Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- Initial Combination Therapy in Type 2 Diabetes
- Ji Yoon Kim, Nam Hoon Kim
- Endocrinol Metab. 2024;39(1):23-32. Published online November 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1816
- 2,070 View
- 250 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
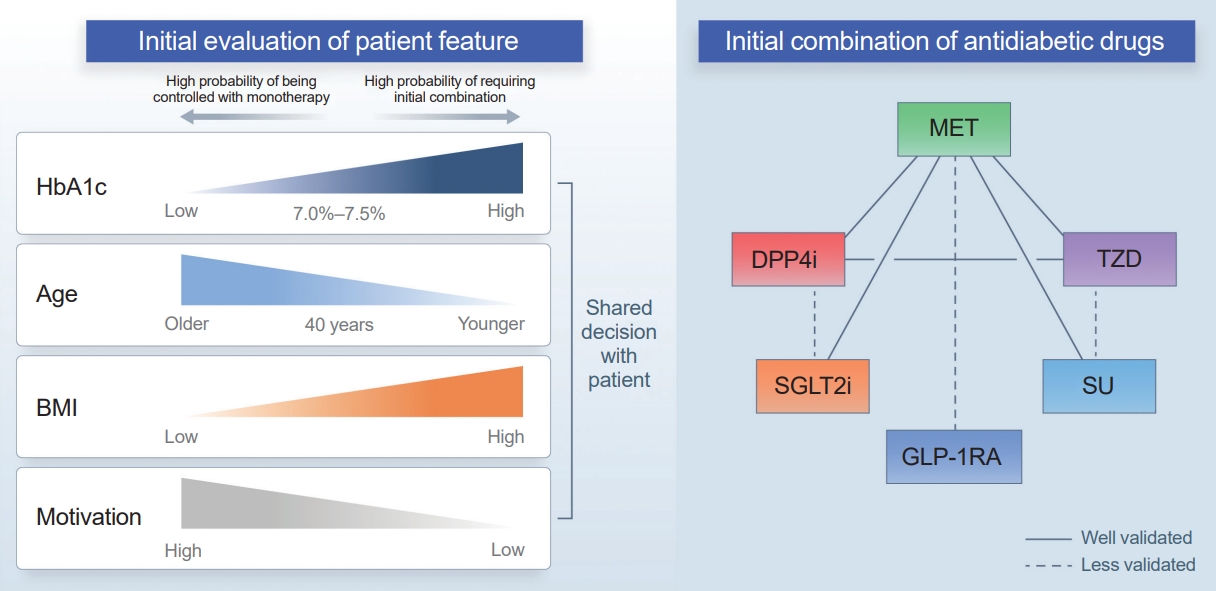
ePub - Type 2 diabetes (T2D) is a progressive disease in which it is challenging to achieve long-term durable glycemic control. However, intensive glycemic control is crucial for preventing diabetes-related complications. Previous studies showed that monotherapy with a stepwise add-on approach was seldom effective for long-term durable glycemic control. Combination therapy, which refers to the use of two or more drugs to control hyperglycemia, has multiple benefits, including the ability to target a variety of pathophysiological processes underlying hyperglycemia. In clinical trials, initial combination therapy showed better glycemic control than monotherapy or a stepwise approach. Emerging evidence indicates that initial combination therapy is associated with preserved β-cell function and fewer complications in T2D. However, cost-effectiveness and adverse events with combination therapy are issues that should be considered. Therefore, initial combination therapy is an important option for patients with T2D that clinicians should consider with a view toward balancing benefits and potential harms. In this review, we summarize the literature addressing initial combination therapy in T2D, and we suggest optimal strategies based on clinical situations and patient characteristics.

- Clinical Study
Big Data Articles (National Health Insurance Service Database) - Effect of Teneligliptin versus Sulfonylurea on Major Adverse Cardiovascular Outcomes in People with Type 2 Diabetes Mellitus: A Real-World Study in Korea
- Da Hea Seo, Kyoung Hwa Ha, So Hun Kim, Dae Jung Kim
- Endocrinol Metab. 2021;36(1):70-80. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.777

- 4,978 View
- 192 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Results regarding the cardiovascular (CV) effects of dipeptidyl peptidase-4 (DPP-4) inhibitors are inconsistent. This study aimed to assess the effects of teneligliptin, a DPP-4 inhibitor, on the risk of major CV outcomes in type 2 diabetes mellitus (T2DM) patients compared to sulfonylurea.
