Search
- Page Path
- HOME > Search
- Thyroid
- Thyroid Hormone Reference Intervals among Healthy Individuals In Lanzhou, China
- Yan Lu, Wen-Xia Zhang, De-Hong Li, Lian-Hua Wei, Yu-Jun Zhang, Fu-Na Shi, Shen Zhou
- Endocrinol Metab. 2023;38(3):347-356. Published online June 14, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1638
- 2,131 View
- 125 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The common reference intervals (RIs) for thyroid hormones currently used in China are provided by equipment manufacturers. This study aimed to establish thyroid hormone RIs in the population of Lanzhou, a city in the subplateau region of northwest China, and compare them with previous reports and manufacturer-provided values.
Methods
In total, 3,123 individuals (1,680 men, 1,443 women) from Lanzhou, an iodine-adequate area of China, perceived as healthy were selected. The Abbott Architect analyzer was used to determine the serum concentration of thyroid hormones. The 95% RI was estimated using the 2.5th and 97.5th percentiles as the lower and upper reference limits, respectively.
Results
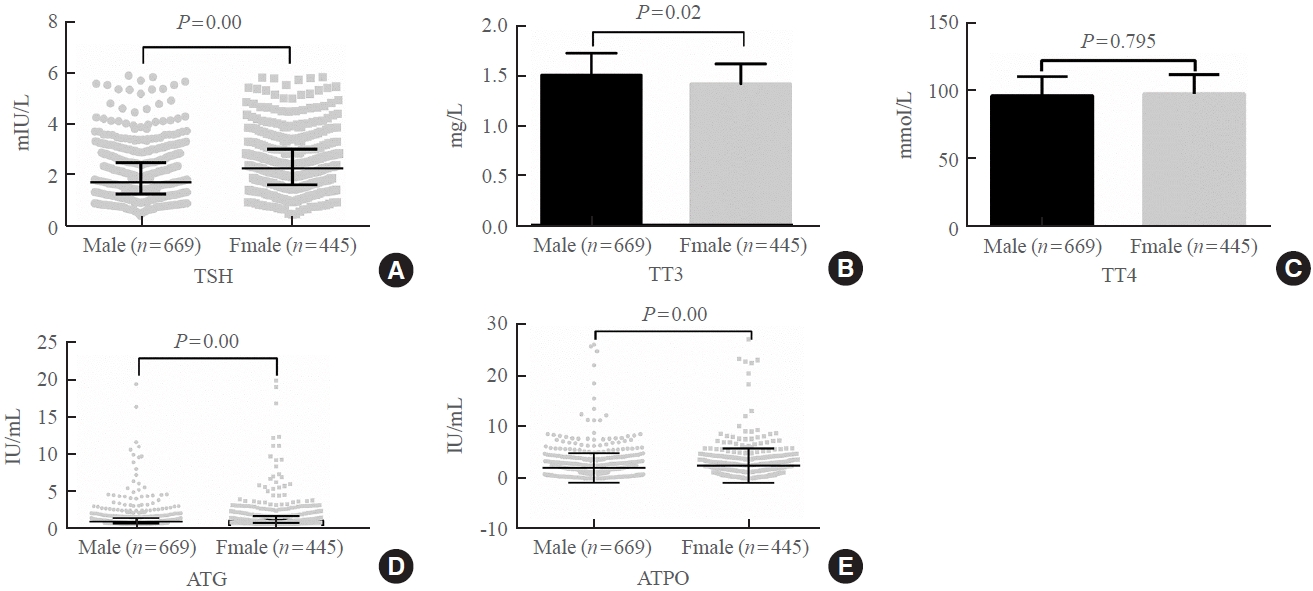
The serum levels of thyroid-stimulating hormone (TSH), total triiodothyronine (TT3), antithyroglobulin (ATG) antibody, and antithyroid peroxidase (ATPO) antibody levels were significantly correlated with sex (P<0.05). TSH, total thyroxine (TT4), and ATPO levels were significantly correlated with age (P<0.05). The serum levels of TSH, ATG, and ATPO in men were significantly lower than in women; in contrast, the serum TT3 level was significantly higher in men than in women (P<0.05). Serum TSH, TT3, TT4, and ATG levels differed across age groups (P<0.05), but no such variation was observed for ATG levels (P>0.05). The established RIs of TSH, ATG, and ATPO in this study differed between sexes (P<0.05). The thyroid hormone RIs established herein were inconsistent with the manufacturer-provided values.
Conclusion
The RIs of thyroid hormones in the healthy population of Lanzhou were inconsistent with those in the manufacturer’s manual. Validated sex-specific values are required for diagnosing thyroid diseases. -
Citations
Citations to this article as recorded by- Burden of non-alcoholic fatty liver disease in subclinical hypothyroidism
Mahmood Dhahir Al-Mendalawi
Journal of Clinical and Scientific Research.2024; 13(1): 68. CrossRef
- Burden of non-alcoholic fatty liver disease in subclinical hypothyroidism

