Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
- Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
- Endocrinol Metab. 2023;38(1):10-24. Published online February 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.102
- 3,745 View
- 262 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - The Korean National Health Information Database (NHID) contains big data combining information obtained from the National Health Insurance Service and health examinations. Data are provided in the form of a cohort, and the NHID can be used to conduct longitudinal studies and research on rare diseases. Moreover, data on the cause and date of death are provided by Statistics Korea. Research and publications based on the NHID have increased explosively in the field of endocrine disorders. However, because the data were not collected for research purposes, studies using the NHID have limitations, particularly the need for the operational definition of diseases. In this review, we describe the characteristics of the Korean NHID, operational definitions of endocrine diseases used for research, and an overview of recent studies in endocrinology using the Korean NHID.
-
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Diabetes severity and the risk of depression: A nationwide population-based study
Yunjung Cho, Bongsung Kim, Hyuk-Sang Kwon, Kyungdo Han, Mee Kyoung Kim
Journal of Affective Disorders.2024; 351: 694. CrossRef - Information Bias Might Exaggerate Lung Cancer Risk of Patients With Rheumatoid Arthritis
Nobuyuki Horita, Kaoru Takase-Minegishi
Journal of Thoracic Oncology.2024; 19(2): 348. CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
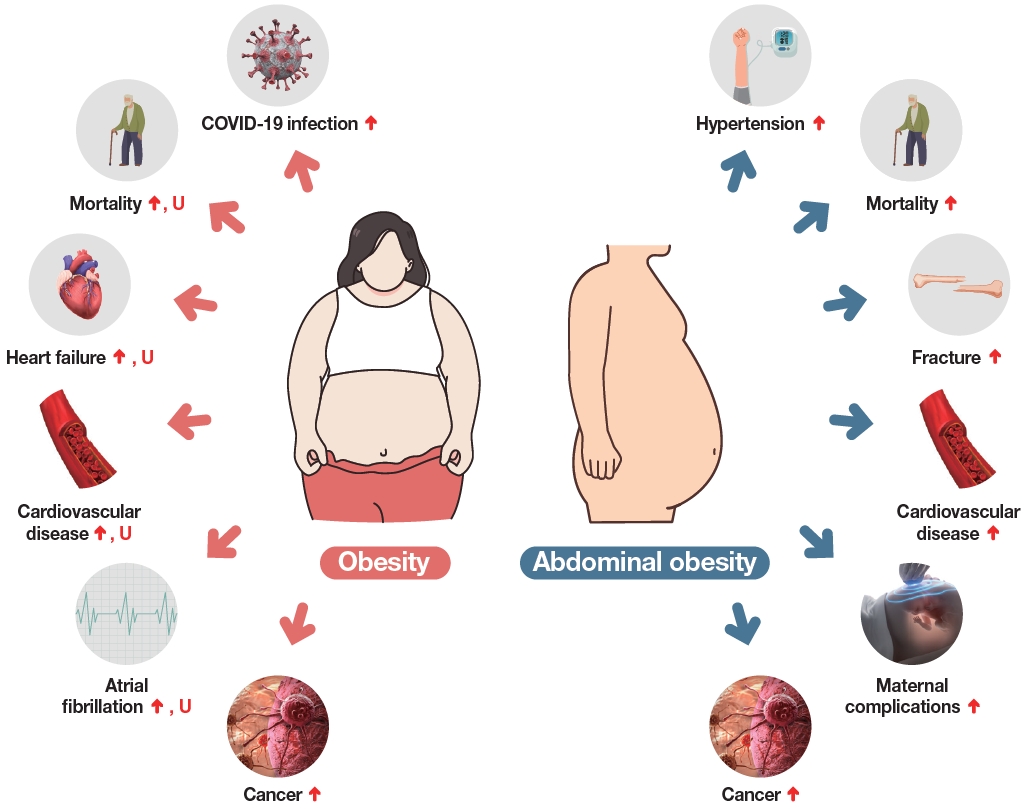
Respiratory Research.2023;[Epub] CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
Endocrinology and Metabolism.2023; 38(6): 690. CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study

- Thyroid
- Immunoglobulin G4-Related Thyroid Disease: A Single-Center Experience and Literature Review
- Meihua Jin, Bictdeun Kim, Ahreum Jang, Min Ji Jeon, Young Jun Choi, Yu-Mi Lee, Dong Eun Song, Won Gu Kim
- Endocrinol Metab. 2022;37(2):312-322. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1318
- 4,023 View
- 180 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
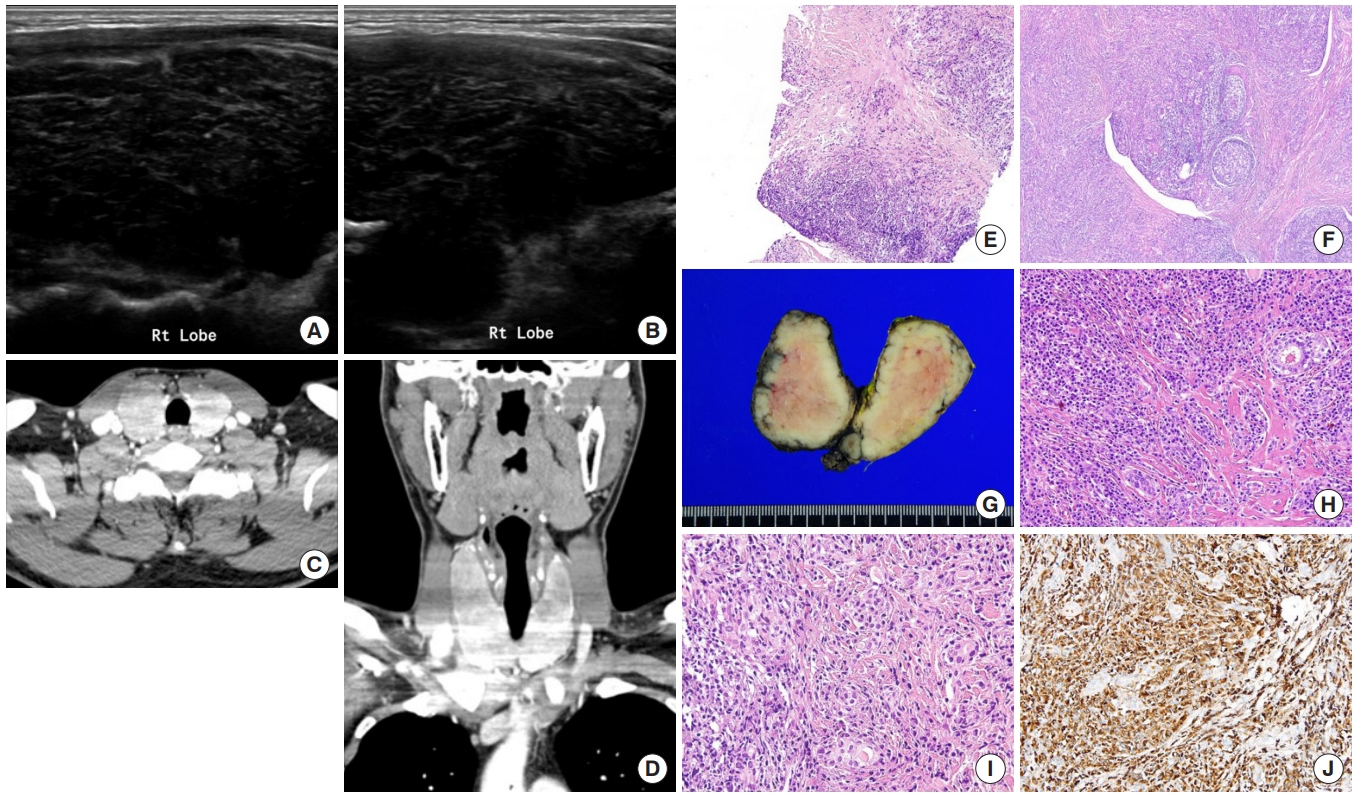
Immunoglobulin G4 (IgG4)-related disease is an entity that can involve the thyroid gland. The spectrum of IgG4-related thyroid disease (IgG4-RTD) includes Hashimoto thyroiditis (HT) and its fibrotic variant, Riedel thyroiditis, as well as Graves’ disease. The early diagnosis of IgG4-RTD is important because it is a medically treatable disease, and a delay in the diagnosis might result in unnecessary surgery. We present a case series of IgG4-RTD with a review of the literature.
