Search
- Page Path
- HOME > Search
- Hypothalamus and Pituitary Gland
Big Data Articles (National Health Insurance Service Database) - Descriptive Epidemiology and Survival Analysis of Prolactinomas and Cushing’s Disease in Korea
- Jin Sun Park, Soo Jin Yun, Jung Kuk Lee, So Young Park, Sang Ouk Chin
- Endocrinol Metab. 2021;36(3):688-696. Published online June 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1000
- 4,751 View
- 135 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Only a few studies have established the epidemiology of prolactinoma and Cushing’s disease in Korea. Furthermore, the incidence of these disease are increasing than before associated with the development of technologies. This study was designed to evaluate the epidemiology of prolactinoma and Cushing’s disease and their survival analysis according to treatment.
Methods
The nationwide, population-based study evaluated incidence and prevalence of prolactinoma and Cushing’s disease using de-identified claims data in The Korean Health Insurance Review and Assessment Service database between 2013 and 2017. The survival analysis investigated regarding treatment over a period of 6 years. A log-rank test and Cox proportional hazard regression analysis were used.
Results
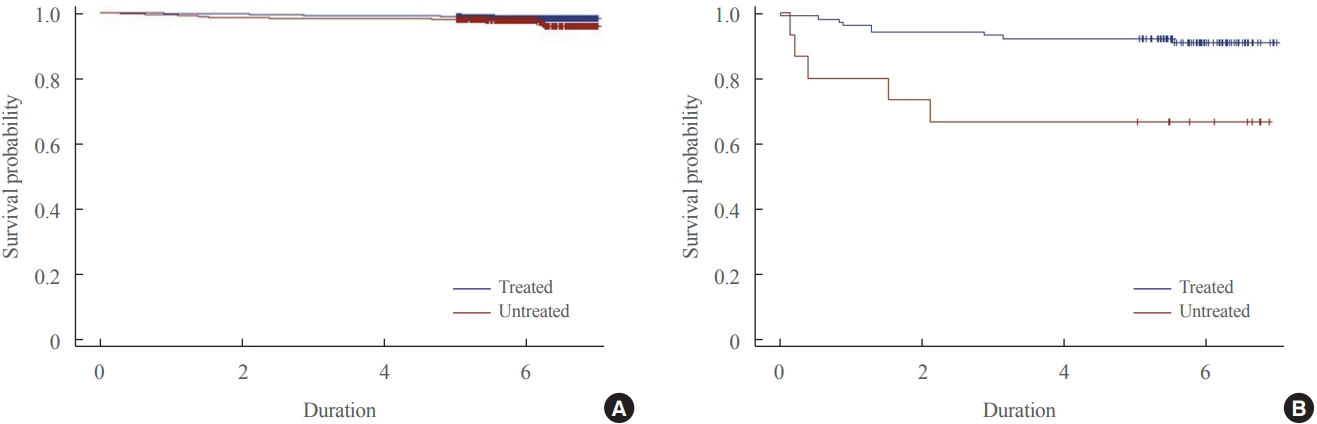
The 6,056 patients with newly diagnosed prolactinoma and 584 patients with Cushing’s disease were recorded between 2013 and 2017. The annual incidence of prolactinoma was 23.5 cases per million, and its prevalence was 82.5 cases per million, and 2.3 cases per million/year and 9.8 cases per million for Cushing’s disease. The survival benefit was insignificant in prolactinoma according to treatment, but treatment of Cushing’s disease ameliorated the survival rate significantly.
Conclusion
Overall, the incidence of prolactinoma and Cushing’s disease was similar with those found previously, but the prevalence of two diseases were inconsistent when compared with the early studies. The present study also proposed necessity of treatment in Cushing’s disease for improving the survival rate. -
Citations
Citations to this article as recorded by- Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Cushing Syndrome
Martin Reincke, Maria Fleseriu
JAMA.2023; 330(2): 170. CrossRef - Clinical Biology of the Pituitary Adenoma
Shlomo Melmed, Ursula B Kaiser, M Beatriz Lopes, Jerome Bertherat, Luis V Syro, Gerald Raverot, Martin Reincke, Gudmundur Johannsson, Albert Beckers, Maria Fleseriu, Andrea Giustina, John A H Wass, Ken K Y Ho
Endocrine Reviews.2022; 43(6): 1003. CrossRef
- Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database

- Reduction of Central Dopamine Release in Hyperprolactinemia.
