Search
- Page Path
- HOME > Search
- Thyroid
- A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
- Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang, MASTER study group
- Endocrinol Metab. 2021;36(3):574-581. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.943
- 6,297 View
- 268 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Postoperative thyroid stimulating hormone (TSH) suppression therapy is recommended for patients with intermediate- and high-risk differentiated thyroid cancer to prevent the recurrence of thyroid cancer. With the recent increase in small thyroid cancer cases, the extent of resection during surgery has generally decreased. Therefore, questions have been raised about the efficacy and long-term side effects of TSH suppression therapy in patients who have undergone a lobectomy.
Methods
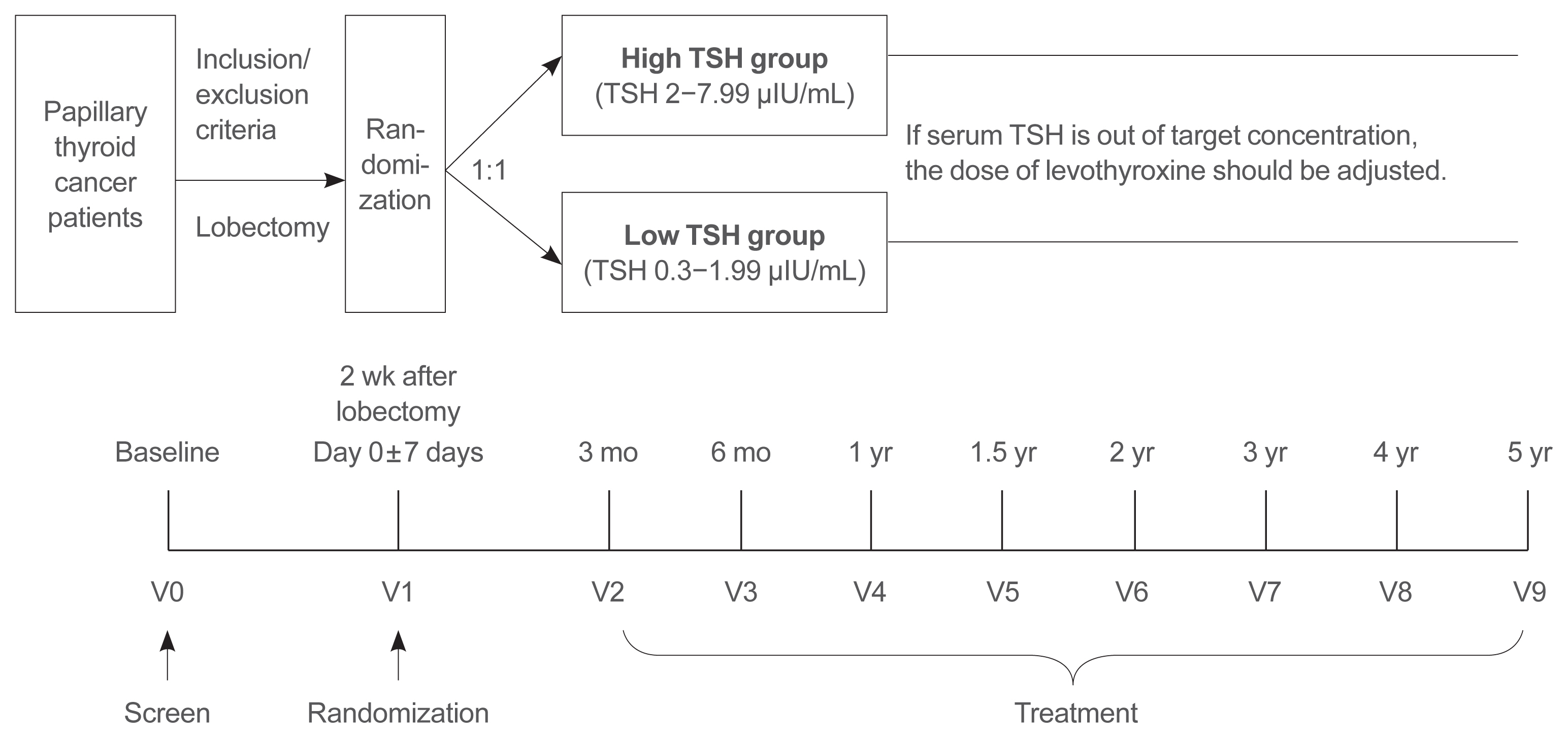
This is a multicenter, prospective, randomized, controlled clinical trial in which 2,986 patients with papillary thyroid cancer are randomized into a high-TSH group (intervention) and a low-TSH group (control) after having undergone a lobectomy. The principle of treatment includes a TSH-lowering regimen aimed at TSH levels between 0.3 and 1.99 μIU/mL in the low-TSH group. The high-TSH group targets TSH levels between 2.0 and 7.99 μIU/mL. The dose of levothyroxine will be adjusted at each visit to maintain the target TSH level. The primary outcome is recurrence-free survival, as assessed by neck ultrasound every 6 to 12 months. Secondary endpoints include disease-free survival, overall survival, success rate in reaching the TSH target range, the proportion of patients with major cardiovascular diseases or bone metabolic disease, the quality of life, and medical costs. The follow-up period is 5 years.
Conclusion
The results of this trial will contribute to establishing the optimal indication for TSH suppression therapy in low-risk papillary thyroid cancer patients by evaluating the benefit and harm of lowering TSH levels in terms of recurrence, metabolic complications, costs, and quality of life. -
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Clinical impact of coexistent chronic lymphocytic thyroiditis on central lymph node metastasis in low- to intermediate-risk papillary thyroid carcinoma: The MASTER study
Da Beom Heo, Ho-Ryun Won, Kyung Tae, Yea Eun Kang, Eonju Jeon, Yong Bae Ji, Jae Won Chang, June Young Choi, Hyeong Won Yu, Eu Jeong Ku, Eun Kyung Lee, Mijin Kim, Jun-Ho Choe, Bon Seok Koo
Surgery.2024; 175(4): 1049. CrossRef - Dynamic Changes in Treatment Response af-ter 131I in Differentiated Thyroid Cancer and Their Relationship with Recurrence Risk Stratification and TNM Staging
璐 狄
Advances in Clinical Medicine.2024; 14(03): 1083. CrossRef - ASO Author Reflections: Active Surveillance may be Possible in Patients with T1b Papillary Thyroid Carcinoma Over 55 Years of Age Without High-Risk Features on Preoperative Examinations
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2254. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis
Timothy M Ullmann, Maria Papaleontiou, Julie Ann Sosa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(2): 271. CrossRef - Age-Dependent Clinicopathological Characteristics of Patients with T1b Papillary Thyroid Carcinoma: Implications for the Possibility of Active Surveillance
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2246. CrossRef - Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Mijin Kim, Yae Eun Kang, Young Joo Park, Bon Seok Koo, Eu Jeong Ku, June Young Choi, Eun Kyung Lee, Bo Hyun Kim
Endocrine.2023; 82(1): 134. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Thyroid stimulating hormone suppression and recurrence after thyroid lobectomy for papillary thyroid carcinoma
Mi Rye Bae, Sung Hoon Nam, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
Endocrine.2022; 75(2): 487. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Clinical Study
- Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study
- Chaiho Jeong, Hye In Kwon, Hansang Baek, Hun-Sung Kim, Dong-Jun Lim, Ki-Hyun Baek, Jeonghoon Ha, Moo Il Kang
- Endocrinol Metab. 2020;35(4):925-932. Published online December 10, 2020
- DOI: https://doi.org/10.3803/EnM.2020.725

