Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- The Benefits Of Continuous Glucose Monitoring In Pregnancy
- Jee Hee Yoo, Jae Hyeon Kim
- Endocrinol Metab. 2023;38(5):472-481. Published online October 11, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1805
- 2,626 View
- 222 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
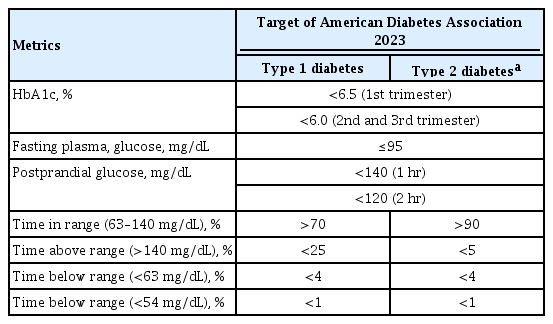
ePub - Previous studies have consistently demonstrated the positive effects of continuous glucose monitoring (CGM) on glycemic outcomes and complications of diabetes in people with type 1 diabetes. Guidelines now consider CGM to be an essential and cost-effective device for managing type 1 diabetes. As a result, insurance coverage for it is available. Evidence supporting CGM continues to grow and expand to broader populations, such as pregnant people with type 1 diabetes, people with type 2 diabetes treated only with basal insulin therapy, and even type 2 diabetes that does not require insulin treatment. However, despite the significant risk of hyperglycemia in pregnancy, which leads to complications in more than half of affected newborns, CGM indications and insurance coverage for those patients are unresolved. In this review article, we discuss the latest evidence for using CGM to offer glycemic control and reduce perinatal complications, along with its cost-effectiveness in pregestational type 1 and type 2 diabetes and gestational diabetes mellitus. In addition, we discuss future prospects for CGM coverage and indications based on this evidence.
-
Citations
Citations to this article as recorded by- Wearable devices for glucose monitoring: A review of state-of-the-art technologies and emerging trends
Mohammad Mansour, M. Saeed Darweesh, Ahmed Soltan
Alexandria Engineering Journal.2024; 89: 224. CrossRef
- Wearable devices for glucose monitoring: A review of state-of-the-art technologies and emerging trends

- Thyroid
- Diagnosis and Management of Thyroid Disease during Pregnancy and Postpartum: 2023 Revised Korean Thyroid Association Guidelines
- Hwa Young Ahn, Ka Hee Yi
- Endocrinol Metab. 2023;38(3):289-294. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1696
- 6,515 View
- 707 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
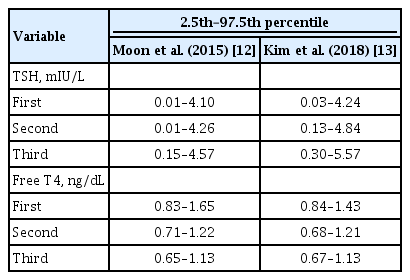
ePub - Thyroid hormone plays a critical role in fetal growth and development, and thyroid dysfunction during pregnancy is associated with several adverse outcomes, such as miscarriage and preterm birth. In this review, we introduce and explain three major changes in the revised Korean Thyroid Association (KTA) guidelines for the diagnosis and management of thyroid disease during pregnancy: first, the normal range of thyroid-stimulating hormone (TSH) during pregnancy; second, the treatment of subclinical hypothyroidism; and third, the management of euthyroid pregnant women with positive thyroid autoantibodies. The revised KTA guidelines adopt 4.0 mIU/L as the upper limit of TSH in the first trimester. A TSH level between 4.0 and 10.0 mIU/L, combined with free thyroxine (T4) within the normal range, is defined as subclinical hypothyroidism, and a TSH level over 10 mIU/L is defined as overt hypothyroidism regardless of the free T4 level. Levothyroxine treatment is recommended when the TSH level is higher than 4 mIU/L in subclinical hypothyroidism, regardless of thyroid peroxidase antibody positivity. However, thyroid hormone therapy to prevent miscarriage is not recommended in thyroid autoantibody-positive women with normal thyroid function.
-
Citations
Citations to this article as recorded by- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2023; 38(4): 381. CrossRef - Maternal isolated hypothyroxinemia in the first trimester is not associated with adverse pregnancy outcomes, except for macrosomia: a prospective cohort study in China
Jing Du, Linong Ji, Xiaomei Zhang, Ning Yuan, Jianbin Sun, Dan Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia

- Thyroid
- Prenatal Exposure to Per- and Polyfluoroalkyl Substances, Maternal Thyroid Dysfunction, and Child Autism Spectrum Disorder
- Hyeong-Moo Shin, Jiwon Oh, Rebecca J. Schmidt, Elizabeth N. Pearce
- Endocrinol Metab. 2022;37(6):819-829. Published online November 23, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1598

- 6,353 View
- 131 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Autism spectrum disorder (ASD), with its high economic and societal costs, is a growing public health concern whose prevalence has risen steadily over the last two decades. Although actual increased incidence versus improved diagnosis remains controversial, the increased prevalence of ASD suggests non-inherited factors as likely contributors. There is increasing epidemiologic evidence that abnormal maternal thyroid function during pregnancy is associated with increased risk of child ASD and other neurodevelopmental disorders. Prenatal exposure to endocrine-disrupting chemicals such as per- and polyfluoroalkyl substances (PFAS) is known to disrupt thyroid function and can affect early brain development; thus, thyroid dysfunction is hypothesized to mediate this relationship. The concept of a potential pathway from prenatal PFAS exposure through thyroid dysfunction to ASD etiology is not new; however, the extant literature on this topic is scant. The aim of this review is to evaluate and summarize reports with regard to potential mechanisms in this pathway.
-
Citations
Citations to this article as recorded by- Endocrine Disruptors and Thyroid Health
Elizabeth N. Pearce
Endocrine Practice.2024; 30(2): 172. CrossRef - Maternal Thyroid Dysfunction During Pregnancy as an Etiologic Factor in Autism Spectrum Disorder: Challenges and Opportunities for Research
Zoe B. Kaplan, Elizabeth N. Pearce, Sun Y. Lee, Hyeong-Moo Shin, Rebecca J. Schmidt
Thyroid®.2024; 34(2): 144. CrossRef - Effects of Endocrine-Disrupting Chemicals on Human Health
Jun Hyung Lee, Sung-Eun Cho
Laboratory Medicine Online.2023; 13(3): 129. CrossRef
- Endocrine Disruptors and Thyroid Health