- Bong Soo Cha, Young Duk Song, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Kap Bum Huh, Su Youn Nam, Eun Jig Lee, Bong Chul Chung, Jung Han Kim, Sei Chang Oh
- J Korean Endocr Soc. 1996;11(3):277-284. Published online November 7, 2019
- 1,134 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Prolactin(PRL) secretion is tonically inhibited by doparnine that originates from the hypothalamic tuberoinfundibular tract and reaches the lactotroph via the hypophyseal portal vessel. Hyperprolactinemia associated with oligomenorrhea-amenorrhea, galactorrhea and/or infertility is mainly due to PRL-secreting pituitary adenoma(PA). The diagnosis of idiopathic hyperprolac- tinemia(IHP) is made, when hyperprolactinemia is sustained and all causes of hyperprolactinemia are excluded without radiological abnormality. It is not known, whether IHP and PA are two distinct entities or two subsequent phases of the same disease. The etiology of both disorders remains unresolved. We investigated that PRL hypersecretion in patients with IHP and PA may be the result of a defect in the central nervous system(CNS)-dopamine release, and that there may be some differences in pathogenesis of both diseases. Methods: We measured 24 hour-urinary dopamine, norepinephrine, epinephrine, and serum and 24 hour-urinary VMA(vanillyl rnandelic acid), HVA(homovanilic acid), DOPAC(3,4-dihydroxy phenylaceticacid), MHPG(3-methoxy 4-hydroxy phenylglycol) in 10 normal controls, 9 patients with IHP, and 17 patients with PA in the early follicular phase. Results: Urinary HVA and DOPAC concentrations, the major metabolites of CNS dopaminergic activity, were signficantly lower in both patients with IHP and PA compared with those in normal controls(p 0.05), whereas they were not different in both disease groups. Dopamine, norepine-phrine, epinephrine, MHPG concentrations were similar to those of the normal controls. Although VMA concentrations of both disease groups were significantly higher than those of normal controls, all of them were within normal range. Conelusion: Although our data are unable to establish the precise biochemical defect responsible for central dopamine deficiency in pathogensis of IHP and PA, we can support the presence of a pathological reduction of brain dopamine activity in IHP and PA.

- Clinical and Endocrinologic Differences between Prolactinoma and Pseudoprolactinoma Proven by Immunohistochemical Study.
- Jae Wha Jo, Eun Jig Lee, Moon Suk Nam, Su Youn Nam, Young Duk Song, Hyun Chul Lee, Kap Bum Huh, Tae Seung Kim, Sun Ho Kim, Kyung Rae Kim, Bong Soo Cha, Ji Hyun Lee, Sung Kil Lim
- J Korean Endocr Soc. 1995;10(4):362-369. Published online November 7, 2019
- 1,610 View
- 54 Download
-
 Abstract
Abstract
 PDF
PDF - Hyperprolactinemia is the most common hypothalamo-pituitary disorder encountered in clinical endocrinology. Excluding the drug-induced hyperprolactinemia, the most common cause of this disorder is a pituitary tumor. Prolactinoma is mainly made up of prolactin-secreting cells but pseudoprolactinoma is tumor that does not secrete prolactin itself. The pseudoprolactinoma interrupts the flow of prolactin inhibiting factor, dopamine, from the hypothalamus through the pituitary stalk to the normal pituitary. The differentiation prolactinoma from pseudoprolactinoma is vitally important since true prolactinomas are most commonly responded well in terms of tumor shrinkage to medical treatment using dopamine agonist therapy, whereas pseudoprolactinomas do not. Thus surgical treatment is clearly indicated as first-line treatment if we know that a lesion is a pseudoprolactinoma. We compared prolactinoma with pseudoprolactinoma in clinical and endocrinologic characteristics of 48 cases after immunohistochemical diagnosis. We could not find any differential point of both tumors in clinical and radiological characteristics although some differences were exist. But we had found the relationship between the mean level of pretreatment serum prolactin and the presence of positive immunohistochemical stain for prolactin. The pretreatment serum prolactin level was significantly higher in patients with tumors showing many prolactin immunohistochemical staining cells than in those with none(p<0.05). When the pretreatment serum prolactin exceeded 100ng/ml, the tumors contain 94% of prolactin positive cells in stain. So, if the pretreatment serum prolactin exceeds 100ng/ml, we primarily suspect prolactinoma and medical treatment should be considered. If the pretreatment level below 100ng/ml, we suspect pseudoprolactinoma and surgical treatment should be considered.

- Recent Progress in the Medical Therapy of Pituitary Tumors
- Fabienne Langlois, Shirley McCartney, Maria Fleseriu
- Endocrinol Metab. 2017;32(2):162-170. Published online May 19, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.162
- 5,381 View
- 63 Download
- 27 Web of Science
- 27 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Management of pituitary tumors is multidisciplinary, with medical therapy playing an increasingly important role. With the exception of prolactin-secreting tumors, surgery is still considered the first-line treatment for the majority of pituitary adenomas. However, medical/pharmacological therapy plays an important role in controlling hormone-producing pituitary adenomas, especially for patients with acromegaly and Cushing disease (CD). In the case of non-functioning pituitary adenomas (NFAs), pharmacological therapy plays a minor role, the main objective of which is to reduce tumor growth, but this role requires further studies. For pituitary carcinomas and atypical adenomas, medical therapy, including chemotherapy, acts as an adjuvant to surgery and radiation therapy, which is often required to control these aggressive tumors. In the last decade, knowledge about the pathophysiological mechanisms of various pituitary adenomas has increased, thus novel medical therapies that target specific pathways implicated in tumor synthesis and hormonal over secretion are now available. Advancement in patient selection and determination of prognostic factors has also helped to individualize therapy for patients with pituitary tumors. Improvements in biochemical and “tumor mass” disease control can positively affect patient quality of life, comorbidities and overall survival. In this review, the medical armamentarium for treating CD, acromegaly, prolactinomas, NFA, and carcinomas/aggressive atypical adenomas will be presented. Pharmacological therapies, including doses, mode of administration, efficacy, adverse effects, and use in special circumstances are provided. Medical therapies currently under clinical investigation are also briefly discussed.
