Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- Effects of an Electronic Medical Records-Linked Diabetes Self-Management System on Treatment Targets in Real Clinical Practice: Retrospective, Observational Cohort Study
- So Jung Yang, Sun-Young Lim, Yoon Hee Choi, Jin Hee Lee, Kun-Ho Yoon
- Endocrinol Metab. 2024;39(2):364-374. Published online March 21, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1878

- 1,025 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study evaluated the effects of a mobile diabetes management program called “iCareD” (College of Medicine, The Catholic University of Korea) which was integrated into the hospital’s electronic medical records system to minimize the workload of the healthcare team in the real clinical practice setting.
Methods
In this retrospective observational study, we recruited 308 patients. We categorized these patients based on their compliance regarding their use of the iCareD program at home; compliance was determined through self-monitored blood glucose inputs and message subscription rates. We analyzed changes in the ABC (hemoglobin A1c, blood pressure, and low-density lipoprotein cholesterol) levels from the baseline to 12 months thereafter, based on the patients’ iCareD usage patterns.
Results
The patients comprised 92 (30%) non-users, 170 (55%) poor-compliance users, and 46 (15%) good-compliance users; the ABC target achievement rate showed prominent changes in good-compliance groups from baseline to 12 months (10.9% vs. 23.9%, P<0.05), whereas no significant changes were observed for poor-compliance users and non-users (13.5% vs. 18.8%, P=0.106; 20.7% vs. 14.1%, P=0.201; respectively).
Conclusion
Implementing the iCareD can improve the ABC levels of patients with diabetes with minimal efforts of the healthcare team in real clinical settings. However, the improvement of patients’ compliance concerning the use of the system without the vigorous intervention of the healthcare team needs to be solved in the future.

- Thyroid
- Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
- Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
- Endocrinol Metab. 2023;38(4):381-391. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1778

- 3,117 View
- 463 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Subclinical hypothyroidism (SCH) is characterized by elevated thyroid-stimulating hormone (TSH) and normal free thyroxine levels. The Korean Thyroid Association recently issued a guideline for managing SCH, which emphasizes Korean-specific TSH diagnostic criteria and highlights the health benefits of levothyroxine (LT4) treatment. A serum TSH level of 6.8 mIU/L is presented as the reference value for diagnosing SCH. SCH can be classified as mild (TSH 6.8 to 10.0 mIU/L) or severe (TSH >10.0 mIU/L), and patients can be categorized as adults (age <70 years) or elderly (age ≥70 years), depending on the health effects of LT4 treatment. An initial increase in serum TSH levels should be reassessed with a subsequent measurement, including a thyroid peroxidase antibody test, preferably 2 to 3 months after the initial assessment. While LT4 treatment is not generally recommended for mild SCH in adults, it is necessary for severe SCH in patients with underlying coronary artery disease or heart failure and it may be considered for those with concurrent dyslipidemia. Conversely, LT4 treatment is generally not recommended for elderly patients, regardless of SCH severity. For those SCH patients who are prescribed LT4 treatment, the dosage should be personalized, and serum TSH levels should be regularly monitored to maintain the optimal LT4 regimen.
