Search
- Page Path
- HOME > Search
- Hypothalamus and pituitary gland
- Clinical Characteristics, Diagnosis, and Treatment of Thyroid Stimulating Hormone-Secreting Pituitary Neuroendocrine Tumor (TSH PitNET): A Single-Center Experience
- Jung Heo, Yeon-Lim Suh, Se Hoon Kim, Doo-Sik Kong, Do-Hyun Nam, Won-Jae Lee, Sung Tae Kim, Sang Duk Hong, Sujin Ryu, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim, Kyu Yeon Hur
- Endocrinol Metab. 2024;39(2):387-396. Published online February 5, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1877
- 1,476 View
- 42 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
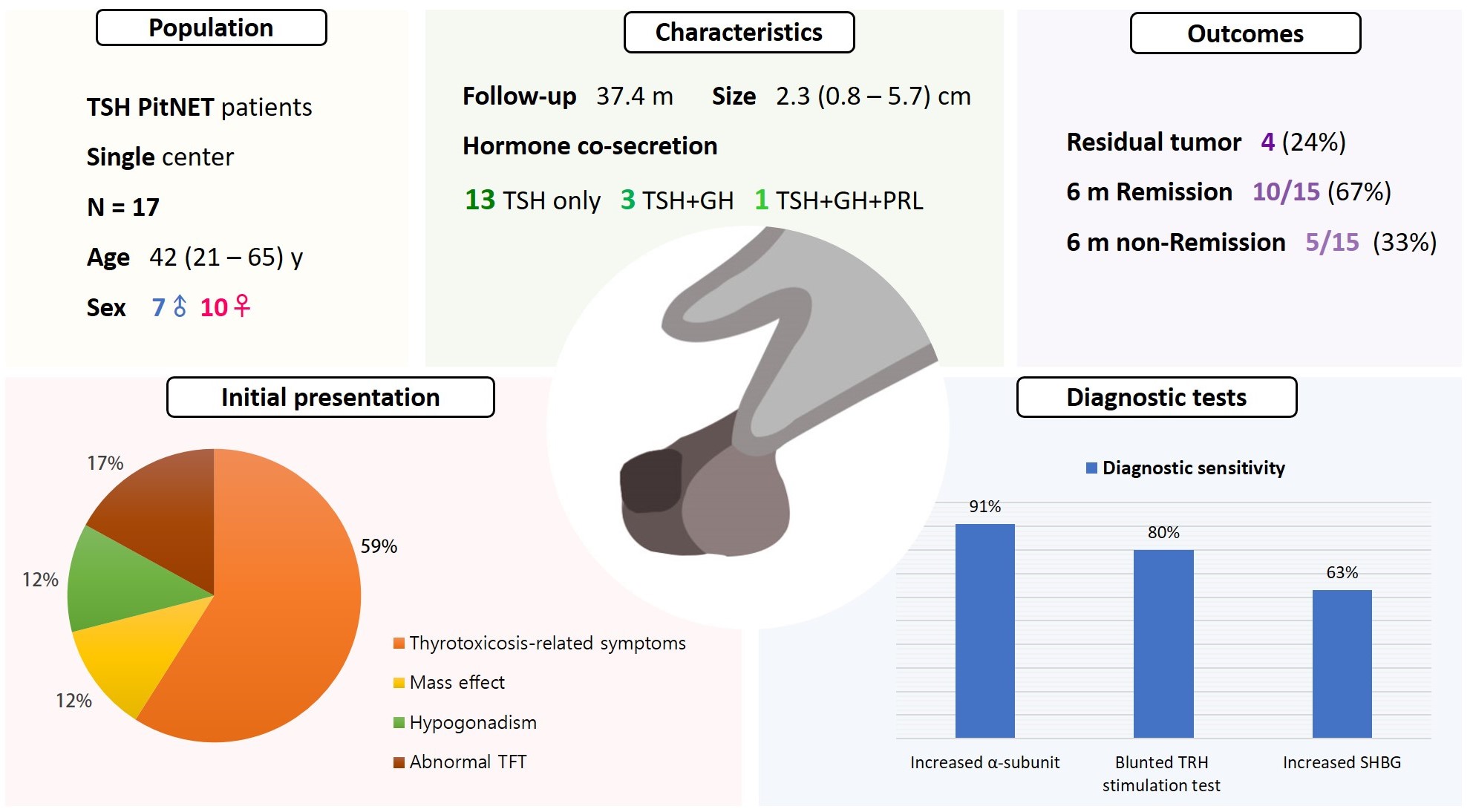
Thyroid-stimulating hormone (TSH)-secreting pituitary neuroendocrine tumor (TSH PitNET) is a rare subtype of PitNET. We investigated the comprehensive characteristics and outcomes of TSH PitNET cases from a single medical center. Also, we compared diagnostic methods to determine which showed superior sensitivity.
