Search
- Page Path
- HOME > Search
- Thyroid
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
- Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Endocrinol Metab. 2021;36(6):1277-1286. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1251
- 5,184 View
- 181 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The detrimental effects of excessive thyroid hormone on glucose metabolism have been widely investigated. However, the risk of diabetes in patients with long-standing hyperthyroidism, especially according to treatment modality, remains uncertain, with few longitudinal studies.
Methods
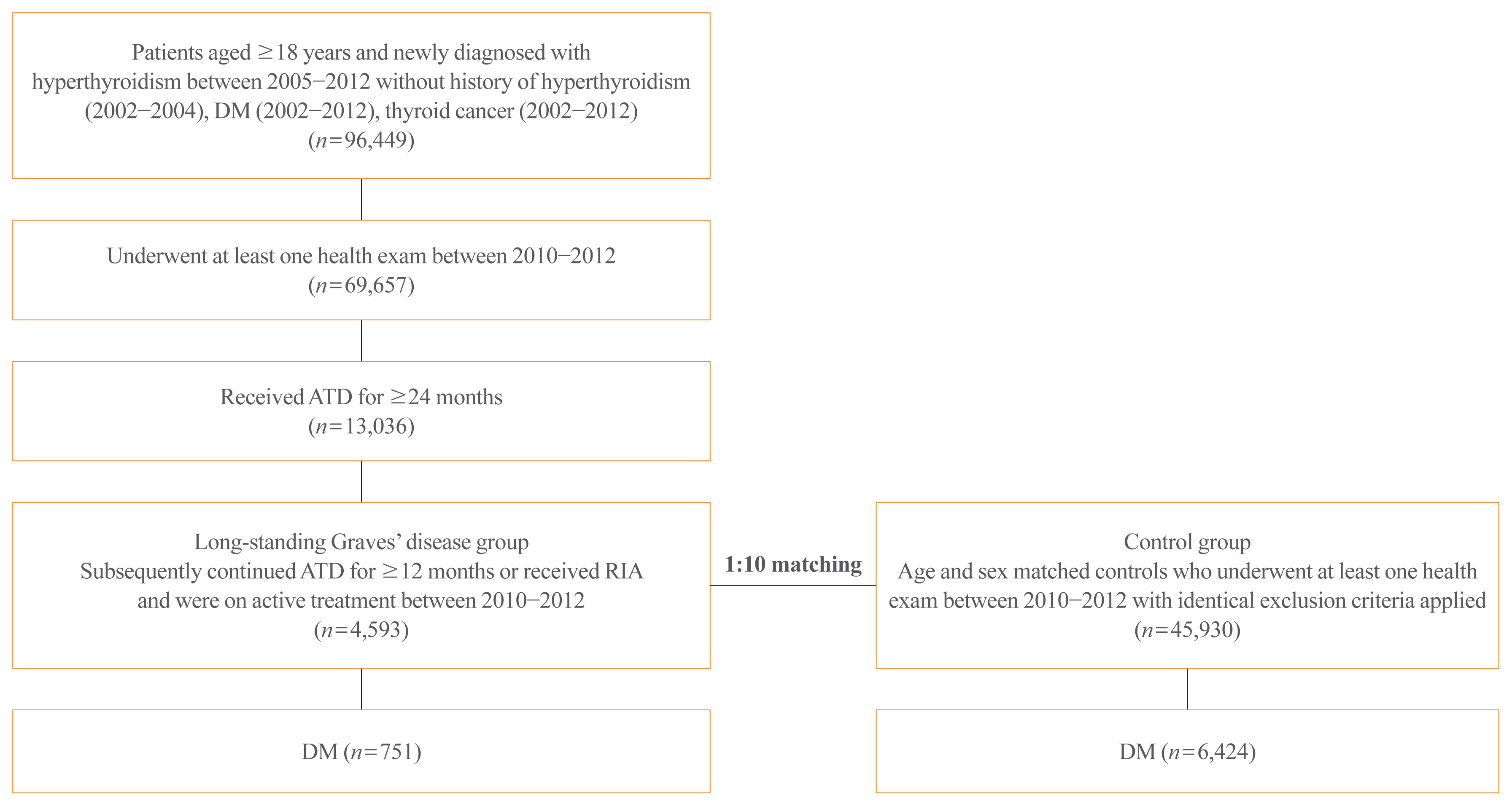
The risk of diabetes in patients with Graves’ disease treated with antithyroid drugs (ATDs) for longer than the conventional duration (≥2 years) was compared with that in age-and sex-matched controls. The risk was further compared according to subsequent treatment modalities after a 24-month course of ATD: continuation of ATD (ATD group) vs. radioactive iodine ablation (RIA) group.