-
Citations
Citations to this article as recorded by- Multiomics Approach to Acromegaly: Unveiling Translational Insights for Precision Medicine
Kyungwon Kim, Cheol Ryong Ku, Eun Jig Lee
Endocrinology and Metabolism.2023; 38(5): 463. CrossRef - PDCD10 promotes the aggressive behaviors of pituitary adenomas by up-regulating CXCR2 and activating downstream AKT/ERK signaling
Jingdian Liu, Junwen Wang, Weidong Tian, Yu Xu, Ran Li, Kai Zhao, Chao You, Yuan Zhu, Joerg Walter Bartsch, Hongquan Niu, Huaqiu Zhang, Kai Shu, Ting Lei
Aging.2022; 14(15): 6066. CrossRef - LncRNA MYMLR promotes pituitary adenoma development by upregulating carbonyl reductase 1 via sponging miR-197-3p
Tuo Wang, Ping Mao, Yan Zhang, Bo Cui, Mao-De Wang, Ya Li, Ke Gao
Anti-Cancer Drugs.2022; 33(10): 1058. CrossRef - Comparative Proteomic Study Shows the Expression of Hint-1 in Pituitary Adenomas
Carolina Carrillo-Najar, Daniel Rembao-Bojórquez, Martha L. Tena-Suck, Sergio Zavala-Vega, Noemí Gelista-Herrera, Miguel A. Ramos-Peek, Juan L. Gómez-Amador, Febe Cazares-Raga, Fidel de la Cruz Hernández-Hernández, Alma Ortiz-Plata
Diagnostics.2021; 11(2): 330. CrossRef - Recent Understanding and Future Directions of Recurrent Corticotroph Tumors
José Miguel Hinojosa-Amaya, César Ernesto Lam-Chung, Daniel Cuevas-Ramos
Frontiers in Endocrinology.2021;[Epub] CrossRef - What to Do with Incidentally Discovered Pituitary Abnormalities?
Fabienne Langlois, Maria Fleseriu
Medical Clinics of North America.2021; 105(6): 1081. CrossRef - Aggressive prolactinoma (Review)
Ana Valea, Florica Sandru, Aida Petca, Mihai Dumitrascu, Mara Carsote, Razvan-Cosmin Petca, Adina Ghemigian
Experimental and Therapeutic Medicine.2021;[Epub] CrossRef - Diagnosis and Treatment of Pituitary Adenomas
O. A. Beylerli, Zhao Shiguang, I. F. Gareev, Chen Xin
Creative surgery and oncology.2020; 9(4): 311. CrossRef - Management of patients with persistent or recurrent Cushing’s disease after initial pituitary surgery
Cristina Capatina, José Miguel Hinojosa-Amaya, Catalina Poiana, Maria Fleseriu
Expert Review of Endocrinology & Metabolism.2020; 15(5): 321. CrossRef - Modern principles of the diagnosis and conservative treatment of Cushing disease
Ashraf Abdali, Ludmila Astafeva, Pavel Kalinin, Yuriy Trunin, I. V. Chernov, G. E. Сhmutin, Abdali Badshahzar, GulSharif Sherzad, Simfukwe Keith
Vestnik nevrologii, psihiatrii i nejrohirurgii (Bulletin of Neurology, Psychiatry and Neurosurgery).2020; (10): 67. CrossRef - Effects of Oxytocin on Cell Proliferation in a Corticotroph Adenoma Cell Line
Jung Soo Lim, Young Woo Eom, Eun Soo Lee, Hyeong Ju Kwon, Ja-Young Kwon, Junjeong Choi, Choon Hee Chung, Young Suk Jo, Eun Jig Lee
Endocrinology and Metabolism.2019; 34(3): 302. CrossRef - Pituitary Adenomas: What Are the Key Features? What Are the Current Treatments? Where Is the Future Taking Us?