- 5,345 View
- 183 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Concomitant papillary thyroid cancer (PTC) and hyperparathyroidism (HPT) have been reported in several studies. Our study aimed to investigate the incidence of concomitant PTC in HPT patients upon preoperative diagnosis and present a clinical opinion on detecting thyroid malignancy in case of parathyroidectomy.
Methods
Patients who underwent parathyroidectomy between January 2009 and December 2019 in two medical centers were included. Of the 279 participants 154 were diagnosed as primary hyperparathyroidism (pHPT) and 125 as secondary hyperparathyroidism (sHPT). The incidence of concomitant PTC and its clinical characteristics were compared with 98 patients who underwent thyroidectomy and were diagnosed with classical PTC during the same period.
Results
Concurrent PTC was detected in 14 patients (9.1%) with pHPT and in nine patients (7.2%) with sHPT. Ten (71.4%) and seven (77.8%) PTCs were microcarcinomas in the pHPT and sHPT cases respectively. In the pHPT patients, vitamin D was lower in the pHPT+PTC group (13.0±3.7 ng/mL) than in the pHPT-only group (18.5±10.4 ng/mL; P=0.01). Vitamin D levels were also lower in the sHPT+PTC group (12.3±5.6 ng/mL) than in the sHPT-only group (18.0±10.2 ng/mL; P=0.12). In the concomitant PTC group, lymph node ratio was higher than in the classical PTC group (P=0.00).
Conclusion
A high prevalence of concomitant PTC was seen in patients with pHPT and sHPT. Those concomitant PTCs were mostly microcarcinomas and had more aggressive features, suggesting that efforts should be made to detect concomitant malignancies in the preoperative parathyroidectomy evaluation. -
Citations
Citations to this article as recorded by- The unexpected effect of parathyroid adenoma on inflammation
Ahmet Tarik Harmantepe, Belma Kocer, Zulfu Bayhan, Emre Gonullu, Ugur Can Dulger
Updates in Surgery.2024; 76(2): 589. CrossRef - Evaluation of Nodular Goiter and Papillary Thyroid Cancer Coincidence in Patients with Primary Hyperparathyroidism
Mustafa ÇALIŞKAN, Hasret CENGİZ, Taner DEMİRCİ
Düzce Tıp Fakültesi Dergisi.2023; 25(2): 200. CrossRef - Papillary thyroid carcinoma coexisting with benign thyroid and parathyroid pathology: clinical and pathomorphological features
A. Dinets, M. Gorobeiko, V. Hoperia, A. Lovin, S. Tarasenko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2023; 19(4): 274. CrossRef - The Nexus of Hyperparathyroidism and Thyroid Carcinoma: Insights into Pathogenesis and Diagnostic Challenges—A Narrative Review
Gregorio Scerrino, Nunzia Cinzia Paladino, Giuseppina Orlando, Giuseppe Salamone, Pierina Richiusa, Stefano Radellini, Giuseppina Melfa, Giuseppa Graceffa
Journal of Clinical Medicine.2023; 13(1): 147. CrossRef - Is preoperative parathyroid localization necessary for tertiary hyperparathyroidism?
Rongzhi Wang, Peter Abraham, Brenessa Lindeman, Herbert Chen, Jessica Fazendin
The American Journal of Surgery.2022; 224(3): 918. CrossRef - Papillary thyroid carcinoma prevalence and its predictors in patients with primary hyperparathyroidism
Elif Tutku DURMUŞ, Ayşegül ATMACA, Mehmet KEFELİ, Ramis ÇOLAK, Buğra DURMUŞ, Cafer POLAT
Journal of Health Sciences and Medicine.2022; 5(5): 1499. CrossRef - Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (Endocrinol Metab 2020;35:925-32, Chaiho Jeong et al.)
Chaiho Jeong, Jeonghoon Ha, Moo Il Kang
Endocrinology and Metabolism.2021; 36(1): 205. CrossRef - Association of Hyperparathyroidism and Papillary Thyroid Cancer: A Multicenter Retrospective Study (Endocrinol Metab 2020;35:925-32, Chaiho Jeong et al.)
Burcu Candemir, Coşkun Meriç
Endocrinology and Metabolism.2021; 36(1): 203. CrossRef
- The unexpected effect of parathyroid adenoma on inflammation

- Clinical Study
- Quality of Life in Patients with Papillary Thyroid Microcarcinoma According to Treatment: Total Thyroidectomy with or without Radioactive Iodine Ablation
- Jonghwa Ahn, Min Ji Jeon, Eyun Song, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
- Endocrinol Metab. 2020;35(1):115-121. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.115
- 5,486 View
- 110 Download
- 8 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Recently, there has been some controversy regarding the role of radioactive iodine (RAI) ablation in the treatment of low-risk differentiated thyroid carcinoma (DTC), especially papillary thyroid microcarcinoma (PTMC). This study aimed to compare quality of life (QoL) parameters between patients with PTMC who underwent total thyroidectomy (TT) alone and those who underwent TT with RAI ablation.
Methods In this cross-sectional study, patients with PTMC who underwent TT with/without RAI remnant ablation were prospectively enrolled between June 2016 and October 2017. All patients completed three questionnaires: the 12-item short-form health survey (SF-12), thyroid cancer-specific quality of life (THYCA-QoL) questionnaire, and fear of progression (FoP) questionnaire.
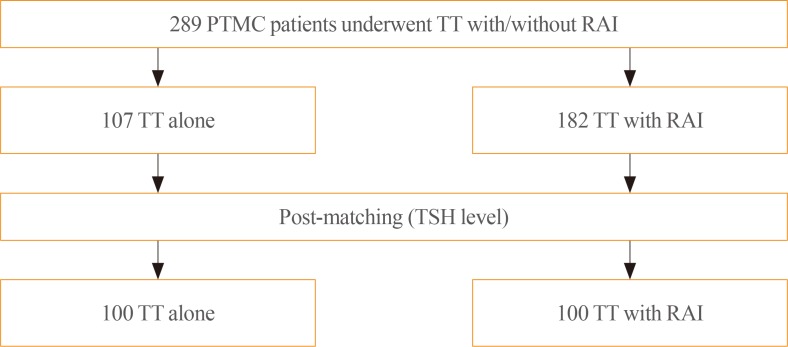
Results The TT and TT with RAI groups comprised 107 and 182 patients, respectively. The TT with RAI group had significantly lower serum thyrotropin (TSH) levels than the TT group. However, after matching for TSH levels between the groups (
n =100 in both groups), there were no significant differences in baseline characteristics. According to the SF-12, the score for general health was significantly lower in the TT with RAI group than in the TT group (P =0.047). The THYCA-QoL also showed a significant difference in the “felt chilly” score between groups (P =0.023). No significant differences in FoP scores were observed between the groups.Conclusion Patients with PTMC who underwent TT with RAI ablation experienced more health-related problems than those managed with TT alone. These findings support the idea that RAI ablation should be carefully considered in patients with low-risk DTCs.
-
Citations
Citations to this article as recorded by- Quality of life of patients with thyroid cancer in Colombia
Oscar Gómez, Alvaro Sanabria
Endocrinología, Diabetes y Nutrición.2024; 71(2): 61. CrossRef - Quality of life of patients with thyroid cancer in Colombia
Oscar Gómez, Alvaro Sanabria
Endocrinología, Diabetes y Nutrición (English ed.).2024; 71(2): 61. CrossRef - Fear of Cancer Recurrence in Differentiated Thyroid Cancer Survivors: A Systematic Review
Jacob Hampton, Ahmad Alam, Nicholas Zdenkowski, Christopher Rowe, Elizabeth Fradgley, Christine J. O'Neill
Thyroid®.2024;[Epub] CrossRef - Review: Improving quality of life in patients with differentiated thyroid cancer
Pia Pace-Asciak, Jonathon O. Russell, Ralph P. Tufano
Frontiers in Oncology.2023;[Epub] CrossRef - Health-Related Quality of Life and Thyroid Cancer-Specific Symptoms in Patients Treated for Differentiated Thyroid Cancer: A Single-Center Cross-Sectional Survey from Mainland China
Changlian Chen, Jiayan Cao, Yueyang Wang, Xuya Han, Yaju Zhang, Shumei Zhuang
Thyroid.2023; 33(4): 474. CrossRef - The "not so good" thyroid cancer: a scoping review on risk factors associated with anxiety, depression and quality of life
Kyle Alexander, Sum-Yu Christina Lee, Stelios Georgiades, Constantina Constantinou
Journal of Medicine and Life.2023; 16(3): 348. CrossRef - Comparison of health‐related quality of life and cosmetic outcome between traditional gasless trans‐axillary endoscopic thyroidectomy and modified gasless trans‐axillary endoscopic thyroidectomy for patients with papillary thyroid microcarcinoma
Deenraj Kush Dhoomun, HuiLan Cai, Ning Li, YanHuan Qiu, XingRui Li, XiaoPeng Hu, WenZhuang Shen
Cancer Medicine.2023; 12(15): 16604. CrossRef - Risk of Adverse Pregnancy Outcomes in Young Women with Thyroid Cancer: A Systematic Review and Meta-Analysis
Shinje Moon, Ka Hee Yi, Young Joo Park
Cancers.2022; 14(10): 2382. CrossRef - Health-related quality of life following FDG-PET/CT for cytological indeterminate thyroid nodules
Elizabeth J de Koster, Olga Husson, Eveline W C M van Dam, G Sophie Mijnhout, Romana T Netea-Maier, Wim J G Oyen, Marieke Snel, Lioe-Fee de Geus-Oei, Dennis Vriens, _ _
Endocrine Connections.2022;[Epub] CrossRef - Is a four-week hormone suspension necessary for thyroid remnant ablation in low and intermediate risk patients? A pilot study with quality-of-life assessment
Poliane A.L. Santos, Maria E.D.M. Flamini, Felipe A. Mourato, Fernando R.A. Lima, Joelan A.L. Santos, Fabiana F. Lima, Estelita T.B. Albuquerque, Alexandra C. De Freitas, Simone C.S. Brandão
Brazilian Journal of Radiation Sciences.2022; 10(4): 1. CrossRef - Health-related quality of life after transoral robotic thyroidectomy in papillary thyroid carcinoma
Chang Myeon Song, Hyang Sook Bang, Hyung Gu Kim, Hae Jin Park, Kyung Tae
Surgery.2021; 170(1): 99. CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef
- Quality of life of patients with thyroid cancer in Colombia