- Thyroid
- Euthyroid Thyroperoxidase Antibody Positivity during Pregnancy, to Treat or Not to Treat?
- Tim I. M. Korevaar
- Endocrinol Metab. 2022;37(3):387-391. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.301
- 3,207 View
- 195 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
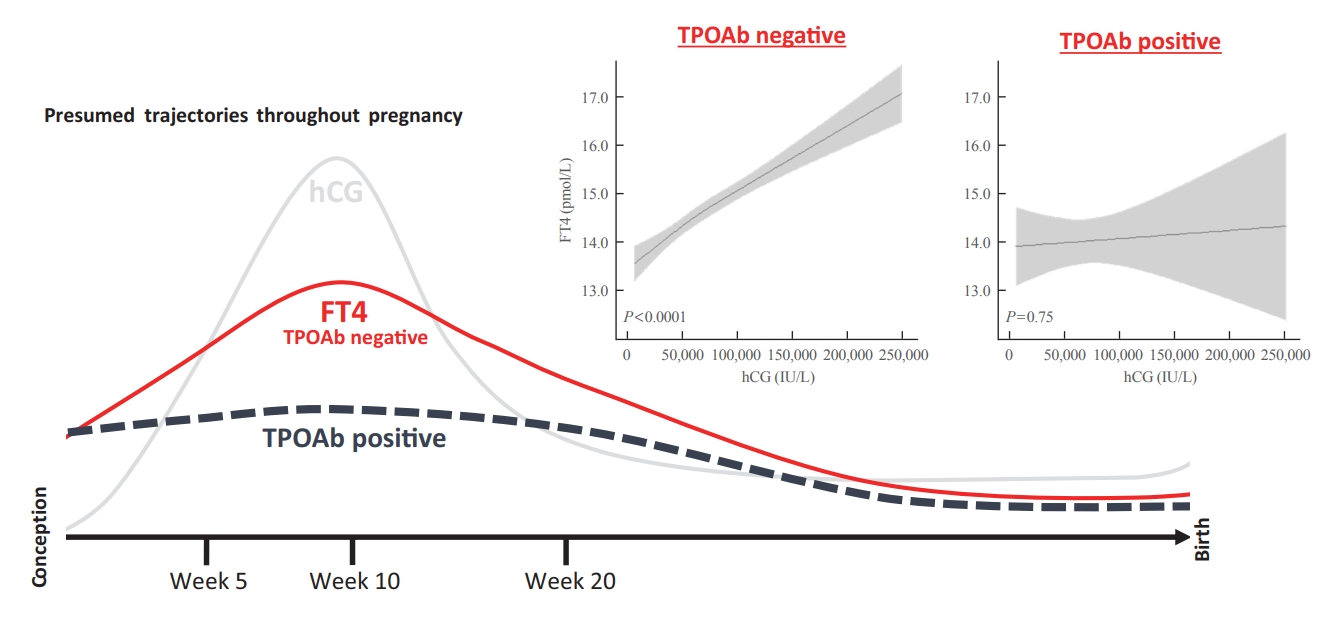
ePub - Thyroperoxidase antibody (TPOAb) positivity is a well-known risk factor for thyroid dysfunction during pregnancy and is associated with a suboptimal response to thyroidal stimulation by human chorionic gonadotropin. About 75% of TPOAb positive women are euthyroid and there seems to be a higher risk of predominantly miscarriage and preterm birth in this subgroup. Nonetheless, clinical decision making with regards to gestational levothyroxine treatment remains difficult due to a lack of large randomized trials. Future studies assessing dose-dependent associations and additional biomarkers that can distinguish low-risk from high-risk individuals will be key in disentangling the crude clinical data.
-
Citations
Citations to this article as recorded by- Thyroid autoimmunity and adverse pregnancy outcomes: A multiple center retrospective study
Yun Xu, Hui Chen, Meng Ren, Yu Gao, Kan Sun, Hongshi Wu, Rui Ding, Junhui Wang, Zheqing Li, Dan Liu, Zilian Wang, Li Yan
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Clinical Implications of Anti-thyroid Peroxidase Antibodies in Graves’ Disease in Basrah
Emad S Alhubaish, Nassar T Alibrahim, Abbas A Mansour
Cureus.2023;[Epub] CrossRef - Research Progress on the Influence of Autoimmune Thyroid Disease on Pregnancy Outcome
敏 李
Advances in Clinical Medicine.2023; 13(08): 13720. CrossRef - The Impact of Maternal Hypothyroidism during Pregnancy on Minipuberty in Boys
Karolina Kowalcze, Robert Krysiak, Anna Obuchowicz
Journal of Clinical Medicine.2023; 12(24): 7649. CrossRef
- Thyroid autoimmunity and adverse pregnancy outcomes: A multiple center retrospective study