- Hypothalamus and Pituitary gland
- Current National and International Guidelines for the Management of Male Hypogonadism: Helping Clinicians to Navigate Variation in Diagnostic Criteria and Treatment Recommendations
- Ahmed Al-Sharefi, Richard Quinton
- Endocrinol Metab. 2020;35(3):526-540. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.760

- 9,691 View
- 510 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Male hypogonadism—rebadged by some as testosterone deficiency syndrome—is a clinical and biochemical diagnosis of increasing worldwide interest. Organic male hypogonadism—usually permanent—is well-established, but aging men may also exhibit lower serum testosterone levels; principally due to burden of extra-gonadal comorbidities such as obesity, diabetes and metabolic syndrome, but with an underlying intact hypothalamo-pituitary-testicular (HPT) axis capable of springing back into operation once comorbidities are addressed. Despite encouraging observational data and plausible theoretical underpinning, evidence for efficacy and safety of testosterone in this “aging” group of men is lacking; addressing comorbid illnesses remains the key priority instead. Nevertheless, in recent years, accumulation of misleading information online has triggered a global tsunami of testosterone prescriptions. Despite this, many men with organic hypogonadism remain undiagnosed or untreated; many more face a diagnostic odyssey before achieving care by the appropriate specialist. As testosterone therapy is not without risk several clinical practice guidelines have been published specialist societies to guide physicians on best practice. However, these are heterogeneous in key areas, reflecting divergent approaches to the same evidence basis. Herein, we navigate the major clinical practice guidelines on male hypogonadism and test their respective recommendations against current best evidence.
-
Citations
Citations to this article as recorded by- Expert Opinion on the Diagnosis and Management of Male Hypogonadism in India
Sanjay Kalra, Jubbin Jacob, A. G. Unnikrishnan, Ganapathi Bantwal, Abhay Sahoo, Rakesh Sahay, Sushil Jindal, Madhu Sudan Agrawal, Nitin Kapoor, Banshi Saboo, Mangesh Tiwaskar, Kapil Kochhar, Henrik Falhammar
International Journal of Endocrinology.2023; 2023: 1. CrossRef - Management Outcomes in Males With Hypogonadotropic Hypogonadism Treated With Gonadotropins
Bahaa O Sahib, Ibrahim H Hussein, Nassar T Alibrahim, Abbas A Mansour
Cureus.2023;[Epub] CrossRef - The Association between Inflammation, Testosterone and SHBG in men: A cross‐sectional Multi‐Ethnic Study of Atherosclerosis
Amar Osmancevic, Bledar Daka, Erin D. Michos, Penelope Trimpou, Matthew Allison
Clinical Endocrinology.2023; 99(2): 190. CrossRef - The Illusory Case for Treatment of an Invented Disease
David J. Handelsman
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of Chronic Heart Failure Complicated with Type 2 Diabetes Mellitus on Cognitive Function in the Elderly
Yang Liu, Rui Meng, Jianzeng Dong, Xiaonan Xi
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Different Factors Are Associated With Sex Hormones and Leydig Cell Function in Israelis and Palestinians in Jerusalem
Guy Vishnevsky, Ronit Sinnreich, Hisham Nassar, Dafna Merom, Maya Ish-Shalom, Jeremy D. Kark, Hagai Levine
American Journal of Men's Health.2022; 16(4): 155798832211060. CrossRef - Association of rs9939609 polymorphism in the FTO gene with features of androgen status in men
S. V. Yankovskaya, K. I. Mosalev, I. D. Ivanov, B. B. Pinkhasov, V. G. Selyatitskaya
Сибирский научный медицинский журнал.2022; 42(2): 18. CrossRef - Clinical and pharmacological basis of the use of testosterone drugs for hormonal replacement therapy for hypogonadism in men
N. I. Volkova, A. V. Safronenko, E. V. Gantsgorn, Yu. S. Degtyareva
Obesity and metabolism.2022; 19(2): 233. CrossRef - Monitoring and Management of Bardet-Biedl Syndrome: What the Multi-Disciplinary Team Can Do
Lavinia Caba, Laura Florea, Elena Emanuela Braha, Valeriu Vasile Lupu, Eusebiu Vlad Gorduza
Journal of Multidisciplinary Healthcare.2022; Volume 15: 2153. CrossRef - Non-alcoholic fatty liver disease across endocrinopathies: Interaction with sex hormones
Sara Arefhosseini, Mehrangiz Ebrahimi-Mameghani, Farzad Najafipour, Helda Tutunchi
Frontiers in Endocrinology.2022;[Epub] CrossRef - Recommendations on the diagnosis, treatment and monitoring of testosterone deficiency in men
Bruno Lunenfeld, George Mskhalaya, Michael Zitzmann, Giovanni Corona, Stefan Arver, Svetlana Kalinchenko, Yuliya Tishova, Abraham Morgentaler
The Aging Male.2021; 24(1): 119. CrossRef
- Expert Opinion on the Diagnosis and Management of Male Hypogonadism in India