Results
A total of 4,593 patients were included. Diabetes was diagnosed in 751 (16.3%) patients over a follow-up of 7.3 years. The hazard ratio (HR) for diabetes, after adjusting for various known risk factors, was 1.18 (95% confidence interval [CI], 1.10 to 1.28) in patients with hyperthyroidism. Among the treatment modality groups, the RIA group (n=102) had a higher risk of diabetes than the ATD group (n=4,491) with HR of 1.56 (95% CI, 1.01 to 2.42). Further, the risk of diabetes increased with an increase in the ATD treatment duration (P for trend=0.019).
Conclusion
The risk of diabetes was significantly higher in patients with long-standing Graves’ disease than in the general population, especially in patients who underwent RIA and prolonged ATD treatment. Special attention to hyperglycemia during follow-up along with effective control of hyperthyroidism may be necessary to reduce the risk of diabetes in these patients. -
Citations
Citations to this article as recorded by- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience
Nadia Sawicka-Gutaj, Dawid Gruszczyński, Natalia Zawalna, Kacper Nijakowski, Agnieszka Skiba, Mateusz Pochylski, Jerzy Sowiński, Marek Ruchała
Pharmacological Reports.2024; 76(1): 185. CrossRef - Increased risk of diabetes mellitus and hyperlipidemia in patients with differentiated thyroid cancer
Hwa Young Ahn, Jooyoung Lee, Jinmo Kang, Eun Kyung Lee
European Journal of Endocrinology.2024; 190(3): 248. CrossRef - Prevalencia de diabetes en personas con disfunción tiroidea
Juan J. Díez, Pedro Iglesias
Medicina Clínica.2023; 160(8): 333. CrossRef - Control of Thyroid Dysfunction in Spanish Population Registered in
the Primary Care Clinical Database: An Analysis of the Proportion of Patients
with Thyrotropin Values Outside the Reference Range
Juan J. Díez, Pedro Iglesias
Hormone and Metabolic Research.2023; 55(03): 184. CrossRef - Prevalence of thyroid dysfunction and its relationship to income level and employment status: a nationwide population-based study in Spain
Juan J. Díez, Pedro Iglesias
Hormones.2023; 22(2): 243. CrossRef - Prevalence of diabetes in people with thyroid dysfunction
Juan J. Díez, Pedro Iglesias
Medicina Clínica (English Edition).2023; 160(8): 333. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Thyroid Eye Disease and Its Association With Diabetes Mellitus: A Major Review
Roshmi Gupta, Pramila Kalra, Lakshmi B. Ramamurthy, Suryasnata Rath
Ophthalmic Plastic & Reconstructive Surgery.2023; 39(6S): S51. CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef
- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience

- Thyroid
- 99mTc-Pertechnetate Scintigraphy Predicts Successful Postoperative Ablation in Differentiated Thyroid Carcinoma Patients Treated with Low Radioiodine Activities
- Luca Giovanella, Gaetano Paone, Teresa Ruberto, Luca Ceriani, Pierpaolo Trimboli
- Endocrinol Metab. 2019;34(1):63-69. Published online February 15, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.63
- 4,283 View
- 66 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Postoperative routine radioiodine (RAI) treatment is currently debated for patients with low-risk differentiated thyroid carcinoma (DTC) patients. If performed, a low 131I activity (i.e., 1 to 2 GBq) is recommended with the aim to ablate thyroid remnant and facilitate subsequent follow-up by thyroglobulin measurement. The purpose of this study was to evaluate the relationship between postsurgical technetium-99m (99mTc)-pertechnetate scintigraphy and the rate of successful remnant ablation after low activity radioiodine ablation in patients with DTC.