Domenico Solari, Rosario Pivonello, Chiara Caggiano, Elia Guadagno, Carmela Chiaramonte, Giovanni Miccoli, Luigi M. Cavallo, Marialaura Del Basso De Caro, Annamaria Colao, Paolo Cappabianca
World Neurosurgery.2019; 127: 695. CrossRef - Expression of Cyclin E/Cdk2/p27Kip1 in Growth Hormone Adenomas
Wei Dong, Haibo Zhu, Hua Gao, Wenjian Shi, Yu Zhang, Hongyun Wang, Chuzhong Li, Guidong Song, Yazhuo Zhang
World Neurosurgery.2019; 121: e45. CrossRef - Acromegaly
Annamaria Colao, Ludovica F. S. Grasso, Andrea Giustina, Shlomo Melmed, Philippe Chanson, Alberto M. Pereira, Rosario Pivonello
Nature Reviews Disease Primers.2019;[Epub] CrossRef - Differenzialdiagnostik und Therapie der Hypophysenadenome
M. Hlaváč, F. Sommer, G. Karpel-Massler, R. Wirtz, T. Hoffmann, A. Paľa
HNO.2019; 67(4): 307. CrossRef - Medical Management of Cushing’s Syndrome: Current and Emerging Treatments
José Miguel Hinojosa-Amaya, Daniel Cuevas-Ramos, Maria Fleseriu
Drugs.2019; 79(9): 935. CrossRef - Aggressive and Malignant Prolactinomas
Nicoleta Cristina Olarescu, Luis G. Perez-Rivas, Federico Gatto, Thomas Cuny, Maria A. Tichomirowa, Gianluca Tamagno, Manuel D. Gahete
Neuroendocrinology.2019; 109(1): 57. CrossRef - New Insights in Cushing Disease Treatment With Focus on a Derivative of Vitamin A
Mariana Fuertes, Julieta Tkatch, Josefina Rosmino, Leandro Nieto, Mirtha Adriana Guitelman, Eduardo Arzt
Frontiers in Endocrinology.2018;[Epub] CrossRef - Prenatal alcohol exposure increases the susceptibility to develop aggressive prolactinomas in the pituitary gland
Shaima Jabbar, Kenneth Reuhl, Dipak K. Sarkar
Scientific Reports.2018;[Epub] CrossRef - Aggressive and malignant pituitary tumours: state-of-the-art
Dorota Dworakowska, Ashley B Grossman
Endocrine-Related Cancer.2018; 25(11): R559. CrossRef - Epidemiología y caracterización general de los tumores cerebrales primarios en el adulto
Maria Isabel Ocampo Navia, Juan Carlos Gómez Vega, Oscar Hernando Feo Lee
Universitas Médica.2018;[Epub] CrossRef - Triptolide inhibits pituitary adenoma cell viability, migration and invasion via ADAM12/EGFR signaling pathway
Junwen Wang, Zhuo Zhang, Ran Li, Wei Sun, Juan Chen, Huaqiu Zhang, Kai Shu, Ting Lei
Life Sciences.2018; 194: 150. CrossRef - Emerging roles of bexarotene in the prevention, treatment and anti-drug resistance of cancers
Danyang Shen, Xiaoming Yu, Yan Wu, Yuanlei Chen, Gonghui Li, Feng Cheng, Liqun Xia
Expert Review of Anticancer Therapy.2018; 18(5): 487. CrossRef - New Molecular Targets for Treatment of Cushing’s Disease
Elizabeth Foulkes, John Newell-Price
Endocrinology and Metabolism Clinics of North America.2018; 47(2): 367. CrossRef - Pituitary-Directed Therapies for Cushing’s Disease
Fabienne Langlois, Jennifer Chu, Maria Fleseriu
Frontiers in Endocrinology.2018;[Epub] CrossRef - Updates in Diagnosis and Treatment of Acromegaly
Roula Zahr, Maria Fleseriu
European Endocrinology.2018; 14(2): 57. CrossRef - Root cause analysis of diagnostic and surgical failures in the treatment of suspected Cushing’s disease
Hasan A. Zaidi, David L. Penn, David J. Cote, Edward R. Laws
Journal of Clinical Neuroscience.2018; 53: 153. CrossRef
- Multiomics Approach to Acromegaly: Unveiling Translational Insights for Precision Medicine

- Adrenal gland
- Early Prediction of Long-Term Response to Cabergoline in Patients with Macroprolactinomas
- Youngki Lee, Cheol Ryong Ku, Eui-Hyun Kim, Jae Won Hong, Eun Jig Lee, Sun Ho Kim
- Endocrinol Metab. 2014;29(3):280-292. Published online September 25, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.3.280
- 4,256 View
- 52 Download
- 12 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Cabergoline is typically effective for treating prolactinomas; however, some patients display cabergoline resistance, and the early characteristics of these patients remain unclear. We analyzed early indicators predicting long-term response to cabergoline.
Methods We retrospectively reviewed the cases of 44 patients with macroprolactinomas who received cabergoline as first-line treatment; the patients were followed for a median of 16 months. The influence of various clinical parameters on outcomes was evaluated.