Methods
A total of 17 patients diagnosed with TSH PitNET after surgery between 2002 and 2022 in Samsung Medical Center was retrospectively reviewed. Data on comprehensive characteristics and treatment outcomes were collected. The sensitivities of diagnostic methods were compared.
Results
Seven were male (41%), and the median age at diagnosis was 42 years (range, 21 to 65); the median follow-up duration was 37.4 months. The most common (59%) initial presentation was hyperthyroidism-related symptoms. Hormonal co-secretion was present in four (23%) patients. Elevated serum alpha-subunit (α-SU) showed the greatest diagnostic sensitivity (91%), followed by blunted response at thyrotropin-releasing hormone (TRH) stimulation (80%) and elevated sex hormone binding globulin (63%). Fourteen (82%) patients had macroadenoma, and a specimen of one patient with heavy calcification was negative for TSH. Among 15 patients who were followed up for more than 6 months, 10 (67%) achieved hormonal and structural remission within 6 months postoperatively. A case of growth hormone (GH)/TSH/prolactin (PRL) co-secreting mixed gangliocytoma-pituitary adenoma (MGPA) was discovered.
Conclusion
The majority of the TSH PitNET cases was macroadenoma, and 23% showed hormone co-secretion. A rare case of GH/TSH/PRL co-secreting MGPA was discovered. Serum α-SU and TRH stimulation tests showed great diagnostic sensitivity. Careful consideration is needed in diagnosing TSH PitNET. Achieving remission requires complete tumor resection. In case of nonremission, radiotherapy or medical therapy can improve the long-term remission rate.

- Hypothalamus and pituitary gland
- Update on Current Evidence for the Diagnosis and Management of Nonfunctioning Pituitary Neuroendocrine Tumors
- Elizabeth Whyte, Masahiro Nezu, Constance Chik, Toru Tateno
- Endocrinol Metab. 2023;38(6):631-654. Published online November 15, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1838

- 2,420 View
- 152 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Pituitary neuroendocrine tumors (PitNETs) are the third most frequently diagnosed intracranial tumors, with nonfunctioning PitNETs (nfPitNETs) accounting for 30% of all pituitary tumors and representing the most common type of macroPitNETs. NfPitNETs are usually benign tumors with no evidence of hormone oversecretion except for hyperprolactinemia secondary to pituitary stalk compression. Due to this, they do not typically present with clinical syndromes like acromegaly, Cushing’s disease or hyperthyroidism and instead are identified incidentally on imaging or from symptoms of mass effects (headache, vision changes, apoplexy). With the lack of effective medical interventions, first-line treatment is transsphenoidal surgical resection, however, nfPitNETs often have supra- or parasellar extension, and total resection of the tumor is often not possible, resulting in residual tumor regrowth or reoccurrence. While functional PitNETs can be easily followed for recurrence using hormonal biomarkers, there is no similar parameter to predict recurrence in nfPitNETs, hence delaying early recognition and timely management. Therefore, there is a need to identify prognostic biomarkers that can be used for patient surveillance and as therapeutic targets. This review focuses on summarizing the current evidence on nfPitNETs, with a special focus on potential new biomarkers and therapeutics.