Methods
We retrospectively reviewed the clinical presentation and the radiological and pathological findings of patients diagnosed with IgG4-RTD between 2017 and 2021 at a tertiary medical center in Korea. We also conducted a literature review of IgG4-RTD.
Results
Five patients were diagnosed with IgG4-RTD during the study period. The patients’ age ranged from 31 to 76 years, and three patients were men. Most patients visited the clinic for a neck mass, and hypoechogenic nodular lesions were observed on neck ultrasonography. Three patients had IgG4 HT, and two patients had IgG4 Riedel thyroiditis. All patients developed hypothyroidism that necessitated L-thyroxine replacement. The diagnosis of IgG4-RTD was confirmed after a pathological examination of the surgical specimen in the first two cases. However, the early diagnosis was possible after a core needle biopsy in three clinically suspected patients.
Conclusion
The diagnosis of IgG4-RTD requires clinical suspicion combined with serology and histological analyses using IgG4 immunostaining. The early diagnosis of IgG4-RTD is difficult; thus, biopsy with IgG4 immunostaining and serum IgG4 measurements will help diagnose patients suspected of having IgG4-RTD. -
Citations
Citations to this article as recorded by- Are sonographic characteristics of Hashimoto’s thyroiditis related with immunologic parameters? A cross-sectional study
K. Kenarlı, A. B. Bahçecioğlu, Ö. B. Aksu, S. Güllü
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Reshaping the Concept of Riedel’s Thyroiditis into the Larger Frame of IgG4-Related Disease (Spectrum of IgG4-Related Thyroid Disease)
Mara Carsote, Claudiu Nistor
Biomedicines.2023; 11(6): 1691. CrossRef
- Are sonographic characteristics of Hashimoto’s thyroiditis related with immunologic parameters? A cross-sectional study

- Thyroid
- Evaluation of Iodine Status among Korean Patients with Papillary Thyroid Cancer Using Dietary and Urinary Iodine
- Ji Yeon Choi, Joon-Hyop Lee, YoonJu Song
- Endocrinol Metab. 2021;36(3):607-618. Published online June 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1005
- 3,903 View
- 122 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
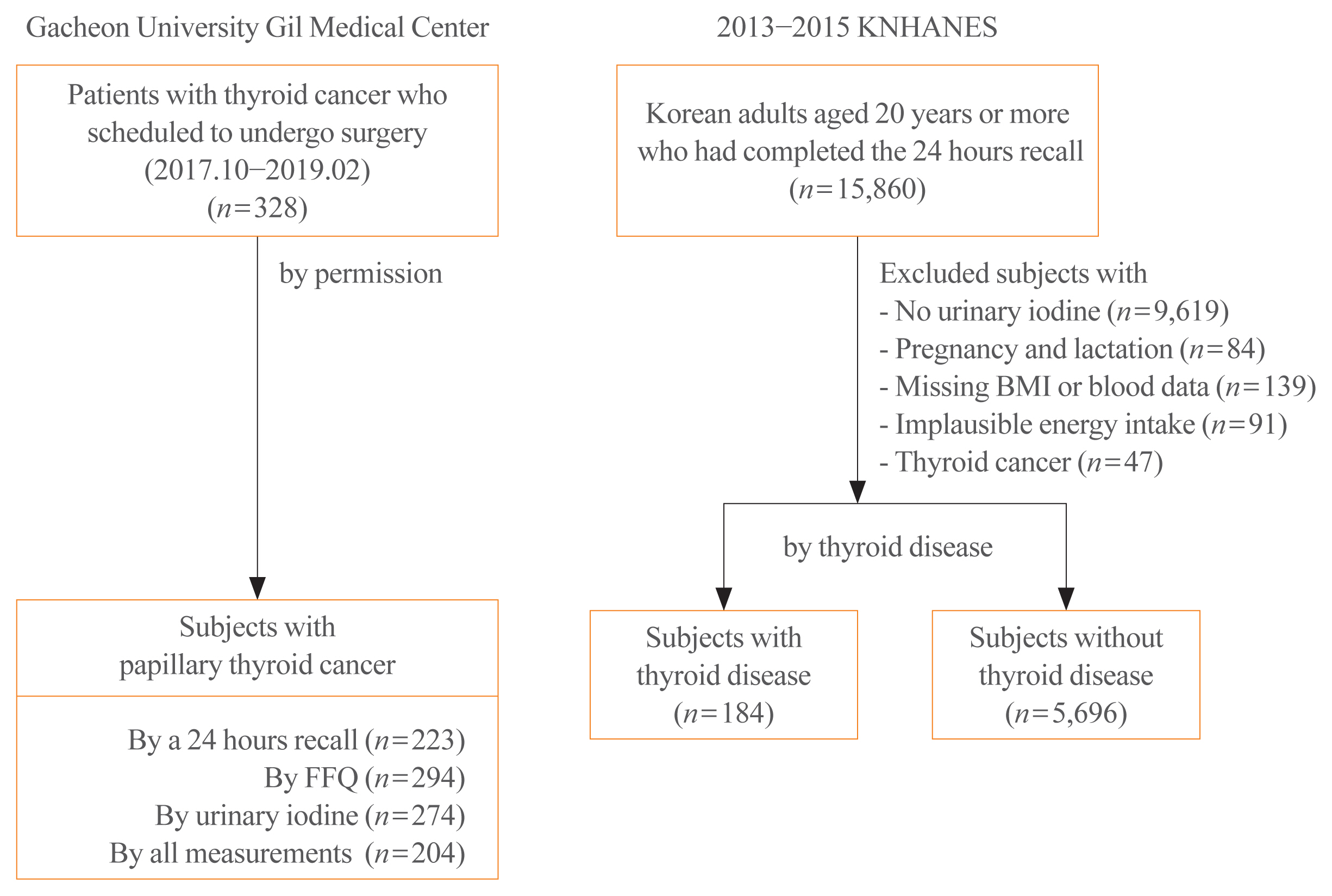
Concerns have been raised regarding thyroid disorders caused by excessive iodine in Koreans, who have iodine-rich diets. This study evaluated iodine status using dietary iodine intake and urinary iodine in papillary thyroid cancer (PTC) patients.