- Clinical Study
- Impact of Subtotal Parathyroidectomy on Clinical Parameters and Quality of Life in Hemodialysis Patients with Secondary Hyperparathyroidism
- Mohamed Mimi Abd Elgawwad El-kholey, Ghada El-said Ibrahim, Osama Ibrahim Elshahat, Ghada El-Kannishy
- Endocrinol Metab. 2019;34(4):367-373. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.367
- 4,429 View
- 81 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Impairment of quality of life (QOL) is a key clinical characteristic of patients with end-stage renal disease (ESRD), and can be especially severe in the presence of secondary hyperparathyroidism (SHPT). Despite the proven success of parathyroidectomy (PTX) in controlling biochemical parameters in patients with severe SHPT, evidence is lacking regarding the effects of PTX on various clinical outcomes, including QOL.
Methods Twenty ESRD patients on maintenance hemodialysis with SHPT who underwent subtotal PTX were included in an observational longitudinal study. All studied patients underwent history-taking, clinical examinations, and laboratory investigations, including a complete blood count and measurements of serum calcium, phosphorus, magnesium, parathyroid hormone (PTH), and albumin levels preoperatively and at 3 months postoperatively. QOL was assessed before surgery and at 3 months after surgery using the Kidney Disease Quality of Life 36-Item Short-Form instrument.
Results After PTX, significant decreases in serum PTH and phosphorus levels were observed, as well as a significant increase in serum magnesium levels. Significant weight gain and improvements of QOL were also detected postoperatively.
Conclusion Subtotal PTX seems to be an efficient alternative to medical management in uncontrolled cases of SHPT, as it is capable of controlling the biochemical derangements that occur in hyperparathyroidism. Furthermore, PTX had a beneficial effect on clinical outcomes, as shown by weight gain and improvements in all QOL scales.
-
Citations
Citations to this article as recorded by- Abnormalities of serum magnesium levels in dialysis patients undergoing parathyroidectomy
Chi-Yu Kuo, Chung-Hsin Tsai, Jie-Jen Lee, Shih-Ping Cheng
Updates in Surgery.2024;[Epub] CrossRef - Effect of Parathyroidectomy on Quality of Life Among Patients Undergoing Dialysis
Lin Wang, Ming-Hui Xin, Yan Ma, Yu Wang, Meng-Yuan Hu, Qiang-Qiang Liu, Jin-Bor Chen
International Journal of General Medicine.2022; Volume 15: 1185. CrossRef - Paricalcitol versus Calcitriol + Cinacalcet for the Treatment of Secondary Hyperparathyroidism in Chronic Kidney Disease in China: A Cost-Effectiveness Analysis
Zhuolin Zhang, Lele Cai, Hong Wu, Xinglu Xu, Wenqing Fang, Xuan He, Xiao Wang, Xin Li
Frontiers in Public Health.2021;[Epub] CrossRef
- Abnormalities of serum magnesium levels in dialysis patients undergoing parathyroidectomy

- Miscellaneous
- Intraoperative Parathyroid Hormone Monitoring in the Surgical Management of Sporadic Primary Hyperparathyroidism
- Zahra F. Khan, John I. Lew
- Endocrinol Metab. 2019;34(4):327-339. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.327
- 5,415 View
- 121 Download
- 22 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Intraoperative parathyroid hormone monitoring (IPM) has been shown to be a useful adjunct during parathyroidectomy to ensure operative success at many specialized medical centers worldwide. Using the Miami or “>50% intraoperative PTH drop” criterion, IPM confirms the complete excision of all hyperfunctioning parathyroid tissue before the operation is finished, and helps guide the surgeon to identify additional hyperfunctioning parathyroid glands that may necessitate further extensive neck exploration when intraoperative parathyroid hormone (PTH) levels do not drop sufficiently. The intraoperative PTH assay is also used to differentiate parathyroid from non-parathyroid tissues during operations using fine needle aspiration samples and to lateralize the side of the neck harboring the hypersecreting parathyroid through differential jugular venous sampling when preoperative localization studies are negative or equivocal. The use of IPM underscores the recognition and understanding of sporadic primary hyperparathyroidism (SPHPT) as a disease of function rather than form, where the surgeon is better equipped to treat such patients with quantitative instead of qualitative information for durable long-term operative success. There has been a significant paradigm shift over the last 2 decades from conventional to focused parathyroidectomy guided by IPM. This approach has proven to be a safe and rapid operation requiring minimal dissection performed in an ambulatory setting for the treatment of SPHPT.
-
Citations
Citations to this article as recorded by- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy
Phillip Staibano, Kevin Um, Sheila Yu, Mohit Bhandari, Michael K. Gupta, Michael Au, JEM (Ted) Young, Han Zhang
Frontiers in Surgery.2024;[Epub] CrossRef - Primary Hyperparathyroidism
Saba Kurtom, Sally E. Carty
Surgical Clinics of North America.2024;[Epub] CrossRef - Characteristics, management and outcomes of primary hyperparathyroidism from 2009 to 2021: a single centre report from South Africa
Kamal Govind, Imran M. Paruk, Ayesha A. Motala
BMC Endocrine Disorders.2024;[Epub] CrossRef - Parathyroidectomy for primary hyperparathyroidism: A retrospective analysis of localization, surgical characteristics, and treatment outcomes
Dongbin Ahn, Ji Hye Kwak, Gil Joon Lee, Jin Ho Sohn
Asian Journal of Surgery.2023; 46(2): 788. CrossRef - Magnitude of parathyroid hormone elevation in primary hyperparathyroidism: Does time of day matter?
C. Corbin Frye, Janessa Sullivan, Sai Anusha Sanka, Jingxia Liu, L. Michael Brunt, William Gillanders, Taylor C. Brown, T.K. Pandian
Surgery.2023; 173(3): 659. CrossRef - Analysis of intraoperative laboratory measurements and imaging techniques such as Tc-99 m-MIBI SPECT/CT, 18F-fluorocholine PET/CT and ultrasound in patients operated with prediagnosis of parathyroid adenoma
Nurullah Bilen, Mehmet Avni Gokalp, Latif Yilmaz, Alper Aytekin, Ilyas Baskonus
Irish Journal of Medical Science (1971 -).2023; 192(4): 1695. CrossRef - Intraoperative Parathyroid Hormone Monitoring Is of Limited Usefulness in Guiding Autotransplantation in Reoperative or Subtotal Parathyroidectomy for Primary Hyperparathyroidism
Bradley A. Richards, Robert A. Vierkant, Benzon M. Dy, Trenton R. Foster, Travis J. McKenzie, Melanie L. Lyden
The American Surgeon™.2023; 89(12): 5421. CrossRef - Does 18F-Fluorocholine PET/CT add value to positive parathyroid scintigraphy in the presurgical assessment of primary hyperparathyroidism?
Alessio Imperiale, Jacob Bani, Gianluca Bottoni, Adrien Latgé, Céline Heimburger, Ugo Catrambone, Michel Vix, Giorgio Treglia, Arnoldo Piccardo
Frontiers in Medicine.2023;[Epub] CrossRef - Intraoperative Identification of Thyroid and Parathyroid Tissues During Human Endocrine Surgery Using the MasSpec Pen
Rachel J. DeHoog, Mary E. King, Michael F. Keating, Jialing Zhang, Marta Sans, Clara L. Feider, Kyana Y. Garza, Alena Bensussan, Anna Krieger, John Q. Lin, Sunil Badal, Elizabeth Alore, Christopher Pirko, Kirtan Brahmbhatt, Wendong Yu, Raymon Grogan, Livi
JAMA Surgery.2023; 158(10): 1050. CrossRef - A Rare Case of Recurrent Parathyroid Adenomas After Initial Parathyroidectomy
Grant N Schalet, Luke Vincent, Carl Eguez, Gerardo Diaz, Mark S Shachner
Cureus.2023;[Epub] CrossRef - Surgical treatment of tertiary hyperparathyroidism: does one fit for all?
Claudio Casella, Claudio Guarneri, Manuela Campanile, Xavier Adhoute, Pier Paolo Gelera, Riccardo Morandi
Frontiers in Endocrinology.2023;[Epub] CrossRef - A >50% Intraoperative Parathyroid Hormone Decrease Into Normal Reference Range Predicts Complete Excision of Malignancy in Patients With Parathyroid Carcinoma
Valerie L. Armstrong, Tanaz M. Vaghaiwalla, Cima Saghira, Cheng-Bang Chen, Yujie Wang, Johan Anantharaj, Mehmet Ackin, John I. Lew
Journal of Surgical Research.2023;[Epub] CrossRef - Variation in parathyroid adenoma size in patients with sporadic, primary hyperparathyroidism: small gland size does not preclude single gland disease
Sophie Dream, Tina W. F. Yen, Kara Doffek, Douglas B. Evans, Tracy S. Wang
Langenbeck's Archives of Surgery.2022; 407(5): 2067. CrossRef - Role and Recent Trend of Intraoperative Parathyroid Hormone Monitoring During Parathyroidectomy in Patients With Primary Hyperparathyroidism
Dongbin Ahn, Ji Hye Kwak
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2022; 65(5): 253. CrossRef - Parathyroid Adenoma: Rare Cause of Acute Recurrent Pancreatitis
Shikha Mahajan, Alka Kumar, Vivek Aggarwal, Vikas Jain, Vipul Baweja, Ajay Ajmani, Diplomate CBNC, Fellow EBNM LNU
Annals of Pediatric Gastroenterology and Hepatology.2022; 2(3-4): 9. CrossRef - Long-term outcome of surgical techniques for sporadic primary hyperparathyroidism in a tertiary referral center in Belgium
Klaas Van Den Heede, Amélie Bonheure, Nele Brusselaers, Sam Van Slycke
Langenbeck's Archives of Surgery.2022; 407(7): 3045. CrossRef - Contribution of intraoperative parathyroid hormone monitoring to the surgical success in minimal invasive parathyroidectomy
Ismail Ethem Akgün, Mehmet Taner Ünlü, Nurcihan Aygun, Mehmet Kostek, Mehmet Uludag
Frontiers in Surgery.2022;[Epub] CrossRef - Surgery for primary hyperparathyroidism
Murilo Catafesta das Neves, Rodrigo Oliveira Santos, Monique Nakayama Ohe
Archives of Endocrinology and Metabolism.2022; 66(5): 678. CrossRef - Використання інтраопераційного моніторингу рівня паратиреоїдного гормону в мінімально інвазивній хірургії щитоподібної та паращитоподібних залоз
S.V. Chernyshov, A.V. Tymkiv, A.V. Vovkanych, I.I. Komisarenko
Endokrynologia.2022; 27(4): 311. CrossRef - Diagnostic Values of Intraoperative (1-84) Parathyroid Hormone Levels are Superior to Intact Parathyroid Hormone for Successful Parathyroidectomy in Patients With Chronic Kidney Disease
Fangyan Xu, Yaoyu Huang, Ming Zeng, Lina Zhang, Wenkai Ren, Hanyang Qian, Ying Cui, Guang Yang, Wenbin Zhou, Shui Wang, Hui Huang, Huimin Chen, Yujie Xiao, Xueyan Gao, Zhanhui Gao, Jing Wang, Cuiping Liu, Jing Zhang, Baiqiao Zhao, Anning Bian, Fan Li, Hui
Endocrine Practice.2021; 27(11): 1065. CrossRef - Delayed Calcium Normalization after Successful Parathyroidectomy in Primary Hyperparathyroidism
Iván Emilio de la Cruz Rodríguez, Elsy Sarahí García Montesinos, María Fernanda Rodríguez-Delgado, Guadalupe Vargas Ortega, Lourdes Balcázar Hernández, Victoria Mendoza Zubieta, Victor Hernández Avendaño, Baldomero González Virla, Micha�l R. Laurent
Case Reports in Endocrinology.2021; 2021: 1. CrossRef - Parathyroid Surgery
Aditya S. Shirali, Uriel Clemente-Gutierrez, Nancy D. Perrier
Neuroimaging Clinics of North America.2021; 31(3): 397. CrossRef - Focused parathyroidectomy without intraoperative parathyroid hormone measurement in primary hyperparathyroidism: Still a valid approach?
Shelby Holt
Surgery.2021; 170(6): 1860. CrossRef - Response to the Comment on “Risk Factors of Redo Surgery After Unilateral Focused Parathyroidectomy – Conclusions From a Comprehensive Nationwide Database of 13,247 Interventions Over 6 Years”
Robert Caiazzo, Camille Marciniak, Francois Pattou
Annals of Surgery.2021; 274(6): e861. CrossRef
- Intraoperative parathyroid hormone monitoring in parathyroidectomy for hyperparathyroidism: a protocol for a network meta-analysis of diagnostic test accuracy

