterations in ATC and poorly-differentiated thyroid cancer, which are distinguished from differentiated thyroid cancers. Clinically relevant genomic alterations and deregulated signaling pathways will be able to shed light on more effective prevention and stratified therapeutic interventions for affected patients.
-
Citations
Citations to this article as recorded by- The genomic and evolutionary landscapes of anaplastic thyroid carcinoma
Peter Y.F. Zeng, Stephenie D. Prokopec, Stephen Y. Lai, Nicole Pinto, Michelle A. Chan-Seng-Yue, Roderick Clifton-Bligh, Michelle D. Williams, Christopher J. Howlett, Paul Plantinga, Matthew J. Cecchini, Alfred K. Lam, Iram Siddiqui, Jianxin Wang, Ren X.
Cell Reports.2024; 43(3): 113826. CrossRef - Comparative study between poorly differentiated thyroid cancer and anaplastic thyroid cancer: real-world pathological distribution, death attribution, and prognostic factor estimation
Kun Zhang, Xinyi Wang, Tao Wei, Zhihui Li, Jingqiang Zhu, Ya-Wen Chen
Frontiers in Endocrinology.2024;[Epub] CrossRef - Dabrafenib and Trametinib Therapy for Advanced Anaplastic Thyroid Cancer – Real-World Outcomes From UK Centres
C. Lorimer, L. Cheng, R. Chandler, K. Garcez, V. Gill, K. Graham, W. Grant, S. Sardo Infirri, J. Wadsley, L. Wall, N. Webber, K.H. Wong, K. Newbold
Clinical Oncology.2023; 35(1): e60. CrossRef - MicroRNA expression profiling of RAS-mutant thyroid tumors with follicular architecture: microRNA signatures to discriminate benign from malignant lesions
E. Macerola, A. M. Poma, P. Vignali, A. Proietti, L. Torregrossa, C. Ugolini, A. Basolo, A. Matrone, R. Elisei, F. Santini, F. Basolo
Journal of Endocrinological Investigation.2023; 46(8): 1651. CrossRef - RBX1 regulates PKM alternative splicing to facilitate anaplastic thyroid carcinoma metastasis and aerobic glycolysis by destroying the SMAR1/HDAC6 complex
Debin Xu, Jichun Yu, Yuting Yang, Yunyan Du, Hongcheng Lu, Shouhua Zhang, Qian Feng, Yi Yu, Liang Hao, Jun Shao, Leifeng Chen
Cell & Bioscience.2023;[Epub] CrossRef - Multi-Omics and Management of Follicular Carcinoma of the Thyroid
Thifhelimbilu Emmanuel Luvhengo, Ifongo Bombil, Arian Mokhtari, Maeyane Stephens Moeng, Demetra Demetriou, Claire Sanders, Zodwa Dlamini
Biomedicines.2023; 11(4): 1217. CrossRef - Genomic landscape of anaplastic thyroid cancer and implications on therapy
Leslie Cheng, Kate Newbold
Current Opinion in Endocrine and Metabolic Research.2023; 30: 100458. CrossRef - Modeling the tumor microenvironment of anaplastic thyroid cancer: an orthotopic tumor model in C57BL/6 mice
Zhen Xu, Hyo Shik Shin, Yoo Hyung Kim, Seong Yun Ha, Jae-Kyung Won, Su-jin Kim, Young Joo Park, Sareh Parangi, Sun Wook Cho, Kyu Eun Lee
Frontiers in Immunology.2023;[Epub] CrossRef - Characterization of the genomic alterations in poorly differentiated thyroid cancer
Yeeun Lee, SeongRyeol Moon, Jae Yeon Seok, Joon-Hyop Lee, Seungyoon Nam, Yoo Seung Chung
Scientific Reports.2023;[Epub] CrossRef - Genetica del carcinoma anaplastico della tiroide
Teresa Ramone, Chiara Mulè, Cristina Romei, Raffaele Ciampi, Eleonora Molinaro, Rossella Elisei
L'Endocrinologo.2022; 23(2): 208. CrossRef - Tissue and circulating PD-L2: moving from health and immune-mediated diseases to head and neck oncology
Elena Muraro, Rebecca Romanò, Giuseppe Fanetti, Emanuela Vaccher, Irene Turturici, Valentina Lupato, Fabio Biagio La Torre, Jerry Polesel, Elisabetta Fratta, Vittorio Giacomarra, Giovanni Franchin, Agostino Steffan, Michele Spina, Salvatore Alfieri
Critical Reviews in Oncology/Hematology.2022; 175: 103707. CrossRef - Recent Improvements in the Treatment of High-Risk Thyroid Cancer
Eun Kyung Lee
Korean Society for Head and Neck Oncology.2022; 38(1): 1. CrossRef - Inhibition of Glycogen Metabolism Induces Reactive Oxygen Species-Dependent Cytotoxicity in Anaplastic Thyroid Cancer in Female Mice
Cole D Davidson, Jennifer A Tomczak, Eyal Amiel, Frances E Carr
Endocrinology.2022;[Epub] CrossRef - Survival prognostic factors for differentiated thyroid cancer patients with pulmonary metastases: A systematic review and meta-analysis
Hao Zhao, Chun-Hao Liu, Yue Cao, Li-Yang Zhang, Ya Zhao, Yue-Wu Liu, Hong-Feng Liu, Yan-Song Lin, Xiao-Yi Li
Frontiers in Oncology.2022;[Epub] CrossRef - 2021 American Thyroid Association Guidelines for Management of Patients with Anaplastic Thyroid Cancer
Keith C. Bible, Electron Kebebew, James Brierley, Juan P. Brito, Maria E. Cabanillas, Thomas J. Clark, Antonio Di Cristofano, Robert Foote, Thomas Giordano, Jan Kasperbauer, Kate Newbold, Yuri E. Nikiforov, Gregory Randolph, M. Sara Rosenthal, Anna M. Saw
Thyroid.2021; 31(3): 337. CrossRef - Intratumoral Heterogeneity in Differentiated Thyroid Tumors: An Intriguing Reappraisal in the Era of Personalized Medicine
Antonio Ieni, Roberto Vita, Cristina Pizzimenti, Salvatore Benvenga, Giovanni Tuccari
Journal of Personalized Medicine.2021; 11(5): 333. CrossRef - The Role of Altered Mitochondrial Metabolism in Thyroid Cancer Development and Mitochondria-Targeted Thyroid Cancer Treatment
Siarhei A. Dabravolski, Nikita G. Nikiforov, Alexander D. Zhuravlev, Nikolay A. Orekhov, Liudmila M. Mikhaleva, Alexander N. Orekhov
International Journal of Molecular Sciences.2021; 23(1): 460. CrossRef - Mechanisms of TERT Reactivation and Its Interaction with BRAFV600E
Young Shin Song, Young Joo Park
Endocrinology and Metabolism.2020; 35(3): 515. CrossRef
- The genomic and evolutionary landscapes of anaplastic thyroid carcinoma