-
Citations
Citations to this article as recorded by- Phenotype Transformation of PitNETs
Zhenwei Li, Yinzi Wu, Guannan He, Renzhi Wang, Xinjie Bao
Cancers.2024; 16(9): 1731. CrossRef
- Phenotype Transformation of PitNETs

- Miscellaneous
- WD40-Repeat Proteins in Ciliopathies and Congenital Disorders of Endocrine System
- Yeonjoo Kim, Soo-Hyun Kim
- Endocrinol Metab. 2020;35(3):494-506. Published online September 8, 2020
- DOI: https://doi.org/10.3803/EnM.2020.302
- 14,900 View
- 199 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
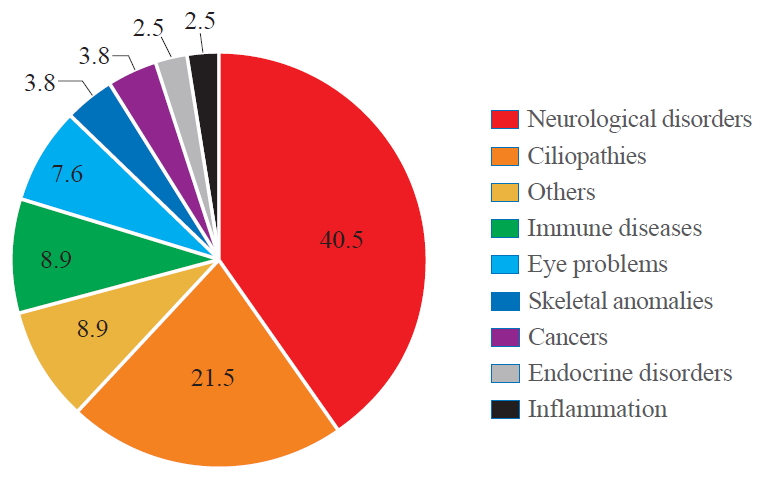
ePub - WD40-repeat (WDR)-containing proteins constitute an evolutionarily conserved large protein family with a broad range of biological functions. In human proteome, WDR makes up one of the most abundant protein-protein interaction domains. Members of the WDR protein family play important roles in nearly all major cellular signalling pathways. Mutations of WDR proteins have been associated with various human pathologies including neurological disorders, cancer, obesity, ciliopathies and endocrine disorders. This review provides an updated overview of the biological functions of WDR proteins and their mutations found in congenital disorders. We also highlight the significant role of WDR proteins in ciliopathies and endocrine disorders. The new insights may help develop therapeutic approaches targeting WDR motifs.
-
Citations
Citations to this article as recorded by- Exosomes Derived from Bone Marrow Mesenchymal Stem Cells Alleviate Rheumatoid Arthritis Symptoms via Shuttling Proteins
Lijun Wang, Fei Li, Liting Wang, Bingxing Wu, Min Du, Hua Xing, Shifeng Pan
Journal of Proteome Research.2024; 23(4): 1298. CrossRef - Structural screens identify candidate human homologs of insect chemoreceptors and cryptic Drosophila gustatory receptor-like proteins
Richard Benton, Nathaniel J Himmel
eLife.2023;[Epub] CrossRef - Changes in protein phosphorylation by insulin administration in the central nervous system of the gastropod mollusk Lymnaea stagnalis
Junko Nakai, Kengo Namiki, Yuki Totani, Shigeki Yasumasu, Teruki Yoshimura, Takashi Aoki, Etsuro Ito
Biophysics and Physicobiology.2023; 20(4): n/a. CrossRef - Unveiling Distinct Proteomic Signatures in Complicated Crohn’s Disease That Could Predict the Disease Course
Laura A. Lucaciu, Radu Seicean, Alina Uifălean, Maria Iacobescu, Cristina A. Iuga, Andrada Seicean
International Journal of Molecular Sciences.2023; 24(23): 16966. CrossRef - Aromatic patterns: Tryptophan aromaticity as a catalyst for the emergence of life and rise of consciousness
Amal Alachkar
Physics of Life Reviews.2022; 42: 93. CrossRef - EML2-S constitutes a new class of proteins that recognizes and regulates the dynamics of tyrosinated microtubules
Takashi Hotta, Thomas S. McAlear, Yang Yue, Takumi Higaki, Sarah E. Haynes, Alexey I. Nesvizhskii, David Sept, Kristen J. Verhey, Susanne Bechstedt, Ryoma Ohi
Current Biology.2022; 32(18): 3898. CrossRef - Susceptibility of craniofacial ciliopathies to oral cancer-A proposed research
G Arun Kumar
Journal of Dental Health, Oral Disorders & Therapy.2022; 13(2): 41. CrossRef - A WDR47 homolog facilitates ciliogenesis by modulating intraflagellar transport
Chun-Xue Song, Xian-Ting Zeng, Wan-Xin Zeng, Rong Liu, Xia-Jing Tong, Qian Li