- Diabetes, Obesity and Metabolism
- How Can We Adopt the Glucose Tolerance Test to Facilitate Predicting Pregnancy Outcome in Gestational Diabetes Mellitus?
- Kyeong Jin Kim, Nam Hoon Kim, Jimi Choi, Sin Gon Kim, Kyung Ju Lee
- Endocrinol Metab. 2021;36(5):988-996. Published online October 15, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1107
- 4,197 View
- 112 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
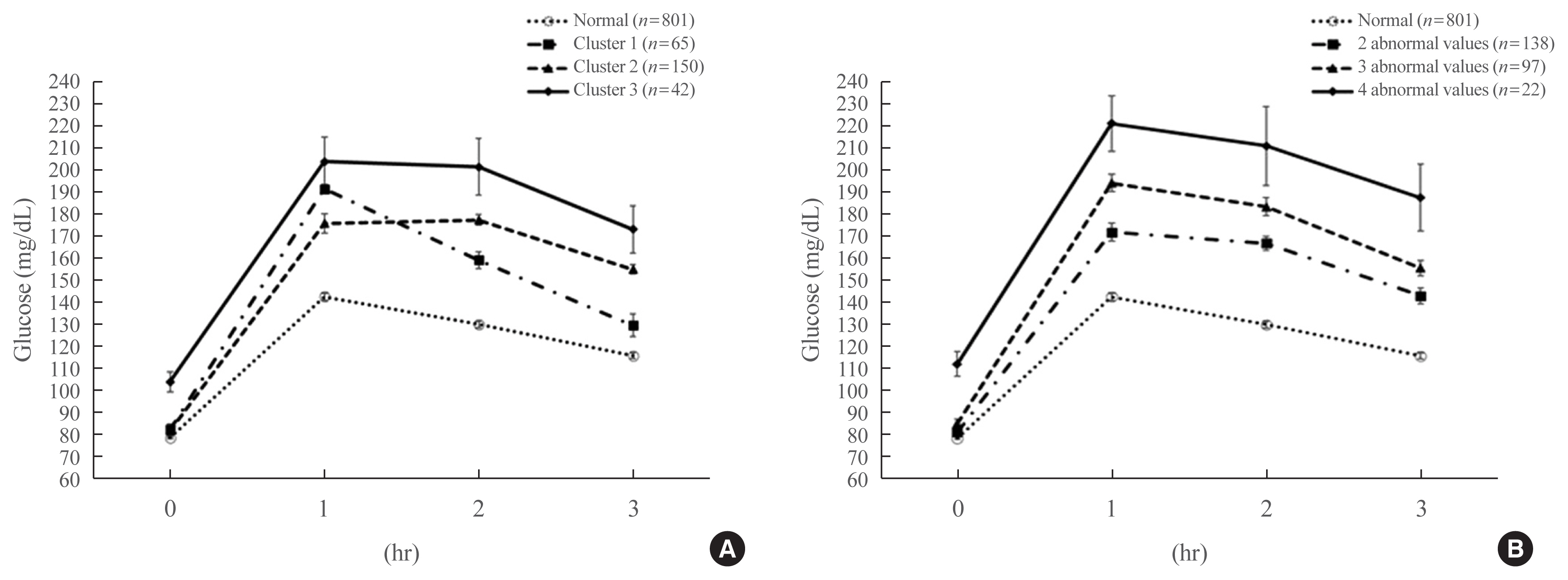
We investigated how 100-g oral glucose tolerance test (OGTT) results can be used to predict adverse pregnancy outcomes in gestational diabetes mellitus (GDM) patients.
Methods
We analyzed 1,059 pregnant women who completed the 100-g OGTT between 24 and 28 weeks of gestation. We compared the risk of adverse pregnancy outcomes according to OGTT patterns by latent profile analysis (LPA), numbers to meet the OGTT criteria, and area under the curve (AUC) of the OGTT graph. Adverse pregnancy outcomes were defined as a composite of preterm birth, macrosomia, large for gestational age, low APGAR score at 1 minute, and pregnancy-induced hypertension.
Results
Overall, 257 participants were diagnosed with GDM, with a median age of 34 years. An LPA led to three different clusters of OGTT patterns; however, there were no significant associations between the clusters and adverse pregnancy outcomes after adjusting for confounders. Notwithstanding, the risk of adverse pregnancy outcome increased with an increase in number to meet the OGTT criteria (P for trend=0.011); odds ratios in a full adjustment model were 1.27 (95% confidence interval [CI], 0.72 to 2.23), 2.16 (95% CI, 1.21 to 3.85), and 2.32 (95% CI, 0.66 to 8.15) in those meeting the 2, 3, and 4 criteria, respectively. The AUCs of the OGTT curves also distinguished the patients at risk of adverse pregnancy outcomes; the larger the AUC, the higher the risk (P for trend=0.007).
Conclusion
The total number of abnormal values and calculated AUCs for the 100-g OGTT may facilitate tailored management of patients with GDM by predicting adverse pregnancy outcomes. -
Citations
Citations to this article as recorded by- Risk factors combine in a complex manner in assessment for macrosomia
Yi-Wen Wang, Yan Chen, Yong-Jun Zhang
BMC Public Health.2023;[Epub] CrossRef - Association of the Severity of Hypertensive Disorders in Pregnancy with Birthweight, Childhood Obesity, and Blood Pressure at Age 7
Yan Chen, Yiwen Wang, Yanjun Li, Guodong Ding, Yongjun Zhang
Nutrients.2023; 15(14): 3104. CrossRef
- Risk factors combine in a complex manner in assessment for macrosomia