Methods
From January 1, 2015 to December 31, 2017, we conducted a retrospective cohort study using the Korean National Health Insurance Service database. A total of 6,682 T2DM patients who were newly prescribed DPP-4 inhibitors or sulfonylurea were selected and matched in a 1:1 ratio by propensity score. The hazard ratios (HRs) for all-cause mortality, hospitalization for heart failure (HHF), all-cause mortality or HHF, myocardial infarction (MI), stroke, and hypoglycemia were assessed.
Results
During 641 days of follow-up, the use of teneligliptin was not associated with an increased risk of all-cause mortality (HR, 1.00; 95% confidence interval [CI], 0.85 to 1.19), HHF (HR, 0.99; 95% CI, 0.86 to 1.14), all-cause mortality or HHF (HR, 1.02; 95% CI, 0.90 to 1.14), MI (HR, 0.90; 95% CI, 0.68 to 1.20), and stroke (HR, 1.00; 95% CI, 0.86 to 1.17) compared to the use of sulfonylurea. However, it was associated with a significantly lower risk of hypoglycemia (HR, 0.68; 95% CI, 0.49 to 0.94) compared to sulfonylurea therapy.
Conclusion
Among T2DM patients, teneligliptin therapy was not associated with an increased risk of CV events including HHF, but was associated with a lower risk of hypoglycemia compared to sulfonylurea therapy. -
Citations
Citations to this article as recorded by- Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study
Da Hea Seo, Mina Kim, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes Research and Clinical Practice.2024; 208: 111098. CrossRef - Systematic review and meta-analysis of teneligliptin for treatment of type 2 diabetes
R. Pelluri, S. Kongara, V. R. Nagasubramanian, S. Mahadevan, J. Chimakurthy
Journal of Endocrinological Investigation.2023; 46(5): 855. CrossRef - Finding the most cost-effective option from commonly used Dipeptidyl peptidase-4 inhibitors in India: a systematic study
Harmanjit Singh, Ekta Arora, Seerat Narula, Mandeep Singla, Armaan Otaal, Jatin Sharma
Expert Review of Endocrinology & Metabolism.2023; 18(4): 347. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef
- Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study

- Diabetes
- The Role of Glucagon-Like Peptide 1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors in Reducing Cardiovascular Events in Patients with Type 2 Diabetes
- Gwang Sil Kim, Joong Hyun Park, Jong Chul Won
- Endocrinol Metab. 2019;34(2):106-116. Published online May 9, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.2.106
- 5,214 View
- 101 Download
- 15 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub The prevalence of type 2 diabetes mellitus (T2DM), which is associated with cardiovascular morbidity and mortality, is increasing worldwide. Although there have been advances in diabetes treatments that reduce microvascular complications (nephropathy, neuropathy, retinopathy), many clinical studies have found that conventional oral hypoglycemic agents and glucose control alone failed to reduce cardiovascular disease. Thus, incretin-based therapies including glucagon-like peptide 1 (GLP-1) receptor agonists (RAs) and sodium-glucose cotransporter 2 inhibitors (SGLT-2Is) represent a new area of research, and may serve as novel therapeutics for treating hyperglycemia and modifying other cardiovascular risk factors. Recently, it has been confirmed that several drugs in these classes, including canagliflozin, empagliflozin, semaglutide, and liraglutide, are safe and possess cardioprotective effects. We review the most recent cardiovascular outcome trials on GLP-1RAs and SGLT-2Is, and discuss their implications for treating patients with T2DM in terms of protective effects against cardiovascular disease.
