Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- MicroRNA-181a-5p Curbs Osteogenic Differentiation and Bone Formation Partially Through Impairing Runx1-Dependent Inhibition of AIF-1 Transcription
- Jingwei Liu, Xueying Chang, Daming Dong
- Endocrinol Metab. 2023;38(1):156-173. Published online January 6, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1516
- 1,609 View
- 101 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Evidence has revealed the involvement of microRNAs (miRNAs) in modulating osteogenic differentiation, implying the promise of miRNA-based therapies for treating osteoporosis. This study investigated whether miR-181a-5p influences osteogenic differentiation and bone formation and aimed to establish the mechanisms in depth.
Methods
Clinical serum samples were obtained from osteoporosis patients, and MC3T3-E1 cells were treated with osteogenic induction medium (OIM) to induce osteogenic differentiation. miR-181a-5p-, Runt-related transcription factor 1 (Runx1)-, and/or allograft inflammatory factor-1 (AIF-1)-associated oligonucleotides or vectors were transfected into MC3T3-E1 cells to explore their function in relation to the number of calcified nodules, alkaline phosphatase (ALP) staining and activity, expression levels of osteogenesis-related proteins, and apoptosis. Luciferase activity, RNA immunoprecipitation, and chromatin immunoprecipitation assays were employed to validate the binding relationship between miR-181a-5p and Runx1, and the transcriptional regulatory relationship between Runx1 and AIF-1. Ovariectomy (OVX)-induced mice were injected with a miR-181a-5p antagonist for in vivo verification.
Results
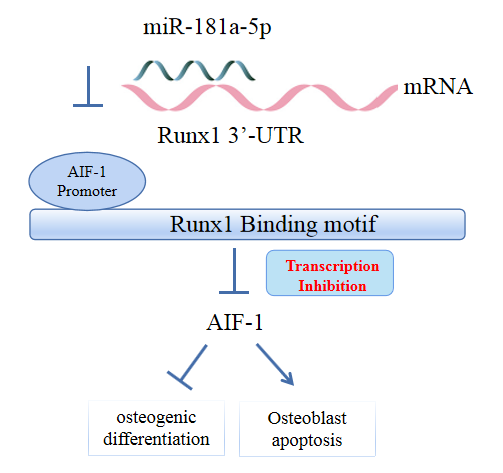
miR-181a-5p was highly expressed in the serum of osteoporosis patients. OIM treatment decreased miR-181a-5p and AIF-1 expression, but promoted Runx1 expression in MC3T-E1 cells. Meanwhile, upregulated miR-181a-5p suppressed OIM-induced increases in calcified nodules, ALP content, and osteogenesis-related protein expression. Mechanically, miR-181a-5p targeted Runx1, which acted as a transcription factor to negatively modulate AIF-1 expression. Downregulated Runx1 suppressed the miR-181a-5p inhibitor-mediated promotion of osteogenic differentiation, and downregulated AIF-1 reversed the miR-181a-5p mimic-induced inhibition of osteogenic differentiation. Tail vein injection of a miR-181a-5p antagonist induced bone formation in OVX-induced osteoporotic mice.