Results Forty patients (90.9%) were treated medically and displayed tumor volume reduction (TVR) of 74.7%, a prolactin normalization (NP) rate of 81.8%, and a complete response (CR; TVR >50% with NP, without surgery) rate of 70.5%. Most patients (93.1%) with TVR ≥25% and NP at 3 months eventually achieved CR, whereas only 50% of patients with TVR ≥25% without NP and no patients with TVR <25% achieved CR. TVR at 3 months was strongly correlated with final TVR (
R =0.785). Patients with large macroadenomas exhibited a low NP rate at 3 months, but eventually achieved TVR and NP rates similar to those of patients with smaller tumors. Surgery independently reduced the final dose of cabergoline (β=-1.181 mg/week), and two of four patients who underwent surgery were able to discontinue cabergoline.Conclusion Determining cabergoline response using TVR and NP 3 months after treatment is useful for predicting later outcomes. However, further cabergoline administration should be considered for patients with TVR >25% at 3 months without NP, particularly those with huge prolactinomas, because a delayed response may be achieved. As surgery can reduce the cabergoline dose necessary for successful disease control, it should be considered for cabergoline-resistant patients.
-
Citations
Citations to this article as recorded by- Resistance to dopamine agonists in the treatment of prolactinomas: diagnostic criteria, mechanisms and ways to overcome it
Irena A. Ilovayskaya, Gulnar R. Vagapova
Almanac of Clinical Medicine.2024; 51(7): 397. CrossRef - Diagnosis and management of prolactin-secreting pituitary adenomas: a Pituitary Society international Consensus Statement
Stephan Petersenn, Maria Fleseriu, Felipe F. Casanueva, Andrea Giustina, Nienke Biermasz, Beverly M. K. Biller, Marcello Bronstein, Philippe Chanson, Hidenori Fukuoka, Monica Gadelha, Yona Greenman, Mark Gurnell, Ken K. Y. Ho, Jürgen Honegger, Adriana G.
Nature Reviews Endocrinology.2023; 19(12): 722. CrossRef - Outcome Measures for Medical and Surgical Treatment of Prolactinomas. Is the Role of Surgery Underestimated?
Andrius Anuzis, Kevin O. Lillehei
Journal of Neurological Surgery Part B: Skull Base.2023;[Epub] CrossRef - Are dopamine agonists still the first-choice treatment for prolactinoma in the era of endoscopy? A systematic review and meta-analysis
Xiangming Cai, Junhao Zhu, Jin Yang, Chao Tang, Zixiang Cong, Chiyuan Ma
Chinese Neurosurgical Journal.2022;[Epub] CrossRef - Italian Association of Clinical Endocrinologists (AME) and International Chapter of Clinical Endocrinology (ICCE). Position statement for clinical practice: prolactin-secreting tumors
Renato Cozzi, Maria Rosaria Ambrosio, Roberto Attanasio, Claudia Battista, Alessandro Bozzao, Marco Caputo, Enrica Ciccarelli, Laura De Marinis, Ernesto De Menis, Marco Faustini Fustini, Franco Grimaldi, Andrea Lania, Giovanni Lasio, Francesco Logoluso, M
European Journal of Endocrinology.2022; 186(3): P1. CrossRef - Biochemical Remission after Cabergoline Withdrawal in Hyperprolactinemic Patients with Visible Remnant Pituitary Adenoma
Kyungwon Kim, Yae Won Park, Daham Kim, Sung Soo Ahn, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Cheol Ryong Ku
The Journal of Clinical Endocrinology & Metabolism.2021; 106(2): e615. CrossRef - Surgery is a safe, effective first-line treatment modality for noninvasive prolactinomas
Ji Yong Park, Wonsuk Choi, A Ram Hong, Jee Hee Yoon, Hee Kyung Kim, Woo-Youl Jang, Shin Jung, Ho-Cheol Kang
Pituitary.2021; 24(6): 955. CrossRef - Molecular Pathways in Prolactinomas: Translational and Therapeutic Implications
Betina Biagetti, Rafael Simò
International Journal of Molecular Sciences.2021; 22(20): 11247. CrossRef - A scoping review to understand the indications, effectiveness, and limitations of cabergoline in radiological and biochemical remission of prolactinomas
Rakesh Mishra, SubhasK Konar, Adesh Shrivastava, Pradeep Chouksey, Sumit Raj, Amit Agrawal
Indian Journal of Endocrinology and Metabolism.2021; 25(6): 493. CrossRef - Predictors of dopamine agonist resistance in prolactinoma patients
Elle Vermeulen, Jean D’Haens, Tadeusz Stadnik, David Unuane, Kurt Barbe, Vera Van Velthoven, Sven Gläsker
BMC Endocrine Disorders.2020;[Epub] CrossRef - The Role of Dopamine Agonists in Pituitary Adenomas
Erica A. Giraldi, Adriana G. Ioachimescu
Endocrinology and Metabolism Clinics of North America.2020; 49(3): 453. CrossRef - Prevalence of Thyroid Disease in Patients Surgically Treated for Pituitary Disease
Kim, Cho, Ku, Jung, Moon, Kim, Shin, Kim, Lee
Journal of Clinical Medicine.2019; 8(8): 1142. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Resistance to dopamine agonists in the treatment of prolactinomas: diagnostic criteria, mechanisms and ways to overcome it

- Normal Repetitive Pregnancies and Tumor Regression Induced by Low-Dose Bromocriptine in a Patient with Macroprolactinoma.