- Bone Metabolism
- Potential Biomarkers to Improve the Prediction of Osteoporotic Fractures
- Beom-Jun Kim, Seung Hun Lee, Jung-Min Koh
- Endocrinol Metab. 2020;35(1):55-63. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.55

- 4,802 View
- 115 Download
- 14 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Osteoporotic fracture (OF) is associated with high disability and morbidity rates. The burden of OF may be reduced by early identification of subjects who are vulnerable to fracture. Although the current fracture risk assessment model includes clinical risk factors (CRFs) and bone mineral density (BMD), its overall ability to identify individuals at high risk for fracture remains suboptimal. Efforts have therefore been made to identify potential biomarkers that can predict the risk of OF, independent of or combined with CRFs and BMD. This review highlights the emerging biomarkers of bone metabolism, including sphongosine-1-phosphate, leucine-rich repeat-containing 17, macrophage migration inhibitory factor, sclerostin, receptor activator of nuclear factor-κB ligand, and periostin, and the importance of biomarker risk score, generated by combining these markers, in enhancing the accuracy of fracture prediction.
-
Citations
Citations to this article as recorded by- The administration of bovine hydroxyapatite-alendronate implant accelerates bone defect healing in an osteoporotic rat
Toetik Aryani, Aniek Setiya Budiatin, Samirah, Aulia Maulidina, Aulia Intan Firdaus, Maria Apriliani Gani, Khoirotin Nisak, Junaidi Khotib, Alvi Jauharotus Syukriya
Technology and Health Care.2023; 31(5): 1747. CrossRef - Impact of Intravenous Iron Substitution on Serum Phosphate Levels and Bone Turnover Markers—An Open-Label Pilot Study
Alexandra Struppe, Jakob E. Schanda, Andreas Baierl, Paul Watzl, Christian Muschitz
Nutrients.2023; 15(12): 2693. CrossRef - Dynamics of Bone Disease Biomarkers Dickkopf-1 and Sclerostin in Patients with Multiple Myeloma
Vladimir Gerov, Daniela Gerova, Ilina Micheva, Miglena Nikolova, Galya Mihaylova, Bistra Galunska
Journal of Clinical Medicine.2023; 12(13): 4440. CrossRef - Impact of vitamin D supplementation on markers of bone turnover: Systematic review and meta‐analysis of randomised controlled trials
Mohammad Hassan Sohouli, Sicong Wang, Faisal Almuqayyid, Mariana Papini Gabiatti, Fateme Mozaffari, Zahra Mohamadian, Nazanin Koushki, Kamar Allayl Alras, Abdullah M. AlHossan, Saud K. Albatati, Aya Alfardous Alazm, Saeed Baradwan, Mihnea‐Alexandru Găman,
European Journal of Clinical Investigation.2023;[Epub] CrossRef - Night shift work and serum markers of bone turnover in male shift workers
Margherita Martelli, Gianmaria Salvio, Raffaella Lazzarini, Marijana Milinkovic, Alessandro Ciarloni, Giancarlo Balercia, Lory Santarelli, Massimo Bracci
Chronobiology International.2023; 40(9): 1270. CrossRef - Circulating sRANKL, Periostin, and Osteopontin as Biomarkers for the Assessment of Activated Osteoclastogenesis in Myeloma Related Bone Disease
Vladimir Gerov, Daniela Gerova, Ilina Micheva, Miglena Nikolova, Milena Pasheva, Neshe Nazifova, Bistra Galunska
Cancers.2023; 15(23): 5562. CrossRef - Oral Administration of Isovitexin, a Naturally Occurring Apigenin Derivative Showed Osteoanabolic Effect in Ovariectomized Mice: A Comparative Study with Teriparatide
Subhashis Pal, Shivani Sharma, Konica Porwal, Mohammed Riyazuddin, Chirag Kulkarni, Sourav Chattopadhyay, Sabyasachi Sanyal, Jiaur R. Gayen, Naibedya Chattopadhyay
Calcified Tissue International.2022; 111(2): 196. CrossRef - Serum sclerostin levels in osteoporotic fracture patients
Erwin A. Gorter, Casper R. Reinders, Pieta Krijnen, Natasha M. Appelman-Dijkstra, Inger B. Schipper
European Journal of Trauma and Emergency Surgery.2022; 48(6): 4857. CrossRef - Elevated gamma-glutamyl transpeptidase level is associated with an increased risk of hip fracture in postmenopausal women
Kyoung Jin Kim, Namki Hong, Min Heui Yu, Seunghyun Lee, Sungjae Shin, Sin Gon Kim, Yumie Rhee
Scientific Reports.2022;[Epub] CrossRef - Effect of androgen deprivation therapy on serum levels of sclerostin, Dickkopf-1, and osteoprotegerin: a cross-sectional and longitudinal analysis
Alice Wang, Nishi Karunasinghe, Lindsay D. Plank, Shuotun Zhu, Sue Osborne, Charis Brown, Karen Bishop, Tiffany Schwass, Sofian Tijono, Michael Holmes, Jonathan Masters, Roger Huang, Christine Keven, Lynnette R. Ferguson, Ross Lawrenson
Scientific Reports.2021;[Epub] CrossRef - Update on Glucocorticoid Induced Osteoporosis
Soo-Kyung Cho, Yoon-Kyoung Sung
Endocrinology and Metabolism.2021; 36(3): 536. CrossRef - Nobiletin promotes osteogenic differentiation of human osteoblastic cell line (MG-63) through activating the BMP-2/RUNX-2 signaling pathway
Ying Pang, Lili Liu, Hong Mu, Vishnu Priya Veeraraghavan
Saudi Journal of Biological Sciences.2021; 28(9): 4916. CrossRef
- The administration of bovine hydroxyapatite-alendronate implant accelerates bone defect healing in an osteoporotic rat

- Miscellaneous
- Rare PTH Gene Mutations Causing Parathyroid Disorders: A Review
- Joon-Hyop Lee, Munkhtugs Davaatseren, Sihoon Lee
- Endocrinol Metab. 2020;35(1):64-70. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.64