Conclusion
In conclusion, miR-181a-5p affects osteogenic differentiation and bone formation partially via the modulation of the Runx1/AIF-1 axis. -
Citations
Citations to this article as recorded by- Scopolamine regulates the osteogenic differentiation of human periodontal ligament stem cells through lactylation modification of RUNX2 protein
Ying Wu, Pan Gong
Pharmacology Research & Perspectives.2024;[Epub] CrossRef
- Scopolamine regulates the osteogenic differentiation of human periodontal ligament stem cells through lactylation modification of RUNX2 protein

- Bone Metabolism
- Recent Topics in Fibrodysplasia Ossificans Progressiva
- Takenobu Katagiri, Sho Tsukamoto, Yutaka Nakachi, Mai Kuratani
- Endocrinol Metab. 2018;33(3):331-338. Published online September 18, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.331
- 5,088 View
- 79 Download
- 19 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Fibrodysplasia ossificans progressiva (FOP) is a rare genetic disease that is characterized by the formation of heterotopic bone tissues in soft tissues, such as skeletal muscle, ligament, and tendon. It is difficult to remove such heterotopic bones via internal medicine or invasive procedures. The identification of activin A receptor, type I (
ACVR1 )/ALK2 gene mutations associated with FOP has allowed the genetic diagnosis of FOP. TheACVR1 /ALK2 gene encodes the ALK2 protein, which is a transmembrane kinase receptor in the transforming growth factor-β family. The relevant mutations activate intracellular signalingin vitro and induce heterotopic bone formationin vivo . Activin A is a potential ligand that activates mutant ALK2 but not wild-type ALK2. Various types of small chemical and biological inhibitors of ALK2 signaling have been developed to establish treatments for FOP. Some of these are in clinical trials in patients with FOP.-
Citations
Citations to this article as recorded by- How Activin A Became a Therapeutic Target in Fibrodysplasia Ossificans Progressiva
Dushyanth Srinivasan, Martin Arostegui, Erich J. Goebel, Kaitlin N. Hart, Senem Aykul, John B. Lees-Shepard, Vincent Idone, Sarah J. Hatsell, Aris N. Economides
Biomolecules.2024; 14(1): 101. CrossRef - Fibrodysplasia Ossificans Progressiva Mimics Generalized Dystonia Disorder: A Case Report
Seraj Makkawi, Osama Khojah, Reema Abualnaja, Abdulaziz Qashqari, Nawaf A Alahmadi, Abdullatif G Bshnaq, Abdulrahman Alharthi, Hashem H Al-Hashemi, Aiman M Shawli
Cureus.2023;[Epub] CrossRef - Exploration of marine natural resources in Indonesia and development of efficient strategies for the production of microbial halogenated metabolites
Hiroyuki Yamazaki
Journal of Natural Medicines.2022; 76(1): 1. CrossRef - A Novel De Novo Frameshift Pathogenic Variant in the FAM111B Resulting in Progressive Osseous Heteroplasia Phenotype
Anna Ryabets-Lienhard, Panadeekarn Panjawatanan, Kyle Vogt, Jianling Ji, Senta Georgia, Pisit Pitukcheewanont
Calcified Tissue International.2022; 112(4): 518. CrossRef - Inhibitory effects of sesquiterpene lactones from the Indonesian marine sponge Lamellodysidea cf. herbacea on bone morphogenetic protein-induced osteoblastic differentiation
Satoshi Ohte, Hiroyuki Yamazaki, Ohgi Takahashi, Henki Rotinsulu, Defny S. Wewengkang, Deiske A. Sumilat, Delfly B. Abdjul, Wilmar Maarisit, Magie M. Kapojos, Huiping Zhang, Fumiaki Hayashi, Michio Namikoshi, Takenobu Katagiri, Hiroshi Tomoda, Ryuji Uchid
Bioorganic & Medicinal Chemistry Letters.2021; 35: 127783. CrossRef - Genomic Context and Mechanisms of the ACVR1 Mutation in Fibrodysplasia Ossificans Progressiva