- Hye Jung Choi, Jin Yong Park, Woo Seok Choi, Jong Gyu Song, Hee Young Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi
- J Korean Endocr Soc. 2009;24(1):42-46. Published online March 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.1.42
- 1,730 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Prolactin-secreting adenomas are the most common pituitary tumors. Menstrual disturbances and infertility are the main complaints in women with prolactinoma. Dopaminergic agonists such as bromocriptine are well-established treatments for prolactinoma when pregnancy is desired. Pregnancy-related outcomes in macroprolactinoma are worse than those in microprolactinoma. In addition, symptomatic tumor expansion during pregnancy occurs in 30% of women with macroprolactinoma. Therefore, when women with macroprolactinoma are planning a pregnancy, serum prolactin level should be normalized and the tumor volume significantly reduced. On the other hand, a spontaneous regression of macroprolactinoma can occur after pregnancy. We report a case of macroprolactinoma showing significant tumor regression during repeated pregnancies and low dose bromocriptine treatment, with a literature review.

- A Case of Multiple Endocrine Neoplasia Type 1 with Papillary Thyroid Carcinoma.
- Hai Jin Kim, Chul Sik Kim, Hyun Chul Je, Jina Park, Jong Suk Park, Jee Hyun Kong, Eun Seok Kang, Chul Woo Ahn, Bong Soo Cha, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Hang Suk Jang, Soon Won Hong
- J Korean Endocr Soc. 2006;21(1):79-84. Published online February 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.1.79
- 1,805 View
- 21 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - This is the first report of papillary thyroid carcinoma combined with multiple endocrine neoplasia type 1 (MEN 1). It is an hereditary syndrome characterized by neoplastic disorders such as pituitary adenoma, parathyroid adenoma or hyperplasia and pancreatic neuroendocrine tumor, such as gastrinoma just like in our case. But sometimes pheochromocytoma, mucosal ganglioneuromas, lipoma, forgut carcinoid and thyroid disease could be accompany the disease, but coincidental papillary thyroid carcinoma was never reported before in Korea. Herein we represent a 39-year-old woman who manifested typical features of MEN 1 with coincidental papillary thyroid carcinoma. Despite with definite family history of MEN 1, her genetic analysis of DNA had not found any germline mutation in MEN 1 gene. Unidentified culprit gene unable further genetic study of finding LOH (loss of heterogeneity) in 11q13, the possible explanation of papillary thyroid carcinoma as a new component of MEN 1. As we have experienced a case of MEN 1 combined with papillary thyroid carcinoma, we report it with the review of literature.
-
Citations
Citations to this article as recorded by- A Case of Multiple Endocrine Neoplasia Type I with Atypical Clinical Course
Yun Sun Choi, Youn Sun Bai, Bon Jeong Ku, Young Suk Jo, Young Kun Kim, Heung Kyu Ro, Minho Shong
Journal of Korean Endocrine Society.2008; 23(4): 266. CrossRef
- A Case of Multiple Endocrine Neoplasia Type I with Atypical Clinical Course

- The Clinical Characteristics of Macroprolactinemia.
- Young Ju Choi, Jun Goo Kang, Sung Yeon Kim, Eui Sil Hong, Sang Wan Kim, Chan Soo Shin, Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee
- J Korean Endocr Soc. 2005;20(3):216-223. Published online June 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.3.216
- 1,650 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Prolactin has been identified by gel chromatography to exist is three different forms in human serum; monomeric prolactin(molecular mass 23kDa), big prolactin (molecular mass 50~60 kDa) and big big prolactin, otherwise known as macroprolactin(molecular mass 150~170kDa). The predominance of macroprolactinemia has long been known in idiopathic hyperprolactinemic patients with maintained fertility. In recent reports, 24% of microprolactinoma patients showed no menstrual disturbances, which was suggestive of macroprolactinemia. The purpose of this study was to evaluate: (1) the frequency of macroprolactinemia among idiopathic hyperprolactinemia and prolactinoma patients, (2) the difference in the clinical characteristics between hyperprolactinemia, with and without macroprolactinemia, among idiopathic hyperprolactinemia and prolactinoma patients, and (3) the follow-up prolactin level using the bromocriptine response. METHODS: We retrospectively analyzed the clinical characteristics and prolactin levels in 43 idiopathic hyperprolactinemia and 51 prolactinoma patients with a poor bromocriptine response. Macroprolactinemia was identified by the prolactin recovery of < 40% using the polyethylene glycol(PEG) precipitation test. RESULTS: (1) Of the 43 idiopathic hyperprolactinemia and 51 prolactinoma patients, 17(39.5%) and 9(17.6%), respectively, were macroprolactinemic(P<0.05). (2) Among the idiopathic hyperprolactinemia patients, galactorrhea combined with amenorrhea was significantly less frequent (P<0.05), with the 1- and 2-year follow-up prolactin levels being significantly higher in those with macroprolactinemia than monomeric prolactinemia(P<0.05). (3) Among the prolactinoma patients, amenorrhea was significantly less frequent(P<0.05), but asymptomatic cases were more frequent in those with macroprolactinemia than monomeric prolactinemia(P <0.05). The 1- and 2-year follow-up prolactin levels were significantly higher in those with macroprolactinemia than monomeric prolactinemia(P<0.05). CONCLUSION: The screening of macroprolactinemia should be considered in idiopathic hyperprolactinemia and prolactinoma patients with a poor bromocriptine response

- High-Dose Hook Effect in Patients with Macroprolactinoma.
