Search
- Page Path
- HOME > Search
Original Articles
- Thyroid
- Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
- Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
- Endocrinol Metab. 2022;37(3):524-532. Published online June 16, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1418
- 4,851 View
- 230 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
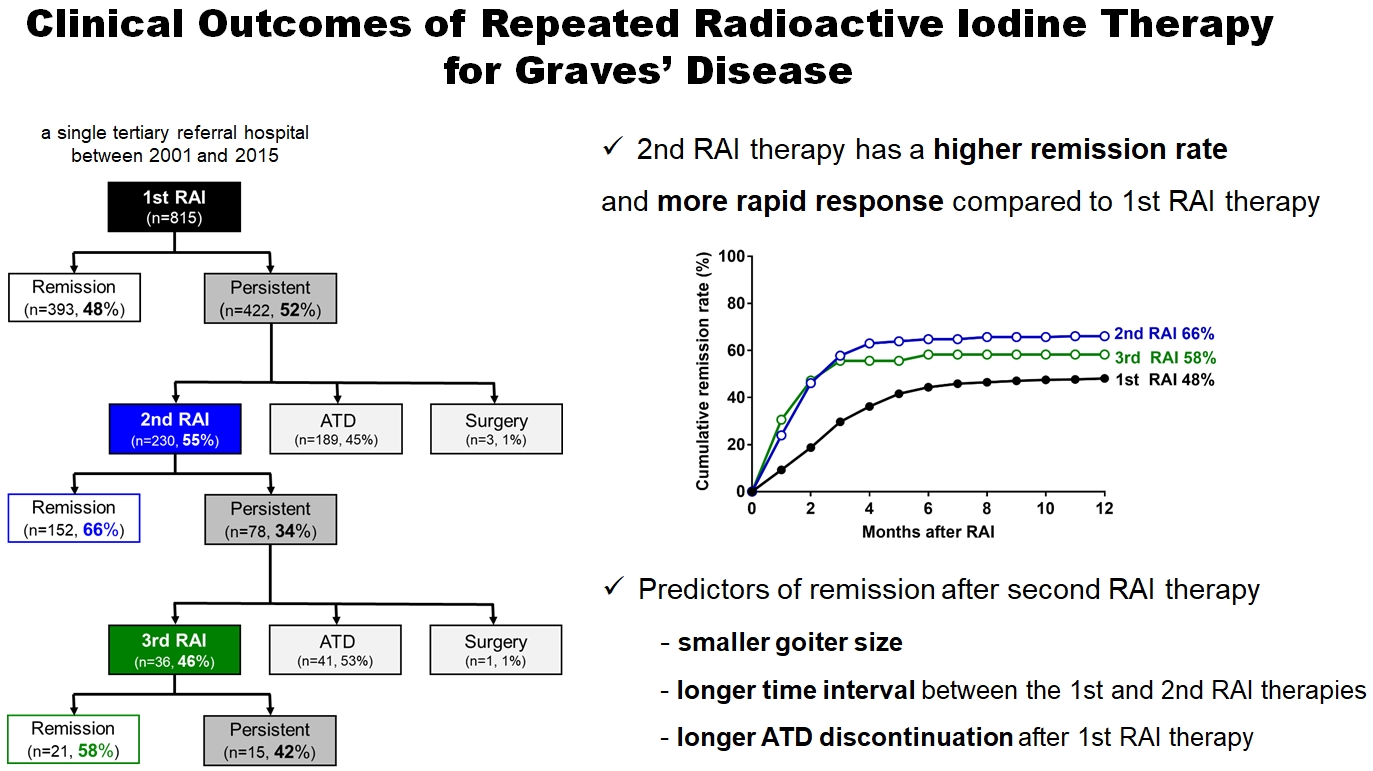
Radioactive iodine (RAI) therapy is a successful therapeutic modality for Graves’ disease. However, RAI therapy can fail, and RAI therapy after antithyroid drugs (ATDs) has a lower remission rate. Therefore, many patients require repeated RAI therapy. This study investigated the clinical outcomes of repeated RAI therapy for Graves’ disease.
Methods
Patients who underwent RAI therapy as second-line therapy after failure of ATD treatment between 2001 and 2015 were reviewed. Remission was defined as hypothyroid or euthyroid status without ATD, and with or without levothyroxine at 12 months after RAI therapy.
Results
The 1-year remission rate after 2nd RAI therapy (66%, 152/230) is significantly higher than that after 1st RAI therapy (48%, 393/815) or long-term ATD treatment after 1st RAI therapy failure (42%). The clinical response to 2nd RAI therapy was more rapid. The median time intervals from the 2nd RAI therapy to ATD discontinuation (1.3 months) and to the start of levothyroxine replacement (2.5 months) were significantly shorter than those for the 1st RAI therapy. A smaller goiter size, a longer time interval between the 1st and 2nd RAI therapies, and a longer ATD discontinuation period predicted remission after the 2nd RAI therapy. Finally, in 78 patients who failed the 2nd RAI therapy, the mean ATD dosage significantly reduced 5.1 mg over 12 months.
Conclusion
Repeated RAI therapy can be a good therapeutic option, especially in patients with smaller goiters and those who are more responsive to the 1st RAI therapy. -
Citations
Citations to this article as recorded by- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Effect of liver dysfunction on outcome of radioactive iodine therapy for Graves’ disease
Yuyang Ze, Fei Shao, Xuefeng Feng, Shanmei Shen, Yan Bi, Dalong Zhu, Xiaowen Zhang
BMC Endocrine Disorders.2022;[Epub] CrossRef
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease

- Clinical Study
- A Phase II Multi-Center, Non-Randomized, Parallel Group, Non-Inferiority Study to Compare the Efficacy of No Radioactive Iodine Remnant Ablation to Remnant Ablation Treatment in Low- to Intermediate-Risk of Papillary Thyroid Cancer: The MOREthyroid Trial Protocol
- Eun Kyung Lee, You Jin Lee, Young Joo Park, Jae Hoon Moon, Ka Hee Yi, Koon Soon Kim, Joo Hee Lee, Sun Wook Cho, Jungnam Joo, Yul Hwangbo, Sujeong Go, Do Joon Park
- Endocrinol Metab. 2020;35(3):571-577. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.681

- 4,640 View
- 119 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Radioactive iodine (RAI) remnant ablation is recommended in patients with papillary thyroid cancer (PTC) and extrathyroidal extension or central lymph node metastasis. However, there exists little evidence about the necessity of remnant ablation in PTC patients with low- to intermediate-risk, those have been increasing in recent decades.
Methods
This multicenter, prospective, non-randomized, parallel group clinical trial will enroll 310 eligible patients with low- to intermediate-risk of thyroid cancer. Inclusion criteria are patients who recently underwent total thyroidectomy for PTC with 3 or less tumors of size 1≤ to ≤2 cm with no microscopic extension and N0/x, or size ≤2 cm with microscopic extension and/or N1a (number of lymph node ≤3, size of tumor foci ≤0.2 cm, and lymph node ratio <0.4). Patients choose to undergo RAI ablation (131I, dose 1.1 GBq) or diagnostic whole-body scan (DxWBS) (131I or 123I, dose 0.074 to 0.222 GBq), followed by subsequent measurement of stimulated thyroglobulin (sTg) within 1 year. Survey for quality of life (QOL) will be performed at baseline and at 1 year after follow-up. The total enrollment period is 5 years, and patients will be followed up for 1 year. The primary endpoint is the non-inferiority of surgery alone to surgery with ablation in terms of biochemical remission (BCR) rate (sTg ≤2 ng/mL) without evidence of structural recurrence. The secondary endpoint was the difference of QOL.
Conclusion
This study will evaluate whether surgery alone achieves similar BCR and improved QOL compared to RAI ablation in patients with low- to intermediate-risk PTC within 1 year.

Case Report
- Mediastinal Uptake Misinterpreted as Metastasis in Papillary Thyroid Cancer.
- Eun Kyung Lee, Kyung Won Kim, So Yeon Park, Young Joo Park, Young Tae Kim, June Key Chung, Hwa Young Cho, Yun Hyi Ku, Hee Suk Min, Seong Hoe Park, Do Joon Park, Bo Youn Cho
- J Korean Endocr Soc. 2007;22(6):460-464. Published online December 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.6.460
- 2,029 View
- 23 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Radioactive iodine (RAI) therapy is used for the removal of remnant thyroid tissue or metastatic thyroid cancer cells in differentiated thyroid cancer. The main mechanism of the therapy is destruction of cells by radioactive iodine that penetrates the cells though the action of the sodium-iodide symporter (NIS). We experienced a case of a 26-year-old woman with mediastinal uptake as detected on a radioiodine scan, who was previously diagnosed with papillary thyroid cancer. For diagnostic tests including chest computed tomography (CT) and a radioiodine scan, the stimulated thyroglobulin level did not show a definite cause of the mediastinal uptake. During regular follow-up, the thymus became triangular with clear margins. The patient had neither specific symptoms nor physical findings related to the presence of a thymic mass. A subsequent CT scan showed an irregular margin of the thymus, suggestive of thymic metastasis. The patient underwent a mediastinectomy. The removed specimen was composed of normal thymic tissue. Moreover, we demonstrated the presence of human NIS by immunohistochemical analysis. After thymectomy, the mediastinal uptake was markedly decreased as compared to the previous scan. This case suggests that a clinician should be suspicious for the functional uptake of thymus when metastasis is unlikely in a clinical situation.
-
Citations
Citations to this article as recorded by- Clinical Significance of Diffuse Intrathoracic Uptake on Post-Therapy I-131 Scans in Thyroid Cancer Patients
Hyun Su Choi, Sung Hoon Kim, Sonya Youngju Park, Hye Lim Park, Ye Young Seo, Woo Hee Choi
Nuclear Medicine and Molecular Imaging.2014; 48(1): 63. CrossRef
- Clinical Significance of Diffuse Intrathoracic Uptake on Post-Therapy I-131 Scans in Thyroid Cancer Patients


 KES
KES

 First
First Prev
Prev