Methods Enrolled were 193 patients with low risk DTC who underwent total thyroidectomy and RAI ablation with a fixed 1.1 GBq activity of 131I. 99mTc-pertechnetate scans were done and thyrotropin stimulated thyroglobulin (sTg) levels measured just before ablation. Ablation effectiveness was assessed 6 to 12 months later by sTg measurement, neck ultrasound and diagnostic whole body scan.
Results A negative 99mTc-perthecnetate scans was the best predictor of successful ablation (
P <0.001) followed by preablative sTg levels <0.8 ng/mL (P =0.008) and 99mTc-pertechnetate uptake rate values <0.9% (P =0.065). Neither sex nor age of the patient at the time of ablation or tumor histology and size showed a significant association with the rate of successful ablation.Conclusion The 99mTc-pertechnetate scintigraphy is a simple and feasible tool to predict effectiveness of low activity 131I thyroid to ablate thyroid remnants in patients with DTC.
-
Citations
Citations to this article as recorded by- Combined clinical variable and radiomics of post-treatment total body scan for prediction of successful I-131 ablation in low-risk papillary thyroid carcinoma patients
Maythinee Chantadisai, Jirarot Wongwijitsook, Napat Ritlumlert, Yothin Rakvongthai
Scientific Reports.2024;[Epub] CrossRef - The prognostic value of post thyroidectomy Tc-99m pertechnetate thyroid scan in patients with differentiated thyroid cancer
L.M. Eloteify, Samy M. Algizawy, Aya K.M. Abdelnaim, Nesreen Mekkawy
Nuclear Medicine Communications.2023; 44(1): 38. CrossRef - Correlation analysis of I-131 SPECT/CT uptake parameters with the success ablation treatment of thyroid remnant in patients with low-intermediate-risk differentiated thyroid cancer
Qian Zhang, Weina Xu
Nuclear Medicine Communications.2022; 43(10): 1051. CrossRef - Clinical significance of extra-thyroid 99mTc-pertechnetate uptake before initial radioiodine therapy for differentiated thyroid carcinoma
Bin Long, Li-Fang Yao, Shou-Cong Chen, Jin Shui, Xue-Mei Ye, He-Qing Yi, Cen Lou
Journal of International Medical Research.2021; 49(5): 030006052110126. CrossRef - Thyroglobulin Changes are Highly Dependent on TSH in Low-risk DTC Patients not Treated with Radioiodine
Antonio Matrone, Alessio Faranda, Francesco Latrofa, Carla Gambale, Delio Stefani Donati, Eleonora Molinaro, Laura Agate, David Viola, Paolo Piaggi, Liborio Torregrossa, Fulvio Basolo, Rossella Elisei
The Journal of Clinical Endocrinology & Metabolism.2020; 105(8): e2845. CrossRef
- Combined clinical variable and radiomics of post-treatment total body scan for prediction of successful I-131 ablation in low-risk papillary thyroid carcinoma patients

- Clinical Study
- Economic Evaluation of Recombinant Human Thyroid Stimulating Hormone Stimulation vs. Thyroid Hormone Withdrawal Prior to Radioiodine Ablation for Thyroid Cancer: The Korean Perspective
- Seo Young Sohn, Hye Won Jang, Yoon Young Cho, Sun Wook Kim, Jae Hoon Chung
- Endocrinol Metab. 2015;30(4):531-542. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.531
- 3,539 View
- 43 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Previous studies have suggested that recombinant human thyroid stimulating hormone (rhTSH) stimulation is an acceptable alternative to thyroid hormone withdrawal (THW) when radioiodine remnant ablation is planned for thyroid cancer treatment, based on superior short-term quality of life with non-inferior remnant ablation efficacy. This study evaluated the cost-effectiveness of radioiodine remnant ablation using rhTSH, compared with the traditional preparation method which renders patients hypothyroid by THW, in Korean perspective.