-
Citations
Citations to this article as recorded by- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism
Won Sang Yoo
Endocrinology and Metabolism.2024; 39(1): 188. CrossRef
- Clinical Implications of Different Thyroid-Stimulating Hormone (TSH) Reference Intervals between TSH Kits for the Management of Subclinical Hypothyroidism

- Diabetes, Obesity and Metabolism
- Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
- Eun-Jung Rhee
- Endocrinol Metab. 2022;37(3):415-429. Published online June 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.304

- 4,553 View
- 263 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The world is suffering from a rapid increase in the number of people with diabetes due to the increased prevalence of obesity and lengthened life span. Since the development of insulin thanks to the efforts of Prof. Banting and Dr. Best in 1922, for which they won the Nobel Prize, remarkable developments in anti-diabetic medications have dramatically lengthened the lifespan of patients with diabetes. However, the control rate of hyperglycemia in patients with diabetes remains unsatisfactory, since glycemic control requires both medication and lifestyle modifications to slow the deterioration of pancreatic beta-cell function and prevent diabetic complications. From the initial “triumvirate” to the “ominous octet,” and now the “egregious eleven,” the number of organs recognized as being involved in hyperglycemia and diabetes has increased with the development of anti-diabetic medications. Recent unexpected results from outcome trials of anti-diabetic medications have enabled anti-diabetic medications to be indicated for the prevention of chronic kidney disease and heart failure, even in patients without diabetes. In this review, I would like to summarize the extra-glycemic effects of anti-diabetic medications.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Glucagon-Like Peptide Receptor Agonist Inhibits Angiotensin II-Induced Proliferation and Migration in Vascular Smooth Muscle Cells and Ameliorates Phosphate-Induced Vascular Smooth Muscle Cells Calcification
Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2024; 48(1): 83. CrossRef - To do one and to get more: Part I. Diabetes and bone
Wen-Ling Lee, Peng-Hui Wang, Szu-Ting Yang, Chia-Hao Liu, Wen-Hsun Chang, Fa-Kung Lee
Journal of the Chinese Medical Association.2022; 85(10): 965. CrossRef
- Association between underweight and risk of heart failure in diabetes patients

- Thyroid
- T4+T3 Combination Therapy: An Unsolved Problem of Increasing Magnitude and Complexity
- Wilmar M. Wiersinga
- Endocrinol Metab. 2021;36(5):938-951. Published online September 30, 2021
- DOI: https://doi.org/10.3803/EnM.2021.501
- 9,048 View
- 336 Download
- 11 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
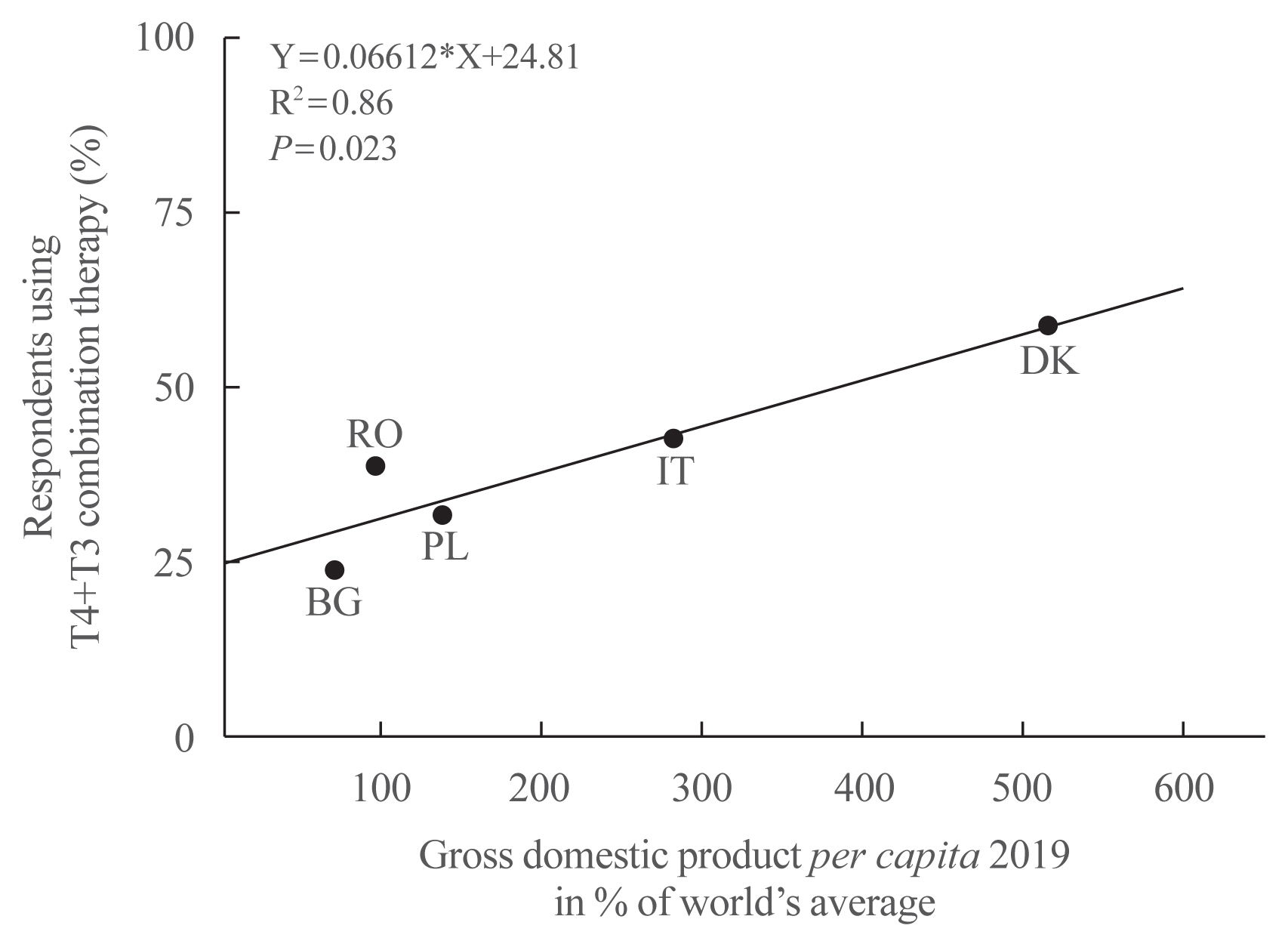
