Search
- Page Path
- HOME > Search
- Hypothalamus and pituitary gland
- Clinical Characteristics, Diagnosis, and Treatment of Thyroid Stimulating Hormone-Secreting Pituitary Neuroendocrine Tumor (TSH PitNET): A Single-Center Experience
- Jung Heo, Yeon-Lim Suh, Se Hoon Kim, Doo-Sik Kong, Do-Hyun Nam, Won-Jae Lee, Sung Tae Kim, Sang Duk Hong, Sujin Ryu, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim, Kyu Yeon Hur
- Endocrinol Metab. 2024;39(2):387-396. Published online February 5, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1877
- 846 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
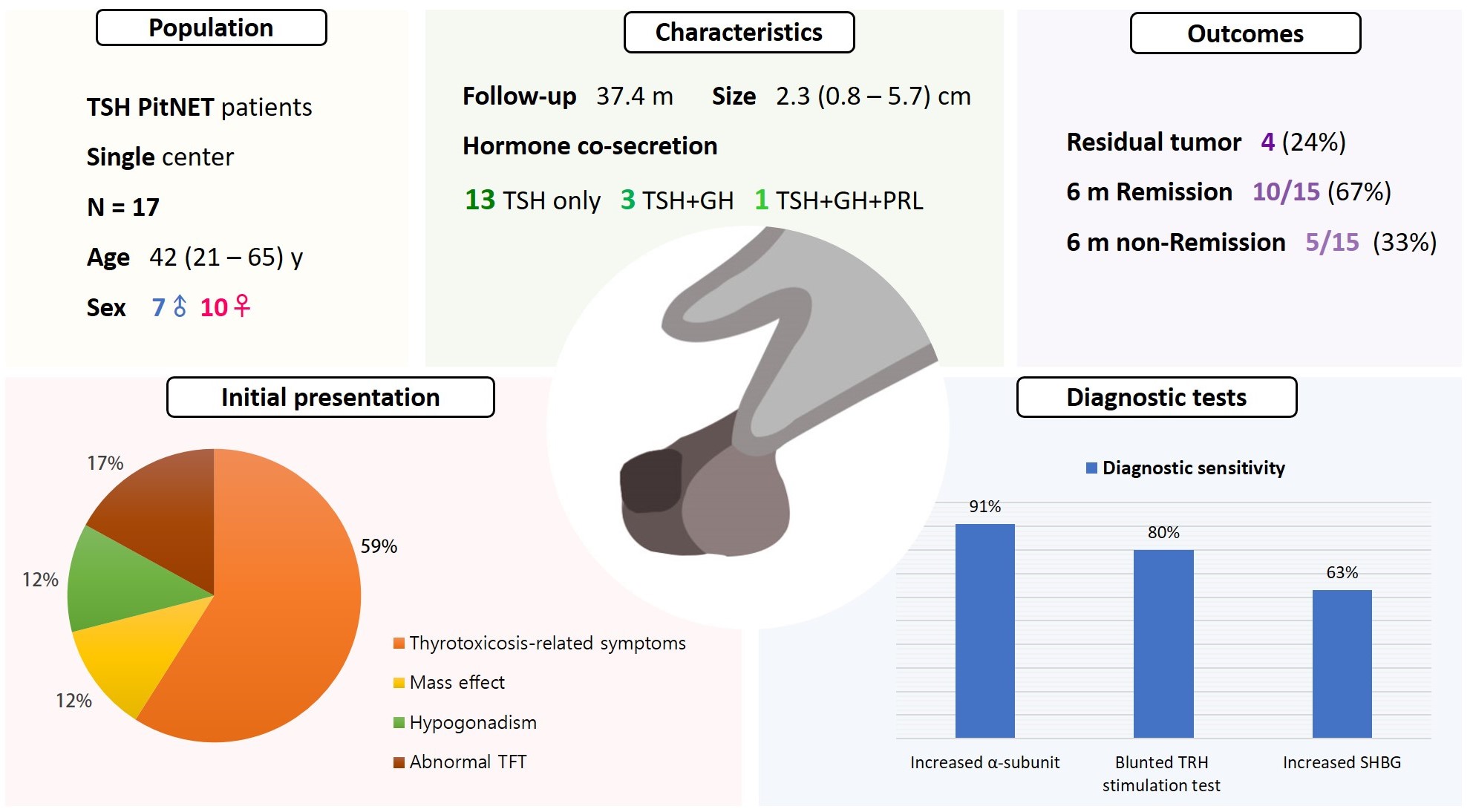
Thyroid-stimulating hormone (TSH)-secreting pituitary neuroendocrine tumor (TSH PitNET) is a rare subtype of PitNET. We investigated the comprehensive characteristics and outcomes of TSH PitNET cases from a single medical center. Also, we compared diagnostic methods to determine which showed superior sensitivity.
Methods
A total of 17 patients diagnosed with TSH PitNET after surgery between 2002 and 2022 in Samsung Medical Center was retrospectively reviewed. Data on comprehensive characteristics and treatment outcomes were collected. The sensitivities of diagnostic methods were compared.