Methods This economic evaluation considered the costs and benefits to the Korean public healthcare system. Clinical experts were surveyed regarding the current practice of radioiodine ablation in Korea and their responses helped inform assumptions used in a cost effectiveness model. Markov modelling with 17 weekly cycles was used to assess the incremental costs per quality-adjusted life year (QALY) associated with rhTSH. Clinical inputs were based on a multi-center, randomized controlled trial comparing remnant ablation success after rhTSH preparation with THW. The additional costs associated with rhTSH were considered relative to the clinical benefits and cost offsets.
Results The additional benefits of rhTSH (0.036 QALY) are achieved with an additional cost of Korean won ₩961,105, equating to cost per QALY of ₩26,697,361. Sensitivity analyses had only a modest impact upon cost-effectiveness, with one-way sensitivity results of approximately ₩33,000,000/QALY.
Conclusion The use of rhTSH is a cost-effective alternative to endogenous hypothyroid stimulation prior to radioiodine ablation for patients who have undergone thyroidectomy in Korea.
-
Citations
Citations to this article as recorded by- Comparison of Recombinant Human Thyroid-Stimulating Hormone and Thyroid Hormone Withdrawal for 131I Therapy in Patients With Intermediate- to High-Risk Thyroid Cancer
Sohyun Park, Ji-In Bang, Keunyoung Kim, Youngduk Seo, Ari Chong, Chae Moon Hong, Dong-Eun Lee, Miyoung Choi, Sang-Woo Lee, So Won Oh
Clinical Nuclear Medicine.2024; 49(3): e96. CrossRef - Thyroid Hormone Withdrawal versus Recombinant Human TSH as Preparation for I-131 Therapy in Patients with Metastatic Thyroid Cancer: A Systematic Review and Meta-Analysis
Luca Giovanella, Maria Luisa Garo, Alfredo Campenní, Petra Petranović Ovčariček, Rainer Görges
Cancers.2023; 15(9): 2510. CrossRef - Health-related quality of life of thyroid cancer patients undergoing radioiodine therapy: a cohort real-world study in a reference public cancer hospital in Brazil
Jayda Eiras Ramim, Marcella Araugio Soares Cardoso, Gessen Lopes Carneiro de Oliveira, Maria Luisa Gomes, Tiago Teixeira Guimarães, Rossana Corbo Ramalho de Mello, Anke Bergmann, Priscilla Brunelli Pujatti
Supportive Care in Cancer.2020; 28(8): 3771. CrossRef - Predictive factors determining incomplete response to radioiodine therapy in patients with differentiated thyroid cancer
Ewelina Szczepanek-Parulska, Magdalena Wojewoda-Korbelak, Martyna Borowczyk, Malgorzata Kaluzna, Barbara Brominska, Katarzyna Ziemnicka, Rafal Czepczynski, Maciej Baczyk, Marek Ruchala
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2020;[Epub] CrossRef - Initial Adoption of Recombinant Human Thyroid-Stimulating Hormone Following Thyroidectomy in the Medicare Thyroid Cancer Patient Population
Michaela A. Dinan, Yanhong Li, Shelby D. Reed, Julie Ann Sosa
Endocrine Practice.2019; 25(1): 31. CrossRef - Triennial Report ofEndocrinology and Metabolism, 2015 to 2017
Eun-Jung Rhee, Hey Yeon Jang, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 195. CrossRef - Recombinant human TSH stimulated thyroglobulin levels at remnant ablation predict structural incomplete response to treatment in patients with differentiated thyroid cancer
Jeonghoon Ha, Min Hee Kim, Kwanhoon Jo, Yejee Lim, Ja Seong Bae, Sohee Lee, Moo Il Kang, Bong Yun Cha, Dong Jun Lim
Medicine.2017; 96(29): e7512. CrossRef - Does the Risk of Metabolic Syndrome Increase in Thyroid Cancer Survivors?