ePub - Thyroxine (T4)+triiodothyronine (T3) combination therapy can be considered in case of persistent symptoms despite normal serum thyroid stimulating hormone in levothyroxine (LT4)-treated hypothyroid patients. Combination therapy has gained popularity in the last two decades, especially in countries with a relatively high gross domestic product. The prevalence of persistent symptoms has also increased; most frequent are complaints about energy levels and fatigue (80% to 90%), weight management (70% to 75%), memory (60% to 80%), and mood (40% to 50%). Pathophysiological explanations for persistent problems are unrealistic patient expectations, comorbidities, somatic symptoms, related disorders (Diagnostic and Statistical Manual of Mental Disorders [DSM-5]), autoimmune neuroinflammation, and low tissue T3. There is fair circumstantial evidence for the latter cause (tissue and specifically brain T3 content is normalized by T4+T3, not by T4 alone), but the other causes are viewed as more relevant in current practice. This might be related to the ‘hype’ that has emerged surrounding T4+T3 therapy. Although more and better-designed trials are needed to validate the efficacy of T4+T3 combination, the management of persistent symptoms should also be directed towards alternative causes. Improving the doctor-patient relationship and including more and better information is crucial. For example, dissatisfaction with the outcomes of T4 treatment for subclinical hypothyroidism can be anticipated as recent trials have demonstrated that LT4 is hardly effective in improving symptoms associated with subclinical hypothyroidism.
-
Citations
Citations to this article as recorded by- Association of DIO2 and MCT10 Polymorphisms With Persistent Symptoms in LT4-Treated Patients in the UK Biobank
Christian Zinck Jensen, Jonas Lynggaard Isaksen, Gustav Ahlberg, Morten Salling Olesen, Birte Nygaard, Christina Ellervik, Jørgen Kim Kanters
The Journal of Clinical Endocrinology & Metabolism.2024; 109(2): e613. CrossRef - Quality of life, daily functioning, and symptoms in hypothyroid patients on thyroid replacement therapy: A Dutch survey
Ellen Molewijk, Eric Fliers, Koen Dreijerink, Ad van Dooren, Rob Heerdink
Journal of Clinical & Translational Endocrinology.2024; 35: 100330. CrossRef - Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Use of Thyroid Hormones in Hypothyroid and Euthyroid Patients: A THESIS questionnaire survey of members of the Irish Endocrine Society
Mohamad Mustafa, Elsheikh Ali, Anne McGowan, Laura McCabe, Laszlo Hegedüs, Roberto Attanasio, Endre V. Nagy, Enrico Papini, Petros Perros, Carla Moran
Irish Journal of Medical Science (1971 -).2023; 192(5): 2179. CrossRef - Levothyroxine: Conventional and Novel Drug Delivery Formulations
Hanqing Liu, Wei Li, Wen Zhang, Shengrong Sun, Chuang Chen
Endocrine Reviews.2023; 44(3): 393. CrossRef - Re: “Exploring the Genetic Link Between Thyroid Dysfunction and Common Psychiatric Disorders: A Specific Hormonal or a General Autoimmune Comorbidity” by Soheili-Nezhad et al.