Results
Seven were male (41%), and the median age at diagnosis was 42 years (range, 21 to 65); the median follow-up duration was 37.4 months. The most common (59%) initial presentation was hyperthyroidism-related symptoms. Hormonal co-secretion was present in four (23%) patients. Elevated serum alpha-subunit (α-SU) showed the greatest diagnostic sensitivity (91%), followed by blunted response at thyrotropin-releasing hormone (TRH) stimulation (80%) and elevated sex hormone binding globulin (63%). Fourteen (82%) patients had macroadenoma, and a specimen of one patient with heavy calcification was negative for TSH. Among 15 patients who were followed up for more than 6 months, 10 (67%) achieved hormonal and structural remission within 6 months postoperatively. A case of growth hormone (GH)/TSH/prolactin (PRL) co-secreting mixed gangliocytoma-pituitary adenoma (MGPA) was discovered.
Conclusion
The majority of the TSH PitNET cases was macroadenoma, and 23% showed hormone co-secretion. A rare case of GH/TSH/PRL co-secreting MGPA was discovered. Serum α-SU and TRH stimulation tests showed great diagnostic sensitivity. Careful consideration is needed in diagnosing TSH PitNET. Achieving remission requires complete tumor resection. In case of nonremission, radiotherapy or medical therapy can improve the long-term remission rate.

- Thyroid
Big Data Articles (National Health Insurance Service Database) - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
- Endocrinol Metab. 2023;38(4):436-444. Published online July 12, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1684
- 1,809 View
- 127 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
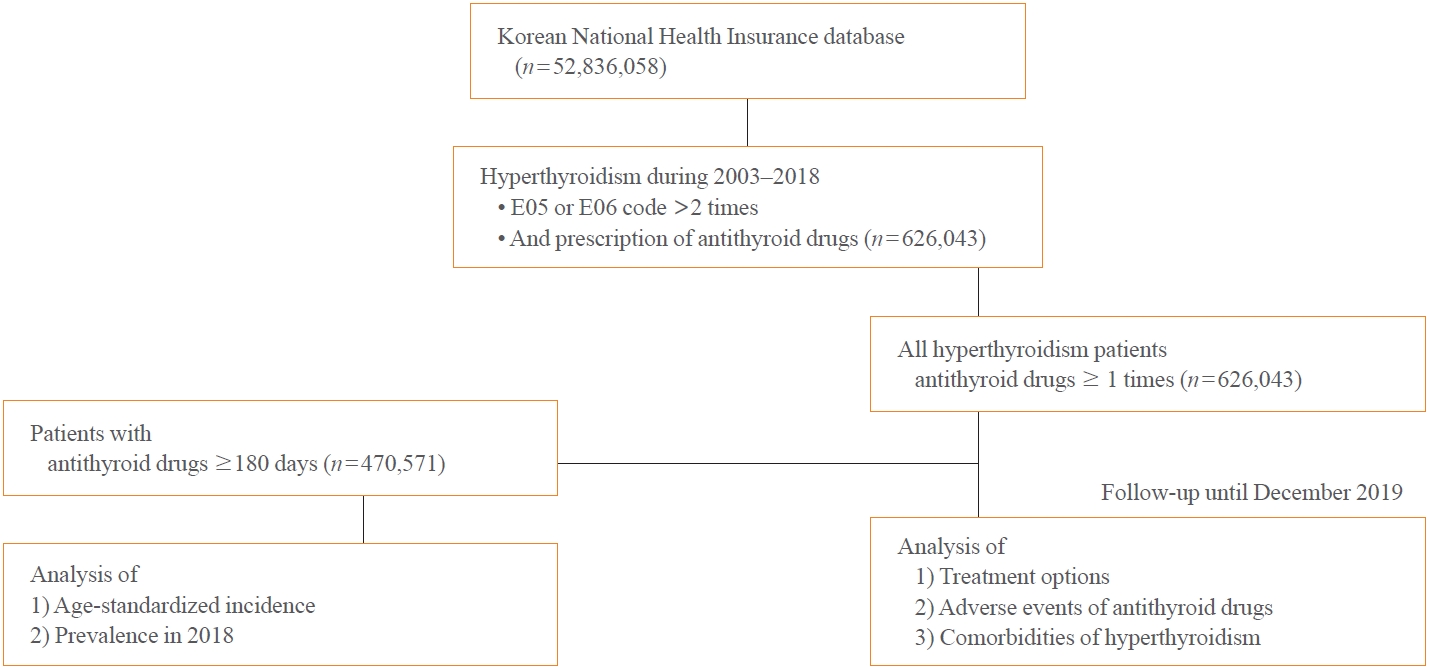
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age. -
Citations
Citations to this article as recorded by- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef
- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients

- Thyroid
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
- Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
- Endocrinol Metab. 2023;38(3):338-346. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1664