Journal of Cell Science.2022;[Epub] CrossRef - Biallelic loss-of-function variants in WDR11 are associated with microcephaly and intellectual disability
Natja Haag, Ene-Choo Tan, Matthias Begemann, Lars Buschmann, Florian Kraft, Petra Holschbach, Angeline H. M. Lai, Maggie Brett, Ganeshwaran H. Mochida, Stephanie DiTroia, Lynn Pais, Jennifer E. Neil, Muna Al-Saffar, Laila Bastaki, Christopher A. Walsh, In
European Journal of Human Genetics.2021; 29(11): 1663. CrossRef
- Exosomes Derived from Bone Marrow Mesenchymal Stem Cells Alleviate Rheumatoid Arthritis Symptoms via Shuttling Proteins

- Thyroid
- A Calcitonin-Negative Neuroendocrine Tumor Derived from Follicular Lesions of the Thyroid
- Ga Young Kim, Chul Yun Park, Chang Ho Cho, June Sik Park, Eui Dal Jung, Eon Ju Jeon
- Endocrinol Metab. 2015;30(2):221-225. Published online December 9, 2014
- DOI: https://doi.org/10.3803/EnM.2015.30.2.221
- 3,406 View
- 30 Download
- 7 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Neuroendocrine lesions of the thyroid are rare. The most common types are medullary thyroid carcinomas (MTCs) and C-cell hyperplasia. MTCs originate from thyroid parafollicular cells that secrete calcitonin which serves as a serum marker of MTCs. Here, the rare case of a calcitonin-negative neuroendocrine tumor (NET) derived from follicular lesions of the thyroid is described. A 34-year-old man presented at our hospital for the surgical management of an incidental thyroid nodule that was observed on an ultrasound sonography (USG) of the neck. Initially, USG-guided aspiration cytology was performed, and a MTC was suspected. The expressions of thyroglobulin and thyroid transcription factor-1, which are thyroid follicular cell markers, and synaptophysin and chromogranin A, which are neuroendocrine markers, was confirmed following surgical pathology. However, the staining of calcitonin, a marker of MTCs, was not observed. A nonmedullary NET of the thyroid is uncommon, and the distinction between calcitonin-negative NETs and MTCs of the thyroid may be important due to differences in their clinical courses and management.
-
Citations
Citations to this article as recorded by- Calcitonin-Negative Neuroendocrine Carcinoma of the Thyroid Gland: Case Report and Literature Review
Ricardo Fernández-Ferreira, Ildefonso Roberto De la Peña-López, Karla Walkiria Zamudio-Coronado, Luis Antonio Delgado-Soler, María Eugenia Torres-Pérez, Christianne Bourlón-de los Ríos, Rubén Cortés-González
Case Reports in Oncology.2021; 14(1): 112. CrossRef - Calcitonin-negative neuroendocrine tumor of the thyroid with metastasis to liver-rare presentation of an unusual tumor: A case report and review of literature
Huai-Jie Cai, Han Wang, Nan Cao, Bin Huang, Fan-Lei Kong, Li-Ren Lu, Ya-Yuan Huang, Wei Wang
World Journal of Clinical Cases.2020; 8(1): 179. CrossRef - Medullary thyroid carcinoma with double negative calcitonin and CEA: a case report and update of literature review
Claudio Gambardella, Chiara Offi, Guglielmo Clarizia, Roberto Maria Romano, Immacolata Cozzolino, Marco Montella, Rosa Maria Di Crescenzo, Massimo Mascolo, Angelo Cangiano, Sergio Di Martino, Giancarlo Candela, Giovanni Docimo
BMC Endocrine Disorders.2019;[Epub] CrossRef - Calcitonin negative Medullary Thyroid Carcinoma: a challenging diagnosis or a medical dilemma?