Christiaan F. Mooij, A.S. Paul van Trotsenburg
Thyroid®.2023; 33(8): 999. CrossRef - Circulating thyroid hormones and clinical parameters of heart failure in men
Iva Turić, Ivan Velat, Željko Bušić, Viktor Čulić
Scientific Reports.2023;[Epub] CrossRef - Evaluation of cortical and trabecular bone structure of the mandible in patients using L-Thyroxine
Melike Gulec, Melek Tassoker, Mediha Erturk
BMC Oral Health.2023;[Epub] CrossRef - The Impact of Hypothyroidism on Satisfaction with Care and Treatment and Everyday Living: Results from E-Mode Patient Self-Assessment of Thyroid Therapy, a Cross-Sectional, International Online Patient Survey
Petros Perros, Laszlo Hegedüs, Endre Vezekenyi Nagy, Enrico Papini, Harriet Alexandra Hay, Juan Abad-Madroñero, Amy Johanna Tallett, Megan Bilas, Peter Lakwijk, Alan J. Poots
Thyroid.2022;[Epub] CrossRef
- Association of DIO2 and MCT10 Polymorphisms With Persistent Symptoms in LT4-Treated Patients in the UK Biobank

- Adrenal gland
- Is Follow-up of Adrenal Incidentalomas Always Mandatory?
- Giuseppe Reimondo, Alessandra Muller, Elisa Ingargiola, Soraya Puglisi, Massimo Terzolo
- Endocrinol Metab. 2020;35(1):26-35. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.26

- 6,514 View
- 250 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Adrenal masses are mainly detected unexpectedly by an imaging study performed for reasons unrelated to any suspect of adrenal diseases. Such masses are commonly defined as “adrenal incidentalomas” and represent a public health challenge because they are increasingly recognized in current medical practice. Management of adrenal incidentalomas is currently matter of debate. Although there is consensus on the need of a multidisciplinary expert team evaluation and surgical approach in patients with significant hormonal excess and/or radiological findings suspicious of malignancy demonstrated at the diagnosis or during follow-up, the inconsistency between official guidelines and the consequent diffuse uncertainty on management of small adrenal incidentalomas still represents a considerable problem in terms of clinical choices in real practice. The aim of the present work is to review the proposed strategies on how to manage patients with adrenal incidentalomas that are not candidates to immediate surgery. The recent European Society of Endocrinology/European Network for the Study of Adrenal Tumors guidelines have supported the view to avoid surveillance in patients with clear benign adrenal lesions <4 cm and/or without any hormonal secretion; however, newer prospective studies are needed to confirm safety of this strategy, in particular in younger patients.
-
Citations
Citations to this article as recorded by- Adrenal Incidentaloma—Innocent Bystander or Intruder?
Laurence Amar, Inga Harbuz-Miller, Adina F Turcu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1303. CrossRef - Diagnosing and managing adrenal incidentalomas
Justine Herndon, Irina Bancos
JAAPA.2023; 36(5): 12. CrossRef - Tumor enlargement in adrenal incidentaloma is related to glaucoma: a new prognostic feature?
M. Caputo, T. Daffara, A. Ferrero, M. Romanisio, E. Monti, C. Mele, M. Zavattaro, S. Tricca, A. Siani, A. Clemente, C. Palumbo, S. De Cillà, A. Carriero, A. Volpe, P. Marzullo, G. Aimaretti, F. Prodam
Journal of Endocrinological Investigation.2023; 47(2): 377. CrossRef - The Role of Biomarkers in Adrenocortical Carcinoma: A Review of Current Evidence and Future Perspectives
Maja Mizdrak, Tina Tičinović Kurir, Joško Božić
Biomedicines.2021; 9(2): 174. CrossRef - An Adrenocortical Carcinoma Evolving After Nine Years of Latency From a Small Adrenal Incidentaloma
Harpreet S Kohli, Sukesh Manthri, Shikha Jain, Rahul Kashyap, Sheng Chen, Thoyaja Koritala, Aysun Tekin, Ramesh Adhikari, Raghavendra Tirupathi, Aram Barbaryan, Simon Zec, Hanyin Wang, Stephanie Welle, Pavan Devulapally, Mack Sheraton, Manpreet Kaur, Vish
Cureus.2021;[Epub] CrossRef - Diagnostic algorithm of the subclinical forms of adrenal neoplasms
Sofya G. Blyumina, Pavel N. Romashchenko, Igor S. Zheleznyak
Bulletin of the Russian Military Medical Academy.2021; 23(3): 67. CrossRef
- Adrenal Incidentaloma—Innocent Bystander or Intruder?

