Search
- Page Path
- HOME > Search
Review Article
- Calcium & bone metabolism
- Bone Loss after Solid Organ Transplantation: A Review of Organ-Specific Considerations
- Kyoung Jin Kim, Jeonghoon Ha, Sang Wan Kim, Jung-Eun Kim, Sihoon Lee, Han Seok Choi, Namki Hong, Sung Hye Kong, Seong Hee Ahn, So Young Park, Ki-Hyun Baek, on Behalf of Metabolic Bone Disease Study Group of Korean Endocrine Society
- Endocrinol Metab. 2024;39(2):267-282. Published online April 25, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1939

- 35 View
- 2 Download
-
 Abstract
Abstract
 PDF
PDF - This review article investigates solid organ transplantation-induced osteoporosis, a critical yet often overlooked issue, emphasizing its significance in post-transplant care. The initial sections provide a comprehensive understanding of the prevalence and multifactorial pathogenesis of transplantation osteoporosis, including factors such as deteriorating post-transplantation health, hormonal changes, and the impact of immunosuppressive medications. Furthermore, the review is dedicated to organ-specific considerations in transplantation osteoporosis, with separate analyses for kidney, liver, heart, and lung transplantations. Each section elucidates the unique challenges and management strategies pertinent to transplantation osteoporosis in relation to each organ type, highlighting the necessity of an organ-specific approach to fully understand the diverse manifestations and implications of transplantation osteoporosis. This review underscores the importance of this topic in transplant medicine, aiming to enhance awareness and knowledge among clinicians and researchers. By comprehensively examining transplantation osteoporosis, this study contributes to the development of improved management and care strategies, ultimately leading to improved patient outcomes in this vulnerable group. This detailed review serves as an essential resource for those involved in the complex multidisciplinary care of transplant recipients.

Original Article
- Calcium & bone metabolism
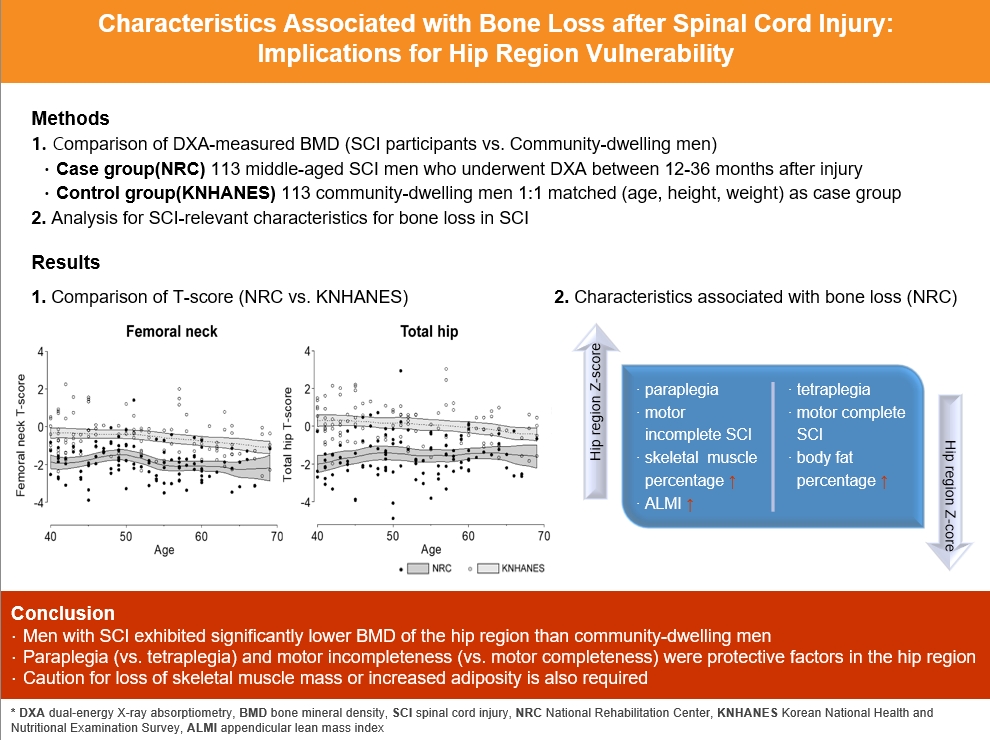
- Characteristics Associated with Bone Loss after Spinal Cord Injury: Implications for Hip Region Vulnerability
- Sora Han, Sungjae Shin, Onyoo Kim, Namki Hong
- Endocrinol Metab. 2023;38(5):578-587. Published online October 10, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1795
- 1,297 View
- 52 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
In individuals with spinal cord injury (SCI), bone loss progresses rapidly to the area below the level of injury, leading to an increased risk of fracture. However, there are limited data regarding SCI-relevant characteristics for bone loss and the degree of bone loss in individuals with SCI compared with that in non-SCI community-dwelling adults.
Methods
Data from men with SCI who underwent dual-energy X-ray absorptiometry at the National Rehabilitation Center (2008 to 2020) between 12 and 36 months after injury were collected and analyzed. Community-dwelling men were matched 1:1 for age, height, and weight as the control group, using data from the Korea National Health and Nutrition Examination Survey (KNHANES, 2008 to 2011).
Results
A comparison of the SCI and the matched control group revealed significantly lower hip region T-scores in the SCI group, whereas the lumbar spine T-score did not differ between groups. Among the 113 men with SCI, the paraplegia group exhibited significantly higher Z-scores of the hip region than the tetraplegia group. Participants with motor-incomplete SCI showed relatively preserved Z-scores of the hip region compared to those of the lumbar region. Moreover, in participants with SCI, the percentage of skeletal muscle displayed a moderate positive correlation with femoral neck Z-scores.
Conclusion
Men with SCI exhibited significantly lower bone mineral density of the hip region than community-dwelling men. Paraplegia rather than tetraplegia, and motor incompleteness rather than motor completeness were protective factors in the hip region. Caution for loss of skeletal muscle mass or increased adiposity is also required.