Methods
Dietary data of PTC patients were assessed using a 24-hour recall and food frequency questionnaire (FFQ), and urinary iodine concentrations (UICs) were also obtained. To compare the iodine status of PTC patients, Korean adults with or without thyroid disease from the Korea National Health and Nutrition Examination Survey, which had 24-hour recall data and urinary iodine measurements, were analyzed.
Results
The median daily iodine intake by 24-hour recall was 341.7 μg/day in PTC patients, similar to the levels of other Korean adults. Based on UICs, the prevalence of excessive iodine was 54.4% in PTC patients, which was similar to the prevalence among subjects with thyroid disease (55.4%) but slightly higher than that in subjects without thyroid disease (47.7%). Based on dietary iodine by 24-hour recall, the prevalence of excessive iodine intake was 7.2%, which was higher than that among subjects with (4.4%) or without (3.9%) thyroid disease. The dietary iodine intake based on 24-hour recall was closely correlated with the UIC (r=0.4826) in PTC patients, but dietary iodine by FFQ was not significantly correlated with either 24-hour recall or UIC-based dietary iodine.
Conclusion
Excessive iodine intake was more common in PTC patients than in subjects without thyroid disease. Further longitudinal research is necessary to elucidate the role of dietary iodine in PTC. -
Citations
Citations to this article as recorded by- Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma
Hengqiang Zhao, Jin Hu, Le Cui, Yiping Gong, Tao Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effect of iodine restriction on short-term changes in thyroid function in patients with subclinical hypothyroidism
Obin Kwon, Dong Yeob Shin, Eun Jig Lee
Journal of Nutrition and Health.2022; 55(2): 250. CrossRef - Iodine nutrition and papillary thyroid cancer
Xueqi Zhang, Fan Zhang, Qiuxian Li, Chuyao Feng, Weiping Teng
Frontiers in Nutrition.2022;[Epub] CrossRef
- Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma

- Thyroid
- Best Achievements in Clinical Thyroidology in 2020
- Eun Kyung Lee, Young Joo Park
- Endocrinol Metab. 2021;36(1):30-35. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2021.103
- 4,445 View
- 246 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - This review highlights the most interesting research in thyroidology conducted in 2020. The publications of interest discussed below dealt with the following topics: thyroid dysfunction, risk of thyroid cancer, molecular diagnostics and new therapeutics for thyroid cancer, and thyroid disease in the coronavirus disease 2019 pandemic era.
-
Citations
Citations to this article as recorded by- Compensation for iodine deficiency conditions with drugs based on duckweed substrate
M. Kh. Sadulaev, M. I. Usmanova, T. T. Tataev, A. M. Inderbiev, A. S.-A. Zhamalullayla, A. Salamova
BIO Web of Conferences.2023; 76: 03002. CrossRef - Use of long non-coding RNAs for the molecular diagnosis of papillary thyroid cancer
Daham Kim, Juyeon Yu, Jiwon Kim, Yoon-a Hwang, Jin Kyong Kim, Cheol Ryong Ku, Jung Hyun Yoon, Jin Young Kwak, Kee-Hyun Nam, Eun Jig Lee
Frontiers in Oncology.2022;[Epub] CrossRef - Ultrasound-Guided Fine-Needle Aspiration with or without Negative Pressure for Different Types of Thyroid Nodules
Qi Zhou, Wenjun Wu, Fang Wang, Xiaohua Gong, Xiaojun Chen
International Journal of General Medicine.2021; Volume 14: 5475. CrossRef
- Compensation for iodine deficiency conditions with drugs based on duckweed substrate

- Thyroid
- Update on the Management of Thyroid Disease during Pregnancy
- Chang Hoon Yim
- Endocrinol Metab. 2016;31(3):386-391. Published online August 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.386
- 4,101 View
- 74 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Thyroid dysfunction during pregnancy can result in serious complications for both the mother and infant; however, these complications can be prevented by optimal treatment of maternal overt thyroid dysfunction. Although several studies have demonstrated that maternal subclinical hypothyroidism is associated with obstetric complications and neurocognitive impairments in offspring, there is limited evidence that levothyroxine treatment can improve these complications. Therefore, most professional societies do not recommend universal screening for thyroid dysfunction during pregnancy, and instead recommend a case-finding approach in which only high-risk women are tested. However, recent studies have estimated that targeted thyroid function testing misses approximately 30% to 55% of hypothyroidism cases in pregnant women, and some associations and researchers have recommended universal screening of pregnant women to facilitate the early detection and treatment of overt hypothyroidism. This review summarizes recent data on thyroid function test changes, thyroid functional disorder management, and thyroid screening during pregnancy.