- Thyroid
- The Diagnosis and Management of Hyperthyroidism in Korea: Consensus Report of the Korean Thyroid Association
- Jae Hoon Moon, Ka Hee Yi
- Endocrinol Metab. 2013;28(4):275-279. Published online December 12, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.4.275
- 5,389 View
- 70 Download
- 54 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hyperthyroidism is one of the causes of thyrotoxicosis and the most common cause of hyperthyroidism in Korea is Graves disease. The diagnosis and treatment of Graves disease are different according to geographical area. Recently, the American Thyroid Association and the American Association of Clinical Endocrinologists suggested new management guidelines for hyperthyroidism. However, these guidelines are different from clinical practice in Korea and are difficult to apply. Therefore, the Korean Thyroid Association (KTA) conducted a survey of KTA members regarding the diagnosis and treatment of hyperthyroidism, and reported the consensus on the management of hyperthyroidism. In this review, we summarized the KTA report on the contemporary practice patterns in the diagnosis and management of hyperthyroidism, and compared this report with guidelines from other countries.
-
Citations
Citations to this article as recorded by- Effect of previous administration of potassium iodine and different durations of low iodine diets for radioiodine therapy on the treatment of Graves' disease in iodine-rich areas
Mika Tamura, Kunihiro Nakada, Haruna Iwanaga, Naotoshi Fujita, Katsuhiko Kato
European Journal of Nuclear Medicine and Molecular Imaging.2024; 51(4): 1060. CrossRef - Effects of altitude on thyroid disorders according to Chinese three-rung, ladder-like topography: national cross-sectional study
Boshen Gong, Youmin Wang, Jin-an Zhang, Qiao Zhang, Jiajun Zhao, Jiashu Li, Xichang Wang, Yutong Han, Ziwei Yu, Chenyu Zhang, Bingcong Peng, Yumin Xing, Qiuxian Li, Ping Wang, Yongze Li, Weiping Teng, Zhongyan Shan
BMC Public Health.2024;[Epub] CrossRef - MACE and Hyperthyroidism Treated With Medication, Radioactive Iodine, or Thyroidectomy
Carol Chiung-Hui Peng, Yu-Jie Lin, Sun Y. Lee, Shu-Man Lin, Cheng Han, Ching-Hui Loh, Huei-Kai Huang, Elizabeth N. Pearce
JAMA Network Open.2024; 7(3): e240904. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - A machine learning-assisted system to predict thyrotoxicosis using patients’ heart rate monitoring data: a retrospective cohort study
Kyubo Shin, Jongchan Kim, Jaemin Park, Tae Jung Oh, Sung Hye Kong, Chang Ho Ahn, Joon Ho Moon, Min Joo Kim, Jae Hoon Moon
Scientific Reports.2023;[Epub] CrossRef - Immunometabolic signatures predict recovery from thyrotoxic myopathy in patients with Graves' disease
Daiki Setoyama, Ho Yeop Lee, Ji Sun Moon, Jingwen Tian, Yea Eun Kang, Ju Hee Lee, Minho Shong, Dongchon Kang, Hyon‐Seung Yi
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(1): 355. CrossRef - Comparison of 99mTc Pertechnetate Thyroid Uptake Rates by Gamma Probe and Gamma Camera Methods for Differentiating Graves’ Disease and Thyroiditis
Meihua Jin, Jonghwa Ahn, Seong-gil Jo, Jangwon Park, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Jin-Sook Ryu
Nuclear Medicine and Molecular Imaging.2022; 56(1): 42. CrossRef - KSNM60 in Nuclear Endocrinology: from the Beginning to the Future
Chae Moon Hong, Young Jin Jeong, Hae Won Kim, Byeong-Cheol Ahn