Min-Hee Kim, Jin-young Huh, Dong-jun Lim, Moo-Il Kang
Thyroid.2017; 27(7): 936. CrossRef
- Comparison of Recombinant Human Thyroid-Stimulating Hormone and Thyroid Hormone Withdrawal for 131I Therapy in Patients With Intermediate- to High-Risk Thyroid Cancer

- Thyroid
- Radioiodine Therapy in Differentiated Thyroid Cancer: The First Targeted Therapy in Oncology
- June-Key Chung, Gi Jeong Cheon
- Endocrinol Metab. 2014;29(3):233-239. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.233
- 4,883 View
- 73 Download
- 34 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Iodide uptake across the membranes of thyroid follicular cells and cancer cells occurs through an active transport process mediated by the sodium-iodide symporter (NIS). The rat and human NIS-coding genes were cloned and identified in 1996. Evaluation of NIS gene and protein expression is critical for the management of thyroid cancer, and several approaches to increase NIS levels have been tried. Identification of the NIS gene has provided a means of expanding its role in radionuclide therapy and molecular target-specific theragnosis (therapy and diagnosis using the same molecular target). In this article, we describe the relationship between NIS expression and the thyroid carcinoma treatment using I-131 and alternative therapeutic approaches.
-
Citations
Citations to this article as recorded by- A Pilot Nonrandomized Controlled Trial Examining the Use of Artificial Tears on the Radioactivity of Tears After Radioactive Iodine Treatment for Thyroid Cancer
Irene T. Lee, Jared V. Grice, Xiangyu Ji, Qingxia Chen, Lindsay A. Bischoff, Aaron C. Jessop, Behin Barahimi, Francois Codere, Louise A. Mawn, Rachel K. Sobel
Thyroid®.2024; 34(1): 82. CrossRef - Research progress of bone metastases: From disease recognition to clinical practice
Wenbo Yang, Qing Pan, Fuhua Huang, Hongzhi Hu, Zengwu Shao
Frontiers in Oncology.2023;[Epub] CrossRef - Letter to the editor regarding “Bone metastases from differentiated thyroid carcinoma: heterogenous tumor response to radioactive Iodine therapy and overall survival”
Maria José Veloza Vega, Manuela Gallo, Gonzalo Ucros, Patricia Bernal
European Journal of Nuclear Medicine and Molecular Imaging.2022; 49(11): 3622. CrossRef - Factors Associated With Radioactive Iodine Therapy–Acquired Nasolacrimal Duct Obstruction
Irene T. Lee, Wencong Chen, Qingxia Chen, Heather A. Cole, Lindsay A. Bischoff, Aaron C. Jessop, Rachel K. Sobel
Endocrine Practice.2022; 28(12): 1210. CrossRef - RNA-Seq transcriptome analysis reveals Maackia amurensis leukoagglutinin has antitumor activity in human anaplastic thyroid cancer cells
Suna Bektas, Engin Kaptan
Molecular Biology Reports.2022; 49(10): 9257. CrossRef - Radio-Iodide Treatment: From Molecular Aspects to the Clinical View
Antonio De la Vieja, Garcilaso Riesco-Eizaguirre
Cancers.2021; 13(5): 995. CrossRef - Current Status and Future Perspective of the Treatment for Radioiodine Refractory Differentiated Thyroid Cancer
Young Kee Shong
International Journal of Thyroidology.2021; 14(2): 98. CrossRef - 18F-fluorodeoxyglucose positron emission tomography combined with computed tomography for the prediction of radioiodine therapy response in patients with metastatic differentiated thyroid cancer
T. M. Geliashvili, A. V. Vazhenin, T. P. Berezovskaya, N. G. Afanasyeva, E. V. Vasilyeva, P. I. Garbuzov, V. V. Krylov
Head and Neck Tumors (HNT).2020; 9(4): 10. CrossRef - Salivary side effects after radioiodine treatment for differentiated papillary thyroid carcinoma: Long‐term study