- Surgical Findings of Benign Thyroid Nodule, Not Decreased After Thyroxine Suppression Therapy.
- Dong Won Byun, Myung Hi Yoo, Kyo Il Suh, Hae Kyung Lee, Guk Bae Kim
- J Korean Endocr Soc. 1996;11(4):401-408. Published online November 7, 2019
- 1,038 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Fine needle aspiration and biopsy(FNAB) has known the most accurate test(about 90%) in the preoperative evaluation of patients with a thyroid nodule. The false negative findings of thyroid cancer by FNAB are mainly due to the aspiration of cystic fluid in cystic degeneration of thyroid cancer and the ipossibility of differentiation between follicular adenoma and carcinoma by aspiration or FNAB because of the failure to evaluate the capsule invasion or angioinvasion of the tumor. Actually more than 80% of the nodules are found as benign nodules in aspiration or FNAB and the findings of follieular lesions are found about half of the samples tested, so limiting the cancer incidence in surgically resected samples up to 50% of the surgical resection. Sa reasonable guidelines to manage the benign nodules on aspiration or FNAB are needed which can select the maligna~nt nodules with false negative findings on aspiration or FNAB. We tried to evaluate whether the thyroxine suppression therapy can increase the malignancy rates on thyroidectomy, Methods: We treated the benign thyroid nodules in FNAB with thyroxine for 1 year and cornpared the nodule volume change before and after treatment (every 6 month) with ultrasonogram. We performed thyroidectomy on 1~7 thyroid nodules wbich showed less than 50% decrease of nodule volume after 1 year of thyroxine suppression therapy. Results: The results were as follows. 1) Of all 17 patients, surgical resection revealed malignant thyroid nodule(Group I) in 10 cases (58.82%, papillary cancer. 6 cases, follicular cancer: 4 cases) and benign thyroid nodule(Group II) in 7 cases(41.18%, follicular adenoma: 4 cases, adenomatous goiter: 3 cases). 2) Between group I and II, there was no significant differences in serum T, T and TSH levels before and after thyroxine suppression therapy. Also, there were no significant difference in TSH suppression % between group I and group II(5.60+5.39%, 14.64+11.48%, respectively). 3) Thyroid nodule volume decrease percent before and after thyroxi~ne therapy showed no significant difference between group I and group II (124.80+54.18% vs 159.42+79.82%, p>0.05). Conclusion: Our data suggested that the benign thyroid nodules on aspiration or FNAB which were not suppressed in volume after thyroixine therapy revealed more than 50% incidence of malignancy on surgical resection, so these nodules were highly reeommended to surgical exploration.