- Thyroid
- Antithyroid Drug Treatment in Graves’ Disease
- Jae Hoon Chung
- Endocrinol Metab. 2021;36(3):491-499. Published online June 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1070
- 4,985 View
- 338 Download
- 6 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
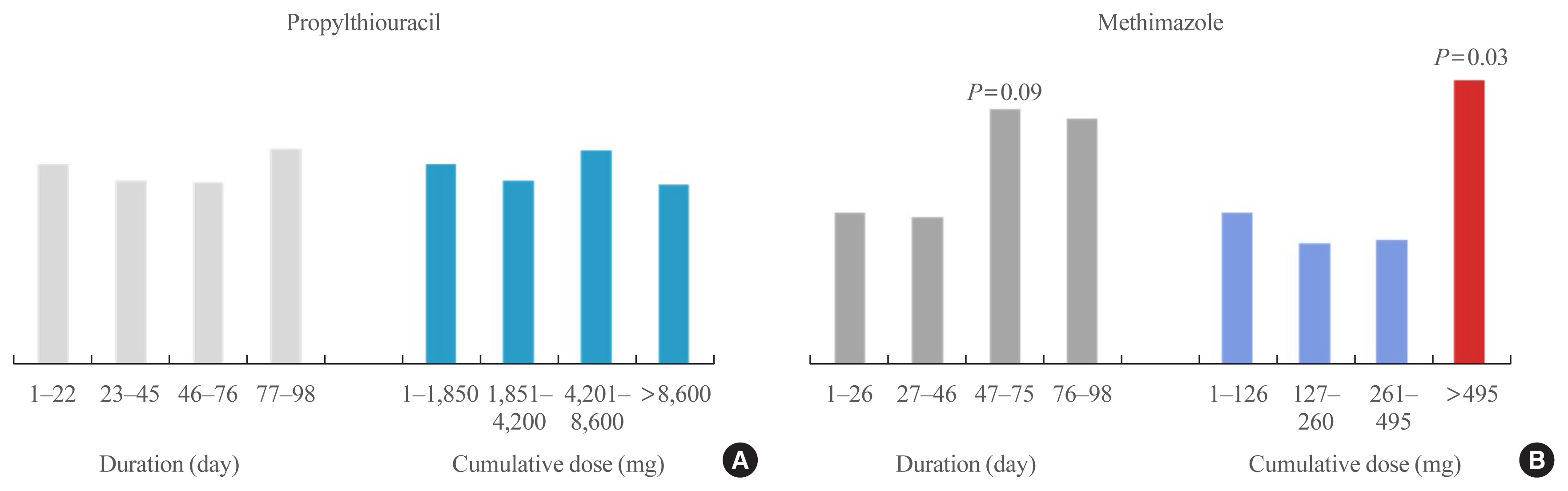
ePub - Graves’ disease is associated with thyrotropin (TSH) receptor stimulating antibody, for which there is no therapeutic agent. This disease is currently treated through inhibition of thyroid hormone synthesis or destruction of the thyroid gland. Recurrence after antithyroid drug (ATD) treatment is common. Recent studies have shown that the longer is the duration of use of ATD, the higher is the remission rate. Considering the relationship between clinical outcomes and iodine intake, recurrence of Graves’ disease is more common in iodine-deficient areas than in iodine-sufficient areas. Iodine restriction in an iodine-excessive area does not improve the effectiveness of ATD or increase remission rates. Recently, Danish and Korean nationwide studies noted significantly higher prevalence of birth defects in newborns exposed to ATD during the first trimester compared to that of those who did not have such exposure. The prevalence of birth defects was lowest when propylthiouracil (PTU) was used and decreased by only 0.15% when methimazole was changed to PTU in the first trimester. Therefore, it is best not to use ATD in the first trimester or to change to PTU before pregnancy.
-
Citations
Citations to this article as recorded by- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза
М. А. Дудина, С. А. Догадин, А. А. Савченко, И. И. Гвоздев
Ateroscleroz.2023; 18(4): 411. CrossRef - Application of oral inorganic iodine in the treatment of Graves’ disease
Yixuan Huang, Yihang Xu, Murong Xu, Xiaotong Zhao, Mingwei Chen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sex-specific risk factors associated with graves’ orbitopathy in Korean patients with newly diagnosed graves’ disease
Jooyoung Lee, Jinmo Kang, Hwa Young Ahn, Jeong Kyu Lee
Eye.2023; 37(16): 3382. CrossRef - Methimazole, an Effective Neutralizing Agent of the Sulfur Mustard Derivative 2-Chloroethyl Ethyl Sulfide
Albert Armoo, Tanner Diemer, Abigail Donkor, Jerrod Fedorchik, Severine Van slambrouck, Rachel Willand-Charnley, Brian A. Logue
ACS Bio & Med Chem Au.2023; 3(5): 448. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The influence of thionamides on intra-thyroidal uptake of 131I during radioiodine-131 treatment of Graves’ disease
Christian Happel, Benjamin Bockisch, Britta Leonhäuser, Amir Sabet, Frank Grünwald, Daniel Groener
Scientific Reports.2023;[Epub] CrossRef - Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
Endocrinology and Metabolism.2022; 37(2): 323. CrossRef - The chemiluminescent and enzymatic activity of blood neutrophils in patients with Graves' disease depending on hyperthyroidism compensation
M. A. Dudina, A. A. Savchenko, S. A. Dogadin, I. I. Gvozdev
Clinical and experimental thyroidology.2022; 18(1): 4. CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef
- Выраженность окислительного стресса и энзиматическая активность нейтрофилов крови у пациентов с болезнью Грейвса в зависимости от компенсации гипертиреоза