-
Citations
Citations to this article as recorded by- The Effect of Inflammatory Markers in the Hemogram Parameters of Pregnant Women with Thyroid Disease on Obstetric and Neonatal Outcomes
Funda DEMİREL, Ünal TURKAY
Düzce Tıp Fakültesi Dergisi.2023; 25(3): 231. CrossRef - Enfermedades tiroideas y embarazo en una unidad de cuidados intensivos. Experiencia 2014-2019
J.G. Vázquez-Rodríguez, A.C. Andrade-Rodríguez
Clínica e Investigación en Ginecología y Obstetricia.2021; 48(3): 100662. CrossRef - Decreased Expression of Ileal Thyroid Hormone Transporters in a Hypothyroid Patient: A Case Report
Chae Won Chung, Eun Young Mo, Gyung Seo Jung, Yoo Hyung Kim, Sun Wook Cho, Do Joon Park, Jeong Mo Bae, Young Joo Park
Frontiers in Endocrinology.2021;[Epub] CrossRef - Tiroidectomía en paciente embarazada con enfermedad de Graves sin respuesta a tratamiento médico: reporte de caso
Elly Morros González, Leonardo Javier Rojas Melo, Viviana Cruz Ramírez, Angélica Imitola
Universitas Médica.2020;[Epub] CrossRef - Thyroid disorders in subfertility and early pregnancy
Samantha Anandappa, Mamta Joshi, Lukasz Polanski, Paul V. Carroll
Therapeutic Advances in Endocrinology and Metabolism.2020; 11: 204201882094585. CrossRef - Addressing thyroid dysfunction in pregnancy
Teodora Onciu, Remus Şipoş
Medic.ro.2020; 3(135): 48. CrossRef - Antenatal/early postnatal hypothyroidism increases the contribution of Rho-kinase to contractile responses of mesenteric and skeletal muscle arteries in adult rats
Dina K. Gaynullina, Svetlana I. Sofronova, Anastasia A. Shvetsova, Ekaterina K. Selivanova, Anna P. Sharova, Andrey A. Martyanov, Olga S. Tarasova
Pediatric Research.2018; 84(1): 112. CrossRef - Voluntary exercise training restores anticontractile effect of NO in coronary arteries of adult rats with antenatal/early postnatal hypothyroidism
D.K. Gaynullina, A.A. Borzykh, S.I. Sofronova, E.K. Selivanova, A.A. Shvetsova, A.A. Martyanov, I.V. Kuzmin, O.S. Tarasova
Nitric Oxide.2018; 74: 10. CrossRef - Impact of positive thyroid autoimmunity on pregnant women with subclinical hypothyroidism
Cristina López-Tinoco, Amparo Rodríguez-Mengual, Almudena Lara-Barea, Julia Barcala, Laura Larrán, Ana Saez-Benito, Manuel Aguilar-Diosdado
Endocrinología, Diabetes y Nutrición (English ed.).2018; 65(3): 150. CrossRef - Impacto de la autoinmunidad antitiroidea positiva en gestantes con hipotiroidismo subclínico
Cristina López-Tinoco, Amparo Rodríguez-Mengual, Almudena Lara-Barea, Julia Barcala, Laura Larrán, Ana Saez-Benito, Manuel Aguilar-Diosdado
Endocrinología, Diabetes y Nutrición.2018; 65(3): 150. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Maternal hypothyroidism: An overview of current experimental models
Mahboubeh Ghanbari, Asghar Ghasemi
Life Sciences.2017; 187: 1. CrossRef
- The Effect of Inflammatory Markers in the Hemogram Parameters of Pregnant Women with Thyroid Disease on Obstetric and Neonatal Outcomes

- Thyroid
- Cost-of-Illness Trends Associated with Thyroid Disease in Korea
- Kyung-Rae Hyun, Sungwook Kang, Sunmi Lee
- Endocrinol Metab. 2014;29(3):257-269. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.257
- 3,712 View
- 30 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study is to analyze the scale of and trends associated with the cost-of-illness of thyroid disease in Korea at 2-year intervals during the last 10 years for which data are available.
Methods Cost-of-illness was estimated in terms of direct and indirect costs. Direct costs include direct medical costs due to hospitalization, outpatient and pharmacy sectors, transportation, and care-giver costs. Indirect costs include future income loss due to premature death and loss of productivity as a result of absence from work.
Results The cost-of-illness of thyroid disease in Korea was estimated at 224.2 billion won in 2002, 303.4 billion won in 2004, 400.3 billion won in 2006, 570.4 billion won in 2008, and 762.2 billion won in 2010. For example, the cost-of-illness of thyroid disease in 2010 was 3.4 times greater compared to 2002. The direct cost of the total cost-of-illness was 69.7%, which accounted for the highest proportion of costs. Cost-of-illness for individuals between the ages of 30 and 50 accounted for the greatest share of costs.
Conclusion The cost-of-illness of thyroid disease was relatively large in economically active age groups, and demonstrated a very rapid growth rate compared to other major diseases in Korea. Therefore, we suggest nationwide recognition of the importance of prevention and management of thyroid disease and prioritization of the management of thyroid disease among current and future health promotion policies in Korea.
-
Citations
Citations to this article as recorded by- Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Who loses more? Identifying the relationship between hospitalization and income loss: prediction of hospitalization duration and differences of gender and employment status
Minsung Sohn, Daseul Moon, Patricia O’Campo, Carles Muntaner, Haejoo Chung
BMC Public Health.2022;[Epub] CrossRef - The importance and effectiveness of nutritional counselling in patients with autoimmune thyroid diseases in Poland
Ewa Czubek, Klaudia Alcer, Mirjana Varjacic, Piotr Romaniuk
Cost Effectiveness and Resource Allocation.2022;[Epub] CrossRef - Socioeconomic Costs of Dementia Based on Utilization of Health Care and Long-Term-Care Services: A Retrospective Cohort Study
Eun-Jeong Han, JungSuk Lee, Eunhee Cho, Hyejin Kim
International Journal of Environmental Research and Public Health.2021; 18(2): 376. CrossRef - Triennial Report ofEndocrinology and Metabolism, 2015 to 2017
Eun-Jung Rhee, Hey Yeon Jang, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 195. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Cost-of-Illness Trend of Thyroid Gland Disease in Korea
Jae Hoon Chung
Endocrinology and Metabolism.2014; 29(3): 248. CrossRef - Letter: Insufficient Experience in Thyroid Fine-Needle Aspiration Leads to Misdiagnosis of Thyroid Cancer (Endocrinol Metab2014;29:293-9, Jung Il Son et al.)
Hyon-Seung Yi, Sihoon Lee
Endocrinology and Metabolism.2014; 29(4): 590. CrossRef
- Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019

- Thyroid
- Effects of Increased Iodine Intake on Thyroid Disorders
- Xin Sun, Zhongyan Shan, Weiping Teng
- Endocrinol Metab. 2014;29(3):240-247. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.240
- 10,735 View
- 135 Download
- 72 Web of Science
- 74 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Iodine is a micronutrient essential for the production of thyroid hormones. Iodine deficiency is the most common cause of preventable mental impairment worldwide. Universal salt iodization (USI) has been introduced in many countries as a cost-effective and sustainable way to eliminate iodine deficiency disorders for more than 25 years. Currently, the relationship between USI and iodine excess has attracted more attention. Iodine excess can lead to hypothyroidism and autoimmune thyroiditis, especially for susceptible populations with recurring thyroid disease, the elderly, fetuses, and neonates. Nationwide USI was introduced in China in 1996. This review focused on the effects of iodine excess worldwide and particularly in China.