Claudio Gambardella, Chiara Offi, Renato Patrone, Guglielmo Clarizia, Claudio Mauriello, Ernesto Tartaglia, Francesco Di Capua, Sergio Di Martino, Roberto Maria Romano, Lorenzo Fiore, Alessandra Conzo, Giovanni Conzo, Giovanni Docimo
BMC Endocrine Disorders.2019;[Epub] CrossRef - Calcitonin-Negative Neuroendocrine Tumor of the Thyroid
Megan Parmer, Stacey Milan, Alireza Torabi
International Journal of Surgical Pathology.2017; 25(2): 191. CrossRef - Clinical and pathological analysis of 19 cases of medullary thyroid carcinoma without an increase in calcitonin
Qiufeng Zhou, Shuanglei Yue, Ye Cheng, Ju Jin, Haimiao Xu
Experimental and Toxicologic Pathology.2017; 69(8): 575. CrossRef - Primary Calcitonin-negative Neuroendocrine Tumor
Sabri Özden, Aysel Colak, Baris Saylam, Ömer Cengiz
World Journal of Endocrine Surgery.2017; 9(3): 104. CrossRef - LONG-TERM RESULTS OF SURGICAL TREATMENT OF PATIENTS WITH FOLLICULAR TUMORS OF THE THYROID
I. N. Zubarovskiy, M. V. Mikhailova, S. K. Osipenko
Grekov's Bulletin of Surgery.2015; 174(5): 32. CrossRef
- Calcitonin-Negative Neuroendocrine Carcinoma of the Thyroid Gland: Case Report and Literature Review

- Transformation of Nonfunctioning Pancreatic Neuroendocrine Carcinoma Cells into Insulin Producing Cells after Treatment with Sunitinib
- Jung Hun Ohn, Yeong Gi Kim, Se-Hoon Lee, Hye Seung Jung
- Endocrinol Metab. 2013;28(2):149-152. Published online June 18, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.2.149
- 3,167 View
- 35 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader We report a rare case of severe hypoglycemia after sunitinib treatment for pancreatic neuroendocrine carcinoma. We describe the initial clinical presentation, laboratory results, pathologic findings, and managment in a patient with a nonfunctioning pancreatic neuroendocrine carcinoma with liver metastases who developed life threatening hypoglycemia after 2 months of sunitinib therapy. A 46-year-old woman presented to the emergency department with loss of consciousness from hypoglycemia. Serum C-peptide and insulin levels at fasting state revealed that the hypoglycemia resulted from endogenous hyperinsulinemia. She had been diagnosed with nonfunctioning pancreatic neuroendocrine carcinoma based on a biopsy of metastatic cervical lymph node and was being treated with sunitinib, a small molecule tyrosine kinase inhibitor. Immunohistochemical stain of the metastatic liver mass demonstrated that the initially nonfunctioning neuroendocrine carcinoma cells had changed into insulin-producing cells after sunitinib therapy. Transarterial chemoembolization of the liver masses and systemic chemotherapy with streptozotocin/adriamycin relieved the hypoglycemia. A nonfunctioning pancreatic neuroendocrine carcinoma was transformed into an insulin-producing tumor after treatment with sunitinib, causing endogenous hyperinsulinemia and severe hypoglycemia.