Review Articles
- Calcium & bone metabolism
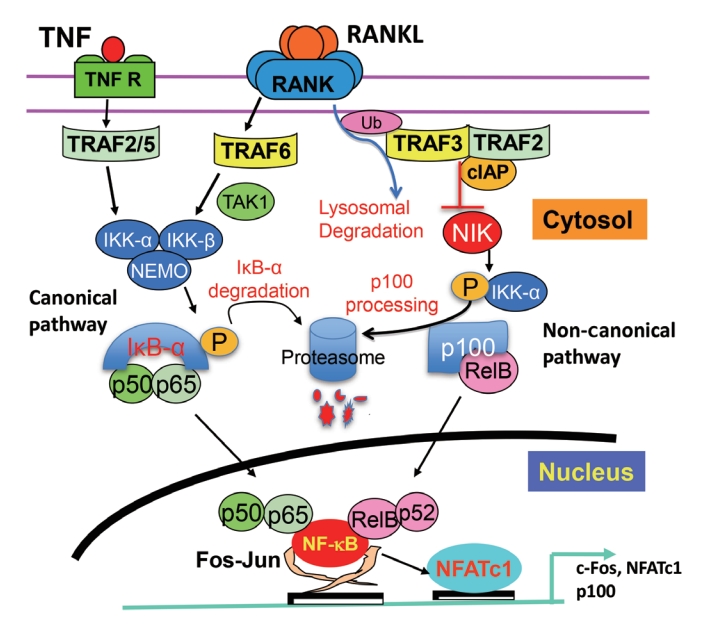
- Nuclear Factor-Kappa B Regulation of Osteoclastogenesis and Osteoblastogenesis
- Brendan F. Boyce, Jinbo Li, Zhenqiang Yao, Lianping Xing
- Endocrinol Metab. 2023;38(5):504-521. Published online September 26, 2023
- DOI: https://doi.org/10.3803/EnM.2023.501
- 2,152 View
- 101 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Maintenance of skeletal integrity requires the coordinated activity of multinucleated bone-resorbing osteoclasts and bone-forming osteoblasts. Osteoclasts form resorption lacunae on bone surfaces in response to cytokines by fusion of precursor cells. Osteoblasts are derived from mesenchymal precursors and lay down new bone in resorption lacunae during bone remodeling. Nuclear factorkappa B (NF-κB) signaling regulates osteoclast and osteoblast formation and is activated in osteoclast precursors in response to the essential osteoclastogenic cytokine, receptor activator of NF-κB ligand (RANKL), which can also control osteoblast formation through RANK-RANKL reverse signaling in osteoblast precursors. RANKL and some pro-inflammatory cytokines, including tumor necrosis factor (TNF), activate NF-κB signaling to positively regulate osteoclast formation and functions. However, these cytokines also limit osteoclast and osteoblast formation through NF-κB signaling molecules, including TNF receptor-associated factors (TRAFs). TRAF6 mediates RANKL-induced osteoclast formation through canonical NF-κB signaling. In contrast, TRAF3 limits RANKL- and TNF-induced osteoclast formation, and it restricts transforming growth factor β (TGFβ)-induced inhibition of osteoblast formation in young and adult mice. During aging, neutrophils expressing TGFβ and C-C chemokine receptor type 5 (CCR5) increase in bone marrow of mice in response to increased NF-κB-induced CC motif chemokine ligand 5 (CCL5) expression by mesenchymal progenitor cells and injection of these neutrophils into young mice decreased bone mass. TGFβ causes degradation of TRAF3, resulting in decreased glycogen synthase kinase-3β/β-catenin-mediated osteoblast formation and age-related osteoporosis in mice. The CCR5 inhibitor, maraviroc, prevented accumulation of TGFβ+/CCR5+ neutrophils in bone marrow and increased bone mass by inhibiting bone resorption and increasing bone formation in aged mice. This paper updates current understanding of how NF-κB signaling is involved in the positive and negative regulation of cytokine-mediated osteoclast and osteoblast formation and activation with a focus on the role of TRAF3 signaling, which can be targeted therapeutically to enhance bone mass.
-
Citations
Citations to this article as recorded by- The Role of Rosavin in the Pathophysiology of Bone Metabolism
Piotr Wojdasiewicz, Paweł Turczyn, Anna Lach-Gruba, Łukasz A. Poniatowski, Daryush Purrahman, Mohammad-Reza Mahmoudian-Sani, Dariusz Szukiewicz
International Journal of Molecular Sciences.2024; 25(4): 2117. CrossRef - The role of monocyte/macrophage chemokines in pathogenesis of osteoarthritis: A review
Hao Luo, Linfeng Li, Song Han, Tao Liu
International Journal of Immunogenetics.2024;[Epub] CrossRef - The effect of low-level laser therapy on osteoclast differentiation: Clinical implications for tooth movement and bone density
Chun-Yi Huang, Huynh Hoai Thuong Le, Hsiao-Chi Tsai, Chih-Hsin Tang, Jian-Hong Yu
Journal of Dental Sciences.2024;[Epub] CrossRef - Genetic Deficiency of the Long Pentraxin 3 Affects Osteogenesis and Osteoclastogenesis in Homeostatic and Inflammatory Conditions
Valentina Granata, Dario Strina, Maria Lucia Schiavone, Barbara Bottazzi, Alberto Mantovani, Antonio Inforzato, Cristina Sobacchi
International Journal of Molecular Sciences.2023; 24(23): 16648. CrossRef
- The Role of Rosavin in the Pathophysiology of Bone Metabolism

- Calcium & bone metabolism
- Skeletal Senescence with Aging and Type 2 Diabetes
- Joshua Nicholas Farr
- Endocrinol Metab. 2023;38(3):295-301. Published online June 14, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1727

- 2,683 View
- 127 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Osteoporosis and type 2 diabetes (T2D) are common diseases that often coexist. While both of these diseases are associated with poor bone quality and increased fracture risk, their pathogenesis of increased fracture risk differs and is multifactorial. Mounting evidence now indicates that key fundamental mechanisms that are central to both aging and energy metabolism exist. Importantly, these mechanisms represent potentially modifiable therapeutic targets for interventions that could prevent or alleviate multiple complications of osteoporosis and T2D, including poor bone quality. One such mechanism that has gained increasing momentum is senescence, which is a cell fate that contributes to multiple chronic diseases. Accumulating evidence has established that numerous boneresident cell types become susceptible to cellular senescence with old age. Recent work also demonstrates that T2D causes the premature accumulation of senescent osteocytes during young adulthood, at least in mice, although it remains to be seen which other bone-resident cell types become senescent with T2D. Given that therapeutically removing senescent cells can alleviate age-related bone loss and T2D-induced metabolic dysfunction, it will be important in future studies to rigorously test whether interventions that eliminate senescent cells can also alleviate skeletal dysfunction in context of T2D, as it does with aging.
-
Citations
Citations to this article as recorded by- Single-cell sequencing reveals an important role of SPP1 and microglial activation in age-related macular degeneration
Shizhen Lei, Mang Hu, Zhongtao Wei
Frontiers in Cellular Neuroscience.2024;[Epub] CrossRef - The synergistic effect of diabetes mellitus and osteoporosis on the all-cause mortality: a cohort study of an American population
Weihua Li, Siyu Xie, Shengdong Zhong, Liting Lan
Frontiers in Endocrinology.2024;[Epub] CrossRef - Identification of systemic biomarkers and potential drug targets for age-related macular degeneration
Shizhen Lei, Mang Hu, Zhongtao Wei
Frontiers in Aging Neuroscience.2024;[Epub] CrossRef
- Single-cell sequencing reveals an important role of SPP1 and microglial activation in age-related macular degeneration