- 1,741 View
- 102 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
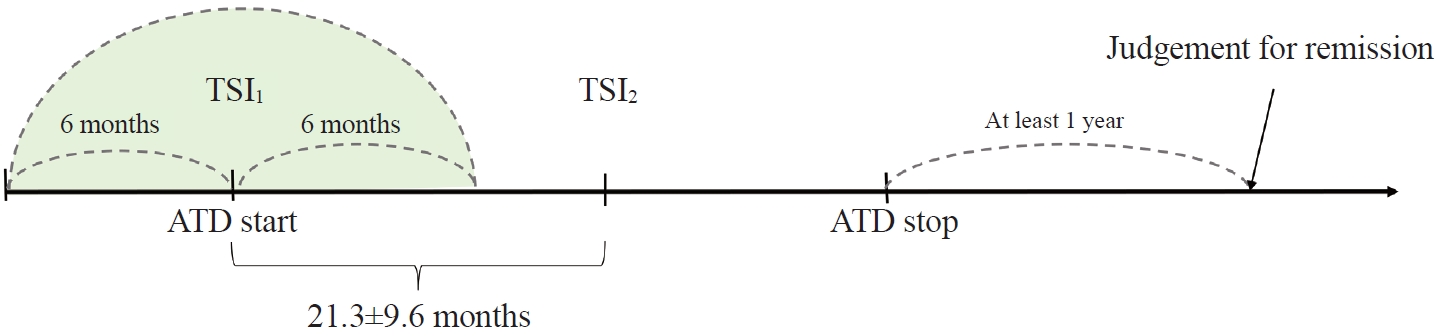
To determine whether baseline thyroid-stimulating immunoglobulin (TSI) bioassay or its early response upon treatment with an anti-thyroid drug (ATD) can predict prognosis of Graves’ disease (GD) in real-world practice.
Methods
This retrospective study enrolled GD patients who had previous ATD treatment with TSI bioassay checked at baseline and at follow-up from April 2010 to November 2019 in one referral hospital. The study population were divided into two groups: patients who experienced relapse or continued ATD (relapse/persistence), and patients who experienced no relapse after ATD discontinuation (remission). The slope and area under the curve at 1st year (AUC1yr) of thyroid-stimulating hormone receptor antibodies including TSI bioassay and thyrotropin-binding inhibitory immunoglobulin (TBII) were calculated as differences between baseline and second values divided by time duration (year).
Results
Among enrolled 156 study subjects, 74 (47.4%) had relapse/persistence. Baseline TSI bioassay values did not show significant differences between the two groups. However, the relapse/persistence group showed less decremental TSI bioassay in response to ATD than the remission group (–84.7 [TSI slope, –198.2 to 8.2] vs. –120.1 [TSI slope, –204.4 to –45.9], P=0.026), whereas the TBII slope was not significantly different between the two groups. The relapse/persistence group showed higher AUC1yr of TSI bioassay and TBII in the 1st year during ATD treatment than the remission group (AUC1yr for TSI bioassay, P=0.0125; AUC1yr for TBII,P =0.001).
Conclusion
Early changes in TSI bioassay can better predict prognosis of GD than TBII. Measurement of TSI bioassay at beginning and follow-up could help predict GD prognosis. -
Citations
Citations to this article as recorded by- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef
- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study

- Thyroid
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
- A Ram Hong, Ho-Cheol Kang