- Thyroid
- Graves' Disease: Can It Be Cured?
- Wilmar M. Wiersinga
- Endocrinol Metab. 2019;34(1):29-38. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.29
- 16,157 View
- 511 Download
- 44 Web of Science
- 46 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Whether or not Graves' hyperthyroidism can be really cured, depends on the definition of “cure.” If eradication of thyroid hormone excess suffices for the label “cure,” then all patients can be cured because total thyroidectomy or high doses of 131I will abolish hyperthyroidism albeit at the expense of creating another disease (hypothyroidism) requiring lifelong medication with levothyroxine. I would not call this a “cure,” which I would like to define as a state with stable thyroid stimulating hormone (TSH), free thyroxine, and triiodothyronine serum concentrations in the normal range in the absence of any thyroid medication. Surgery and radioiodine are unlikely to result in so-defined cures, as their preferable aim as stated in guidelines is to cause permanent hypothyroidism. Discontinuation of antithyroid drugs is followed by 50% recurrences within 4 years; before starting therapy the risk of recurrences can be estimated with the Graves' Recurrent Events After Therapy (GREAT) score. At 20-year follow-up about 62% had developed recurrent hyperthyroidism, 8% had subclinical hypothyroidism, and 3% overt hypothyroidism related to TSH receptor blocking antibodies and thyroid peroxidase antibodies. Only 27% was in remission, and might be considered cured. If the definition of “cure” would also include the disappearance of thyroid antibodies in serum, the proportion of cured patients would become even lower.
-
Citations
Citations to this article as recorded by- Multifunctional nanoparticle-mediated combining therapy for human diseases
Xiaotong Li, Xiuju Peng, Makhloufi Zoulikha, George Frimpong Boafo, Kosheli Thapa Magar, Yanmin Ju, Wei He
Signal Transduction and Targeted Therapy.2024;[Epub] CrossRef - Prenatal double-hit with aluminium and cadmium mediate testicular atrophy and hypothalamic hypoplasia: the role of oxido-nitrergic stress and endocrine perturbations
Emmanuel Okhue, Helen Ejiro Kadiri, Patrick Chukwuyenum Ichipi-Ifukor, Benneth Ben-Azu, Samuel Ogheneovo Asagba, Fidelis Ifeakachuku Achuba, John Chukwuma Oyem
BioMetals.2024; 37(2): 477. CrossRef - Surgical outcome after thyroidectomy due to Graves’ disease and Lugol iodine treatment: a retrospective register-based cohort study
Fredric Hedberg, Henrik Falhammar, Jan Calissendorff, Robert Bränström
Endocrine.2024;[Epub] CrossRef - Graves disease is associated with increased risk of clinical Alzheimer’s disease: evidence from the Medicare system
Arseniy Pavlovich Yashkin, Stanislav Kolpakov, Svetlana Ukraintseva, Anatoliy Yashin, Igor Akushevich
Clinical Diabetes and Endocrinology.2024;[Epub] CrossRef - A 2023 International Survey of Clinical Practice Patterns in the Management of Graves Disease: A Decade of Change
Danilo Villagelin, David S Cooper, Henry B Burch
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Predictors of Prolonged Euthyroidism After Radioactive Iodine Treatment for Graves’ Disease: A Pilot Study
Jin-Ying Lu, Kuan-Hua Chen, Shyang-Rong Shih, Fang-Yu Wen, Wan-Chen Wu, Ting-Chu Chen, Fu-Chang Hu
Endocrine Practice.2023; 29(2): 89. CrossRef - Case of Graves’ disease recovery
Andrey Valerievich Ushakov
Journal of Clinical and Translational Endocrinology: Case Reports.2023; 27: 100139. CrossRef - Outcomes of Radioactive Iodine Versus Surgery for the Treatment of Graves’ Disease: a Systematic Review and Meta-analysis
Mohamed AbdAlla Salman, Mohamed Moustafa Assal, Ahmed Salman, Mohammed Elsherbiney
Indian Journal of Surgery.2023;[Epub] CrossRef - Association between high mobility group box-1 circulation level and Graves' ophthalmopathy
Mohammad Robikhul Ikhsan, Nyoman Kertia, Supanji Supanji, Bambang Udji djoko Rianto, Dhite Bayu Nugroho
F1000Research.2023; 12: 767. CrossRef - New-onset and relapsed Graves’ disease following COVID-19 vaccination: a comprehensive review of reported cases
Kan Chen, Yiyang Gao, Jing Li
European Journal of Medical Research.2023;[Epub] CrossRef - REVIEW OF SARS-CORONAVIRUS-2 REPERCUSSIONS ON THYROID GLAND IN THE CONTEXT OF HYPERTHYROIDISM
SHUBHAM SINGH, MONIKA, RUPA MAZUMDER, AVIJIT MAZUMDER
International Journal of Applied Pharmaceutics.2023; : 17. CrossRef - Effectiveness and potential mechanism of Jiawei-Xiaoyao-San for hyperthyroidism: a systematic review
Wenxin Ma, Xiaowen Zhang, Ruotong Zhao, Yang Tang, Xiaoyun Zhu, Longkun Liu, Mingyuan Xu, Ge Wang, Peiyue Peng, Jianping Liu, Zhaolan Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Associations of serum keratin 1 with thyroid function and immunity in Graves’ disease
Chao-Wen Cheng, Wen-Fang Fang, Jiunn-Diann Lin, Appuwawadu Mestri Nipun Lakshitha de Silva
PLOS ONE.2023; 18(11): e0289345. CrossRef - Management of Graves’ hyperthyroidism: present and future
Luigi Bartalena, Eliana Piantanida, Daniela Gallo, Silvia Ippolito, Maria Laura Tanda
Expert Review of Endocrinology & Metabolism.2022; 17(2): 153. CrossRef - The Prediction Model Using Thyroid-stimulating Immunoglobulin Bioassay For Relapse of Graves’ Disease
Han-Sang Baek, Jaejun Lee, Chai-Ho Jeong, Jeongmin Lee, Jeonghoon Ha, Kwanhoon Jo, Min-Hee Kim, Jae Hyoung Cho, Moo Il Kang, Dong-Jun Lim
Journal of the Endocrine Society.2022;[Epub] CrossRef - Efficacy of Radioiodine Therapy in Patients With Primary Hyperthyroidism: An Institutional Review From Pakistan
Asim Munir Alvi, Umal Azmat, Waqas Shafiq, Abdul Hannan Ali Rasheed, Ahmed Imran Siddiqi, Sardar Khan, Sara Ashfaq, Hira Irfan , Humayun Bashir, Muhammad Abu Bakar, Kashif Asghar
Cureus.2022;[Epub] CrossRef - Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
Endocrinology and Metabolism.2022; 37(3): 524. CrossRef - Endocrine Surgery and Pediatic Surgery Partnership Reduces Complication Rate of Pediatric Thyroidectomy
Ali Sayan, Mehmet Üstün, Mehmet Mert, Cem Karaali, Gökhan Köylüoğlu
Journal of Dr Behcet Uz Children s Hospital.2022; 12(2): 164. CrossRef - Thyroid-related adverse events induced by immune checkpoint inhibitors
Alexandra Chera, Andreea Lucia Stancu, Octavian Bucur
Frontiers in Endocrinology.2022;[Epub] CrossRef - A case of Hashimoto's thyroiditis following Graves' disease
Ibtissem Oueslati, Salma Salhi, Meriem Yazidi, Fatma Chaker, Melika Chihaoui
Clinical Case Reports.2022;[Epub] CrossRef - Changes in the T and B lymphocyte subset profiles upon treatment of patients with Graves’ disease with radioactive iodine
A. A. Savchenko, M. A. Dudina, S. A. Dogadin, A. G. Borisov, I. V. Kudryavtsev, D. V. Fomina, V. D. Belenyuk
Medical Immunology (Russia).2022; 24(5): 1007. CrossRef - A survey of the young person’s experience of Graves’ disease and its management
Laura Claire Lane, Judith Rankin, Tim Cheetham
Clinical Endocrinology.2021; 94(2): 330. CrossRef - Serum T3 Level and Duration of Minimum Maintenance Dose Therapy Predict Relapse in Methimazole-Treated Graves Disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Rajata Rajatanavin, Thep Himathongkam
Journal of the Endocrine Society.2021;[Epub] CrossRef - Dosimetry-guided radioiodine therapy of hyperthyroidism: long-term experience and implications for guidelines
Thomas Leitha, Manuela Schartel, Ingrid Hurtl, Rudolf Bednar, Franz König, Karl Mayrhofer, Flavia Pietschmann
Nuclear Medicine Communications.2021; 42(2): 150. CrossRef - Practice patterns and outcomes in the management of Thai patients with Graves’ disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanathayanoroj, Nampetch Lekpittaya, Worawit Kittipoom, Tawee Anuntakulnatee, Somboon Vongterapak, Siriwan Butadej, Soontaree Nakas
Thyroid Research.2021;[Epub] CrossRef - Un case report letterario di tireotossicosi in La coscienza di Zeno di Italo Svevo
Francesco Trimarchi, Luigi Bartalena, Stefano Arieti, Roberto Toni
L'Endocrinologo.2021; 22(2): 149. CrossRef - Medical treatment of thyrotoxicosis
Lorenzo SCAPPATICCIO, Giuseppe BELLASTELLA, Maria I. MAIORINO, Luca GIOVANELLA, Katherine ESPOSITO
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2021;[Epub] CrossRef - Hiccups as a Rare Presentation of Thyrotoxicosis Triaged by an Epidural Steroid Injection
Omar Al-Radideh, Iyad Farouji, Theodore DaCosta, Hossam Abed, Nicholas Baranestky
Cureus.2021;[Epub] CrossRef - Long-term antithyroid drug therapy
David S. Cooper
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 510. CrossRef - The Continuum of Thyroid Disorders Related to Immune Checkpoint Inhibitors: Still Many Pending Queries
Maria V. Deligiorgi, Sofia Sagredou, Lampros Vakkas, Dimitrios T. Trafalis
Cancers.2021; 13(21): 5277. CrossRef - Recurrence of Graves’ Disease: What Genetics of HLA and PTPN22 Can Tell Us
Daniela Vejrazkova, Josef Vcelak, Eliska Vaclavikova, Marketa Vankova, Katerina Zajickova, Jana Vrbikova, Michaela Duskova, Petra Pacesova, Zdenek Novak, Bela Bendlova
Frontiers in Endocrinology.2021;[Epub] CrossRef - Most Patients with Graves’ Disease Treated with Antithyroid Drugs Eventually Require Additional Therapies
Mary H. Samuels
Clinical Thyroidology.2020; 32(1): 9. CrossRef - Patterns of Use, Efficacy, and Safety of Treatment Options for Patients with Graves' Disease: A Nationwide Population-Based Study
Juan P. Brito, Stephanie Payne, Naykky Singh Ospina, Rene Rodriguez-Gutierrez, Spyridoula Maraka, Lindsey R. Sangaralingham, Nicole M. Iñiguez-Ariza, Victor M. Montori, Marius N. Stan
Thyroid.2020; 30(3): 357. CrossRef - Long-Term Treatment of Hyperthyroidism with Antithyroid Drugs: 35 Years of Personal Clinical Experience
Fereidoun Azizi
Thyroid.2020; 30(10): 1451. CrossRef - Predictive factors for early hypothyroidism following the radioactive iodine therapy in Graves’ disease patients
Rui-Ting Hu, De-Shan Liu, Bin Li
BMC Endocrine Disorders.2020;[Epub] CrossRef - The Concept of Cure in Thyroid Diseases
Fereidoun Azizi
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Der Biomarker TSH bei Schilddrüsenautonomien
K. Passek, N. Zulauf, E. Wanke, G. M. Oremek
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie.2020; 70(4): 177. CrossRef - Management of Graves’ Hyperthyroidism: More Than a Century of Progression
Hengameh Abdi, Atieh Amouzegar
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Corticosteroid Pulse Therapy for Graves' Ophthalmopathy Reduces the Relapse Rate of Graves' Hyperthyroidism
Rosario Le Moli, Pasqualino Malandrino, Marco Russo, Fabrizio Lo Giudice, Francesco Frasca, Antonino Belfiore, Riccardo Vigneri
Frontiers in Endocrinology.2020;[Epub] CrossRef - Prediction of Relapse After Antithyroid Drugs Withdrawal: A Narrative Review
Pei-Wen Wang
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Radioiodine-131 therapy (RIT) in benign thyroid diseases: Personalized prescription based on objectives with optional use of pharmacological modulators
J. Clerc
Médecine Nucléaire.2020; 44(4): 250. CrossRef - Predicting the Risk of Graves Disease Relapse: Commentary on “Thyroid Peroxidase Antibody Positivity is Associated with Relapse-Free Survival Following Antithyroid Drug Treatment for Graves Disease”
D. Gallo, M.L. Tanda, E. Piantanida
Endocrine Practice.2020; 26(9): 1039. CrossRef - Integrating Five Feature Types Extracted From Ultrasonograms to Improve the Prediction of Thyroid Papillary Carcinoma
Renxiang Zhu, Zhongyu Wang, Yifan Zhang, Bingxin Yu, Mingran Qi, Xin Feng, Chenjun Wu, Yuxuan Cui, Lan Huang, Fan Li, Fengfeng Zhou
IEEE Access.2019; 7: 101820. CrossRef - Serum TSH Receptor Antibodies Fall Gradually and Only Rarely Switch Functional Activity in Treated Graves’ Disease
Mary H. Samuels
Clinical Thyroidology.2019; 31(8): 330. CrossRef - Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinology and Metabolism.2019; 34(3): 268. CrossRef - A transgenic mouse that spontaneously develops pathogenic TSH receptor antibodies will facilitate study of antigen-specific immunotherapy for human Graves’ disease
Sandra M. McLachlan, Basil Rapoport
Endocrine.2019; 66(2): 137. CrossRef
- Multifunctional nanoparticle-mediated combining therapy for human diseases