Roberto Ravazzolo, Renata Bocciardi
Biomedicines.2021; 9(2): 154. CrossRef - New insights on fibrodysplasia ossificans progressiva: discussion of an autoptic case report and brief literature review
Vittorio Bolcato, Claudia Carelli, Silvia Damiana Visonà, Marcella Reguzzoni, Maja Di Rocco, Alessandra Radogna, Livio Pietro Tronconi, Matteo Moretti
Intractable & Rare Diseases Research.2021; 10(2): 136. CrossRef - Accumulated Knowledge of Activin Receptor-Like Kinase 2 (ALK2)/Activin A Receptor, Type 1 (ACVR1) as a Target for Human Disorders
Takenobu Katagiri, Sho Tsukamoto, Mai Kuratani
Biomedicines.2021; 9(7): 736. CrossRef - Cytoskeleton Reorganization in EndMT—The Role in Cancer and Fibrotic Diseases
Wojciech Michał Ciszewski, Marta Ewelina Wawro, Izabela Sacewicz-Hofman, Katarzyna Sobierajska
International Journal of Molecular Sciences.2021; 22(21): 11607. CrossRef - Alendronate disturbs femoral growth due to changes during immunolocalization of transforming growth factor-β1 and bone morphogenetic protein-2 in epiphyseal plate
Juliana Souza Vieira, Emanuelle Juliana Cunha, Juliana Feltrin de Souza, Luis Henrique Koeler Chaves, Jessica Lakes de Souza, Allan Fernando Giovanini
World Journal of Experimental Medicine.2020; 10(1): 1. CrossRef - ALK2: A Therapeutic Target for Fibrodysplasia Ossificans Progressiva and Diffuse Intrinsic Pontine Glioma
Katsuhiko Sekimata, Tomohiro Sato, Naoki Sakai
Chemical and Pharmaceutical Bulletin.2020; 68(3): 194. CrossRef - Role of Signal Transduction Pathways and Transcription Factors in Cartilage and Joint Diseases
Riko Nishimura, Kenji Hata, Yoshifumi Takahata, Tomohiko Murakami, Eriko Nakamura, Maki Ohkawa, Lerdluck Ruengsinpinya
International Journal of Molecular Sciences.2020; 21(4): 1340. CrossRef - Design of primers for direct sequencing of nine coding exons in the human ACVR1 gene
Masaru Matsuoka, Sho Tsukamoto, Yuta Orihara, Rieko Kawamura, Mai Kuratani, Nobuhiko Haga, Kenji Ikebuchi, Takenobu Katagiri
Bone.2020; 138: 115469. CrossRef - A new diketopiperazine-like inhibitor of bone morphogenetic protein-induced osteoblastic differentiation produced by marine-derived Aspergillus sp. BFM-0085
Satoshi Ohte, Takehiro Shiokawa, Nobuhiro Koyama, Takenobu Katagiri, Chiaki Imada, Hiroshi Tomoda
The Journal of Antibiotics.2020; 73(8): 554. CrossRef - Penicillic Acid Congener, a New Inhibitor of BMP-Induced Alkaline Phosphatase Activity in Myoblasts, Produced by the Fungus Penicillium sp. BF-0343
Nobuhiro Koyama, Yasuhiro Otoguro, Satoshi Ohte, Takenobu Katagiri, Hiroshi Tomoda
Natural Product Communications.2020; 15(9): 1934578X2094265. CrossRef - Fibrodysplasia ossificans progressiva: current concepts from bench to bedside
Arun-Kumar Kaliya-Perumal, Tom J. Carney, Philip W. Ingham
Disease Models & Mechanisms.2020;[Epub] CrossRef - Clinical Aspects and Current Therapeutic Approaches for FOP
Hiroshi Kitoh
Biomedicines.2020; 8(9): 325. CrossRef - Screening for Small Molecule Inhibitors of BMP-Induced Osteoblastic Differentiation from Indonesian Marine Invertebrates
Hiroyuki Yamazaki, Satoshi Ohte, Henki Rotinsulu, Defny S. Wewengkang, Deiske A. Sumilat, Delfly B. Abdjul, Wilmar Maarisit, Magie M. Kapojos, Michio Namikoshi, Takenobu Katagiri, Hiroshi Tomoda, Ryuji Uchida
Marine Drugs.2020; 18(12): 606. CrossRef - Propranolol and ascorbic acid in control of fibrodysplasia ossificans progressiva flare-ups due to accidental falls