-
Citations
Citations to this article as recorded by- Switch to gliflozins and biventricular function improvement in patients with chronic heart failure and diabetes mellitus
Michele Correale, Pietro Mazzeo, Martino Fortunato, Matteo Paradiso, Andrea Furore, Angela I. Fanizzi, Lucia Tricarico, Giuseppe Pastore, Simona Alfieri, Natale D. Brunetti, Olga Lamacchia
Clinical Physiology and Functional Imaging.2024; 44(1): 112. CrossRef - Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - Posing the rationale for synthetic lipoxin mimetics as an adjuvant treatment to gold standard atherosclerosis therapies
Braden Millar, Monica de Gaetano
Frontiers in Pharmacology.2023;[Epub] CrossRef - Improvement of Left Ventricular Global Longitudinal Strain after 6-Month Therapy with GLP-1RAs Semaglutide and Dulaglutide in Type 2 Diabetes Mellitus: A Pilot Study
Paolo Basile, Andrea Igoren Guaricci, Giuseppina Piazzolla, Sara Volpe, Alfredo Vozza, Marina Benedetto, Maria Cristina Carella, Daniela Santoro, Francesco Monitillo, Andrea Baggiano, Saima Mushtaq, Laura Fusini, Fabio Fazzari, Cinzia Forleo, Nunziata Rib
Journal of Clinical Medicine.2023; 12(4): 1586. CrossRef - Rationale and design of the Biventricular Evaluation of Gliflozins effects In chroNic Heart Failure: BEGIN‐HF study
Michele Correale, Elena‐Laura Antohi, Riccardo M. Inciardi, Pietro Mazzeo, Stefano Coiro, Shiro Ishihara, Renata Petroni, Francesco Monitillo, Marta Leone, Marco Triggiani, Chaudhry M.S. Sarwar, Hans‐Dirk Dungen, Khawaja M. Talha, Natale D. Brunetti, Jave
ESC Heart Failure.2023; 10(3): 2066. CrossRef - Effects of Incretin-Based Treatment on the Diastolic (Dys)Function in Patients with Uncontrolled Type 2 Diabetes Mellitus: A Prospective Study with 1-Year Follow-Up
Elena-Daniela Grigorescu, Cristina-Mihaela Lăcătușu, Mariana Floria, Georgiana-Diana Cazac, Alina Onofriescu, Livia-Amira Sauciuc, Alexandr Ceasovschih, Ioana Crețu, Bogdan-Mircea Mihai, Laurențiu Șorodoc
Diagnostics.2023; 13(17): 2817. CrossRef - Role of moesin in the effect of glucagon-like peptide-1 on advanced glycation end products-induced endothelial barrier dysfunction
Yan Liu, Zhenzhen Chen, Lei Liu, Haitao Tang, Huaqing Zhu, Songtao Tang
Cellular Signalling.2022; 90: 110193. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Effectiveness of liraglutide 3 mg for the treatment of obesity in a real-world setting without intensive lifestyle intervention
Jung Ha Park, Ju Young Kim, Jong Han Choi, Hye Soon Park, Hyun-Young Shin, Jae Min Lee, Jin-Wook Kim, Hae-Jin Ko, Suk Chon, Bu Kyung Kim, Chul Sik Kim, Soo Lim
International Journal of Obesity.2021; 45(4): 776. CrossRef - Sodium-glucose co-transporter 2 inhibitor therapy: mechanisms of action in heart failure
Shruti S Joshi, Trisha Singh, David E Newby, Jagdeep Singh
Heart.2021; 107(13): 1032. CrossRef - Effects of antidiabetic drugs on left ventricular function/dysfunction: a systematic review and network meta-analysis
Da-Peng Zhang, Li Xu, Le-Feng Wang, Hong-Jiang Wang, Feng Jiang
Cardiovascular Diabetology.2020;[Epub] CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Benefit-Risk Assessment of Alogliptin for the Treatment of Type 2 Diabetes Mellitus
Kohei Kaku, Koichi Kisanuki, Mari Shibata, Takashi Oohira
Drug Safety.2019; 42(11): 1311. CrossRef
- Switch to gliflozins and biventricular function improvement in patients with chronic heart failure and diabetes mellitus

- Obesity and Metabolism
- Diabetes Drugs and Cardiovascular Safety
- Ji Cheol Bae
- Endocrinol Metab. 2016;31(2):239-244. Published online June 10, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.239
- 3,616 View
- 38 Download
- 15 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetes is a well-known risk factor of cardiovascular morbidity and mortality, and the beneficial effect of improved glycemic control on cardiovascular complications has been well established. However, the rosiglitazone experience aroused awareness of potential cardiovascular risk associated with diabetes drugs and prompted the U.S. Food and Drug Administration to issue new guidelines about cardiovascular risk. Through postmarketing cardiovascular safety trials, some drugs demonstrated cardiovascular benefits, while some antidiabetic drugs raised concern about a possible increased cardiovascular risk associated with drug use. With the development of new classes of drugs, treatment options became wider and the complexity of glycemic management in type 2 diabetes has increased. When choosing the appropriate treatment strategy for patients with type 2 diabetes at high cardiovascular risk, not only the glucose-lowering effects, but also overall benefits and risks for cardiovascular disease should be taken into consideration.