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
- Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
- Endocrinol Metab. 2021;36(3):628-636. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.948
- 5,805 View
- 170 Download
- 10 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the clinical characteristics of gestational diabetes mellitus (GDM) in Korea, using a nationwide database.
Methods
We analyzed 417,139 women who gave birth between 2011 and 2015 using the Korean National Health Information Database. They underwent the Korean National Health Screening Program within one year before pregnancy and were not prescribed drugs for diabetes nor diagnosed with diabetes mellitus before 280 days antepartum. Patients with GDM were defined as those who visited the outpatient clinic more than twice with GDM codes.
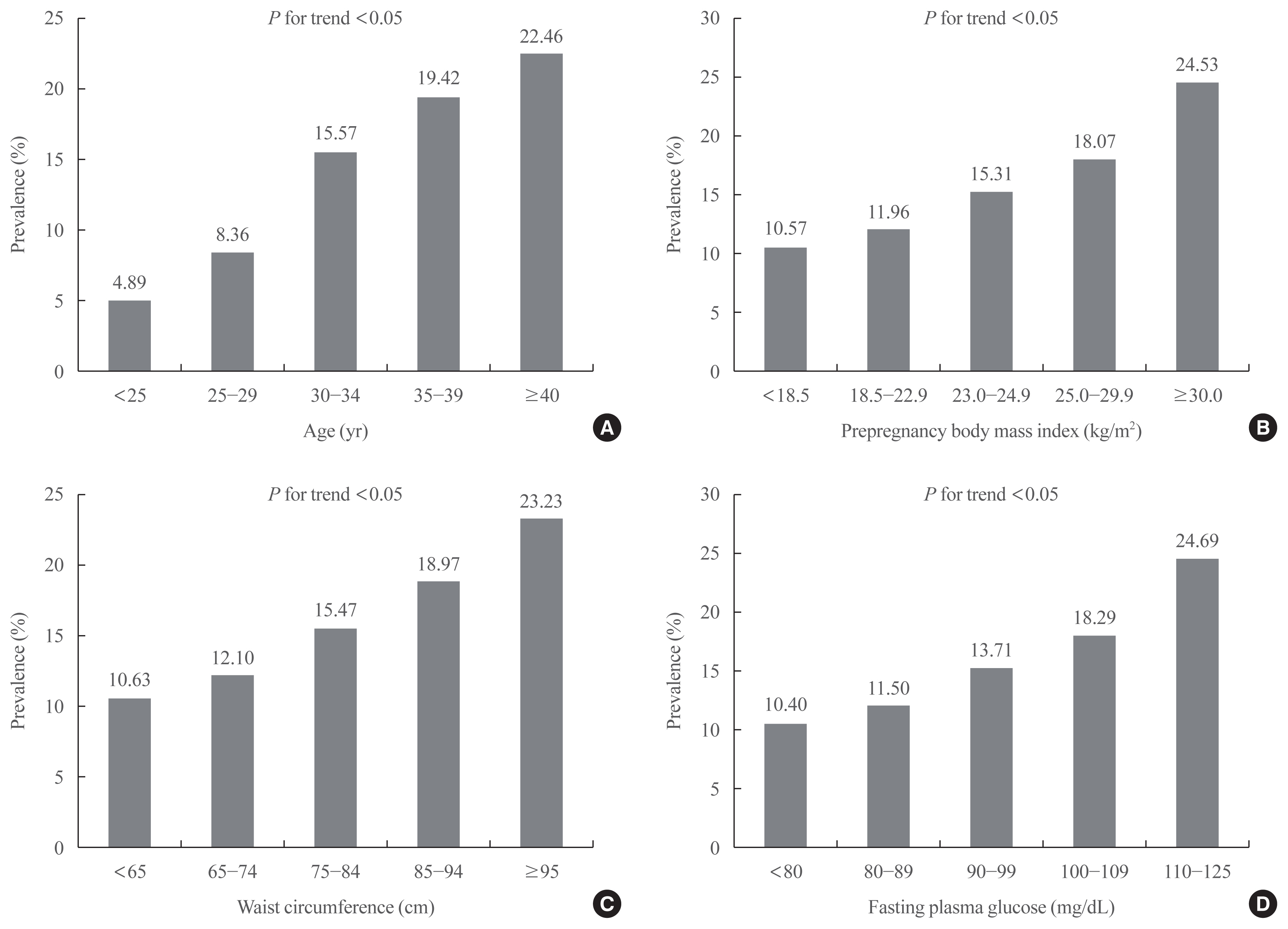
Results
The prevalence of GDM was 12.70% and increased with increasing maternal age, prepregnancy body mass index (BMI), waist circumference (WC), and fasting plasma glucose (FPG) (P for trend <0.05). As compared with those aged <25 years, the odds ratio for women with GDM aged ≥40 years were 4.804 (95% confidence interval [CI], 4.436 to 5.203) after adjustment for covariates. Women with prepregnancy BMI ≥30 kg/m2 were at 1.898 times (95% CI, 1.736 to 2.075) greater risk for GDM than those with prepregnancy BMI <18.5 kg/m2. Women with WC of ≥95 cm were at 1.158 times (95% CI, 1.029 to 1.191) greater risk for GDM than women with WC of less than 65 cm. High FPG, high income, smoking, and drinking were associated with an elevated risk of GDM.
Conclusion
The prevalence of GDM in Korean women increased up to 12.70% during 2011 to 2015. These data suggest the importance of GDM screening and prevention in high-risk groups in Korea. -
Citations
Citations to this article as recorded by- Relationships between triglyceride-glucose index and incident gestational diabetes mellitus: a prospective cohort study of a Korean population using publicly available data
Zihe Mo, Changchun Cao, Yong Han, Haofei Hu, Yongcheng He, Xin Zuo
Frontiers in Public Health.2024;[Epub] CrossRef - Glucose tolerance test with a single abnormal value as a predictor of type 2 diabetes mellitus: a multicenter retrospective study
Seon Ui Lee, Subeen Hong, Sae Kyung Choi, Su Mi Kim, Jae Eun Shin, Ki Cheol Kil, Yeon Hee Kim, Jeong Ha Wie, Yun Sung Jo, Hyun Sun Ko
Scientific Reports.2024;[Epub] CrossRef - Exploring the influence of microbiota on gestational diabetes and its potential as a biomarker
Suresh Bokoliya, Stephanie McClellan, Yanjiao Zhou, Nini Fan
Frontiers in Bacteriology.2024;[Epub] CrossRef - Serum afamin levels in predicting gestational diabetes mellitus and preeclampsia: A systematic review and meta-analysis
Ying Yuan, Wenyin He, Xuejiao Fan, Junyu Liang, Zhen Cao, Lei Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Smoking during pregnancy and gestational diabetes mellitus: a systematic review and meta-analysis
Kleoniki I. Athanasiadou, Stavroula A. Paschou, Evgenia Papakonstantinou, Vasiliki Vasileiou, Fotini Kanouta, Paraskevi Kazakou, Katerina Stefanaki, Georgia N. Kassi, Theodora Psaltopoulou, Dimitrios G. Goulis, Eleni Anastasiou
Endocrine.2023; 82(2): 250. CrossRef - Association between the triglyceride to high-density lipoprotein cholesterol ratio and the risk of gestational diabetes mellitus: a second analysis based on data from a prospective cohort study
Yun You, Haofei Hu, Changchun Cao, Yong Han, Jie Tang, Weihua Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study
Bingbing Guo, Jingjing Pei, Yin Xu, Yajie Wang, Xinye Jiang
Scientific Reports.2023;[Epub] CrossRef - The Benefits Of Continuous Glucose Monitoring In Pregnancy
Jee Hee Yoo, Jae Hyeon Kim
Endocrinology and Metabolism.2023; 38(5): 472. CrossRef - Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(1): 3. CrossRef - Current Trends of Big Data Research Using the Korean National Health Information Database
Mee Kyoung Kim, Kyungdo Han, Seung-Hwan Lee
Diabetes & Metabolism Journal.2022; 46(4): 552. CrossRef - Maternal Gestational Diabetes Influences DNA Methylation in the Serotonin System in the Human Placenta
Jae Yen Song, Kyung Eun Lee, Eun Jeong Byeon, Jieun Choi, Sa Jin Kim, Jae Eun Shin
Life.2022; 12(11): 1869. CrossRef - Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus (Diabetes Metab J 2021;45:547-57)
Kyung-Soo Kim
Diabetes & Metabolism Journal.2021; 45(6): 966. CrossRef
- Relationships between triglyceride-glucose index and incident gestational diabetes mellitus: a prospective cohort study of a Korean population using publicly available data