Durval Batista Palhares, Deborah Ribeiro Nascimento, Marilene Garcia Palhares, Suzana Lopes Bomfim Balaniuc, Liane de Rosso Giuliani, Paula Cristhina Niz Xavier, José Mauro Goulart Brum, Fabiana Alves, Francisco Oliveira Vieira, Elaine Maria Souza-Fagunde
Intractable & Rare Diseases Research.2019; 8(1): 24. CrossRef - Late-onset fibrodysplasia ossificans progressiva with atypical presentation: A case report
Conor M. Cunningham, J. Matthew Royeca, Samuel W. King, Hemant Pandit
Case Reports in Women's Health.2019; 23: e00134. CrossRef - Fibrodysplasia ossificans progressiva: lessons learned from a rare disease
Gulseren Akyuz, Kardelen Gencer-Atalay, Pinar Ata
Current Opinion in Pediatrics.2019; 31(6): 716. CrossRef - Discovery of Heterotopic Bone-Inducing Activity in Hard Tissues and the TGF-β Superfamily
Takenobu Katagiri, Sho Tsukamoto, Yutaka Nakachi, Mai Kuratani
International Journal of Molecular Sciences.2018; 19(11): 3586. CrossRef
- How Activin A Became a Therapeutic Target in Fibrodysplasia Ossificans Progressiva

- Bone Metabolism
- Expression of Glucagon-Like Peptide 1 Receptor during Osteogenic Differentiation of Adipose-Derived Stem Cells
- Yun Kyung Jeon, Min Jung Bae, Ju In Kim, Joo Hyoung Kim, Soo Jong Choi, Su Kyoung Kwon, Joon Hyop An, Sang Soo Kim, Bo Hyun Kim, Yong Ki Kim, In Joo Kim
- Endocrinol Metab. 2014;29(4):567-573. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.567
- 4,355 View
- 35 Download
- 29 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Glucagon-like peptide 1 (GLP-1), an incretin hormone well known for its glucose-lowering effect, was recently reported to exert an anabolic effect on bone. Although the exact mechanism is not known, it likely involves the GLP-1 receptor (GLP-1R), which is expressed in some osteoblastic cell lines. Adipose-derived stem cells (ADSCs) have mesenchymal stem cell-specific characteristics, including osteoblastic differentiation potential. We evaluated the expression of GLP-1R during osteogenic differentiation of ADSCs.
Methods ADSCs were isolated from subcutaneous adipose tissue obtained from three male donors during plastic surgery and were subjected to osteogenic induction. Mineralization was assessed by Alizarin Red staining on day 21. Expression of alkaline phosphatase (ALP), osteocalcin (OC), and GLP-1R was measured by real-time polymerase chain reaction in triplicate for each patient on days 0, 7, 14, and 21. Target mRNA expression levels were normalized to that of β-actin.
Results ADSCs were fibroblast-like in morphology, adhered to plastic, and had multipotent differentiation potential, as assessed using specific antigen markers. The osteogenic markers ALP and OC were notably upregulated at 21 days. Osteogenic differentiation resulted in a time-dependent increase in the expression of GLP-1R (
P =0.013).Conclusion We demonstrated upregulation of GLP-1R gene expression during osteogenic differentiation of ADSCs. This finding suggests that GLP-1 may induce osteogenic differentiation in bone tissue.
-
Citations
Citations to this article as recorded by- Effect of gut hormones on bone metabolism and their possible mechanisms in the treatment of osteoporosis
Hongyu Liu, Huimin Xiao, Sufen Lin, Huan Zhou, Yizhao Cheng, Baocheng Xie, Daohua Xu
Frontiers in Pharmacology.2024;[Epub] CrossRef - Glucagon-like peptide-1 receptor promotes osteoblast differentiation of dental pulp stem cells and bone formation in a zebrafish scale regeneration model
Shafei Zhai, Changkui Liu, Selvaraj Vimalraj, Raghunandhakumar Subramanian, Shahabe Saquib abullais, Suraj Arora, Sekaran Saravanan
Peptides.2023; 163: 170974. CrossRef - The associations of gut microbiota, endocrine system and bone metabolism