- Thyroid
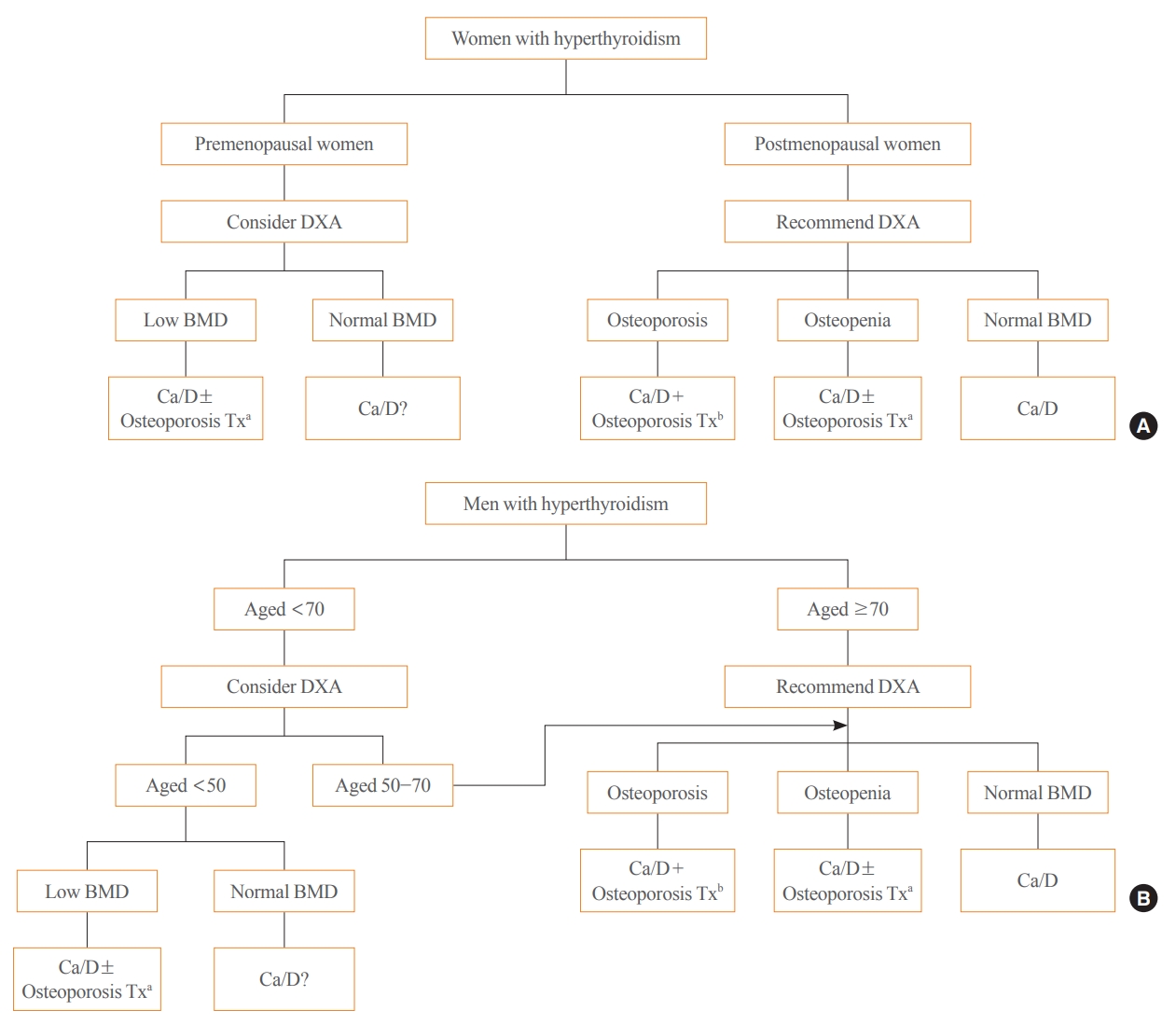
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
- A Ram Hong, Ho-Cheol Kang
- Endocrinol Metab. 2023;38(2):175-189. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1701
- 3,918 View
- 248 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thyroid hormones play an important physiological role in maintaining adult bone structure and strength. Consequently, thyroid dysfunction is related to skeletal outcomes. Overt hyperthyroidism is an established cause of high bone turnover with accelerated bone loss, leading to osteoporosis and increased fracture risk. Hyperthyroidism induced by thyroid-stimulating hormone-suppressive therapy in patients with differentiated thyroid cancer is a cause of secondary osteoporosis. In contrast, there is a lack of evidence on the negative impact of hypothyroidism on bone health. Considering the clinical updates on the importance of bone health in thyroid dysfunction, the Task Force from the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association recently developed a position statement on the evaluation and management of bone health of patients with thyroid diseases, particularly focused on endogenous hyperthyroidism and thyroid-stimulating hormone-suppressive therapy-associated hyperthyroidism in patients with differentiated thyroid cancer. Herein, we review the Korean Thyroid Association’s position statement on the evaluation and management of bone health associated with thyroid diseases.
-
Citations
Citations to this article as recorded by- Diagnosis and therapeutic approach to bone health in patients with hypopituitarism
Justyna Kuliczkowska-Płaksej, Aleksandra Zdrojowy-Wełna, Aleksandra Jawiarczyk-Przybyłowska, Łukasz Gojny, Marek Bolanowski
Reviews in Endocrine and Metabolic Disorders.2024;[Epub] CrossRef - Osteoporosis, Osteoarthritis, and Subchondral Insufficiency Fracture: Recent Insights
Shunichi Yokota, Hotaka Ishizu, Takuji Miyazaki, Daisuke Takahashi, Norimasa Iwasaki, Tomohiro Shimizu
Biomedicines.2024; 12(4): 843. CrossRef - Review on the protective activity of osthole against the pathogenesis of osteoporosis
Jincai Chen, Xiaofei Liao, Juwen Gan
Frontiers in Pharmacology.2023;[Epub] CrossRef
- Diagnosis and therapeutic approach to bone health in patients with hypopituitarism

Original Article
- Calcium & bone metabolism
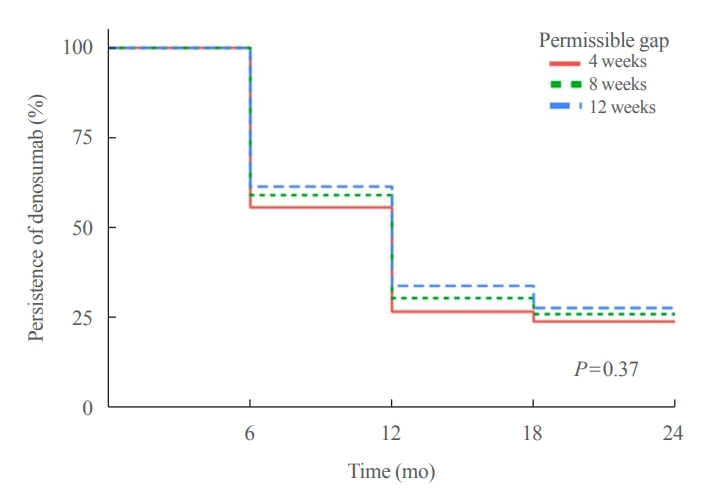
- Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
- Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
- Endocrinol Metab. 2023;38(2):260-268. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1663
- 1,754 View
- 109 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Persistence with denosumab in male patients has not been adequately investigated, although poor denosumab persistence is associated with a significant risk of rebound vertebral fractures.
Methods
We retrospectively evaluated 294 Korean male osteoporosis patients treated with denosumab at three medical centers and examined their persistence with four doses of denosumab injection over 24 months of treatment. Persistence was defined as the extent to which a patient adhered to denosumab treatment in terms of the prescribed interval and dose, with a permissible gap of 8 weeks. For patients who missed their scheduled treatment appointment(s) during the follow-up period (i.e., no-shows), Cox proportional regression analysis was conducted to explore the factors associated with poor adherence. Several factors were considered, such as age, prior anti-osteoporotic drug use, the treatment provider’s medical specialty, the proximity to the medical center, and financial burdens of treatment.
Results
Out of 294 male patients, 77 (26.2%) completed all four sequential rounds of the denosumab treatment. Out of 217 patients who did not complete the denosumab treatment, 138 (63.6%) missed the scheduled treatment(s). Missing treatment was significantly associated with age (odds ratio [OR], 1.03), prior bisphosphonate use (OR, 0.76), and prescription by non-endocrinologists (OR, 2.24). Denosumab was stopped in 44 (20.3%) patients due to medical errors, in 24 (11.1%) patients due to a T-score improvement over –2.5, and in five (2.3%) patients due to expected dental procedures.
Conclusion
Our study showed that only one-fourth of Korean male osteoporosis patients were fully adherent to 24 months of denosumab treatment. -
Citations
Citations to this article as recorded by- Denosumab
Reactions Weekly.2023; 1963(1): 206. CrossRef
- Denosumab