-
Citations
Citations to this article as recorded by- Small Insulinoma Followed-up as an Indolent Pancreatic Tumor: A Case Report
Hiroki Sato, Shozaburo Fujii, Tetsuhiro Okada, Hidemasa Kawabata, Yuki Kamikokura, Mikihiro Fujiya
Internal Medicine.2024;[Epub] CrossRef - A Case of a Metastatic Pancreatic Neuroendocrine Tumor: A Surgical Conundrum Wrapped in Functionality's Embrace
Adam Mylonakis, Michail Vailas, Panagiotis Sakarellos, Lysandros Karydakis, Eleandros Kyros, Spyridon Davakis, Alexandros Papalampros, Evaggelos Felekouras
Cureus.2024;[Epub] CrossRef - Malignant Insulinoma Arising From Nonfunctioning Pancreatic Neuroendocrine Tumor
Ritodhi Chatterjee, Basim Ali, Son H. Nguyen, Rui Chen, Yvonne H. Sada
ACG Case Reports Journal.2023; 10(1): e00954. CrossRef - Case Report: Giant insulinoma, a very rare tumor causing hypoglycemia
Georges Tarris, Alexia Rouland, Kévin Guillen, Romaric Loffroy, Anne-Cécile Lariotte, Patrick Rat, Benjamin Bouillet, Haingo Andrianiaina, Jean-Michel Petit, Laurent Martin
Frontiers in Endocrinology.2023;[Epub] CrossRef - Case Reports: Transformation of End-Stage Neuroendocrine Tumors With Uncontrollable Liver Metastasis Into a Novel or Additional Functional Phenotype
Takaomi Kessoku, Noritoshi Kobayashi, Masato Yoneda, Yuki Kasai, Anna Ozaki, Naoki Okubo, Michihiro Iwaki, Takashi Kobayashi, Tsutomu Yoshihara, Yusuke Kurita, Yasushi Honda, Motohiko Tokuhisa, Hiroto Ishiki, Takashi Hibiya, Satoshi Fujii, Atsushi Nakajim
Frontiers in Oncology.2020;[Epub] CrossRef - Transformation of a non-secretory neuroendocrine tumor to insulinoma after treatment with Sunitinib: A case report and review of the literature
Todd Clover, Amrou Abdelkader, Guru Subramanian Guru Murthy
Journal of Oncology Pharmacy Practice.2019; 25(6): 1516. CrossRef - Hyperglycaemia Induced by Novel Anticancer Agents: An Undesirable Complication or a Potential Therapeutic Opportunity?
Rashmi R. Shah
Drug Safety.2017; 40(3): 211. CrossRef - Medical management of secretory syndromes related to gastroenteropancreatic neuroendocrine tumours
Georgios K Dimitriadis, Martin O Weickert, Harpal S Randeva, Gregory Kaltsas, Ashley Grossman
Endocrine-Related Cancer.2016; 23(9): R423. CrossRef - Different Hormonal Expression Patterns Between Primary Pancreatic Neuroendocrine Tumors and Metastatic Sites
Hideyo Kimura, Takao Ohtsuka, Takaaki Fujimoto, Kenjiro Date, Taketo Matsunaga, Ana Ines Cases, Atsushi Abe, Yusuke Mizuuchi, Yoshihiro Miyasaka, Tetsuhide Ito, Yoshinao Oda, Masafumi Nakamura, Masao Tanaka
Pancreas.2016; 45(7): 947. CrossRef - Tyrosine Kinase Inhibitors and Diabetes: A Novel Treatment Paradigm?
Athanasios Fountas, Leonidas-Nikolaos Diamantopoulos, Agathocles Tsatsoulis
Trends in Endocrinology & Metabolism.2015; 26(11): 643. CrossRef - Transformation of nonfunctioning pancreatic tumor into malignant insulinoma after 3 years: an uncommon clinical course of insulinoma
Muyesser Sayki Arslan, Mustafa Ozbek, Melia Karakose, Esra Tutal, Bekir Ucan, Demet Yilmazer, Alper Dilli, Salih Sinan Gultekin, Erman Cakal, Tuncay Delibasi
Archives of Endocrinology and Metabolism.2015; 59(3): 270. CrossRef - Pancreatic neuroendocrine tumors with transformation to insulinoma: an unusual presentation of a rare disease
Avital Nahmias, Simona Grozinsky-Glasberg, Asher Salmon, David J Gross
Endocrinology, Diabetes & Metabolism Case Reports.2015;[Epub] CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Small Insulinoma Followed-up as an Indolent Pancreatic Tumor: A Case Report

- A Case of Ectopic ACTH Syndrome Associated with Metastatic Prostate Cancer.