Ye Tu, Xinyi Kuang, Ling Zhang, Xin Xu
Frontiers in Microbiology.2023;[Epub] CrossRef - Effect of Liraglutide on Osteoporosis in a Rat Model of Type 2 Diabetes Mellitus: A Histological, Immunohistochemical, and Biochemical Study
Maha Abdelhamid Fathy, Amal Anbaig, Raja Aljafil, Sherein F El-Sayed, Hanim Magdy Abdelnour, Mona Mostafa Ahmed, Eman M A Abdelghany, Sulaiman Mohammed Alnasser, Shaimaa Mohamed Abdelfattah Hassan, Amany Mohamed Shalaby
Microscopy and Microanalysis.2023; 29(6): 2053. CrossRef - Metabolic responses and benefits of glucagon‐like peptide‐1 (GLP‐1) receptor ligands
Neil Tanday, Peter R. Flatt, Nigel Irwin
British Journal of Pharmacology.2022; 179(4): 526. CrossRef - Exendin‐4 enhances osteogenic differentiation of adipose tissue mesenchymal stem cells through the receptor activator of nuclear factor‐kappa B and osteoprotegerin signaling pathway
Sarah A. Habib, Mohamed M. Kamal, Shohda A. El‐Maraghy, Mahmoud A. Senousy
Journal of Cellular Biochemistry.2022; 123(5): 906. CrossRef - Risk of fracture caused by anti-diabetic drugs in individuals with type 2 diabetes: A network meta-analysis
Wen-Hsuan Tsai, Siang-Ke Kong, Chu-Lin Lin, Kai-Hsuan Cheng, Yi-Ting Cheng, Ming-Nan Chien, Chun-Chuan Lee, Ming-Chieh Tsai
Diabetes Research and Clinical Practice.2022; 192: 110082. CrossRef - Comprehensive Analysis of Novel Genes and Pathways Associated with Osteogenic Differentiation of Adipose Stem Cells
Qiuni Gao, Xiaorong Ma, Zuoliang Qi, Jianxin Shi
Disease Markers.2022; 2022: 1. CrossRef - Novel Insights into the Roles and Mechanisms of GLP-1 Receptor Agonists against Aging-Related Diseases
Wei Peng, Rui Zhou, Ze-Fang Sun, Jia-Wei Long, Yong-Qiang Gong
Aging and disease.2022; 13(2): 468. CrossRef - Correlation of Osteoporosis in Patients With Newly Diagnosed Type 2 Diabetes: A Retrospective Study in Chinese Population
Yuhua Wen, Huijuan Li, Xiaoya Zhang, Peipei Liu, Jing Ma, Liya Zhang, Keqin Zhang, Lige Song
Frontiers in Endocrinology.2021;[Epub] CrossRef - Effects of Incretin-Related Diabetes Drugs on Bone Formation and Bone Resorption
Hideki Kitaura, Saika Ogawa, Fumitoshi Ohori, Takahiro Noguchi, Aseel Marahleh, Yasuhiko Nara, Adya Pramusita, Ria Kinjo, Jinghan Ma, Kayoko Kanou, Itaru Mizoguchi
International Journal of Molecular Sciences.2021; 22(12): 6578. CrossRef - Liraglutide regulates bone destruction and exhibits anti-inflammatory effects in periodontitis in vitro and in vivo
Yunxia Zhang, Xuemin Yuan, Yuyan Wu, Minyu Pei, Man Yang, Xuanye Wu, Yunqing Pang, Jing Wang
Journal of Dentistry.2020; 94: 103310. CrossRef - Exendin-4 regulates Wnt and NF-κB signaling in lipopolysaccharide-induced human periodontal ligament stem cells to promote osteogenic differentiation
Honghong Liu, Jiawen Zheng, Taijing Zheng, Ping Wang
International Immunopharmacology.2019; 75: 105801. CrossRef - Effects of malvidin, cyanidin and delphinidin on human adipose mesenchymal stem cell differentiation into adipocytes, chondrocytes and osteocytes
Liga Saulite, Kaspars Jekabsons, Maris Klavins, Ruta Muceniece, Una Riekstina
Phytomedicine.2019; 53: 86. CrossRef - Exendin-4 relieves the inhibitory effects of high glucose on the proliferation and osteoblastic differentiation of periodontal ligament stem cells
Zijun Guo, Rui Chen, Fujun Zhang, Ming Ding, Ping Wang
Archives of Oral Biology.2018; 91: 9. CrossRef - Effects of gastric inhibitory polypeptide, glucagon‐like peptide‐1 and glucagon‐like peptide‐1 receptor agonists on Bone Cell Metabolism