- Bone Metabolism
- Testosterone Replacement and Bone Mineral Density in Male Pituitary Tumor Patients
- Min Jeong Lee, Hyoung Kyu Ryu, So-Yeon An, Ja Young Jeon, Ji In Lee, Yoon-Sok Chung
- Endocrinol Metab. 2014;29(1):48-53. Published online March 14, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.1.48
- 3,590 View
- 33 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypopituitarism is associated with osteoporosis and osteopenia especially when hypogonadotropic hypogonadism is present. Despite hypopituitarism being an important cause of secondary osteoporosis, osteoporosis in patients receiving surgery for pituitary tumors in Korea has not been studied. In this study, we evaluated the effects of testosterone replacement therapy (TRT) on bone mineral density (BMD) in postoperative hypogonadal patients with pituitary tumors.
Methods To examine the effect of TRT on BMD, we performed a retrospective observational study in 21 postoperative male patients who underwent pituitary tumor surgery between 2003 and 2012 at the Ajou University Hospital. Testosterone was replaced in postoperative hypogonadal patients by regular intramuscular injection, daily oral medication, or application of transdermal gel. BMD (g/cm2) measurements of central skeletal sites (lumbar spine, femoral neck, and total femur) were obtained using dual-energy X-ray absorptiometry (GE Lunar). For lumbar spine BMD, L1 to L4 values were chosen for analysis. Femur neck and total femur were also analyzed.
Results During the follow-up period (mean, 56 months; range, 12 to 99 months) serum testosterone levels increased with the administration of TRT (
P =0.007). There was significant improvement (4.56%±9.81%) in the lumbar spine BMD compared to baseline BMD. There were no significant changes in the femur neck BMD or total femur BMD. We did not find any statistically significant relationships between changes in testosterone levels and BMD using Spearman correlation analysis.Conclusion Our results indicated that TRT used in the postoperative period for hypogonadal pituitary tumor surgery patients may have beneficial effects on the BMD of the spine.
-
Citations
Citations to this article as recorded by- Testosterone supplementation and bone parameters: a systematic review and meta-analysis study
G. Corona, W. Vena, A. Pizzocaro, V. A. Giagulli, D. Francomano, G. Rastrelli, G. Mazziotti, A. Aversa, A. M. Isidori, R. Pivonello, L. Vignozzi, E. Mannucci, M. Maggi, A. Ferlin
Journal of Endocrinological Investigation.2022; 45(5): 911. CrossRef - Physiological testosterone replacement effects on male aged rats with orchiectomy-induced osteoporosis in advanced stage: a tomographic and biomechanical pilot study
Vinícius de Paiva Gonçalves, Adriana Alicia Cabrera-Ortega, Jhonatan de Souza Carvalho, Dania Ramadan, Luís Carlos Spolidorio
The Aging Male.2021; 24(1): 139. CrossRef - Androgens and Androgen Receptor Actions on Bone Health and Disease: From Androgen Deficiency to Androgen Therapy
Jia-Feng Chen, Pei-Wen Lin, Yi-Ru Tsai, Yi-Chien Yang, Hong-Yo Kang
Cells.2019; 8(11): 1318. CrossRef - Testosterone and male rejuvenation
Sevann Helo, Peyton Thomas, Nicholas N. Tadros
Panminerva Medica.2019;[Epub] CrossRef - Systemic Non-Reproductive Effects of Sex Steroids in Adult Males and Females
Syed Imran Ali Shah
Human Physiology.2018; 44(1): 83. CrossRef - Benefits and Health Implications of Testosterone Therapy in Men With Testosterone Deficiency
Abdulmaged M. Traish
Sexual Medicine Reviews.2018; 6(1): 86. CrossRef - Multiple Fractures in Patient with Graves' Disease Accompanied by Isolated Hypogonadotropic Hypogonadism
Hyon-Seung Yi, Ji Min Kim, Sang Hyeon Ju, Younghak Lee, Hyun Jin Kim, Koon Soon Kim
Journal of Bone Metabolism.2016; 23(1): 40. CrossRef - Severity and pattern of bone mineral loss in endocrine causes of osteoporosis as compared to age-related bone mineral loss
D Dutta, P Dharmshaktu, A Aggarwal, K Gaurav, R Bansal, N Devru, UC Garga, B Kulshreshtha
Journal of Postgraduate Medicine.2016; 62(3): 162. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Bone health in hypogonadal men
Michael S. Irwig
Current Opinion in Urology.2014; 24(6): 608. CrossRef - Testosterone Replacement Therapy and Bone Mineral Density in Men with Hypogonadism
Se Hwa Kim
Endocrinology and Metabolism.2014; 29(1): 30. CrossRef
- Testosterone supplementation and bone parameters: a systematic review and meta-analysis study