-
Citations
Citations to this article as recorded by- Comparison of effects of potassium iodide and potassium chloride on structure and physicochemical properties of proteins
Fuge Niu, Yi Gao, Xinyu Yan, Huabin Liao, Zhe Li, Yanren Cao, Mengdi Zhao, Beibei Wang, Jiao Yu, Weichun Pan
Journal of Molecular Liquids.2024; 395: 123844. CrossRef - Micronutrients throughout the Life Cycle: Needs and Functions in Health
and Disease
Mohit Kumar, Devesh Kumar, Ankita Sharma, Shivam Bhadauria, Anil Thakur, Amit Bhatia
Current Nutrition & Food Science.2024; 20(1): 62. CrossRef - Relationship Between Urinary Iodine Concentration and the Prevalence
of Thyroid Nodules and Subclinical Hypothyroidism
Huachao Zhu, Pu Chen, Xi Ding, Yanru Zhao
Hormone and Metabolic Research.2024;[Epub] CrossRef - Associations of Combined Exposure to Metabolic and Inflammatory Indicators with Thyroid Nodules in Adults: A Nested Case-Control Study
Xin-Yi Zhu, Xing-Chen Meng, Bei-Jing Cheng, Chun Wang, Jia Wang, Tian-Lin Li, Hui Li, Ke Meng, Ran Liu, Alexander Schreiber
International Journal of Endocrinology.2024; 2024: 1. CrossRef - Thyroid-Stimulating Hormone Levels within the Trimester-Specific Reference Intervals Are Correlated with Non–High-Density Lipoprotein Cholesterol and Remnant Cholesterol Concentrations in Pregnant Women
Guocheng Wang, Feng Jin, Limin Xie, Xiaofen Zhang, Yawei Zhang, Xin Ni, Wei Li, Guojun Zhang
Laboratory Medicine.2023; 54(5): 449. CrossRef - Factors associated with inadequate urinary iodine concentration among pregnant women in Mbeya region Tanzania.
Tedson Lukindo, Ray Masumo, Adam Hancy, Sauli E. John, Heavenlight A. Paulo, Abraham Sanga, Ramadhan Noor, Fatoumata Lankoande, Elifatio Towo, Germana H. Leyna, Gemma Bridge, Raman Bedi
F1000Research.2023; 10: 858. CrossRef - Iodine status and its association with prevalence of thyroid diseases in adults from Jiangxi Province, China
Di-en Yan, Lei Hu, Yun-feng Shen, Xiao-yang Lai, Mei-ying Zhang, Min Zhou, Chao Chen, Mei-mei Liu, Li-ting Wu, Li-qun Liu, Qi-wei Fan, Wen-lan Min, Si-cong Wan, Fang Zou, Jing Li, Xia Cai, Shui-hong Lei, Yan Xiong, Ya Yang, Rong Yu, Wei-wei Gao, Ying Zhan
Endocrine.2023; 82(2): 335. CrossRef - Autoimmune thyroid status in subclinical thyroid disorders in patients attending a tertiary care center in Nepal: a hospital-based cross-sectional study
Vijay Kumar Sharma, Apeksha Niraula, Eans Tara Tuladhar, Aseem Bhattarai, Mithileshwer Raut, Raju Kumar Dubey, Sujata Baidya, Naresh Parajuli
BMC Endocrine Disorders.2023;[Epub] CrossRef - INFLUÊNCIA DA NUTRIÇÃO NO MANEJO DO HIPOTIREOIDISMO
Karine Rodrigues da Silva Neumann , Isadora Neres Silva, Elaine Cristina Rocha Oliveira, Taís Cristina Macêdo de Carvalho
Revista Saúde Dos Vales.2023;[Epub] CrossRef - Relationship between Thyroid CT Density, Volume, and Future TSH Elevation: A 5-Year Follow-Up Study
Tomohiro Kikuchi, Shouhei Hanaoka, Takahiro Nakao, Yukihiro Nomura, Takeharu Yoshikawa, Md Ashraful Alam, Harushi Mori, Naoto Hayashi
Life.2023; 13(12): 2303. CrossRef - The relationship between urinary iodine concentration and papillary thyroid cancer: A systematic review and meta-analysis
Xueqi Zhang, Fan Zhang, Qiuxian Li, Renaguli Aihaiti, Chuyao Feng, Deshi Chen, Xu Zhao, Weiping Teng
Frontiers in Endocrinology.2022;[Epub] CrossRef - The impact of the micronutrient iodine in health and diseases
Ma. Cecilia Opazo, Irenice Coronado-Arrázola, Omar P. Vallejos, Rodrigo Moreno-Reyes, Carlos Fardella, Lorena Mosso, Alexis M. Kalergis, Susan M. Bueno, Claudia A. Riedel
Critical Reviews in Food Science and Nutrition.2022; 62(6): 1466. CrossRef - Halogens in Seaweeds: Biological and Environmental Significance
Hanan Al-Adilah, Martin C. Feiters, Lucy J. Carpenter, Puja Kumari, Carl J. Carrano, Dhia Al-Bader, Frithjof C. Küpper
Phycology.2022; 2(1): 132. CrossRef - Solid sorbents for gaseous iodine capture and their conversion into stable waste forms
R. Pénélope, L. Campayo, M. Fournier, A. Gossard, A. Grandjean
Journal of Nuclear Materials.2022; 563: 153635. CrossRef - Secular Trends in the Prevalence of and Disability-Adjusted Life Years Due to Common Micronutrient Deficiencies in China From 1990 to 2019: An Age-Period-Cohort Study and Joinpoint Analysis
Haiying Chen, Jinxin Lu, Yongze Li
Frontiers in Nutrition.2022;[Epub] CrossRef - Iodine Concentrations in Conventional and Organic Milk in the Northeastern U.S.
Nobumitsu Sakai, Ola Yetunde Esho, Motoko Mukai
Dairy.2022; 3(2): 211. CrossRef - Effect of iodine restriction on short-term changes in thyroid function in patients with subclinical hypothyroidism
Obin Kwon, Dong Yeob Shin, Eun Jig Lee
Journal of Nutrition and Health.2022; 55(2): 250. CrossRef - Excessive iodine in iodized household salt in Nepal
Basant Giri, Shishir Pandey, Sadiksha Shakya, Bhanu Bhakta Neupane, Krishna Prasad Kandel, Chandradip Kumar Yadav, Ram Prabodh Yadav, Bishnu Prasad Neupane, Rajendra Bahadur GC, Prem Singh Saud, Meghraj Yonjan
Annals of the New York Academy of Sciences.2022; 1514(1): 166. CrossRef - Factors associated with inadequate urinary iodine concentration among pregnant women in Mbeya region Tanzania.