Morten S. S. Hansen, Michaela Tencerova, Jacob Frølich, Moustapha Kassem, Morten Frost
Basic & Clinical Pharmacology & Toxicology.2018; 122(1): 25. CrossRef - Liraglutide, a glucagon-like peptide-1 receptor agonist, facilitates osteogenic proliferation and differentiation in MC3T3-E1 cells through phosphoinositide 3-kinase (PI3K)/protein kinase B (AKT), extracellular signal-related kinase (ERK)1/2, and cAMP/pro
Xuelun Wu, Shilun Li, Peng Xue, Yukun Li
Experimental Cell Research.2017; 360(2): 281. CrossRef - The Impact of Glucagon-Like Peptide-1 on Bone Metabolism and Its Possible Mechanisms
Chenhe Zhao, Jing Liang, Yinqiu Yang, Mingxiang Yu, Xinhua Qu
Frontiers in Endocrinology.2017;[Epub] CrossRef - Pathophysiology of Bone Fragility in Patients with Diabetes
Andrea Palermo, Luca D’Onofrio, Raffaella Buzzetti, Silvia Manfrini, Nicola Napoli
Calcified Tissue International.2017; 100(2): 122. CrossRef - Activation of GLP-1 Receptor Promotes Bone Marrow Stromal Cell Osteogenic Differentiation through β-Catenin
Jingru Meng, Xue Ma, Ning Wang, Min Jia, Long Bi, Yunying Wang, Mingkai Li, Huinan Zhang, Xiaoyan Xue, Zheng Hou, Ying Zhou, Zhibin Yu, Gonghao He, Xiaoxing Luo
Stem Cell Reports.2016; 6(4): 579. CrossRef - Mechanisms for the cardiovascular effects of glucagon-like peptide-1
H. Poudyal
Acta Physiologica.2016; 216(3): 277. CrossRef - Perspectives in GLP-1 Research: New Targets, New Receptors
Giulia Cantini, Edoardo Mannucci, Michaela Luconi
Trends in Endocrinology & Metabolism.2016; 27(6): 427. CrossRef - Chronic administration of Glucagon-like peptide-1 receptor agonists improves trabecular bone mass and architecture in ovariectomised mice
M. Pereira, J. Jeyabalan, C.S. Jørgensen, M. Hopkinson, A. Al-Jazzar, J.P. Roux, P. Chavassieux, I.R. Orriss, M.E. Cleasby, C. Chenu
Bone.2015; 81: 459. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Impact of Anti-hyperglycemic Medications on Bone Health
Naim M. Maalouf
Clinical Reviews in Bone and Mineral Metabolism.2015; 13(1): 43. CrossRef
- Effect of gut hormones on bone metabolism and their possible mechanisms in the treatment of osteoporosis

- A Case of Type I Osteogenesis Imperfecta Differentially Diagnosed as a Cause of a Spinal Compression Fracture.
- Sang Youl Rhee, Soo Young Moon, Suk Chon, In Kyung Jeong, Seungjoon Oh, Kyu Jeung Ahn, Ho Yeon Chung, Jeong Taek Woo, Sung Woon Kim, Young Seol Kim, Jin Woo Kim
- J Korean Endocr Soc. 2007;22(6):446-452. Published online December 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.6.446
- 1,838 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Osteogenesis imperfecta (OI) is a genetic disease that is caused by a synthetic anomaly of type I collagen. It is characterized by such features as low bone density, multiple fractures, bone deformities and chronic bone pain. According to the hereditary pattern and degree of phenotypical expression, it also has various extraskeletal manifestations such as blue sclera, hearing deformities and dentinogenesis imperfecta. Recently, an expanded seven subgroup classification of OI has been suggested by means of its clinical severity and mutational characteristics. However, most of the OI cases reported in Korea have been classified as type II or III that can be diagnosed easily and present with severe clinical manifestations. Only rare type I OI cases have been currently reported in Korea. Herein, we report a case of type I OI that was differentially diagnosed as a cause of a spinal compression fracture.

- Effects of Pamidronate Treatment on Osteogenesis Imperfecta.