Marc‐Kevin Le Roux, Nicolas Graillon, Laurent Guyot, David Taieb, Philippe Galli, Yves Godio‐Raboutet, Cyrille Chossegros, Jean‐Marc Foletti
Head & Neck.2020; 42(11): 3133. CrossRef - β-radiating radionuclides in cancer treatment, novel insight into promising approach
Samieh Asadian, Hamed Mirzaei, Bagher Aziz Kalantari, Mohamad Reza Davarpanah, Morteza Mohamadi, Anastasia Shpichka, Leila Nasehi, Hamidreza Aboulkheyr Es, Peter Timashev, Mustapha Najimi, Nematollah Gheibi, Moustapha Hassan, Massoud Vosough
Pharmacological Research.2020; 160: 105070. CrossRef - Peptide Receptor Radionuclide Therapy in Patients With Differentiated Thyroid Cancer
Dong Yun Lee, Yong-il Kim
Clinical Nuclear Medicine.2020; 45(8): 604. CrossRef - FDG PET/CT for the early prediction of RAI therapy response in patients with metastatic differentiated thyroid carcinoma
Seo Young Kang, Ji-In Bang, Keon Wook Kang, Ho-young Lee, June-Key Chung, Juri G. Gelovani
PLOS ONE.2019; 14(6): e0218416. CrossRef - Role of iodide metabolism in physiology and cancer
Antonio De la Vieja, Pilar Santisteban
Endocrine-Related Cancer.2018; 25(4): R225. CrossRef - Star-Shaped Intense Uptake of 131I on Whole Body Scans Can Reflect Good Therapeutic Effects of Low-Dose Radioactive Iodine Treatment of 1.1 GBq
Sung Hye Kong, Jung Ah Lim, Young Shin Song, Shinje Moon, Ye An Kim, Min Joo Kim, Sun Wook Cho, Jae Hoon Moon, Ka Hee Yi, Do Joon Park, Bo Youn Cho, Young Joo Park
Endocrinology and Metabolism.2018; 33(2): 228. CrossRef - Sodium Iodide Symporter (NIS) in the Management of Patients with Thyroid Carcinoma
June-Key Chung, Hyun Woo Kim, Haewon Youn, Gi Jeong Cheon
Nuclear Medicine and Molecular Imaging.2018; 52(5): 325. CrossRef - LARP7 in papillary thyroid carcinoma induces NIS expression through suppression of the SHH signaling pathway
Xiaomei Sui, Yana Sui, Yonghui Wang
Molecular Medicine Reports.2018;[Epub] CrossRef - Human sodium iodide transporter gene-mediated imaging and therapy of mouse glioma, comparison between 188Re and 131I
Rui Guo, Yun Xi, Min Zhang, Ying Miao, Miao Zhang, Biao Li
Oncology Letters.2018;[Epub] CrossRef - Iodine-131 Therapy and Lacrimal Drainage System Toxicity: Nasal Localization Studies Using Whole Body Nuclear Scintigraphy and SPECT-CT
Mohammad Javed Ali, Achyut Ram Vyakaranam, Jyotsna Eleshwarapu Rao, Giri Prasad, Palkonda Vijay Anand Reddy
Ophthalmic Plastic & Reconstructive Surgery.2017; 33(1): 13. CrossRef - Targeted Radionuclide Therapy: An Evolution Toward Precision Cancer Treatment
Hossein Jadvar
American Journal of Roentgenology.2017; 209(2): 277. CrossRef - Radioprotective effect of vitamin E on salivary glands after radioiodine therapy for differentiated thyroid cancer
Arun Upadhyaya, Pingping Zhou, Zhaowei Meng, Peng Wang, Guizhi Zhang, Qiang Jia, Jian Tan, Xue Li, Tianpeng Hu, Na Liu, Sen Wang, Xiaoxia Liu, Huiying Wang, Chunmei Zhang, Fengxiao Zhao, Ziyu Yan, Xiaoran Wang, Xuemeng Zhang, Wan Zhang
Nuclear Medicine Communications.2017; 38(11): 891. CrossRef - Effects of first radioiodine ablation on functions of salivary glands in patients with differentiated thyroid cancer
Arun Upadhyaya, Zhaowei Meng, Peng Wang, Guizhi Zhang, Qiang Jia, Jian Tan, Xue Li, Tianpeng Hu, Na Liu, Pingping Zhou, Sen Wang, Xiaoxia Liu, Huiying Wang, Chunmei Zhang, Fengxiao Zhao, Ziyu Yan
Medicine.2017; 96(25): e7164. CrossRef - Growth Kinetics of Macronodular Lung Metastases and Survival in Differentiated Thyroid Carcinoma