Review Articles
- Calcium & bone metabolism
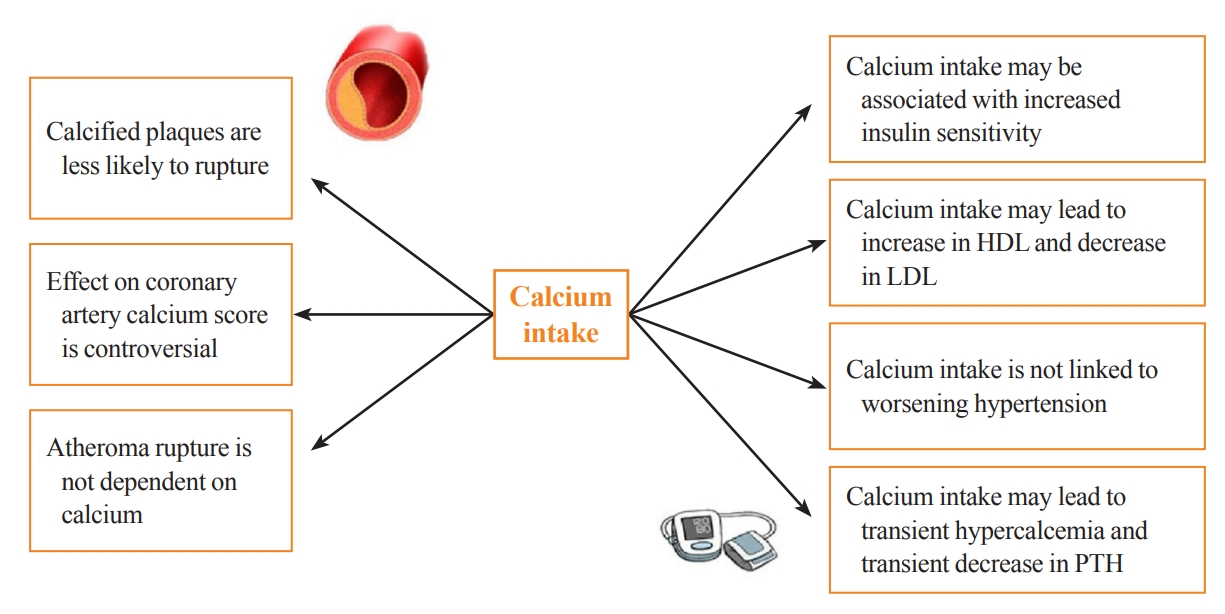
- Cardiovascular Impact of Calcium and Vitamin D Supplements: A Narrative Review
- Fatima Zarzour, Ahmad Didi, Mohammed Almohaya, David Kendler
- Endocrinol Metab. 2023;38(1):56-68. Published online February 16, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1644
- 3,895 View
- 275 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Calcium and vitamin D play an important role in mineral homeostasis and the maintenance of skeletal health. Calcium and vitamin D supplements have been widely used for fracture prevention in elderly populations. Many trials have studied the effectiveness and cardiovascular safety of calcium and vitamin D supplementation, with disparate results. In this review, we summarize the most important trials and systematic reviews. There is significant heterogeneity in clinical trial design, differences in the nature of trial outcomes (self-reported vs. verified), prior calcium intake, and trial size. Inconsistent results have been reported concerning the effects of calcium and vitamin D supplementation on cardiovascular outcomes. Most current guidelines recommend calcium intake of up to 1,200 mg daily, preferably from the diet, without concern for cardiovascular risk. Recommendations regarding vitamin D supplementation vary widely. There is compelling evidence from well-conducted randomized trials that modest vitamin D supplementation is safe but does not confer cardiovascular benefit or cardiovascular harm.
-
Citations
Citations to this article as recorded by- Evaluating adherence, tolerability and safety of oral calcium citrate in elderly osteopenic subjects: a real-life non-interventional, prospective, multicenter study
Mariangela Rondanelli, Salvatore Minisola, Marco Barale, Daniele Barbaro, Francesca Mansueto, Santina Battaglia, Gloria Bonaccorsi, Santina Caliri, Alessandro Cavioni, Luciano Colangelo, Sabrina Corbetta, Federica Coretti, Giorgia Dito, Valentina Gavioli,
Aging Clinical and Experimental Research.2024;[Epub] CrossRef - Association between Daily Dietary Calcium Intake and the Risk of Cardiovascular Disease (CVD) in Postmenopausal Korean Women
Jae Kyung Lee, Thi Minh Chau Tran, Euna Choi, Jinkyung Baek, Hae-Rim Kim, Heeyon Kim, Bo Hyon Yun, Seok Kyo Seo
Nutrients.2024; 16(7): 1043. CrossRef - Effect of Denosumab on Bone Density in Postmenopausal Osteoporosis: A Comparison with and without Calcium Supplementation in Patients on Standard Diets in Korea
Chaiho Jeong, Jinyoung Kim, Jeongmin Lee, Yejee Lim, Dong-Jun Lim, Ki-Hyun Baek, Jeonghoon Ha
Journal of Clinical Medicine.2023; 12(21): 6904. CrossRef
- Evaluating adherence, tolerability and safety of oral calcium citrate in elderly osteopenic subjects: a real-life non-interventional, prospective, multicenter study

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
- Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
- Endocrinol Metab. 2023;38(1):10-24. Published online February 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.102