- 5,078 View
- 107 Download
- 8 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Since parathyroid hormone (PTH) was first isolated and its gene (
PTH ) was sequenced, only eightPTH mutations have been discovered. The C18R mutation inPTH , discovered in 1990, was the first to be reported. This autosomal dominant mutation induces endoplasmic reticulum stress and subsequent apoptosis in parathyroid cells. The next mutation, which was reported in 1992, is associated with exon skipping. The substitution of G with C in the first nucleotide of the second intron results in the exclusion of the second exon; since this exon includes the initiation codon, translation initiation is prevented. An S23P mutation and an S23X mutation at the same residue were reported in 1999 and 2012, respectively. Both mutations resulted in hypoparathyroidism. In 2008, a somatic R83X mutation was detected in a parathyroid adenoma tissue sample collected from a patient with hyperparathyroidism. In 2013, a heterozygous p.Met1_Asp6del mutation was incidentally discovered in a case-control study. Two years later, the R56C mutation was reported; this is the only reported hypoparathyroidism-causing mutation in the mature bioactive part ofPTH . In 2017, another heterozygous mutation, M14K, was detected. The discovery of these eight mutations in thePTH gene has provided insights into its function and broadened our understanding of the molecular mechanisms underlying mutation progression. Further attempts to detect other such mutations will help elucidate the functions of PTH in a more sophisticated manner.-
Citations
Citations to this article as recorded by- Molecular and Clinical Spectrum of Primary Hyperparathyroidism
Smita Jha, William F Simonds
Endocrine Reviews.2023; 44(5): 779. CrossRef - Rare cause of persistent hypocalcaemia in infancy due to PTH gene mutation
Savita Khadse, Vrushali Satish Takalikar, Radha Ghildiyal, Nikhil Shah
BMJ Case Reports.2023; 16(9): e256358. CrossRef - Homozygous Ser-1 to Pro-1 mutation in parathyroid hormone identified in hypocalcemic patients results in secretion of a biologically inactive pro-hormone
Patrick Hanna, Ashok Khatri, Shawn Choi, Severine Brabant, Matti L. Gild, Marie L. Piketty, Bruno Francou, Dominique Prié, John T. Potts, Roderick J. Clifton-Bligh, Agnès Linglart, Thomas J. Gardella, Harald Jüppner
Proceedings of the National Academy of Sciences.2023;[Epub] CrossRef - Genetics of monogenic disorders of calcium and bone metabolism
Paul J. Newey, Fadil M. Hannan, Abbie Wilson, Rajesh V. Thakker
Clinical Endocrinology.2022; 97(4): 483. CrossRef - Homozygous missense variant of PTH (c.166C>T, p.(Arg56Cys)) as the cause of familial isolated hypoparathyroidism in a three-year-old child
Stine Linding Andersen, Anja Lisbeth Frederiksen, Astrid Bruun Rasmussen, Mette Madsen, Ann-Margrethe Rønholt Christensen
Journal of Pediatric Endocrinology and Metabolism.2022; 35(5): 691. CrossRef - Novel PTH Gene Mutations Causing Isolated Hypoparathyroidism
Colin P Hawkes, Jamal M Al Jubeh, Dong Li, Susan E Tucker, Tara Rajiyah, Michael A Levine
The Journal of Clinical Endocrinology & Metabolism.2022; 107(6): e2449. CrossRef
- Molecular and Clinical Spectrum of Primary Hyperparathyroidism

- Miscellaneous
- Machine Learning Applications in Endocrinology and Metabolism Research: An Overview
- Namki Hong, Heajeong Park, Yumie Rhee
- Endocrinol Metab. 2020;35(1):71-84. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.71

- 15,505 View
- 205 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Machine learning (ML) applications have received extensive attention in endocrinology research during the last decade. This review summarizes the basic concepts of ML and certain research topics in endocrinology and metabolism where ML principles have been actively deployed. Relevant studies are discussed to provide an overview of the methodology, main findings, and limitations of ML, with the goal of stimulating insights into future research directions. Clear, testable study hypotheses stem from unmet clinical needs, and the management of data quality (beyond a focus on quantity alone), open collaboration between clinical experts and ML engineers, the development of interpretable high-performance ML models beyond the black-box nature of some algorithms, and a creative environment are the core prerequisites for the foreseeable changes expected to be brought about by ML and artificial intelligence in the field of endocrinology and metabolism, with actual improvements in clinical practice beyond hype. Of note, endocrinologists will continue to play a central role in these developments as domain experts who can properly generate, refine, analyze, and interpret data with a combination of clinical expertise and scientific rigor.
-
Citations
Citations to this article as recorded by- Artificial Intelligence for Predicting and Diagnosing Complications of Diabetes
Jingtong Huang, Andrea M. Yeung, David G. Armstrong, Ashley N. Battarbee, Jorge Cuadros, Juan C. Espinoza, Samantha Kleinberg, Nestoras Mathioudakis, Mark A. Swerdlow, David C. Klonoff
Journal of Diabetes Science and Technology.2023; 17(1): 224. CrossRef - Expressions of Cushing’s syndrome in multiple endocrine neoplasia type 1
William F. Simonds
Frontiers in Endocrinology.2023;[Epub] CrossRef - Application of machine learning and artificial intelligence in the diagnosis and classification of polycystic ovarian syndrome: a systematic review
Francisco J. Barrera, Ethan D.L. Brown, Amanda Rojo, Javier Obeso, Hiram Plata, Eddy P. Lincango, Nancy Terry, René Rodríguez-Gutiérrez, Janet E. Hall, Skand Shekhar
Frontiers in Endocrinology.2023;[Epub] CrossRef - Predictors of rituximab effect on modified Rodnan skin score in systemic sclerosis: a machine-learning analysis of the DesiReS trial
Satoshi Ebata, Koji Oba, Kosuke Kashiwabara, Keiko Ueda, Yukari Uemura, Takeyuki Watadani, Takemichi Fukasawa, Shunsuke Miura, Asako Yoshizaki-Ogawa, Asano Yoshihide, Ayumi Yoshizaki, Shinichi Sato
Rheumatology.2022; 61(11): 4364. CrossRef - Automating and improving cardiovascular disease prediction using Machine learning and EMR data features from a regional healthcare system
Qi Li, Alina Campan, Ai Ren, Wael E. Eid
International Journal of Medical Informatics.2022; 163: 104786. CrossRef - An Interactive Online App for Predicting Diabetes via Machine Learning from Environment-Polluting Chemical Exposure Data
Rosy Oh, Hong Kyu Lee, Youngmi Kim Pak, Man-Suk Oh
International Journal of Environmental Research and Public Health.2022; 19(10): 5800. CrossRef - Ensemble blood glucose prediction in diabetes mellitus: A review
M.Z. Wadghiri, A. Idri, Touria El Idrissi, Hajar Hakkoum
Computers in Biology and Medicine.2022; 147: 105674. CrossRef - The maze runner: navigating through basic kinetics to AI models of human metabolism pathology
Arina V. Martyshina, Oksana M. Tilinova, Anastasia A. Simanova, Olga S. Knyazeva, Irina V. Dokukina
Procedia Computer Science.2022; 213: 271. CrossRef - Applications of Machine Learning in Bone and Mineral Research
Sung Hye Kong, Chan Soo Shin
Endocrinology and Metabolism.2021; 36(5): 928. CrossRef - Facial Recognition Intensity in Disease Diagnosis Using Automatic Facial Recognition
Danning Wu, Shi Chen, Yuelun Zhang, Huabing Zhang, Qing Wang, Jianqiang Li, Yibo Fu, Shirui Wang, Hongbo Yang, Hanze Du, Huijuan Zhu, Hui Pan, Zhen Shen
Journal of Personalized Medicine.2021; 11(11): 1172. CrossRef - The Application of Artificial Intelligence and Machine Learning in Pituitary Adenomas
Congxin Dai, Bowen Sun, Renzhi Wang, Jun Kang
Frontiers in Oncology.2021;[Epub] CrossRef - Real World Data and Artificial Intelligence in Diabetology
Kwang Joon Kim
The Journal of Korean Diabetes.2020; 21(3): 140. CrossRef - A Novel Detection Framework for Detecting Abnormal Human Behavior
Chengfei Wu, Zixuan Cheng, Yi-Zhang Jiang
Mathematical Problems in Engineering.2020; 2020: 1. CrossRef
- Artificial Intelligence for Predicting and Diagnosing Complications of Diabetes