Mijin Kim, Won Gu Kim, Suyeon Park, Hyemi Kwon, Min Ji Jeon, Sang Min Lee, Jeong Hyun Lee, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(7): 915. CrossRef - Initial Size of Metastatic Lesions Is Best Prognostic Factor in Patients with Metastatic Differentiated Thyroid Carcinoma Confined to the Lung
Mijin Kim, Won Gu Kim, Suyeon Park, Hyemi Kwon, Min Ji Jeon, Jong Jin Lee, Jin-Sook Ryu, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(1): 49. CrossRef - Lack of Efficacy of Radioiodine Remnant Ablation for Papillary Thyroid Microcarcinoma: Verification Using Inverse Probability of Treatment Weighting
Hyemi Kwon, Min Ji Jeon, Won Gu Kim, Suyeon Park, Mijin Kim, Tae Yong Kim, Minkyu Han, Dong Eun Song, Tae-Yon Sung, Jong Ho Yoon, Suck Joon Hong, Jin-Sook Ryu, Young Kee Shong, Won Bae Kim
Annals of Surgical Oncology.2017; 24(9): 2596. CrossRef - Preparation and evaluation of 131I-quercetin as a novel radiotherapy agent against dedifferentiated thyroid cancer
Qinghua Xie, Xia Li, Guanquan Wang, Xuan Hou, Yujun Wang, Hongbo Yu, Changfa Qu, Shunzhong Luo, Yali Cui, Chuanqin Xia, Ruibing Wang
Journal of Radioanalytical and Nuclear Chemistry.2017; 311(3): 1697. CrossRef - Molecular radiotheragnostics in thyroid disease
Nitasha Singh, Val Lewington
Clinical Medicine.2017; 17(5): 453. CrossRef - Inhibition of BRD4 suppresses tumor growth and enhances iodine uptake in thyroid cancer
Xuemei Gao, Xinchao Wu, Xiao Zhang, Wenjuan Hua, Yajing Zhang, Yusufu Maimaiti, Zairong Gao, Yongxue Zhang
Biochemical and Biophysical Research Communications.2016; 469(3): 679. CrossRef - Hepatoprotective Effect of Dexmedetomidine Against Radioiodine Toxicity in Rats: Evaluation of Oxidative Status and Histopathologic Changes
Kemal Kismet, Murat Sadic, Yusuf Murat Bag, Hasan Ikbal Atilgan, Gokhan Koca, Ali Kemal Onalan, Mehmet Senes, Seydi Ali Peker, Nihat Yumusak, Meliha Korkmaz
International Surgery.2016; 101(3-4): 176. CrossRef - FoxP3 in papillary thyroid carcinoma induces NIS repression through activation of the TGF-β1/Smad signaling pathway
Siyuan Ma, Qingzhu Wang, Xiaojun Ma, Lina Wu, Feng Guo, Hongfei Ji, Fei Liu, Yanyan Zhao, Guijun Qin
Tumor Biology.2016; 37(1): 989. CrossRef - Iodine-131 Therapy and Nasolacrimal Duct Obstructions: What We Know and What We Need to Know
Mohammad Javed Ali
Ophthalmic Plastic & Reconstructive Surgery.2016; 32(4): 243. CrossRef - I-131 remnant ablation after thyroidectomy induced hepatotoxicity in a case of thyroid cancer
Rong Lin, Omar Banafea, Jin Ye
BMC Gastroenterology.2015;[Epub] CrossRef - Sub-Classification of Lateral Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma by Pathologic Criteria
Min Ji Jeon, Won Gu Kim, Eun Kyung Jang, Yun Mi Choi, Dong Eun Song, Tae-Yon Sung, Jong Ho Yoon, Ki-Wook Chung, Suck Joon Hong, Jin-Sook Ryu, Ji Min Han, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Konradin Metze
PLOS ONE.2015; 10(7): e0133625. CrossRef - Targeted Radionuclide Therapy of Human Tumors
Sergey Gudkov, Natalya Shilyagina, Vladimir Vodeneev, Andrei Zvyagin
International Journal of Molecular Sciences.2015; 17(1): 33. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- A Pilot Nonrandomized Controlled Trial Examining the Use of Artificial Tears on the Radioactivity of Tears After Radioactive Iodine Treatment for Thyroid Cancer

- A Retrospective Review of the Effectiveness of Recombinant Human TSH-Aided Radioiodine Treatment of Differentiated Thyroid Carcinoma.