- 3,739 View
- 262 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - The Korean National Health Information Database (NHID) contains big data combining information obtained from the National Health Insurance Service and health examinations. Data are provided in the form of a cohort, and the NHID can be used to conduct longitudinal studies and research on rare diseases. Moreover, data on the cause and date of death are provided by Statistics Korea. Research and publications based on the NHID have increased explosively in the field of endocrine disorders. However, because the data were not collected for research purposes, studies using the NHID have limitations, particularly the need for the operational definition of diseases. In this review, we describe the characteristics of the Korean NHID, operational definitions of endocrine diseases used for research, and an overview of recent studies in endocrinology using the Korean NHID.
-
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Diabetes severity and the risk of depression: A nationwide population-based study
Yunjung Cho, Bongsung Kim, Hyuk-Sang Kwon, Kyungdo Han, Mee Kyoung Kim
Journal of Affective Disorders.2024; 351: 694. CrossRef - Information Bias Might Exaggerate Lung Cancer Risk of Patients With Rheumatoid Arthritis
Nobuyuki Horita, Kaoru Takase-Minegishi
Journal of Thoracic Oncology.2024; 19(2): 348. CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
Endocrinology and Metabolism.2023; 38(6): 690. CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study

Original Article
- Calcium & bone metabolism
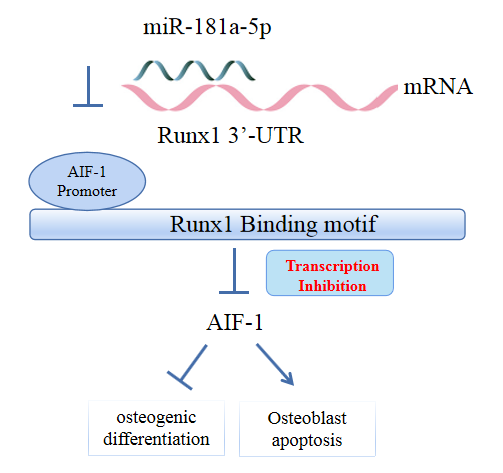
- MicroRNA-181a-5p Curbs Osteogenic Differentiation and Bone Formation Partially Through Impairing Runx1-Dependent Inhibition of AIF-1 Transcription
- Jingwei Liu, Xueying Chang, Daming Dong
- Endocrinol Metab. 2023;38(1):156-173. Published online January 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1516
- 1,575 View
- 101 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Evidence has revealed the involvement of microRNAs (miRNAs) in modulating osteogenic differentiation, implying the promise of miRNA-based therapies for treating osteoporosis. This study investigated whether miR-181a-5p influences osteogenic differentiation and bone formation and aimed to establish the mechanisms in depth.
Methods
Clinical serum samples were obtained from osteoporosis patients, and MC3T3-E1 cells were treated with osteogenic induction medium (OIM) to induce osteogenic differentiation. miR-181a-5p-, Runt-related transcription factor 1 (Runx1)-, and/or allograft inflammatory factor-1 (AIF-1)-associated oligonucleotides or vectors were transfected into MC3T3-E1 cells to explore their function in relation to the number of calcified nodules, alkaline phosphatase (ALP) staining and activity, expression levels of osteogenesis-related proteins, and apoptosis. Luciferase activity, RNA immunoprecipitation, and chromatin immunoprecipitation assays were employed to validate the binding relationship between miR-181a-5p and Runx1, and the transcriptional regulatory relationship between Runx1 and AIF-1. Ovariectomy (OVX)-induced mice were injected with a miR-181a-5p antagonist for in vivo verification.
Results
miR-181a-5p was highly expressed in the serum of osteoporosis patients. OIM treatment decreased miR-181a-5p and AIF-1 expression, but promoted Runx1 expression in MC3T-E1 cells. Meanwhile, upregulated miR-181a-5p suppressed OIM-induced increases in calcified nodules, ALP content, and osteogenesis-related protein expression. Mechanically, miR-181a-5p targeted Runx1, which acted as a transcription factor to negatively modulate AIF-1 expression. Downregulated Runx1 suppressed the miR-181a-5p inhibitor-mediated promotion of osteogenic differentiation, and downregulated AIF-1 reversed the miR-181a-5p mimic-induced inhibition of osteogenic differentiation. Tail vein injection of a miR-181a-5p antagonist induced bone formation in OVX-induced osteoporotic mice.
Conclusion
In conclusion, miR-181a-5p affects osteogenic differentiation and bone formation partially via the modulation of the Runx1/AIF-1 axis. -
Citations
Citations to this article as recorded by- Scopolamine regulates the osteogenic differentiation of human periodontal ligament stem cells through lactylation modification of RUNX2 protein
Ying Wu, Pan Gong
Pharmacology Research & Perspectives.2024;[Epub] CrossRef
- Scopolamine regulates the osteogenic differentiation of human periodontal ligament stem cells through lactylation modification of RUNX2 protein

Review Articles
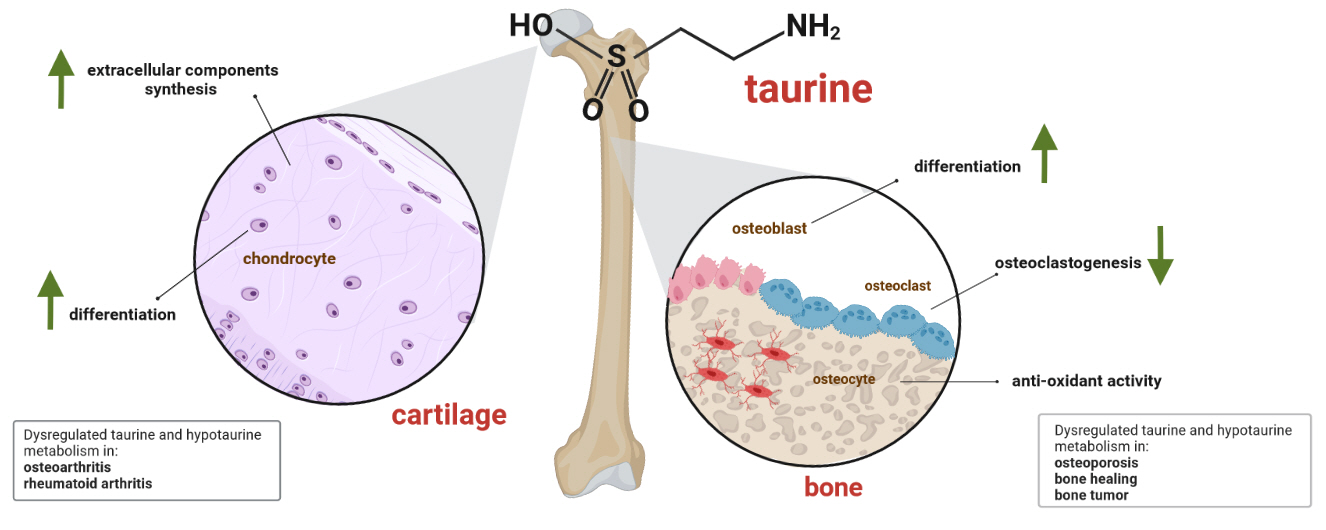
- Calcium & Bone Metabolism
- A Key Metabolic Regulator of Bone and Cartilage Health
- Elizabeth Pérez-Hernández, Jesús Javier Pastrana-Carballo, Fernando Gómez-Chávez, Ramesh C. Gupta, Nury Pérez-Hernández
- Endocrinol Metab. 2022;37(4):559-574. Published online August 8, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1443
- 7,881 View
- 341 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Taurine, a cysteine-derived zwitterionic sulfonic acid, is a common ingredient in energy drinks and is naturally found in fish and other seafood. In humans, taurine is produced mainly in the liver, and it can also be obtained from food. In target tissues, such as the retina, heart, and skeletal muscle, it functions as an essential antioxidant, osmolyte, and antiapoptotic agent. Taurine is also involved in energy metabolism and calcium homeostasis. Taurine plays a considerable role in bone growth and development, and high-profile reports have demonstrated the importance of its metabolism for bone health. However, these reports have not been collated for more than 10 years. Therefore, this review focuses on taurine–bone interactions and covers recently discovered aspects of taurine’s effects on osteoblastogenesis, osteoclastogenesis, bone structure, and bone pathologies (e.g., osteoporosis and fracture healing), with due attention to the taurine–cartilage relationship.
-
Citations
Citations to this article as recorded by- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis
Mengxing Yin, Dezhi Zhou, Fu Jia, Xiaosan Su, Xiufang Li, Ruifen Sun, Junmin Li
Journal of Orthopaedic Surgery and Research.2023;[Epub] CrossRef - An in-silico approach to the potential modulatory effect of taurine on sclerostin (SOST) and its probable role during osteoporosis
Mazumder Adhish, I. Manjubala
Journal of Biomolecular Structure and Dynamics.2023; : 1. CrossRef - Flattening the biological age curve by improving metabolic health: to taurine or not to taurine, that’ s the question
Kwok M. Ho, Anna Lee, William Wu, Matthew T.V. Chan, Lowell Ling, Jeffrey Lipman, Jason Roberts, Edward Litton, Gavin M. Joynt, Martin Wong
Journal of Geriatric Cardiology.2023; 20(11): 813. CrossRef
- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis

- Diabetes, Obesity and Metabolism
- Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
- Eun-Jung Rhee
- Endocrinol Metab. 2022;37(3):415-429. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.304

- 4,499 View
- 262 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The world is suffering from a rapid increase in the number of people with diabetes due to the increased prevalence of obesity and lengthened life span. Since the development of insulin thanks to the efforts of Prof. Banting and Dr. Best in 1922, for which they won the Nobel Prize, remarkable developments in anti-diabetic medications have dramatically lengthened the lifespan of patients with diabetes. However, the control rate of hyperglycemia in patients with diabetes remains unsatisfactory, since glycemic control requires both medication and lifestyle modifications to slow the deterioration of pancreatic beta-cell function and prevent diabetic complications. From the initial “triumvirate” to the “ominous octet,” and now the “egregious eleven,” the number of organs recognized as being involved in hyperglycemia and diabetes has increased with the development of anti-diabetic medications. Recent unexpected results from outcome trials of anti-diabetic medications have enabled anti-diabetic medications to be indicated for the prevention of chronic kidney disease and heart failure, even in patients without diabetes. In this review, I would like to summarize the extra-glycemic effects of anti-diabetic medications.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Glucagon-Like Peptide Receptor Agonist Inhibits Angiotensin II-Induced Proliferation and Migration in Vascular Smooth Muscle Cells and Ameliorates Phosphate-Induced Vascular Smooth Muscle Cells Calcification
Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2024; 48(1): 83. CrossRef - To do one and to get more: Part I. Diabetes and bone
Wen-Ling Lee, Peng-Hui Wang, Szu-Ting Yang, Chia-Hao Liu, Wen-Hsun Chang, Fa-Kung Lee
Journal of the Chinese Medical Association.2022; 85(10): 965. CrossRef
- Association between underweight and risk of heart failure in diabetes patients

Original Articles
- Calcium & Bone Metabolism
- Bone Mineral Density Screening Interval and Transition to Osteoporosis in Asian Women
- Hyunju Park, Heera Yang, Jung Heo, Hye Won Jang, Jae Hoon Chung, Tae Hyuk Kim, Yong-Ki Min, Sun Wook Kim
- Endocrinol Metab. 2022;37(3):506-512. Published online June 9, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1429

- 3,047 View
- 103 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Bone mineral density (BMD) testing is indicated for women aged 65 years, but screening strategies for osteoporosis are controversial. Currently, there is no study focusing on the BMD testing interval in Asian populations. The current study aimed to evaluate the estimated time interval for screening osteoporosis.
Methods
We conducted a study of 6,385 subjects aged 50 years and older who underwent dual-energy X-ray absorptiometry screening more than twice at Samsung Medical Center as participants in a routine health checkup. Subjects were divided based on baseline T-score into mild osteopenia (T-score, <–1.0 to >–1.5), moderate osteopenia (T-score, ≤–1.5 to >–2.0), and severe osteopenia (T-score, ≤–2.0 to >–2.5). Information about personal medical and social history was collected by a structured questionnaire.
Results
The adjusted estimated BMD testing interval for 10% of the subjects to develop osteoporosis was 13.2 years in mild osteopenia, 5.0 years in moderate osteopenia, and 1.5 years in severe osteopenia.
Conclusion
Our study provides extended information about BMD screening intervals in Asian female population. Baseline T-score was important for predicting BMD screening interval, and repeat BMD testing within 5 years might not be necessary in mild osteopenia subjects. -
Citations
Citations to this article as recorded by- Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial
Chaiho Jeong, Jeonghoon Ha, Jun-Il Yoo, Young-Kyun Lee, Jung Hee Kim, Yong-Chan Ha, Yong-Ki Min, Dong-Won Byun, Ki-Hyun Baek, Ho Yeon Chung
Journal of Bone Metabolism.2023; 30(2): 189. CrossRef - Bone-modifying agents for non–small-cell lung cancer patients with bone metastases during the era of immune checkpoint inhibitors: A narrative review
Jinyoung Kim, Chaiho Jeong, Jeongmin Lee, Jeonghoon Ha, Ki-Hyun Baek, Seohyun Kim, Tai Joon An, Chan Kwon Park, Hyoung Kyu Yoon, Jeong Uk Lim
Seminars in Oncology.2023; 50(3-5): 105. CrossRef
- Effects of Bazedoxifene/Vitamin D Combination Therapy on Serum Vitamin D Levels and Bone Turnover Markers in Postmenopausal Women with Osteopenia: A Randomized Controlled Trial

- Calcium & Bone Metabolism
- Real-World Safety and Effectiveness of Denosumab in Patients with Osteoporosis: A Prospective, Observational Study in South Korea
- Yumie Rhee, Dong-Gune Chang, Jeonghoon Ha, Sooa Kim, Yusun Lee, Euna Jo, Jung-Min Koh
- Endocrinol Metab. 2022;37(3):497-505. Published online June 3, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1427