- Diabetes
- Prevalence and Current Management of Cardiovascular Risk Factors in Korean Adults Based on Fact Sheets
- Eun-Jung Rhee
- Endocrinol Metab. 2020;35(1):85-94. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.85
- 8,660 View
- 161 Download
- 28 Web of Science
- 38 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Korea is currently an aged society and is on the cusp of becoming a superaged society in a few years. The health burden of cardiovascular diseases increases with age, and the increasing prevalence of cardiovascular risk factors, such as obesity, hypertension, diabetes mellitus, and dyslipidemia, may be linked to increased population-level cardiovascular risk. In 2018, the prevalence of obesity in Korea was 35.7% (men, 45.4%; women, 26.5%) according to the Obesity Fact Sheet 2019, based on National Health Insurance Corporation medical checkup data. In 2016, the prevalence of diabetes was 14.4% in Koreans older than 30 years according to the Diabetes Fact Sheet published by the Korean Diabetes Association, based on data from the Korean National Health and Nutrition Examination Survey. The prevalence of hypertension in the total population of Korea in 2018 was 28.3% according to the Korean Hypertension Fact Sheet produced by the Korean Society of Hypertension. Lastly, the prevalence of dyslipidemia in 2018 was 40.5% according to the Dyslipidemia Fact Sheet published by the Korean Society of Lipid and Atherosclerosis. In this article, I would like to review the prevalence and current management of cardiovascular risk factors in Korea according to the fact sheets released by various associations.
-
Citations
Citations to this article as recorded by- Non-invasive coronary artery disease identification through the iris and bio-demographic health profile features using stacking learning
Ferdi Özbilgin, Çetin Kurnaz, Ertan Aydın
Image and Vision Computing.2024; 146: 105046. CrossRef - A Study on Changes in Nutritional and Blood Conditions Before and After Consumption of Diabetic Soymilk in Elderly Women with Diabetes
Hyo-Jeong Hwang, Soon-Hee Park, Seon-Young Park, Soo-Rin Ahn, Su-Jin Park, Yoo-Jin Lee, Kwang-Jin Chon, Chung-Hwa Song, Dae-Gyun Moon, Kyung-Ok Shin
Journal of the Korean Society of Food Science and Nutrition.2023; 52(4): 341. CrossRef - Effect of hemp seed oil on lipid metabolism in rats fed a high-cholesterol diet
Jin A Lee, Seong-Soo Roh, Woo Rak Lee, Mi-Rae Shin
Journal of Nutrition and Health.2023; 56(4): 361. CrossRef - The Longitudinal Effect of Ultra‐Processed Food on the Development of Dyslipidemia/Obesity as Assessed by the NOVA System and Food Compass Score
Li‐Juan Tan, Su Bin Hwang, Sangah Shin
Molecular Nutrition & Food Research.2023;[Epub] CrossRef - Sex Differences in Coronary Artery Disease: Insights From the KoRean wOmen’S chest pain rEgistry (KoROSE)
Hack-Lyoung Kim, Myung-A Kim
Korean Circulation Journal.2023; 53(10): 655. CrossRef - Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea
Jeonghee Jeong, Mijin Kim
Healthcare.2022; 10(1): 112. CrossRef - Genetic Determinants of Visit-to-Visit Lipid Variability: Genome-Wide Association Study in Statin-Naïve Korean Population
Jun-Bean Park, Eunsoon Shin, Jong-Eun Lee, Seung Jae Lee, Heesun Lee, Su-Yeon Choi, Eun Kyung Choe, Seung Ho Choi, Hyo Eun Park
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - TheIn VitroAntioxidant and Antidiabetic Activity of Various Fractions from Monascus-Fermented Ginger Extract
Su-Min Yoon, Young-Hee Pyo
Journal of the Korean Society of Food Science and Nutrition.2022; 51(2): 125. CrossRef - The Influence of Obesity and Metabolic Health on Vascular Health
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(1): 1. CrossRef - Correlates of Objectively Measured Sitting Time in South Korean Adults: 2014–2015 Korea National Health and Nutrition Examination Survey
Hyo Lee, Miyoung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Association between metabolic syndrome and left ventricular geometric change including diastolic dysfunction
Seung‐Jae Lee, Hyunah Kim, Byeong Kil Oh, Hyo‐In Choi, Ki‐Chul Sung, Jeonggyu Kang, Mi Yeon Lee, Jong‐Young Lee
Clinical Cardiology.2022; 45(7): 767. CrossRef - Sex and Gender Determinants of Vascular Disease in the Global Context
Rubee Dev, Alayne M. Adams, Valeria Raparelli, Colleen M. Norris, Louise Pilote
Canadian Journal of Cardiology.2022; 38(12): 1799. CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Dyslipidaemia—Genotype Interactions with Nutrient Intake and Cerebro-Cardiovascular Disease
Sung-Bum Lee, Ja-Eun Choi, Byoungjin Park, Mi-Yeon Cha, Kyung-Won Hong, Dong-Hyuk Jung
Biomedicines.2022; 10(7): 1615. CrossRef - Current status of obesity treatment in Korea: based on the 2020 Korean Society for the Study of Obesity guidelines for obesity management
Eun-Jung Rhee
Journal of the Korean Medical Association.2022; 65(7): 388. CrossRef - Association between endocrine-disrupting chemical mixture and metabolic indices among children, adolescents, and adults: A population-based study in Korea
Byungmi Kim, Bohyun Park, Chung Ho Kim, Seyoung Kim, Bomi Park
Environmental Pollution.2022; 315: 120399. CrossRef - Genetic variation rs1121980 in the fat mass and obesity-associated gene (FTO) is associated with dietary intake in Koreans
Young Goh, Jeong-Hwa Choi