-
Citations
Citations to this article as recorded by- Dipeptidyl peptidase-4 inhibitor compared with sulfonylurea in combination with metformin: cardiovascular and renal outcomes in a propensity-matched cohort study
Kyoung Jin Kim, Jimi Choi, Juneyoung Lee, Jae Hyun Bae, Jee Hyun An, Hee Young Kim, Hye Jin Yoo, Ji A. Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Cardiovascular Diabetology.2019;[Epub] CrossRef - Sodium‐glucose cotransporter 2 inhibitors regulate ketone body metabolism via inter‐organ crosstalk
Jin Hee Kim, Minyoung Lee, Soo Hyun Kim, So Ra Kim, Byung‐Wan Lee, Eun Seok Kang, Bong‐Soo Cha, Jin Won Cho, Yong‐ho Lee
Diabetes, Obesity and Metabolism.2019; 21(4): 801. CrossRef - Glitazones and alpha-glucosidase inhibitors as the second-line oral anti-diabetic agents added to metformin reduce cardiovascular risk in Type 2 diabetes patients: a nationwide cohort observational study
Cheng-Wei Chan, Chu-Leng Yu, Jiunn-Cherng Lin, Yu-Cheng Hsieh, Che-Chen Lin, Chen-Ying Hung, Cheng-Hung Li, Ying-Chieh Liao, Chu-Pin Lo, Jin-Long Huang, Ching-Heng Lin, Tsu-Juey Wu
Cardiovascular Diabetology.2018;[Epub] CrossRef - Normoglucemiantes orales y riesgo cardiovascular
Guillermo Guzmán, Juan Esteban Gómez, Leidy Johanna Plaza, María Claudia Sánchez
Revista Colombiana de Cardiología.2018; 25(5): 333. CrossRef - Dipeptidyl peptidase-4 inhibitor use and risk of diabetic retinopathy: A population-based study
N.H. Kim, J. Choi, N.H. Kim, K.M. Choi, S.H. Baik, J. Lee, S.G. Kim
Diabetes & Metabolism.2018; 44(4): 361. CrossRef - Obesity and Type 2 Diabetes in Our Youth: A Recipe for Cardiovascular Disease
Angela Kaye Wooton, Lynne M. Melchior
The Journal for Nurse Practitioners.2017; 13(3): 222. CrossRef - Sex-gender-related therapeutic approaches for cardiovascular complications associated with diabetes
Ilaria Campesi, Flavia Franconi, Giuseppe Seghieri, Marco Meloni
Pharmacological Research.2017; 119: 195. CrossRef - The Landscape of Glucose-Lowering Therapy and Cardiovascular Outcomes: From Barren Land to Metropolis
Mona P. Nasrallah, Charbel Abi Khalil, Marwan M. Refaat
BioMed Research International.2017; 2017: 1. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Dipeptidyl peptidase-4 inhibitor compared with sulfonylurea in combination with metformin: cardiovascular and renal outcomes in a propensity-matched cohort study

- Obesity and Metabolism
- Factors Associated with Glycemic Variability in Patients with Type 2 Diabetes: Focus on Oral Hypoglycemic Agents and Cardiovascular Risk Factors
- Soyeon Yoo, Sang-Ouk Chin, Sang-Ah Lee, Gwanpyo Koh
- Endocrinol Metab. 2015;30(3):352-360. Published online August 4, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.3.352
- 3,882 View
- 46 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background The role of glycemic variability (GV) in development of cardiovascular diseases remains controversial, and factors that determine glucose fluctuation in patients with diabetes are unknown. We investigated relationships between GV indices, kinds of oral hypoglycemic agents (OHAs), and cardiovascular risk factors in patients with type 2 diabetes mellitus (T2DM).
Methods We analyzed 209 patients with T2DM. The GV index (standard deviation [SD] and mean absolute glucose change [MAG]) were calculated from 7-point self-monitoring of blood glucose profiles. The patients were classified into four groups according to whether they take OHAs known as GV-lowering (A) and GV-increasing (B): 1 (A only), 2 (neither), 3 (both A and B), and 4 (B only). The 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was calculated using the Pooled Cohort Equations.