- Changes of Thyroid Function According to the Stages of Normal Pregnancy.
- W B Kim, B H Yoon, J H Chung, S I Lee, M S Kim, T G Oh, B Y Cho, H K Lee, C S Koh
- J Korean Endocr Soc. 1994;9(3):183-189. Published online November 6, 2019
- 1,108 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - It is well known that normal pregnancy is accompanied by a rise in serum concentrations of thyroxine-binding globulin(TBG) and human chorionic gonadotropin (hCG). Alterations of biochemical parameters of thyroid function are recognized during gestation and sensitive tests to evaluate the alterations easily are required. Therefore, a cross-sectional study was undertaken in 140 healthy pregnant women to evaluate the efficacy of free T_4 measured by 2-step RIA compared to other thyroid function tests and to confirm the changes of thyroid function according to the stages of normal pregnancy.The sensitivities of free T_4 index, free T_4(by 2-step RIA), T_3 and TSH were realtively high(99.3%, 93.6%, 92.9%, 83.6%, respectively) compared to those of T_4 and T_3 bead upgake(49.3%, 21.4%) during all stages of pregnancy. There were positive correlations between free T_4 index and free T_4 or total T_4(r=0.68, r=0.72; p<0.001). The values of free T_4 index sharply decreased from 3.22+-0.10(meam +-SEM) during 6th-12th week to an plateau after 16th-20th week of gestation(p<0.01). The serum concentrations free T_4 and T_3 bead uptake also significantly decreased from 1.65+-0.05 ng/dl, 24.7+- 0.7% during 6th-12th week to an plateau after 16th-20th week of gestation, respectively(p<0.001), No differences were found in the changes of serum concentrations of T_3, T_4 and TSH according to the stages of pregnancy.In conclusion, it is adequate to measure some tests including free T_4 index and free T_4 to evaluate thyroid function during pregnancy. The thyroid physiology and changes of thyroid function according to the stages of pregnancy should be considered in the interpretation of thyroid function status during pregnancy.

- A Case of Adrenal adenoma Associated with Pregnancy.
- Jung Gyn Kim, Jang Sik Choo, Yang Kyu Lee, Bung Chul Han, Seung Bum Jin, Sang Gi Yang, Chang Sup Song, Me Gyung Sin
- J Korean Endocr Soc. 1994;9(1):39-45. Published online November 6, 2019
- 1,275 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - We experienced a case of aldosterone and cortisol secreting adrenal adenoma associated with pregnancy in a 23 year old female patient.The patient complained of severe thoraco-lumbar pain, weight gain, sweating, anxiety, and mild abdominal discomfort. On physical findings, hypertension, tachycardia, facial plethora, moon face, buffalo hump and truncal obesity were found.

- Thyroid
- Thyroid-Stimulating Hormone Reference Ranges in the First Trimester of Pregnancy in an Iodine-Sufficient Country
- Carmen Castillo, Nicole Lustig, Paula Margozzini, Andrea Gomez, María Paulina Rojas, Santiago Muzzo, Lorena Mosso
- Endocrinol Metab. 2018;33(4):466-472. Published online November 30, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.4.466
- 6,124 View
- 86 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Thyroid dysfunction is associated with negative neonatal and obstetric outcomes. Large differences in thyroid function reference intervals exist across different populations. These differences can be explained by population-specific factors, such as iodine status. Many countries in Latin America report iodine sufficiency, but relatively few countries have published up-to-date data on iodine levels and thyroid function in the overall population, and especially in pregnant women. We evaluated the iodine status of pregnant women in Chile and determined thyroid hormone reference ranges in this population.
Methods This was a prospective observational study of healthy Chilean women at their first prenatal visit before week 14. Thyroid-stimulating hormone (TSH), total thyroxine (T4), free T4, antithyroid peroxidase antibody (TPOAb), and iodine levels from spot urine samples were measured. Iodine status and the reference ranges for TSH were calculated.
Results A total of 1,022 pregnant women in the first trimester were selected. Urinary iodine levels were measured in 302 randomly-selected women. The median urinary iodine concentration was 173.45 µg/L (interquartile range, 108.11 to 249.35).The reference ranges of TSH were calculated in 670 patients selected according to the National Academy of Clinical Biochemistry guidelines. The median TSH level was 1.88 µIU/mL (2.5th percentile: 0.13 to 97.5th percentile: 5.37). Using the reference range in the 1,022 women, the prevalence of clinical hypothyroidism was 1.76%, and that of subclinical hypothyroidism was 3.92%. TPOAb positivity was more common in women with TSH levels above 3.5 µIU/mL.
Conclusion We found adequate iodine intake and a right-shifted distribution of serum TSH levels in pregnant women in Chile. The prevalence of hypothyroidism in our sample of pregnant women was higher than has been described in the literature.
-
Citations
Citations to this article as recorded by- Long-term impact of hypothyroidism during gestation and lactation on the mammary gland
Fiorella Campo Verde Arboccó, Fabio A. Persia, Leila Zyla, Nicolás Bernal, Verónica C. Sasso, Flavia Santiano, Silvina Gomez, Flavia Bruna, Virginia Pistone-Creydt, Constanza Lopez-Fontana, Graciela A. Jahn, María Belén Hapon, Ruben W. Carón
Journal of Developmental Origins of Health and Disease.2023; 14(1): 122. CrossRef - Evaluation of first and second trimester maternal thyroid profile on the prediction of gestational diabetes mellitus and post load glycemia
Daniela Mennickent, Bernel Ortega-Contreras, Sebastián Gutiérrez-Vega, Erica Castro, Andrés Rodríguez, Juan Araya, Enrique Guzmán-Gutiérrez, Surangi Nilanka Jayakody Mudiyanselage
PLOS ONE.2023; 18(1): e0280513. CrossRef - Clinical and histopathological features of follicular thyroid cancer in Chile
René Díaz, José Miguel Domínguez, Hernán Tala, Roberto Olmos, Pedro Pineda, Daniela Olivarí, Marcela Jiménez, Ximena Mimica, Alejandra Lanas, Gerson Ocares, Jorge Sapunar
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Effect of the Cut-Off Level for Thyroid-Stimulating Hormone on the Prevalence of Subclinical Hypothyroidism among Infertile Mexican Women
Lidia Arce-Sánchez, Salvatore Giovanni Vitale, Claudia Montserrat Flores-Robles, Myrna Souraye Godines-Enriquez, Marco Noventa, Carmen Marcela Urquia-Figueroa, Nayeli Martínez-Cruz, Guadalupe Estrada-Gutierrez, Salvador Espino y Sosa, José Romo-Yañez, Ara
Diagnostics.2021; 11(3): 417. CrossRef - Subclinical hypothyroidism in pregnancy
Freddy J.K. Toloza, Sanaz Abedzadeh-Anaraki, Spyridoula Maraka
Current Opinion in Endocrinology, Diabetes & Obesity.2019; 26(5): 225. CrossRef - Letter: Thyroid-Stimulating Hormone Reference Ranges in the First Trimester of Pregnancy in an Iodine-Sufficient Country (Endocrinol Metab 2018;33:466-72, Carmen Castillo et al.)
Hyemi Kwon
Endocrinology and Metabolism.2019; 34(1): 93. CrossRef - Response: Thyroid-Stimulating Hormone Reference Ranges in the First Trimester of Pregnancy in an Iodine-Sufficient Country (Endocrinol Metab 2018;33:466–72, Carmen Castillo et al.)
Lorena Mosso
Endocrinology and Metabolism.2019; 34(2): 213. CrossRef - Thyroid-Stimulating Hormone Reference Ranges in Early Pregnancy: Possible Influence of Iodine Status
Tae Yong Kim
Endocrinology and Metabolism.2018; 33(4): 445. CrossRef
- Long-term impact of hypothyroidism during gestation and lactation on the mammary gland