Food & Nutrition Research.2022;[Epub] CrossRef - The association between hyperuricemia and cardiovascular disease history: A cross-sectional study using KoGES HEXA data
Joo-Hee Kim, Mi Jung Kwon, Hyo Geun Choi, Sang Jun Lee, Sung-Woo Kim, Ji Hee Kim, Bong Cheol Kwon, Jung Woo Lee
Medicine.2022; 101(51): e32338. CrossRef - Association between Endocrine-Disrupting Chemical Mixture and Metabolic Indices Among Children, Adolescents, And Adults: A Population-Based Study in Korea
Byungmi Kim, Chung Ho Kim, Bohyun Park, Seyoung Kim, Bomi Park
SSRN Electronic Journal .2022;[Epub] CrossRef - Thirty-six Year Trends in Mortality from Diseases of Circulatory System in Korea
Jongmin Baek, Hokyou Lee, Hyeok-Hee Lee, Ji Eun Heo, So Mi Jemma Cho, Hyeon Chang Kim
Korean Circulation Journal.2021; 51(4): 320. CrossRef - Identification of susceptibility loci for cardiovascular disease in adults with hypertension, diabetes, and dyslipidemia
Youhyun Song, Ja-Eun Choi, Yu-Jin Kwon, Hyuk-Jae Chang, Jung Oh Kim, Da-Hyun Park, Jae-Min Park, Seong-Jin Kim, Ji Won Lee, Kyung-Won Hong
Journal of Translational Medicine.2021;[Epub] CrossRef - Association of Maintaining Healthy Habits with Clinical Outcomes in Patients with Diabetes, Dyslipidemia or Hypertension
Jeong Hyeon Kim, Young Ho Yun
Korean Journal of Family Practice.2021; 11(1): 74. CrossRef - Epidemiology of cardiovascular disease and its risk factors in Korea
Hyeon Chang Kim
Global Health & Medicine.2021; 3(3): 134. CrossRef - Cumulative exposure to impaired fasting glucose and future risk of type 2 diabetes mellitus
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Oak-Kee Hong, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Diabetes Research and Clinical Practice.2021; 175: 108799. CrossRef - Association between Diabetes Mellitus and Oral Health Status in Patients with Cardiovascular Diseases: A Nationwide Population-Based Study
Su-Jin Han, Youn-Jung Son, Bo-Hwan Kim
International Journal of Environmental Research and Public Health.2021; 18(9): 4889. CrossRef - Comorbidities and Factors Determining Medical Expenses and Length of Stay for Admitted COVID-19 Patients in Korea
Su Yeon Jang, Jeong-Yeon Seon, Seok-Jun Yoon, So-Youn Park, Seung Heon Lee, In-Hwan Oh
Risk Management and Healthcare Policy.2021; Volume 14: 2021. CrossRef - Metabolic Syndrome Fact Sheet 2021: Executive Report
Ji Hye Huh, Dae Ryong Kang, Jang Young Kim, Kwang Kon Koh
CardioMetabolic Syndrome Journal.2021; 1(2): 125. CrossRef - Effect of Triticum turgidum ssp. turanicum on serum lipid levels and colonic microbiota of dyslipidemia-induced rats
Hyeon-Ju Seo, Kyoung-Sik Han
Toxicology and Environmental Health Sciences.2021; 13(3): 195. CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - Comparison of the Efficacy and Safety of Atorvastatin 40 mg/ω-3 Fatty Acids 4 g Fixed-dose Combination and Atorvastatin 40 mg Monotherapy in Hypertriglyceridemic Patients who Poorly Respond to Atorvastatin 40 mg Monotherapy: An 8-week, Multicenter, Random
Jong Shin Woo, Soon Jun Hong, Dong Hoon Cha, Kee Sik Kim, Moo Hyun Kim, Jun-Won Lee, Myung Ho Jeong, Jin-Ok Jeong, Jun-Hee Lee, Doo Soo Jeon, Eun Joo Cho, Soon Kil Kim, Jun Kwan, Chang Gyu Park, Hae Young Lee, Taek Jong Hong, Jinho Shin, Ho Joong Youn, Do
Clinical Therapeutics.2021; 43(8): 1419. CrossRef - Differing Nutrient Intake and Dietary Patterns According to the Presence of Hyper-Low-Density Lipoprotein Cholesterolemia or Hypertriglyceridemia
Yu-Jin Kwon, Sujee Lee, Hye Sun Lee, Ji-Won Lee
Nutrients.2021; 13(9): 3008. CrossRef - A Century of Progress in Diabetes Care with Insulin: A History of Innovations and Foundation for the Future
Seung-Hwan Lee, Kun-Ho Yoon
Diabetes & Metabolism Journal.2021; 45(5): 629. CrossRef - Frequency of Exposure to Impaired Fasting Glucose and Risk of Mortality and Cardiovascular Outcomes
Seung-Hwan Lee, Kyungdo Han, Hyuk-Sang Kwon, Mee Kyoung Kim
Endocrinology and Metabolism.2021; 36(5): 1007. CrossRef - Metabolic risks in living kidney donors in South Korea
Eunjeong Kang, Jina Park, Hyo Jeong Kim, Sehoon Park, Minsu Park, Yaerim Kim, Kwangsoo Kim, Sang Min Park, Dong-Wan Chae, Ho Jun Chin, Jung Pyo Lee, Sik Lee, Soo Wan Kim, Jang-Hee Cho, Miyeun Han, Yong Chul Kim, Yon Su Kim, Insun Choi, Hajeong Lee
Kidney Research and Clinical Practice.2021; 40(4): 645. CrossRef - Invited commentary on “Prediction of postoperative mortality and morbidity in octogenarians with gastric cancer - Comparison of P-POSSUM, O-POSSUM, and E-POSSUM: A retrospective single-center cohort study”
Alessandro M. Paganini, Andrea Balla
International Journal of Surgery.2020; 78: 22. CrossRef - Association of the Healthy Eating Index with Estimated Cardiovascular Age in Adults from the KNHANES 2013–2017
Sunmin Park, Kyungjin Kim, Byung-Kook Lee, Jaeouk Ahn
Nutrients.2020; 12(10): 2912. CrossRef - Anti-Obesity and Antidiabetic Effects of Nelumbinis Semen Powder in High-Fat Diet-Induced Obese C57BL/6 Mice
Su Bin Hwang, Bog-Hieu Lee
Nutrients.2020; 12(11): 3576. CrossRef - Inhibitory Effect of Jeju Tea Extracts and Vanadate on Postprandial Hyperglycemia and Hypertension, and In Vitro Study
Shin Young Park
The Korean Journal of Clinical Laboratory Science.2020; 52(4): 398. CrossRef
- Non-invasive coronary artery disease identification through the iris and bio-demographic health profile features using stacking learning