- Thyroid
- Can Robotic Thyroidectomy Be Performed Safely in Thyroid Carcinoma Patients?
- Young Jun Chai, Kyu Eun Lee, Yeo-Kyu Youn
- Endocrinol Metab. 2014;29(3):226-232. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.226
- 4,328 View
- 40 Download
- 20 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Since the adoption of the Da Vinci robotic system for remote access thyroid surgery, robotic thyroidectomy (RT) has become a popular surgical option for patients who want to avoid neck scars. Surgeons in South Korea pioneered this surgical technique and have reported successful outcomes. Although many studies have reported that RT is a feasible and safe therapeutic alternative, concerns over the surgical and oncological safety of RT remain. This article reviews the advantages and disadvantages of RT and compares the surgical safety and oncological completeness of RT with conventional open thyroidectomy.
-
Citations
Citations to this article as recorded by- Comparative surgical outcomes of transoral endoscopic and robotic thyroidectomy for thyroid carcinoma: a propensity score-matched analysis
Min Jung Lee, Moon Young Oh, Jung-Man Lee, Jiyu Sun, Young Jun Chai
Surgical Endoscopy.2023; 37(2): 1132. CrossRef - Comparison of surgical completeness in patients operated on conventional open total thyroidectomy (OT) or trans-axillary robot-assisted total thyroidectomy (RATT) by a single axillary approach
Valeria Matteucci, Lorenzo Fregoli, Piermarco Papini, Leonardo Rossi, Antonio Matrone, Mario Miccoli, Rossella Elisei, Gabriele Materazzi
Updates in Surgery.2023; 75(5): 1267. CrossRef - Bilateral axillo-breast approach robotic thyroidectomy (BABA-RT) versus transoral robotic thyroidectomy (TORT): a systematic review and meta-analysis
Ebraheem Albazee, Ahmed Abdelaziz, Reham Alabdulhadi, Danah Ibrahim Alkandari, Aysha Abduljabbar, Sara Sulaiman, Mohammad Alnifise, Jasem Ameen, Houda Magzoub, Karim Alomar, Shaima Ali Maghdi, Ahmed Abu-Zaid
Updates in Surgery.2023; 75(5): 1277. CrossRef - Transoral endoscopic thyroidectomy vestibular approach vs. transoral robotic thyroidectomy: systematic review and meta-analysis
Moon Young Oh, Young Jun Chai, Hyeong Won Yu, Su-Jin Kim, June Young Choi, Kyu Eun Lee
Updates in Surgery.2023; 75(7): 1773. CrossRef - Transoral Endoscopic Thyroidectomy by Vestibular Approach with Central Lymph Node Dissection for Thyroid Microcarcinoma
Hau Xuan Nguyen, Hien Xuan Nguyen, Hung Van Nguyen, Long Thanh Nguyen, Thao Thi Phuong Nguyen, Quang Van Le
Journal of Laparoendoscopic & Advanced Surgical Techniques.2021; 31(4): 410. CrossRef - Robotik in der Kopf-Hals-Chirurgie
P. J. Schuler, F. Boehm, L. R. Schild, J. Greve, T. K. Hoffmann
HNO.2021; 69(2): 131. CrossRef - Current Advances in Robotics for Head and Neck Surgery—A Systematic Review
Felix Boehm, Rene Graesslin, Marie-Nicole Theodoraki, Leon Schild, Jens Greve, Thomas K. Hoffmann, Patrick J. Schuler
Cancers.2021; 13(6): 1398. CrossRef - Institutional experience of 200 consecutive papillary thyroid carcinoma patients in transoral robotic thyroidectomy surgeries
Dawon Park, Hoon Yub Kim, Hong Kyu Kim, Ji‐Young You, Gianlorenzo Dionigi, Jonathon O. Russell, Ralph P. Tufano
Head & Neck.2020; 42(8): 2106. CrossRef - Transoral Robotic Thyroidectomy for Papillary Thyroid Carcinoma: Perioperative Outcomes of 100 Consecutive Patients
Hong Kyu Kim, Young Jun Chai, Gianlorenzo Dionigi, Eren Berber, Ralph P. Tufano, Hoon Yub Kim
World Journal of Surgery.2019; 43(4): 1038. CrossRef - Endoscopic interventions on the thyroid gland, as operations in a potential workspace
M. Sh. Mamistvalov, I. A. Kurganov, S. I. Emelyanov, D. Yu. Bogdanov, D. V. Lukyanchenko
Endoskopicheskaya khirurgiya.2019; 25(5): 54. CrossRef - Robotic Thyroidectomy Decreases Postoperative Pain Compared With Conventional Thyroidectomy
Min Kyoung Kim, Hyun Kang, Geun Joo Choi, Kyung Ho Kang
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2019; 29(4): 255. CrossRef - Comparative analysis of 2 robotic thyroidectomy procedures: Transoral versus bilateral axillo‐breast approach
Young Jun Chai, Hoon Yub Kim, Hong Kyu Kim, Sang Ho Jun, Gianlorenzo Dionigi, Angkoon Anuwong, Jeremy D. Richmon, Ralph P. Tufano
Head & Neck.2018; 40(5): 886. CrossRef - Robotic-assisted modified radical neck dissection using a bilateral axillo-breast approach (robotic BABA MRND) for papillary thyroid carcinoma with lateral lymph node metastasis
Hyeong Won Yu, Young Jun Chai, Su-jin Kim, June Young Choi, Kyu Eun Lee
Surgical Endoscopy.2018; 32(5): 2322. CrossRef - Recent advances in robot‐assisted head and neck surgery
Daniel T. Friedrich, Marc O. Scheithauer, Jens Greve, Thomas K. Hoffmann, Patrick J. Schuler
The International Journal of Medical Robotics and Computer Assisted Surgery.2017;[Epub] CrossRef - Surgical safety and oncological completeness of robotic thyroidectomy for thyroid carcinoma larger than 2 cm
Young Jun Chai, Hyunsuk Suh, Jung-Woo Woo, Hyeong Won Yu, Ra-Yeong Song, Hyungju Kwon, Kyu Eun Lee
Surgical Endoscopy.2017; 31(3): 1235. CrossRef - Experience of transaxillary endoscopic thyroid surgery
V. K. Lyadov, M. V. Neklyudova, D. R. Pashayeva
Khirurgiya. Zhurnal im. N.I. Pirogova.2016; (11): 4. CrossRef - Robotergestützte Chirurgie im Kopf-Hals-Bereich
T. K. Hoffmann, D. T. Friedrich, P. J. Schuler
HNO.2016; 64(9): 658. CrossRef - Management of Thyroid Nodules
Ashokkumar Sithamparapillai
Journal of Otolaryngology-ENT Research.2016;[Epub] CrossRef - Ethical issues in robotic-assisted transaxillary thyroidectomy
Peter Angelos
International Journal of Endocrine Oncology.2015; 2(2): 129. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Comparative surgical outcomes of transoral endoscopic and robotic thyroidectomy for thyroid carcinoma: a propensity score-matched analysis