- Clinical Study
- Effects of Maternal Iodine Status during Pregnancy and Lactation on Maternal Thyroid Function and Offspring Growth and Development: A Prospective Study Protocol for the Ideal Breast Milk Cohort
- Young Ah Lee, Sun Wook Cho, Ho Kyung Sung, Kyungsik Kim, Young Shin Song, Sin Je Moon, Jung Won Oh, Dal Lae Ju, Sooyeon Choi, Sang Hoon Song, Gi Jeong Cheon, Young Joo Park, Choong Ho Shin, Sue K. Park, Jong Kwan Jun, June-Key Chung
- Endocrinol Metab. 2018;33(3):395-402. Published online September 18, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.395
- 4,926 View
- 84 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Iodine is an intrinsic element of thyroid hormone, which is essential for childhood growth and development. The Ideal Breast Milk (IBM) cohort study aims to evaluate the effects of maternal iodine status during pregnancy and lactation on maternal thyroid function, offspring growth and development, and offspring thyroid function.
Methods The IBM cohort study recruited pregnant women from Seoul National University Hospital between June 2016 and August 2017, followed by enrollment of their offspring after delivery. For the maternal participants, iodine status is evaluated by urinary iodine concentration (UIC) and dietary records in the third trimester and at 3 to 4 weeks and 12 to 15 months postpartum. For the child participants, cord blood sampling and UIC measurements are performed at birth. At 3 to 4 weeks of age, UIC and breastmilk iodine concentrations are measured. At 12 to 15 months of age, growth and development are assessed and measurements of UIC, a thyroid function test, and ultrasonography are performed.
Results A total of 198 pregnant women in their third trimester were recruited. Their mean age was 35.1±3.5 years, and 78 (39.4%) of them were pregnant with twins. Thirty-three (16.7%) of them had a previous history of thyroid disease.
Conclusion Korea is an iodine-replete area. In particular, lactating women in Korea are commonly exposed to excess iodine due to the traditional practice of consuming brown seaweed soup postpartum. The study of the IBM cohort is expected to contribute to developing guidelines for optimal iodine nutrition in pregnant or lactating women.
-
Citations
Citations to this article as recorded by- High intakes of iodine among women during pregnancy and the postpartum period has no adverse effect on thyroid function
Dal Lae Ju, Sun Wook Cho, Chae Won Chung, Young Ah Lee, Gi Jeong Cheon, Young Joo Park, Choong Ho Shin, Jong Kwan Jun, June-Key Chung, Sue K. Park, YoonJu Song
European Journal of Nutrition.2023; 62(1): 239. CrossRef - Associations between maternal thyroid function in pregnancy and child neurodevelopmental outcomes at 20 months in the Seychelles Child Development Study, Nutrition Cohort 2 (SCDS NC2)
Anna M. Monaghan, Maria S. Mulhern, Emeir M. Mc Sorley, J.J. Strain, Theresa Winter, Edwin van Wijngaarden, Gary J. Myers, Philip W. Davidson, Conrad Shamlaye, Jude Gedeon, Alison J. Yeates
Journal of Nutritional Science.2021;[Epub] CrossRef
- High intakes of iodine among women during pregnancy and the postpartum period has no adverse effect on thyroid function

- Thyroid
- Update on the Management of Thyroid Disease during Pregnancy
- Chang Hoon Yim
- Endocrinol Metab. 2016;31(3):386-391. Published online August 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.386
- 4,102 View
- 74 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Thyroid dysfunction during pregnancy can result in serious complications for both the mother and infant; however, these complications can be prevented by optimal treatment of maternal overt thyroid dysfunction. Although several studies have demonstrated that maternal subclinical hypothyroidism is associated with obstetric complications and neurocognitive impairments in offspring, there is limited evidence that levothyroxine treatment can improve these complications. Therefore, most professional societies do not recommend universal screening for thyroid dysfunction during pregnancy, and instead recommend a case-finding approach in which only high-risk women are tested. However, recent studies have estimated that targeted thyroid function testing misses approximately 30% to 55% of hypothyroidism cases in pregnant women, and some associations and researchers have recommended universal screening of pregnant women to facilitate the early detection and treatment of overt hypothyroidism. This review summarizes recent data on thyroid function test changes, thyroid functional disorder management, and thyroid screening during pregnancy.
-
Citations
Citations to this article as recorded by- The Effect of Inflammatory Markers in the Hemogram Parameters of Pregnant Women with Thyroid Disease on Obstetric and Neonatal Outcomes
Funda DEMİREL, Ünal TURKAY
Düzce Tıp Fakültesi Dergisi.2023; 25(3): 231. CrossRef - Enfermedades tiroideas y embarazo en una unidad de cuidados intensivos. Experiencia 2014-2019
J.G. Vázquez-Rodríguez, A.C. Andrade-Rodríguez
Clínica e Investigación en Ginecología y Obstetricia.2021; 48(3): 100662. CrossRef - Decreased Expression of Ileal Thyroid Hormone Transporters in a Hypothyroid Patient: A Case Report
Chae Won Chung, Eun Young Mo, Gyung Seo Jung, Yoo Hyung Kim, Sun Wook Cho, Do Joon Park, Jeong Mo Bae, Young Joo Park
Frontiers in Endocrinology.2021;[Epub] CrossRef - Tiroidectomía en paciente embarazada con enfermedad de Graves sin respuesta a tratamiento médico: reporte de caso
Elly Morros González, Leonardo Javier Rojas Melo, Viviana Cruz Ramírez, Angélica Imitola
Universitas Médica.2020;[Epub] CrossRef - Thyroid disorders in subfertility and early pregnancy
Samantha Anandappa, Mamta Joshi, Lukasz Polanski, Paul V. Carroll
Therapeutic Advances in Endocrinology and Metabolism.2020; 11: 204201882094585. CrossRef - Addressing thyroid dysfunction in pregnancy
Teodora Onciu, Remus Şipoş
Medic.ro.2020; 3(135): 48. CrossRef - Antenatal/early postnatal hypothyroidism increases the contribution of Rho-kinase to contractile responses of mesenteric and skeletal muscle arteries in adult rats
Dina K. Gaynullina, Svetlana I. Sofronova, Anastasia A. Shvetsova, Ekaterina K. Selivanova, Anna P. Sharova, Andrey A. Martyanov, Olga S. Tarasova
Pediatric Research.2018; 84(1): 112. CrossRef - Voluntary exercise training restores anticontractile effect of NO in coronary arteries of adult rats with antenatal/early postnatal hypothyroidism
D.K. Gaynullina, A.A. Borzykh, S.I. Sofronova, E.K. Selivanova, A.A. Shvetsova, A.A. Martyanov, I.V. Kuzmin, O.S. Tarasova
Nitric Oxide.2018; 74: 10. CrossRef - Impact of positive thyroid autoimmunity on pregnant women with subclinical hypothyroidism
Cristina López-Tinoco, Amparo Rodríguez-Mengual, Almudena Lara-Barea, Julia Barcala, Laura Larrán, Ana Saez-Benito, Manuel Aguilar-Diosdado
Endocrinología, Diabetes y Nutrición (English ed.).2018; 65(3): 150. CrossRef - Impacto de la autoinmunidad antitiroidea positiva en gestantes con hipotiroidismo subclínico
Cristina López-Tinoco, Amparo Rodríguez-Mengual, Almudena Lara-Barea, Julia Barcala, Laura Larrán, Ana Saez-Benito, Manuel Aguilar-Diosdado
Endocrinología, Diabetes y Nutrición.2018; 65(3): 150. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Maternal hypothyroidism: An overview of current experimental models
Mahboubeh Ghanbari, Asghar Ghasemi
Life Sciences.2017; 187: 1. CrossRef
- The Effect of Inflammatory Markers in the Hemogram Parameters of Pregnant Women with Thyroid Disease on Obstetric and Neonatal Outcomes