- Endocrinol Metab. 2023;38(2):175-189. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1701
- 3,925 View
- 248 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
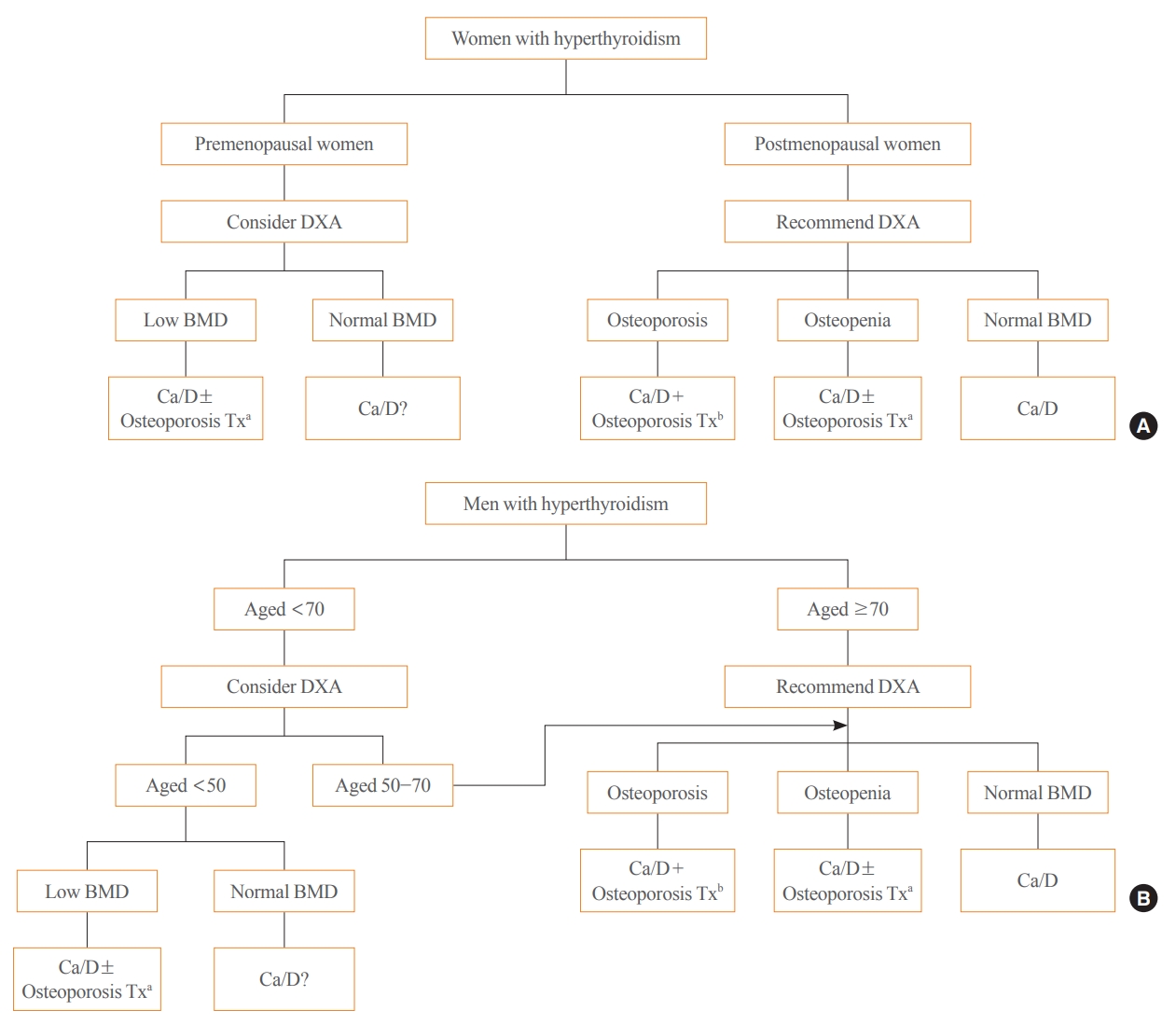
ePub - Thyroid hormones play an important physiological role in maintaining adult bone structure and strength. Consequently, thyroid dysfunction is related to skeletal outcomes. Overt hyperthyroidism is an established cause of high bone turnover with accelerated bone loss, leading to osteoporosis and increased fracture risk. Hyperthyroidism induced by thyroid-stimulating hormone-suppressive therapy in patients with differentiated thyroid cancer is a cause of secondary osteoporosis. In contrast, there is a lack of evidence on the negative impact of hypothyroidism on bone health. Considering the clinical updates on the importance of bone health in thyroid dysfunction, the Task Force from the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association recently developed a position statement on the evaluation and management of bone health of patients with thyroid diseases, particularly focused on endogenous hyperthyroidism and thyroid-stimulating hormone-suppressive therapy-associated hyperthyroidism in patients with differentiated thyroid cancer. Herein, we review the Korean Thyroid Association’s position statement on the evaluation and management of bone health associated with thyroid diseases.
-
Citations
Citations to this article as recorded by- Diagnosis and therapeutic approach to bone health in patients with hypopituitarism
Justyna Kuliczkowska-Płaksej, Aleksandra Zdrojowy-Wełna, Aleksandra Jawiarczyk-Przybyłowska, Łukasz Gojny, Marek Bolanowski
Reviews in Endocrine and Metabolic Disorders.2024;[Epub] CrossRef - Osteoporosis, Osteoarthritis, and Subchondral Insufficiency Fracture: Recent Insights
Shunichi Yokota, Hotaka Ishizu, Takuji Miyazaki, Daisuke Takahashi, Norimasa Iwasaki, Tomohiro Shimizu
Biomedicines.2024; 12(4): 843. CrossRef - Review on the protective activity of osthole against the pathogenesis of osteoporosis
Jincai Chen, Xiaofei Liao, Juwen Gan
Frontiers in Pharmacology.2023;[Epub] CrossRef