Tedson Lukindo, Ray Masumo, Adam Hancy, Sauli E. John, Heavenlight A. Paulo, Abraham Sanga, Ramadhan Noor, Fatoumata Lankoande, Elifatio Towo, Germana H. Leyna, Gemma Bridge, Raman Bedi
F1000Research.2022; 10: 858. CrossRef - Iodine nutrition and papillary thyroid cancer
Xueqi Zhang, Fan Zhang, Qiuxian Li, Chuyao Feng, Weiping Teng
Frontiers in Nutrition.2022;[Epub] CrossRef - Thyroid function disorders
Mirjana Stojković
Arhiv za farmaciju.2022; 72(5): 429. CrossRef - Serum T3 Level and Duration of Minimum Maintenance Dose Therapy Predict Relapse in Methimazole-Treated Graves Disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Rajata Rajatanavin, Thep Himathongkam
Journal of the Endocrine Society.2021;[Epub] CrossRef - Factors influencing the reference interval of thyroid‐stimulating hormone in healthy adults: A systematic review and meta‐analysis
Dongyang Xing, Delong Liu, Ri Li, Qi Zhou, Jiancheng Xu
Clinical Endocrinology.2021; 95(3): 378. CrossRef - The Iodine Status and Prevalence of Thyroid Disorders Among Women of Childbearing Age in China: National Cross-sectional Study
Yongze Li, Zhongyan Shan, Weiping Teng
Endocrine Practice.2021; 27(10): 1028. CrossRef - Environmental and human iodine and selenium status: lessons from Gilgit-Baltistan, North-East Pakistan
Saeed Ahmad, Elizabeth H. Bailey, Muhammad Arshad, Sher Ahmed, Michael J. Watts, Alex G. Stewart, Scott D. Young
Environmental Geochemistry and Health.2021; 43(11): 4665. CrossRef - Factors associated with inadequate urinary iodine concentration among pregnant women in Mbeya region Tanzania.
Tedson Lukindo, Ray Masumo, Adam Hancy, Sauli E. John, Heavenlight A. Paulo, Abraham Sanga, Ramadhan Noor, Fatoumata Lankoande, Elifatio Towo, Germana H. Leyna, Gemma Bridge, Raman Bedi
F1000Research.2021; 10: 858. CrossRef - Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study
Kyungsik Kim, Sun Wook Cho, Young Joo Park, Kyu Eun Lee, Dong-Wook Lee, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 790. CrossRef - Age‐specific thyrotropin references decrease over‐diagnosis of hypothyroidism in elderly patients in iodine‐excessive areas
Yingchai Zhang, Yu Sun, Zhiwei He, Shuhang Xu, Chao Liu, Yongze Li, Zhongyan Shan, Weiping Teng
Clinical Endocrinology.2021;[Epub] CrossRef - Dietary Micronutrients from Zygote to Senility: Updated Review of Minerals’ Role and Orchestration in Human Nutrition throughout Life Cycle with Sex Differences
Mohamed A. Farag, Samia Hamouda, Suzan Gomaa, Aishat A. Agboluaje, Mohamad Louai M. Hariri, Shimaa Mohammad Yousof
Nutrients.2021; 13(11): 3740. CrossRef - Епідеміологія автоімунного тиреоїдиту
V.I. Кravchenko, О.А. Тоvkay, О.V. Rakov, М.D. Тronko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(2): 136. CrossRef - Association between urinary sodium levels and iodine status in Korea
Jonghwa Ahn, Jang Ho Lee, Jiwoo Lee, Ji Yeon Baek, Eyun Song, Hye-Seon Oh, Mijin Kim, Suyeon Park, Min Ji Jeon, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
The Korean Journal of Internal Medicine.2020; 35(2): 392. CrossRef - Is heart disease a risk factor for low dementia test battery scores in older persons with Down syndrome? Exploratory, pilot study, and commentary
Maire E. Percy, Walter J. Lukiw
International Journal of Developmental Disabilities.2020; 66(1): 22. CrossRef - A cross-sectional research of iodine status of pregnant women in Chongqing, south-west China
Ning Yao, Chunbei Zhou, Jun Xie, Shuang Zhou
Public Health Nutrition.2020; 23(5): 769. CrossRef - The Diverse Upper Reference Limits of Serum Thyroid-Stimulating Hormone on the Same Platform for Pregnant Women in China
Guocheng Wang, Guojun Zhang
Laboratory Medicine.2020; 51(4): 416. CrossRef - Efficacy and Safety of Long-Term Universal Salt Iodization on Thyroid Disorders: Epidemiological Evidence from 31 Provinces of Mainland China
Yongze Li, Di Teng, Jianming Ba, Bing Chen, Jianling Du, Lanjie He, Xiaoyang Lai, Xiaochun Teng, Xiaoguang Shi, Yanbo Li, Haiyi Chi, Eryuan Liao, Chao Liu, Libin Liu, Guijun Qin, Yingfen Qin, Huibiao Quan, Bingyin Shi, Hui Sun, Xulei Tang, Nanwei Tong, Gu
Thyroid.2020; 30(4): 568. CrossRef - High prevalence of TPO-Abs and subclinical hypothyroidism in iodine-sufficient pregnant women in Northern Algeria
Samira Akdader-Oudahmane, Zohra Hamouli-Saïd, Michael B. Zimmermann, Hanane Kherrab, Said Azzoug, Djamila Meskine
Journal of Trace Elements in Medicine and Biology.2020; 61: 126533. CrossRef - An Inverse Relationship Between Iodine Intake and Thyroid Antibodies: A National Cross-Sectional Survey in Mainland China
Di Teng, Wenqing Yang, Xiaoguang Shi, Yongze Li, Jianming Ba, Bing Chen, Jianling Du, Lanjie He, Xiaoyang Lai, Yanbo Li, Haiyi Chi, Eryuan Liao, Chao Liu, Libin Liu, Guijun Qin, Yingfen Qin, Huibiao Quan, Bingyin Shi, Hui Sun, Xulei Tang, Nanwei Tong, Gui
Thyroid.2020; 30(11): 1656. CrossRef - Therapeutic Effects of Combination Regimens Including Methimazole on Graves Hyperthyroidism: A Network Meta-Analysis of Randomized Controlled Trials
Maorong Wang, Yerong Yu
Endocrine Practice.2020; 26(6): 675. CrossRef - The change in the clinical presentation of Graves’ disease: a 30 years retrospective survey in an academic Brazilian tertiary center
Wanesa Pinto, João H. Romaldini, Nicolas Perini, Roberto B. Santos, Danilo Villagelin
Archives of Endocrinology and Metabolism.2020;[Epub] CrossRef - Association between Urinary Iodine Concentration and Thyroid Nodules in Adults: A Cross-Sectional Study in China
Hui Sun, Hanyu Wang, Xiaolan Lian, Chao Liu, Bingyin Shi, Lixin Shi, Nanwei Tong, Shu Wang, Jianping Weng, Jiajun Zhao, Jiaoyue Zhang, Juan Zheng, Xiang Hu, Yunxia Tu, Li Yu, Zhongyan Shan, Weiping Teng, Lulu Chen, Ali Abbara
BioMed Research International.2020; 2020: 1. CrossRef - The effect of intake of sausages fortified with β-CD-I2 complex on iodine status and thyroid function: A preliminary study
Maksym Polumbryk, Victor Kravchenko, Vasyl Pasichnyi, Chrystyna Omelchenko, Irina Pachitskaya