Nuclear Medicine and Molecular Imaging.2022; 56(1): 17. CrossRef - Graves’ disease and the risk of Parkinson’s disease: a Korean population-based study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Jinyoung Youn, Ji Oh Mok, Chul-Hee Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Brain Communications.2022;[Epub] CrossRef - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Endocrinology and Metabolism.2022; 37(2): 281. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Patient Population and Test Utilization for Thyroid Function in Local Clinics and Hospitals in Korea
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Diagnostics.2022; 12(7): 1638. CrossRef - 2021 Asia-Pacific Graves’ Disease Consortium Survey of Clinical Practice Patterns in the Management of Graves’ Disease
Rajeev Parameswaran, Mechteld Christine de Jong, James Lee Wai Kit, Kathleen Sek, Tran Quang Nam, Tran Viet Thang, Nguyen Thy Khue, Than Than Aye, Phone Myint Tun, Timothy Cole, Julie A. Miller, Michael Villa, Benjapa Khiewvan, Sirinart Sirinvaravong, Yon
Endocrine.2022; 79(1): 135. CrossRef - Graves’ disease, its treatments, and the risk of atrial fibrillation: A Korean population-based study
Yoon Young Cho, Bongseong Kim, Dughyun Choi, Chul-Hee Kim, Dong Wook Shin, Jee Soo Kim, Seung-Jung Park, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - Evaluation of the role of thyroid scintigraphy in the differential diagnosis of thyrotoxicosis
Carolina M. Perdomo, Marta García‐Goñi, Lidia Sancho, José J. Paricio, María D. Lozano, Magdalena de la Higuera, María Currás, Javier Arbizu, Juan C. Galofré
Clinical Endocrinology.2021; 94(3): 466. CrossRef - Treatment of patients with Graves’ disease in Sweden compared to international surveys of an ‘index patient’
Gabriel Sjölin, Kristina Byström, Mats Holmberg, Ove Törring, Selwan Khamisi, Jan Calissendorff, Mikael Lantz, Bengt Hallengren, Helena Filipsson Nyström, Tereza Planck, Göran Wallin
Endocrinology, Diabetes & Metabolism.2021;[Epub] CrossRef - Secular Trends in Ablation Therapy for Graves’ Disease: An Analysis of a 15-Year Experience at a Tertiary Hospital in South Korea
Min Joo Kim, Ye An Kim, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Young Joo Park, Do Joon Park, Bo Youn Cho
Journal of Clinical Medicine.2021; 10(8): 1629. CrossRef - Long-Term Antithyroid Drug Treatment of Graves’ Disease in Children and Adolescents: A 20-Year Single-Center Experience
Ari Song, Su Jin Kim, Min-Sun Kim, Jiyeon Kim, Insung Kim, Ga Young Bae, Eunseop Seo, Young Seok Cho, Joon Young Choi, Sung Yoon Cho, Dong-Kyu Jin
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of Polygenetic Risk Scores Related to Immunity and Inflammation with Hyperthyroidism Risk and Interactions between the Polygenetic Scores and Dietary Factors in a Large Cohort
Mi Young Song, Sunmin Park, Anjali Mishra
Journal of Thyroid Research.2021; 2021: 1. CrossRef - Treatment Modality and Risk of Heart Failure in Patients With Long-Standing Graves’ Disease: A Nationwide Population-Based Cohort Study
Eyun Song, Mina Kim, Sojeong Park, Min Jeong Park, Jung A. Kim, Eun Roh, Ji Hee Yu, Nam Hoon Kim, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Frontiers in Endocrinology.2021;[Epub] CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef - Incidence and Mortality of Myocardial Infarction and Stroke in Patients with Hyperthyroidism: A Nationwide Cohort Study in Korea