- Adrenal gland
- A Brief Overview of the Epidemiology of Pheochromocytoma and Paraganglioma in Korea
- Yun Mi Choi
- Endocrinol Metab. 2020;35(1):95-96. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.95
- 4,186 View
- 85 Download

- Clinical Study
- Vitamin D Deficiency at Mid-Pregnancy Is Associated with a Higher Risk of Postpartum Glucose Intolerance in Women with Gestational Diabetes Mellitus
- Kyung-Soo Kim, Seok Won Park, Yong-Wook Cho, Soo-Kyung Kim
- Endocrinol Metab. 2020;35(1):97-105. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.97

- 5,497 View
- 117 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background To evaluate the association between serum 25-hydroxyvitamin D (25(OH)D) at mid-pregnancy and postpartum glucose intolerance in women with gestational diabetes mellitus (GDM).
Methods We enrolled 348 pregnant women diagnosed with GDM from August 2012 to October 2016. We measured serum 25(OH)D levels at mid-pregnancy and carried out a 75-g oral glucose tolerance test at 6 to 12 weeks after delivery. Vitamin D deficiency was defined as serum 25(OH)D <20 ng/mL.
Results The prevalence of vitamin D deficiency was 76.7% (
n =267). Women with vitamin D deficiency had a higher prevalence of postpartum glucose intolerance than did those without vitamin D deficiency (48.7% vs. 32.1%,P =0.011). Serum 25(OH)D level was negatively correlated with hemoglobin A1c at antepartum and postpartum period (antepartum:r =−0.186,P =0.001; postpartum:r =−0.129,P =0.047). Homeostasis model assessment of β-cell function was positively correlated with serum 25(OH)D level only postpartum (r =0.138,P =0.035). The risk of postpartum glucose intolerance was 2.00 times (95% confidence interval, 1.13 to 3.55) higher in women with vitamin D deficiency than in those without vitamin D deficiency (P =0.018).Conclusion In women with GDM, vitamin D deficiency at mid-pregnancy is associated with an elevated risk of postpartum glucose intolerance.
-
Citations
Citations to this article as recorded by- Vitamin D Supplementation for the Outcomes of Patients with Gestational Diabetes Mellitus and Neonates: A Meta-Analysis and Systematic Review
Chunfeng Wu, Yang Song, Xueying Wang, Pier P. Sainaghi
International Journal of Clinical Practice.2023; 2023: 1. CrossRef - Influence of hypovitaminosis D during pregnancy on glycemic and lipid profile, inflammatory indicators and anthropometry of pregnant and newborn
Sara de Figueiredo dos Santos, Paula Normando dos Reis Costa, Thaise Gasser Gouvêa, Nathalia Ferreira Antunes de Almeida, Felipe de Souza Cardoso
Clinical Nutrition ESPEN.2023; 54: 81. CrossRef - Risk factors associated with early postpartum glucose intolerance in women with a history of gestational diabetes mellitus: a systematic review and meta-analysis
Zhe Liu, Qianghuizi Zhang, Leyang Liu, Weiwei Liu
Endocrine.2023; 82(3): 498. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - Effect of Evidence-Based Diet Nursing on Intestinal Flora and Maternal and Infant Prognosis in Patients with Gestational Diabetes
Ying Jiang, Chunbo Qiu, Yuanping Wang, Bin He, Peng-Yue Zhang
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Vitamin D in gestational diabetes: A broadened frontier
Yu Zhu, Ling Li, Ping Li
Clinica Chimica Acta.2022; 537: 51. CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus (Diabetes Metab J 2021;45:547-57)
Kyung-Soo Kim
Diabetes & Metabolism Journal.2021; 45(6): 966. CrossRef
- Vitamin D Supplementation for the Outcomes of Patients with Gestational Diabetes Mellitus and Neonates: A Meta-Analysis and Systematic Review

- Clinical Study
- Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study
- Mijin Kim, Bo Hyun Kim, Hyungi Lee, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
- Endocrinol Metab. 2020;35(1):106-114. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.106
- 6,104 View
- 120 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
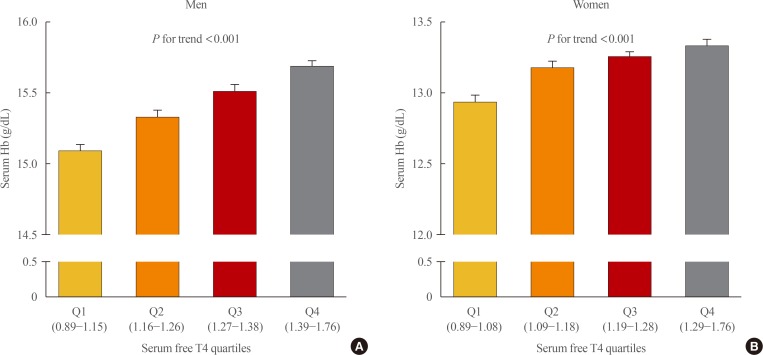
ePub Background Studies on the relationship between thyroid function and anemia in the euthyroid range are scarce. We aimed to evaluate the association between anemia and serum free thyroxine (fT4) and thyrotropin (TSH) in euthyroid adults.
Methods Data on 5,352 participants aged ≥19 years were obtained from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015). Anemia was defined as hemoglobin (Hb) <13 and <12 g/dL for men and women, respectively.
Results Overall, 6.1% of participants had anemia, and more women (9.9%) had anemia than men (2.8%,
P <0.001). In multivariate analysis, serum fT4 levels, but not TSH, were positively associated with serum Hb levels in both sexes (P <0.001, each). Serum Hb levels linearly reduced across decreasing serum fT4 quartile groups in both sexes (P <0.001, each). After adjusting for potential confounding factors, participants with low-normal fT4 had 4.4 (P =0.003) and 2.8 times (P <0.001) higher risk for anemia than those with high-normal fT4 among men and women, respectively. When participants were divided into two groups at 50 years of age, in younger participants, men and women with the first quartile were at higher risk of anemia than men with the second quartile (odds ratio [OR], 3.3;P =0.029) and women with the forth quartile (OR, 3.2;P <0.001), respectively. This association was not observed in older participants.Conclusion These results suggest that a low-normal level of serum fT4 was associated with a lower serum Hb level and a higher risk of anemia in euthyroid adults, especially in younger participants.
-
Citations
Citations to this article as recorded by- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank
Nicolien A van Vliet, Annelies E P Kamphuis, Wendy P J den Elzen, Gerard J Blauw, Jacobijn Gussekloo, Raymond Noordam, Diana van Heemst
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e643. CrossRef - Thyroid function, pernicious anemia and erythropoiesis: a two-sample Mendelian randomization study
Alisa D Kjaergaard, Alexander Teumer, Eirini Marouli, Panos Deloukas, Aleksander Kuś, Rosalie Sterenborg, Bjørn O Åsvold, Marco Medici, Christina Ellervik
Human Molecular Genetics.2022; 31(15): 2548. CrossRef - Changes of hematological indices in patients with diffuse toxic goiter
F. H. Saidova, L. M. Ahmedova, Zh. B. Aslanova, N. A. Najafov
Klinicheskaia khirurgiia.2021; 88(3-4): 76. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Zheng Feei Ma
Endocrinology and Metabolism.2020; 35(2): 484. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2020; 35(3): 669. CrossRef
- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank

- Clinical Study
- Quality of Life in Patients with Papillary Thyroid Microcarcinoma According to Treatment: Total Thyroidectomy with or without Radioactive Iodine Ablation
- Jonghwa Ahn, Min Ji Jeon, Eyun Song, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
- Endocrinol Metab. 2020;35(1):115-121. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.115
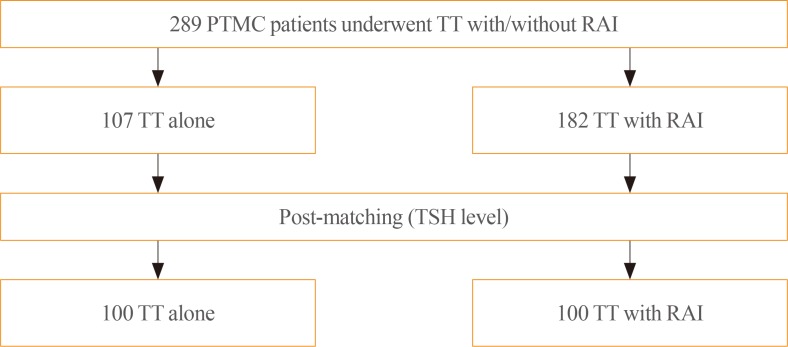
- 5,484 View
- 110 Download
- 8 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Recently, there has been some controversy regarding the role of radioactive iodine (RAI) ablation in the treatment of low-risk differentiated thyroid carcinoma (DTC), especially papillary thyroid microcarcinoma (PTMC). This study aimed to compare quality of life (QoL) parameters between patients with PTMC who underwent total thyroidectomy (TT) alone and those who underwent TT with RAI ablation.
Methods In this cross-sectional study, patients with PTMC who underwent TT with/without RAI remnant ablation were prospectively enrolled between June 2016 and October 2017. All patients completed three questionnaires: the 12-item short-form health survey (SF-12), thyroid cancer-specific quality of life (THYCA-QoL) questionnaire, and fear of progression (FoP) questionnaire.
Results The TT and TT with RAI groups comprised 107 and 182 patients, respectively. The TT with RAI group had significantly lower serum thyrotropin (TSH) levels than the TT group. However, after matching for TSH levels between the groups (
n =100 in both groups), there were no significant differences in baseline characteristics. According to the SF-12, the score for general health was significantly lower in the TT with RAI group than in the TT group (P =0.047). The THYCA-QoL also showed a significant difference in the “felt chilly” score between groups (P =0.023). No significant differences in FoP scores were observed between the groups.Conclusion Patients with PTMC who underwent TT with RAI ablation experienced more health-related problems than those managed with TT alone. These findings support the idea that RAI ablation should be carefully considered in patients with low-risk DTCs.
-
Citations
Citations to this article as recorded by- Quality of life of patients with thyroid cancer in Colombia
Oscar Gómez, Alvaro Sanabria
Endocrinología, Diabetes y Nutrición.2024; 71(2): 61. CrossRef - Quality of life of patients with thyroid cancer in Colombia
Oscar Gómez, Alvaro Sanabria
Endocrinología, Diabetes y Nutrición (English ed.).2024; 71(2): 61. CrossRef - Fear of Cancer Recurrence in Differentiated Thyroid Cancer Survivors: A Systematic Review
Jacob Hampton, Ahmad Alam, Nicholas Zdenkowski, Christopher Rowe, Elizabeth Fradgley, Christine J. O'Neill
Thyroid®.2024;[Epub] CrossRef - Review: Improving quality of life in patients with differentiated thyroid cancer
Pia Pace-Asciak, Jonathon O. Russell, Ralph P. Tufano
Frontiers in Oncology.2023;[Epub] CrossRef - Health-Related Quality of Life and Thyroid Cancer-Specific Symptoms in Patients Treated for Differentiated Thyroid Cancer: A Single-Center Cross-Sectional Survey from Mainland China
Changlian Chen, Jiayan Cao, Yueyang Wang, Xuya Han, Yaju Zhang, Shumei Zhuang
Thyroid.2023; 33(4): 474. CrossRef - The "not so good" thyroid cancer: a scoping review on risk factors associated with anxiety, depression and quality of life
Kyle Alexander, Sum-Yu Christina Lee, Stelios Georgiades, Constantina Constantinou
Journal of Medicine and Life.2023; 16(3): 348. CrossRef - Comparison of health‐related quality of life and cosmetic outcome between traditional gasless trans‐axillary endoscopic thyroidectomy and modified gasless trans‐axillary endoscopic thyroidectomy for patients with papillary thyroid microcarcinoma
Deenraj Kush Dhoomun, HuiLan Cai, Ning Li, YanHuan Qiu, XingRui Li, XiaoPeng Hu, WenZhuang Shen
Cancer Medicine.2023; 12(15): 16604. CrossRef - Risk of Adverse Pregnancy Outcomes in Young Women with Thyroid Cancer: A Systematic Review and Meta-Analysis
Shinje Moon, Ka Hee Yi, Young Joo Park
Cancers.2022; 14(10): 2382. CrossRef - Health-related quality of life following FDG-PET/CT for cytological indeterminate thyroid nodules
Elizabeth J de Koster, Olga Husson, Eveline W C M van Dam, G Sophie Mijnhout, Romana T Netea-Maier, Wim J G Oyen, Marieke Snel, Lioe-Fee de Geus-Oei, Dennis Vriens, _ _
Endocrine Connections.2022;[Epub] CrossRef - Is a four-week hormone suspension necessary for thyroid remnant ablation in low and intermediate risk patients? A pilot study with quality-of-life assessment
Poliane A.L. Santos, Maria E.D.M. Flamini, Felipe A. Mourato, Fernando R.A. Lima, Joelan A.L. Santos, Fabiana F. Lima, Estelita T.B. Albuquerque, Alexandra C. De Freitas, Simone C.S. Brandão
Brazilian Journal of Radiation Sciences.2022; 10(4): 1. CrossRef - Health-related quality of life after transoral robotic thyroidectomy in papillary thyroid carcinoma
Chang Myeon Song, Hyang Sook Bang, Hyung Gu Kim, Hae Jin Park, Kyung Tae
Surgery.2021; 170(1): 99. CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef
- Quality of life of patients with thyroid cancer in Colombia