- Diagnosis and therapeutic approach to bone health in patients with hypopituitarism

- Thyroid
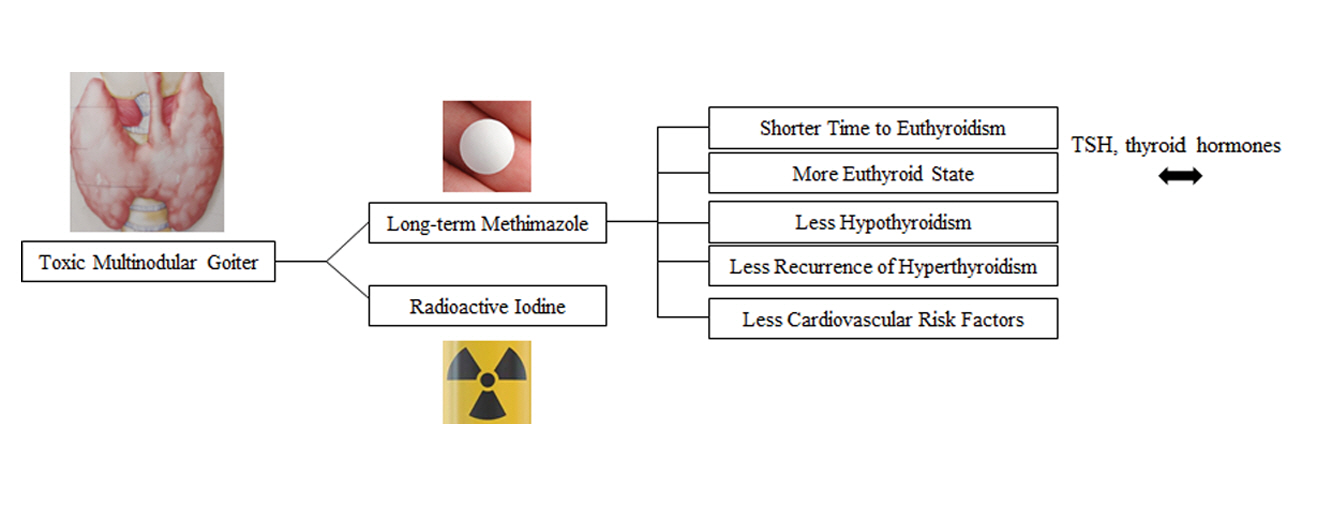
- Efficacy and Safety of Long-Term Methimazole versus Radioactive Iodine in the Treatment of Toxic Multinodular Goiter
- Fereidoun Azizi, Navid Saadat, Mir Alireza Takyar, Hengameh Abdi, Ladan Mehran, Atieh Amouzegar
- Endocrinol Metab. 2022;37(6):861-869. Published online November 23, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1476
- 3,923 View
- 372 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study compared the degree of sustained control of hyperthyroidism in patients with toxic multinodular goiter (TMNG) treated with long-term methimazole (LT-MMI) or radioactive iodine (RAI).
Methods
In this clinical trial, 130 untreated patients with TMNG were randomized to either LT-MMI or RAI treatment. Both groups were followed for 108 to 148 months, with median follow-up durations of 120 and 132 months in the LT-MMI and RAI groups, respectively. Both groups of patients were followed every 1 to 3 months in the first year and every 6 months thereafter.
Results
After excluding patients in whom the treatment modality was changed and those who were lost to follow-up, 53 patients in the LT-MMI group and 54 in the RAI group completed the study. At the end of the study period, 50 (96%) and 25 (46%) patients were euthyroid, and two (4%) and 25 (46%) were hypothyroid in LT-MMI and RAI groups, respectively. In the RAI group, four (8%) patients had subclinical hyperthyroidism. The mean time to euthyroidism was 4.3±1.3 months in LT-MMI patients and 16.3± 15.0 months in RAI recipients (P<0.001). Patients treated with LT-MMI spent 95.8%±5.9% of the 12-year study period in a euthyroid state, whereas this proportion was 72.4%±14.8% in the RAI-treated patients (P<0.001). No major treatment-related adverse events were observed in either group.
Conclusion
In patients with TMNG, LT-MMI therapy is superior to RAI treatment, as shown by the earlier achievement of euthyroidism and the longer duration of sustained normal serum thyrotropin. -
Citations