- Eun Ky Kim, Soo Heon Kwak, Hwa Young Ahn, Ah Reum Khang, Hyo Jin Park, So Yeon Park, Sang Eun Lee, Hak Chul Jang, Seong Yeon Kim, Young Joo Park
- Endocrinol Metab. 2012;27(3):237-243. Published online September 19, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.3.237
- 1,813 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Ectopic adrenocorticotropic hormone (ACTH) syndrome is mostly associated with neuroendocrine tumors and small cell carcinoma of the lung. This syndrome of prostate cancer is rare and has been reported in only a few cases. We report a patient with ectopic ACTH production associated with metastatic prostate cancer. A 70-year-old patient with metastatic prostate cancer was admitted to our hospital with septic shock. He had a history of hormonal therapy and transurethral prostatectomy. Adrenocortical function was checked due to consistent fever and poor general condition, which revealed markedly increased levels of basal plasma ACTH and serum cortisol. The patient did not present typical signs of the Cushing's syndrome, however, hypokalemia and a history of hypertension were found. He died in days as a result of multi-organ failure. On pathology, the prostatectomy specimen showed a tumor composed of mixed populations of adenocarcinoma and small cell carcinoma. The tumor cells in the small cell component were positive for chromogranin and ACTH. Although neuroendocrine differentiation in prostate cancer is rare, etopic ACTH production should be considered in patients with prostate cancer as well as in clinical features of ACTH hypersecretion.

- A Case of von Hippel-Lindau Disease Presenting with Pancreatic Neuroendocrine Tumor.
- Jung Hun Ohn, Junghee Kim, Hyun Jung Lee, Won Woo Seo, Yul Hwang-Bo, Eun Shil Hong, Jin Joo Park, Seong Yeon Kim
- Endocrinol Metab. 2011;26(1):89-91. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.89
- 2,000 View
- 20 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Von Hippel-Lindau (VHL) disease is an autosomal dominant disorder that results from a germline mutation of the VHL gene. The affected individuals might develop several benign or malignant tumors such as central nervous system or retinal haemangioblastomas, endolymphatic sac tumors, renal cell carcinomas, pheochromocytomas or pancreatic cysts and neuroendocrine tumors. We report here on a case of a 21 year old female with von Hippel-Lindau disease and she presented with only pancreatic neuroendocrine tumor and no evidence of haemangioblastomas or other visceral complications. Further, direct sequencing of the VHL gene reveals a novel germline frameshift mutation of codon 198 from the deletion of nucleotide 592 (cytosine), leading to truncation of the VHL protein.
-
Citations
Citations to this article as recorded by- Germline mutation of Glu70Lys is highly frequent in Korean patients with von Hippel–Lindau (VHL) disease
Sena Hwang, Cheol Ryong Ku, Ji In Lee, Kyu Yeon Hur, Myung-Shik Lee, Chul-Ho Lee, Kyo Yeon Koo, Jin-Sung Lee, Yumie Rhee
Journal of Human Genetics.2014; 59(9): 488. CrossRef
- Germline mutation of Glu70Lys is highly frequent in Korean patients with von Hippel–Lindau (VHL) disease

- 2 Cases of Ectopic ACTH Syndrome due to Thymic Neuroendocrine Carcinoma Associated with Different Clinical Manifestations.
- Yu Jeong Park, Moon Kyu Lee, Jong Ryeal Hahm, Jung Ho Do, Sang Taek Heo, Ju Sung Kim, Yong Ki Min, Myung Shik Lee, Kwang Won Kim, Joung Ho Han
- J Korean Endocr Soc. 2001;16(1):115-122. Published online February 1, 2001
- 1,037 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Primary neuroendocrine carcinoma of the thymus (formerly known as thymic carcinoids) are unusual tumors that account for 5% of all anterior mediastinal neoplasms. Thymic neuroendocrine carcinomas exhibit a much more aggressive behavior than those originating from other foregut locations and are associated with the ectopic ACTH syndrome in 38% of cases. Patients having a thymic neuroendocrine carcinoma usually present with symptoms such as chest tightness, dyspnea, a palpable neck mass and sometimes a weight gain. We report on 2 patients with thymic neuroendocrine carcinoma who showed different clinical manifestations each other. One presented with a typical. Cushingoid appearance and the other had symptoms of fatigue and weight loss which is a common symptom of malignant tumors.


 KES
KES

 First
First Prev
Prev