- A Case of Kallmann's Syndrome Mildly Presenting as Secondary Amenorrhea.
- Na Rae Joo, Cheol Young Park, Hong Ju Moon, Jun Goo Kang, Sung Hee Ihm, Moon Gi Choi, Hyung Joon Yoo, Yul Lee, Ki Won Oh, Sung woo Park
- J Korean Endocr Soc. 2007;22(2):130-134. Published online April 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.2.130
- 2,138 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Kallmann's syndrome is very rare congenital defect in GnRH (gonadotrophin releasing hormone) secretion involving both sexes. The mode of inheritance has not been fully understood. But, including X-linked inheritance, the ratio of incidence between male versus female is 5:1, and there is a few case reports of female Kallmann's syndrome in Korea, especially in internal medicine department. We report a case of 35 year-old female Kallmann's syndrome presenting secondary amenorrhea as a mild presentation.

- Regulation of Prolactin Gene Expression by Hypothalamic Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP) in the Female Rat Pituitary Gland.
- Young Il Kim, Tae Young Ha, Eun Sook Kim, Il Seong Nam-Goong, M S O'Dorisio, Min Kyu Hur, Sang Kyu Park
- J Korean Endocr Soc. 2004;19(2):152-164. Published online April 1, 2004
- 982 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Pituitary adenylate cyclase-activating polypeptide (PACAP) plays the role of a hypophysiotropic factor, which regulates the synthesis and secretion of pituitary hormones through the hypothalamo-hypophysial portal system. No clear evidence has yet been reported regarding the regulation of prolactin (PRL) by PACAP. In the present study, we tested a hypothesis that PACAP regulates the synthetic machinery of PRL during the estrus cycle and pubertal process using intracerebroventricular (i.c.v.) injection of an antisense oligodeoxynucleotide (ODN) against type I PACAP receptor (PAC1). METHODS: An RNase protection assay (RPA) was used to determine the pattern of hypothalamic PACAP and PAC1 mRNA expressions during the estrus cycle. Antisense PAC1 ODN was administered via i.c.v. injection to the female rats in normal estrus cycle of pubertal process. Northern blot analysis was used to determine the mRNA ievel of PRL in the pituitary gland. RESULTS: 1) PACAP mRNA in the medial basal hypothalamus was significantly increased at the diestrus I, while PAC1 mRNA showed no significant change. 2) PRL mRNA level of pituitary was increased by an injection of antisense PAC1 ODN at the proestrus and estrus stages. 3) PRL mRNA level of pituitary was significantly decreased by antisense PAC1 ODN injection at stage of prepuberty and initiate puberty, while its level was increased at stage of puberty. CONCLUSION: These data suggest that PACAP suppresses PRL mRNA synthesis through the PAC1 signaling pathway in the certain estrus cycle environments. It may be also involved in the regulation of pituitary PRL gene expression during the pubertal process