Journal of Trace Elements in Medicine and Biology.2019; 51: 159. CrossRef - Association between Iodine Nutrition Status and Thyroid Disease-Related Hormone in Korean Adults: Korean National Health and Nutrition Examination Survey VI (2013–2015)
Kim, Kwon, Kim, Hong, Park
Nutrients.2019; 11(11): 2757. CrossRef - Association Between Thyroid Nodules and Volume and Metabolic Syndrome in an Iodine-Adequate Area: A Large Community-Based Population Study
Yue Su, Yan-ling Zhang, Meng Zhao, Hai-qing Zhang, Xu Zhang, Qing-bo Guan, Chun-xiao Yu, Shan-shan Shao, Jin Xu
Metabolic Syndrome and Related Disorders.2019; 17(4): 217. CrossRef - Analytical evaluation of the new Seal Autoanalyzer 3 High Resolution for urinary iodine determination
Valentina Vidranski, Maja Franceschi, Dražena Krilić, Tomislav Jukić, Ivan Mihaljević, Zvonko Kusić
Biochemia medica.2019; 29(2): 394. CrossRef - Increased Incidence Rate of Hypothyroidism After Iodine Fortification in Denmark: A 20-Year Prospective Population-Based Study
Mads Petersen, Nils Knudsen, Allan Carlé, Stig Andersen, Torben Jørgensen, Hans Perrild, Lars Ovesen, Lone Banke Rasmussen, Betina Heinsbæk Thuesen, Inge Bülow Pedersen
The Journal of Clinical Endocrinology & Metabolism.2019; 104(5): 1833. CrossRef - Relationship of gender and age on thyroid hormone parameters in a large Chinese population
Xinxin Chen, Xulei Zheng, Zhaojun Ding, Yang Su, Shu Wang, Bin Cui, Zhen Xie
Archives of Endocrinology and Metabolism.2019;[Epub] CrossRef - Sex differences in the association between thyroid-stimulating hormone levels and depressive symptoms among the general population with normal free T4 levels
San Lee, Sarah Soyeon Oh, Eun-Cheol Park, Sung-In Jang
Journal of Affective Disorders.2019; 249: 151. CrossRef - Reference intervals of thyroid hormones in a previously iodine-deficient area in Darfur, Sudan
Nagi I. Ali, Abdullah O. Alamoudi, Ishag Adam
Therapeutic Advances in Endocrinology and Metabolism.2018; 9(9): 293. CrossRef - Highly sensitive electrochemical detection of iodate based on glassy carbon electrode modified with iridium oxide
Yanna Lazarova, Ivan Shterev, Totka Dodevska
Monatshefte für Chemie - Chemical Monthly.2018; 149(11): 1955. CrossRef - Acute Delirium in a Hypothyroid Patient Precipitated by Iodine Supplements Use
Gaby S. Gil, Bradford W. Smith, Jose R. Guerra, William T. Williams
American Journal of Therapeutics.2018; 25(6): e717. CrossRef - Iodine Deficiency in Zhejiang Pregnant Women in the Context of Universal Salt Iodization Programme
Zhifang Wang, Mingluan Xing, Wenming Zhu, Guangming Mao, Zhe Mo, Yuanyang Wang, Zhijian Chen, Xiaoming Lou, Shichang Xia, Xiaofeng Wang
Scientific Reports.2018;[Epub] CrossRef - Age- and gender-specific reference intervals of TSH and free T4 in an iodine-replete area: Data from Korean National Health and Nutrition Examination Survey IV (2013–2015)
So Young Park, Hae In Kim, Hyun-Kyung Oh, Tae Hyuk Kim, Hye Won Jang, Jae Hoon Chung, Myung-Hee Shin, Sun Wook Kim, Sun Y Lee
PLOS ONE.2018; 13(2): e0190738. CrossRef - Age-specific reference interval of serum TSH levels is high in adolescence in an iodine excess area: Korea national health and nutrition examination survey data
Hyemi Kwon, Won Gu Kim, Min Ji Jeon, Minkyu Han, Mijin Kim, Suyeon Park, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrine.2017; 57(3): 445. CrossRef - Urinary iodine levels and dairy consumption in pre-school children in Southwest Asturias (Spain)
Esther Arbesú Fernández, María Haydee Serrano Peraza, Hans Abdón Eguia Angeles, César Oliver Sotelo García, Claude Henrry Saint Jean, Nache Ismael Musa Martín
Anales de Pediatría (English Edition).2017; 87(1): 18. CrossRef - Association of iodized salt with goiter prevalence in Chinese populations: a continuity analysis over time
Zhen Liang, Chen Xu, Yong-Jun Luo
Military Medical Research.2017;[Epub] CrossRef - Yodurias y consumo de lácteos en preescolares del Área Suroccidental de Asturias
Esther Arbesú Fernández, M. Haydee Serrano Peraza, Hans Abdón Eguia Angeles, César Oliver Sotelo García, Claude Henrry Saint Jean, Nache Ismael Musa Martín
Anales de Pediatría.2017; 87(1): 18. CrossRef - Role of medical resource level in iodine deficiency disorder
Chen Xu, Zhen Liang, Yong-Jun Luo
Military Medical Research.2017;[Epub] CrossRef - Strong association of relatively low and extremely excessive iodine intakes with thyroid cancer in an iodine-replete area
Hye Jeong Kim, Na Kyung Kim, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo, Yong-Ki Min, Sun Wook Kim, Jae Hoon Chung
European Journal of Nutrition.2017; 56(3): 965. CrossRef - Excessive Iodine Intake and Thyrotropin Reference Interval: Data from the Korean National Health and Nutrition Examination Survey
Min Ji Jeon, Won Gu Kim, Hyemi Kwon, Mijin Kim, Suyeon Park, Hye-Seon Oh, Minkyu Han, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(7): 967. CrossRef - Metabolic syndrome is associated with an increased incidence of subclinical hypothyroidism – A Cohort Study
Chia-Hsuin Chang, Yi-Chun Yeh, James L. Caffrey, Shyang-Rong Shih, Lee-Ming Chuang, Yu-Kang Tu
Scientific Reports.2017;[Epub] CrossRef - Associations between thyroid dysfunction and developmental status in children with excessive iodine status
Inger Aakre, Tor A. Strand, Khalil Moubarek, Ingrid Barikmo, Sigrun Henjum, Hiroyoshi Ariga
PLOS ONE.2017; 12(11): e0187241. CrossRef - Vitamin D deficiency affects thyroid autoimmunity and dysfunction in iodine-replete area: Korea national health and nutrition examination survey
Mijin Kim, Eyun Song, Hye-Seon Oh, Suyeon Park, Hyemi Kwon, Min Ji Jeon, Won Gu Kim, Won Bae Kim, Young Kee Shong, Tae Yong Kim
Endocrine.2017; 58(2): 332. CrossRef - Thyroid Function Status in Indian Adult Nonpregnant Females in Ranchi, India
Nandita Hazra, Sarvinder Singh, Binay Mitra, Bhaskar Shahbabu