Hyun Jung Kim, Taeuk Kang, Min Ji Kang, Hyeong Sik Ahn, Seo Young Sohn
Thyroid.2020; 30(7): 955. CrossRef - Diagnosis and Management of Graves’ Disease in Thailand: A Survey of Current Practice
Chutintorn Sriphrapradang
Journal of Thyroid Research.2020; 2020: 1. CrossRef - The success rate of radioactive iodine therapy for Graves’ disease in iodine-replete area and affecting factors: a single-center study
Hyunju Park, Hye In Kim, Jun Park, So Young Park, Tae Hyuk Kim, Jae Hoon Chung, Joon Young Choi, Sun Wook Kim
Nuclear Medicine Communications.2020; 41(3): 212. CrossRef - Tirotoksikoz nedenli erektil disfonksiyon üzerine sildenafil etkisinin histopatolojik olarak değerlendirilmesi
Murat ÖZDEMİR, Canberk TOMRUK, Gürkan YİĞİTTÜRK, Varlık EROL, Emel Öykü ÇETİN, Ilgın YILDIRIM ŞİMŞİR, Çiğdem YENİSEY, Yiğit UYANIKGİL, Adnan ŞİMŞİR, Özer MAKAY
Ege Tıp Dergisi.2020; 59(3): 215. CrossRef - The Management of Thyroid Disease in COVID-19 Pandemic
Won Sang Yoo, Hyun-Kyung Chung
International Journal of Thyroidology.2020; 13(2): 65. CrossRef - Is Hyperthyroidism Diagnosed and Treated Appropriately in the United States?
Ammar Asban, Sophie Dream, Brenessa Lindeman
Advances in Surgery.2019; 53: 117. CrossRef - Long-term remission following antithyroid drug withdrawal in patients with Graves’ hyperthyroidism: parameters with prognostic value
Ricardo V. García-Mayor, Paula Álvarez-Vázquez, Enrique Fluiters, Diana Valverde, Amalia Andrade
Endocrine.2019; 63(2): 316. CrossRef - Safety of long-term antithyroid drug treatment? A systematic review
F. Azizi, R. Malboosbaf
Journal of Endocrinological Investigation.2019; 42(11): 1273. CrossRef - Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinology and Metabolism.2019; 34(3): 268. CrossRef - Prevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
Hyemi Kwon, Jin-hyung Jung, Kyung-Do Han, Yong-Gyu Park, Jung-Hwan Cho, Da Young Lee, Ji Min Han, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 260. CrossRef - An update in the treatment preference for hyperthyroidism
Obin Kwon
Nature Reviews Endocrinology.2018; 14(7): 438. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef - Graves' Disease Patients with Large Goiters Respond Best to Radioactive Iodine Doses of at Least 15 mCi: a Sonographic Volumetric Study
Yun Ah Jeong, Jee Hee Yoon, Hee Kyung Kim, Ho-Cheol Kang
International Journal of Thyroidology.2018; 11(2): 137. CrossRef - Chylothorax Associated with Substernal Goiter in Graves’ Disease Treated with Radioactive Iodine
Seo Young Oh, Bo Hyun Kim, Do Young Kim, Kyu Min Lee, Min Jin Lee, Sung Su Kim, Jong Ho Kim, Yun Kyung Jeon, Sang Soo Kim, Yong Ki Kim, In Joo Kim
International Journal of Endocrinology and Metabolism.2017;[Epub] CrossRef - Vitiligo and overt thyroid diseases: A nationwide population-based study in Korea
Jung Min Bae, June Hyunkyung Lee, Jae Seung Yun, Byeol Han, Tae Young Han
Journal of the American Academy of Dermatology.2017; 76(5): 871. CrossRef - Increased risk of thyroid diseases in patients with systemic lupus erythematosus: A nationwide population-based Study in Korea
Jae-Seung Yun, Jung Min Bae, Ki-Jo Kim, Yu Seok Jung, Gyong Moon Kim, Hyung-Rae Kim, Jun-Seok Lee, Seung-Hyun Ko, Seon-Ah Cha, Yu-Bae Ahn, Ludmila Prokunina-Olsson