- A Case of 46 XX Male Syndrome.
- Jae Myoung Lee, Myung Sook Shim, Young Uck Kim, Young Goo Shin, Choon Hee Chung
- J Korean Endocr Soc. 2001;16(1):148-152. Published online February 1, 2001
- 1,233 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - The 46, XX male syndrome is rare disease that is characterized by a phenotypic male who has a 46, XX female karyotype. Since the first report by de la Chapelle and associates in 1964, several cases have been reported, but it is still a rare entity. Recently we examined a 20-year-old XX male who had the symptoms of gynecomastia, an infantile appearance of the external genitalia, scanty pubic hair, no Adams apple, and no axillary hair. We presently describe a patient with the 46, XX male syndrome who showed a 46, XX karyotype on chromosomal study and review the literatures.

- Clonical Experience on Non-Scrotal Testosterone Transdermal Patch in the Middle Aged Male.
- Young Chan Kim, Jong Ho Park, Suk Ki Lee, Young Jin Lee, Chul Young Bae, Yong Wook Cho, Myung Seo Kang, Jung Hoon Kim
- J Korean Endocr Soc. 1999;14(1):102-121. Published online January 1, 2001
- 1,030 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
To evaluate metabolic effects of testosterone on whole bodily systems, non-scrotal testosterone transdermal patch was given to middle aged men. METHODS: Sixteen impotent patients with serum testosterone levels between 300 and 500 ng/dL, were recruited for 6 month of treatment with non-scrotal testosterone transdermal delivery system, and six patients dropped during the study. All patients have a non-organic impotence (mean age:48 +/- 7). After 1 month placebo patch running period, patients were given 1 or 2 patches. The parameters were evaluated at each stage; before treatment, after placebo patch, and after testosterone patch for 3 months and 6 months. The evaluation parameters included body weight, blood pressure, heart rate, body mass index (BMI), body fat, haemoglobin, haematocrit, RBC, lipid profiles, Prostatic Specific Antigen (PSA), Transrectal Ultrasonography (TRUS), International Prostatic Symptom Score (IPSS), bone markers such as osteocalcin and Deoxypyridinoline (dPyr), Bone Mineral Density (BMD), psychological evaluation with Questionnaire and hormones such as cortisol, Dehydroepiandrosterone sulfate (DHEA-S), Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH), prolactin, testosterone and Sex Hormone Binding Globulin (SHBG). Sexual functions were evaluated by means of sexual Questionnaire which has grade systems (high grade means good response) on each domain. RESULTS: Hormonal, hematopoietic, lipid and prostatic parametem were not changed with statistical insignificance. There were no significant changes in BMD. But mean osteocalcin values increased about 31.5% (p<0.05). Bone resorption marker, D-Pyr values were also decreased significantly about 18.6% after 4 montbs treatment, but such changes were not shown after 6 months. Tendencies of improvement in all domains of Sexual Questionnaire were noticed, even though they were not statistically significant except in frequency of coitus and satisfaction with ejaculation (p<0.05), CONCLUSION: Decreased bone resorption was noticed while persistent increased bone formation occurred after 4 months treatment of testosterone. Testosterone supplementation has a beneficial effects on mood and sexual function in the impotent patients with lower borderline testosterone level. And it can be concluded that 6 months testosterone treatment dose not produce any adverse reactions on bodily system.


 KES
KES

 First
First Prev
Prev