- Clinical Study
- Associations of Perirenal Fat Thickness with Renal and Systemic Calcified Atherosclerosis
- Bo Kyung Koo, Julie O. Denenberg, C. Michael Wright, Michael H. Criqui, Matthew A. Allison
- Endocrinol Metab. 2020;35(1):122-131. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.122
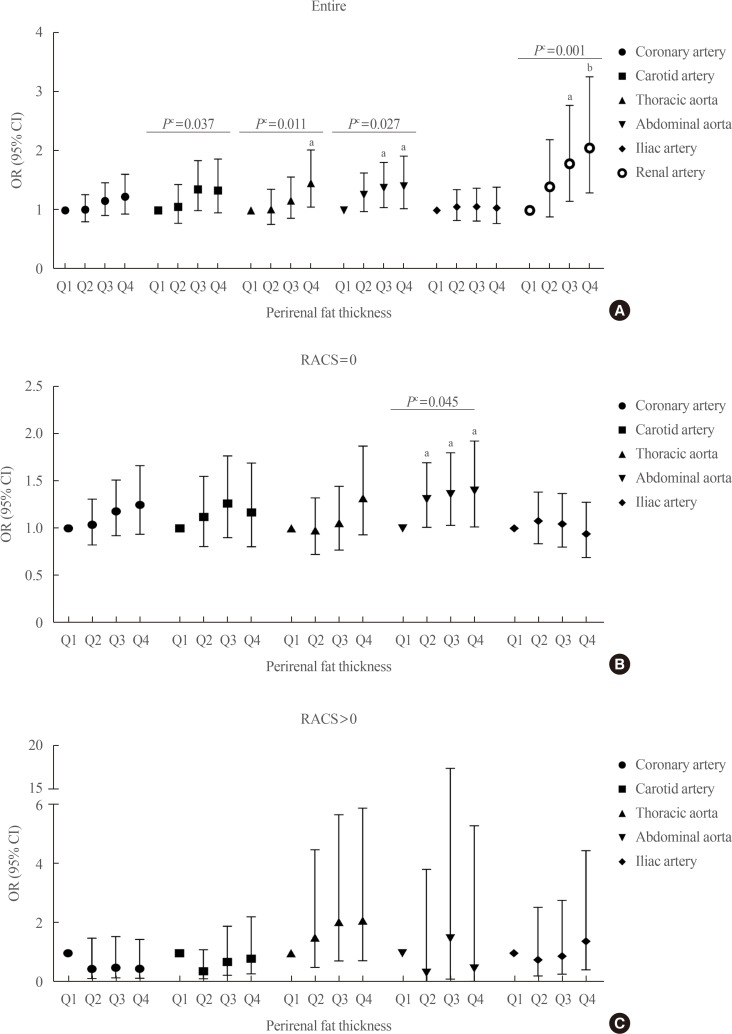
- 6,075 View
- 103 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background We investigated associations between perirenal fat thickness and atherosclerotic calcification in six different vascular beds.
Methods Using a community-based cohort (
n =3,919), perirenal fat thickness was estimated from computed tomography scans. It was classified as Q1 (the lowest quartile) to Q4 (the highest quartile) in each sex. Calcification in the carotid arteries, coronary arteries, thoracic aorta, abdominal aorta, iliac arteries, and renal arteries was evaluated.Results Perirenal fat thickness was associated with older age (
P <0.01) and a higher prevalence of obesity, hypertension, and dyslipidemia (P <0.01 for all). Perirenal fat thickness was independently associated with renal arterial calcification even after adjustment for age, sex, body mass index, hypertension, dyslipidemia, smoking history, and family history of heart diseases in first-degree relatives (odds ratio [OR] per quartile of perirenal fat thickness, 1.25; 95% confidence interval [CI], 1.09 to 1.44). Compared to Q1, the odds of renal arterial calcification in Q4 was about two times higher (OR, 2.05; 95% CI, 1.29 to 3.25). After adjustment for renal arterial calcification and atherosclerotic risk factors, the only other vascular bed where perirenal fat thickness showed a significant association with calcification was the abdominal aorta (OR, 1.11; 95% CI, 1.00 to 1.23;P =0.045).Conclusion Perirenal fat thickness was independently associated with vascular calcification in the renal artery and abdominal aorta.
-
Citations
Citations to this article as recorded by- Impact of Liver Transplantation on Adipose Tissue Compartments and Its Association With Metabolic Sequela
Ramzi Hassouneh, Sean Flynn, Steve Shen, Michael Tseng, Anh Tuan Bui, Jay Pham, Dan Park, Scott Matherly, David Bruno, Seung Lee, Vinay Kumaran, Vaishali Patel, Mark Muthiah, Amit Sharma, Mohammad Shadab Siddiqui
Transplantation.2024; 108(1): 235. CrossRef - High perirenal fat thickness predicts a greater risk of recurrence in Chinese patients with unilateral nephrolithiasis
Haichao Huang, Shi Chen, Wenzhao Zhang, Tao Wang, Peide Bai, Jinchun Xing, Huiqiang Wang, Bin Chen
Renal Failure.2023;[Epub] CrossRef - Development and validation of a preoperative nomogram for predicting the surgical difficulty of laparoscopic colectomy for right colon cancer: a retrospective analysis
Ao Yu, Yuekai Li, Haifeng Zhang, Guanbo Hu, Yuetang Zhao, Jinghao Guo, Meng Wei, Wenbin Yu, Zhibo Yan
International Journal of Surgery.2023; 109(4): 870. CrossRef - Perirenal Adipose Tissue Is Associated With Renal Dysfunction and Abnormal Hemodynamics in Patients With HFpEF
Eva M. Boorsma, Hidemi Sorimachi, Jozine M. ter Maaten, Dirk J. van Veldhuisen, Kazunori Omote, Naoki Takahashi, Jeffrey M. Testani, Tineke P. Willems, Adriaan A. Voors, Barry A. Borlaug
JACC: Heart Failure.2023; 11(10): 1463. CrossRef - Renal Compression in Heart Failure
Eva M. Boorsma, Jozine M. ter Maaten, Adriaan A. Voors, Dirk J. van Veldhuisen
JACC: Heart Failure.2022; 10(3): 175. CrossRef - The perirenal fat thickness was independently associated with serum uric acid level in patients with type 2 diabetes mellitus
Yuxian Yang, Yan Ma, Yanan Cheng, Yuechao Xu, Yuan Fang, Jing Ke, Dong Zhao
BMC Endocrine Disorders.2022;[Epub] CrossRef - Cardiorenal Fat: A Cardiovascular Risk Factor With Implications in Chronic Kidney Disease
Luis D'Marco, María Jesús Puchades, Nayara Panizo, María Romero-Parra, Lorena Gandía, Elena Giménez-Civera, Elisa Pérez-Bernat, Miguel Gonzalez-Rico, José Luis Gorriz
Frontiers in Medicine.2021;[Epub] CrossRef - Anti-Obesity Effects of a Prunus persica and Nelumbo nucifera Mixture in Mice Fed a High-Fat Diet
Jungbin Song, Jiye Kim, Hyo Jin Park, Hocheol Kim
Nutrients.2020; 12(11): 3392. CrossRef
- Impact of Liver Transplantation on Adipose Tissue Compartments and Its Association With Metabolic Sequela


 KES
KES



 First
First Prev
Prev