Results GV indices were significantly higher in patients taking sulfonylureas (SUs), but lower in those taking dipeptidyl peptidase-4 inhibitors. In hierarchical regression analysis, the use of SUs remained independent correlates of the SD (β=0.209,
P =0.009) and MAG (β=0.214,P =0.011). In four OHA groups, GV indices increased progressively from group 1 to group 4. However, these did not differ according to quartiles of 10-year ASCVD risk.Conclusion GV indices correlated significantly with the use of OHAs, particularly SU, and differed significantly according to combination of OHAs. However, cardiovascular risk factors and 10-year ASCVD risk were not related to GV indices. These findings suggest that GV is largely determined by properties of OHAs and not to cardiovascular complications in patients with T2DM.
-
Citations
Citations to this article as recorded by- Prognostic value of longitudinal HbA1c variability in predicting the development of diabetic sensorimotor polyneuropathy among patients with type 2 diabetes mellitus: A prospective cohort observational study
Yun‐Ru Lai, Wen‐Chan Chiu, Chih‐Cheng Huang, Ben‐Chung Cheng, I‐Hsun Yu, Chia‐Te Kung, Ting Yin Lin, Hui Ching Chiang, Chun‐En Aurea Kuo, Cheng‐Hsien Lu
Journal of Diabetes Investigation.2024; 15(3): 326. CrossRef - Influence of dipeptidyl peptidase-4 inhibitors on glycemic variability in patients with type 2 diabetes: A meta-analysis of randomized controlled trials
Shangyu Chai, Ruya Zhang, Ye Zhang, Richard David Carr, Yiman Zheng, Swapnil Rajpathak, Miao Yu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Glycemic Variability in Subjects with Diabetes and Hypogonadism during Testosterone Replacement Treatment: A Pilot Study
Giuseppe Defeudis, Ernesto Maddaloni, Giovanni Rossini, Alfonso Maria Di Tommaso, Rossella Mazzilli, Paolo Di Palma, Paolo Pozzilli, Nicola Napoli
Journal of Clinical Medicine.2022; 11(18): 5333. CrossRef - New Insights into the Role of Visit-to-Visit Glycemic Variability and Blood Pressure Variability in Cardiovascular Disease Risk
Jin J. Zhou, Daniel S. Nuyujukian, Peter D. Reaven
Current Cardiology Reports.2021;[Epub] CrossRef - Prevalence of glycemic variability and factors associated with the glycemic arrays among end-stage kidney disease patients on chronic hemodialysis
Abdul Hanif Khan Yusof Khan, Nor Fadhlina Zakaria, Muhammad Adil Zainal Abidin, Nor Azmi Kamaruddin
Medicine.2021; 100(30): e26729. CrossRef - Dipeptidyl-Peptidase-IV Inhibitors, Imigliptin and Alogliptin, Improve Beta-Cell Function in Type 2 Diabetes
Xu Liu, Yang Liu, Hongzhong Liu, Haiyan Li, Jianhong Yang, Pei Hu, Xinhua Xiao, Dongyang Liu
Frontiers in Endocrinology.2021;[Epub] CrossRef - HbA 1C variability and hypoglycemia hospitalization in adults with type 1 and type 2 diabetes: A nested case-control study
Victor W. Zhong, Juhaeri Juhaeri, Stephen R. Cole, Christina M. Shay, Penny Gordon-Larsen, Evangelos Kontopantelis, Elizabeth J. Mayer-Davis
Journal of Diabetes and its Complications.2018; 32(2): 203. CrossRef - Glucose fluctuation and the resultant endothelial injury are correlated with pancreatic β cell dysfunction in patients with coronary artery disease
Makoto Murata, Hitoshi Adachi, Shigeru Oshima, Masahiko Kurabayashi
Diabetes Research and Clinical Practice.2017; 131: 107. CrossRef - Efficacy of lifestyle interventions in patients with type 2 diabetes: A systematic review and meta-analysis
Xiao-Li Huang, Jian-Hua Pan, Dan Chen, Jing Chen, Fang Chen, Tao-Tao Hu
European Journal of Internal Medicine.2016; 27: 37. CrossRef
- Prognostic value of longitudinal HbA1c variability in predicting the development of diabetic sensorimotor polyneuropathy among patients with type 2 diabetes mellitus: A prospective cohort observational study


 KES
KES

 First
First Prev
Prev