- A Case of Hypothyroidism in Remission during Pregnancy.
- Ha Do Song, Eun Jin Han, Sung Ja Lee, Ji Hoon Yang, So Young Park, Sung Hoon Kim, Ki Ok Han, Hyun Koo Yoon, Chang Hoon Yim
- Endocrinol Metab. 2012;27(4):295-298. Published online December 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.4.295
- 2,169 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - Hypothyroidism should be treated in pregnancy, because it has been associated with an increased risk of adverse pregnancy complications, as well as detrimental effects upon fetal neurocognitive development. The goal of L-thyroxine (LT4) treatment is to normalize maternal serum TSH values within the trimester-specific pregnancy reference range. 50% to 85% of hypothyroid women being treated with exogenous LT4 need to increase the dose during pregnancy. In this study, we report a case of a 29-year-old woman with hypothyroidism who had been in remission and discontinued LT4 treatment during her pregnancy. Three months after delivery she had a relapse of hypothyroidism and was retreated with LT4. Many factors can influence the gestational requirement for LT4, therefore maternal serum TSH should be monitored and the LT4 dose should be adjusted in pregnant patients with treated hypothyroidism.

- A Case of Cushing's Disease in Pregnancy.
- Jeong Tae Kim, Mun Hyuk Sung, Woo Ri Park, Jeong Ho Han, Hye Suk Han, Young Kwang Sim, Tae Gun Oh, Hyun Jeong Jeon
- Endocrinol Metab. 2011;26(4):348-354. Published online December 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.4.348
- 1,884 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - Developing Cushing's syndrome during pregnancy is rare because menstruation is irregular and hypercortisolism causes infertility. Developing Cushing's disease during pregnancy is very rare because there is even less ovulation than those with the adrenal adenoma. The clinical manifestations of Cushing's syndrome may easily be missed during pregnancy as the features of weight gain, hypertension, and hyperglycemia overlap with those that occur during a pregnancy. Diagnosing Cushing's syndrome during a pregnancy is complex because the biochemical features are obscured by the natural changes in the hypothalamic-pituitary-adrenal axis that occur during pregnancy. Having Cushing's syndrome during a pregnancy results in increased fetal and maternal complications, so early diagnosis and treatment are critical. We report the clinical and endocrine findings of a pregnant women with Cushing's disease who underwent transsphenoidal surgery after delivery.

- Pregnancy-induced Osteoporosis Combined with Multiple Compression Fractures: A Case Report.
- Ji Eun Lee, Jin Sun Jang, Sun Hee Ko, Min Hee Kim, Dong Jun Lim, Moo Il Kang, Bong Yun Cha, Sook Hee Hong, Ja seong Bae, Kyeoung Sik Ryu
- Endocrinol Metab. 2011;26(2):150-154. Published online June 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.2.150
- 2,073 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pregnancy associated osteoporosis (PAO) is a rare condition. It may affect women during pregnancy or after the delivery and it can induce severe back pain. Physicians can find multiple compression fractures on the plain images of these patients. However, little is known about PAO, including the prevalence, the cause, the risk factors and the prognosis. Herein we report on a case of PAO in a 38-year-old female who suffered from severe back pain induced by multiple vertebral compression fractures. After excluding the possibility of unknown malignancy, the patient underwent vertebroplasty to improve the clinical symptom. The bone biopsy results confirmed multiple benign acute compression fractures. The patient was treated with oral bisphosphonate, calcium and vitamin D. She showed clinical improvement without developing any additional vertebral fracture. When young women during pregnancy or just after the delivery complain of persistent back pain, PAO should be considered in the differential diagnosis, and early recognition and treatment are needed for PAO.
-
Citations
Citations to this article as recorded by- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures
Eun Yeong Choe, Je Eun Song, Kyeong Hye Park, Hannah Seok, Eun Jig Lee, Sung-Kil Lim, Yumie Rhee
Journal of Bone and Mineral Metabolism.2012; 30(5): 596. CrossRef
- Effect of teriparatide on pregnancy and lactation-associated osteoporosis with multiple vertebral fractures


 KES
KES

 First
First Prev
Prev