Citations to this article as recorded by- Mechanism of Huatan Sanjie Fang in improving goiter in Graves' disease mice based on the Hippo signaling pathway
Huimin Yuan, Wenxin Ma, Yifei Song, Hang Wang, Shuxin Yan, Silan Hao, Xiaoyun Zhu, Yang Tang
Journal of Traditional Chinese Medical Sciences.2023; 10(3): 289. CrossRef
- Mechanism of Huatan Sanjie Fang in improving goiter in Graves' disease mice based on the Hippo signaling pathway

- Thyroid
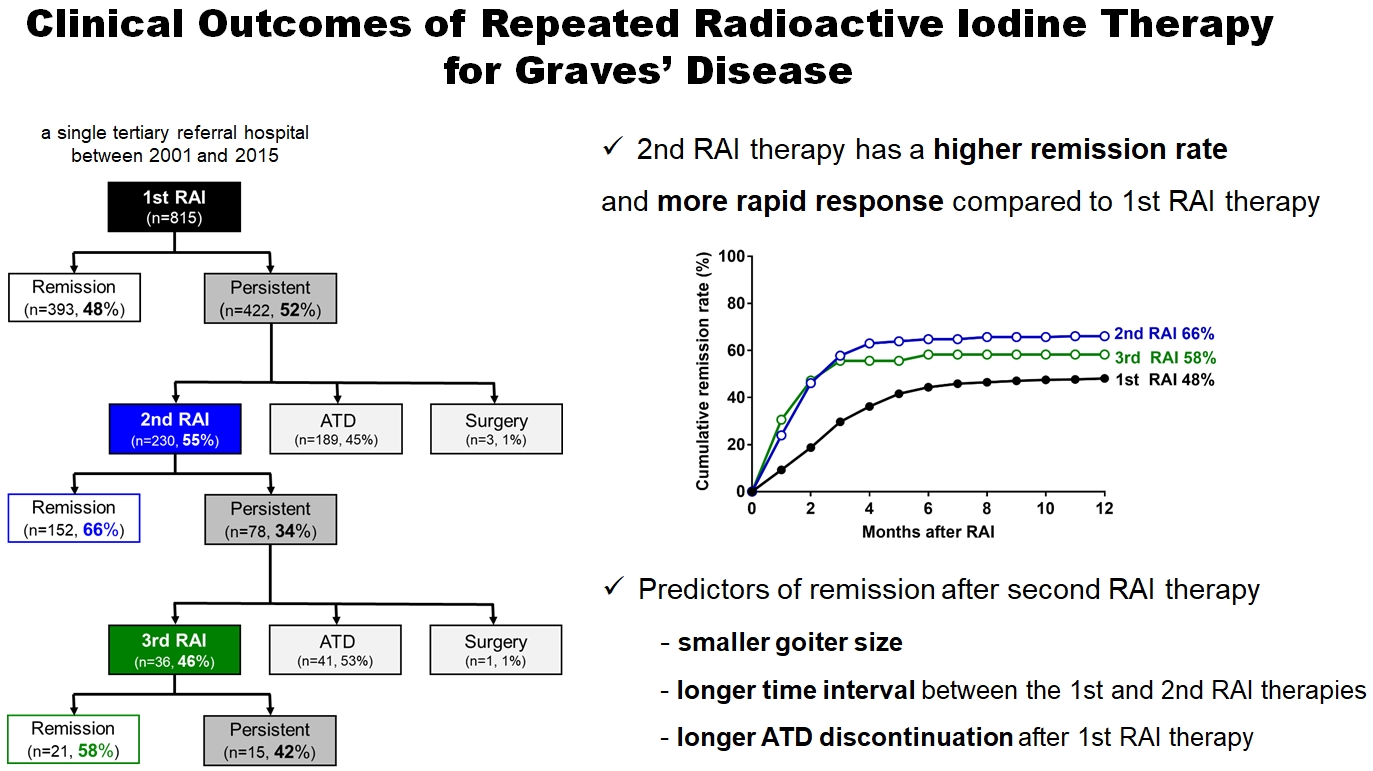
- Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
- Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
- Endocrinol Metab. 2022;37(3):524-532. Published online June 16, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1418
- 4,846 View
- 230 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Radioactive iodine (RAI) therapy is a successful therapeutic modality for Graves’ disease. However, RAI therapy can fail, and RAI therapy after antithyroid drugs (ATDs) has a lower remission rate. Therefore, many patients require repeated RAI therapy. This study investigated the clinical outcomes of repeated RAI therapy for Graves’ disease.
Methods
Patients who underwent RAI therapy as second-line therapy after failure of ATD treatment between 2001 and 2015 were reviewed. Remission was defined as hypothyroid or euthyroid status without ATD, and with or without levothyroxine at 12 months after RAI therapy.
Results
The 1-year remission rate after 2nd RAI therapy (66%, 152/230) is significantly higher than that after 1st RAI therapy (48%, 393/815) or long-term ATD treatment after 1st RAI therapy failure (42%). The clinical response to 2nd RAI therapy was more rapid. The median time intervals from the 2nd RAI therapy to ATD discontinuation (1.3 months) and to the start of levothyroxine replacement (2.5 months) were significantly shorter than those for the 1st RAI therapy. A smaller goiter size, a longer time interval between the 1st and 2nd RAI therapies, and a longer ATD discontinuation period predicted remission after the 2nd RAI therapy. Finally, in 78 patients who failed the 2nd RAI therapy, the mean ATD dosage significantly reduced 5.1 mg over 12 months.