Indian journal of Medical Biochemistry.2017; 21(1): 25. CrossRef - Iodine Status and Prevalence of Thyroid Disorders After Introduction of Mandatory Universal Salt Iodization for 16 Years in China: A Cross-Sectional Study in 10 Cities
Zhongyan Shan, Lulu Chen, Xiaolan Lian, Chao Liu, Bingyin Shi, Lixin Shi, Nanwei Tong, Shu Wang, Jianping Weng, Jiajun Zhao, Xiaochun Teng, Xiaohui Yu, Yaxin Lai, Weiwei Wang, Chenyan Li, Jinyuan Mao, Yongze Li, Chenling Fan, Weiping Teng
Thyroid.2016; 26(8): 1125. CrossRef - Iodine nutrition status and thyroid disorders: a cross-sectional study from the Xinjiang Autonomous Region of China
Y Guo, J Zynat, Z Xu, X Wang, R Osiman, H Zhao, A Tuhuti, M Abdunaimu, H Wang, X Jin, S Xing
European Journal of Clinical Nutrition.2016; 70(11): 1332. CrossRef - Effect of Prolonged Iodine Overdose on Type 2 Iodothyronine Deiodinase Ubiquitination-Related Enzymes in the Rat Pituitary
Xiaowen Zhang, Yaqiu Jiang, Wenqing Han, Aihua Liu, Xiaochen Xie, Cheng Han, Chenling Fan, Hong Wang, Hongmei Zhang, Shuangning Ding, Zhongyan Shan, Weiping Teng
Biological Trace Element Research.2016; 174(2): 377. CrossRef - Reference intervals of thyroid hormones in a previously iodine-deficient but presently more than adequate area of Western China: a population-based survey
Jing Cai, Yujie Fang, Da Jing, Shaoyong Xu, Jie Ming, Bin Gao, Han Shen, Rong Zhang, Qiuhe Ji
Endocrine Journal.2016; 63(4): 381. CrossRef - Urinary Iodine Excretion among Nepalese School Children in Terai Region
Saroj Khatiwada, Basanta Gelal, Prem Raj Shakya, Madhab Lamsal, Nirmal Baral
The Indian Journal of Pediatrics.2016; 83(1): 15. CrossRef - Usefulness of Measuring Thyroid Stimulating Antibody at the Time of Antithyroid Drug Withdrawal for Predicting Relapse of Graves Disease
Hyemi Kwon, Won Gu Kim, Eun Kyung Jang, Mijin Kim, Suyeon Park, Min Ji Jeon, Tae Yong Kim, Jin-Sook Ryu, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2016; 31(2): 300. CrossRef - Evaluation of energy spectrum CT for the measurement of thyroid iodine content
Weiguang Shao, Jingang Liu, Dianmei Liu
BMC Medical Imaging.2016;[Epub] CrossRef - Iodide Residues in Milk Vary between Iodine‐Based Teat Disinfectants
Elizabeth A. French, Motoko Mukai, Michael Zurakowski, Bradley Rauch, Gloria Gioia, Joseph R. Hillebrandt, Mark Henderson, Ynte H. Schukken, Thomas C. Hemling
Journal of Food Science.2016;[Epub] CrossRef - Total thyroidectomy as primary surgical management for thyroid disease: surgical therapy experience from 5559 thyroidectomies in a less-developed region
Jisheng Hu, Nan Zhao, Rui Kong, Dawei Wang, Bei Sun, Lifeng Wu
World Journal of Surgical Oncology.2015;[Epub] CrossRef - Tg in Adults as a Sensitive Biomarker of Iodine Status: A 5-Year Follow up Population Study in Different Levels of Iodine Intake Regions
Wei Chong, Xiaoguang Shi, Zhongyan Shan, Xiaochun Teng, Di Teng, Haixia Guan, Yushu Li, Ying Jin, Xiaohui Yu, Chenling Fan, Fan Yang, Hong Dai, Yang Yu, Jia Li, Yanyan Chen, Dong Zhao, Fengnan Hu, Jinyuan Mao, Xiaolan Gu, Rong Yang, Yajie Tong, Weibo Wang
PLOS ONE.2015; 10(8): e0135553. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Comparison of effects of potassium iodide and potassium chloride on structure and physicochemical properties of proteins

- Measurement of Anti-GAD65 Autoantibodies in Patients with Type 1 Diabetes Mellitus with / without Autoimmune Thyroid Diseases (Immunoblotting followed by Immunoprecipitation).
- Yong Soo Park, Hye Won Park, Jin Bae Kim, Dong Sun Kim, Woong Hwan Choi, Tae Hwa Kim, Joon Yong Chung, Sei Won Yang, Won Bae Kim
- J Korean Endocr Soc. 2000;15(2):190-203. Published online January 1, 2001
- 1,228 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Type 1 diabetes mellitus is frequently associated with other autoimmune diseases. The broad concept of polyendocrinopathies takes into consideration that patients affected by at least one endocrine disease may have another autoimmune disorder or express specific autoantibodies. Anti-glutamic acid decarboxylase autoantibodies, now recognized as one of the major serological markers for type 1 diabetes has been reported to be higher in type 1 diabetes patients with autoimmune thyroid diseases (ATD) than in those without ATD. The objective of the present study was to evaluate the prevalences of GAD65 antibodies applying a newly developed assay(anti-GAD65) in type 1 diabetes patients with and without ATD. METHODS: We developed a new anti-GAD65 assay after mammalian expression of a recombinant GAD65 antigen. Since the detection of anti-GAD65 is rather complicated and insensitive due to inherent antigenic difference of antibody recognition in conventional assays, we applied this new approach in measuring anti-GAD autoantibodies and compared the result with ICA and anti-GAD measurement using the purified porcine GAD (anti-GAD) in 109 cases of type 1 diabetes, 29 of whom had concomitant ATD (mean age at diagnosis: 7.9 yr, mean duration of type 1 diabetes: 4.5 yrs). RESULTS: The overall prevalence of anti-GAD65 antibodies was 65% (71 of 109) in patients with Korean type 1 diabetes. Prevalences and titers of anti-GAD65 had not changed much after controlling for the duration and the status of concomitant ATD. In contrast, the prevalence of anti-GAD was 56%(61 of 109), while that of ICA(+) WAS 36% in type 1 diabetes patients. We found significant, but not strong association of anti-GAD65 either with anti-GAD(r=0.4, p<0.01) or with ICA(r=0.6, p< 0.001). CONCLUSION: From this, we could assess that autoantibodies are present at comparable sensitivity and specificity in Korean type 1 diabetes patients. This anti-GAD65 assay, another immunologic marker for type 1 diabetes might also confer disease susceptibility among Koreans, but no increase in the prevalence or in the titer in patients with ATD may suggest that this marker is unlikely to give much benefit, for the detection of the overlapping disease of type 1 diabetes and ATD.


 KES
KES

 First
First Prev
Prev