- Seung Won Lee, Hyon J Kim, Jae Hyun Cho, Hyoung Suk Lee, Youn Mu Jung, Dae Jung Kim, Kwan Woo Lee, Yoon Sok Chung
- J Korean Endocr Soc. 2004;19(5):485-491. Published online October 1, 2004
- 1,037 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Osteogenesis imperfecta (OI) is a congenital disorder of type I collagen, with variable phenotypes, due to increased bone fragility and low bone mass. Previous pharmacological treatments for OI have been attempted with calcitonin and growth hormone but with little beneficial effects. Recently, Glorieux reported the beneficial effects of bisphosphonates in OI. METHODS: In this study, the effects of pamidronate treatment were evaluated in 9 patients with OI. All patients received intravenous pamidronate infusions, which was dose adjusted according to the patients' age. The outcome measures included the biochemical bone markers; serum alkaline phosphatase, urine deoxy-pyridinoline, urine Ca/Cr ratio, and bone mineral density (BMD). RESULTS: Serum alkaline phosphatase, urine deoxypyridinoline, and urine Ca/Cr ratio were slightly decreased after 1 year of therapy, although these changes were not statistically significant. The BMDs of the lumbar spine and proximal femur were significantly increased after 1-year of pamidronate treatment. No fractures were reported during the 1 year treatment periods. CONCLUSION: Pamidronate treatment had an effect on the BMD in osteogenesis imperfecta, probably due to decreasing bone resorption

- Clinical Characteristics of 10 Cases of Korean Osteogenesis Imperfecta.
- Hyoung Suk Lee, Hyon J Kim, Jae Hyun Cho, Seong Won Lee, Hyun A Kim, Joon Hyuck Choi, Young Jun Song, Dae Jung Kim, Kwan Woo Lee, Yoon Sok Chung
- J Korean Endocr Soc. 2003;18(5):496-503. Published online October 1, 2003
- 1,219 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Osteogenesis Imperfecta (OI) is a relatively rare hereditary disease, which is characterized by multiple bone fractures and spine scoliosis, due to the fragility of bone, and is often associated with blue sclerae, deafness and dentinogenesis imperfecta. Four types of OI can be distinguished, according to the clinical findings. Although mutations affecting type I collagen are responsible for the disease in most patients, the mechanism by which the genetic defects cause abnormal bone development remains to be fully understood. Here, the clinical characteristics of 10 OI patient cases are reported, with a review of the literature. All the cases, including 4 type I, 4 type III and 2 type IV, inherited OI as an autosomal dominant trait. All the subjects had multiple old fractures and decreased bone densities. In this study, the biochemical marker of bone formation, serum alkaline phosphatase, was found to be increased only in the pediatric OI patients, while the biochemical marker of bone resorption, urinary deoxypyridinoline, was increased in all cases. The mobility score was found to correlate with the severity of the type on diagnosis.

- Histomorphometry of Osteogenesis Imperfecta I.
- Seong Bin Hong, Suk Myun Ko, Yong Koo Park, Young Joo Park, Yoon Juo Oh, Young Wan Kim, Sung Ki Kim, Moon Suk Nam, Yong Seong Kim
- J Korean Endocr Soc. 2002;17(1):117-123. Published online February 1, 2002
- 1,081 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Osteoporosis imperfecta (OI) is a genetic disorder characterized by fragility of bone, deafness, blue sclerae; and laxity of joints. Four types of OI are distinguished by clinical findings. Although mutations affecting collagen I are responsible for the disease in the most patients, the mechanism by which the genetic defects cause abnormal bone development has not been well established. Therefore we evaluated static and dynamic bone histomorphometry of type I OI in the case study of a 15 year old boy with OI who had blue sclerae, a history of frequent fracture and a familial history of blue sclerae. Biopsy of the ilium showed loss of connection between the cortical bone and trabecular bones. The Harversian system in the cortical bone was poorly developed. In the trabecular bones, the lamellar pattern was poorly developed. Mineral apposition rate of the cortical bone was 1.0 m/day and of the trabecular bone was 0.79 m/day. Thus OI might be regard as a disease whereby abnormal collagen synthesis interferes with bone strength by multiple mechanisms.


 KES
KES

 First
First Prev
Prev