- Sung Yeon Kim, Chul Gu Park, Young Ju Choi, Eui Sil Hong, Sang Wan Kim, Chan Soo Shin, Hak Chul Jang, Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee
- J Korean Endocr Soc. 2005;20(2):148-153. Published online April 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.2.148
- 1,988 View
- 20 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Large amounts of antigen may produce false low values on immunoradiometric assays due to the so-called high-dose hook effect. The physicians' awareness of the possibility of the "high-dose hook effect" will prevent preoperative misdiagnosis. The study was designed to identify the frequency and clinical features of patients with pituitary macroadenomas in whom a high-dose PRL hook effect was documented. METHODS: Our retrospective study involved 42 patients with non-functioning pituitary adenomas (tumor diameter >30mm) who underwent transsphenoidal microsurgery from between Jan 1999 to Aug 2004, and 6 patients with non-functioning pituitary adenoma(tumor diameter>30mm) were selected for prospective study from Sep 2003 to Feb 2004. Our retrospective study also involved 13 patients with macroprolactinoma for the comparison of the clinical features. RESULTS: 1) The presence of a high-dose hook effect was retrospectively suggested when the PRL levels increased in 4 out of the 42 patients with non- functioning adenomas(tumor diameter >30mm) after surgery. Post-operative immunohistochemical staining of their pituitary specimens revealed the tumors to be prolactinoma. 2) Prospectively, dilution testing of the specimens obtained before surgery was done in the 6 patients, and one patient presented with a case of the hook effect. The patient's prolactin level was measured at 53.1ng/mL before dilution and this was increased up to 22,600ng/mL upon the 1:1000 dilution. 3) Conclusively, the hook effect was seen in 5 of the 48 patients(10.4%) with non-functioning pituitary adenoma(tumor diameter >30mm) 4) Compared with other 2 patient groups(the macroprolactinoma(N=13) group, and the non-functioning pituitary tumor(N=43) group), the high-dose PRL hook effect is more likely to be observed in male patients with large pituitary tumors. CONCLUSION: In order to avoid the high-dose hook effect, PRL should be assayed at 1:100~1:200 or even higher dilutions of serum from all patients(and especially the male patients) with large pituitary tumors -
Citations
Citations to this article as recorded by- Multiple Endocrine Neoplasia Type 1 Presenting with an Invasive Giant Prolactinoma
Jinhoon Cha, Jin Seo Kim, Jung Suk Han, Yeon Won Park, Min Joo Kim, Yun Hyi Ku, Hong Il Kim
The Korean Journal of Medicine.2016; 91(3): 300. CrossRef
- Multiple Endocrine Neoplasia Type 1 Presenting with an Invasive Giant Prolactinoma

- A Case of Multiple Endocrine Neoplasia Type 1 with Mutation in MENIN Gene.
- Se Eun Park, Eun Seok Kang, Hyun Joo Lee, So Hun Kim, Mi Young Do, Shin Ae Kang, Seung Jin Han, Hyeong Jin Kim, Chul Woo Ahn, Bong Soo Cha, Sung Kil Lim, Kyung Rae Kim, Il Jin Kim, Hyun Chul Lee
- J Korean Endocr Soc. 2005;20(1):71-77. Published online February 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.1.71
- 2,053 View
- 22 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Multiple endocrine neoplasia type 1(MEN 1) is an autosomal dominantly inherited syndrome, characterized by the combined occurrence of tumors of the parathyroid glands, endocrine pancreas, and anterior pituitary gland. The MENIN gene, which is a kind of tumor suppressor gene, is located at the chromosomal locus 11q13. It consists of one untranslated exon and nine exons encoding the menin protein. We report a case of a 22-yearss-old woman with MEN type 1, who was proven to have a mutation in the MENIN gene. The patient was admitted because of repeated hypoglycemia. The fasting plasma glucose level was 32mg/dL. Seventy two hours fasting test showed an the insulin/glucose ratio as 0.33. Endoscopic ultrasonography detected multiple masses on the pancreas. The arterial -stimulated venous sampling(ASVS) with calcium showed sudden step up of insulin at the head and tail portions of the pancreas. The sellar MRI showed a pituitary mass that produced prolactin. Instead of a pathologic diagnosis from operational specimen, the genetic analysis revealed a mutation in the MENIN 1 gene(exon 2, 200~201insAGCCC).