Conclusion
Repeated RAI therapy can be a good therapeutic option, especially in patients with smaller goiters and those who are more responsive to the 1st RAI therapy. -
Citations
Citations to this article as recorded by- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Effect of liver dysfunction on outcome of radioactive iodine therapy for Graves’ disease
Yuyang Ze, Fei Shao, Xuefeng Feng, Shanmei Shen, Yan Bi, Dalong Zhu, Xiaowen Zhang
BMC Endocrine Disorders.2022;[Epub] CrossRef
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease

- Thyroid
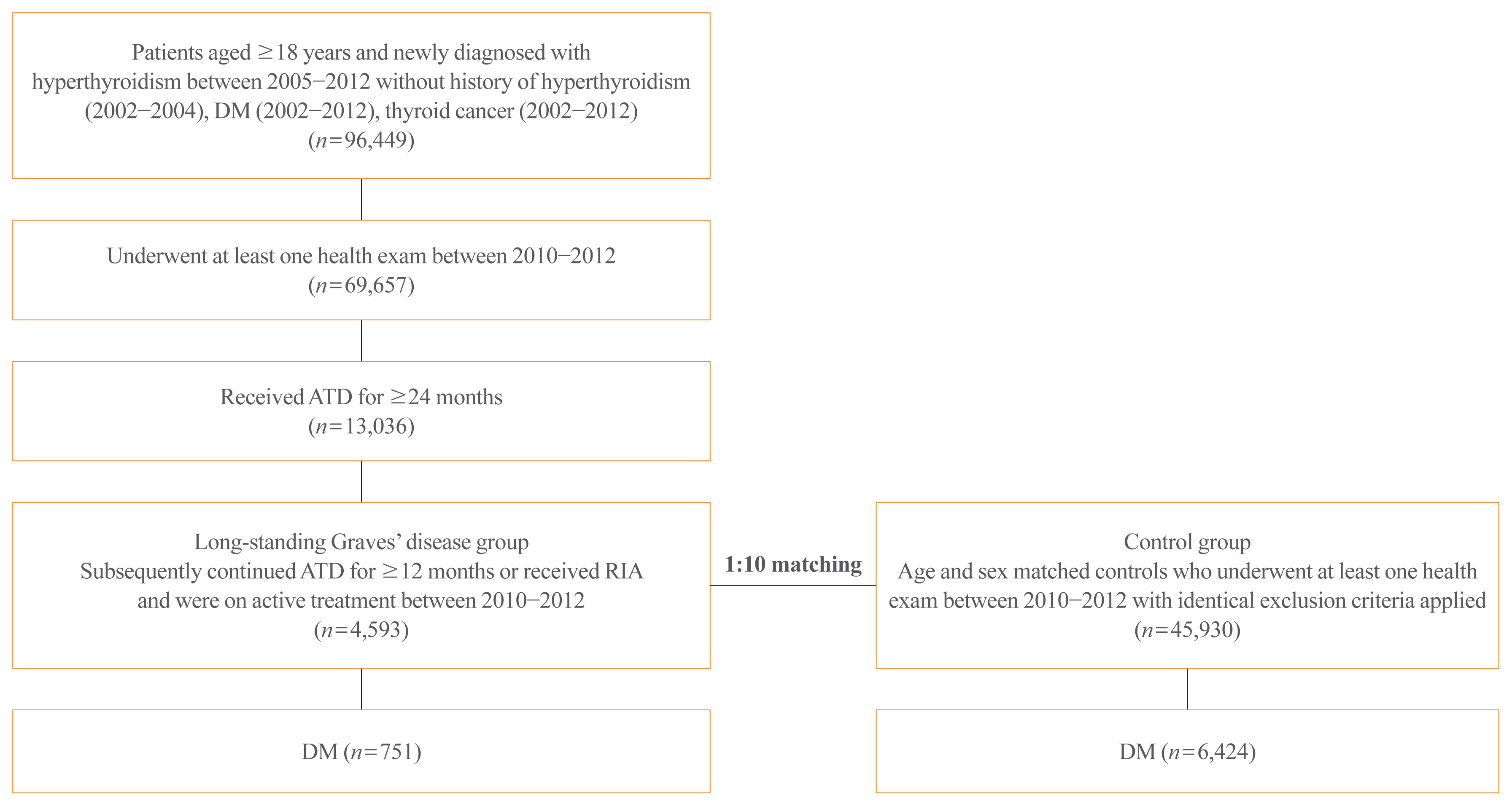
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
- Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Endocrinol Metab. 2021;36(6):1277-1286. Published online December 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1251
- 5,181 View
- 181 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The detrimental effects of excessive thyroid hormone on glucose metabolism have been widely investigated. However, the risk of diabetes in patients with long-standing hyperthyroidism, especially according to treatment modality, remains uncertain, with few longitudinal studies.
Methods
The risk of diabetes in patients with Graves’ disease treated with antithyroid drugs (ATDs) for longer than the conventional duration (≥2 years) was compared with that in age-and sex-matched controls. The risk was further compared according to subsequent treatment modalities after a 24-month course of ATD: continuation of ATD (ATD group) vs. radioactive iodine ablation (RIA) group.
Results
A total of 4,593 patients were included. Diabetes was diagnosed in 751 (16.3%) patients over a follow-up of 7.3 years. The hazard ratio (HR) for diabetes, after adjusting for various known risk factors, was 1.18 (95% confidence interval [CI], 1.10 to 1.28) in patients with hyperthyroidism. Among the treatment modality groups, the RIA group (n=102) had a higher risk of diabetes than the ATD group (n=4,491) with HR of 1.56 (95% CI, 1.01 to 2.42). Further, the risk of diabetes increased with an increase in the ATD treatment duration (P for trend=0.019).