- Thyroid
- Graves' Disease that Developed Shortly after Surgery for Thyroid Cancer
- Hea Min Yu, Soon Hyun Park, Jae Min Lee, Kang Seo Park
- Endocrinol Metab. 2013;28(3):226-230. Published online September 13, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.3.226
- 3,153 View
- 31 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Graves' disease is an autoimmune disorder that may present with various clinical manifestations of hyperthyroidism. Patients with Graves' disease have a greater number of thyroid nodules and a higher incidence of thyroid cancer compared with patients with normal thyroid activity. However, cases in which patients are diagnosed with recurrence of Graves' disease shortly after partial thyroidectomy for thyroid cancer are very rare. Here we report a case of hyperthyroid Graves' disease that occurred after partial thyroidectomy for papillary thyroid cancer. In this case, the patient developed hyperthyroidism 9 months after right hemithyroidectomy, and antithyroglobulin autoantibody and thyroid stimulating hormone receptor stimulating autoantibody were positive. Therefore, we diagnosed Graves' disease on the basis of the laboratory test results and thyroid ultrasonography findings. The patient was treated with and maintained on antithyroid drugs. The mechanism of the recurrence of Graves' disease in this patient is still unclear. The mechanism may have been the improper response of the immune system after partial thyroidectomy. To precisely determine the mechanisms in Graves' disease after partial thyroidectomy, further studies based on a greater number of cases are needed.
-
Citations
Citations to this article as recorded by- Graves’ disease diagnosed in remnant thyroid after lobectomy for thyroid cancer
Meihua Jin, Ahreum Jang, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Byeong-Cheol Ahn
PLOS ONE.2022; 17(3): e0265332. CrossRef - Graves’ thyrotoxicosis soon after hemithyroidectomy for low-risk papillary thyroid carcinoma
Ahmad Housin, Michael Tamilia
BMJ Case Reports.2022; 15(5): e250149. CrossRef - Effects of energy-based ablation on thyroid function in treating benign thyroid nodules: a systematic review and meta-analysis
Yuan Fei, Yuxuan Qiu, Dong Huang, Zhichao Xing, Zhe Li, Anping Su, Jingqiang Zhu
International Journal of Hyperthermia.2020; 37(1): 1090. CrossRef - Total Thyroidectomy for Thyroid Cancer Followed by Thyroid Storm due to Thyrotropin Receptor Antibody Stimulation of Metastatic Thyroid Tissue
Lars Folkestad, Frans Brandt, Thomas Brix, Marianne Vogsen, Lars Bastholt, Peter Grupe, Jeanette Krogh Petersen, Laszlo Hegedüs
European Thyroid Journal.2017; 6(5): 276. CrossRef - Percutaneous microwave ablation of thyroid nodules: effects on thyroid function and antibodies
Kristina Heck, Christian Happel, Frank Grünwald, Huedayi Korkusuz
International Journal of Hyperthermia.2015; 31(5): 560. CrossRef - Development of Thyroid-Associated Ophthalmopathy in Patients Who Underwent Total Thyroidectomy
Sun Young Jang, Ka Hyun Lee, Jong Rok Oh, Bo Yeon Kim, Jin Sook Yoon
Yonsei Medical Journal.2015; 56(5): 1389. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Graves’ disease diagnosed in remnant thyroid after lobectomy for thyroid cancer

- Predictive Factors for Incidental Contralateral Carcinoma in Patients with Unilateral Micropapillary Thyroid Carcinoma.
- Jung Eun Huh, Sang Soo Kim, Ji Hyun Kang, Bo Gwang Choi, Byung Joo Lee, Jin Choon Lee, Yun Kyung Jeon, Bo Hyun Kim, Soo Geun Wang, Yong Ki Kim, In Joo Kim
- Endocrinol Metab. 2012;27(3):194-199. Published online September 19, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.3.194
- 54,228 View
- 21 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Whether thyroid lobectomy alone is a sufficient treatment for papillary thyroid microcarcinoma (PTMC) remains controversial. The aim of this study is to evaluate the predictive factors for incidental contralateral carcinoma in patients confirmed of unilateral PTMC preoperatively. METHODS: Between January 2007 and December 2009, 393 patients underwent thyroid surgery for unifocal and unilateral PTMC preoperatively at Pusan National University Hospital. A total thyroidectomy with central neck dissection was routinely performed for these patients during this study period. RESULTS: Among the 393 cases in the cohort, 77 patients (19.6%) had incidental PTMC in the contralateral lobe. In patients with incidental contralateral carcinoma, there was higher prevalence in extrathyroid extension, occult ipsilateral carcinoma, pathologic Hashimoto's thyroiditis, and central lymph node metastasis compared to those without contralateral carcinoma. The mean tumor size also increased in patients with contralateral carcinoma. Multivariate logistic regression showed that extrathyroid extension (P = 0.049), occult ipsilateral carcinoma (P < 0.001), pathologic Hashimoto's thyroiditis (P = 0.038), and central lymph node metastasis (P = 0.002) were predictive factors for incidental contralateral carcinoma. CONCLUSION: In conclusion, multifocality in the ipsilateral lobe, central lymph node metastasis, extrathyroid extension, and Hashimoto's thyroiditis is associated with the presence of contralateral carcinoma. Thus, if these factors are found by preoperative and/or postoperative evaluation, total thyroidectomy or completion thyroidectomy is necessary for the treatment of PTMC. -
Citations
Citations to this article as recorded by- Extent of surgery did not affect recurrence during 7‐years follow‐up in papillary thyroid cancer sized 1‐4 cm: Preliminary results
Min Joo Kim, Myung‐Chul Lee, Guk Haeng Lee, Hoon Sung Choi, Sun Wook Cho, Su‐jin Kim, Kyu Eun Lee, Young Joo Park, Do Joon Park
Clinical Endocrinology.2017; 87(1): 80. CrossRef
- Extent of surgery did not affect recurrence during 7‐years follow‐up in papillary thyroid cancer sized 1‐4 cm: Preliminary results