-
Citations
Citations to this article as recorded by- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1
Yoon Jung Chung, Sena Hwang, Jong Ju Jeong, Sun Yong Song, Se Hoon Kim, Yumie Rhee
Endocrinology and Metabolism.2014; 29(3): 270. CrossRef - A Case of Familial Multiple Endocrine Neoplasia Type 1 with a Novel Mutation in theMEN1Gene
Min Jung Kim, Eun Hee Kim, Mi-Seon Shin, Joo Hui Kim, Hee Kyung Na, Seong Joon Park, Sang Ah Lee, Eun Hee Koh, Woo Je Lee, Ki Ho Song, Joong-Yeol Park, Ki-Up Lee, Gu-Hwan Kim, Han-Wook Yoo, Min-Seon Kim
Endocrinology and Metabolism.2011; 26(2): 171. CrossRef - Somatic Mutational Analysis of MEN1 and Phenotypic Correlation in Sporadic Parathyroid Tumors
Young Su Chae, Hee Jin Kim, Sun Wook Kim, Myung-Chul Chang
Journal of the Korean Surgical Society.2009; 76(1): 15. CrossRef - Multiple Endocrine Neoplasia Type 1 with Multiple Leiomyomas Linked to a Novel Mutation in the MEN1 Gene
Heekyoung Choi, Sehyun Kim, Jae-Hoon Moon, Yoon Hee Lee, Yumie Rhee, Eun Seok Kang, Chul Woo Ahn, Bong Soo Cha, Eun Jig Lee, Kyung Rae Kim, Hyun Chul Lee, Seon Yong Jeong, Hyun Ju Kim, Sung-Kil Lim
Yonsei Medical Journal.2008; 49(4): 655. CrossRef - A Case of Familial Multiple Endocrine Neoplasia Type 1 with MEN1 Gene Mutation
Young Eun Jo, Yong-Jun Choi, Yun Kyung Kim, Sang Mi Ahn, Sun Hye Jung, Hae Jin Kim, Dae Jung Kim, Kwan Woo Lee, Ji-Hee Hong, Seon-Yong Jeong, Hyon J Kim, Yoon-Sok Chung
Journal of Korean Endocrine Society.2007; 22(1): 68. CrossRef - A Case of Familial Multiple Endocrine Neoplasia with MEN1 Gene Mutation
Hye-Young Sung, Yeon-Joo Chun, Hyeug Lee, Bum Jun Kwon, Kun Woo Park, Jung Min Lee, Sung Dae Moon, Sang Ah Chang, Je-Ho Han
Journal of Korean Endocrine Society.2006; 21(6): 560. CrossRef
- Genetic and Epigenetic Analysis in Korean Patients with Multiple Endocrine Neoplasia Type 1

- Comparison of Treatment Modalities in Hyperprolactinemia.
- Sun Hee Park, Hyeon Jeong Jeon, Do Joon Park, Kyong Soo Park, Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee
- J Korean Endocr Soc. 2002;17(1):32-42. Published online February 1, 2002
- 1,070 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Prolactinomas have been treated primarily with bromocriptine, a dopamine agonists, rather than by transsphenoidal pituitary adenomectomy. However, lower success rates, as well as intolerance or resistance to medical therapy, have been reported in some recent series. The purpose of this study was to compare the effects of surgery and bromocriptine in the treatment of prolactinomas patients. Also we investigated the natural history and effects of bromocriptine on patients with idiopathic hyperprolactinemia. METHEODS: We retrospectively compared the effects of treatment with surgery and with bromocriptine in 27 idiopathic hyperprolactinemia patients, 35 microprolactinoma patients and 61 macroprolactinoma patients. RESULTS: (1) In 14 patients with untreated idiopathic hyperprolactinemia, 8 (57%) achieved remission. In patients without remission, preoperative serum prolactin level was significantly higher than patients with remission (p<0.05). In 13 patients on bromocriptine, 11 (85%) achieved remission, while the other 2, taking bromocriptine irregularly because of side effects, had persistent hyperprolactinemia. (2) In 35 patients with microprolactinoma, 11 (30%) surgery as initial therapy and surgical remission was achieved in only 5 of the 11 (45%). In 23 patients on bromocriptine, 17 (74%) achieved remission. Among the 6 patients without remission, 5 patients took bromocriptine irregularly because of side effect. (3) In 61 patients with macroprolactinoma, 49 (80%) underwent surgery as initial therapy and surgical remission was achieved in only 9 of the 49 (18%). In 50 patients on bromocriptine, 30 (60%) achieved remission. Among the 20 patients without remission, 13 took bromocriptine irregularly because of side effect and 5 were resistant to bromocriptine. CONCLUSION: In idiopathic hyperprolactinemia, the requirement for medical treatment is doubtful because of a high tendency to ward spontaneous cure. In spite of the low success rate, surgery has been used as the primary therapy for prolactinoma in Korea. And yet, medical treatment with bromocriptine is superior to surgery. However, irrgular administration of medication due to drug side effects was the main cause of the low success rate. Therefore, the necessity for new drug development is emphasized


 KES
KES

 First
First Prev
Prev