- 5,375 View
- 268 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The efficacy and safety of denosumab have been established in a phase 3, randomized, placebo-controlled trial in Korean postmenopausal women with osteoporosis. This postmarketing surveillance study was aimed to investigate the safety and effectiveness of denosumab in Korean real-world clinical practice.
Methods
Patients with osteoporosis who had received denosumab per the Korean approved indications in the postmarketing setting between September 2014 and September 2019 were enrolled. The primary endpoint was the incidence of adverse events (AEs) and adverse drug reactions (ADRs). The secondary endpoint was the percent change from baseline in bone mineral density (BMD) of the lumbar spine, total hip, and femoral neck.
Results
Of the 3,221 patients enrolled, 3,185 were included in the safety analysis set; 2,973 (93.3%) were female, and the mean± standard deviation (SD) age was 68.9±9.9 years. The mean±SD study period was 350.0±71.4 days. AEs, fatal AEs, and ADRs occurred in 19.3%, 0.8%, and 1.6%, respectively. The most frequent AEs, occurring in >0.5% of patients, were dizziness (0.7%), arthralgia (0.7%), back pain (0.6%), and myalgia (0.6%). Hypocalcemia occurred in 0.3% of patients. There were no cases of osteonecrosis of the jaw and atypical femoral fracture. Mean±SD percent change from baseline in BMD of the lumbar spine, total hip, and femoral neck was 7.3%±23.6%, 3.6%±31.4%, and 3.2%±10.7%, respectively.
Conclusion
The safety and effectiveness of denosumab in Korean patients with osteoporosis in this study were comparable with those in the Korean randomized controlled trial, with no new safety findings. -
Citations
Citations to this article as recorded by- Prevalence of denosumab-induced hypocalcemia: a retrospective observational study of patients routinely monitored with ionized calcium post-injection
Anna Spångeus, Johan Rydetun, Mischa Woisetschläger
Osteoporosis International.2024; 35(1): 173. CrossRef - Cost-consequence analysis of continuous denosumab therapy for osteoporosis treatment in South Korea
Seungju Cha, Minjeong Sohn, Hyowon Yang, Eric J. Yeh, Ki-Hyun Baek, Jeonghoon Ha, Hyemin Ku
BMC Musculoskeletal Disorders.2024;[Epub] CrossRef - Denosumab and the Risk of Diabetes in Patients Treated for Osteoporosis
Huei-Kai Huang, Albert Tzu-Ming Chuang, Tzu-Chi Liao, Shih-Chieh Shao, Peter Pin-Sung Liu, Yu-Kang Tu, Edward Chia-Cheng Lai
JAMA Network Open.2024; 7(2): e2354734. CrossRef - Adverse Effects of Denosumab in Kidney Transplant Recipients: A 20-Year Retrospective Single-Center Observation Study in Central Taiwan
Tsung-Yin Tsai, Zi-Hong You, Shang-Feng Tsai, Ming-Ju Wu, Tung-Min Yu, Ya-Wen Chuang, Yung-Chieh Lin, Ya-Lian Deng, Chiann-Yi Hsu, Cheng-Hsu Chen
Transplantation Proceedings.2023; 55(4): 837. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef - Effect of Denosumab on Bone Density in Postmenopausal Osteoporosis: A Comparison with and without Calcium Supplementation in Patients on Standard Diets in Korea
Chaiho Jeong, Jinyoung Kim, Jeongmin Lee, Yejee Lim, Dong-Jun Lim, Ki-Hyun Baek, Jeonghoon Ha
Journal of Clinical Medicine.2023; 12(21): 6904. CrossRef - Denosumab
Reactions Weekly.2022; 1919(1): 221. CrossRef - Denosumab, an effective osteoporosis treatment option for men
Sung Hye Kong
The Korean Journal of Internal Medicine.2022; 37(5): 947. CrossRef
- Prevalence of denosumab-induced hypocalcemia: a retrospective observational study of patients routinely monitored with ionized calcium post-injection

Review Article
- Calcium & Bone Metabolism
- Discontinuing Denosumab: Can It Be Done Safely? A Review of the Literature
- Wei Lin Tay, Donovan Tay
- Endocrinol Metab. 2022;37(2):183-194. Published online April 14, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1369

- 16,179 View
- 898 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Denosumab, which has been approved for the treatment of osteoporosis since 2010, is a fully humanised monoclonal antibody against a cytokine, receptor activator of nuclear factor kappa B ligand (RANKL), involved in bone resorption. Continued use of denosumab results in a potent and sustained decrease in bone turnover, an increase in bone mineral density (BMD), and a reduction in vertebral and hip fractures. The anti-resorptive effects of denosumab are reversible upon cessation, and this reversal is accompanied by a transient marked increase in bone turnover that is associated with bone loss, and of concern, an increased risk of multiple vertebral fractures. In this review, we outline the effects of denosumab withdrawal on bone turnover markers, BMD, histomorphometry, and fracture risk. We provide an update on recent clinical trials that sought to answer how clinicians can transition away from denosumab safely with follow-on therapy to mitigate bone loss and summarise the recommendations of various international guidelines.
-
Citations
Citations to this article as recorded by- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury
Christopher M. Cirnigliaro, Michael F. La Fountaine, J. Scott Parrott, Steven C. Kirshblum, Susan J. Sauer, Sue A. Shapses, Isa A. McClure, William A. Bauman
Osteoporosis International.2023; 34(4): 741. CrossRef - Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
Endocrinology and Metabolism.2023; 38(2): 260. CrossRef
- Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury

Original Article
- Calcium & Bone Metabolism
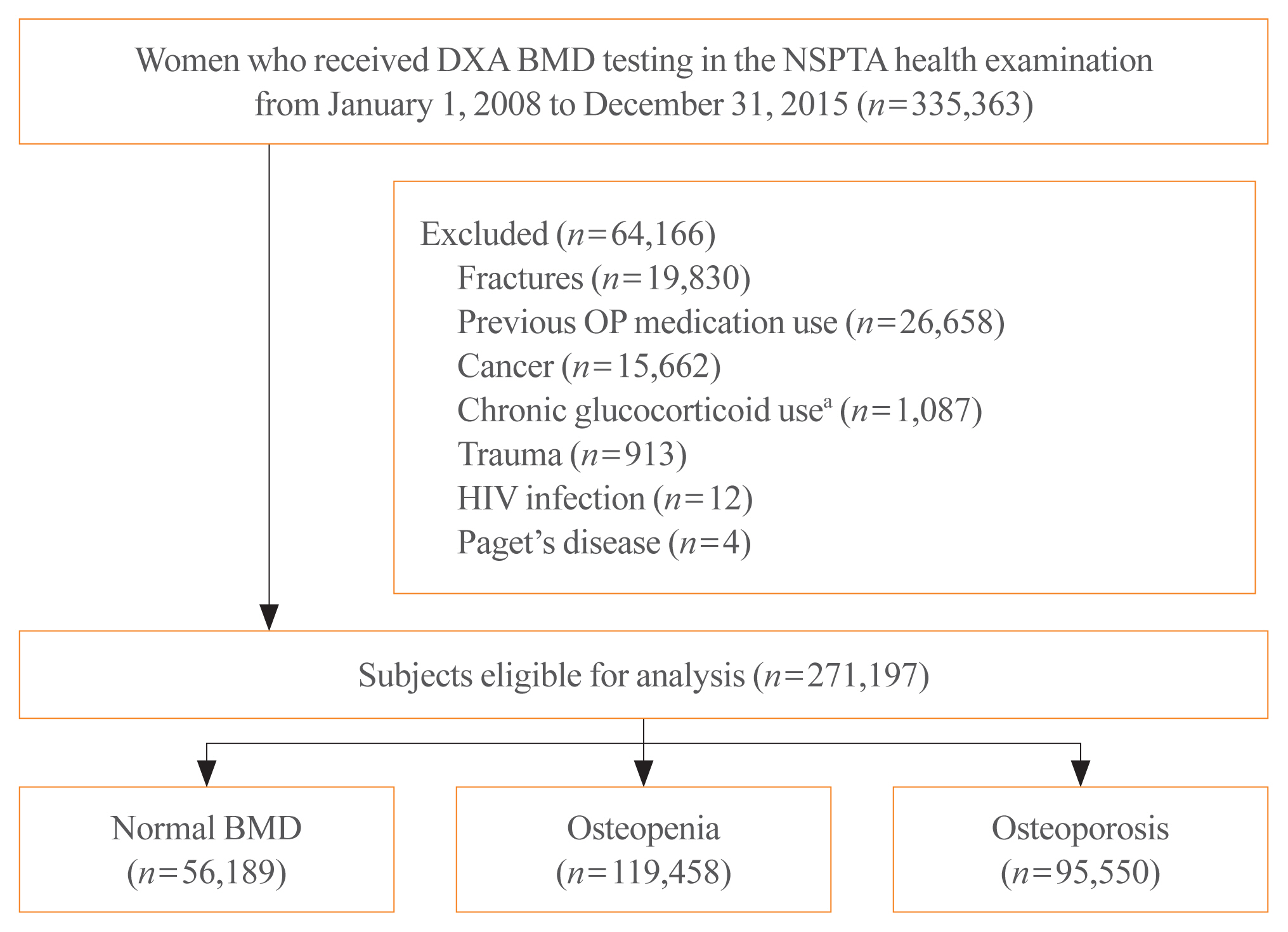
Big Data Articles (National Health Insurance Service Database) - 10-Year Fracture Risk in Postmenopausal Women with Osteopenia and Osteoporosis in South Korea
- Yeon-Hee Baek, Sun Wook Cho, Han Eol Jeong, Ju Hwan Kim, Yunji Hwang, Jeffrey L. Lange, Ju-Young Shin
- Endocrinol Metab. 2021;36(6):1178-1188. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1215
- 5,274 View
- 248 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
In South Korea, women aged 66 years are eligible for complimentary bone mineral density (BMD) screening via the National Screening Program for Transitional Ages. We aimed to evaluate the 10-year fracture risk in women receiving BMD screening between January 2008 and December 2015.
Methods
BMD was classified as normal (T-score ≥–1.0 standard deviation [SD]), osteopenia (T-score <–1.0 SD and >–2.5 SD), and osteoporosis (T score ≤–2.5 SD) from dual-energy X-ray absorptiometry. Follow-up continued from the screening date until a diagnosis for clinical fragility fracture (including sites of the vertebrae, hip, pelvis, clavicle, humerus, forearm, wrist, lower leg, and ankle), censored at the earliest date of trauma, death, or December 2017; fracture was ascertained using diagnostic codes from the National Health Insurance Service database. A multivariable Cox proportional hazard model was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of fracture in women with osteopenia or osteoporosis relative to women with normal BMD.
Results
Among the 271,197 women screened, 44.0% had osteopenia and 35.2% had osteoporosis. The 10 year cumulative incidence of fragility fractures was 31.1%, 37.5%, and 44.3% in women with normal BMD, osteopenia, and osteoporosis, respectively. Fracture risk was higher in women with osteopenia (HR, 1.31; 95% CI, 1.28 to 1.34) and osteoporosis (HR, 1.68; 95% CI, 1.64 to 1.72) than in women with normal BMD.
Conclusion
Women with osteopenia and women with osteoporosis, identified by the national BMD screening program, demonstrated a substantially elevated risk of fracture. -
Citations
Citations to this article as recorded by- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women
S. Han, S. Kim, E.J. Yeh, H.S. Suh
Osteoporosis International.2024; 35(2): 339. CrossRef - Duration of osteoporosis treatment to reduce the risk of subsequent osteoporotic fracture and all-cause mortality in elderly hip fracture patients in a Korean real-world study
Soong Joon Lee, Minjoon Cho, Hojoon Lee, Hyuna Lim, Jae Hyup Lee
Archives of Osteoporosis.2024;[Epub] CrossRef - Do Patients with Benign Paroxysmal Positional Vertigo Have a Higher Prevalence of Osteoporosis? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Keunho Kim, Yeonjoo Choi
Journal of Personalized Medicine.2024; 14(3): 303. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Chronic airway disease as a major risk factor for fractures in osteopenic women: Nationwide cohort study
Sung Hye Kong, Ae Jeong Jo, Chan Mi Park, Kyun Ik Park, Ji Eun Yun, Jung Hee Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biomimetic Porous Magnesium Alloy Scaffolds Promote the Repair of Osteoporotic Bone Defects in Rats through Activating the Wnt/β-Catenin Signaling Pathway
Yuanchao Zhu, Gaozhi Jia, Yifei Yang, Jian Weng, Su Liu, Mengwei Zhang, Geng Zhang, Haotian Qin, Yixiao Chen, Qi Yang, Guangyin Yuan, Fei Yu, Hui Zeng
ACS Biomaterials Science & Engineering.2023; 9(6): 3435. CrossRef - Correlation between bone mineral density and bone metabolic markers in postmenopausal women with osteoporotic fractures at different C-terminal telopeptide of type 1 collagen levels: a retrospective analysis study
Xiaonan Zhu, Lin Chen, Ling Pan, Yuexi Zeng, Qiang Fu, Yanbin Liu, Yongde Peng, Yufan Wang, Li You
Menopause.2023; 30(11): 1139. CrossRef - Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
Endocrinology and Metabolism.2023; 38(6): 669. CrossRef - A Meaningful Journey to Predict Fractures with Deep Learning
Jeonghoon Ha
Endocrinology and Metabolism.2022; 37(4): 617. CrossRef - The Efficacy of Selective Estrogen Receptor Modulators Monotherapies in Postmenopausal Women with Osteopenia
Kyung Wook Kim, Young Il Kim, Ki-Choul Kim
Journal of Bone Metabolism.2022; 29(3): 185. CrossRef - Correlation of Psoas Muscle Index with Fragility Vertebral Fracture: A Retrospective Cross-Sectional Study of Middle-Aged and Elderly Women
Yihui Zhang, Yilihamu Dilixiati, Wei Jiang, Xiufeng Cao, Yuanyuan Chen, Hui Guo, Christian-Heinz Anderwald
International Journal of Endocrinology.2022; 2022: 1. CrossRef
- Understanding the long-term impact of incident osteoporotic fractures on healthcare utilization and costs in Korean postmenopausal women


 KES
KES

 First
First Prev
Prev