- Association of the Parathyroid Adenoma Volume and the Biochemical Parameters in Primary Hyperparathyroidism.
- Yul Hwang-Bo, Jung Hee Kim, Jee Hyun An, Eun Shil Hong, Jung Hun Ohn, Eun Ky Kim, Ah Reum Khang, Sun Wook Cho, Do Joon Park, Kyong Soo Park, Seong Yeon Kim, Bo Youn Cho, Chan Soo Shin
- Endocrinol Metab. 2011;26(1):62-66. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.62
- 1,866 View
- 22 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The objective of this study is to demonstrate the relationship between the volume of a parathyroid adenoma and the preoperative biochemical parameters in patients undergoing surgery for primary hyperparathyroidism. METHODS: The medical records of 68 patients who underwent a parathyroidectomy for a single parathyroid adenoma were retrospectively reviewed. The volume of the adenoma was estimated using its measured size and a mathematical formula. The correlation between the volume of the parathyroid adenoma and the preoperative laboratory data was assessed. RESULTS: There were no correlations between the estimated volume of the adenoma and the serum calcium, alkaline phosphatase and parathyroid hormone levels. However, the volume of the adenoma was associated with the preoperative level of serum phosphorus. After excluding 5 adenomas with cystic degeneration, a positive correlation was noted between the adenoma volume and the preoperative levels of alkaline phosphatase and parathyroid hormone. CONCLUSION: The preoperative serum levels of calcium, alkaline phosphatase and parathyroid hormone are of limited use to predict the volume of the parathyroid adenoma in patients with a single parathyroid adenoma. We suggest that the absence of a correlation between the volume of the adenoma and the biochemical parameters can be attributed to the cystic degeneration of the adenomas. -
Citations
Citations to this article as recorded by- Differentiating pathologic parathyroid glands from thyroid nodules on neck ultrasound: the PARATH-US cross-sectional study
Dolly Yazgi, Carine Richa, Sylvie Salenave, Peter Kamenicky, Amel Bourouina, Lorraine Clavier, Margot Dupeux, Jean-François Papon, Jacques Young, Philippe Chanson, Luigi Maione
The Lancet Regional Health - Europe.2023; 35: 100751. CrossRef - Primer hiperparatiroidide Tc99m-MIBI sintigrafi sonuçlarının biyokimyasal ve histopatolojik bulgular ile ilişkisi
Seda TURGUT, Ezgi Başak ERDOĞAN
OSMANGAZİ JOURNAL OF MEDICINE.2020;[Epub] CrossRef - Letter: Association of the Parathyroid Adenoma Volume and the Biochemical Parameters in Primary Hyperparathyroidism (Endocrinol Metab 26:62-66, 2011, Yul Hwang-Bo et al.)
Dong Jin Chung
Endocrinology and Metabolism.2011; 26(2): 185. CrossRef
- Differentiating pathologic parathyroid glands from thyroid nodules on neck ultrasound: the PARATH-US cross-sectional study

- A Case of Painful Hashimoto's Thyroiditis Successfully Treated with Total Thyroidectomy.
- Hee Kyung Kim, Hong Joon Shin, Ho Cheol Kang
- J Korean Endocr Soc. 2008;23(6):438-443. Published online December 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.6.438
- 1,938 View
- 22 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Painful Hashimoto's thyroiditis (HT) is a subtype of HT characterized by thyroid pain with overt elevation in inflammatory markers and thyroid autoantibodies. The differential diagnosis of painful HT with subacute granulomatous thyroiditis is often difficult because initial clinical findings are very similar. Findings that favor the diagnosis of painful HT include preceding history of chronic goiter or autoimmune thyroid diseases, a high titer of thyroid autoantibodies, and repeated painful attacks even with chronic glucocorticoid therapy. Surgery is often needed to relieve the thyroid pain.
-
Citations
Citations to this article as recorded by- Painful immunoglobulin G4-related thyroiditis treated by total thyroidectomy
Ihn Suk Lee, Jung Uee Lee, Kwan-Ju Lee, Yi Sun Jang, Jong Min Lee, Hye Soo Kim
The Korean Journal of Internal Medicine.2016; 31(2): 399. CrossRef - A Case of Painful Hashimoto Thyroiditis that Mimicked Subacute Thyroiditis
Hye Mi Seo, Miyeon Kim, Jaeseok Bae, Jo-Heon Kim, Jeong Won Lee, Sang Ah Lee, Gwanpyo Koh, Dae Ho Lee
Chonnam Medical Journal.2012; 48(1): 69. CrossRef
- Painful immunoglobulin G4-related thyroiditis treated by total thyroidectomy

- A Case of Graves' Disease Associated with Systemic Sclerosis.
- Yune Jeong Lee, Mee Kyoung Kim, Dong Jun Lim, Ki Hoon Hur, Ki Hyun Baek, Moo Il Kang, Chul Soo Cho, Kwang Woo Lee, Gyeong Sin Park
- J Korean Endocr Soc. 2007;22(3):220-224. Published online June 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.3.220
- 2,007 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Systemic sclerosis is associated with a broad spectrum of autoimmune thyroid diseases. The association between systemic scleroderma and hypothyroidism is well established. However, there have been very few reports concerning the association between hyperthyroidism and systemic scleroderma. We experienced a patient with Graves' disease who presented with muscle weakness and the patient was finally diagnosed with systemic sclerosis via pathological examination of the muscle. We describe here a rare case of systemic sclerosis associated with Graves` disease.
-
Citations
Citations to this article as recorded by- Systemic Sclerosis Associated with Non-small Cell Lung Cancer and Papillary Thyroid Cancer: Case Report and Literature Review
Ho Jae Kim, Jung Joo Kim, Hee Jung Park, Yong Tai Kim
The Korean Journal of Medicine.2017; 92(3): 316. CrossRef
- Systemic Sclerosis Associated with Non-small Cell Lung Cancer and Papillary Thyroid Cancer: Case Report and Literature Review

- Duration of Preparation for Postoperative Radioiodine Administration in Differentiated Thyroid Carcinoma.
- Hyeon Kyu Kim, Min Ho Cho, Choel Young Park, Seong Jin Lee, Gi Weon Oh, In Kyung Jeong, Eun Gyung Hong, Sung Hee Ihm, Doo Man Kim, Jae Myung Yu, Moon Gi Choi, Hyung Joon Yoo, Sung Woo Park, Jin Hwan Kim, Young Soo Rho
- J Korean Endocr Soc. 2005;20(5):460-466. Published online October 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.5.460
- 1,862 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Radioiodine treatment is effective for the removal of remnant thyroid tissues after thyroidectomy in patients with differentiated thyroid carcinoma. To induce the elevation of serum TSH level which facilitates the uptake of radioiodine into remnants, a 4 to 6 week interval between thyroidectomy and radioiodine administration has been established. During the period of preparation, most patients have experienced overt symptoms of hypothyroidism which have led to the development of alternative strategies. Some reports have suggested that the interval could be reduced to about 3 weeks with less symptoms. We reevaluated the adequate time needed for the elevation of serum TSH level above 30microU/mL after thyroidectomy. METHODS: Forty five patients who had undergone total thyroidectomy for differentiated thyroid carcinoma were investigated. Serum TSH and free T4 levels were measured one or more times within 3 weeks after operation(total 97 blood samples). Eighty nine blood samples were obtained within 15 days. RESULTS: In 41 patients (91.1%) serum TSH levels increased to 30 microU/mL until 15 days after operation. Until postoperative 21 days, serum TSH levels in all the other patients reached 30microU/mL. In linear equation, the daily increment of serum TSH levels was 2.62microU/mL for the first 8 days after operation and 5.34micorU/mL for the next 7 days. The half-life of serum free T4 levels showed marked individual variations. CONCLUSION: Measurement of serum TSH level at about 15 days after total thyroidectomy for differentiated thyroid carcinoma may be useful in determining the time of radioiodine administration.

- Completion Thyroidectomy in Patient with Differentiated Thyroid Cancer Who Initially Underwent Ipsilateral Operation.
- Eun Sook Kim, Jung Min Koh, Won Bae Kim, Suck Joon Hong, Young Kee Shong
- J Korean Endocr Soc. 2002;17(5):657-663. Published online October 1, 2002
- 1,050 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
In some instances, thyroid cancer may be diagnosed only after resection of a putative or suspected benign nodule. In these cases a complete thyroidectomy is usually recommended to prevent recurrence. We analyzed the frequency of malignancy in the contralateral lobe after a complete thyroidectomy, and assessed the factors that may predict the presence of a malignancy, which might necessitate a complete thyroidectomy. METHODS: Between 1995 and 2001, 65 patients, who initially underwent a lobectomy and isthmectomy, but were finally diagnosed with differentiated thyroid carcinoma, underwent complete thyroidectomies. Their mean age was 39.8 +/- 12.4 years, ranging, 14 to 71 years. After initial surgery, 45 proved to have follicular carcinomas, 18 papillary carcinomas, 1 medullary and 1 insular carcinoma. The mean tumor size was 4.0 +/- 1.8 cm, ranging from 0.3 to 8.5 cm. After a complete thyroidectomy, the presence of a tumor the at contralateral lobe was assessed according to clinical parameters and the pathological findings in the ipsilateral lobe. RESULTS: The first surgeries revealed tumor multifocality in 27 cases, perithyroidal tumor extension in 4 and lymph node metastasis in 1. On completion of the thyroidectomy, 22 of the 65 patients had a malignancy in the contralateral lobe. Age, sex, size or the pathological primary tumor type, were not associated with the presence of additional tumors at the contralateral lobe. Tumor multifocality at the first surgery was the only significant variable to predict the presence of a tumor in the contralateral lobe. CONCLUSION: When thyroid cancer is diagnosed after ipsilateral surgery, the only predictive factor for the presence of a contralateral tumor was multifocality. We believe that a complete thyroidectomy is mandatory in these cases.


 KES
KES

 First
First Prev
Prev