PLOS ONE.2017; 12(6): e0179088. CrossRef - The Second Antithyroid Drug Treatment Is Effective in Relapsed Graves' Disease Patients: A Median 11-Year Follow-Up Study
Ye An Kim, Sun Wook Cho, Hoon Sung Choi, Shinje Moon, Jae Hoon Moon, Kyung Won Kim, Do Joon Park, Ka Hee Yi, Young Joo Park, Bo Youn Cho
Thyroid.2017; 27(4): 491. CrossRef - Free Thyroxine, Anti-Thyroid Stimulating Hormone Receptor Antibody Titers, and Absence of Goiter Were Associated with Responsiveness to Methimazole in Patients with New Onset Graves' Disease
Hoon Sung Choi, Won Sang Yoo
Endocrinology and Metabolism.2017; 32(2): 281. CrossRef - Long-Term Antithyroid Drug Treatment: A Systematic Review and Meta-Analysis
Fereidoun Azizi, Ramin Malboosbaf
Thyroid.2017; 27(10): 1223. CrossRef - The Recurrence Rate of Graves' Disease among Patients with Subclinical Thyrotoxicosis after Initial Remission with Antithyroid Agents
Myoung Sook Shim, Soo Min Nam, Jin Sae Yoo, Hae Kyung Kim, Sang Jun Lee, Mi Young Lee
International Journal of Thyroidology.2017; 10(2): 77. CrossRef - Serum 25-hydroxyvitamin D might be an independent prognostic factor for Graves disease recurrence
Hwa Young Ahn, Yun Jae Chung, Bo Youn Cho
Medicine.2017; 96(31): e7700. CrossRef - Recent Advances in Autoimmune Thyroid Diseases
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2016; 31(3): 379. CrossRef - Usefulness of Measuring Thyroid Stimulating Antibody at the Time of Antithyroid Drug Withdrawal for Predicting Relapse of Graves Disease
Hyemi Kwon, Won Gu Kim, Eun Kyung Jang, Mijin Kim, Suyeon Park, Min Ji Jeon, Tae Yong Kim, Jin-Sook Ryu, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2016; 31(2): 300. CrossRef - Hyperthyroidism
Simone De Leo, Sun Y Lee, Lewis E Braverman
The Lancet.2016; 388(10047): 906. CrossRef - Differentiating Graves' disease from subacute thyroiditis using ratio of serum free triiodothyronine to free thyroxine
Chutintorn Sriphrapradang, Adikan Bhasipol
Annals of Medicine and Surgery.2016; 10: 69. CrossRef - Management of hyperthyroid patients in dental emergencies: a case report
Kyung-Jin Lee, Wonse Park, Nan-Sim Pang, Jin-Hyung Cho, Kee-Deog Kim, Bock Young Jung, Eun-Jung Kwak
Journal of Dental Anesthesia and Pain Medicine.2016; 16(2): 147. CrossRef - The Presence of Thyroid-Stimulation Blocking Antibody Prevents High Bone Turnover in Untreated Premenopausal Patients with Graves’ Disease
Sun Wook Cho, Jae Hyun Bae, Gyeong Woon Noh, Ye An Kim, Min Kyong Moon, Kyoung Un Park, Junghan Song, Ka Hee Yi, Do Joon Park, June-Key Chung, Bo Youn Cho, Young Joo Park, Jung-Eun Kim
PLOS ONE.2015; 10(12): e0144599. CrossRef - Refractory Graves' Disease Successfully Cured by Adjunctive Cholestyramine and Subsequent Total Thyroidectomy
Yeoree Yang, Seawon Hwang, Minji Kim, Yejee Lim, Min-Hee Kim, Sohee Lee, Dong-Jun Lim, Moo-Il Kang, Bong-Yun Cha
Endocrinology and Metabolism.2015; 30(4): 620. CrossRef - Improved quality of life in hyperthyroidism patients after surgery
Branka Bukvic, Vladan Zivaljevic, Sandra Sipetic, Aleksandar Diklic, Katarina Tausanovic, Dragos Stojanovic, Dejan Stevanovic, Ivan Paunovic
Journal of Surgical Research.2015; 193(2): 724. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Effect of previous administration of potassium iodine and different durations of low iodine diets for radioiodine therapy on the treatment of Graves' disease in iodine-rich areas


 KES
KES

 First
First Prev
Prev