- Min Ah Na, Sun Hae Shin, Yang Ho Kang, Seok Man Son, In Joo Kim, Yong Ki Kim
- J Korean Endocr Soc. 2006;21(4):274-280. Published online August 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.4.274
- 1,946 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of the study was to evaluate the biochemical effects of recombinant human thyroid stimulating hormone (rhTSH) as an adjunct to radioiodine (RI) treatment of a differentiated thyroid carcinoma (DTC). We retrospectively reviewed the clinical response rates of DTC patients treated with RI after thyroid hormone withdrawal and compared with those after rhTSH stimulation. METHOD: We included the patients treated with RI for locally recurrent DTC from February 1, 2002 to August 31, 2005 and followed with diagnostic studies at our hospital. Forty totally (or near totally) thyroidectomized adults were included in this study. Nine patients underwent RI treatment after rhTSH stimulation while euthyoid on L-thyroxine (LT4), and 31 patients were treated with RI after thyroid hormone withdrawal. The clinical response was defined as >25% decrease in serum thyroglobulin (Tg) level on LT4 3 months after the RI treatment. RESULTS: In each group, serum Tg levels were significantly decreased 3 months after the RI treatment. And we found that 77.8 and 71.0% of those prepared by rhTSH and LT4 withdrawal, respectively, had clinical responses 3 months after the RI treatment by our criteria and there was no significant difference in response rates between two groups (P=0.238). CONCLUSIONS: Given the biases that exist in retrospective studies, at the current time we cannot recommend the routine use of rhTSH to prepare RI treatment of DTC. However, our study provided preliminary evidence that rhTSH effectively aided RI treatment of DTC at least to an equivalent degree as LT4 withdrawal.

- Changes in Properties of Thyrotropin Receptor Antibodies Following Radioiodine Treatment in Patients with Graves' Disease.
- Won Bae Kim, Hyun Kyung Chung, Bo Youn Cho, Hong Kyu Lee, Chang Soon Koh, Do Joon Park, Yeon Sahng Oh
- J Korean Endocr Soc. 1997;12(2):194-206. Published online January 1, 2001
- 1,127 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It has been suggested that thyroid stimulation blocking antibody (TSBAb) is involved in the development of early hypothyroidism after radioiodine treatment in patient with Graves disease. However, previous studies have reported the effect of radioiodine treatment on overall changes of TSH receptor antibodies without detailed observation of changes in properties of TSH receptor antibodies. The aim of this study is to evaluate the effect of radioiodine treatment on thyroid stimulation antibody (TSAb) or on thyroid stimulation blocking antibody (TSBAb) activities and to see whether the appearance of TSBAb after radioiodine treatment is involved in the development of early hypothyroidism in patients with Graves disease. METHODS: The activities of TSAb, TSBAb were measured serially with human TSH receptor transfected Chinese hamster ovary (CHO) cells in 36 patients with Graves disease who received 131I treatment. In addition to the wild type TSH receptor-expressing cells, we used a chimeric receptor that 90-165 amino acid residues were substituted by those of rat LH/CG receptor (Mc2) for measurement of TSBAb without interference by the presence of TSAb and for evaluation of TSAb epitope spreading. We evaluated the association of early hypothyroidism after 131I treatment with changes of various immunologic parameters. RESULTS: In 14 (39%) of 36 patients, TSBAb activities were present in their sera before or after 131I treatment. Four of them had TSBAb activities before 131 treatment, and 12 newly acquired TSBAb activities after 131I treatment. The existence of TSBAb was not associated with the development of early hypothyroidism after 131I treatment but with low TSAb activities before 131 treatment, high thyroidal uptake of 131I given and with old age. The phenomena of epitope spreading measured by TSAb with Mc2 mutant clone before and after 131I treatment was not infrequent, but it had no clinical relevance. CONCLUSION: These results suggest that the existence of TSBAb may be not a major factor in the development of early hypothyroidism after radioiodine treatment in Graves disease. Other factors such as TSAb activities before radioiodine treatment, the efficiency of thyroidal uptake of 131I or old age are associated with the development of early hypothyroidism.


 KES
KES

 First
First Prev
Prev