Conclusion
The risk of diabetes was significantly higher in patients with long-standing Graves’ disease than in the general population, especially in patients who underwent RIA and prolonged ATD treatment. Special attention to hyperglycemia during follow-up along with effective control of hyperthyroidism may be necessary to reduce the risk of diabetes in these patients. -
Citations
Citations to this article as recorded by- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience
Nadia Sawicka-Gutaj, Dawid Gruszczyński, Natalia Zawalna, Kacper Nijakowski, Agnieszka Skiba, Mateusz Pochylski, Jerzy Sowiński, Marek Ruchała
Pharmacological Reports.2024; 76(1): 185. CrossRef - Increased risk of diabetes mellitus and hyperlipidemia in patients with differentiated thyroid cancer
Hwa Young Ahn, Jooyoung Lee, Jinmo Kang, Eun Kyung Lee
European Journal of Endocrinology.2024; 190(3): 248. CrossRef - Prevalencia de diabetes en personas con disfunción tiroidea
Juan J. Díez, Pedro Iglesias
Medicina Clínica.2023; 160(8): 333. CrossRef - Control of Thyroid Dysfunction in Spanish Population Registered in
the Primary Care Clinical Database: An Analysis of the Proportion of Patients
with Thyrotropin Values Outside the Reference Range
Juan J. Díez, Pedro Iglesias
Hormone and Metabolic Research.2023; 55(03): 184. CrossRef - Prevalence of thyroid dysfunction and its relationship to income level and employment status: a nationwide population-based study in Spain
Juan J. Díez, Pedro Iglesias
Hormones.2023; 22(2): 243. CrossRef - Prevalence of diabetes in people with thyroid dysfunction
Juan J. Díez, Pedro Iglesias
Medicina Clínica (English Edition).2023; 160(8): 333. CrossRef - Diabetes Mellitus Secondary to Endocrine Diseases: An Update of Diagnostic and Treatment Particularities
Mihaela Simona Popoviciu, Lorena Paduraru, Raluca Marinela Nutas, Alexandra Maria Ujoc, Galal Yahya, Kamel Metwally, Simona Cavalu
International Journal of Molecular Sciences.2023; 24(16): 12676. CrossRef - Thyroid Eye Disease and Its Association With Diabetes Mellitus: A Major Review
Roshmi Gupta, Pramila Kalra, Lakshmi B. Ramamurthy, Suryasnata Rath
Ophthalmic Plastic & Reconstructive Surgery.2023; 39(6S): S51. CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef
- Safety of non-standard regimen of systemic steroid therapy in patients with Graves’ orbitopathy: a single-centre experience

- Thyroid
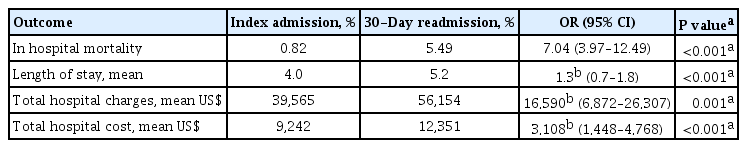
- Outcomes and Predictors of 30-Day Readmissions for Hyperthyroidism: A Nationwide Study
- Michael Salim, Zain El-amir, Asim Kichloo, Farah Wani, Ehizogie Edigin, Hafeez Shaka
- Endocrinol Metab. 2021;36(6):1307-1311. Published online December 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1190
- 3,863 View
- 85 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Hyperthyroidism is associated with an elevated risk of cardiovascular events and worse hospital outcomes. The Nationwide Readmissions Database (NRD) 2018 was used to determine the characteristics of 30-day readmission in patients with hyperthyroidism. The 30-day all-cause readmission rate for hyperthyroidism was 10.3%. About 21.7% had hyperthyroidism as the principal diagnosis on readmission. Readmissions were associated with an increased odds of inpatient mortality (odds ratio, 7.04; 95% confidence interval [CI], 3.97 to 12.49), length of stay (5.2 days vs. 4.0 days; 95% CI, 0.7 to 1.8), total hospital charges, and cost of hospitalizations. Independent predictors of 30-day all-cause readmissions included Charlson Comorbidity Index ≥3 (adjusted hazard ratio [aHR], 1.76; 95% CI, 1.15 to 2.71), discharge against medical advice (aHR, 2.30; 95% CI, 1.50 to 3.53), protein-energy malnutrition (aHR, 1.54; 95% CI, 1.15 to 2.07), and atrial fibrillation (aHR, 1.41; 95% CI, 1.11 to 1.79). Aggressive but appropriate monitoring is warranted in patients with hyperthyroidism to prevent readmissions.

- Clinical Study
- The Association of Overt and Subclinical Hyperthyroidism with the Risk of Cardiovascular Events and Cardiovascular Mortality: Meta-Analysis and Systematic Review of Cohort Studies
- Seo Young Sohn, Eunyoung Lee, Min Kyung Lee, Jae Hyuk Lee
- Endocrinol Metab. 2020;35(4):786-800. Published online November 25, 2020
- DOI: https://doi.org/10.3803/EnM.2020.728
- 6,045 View
- 288 Download
- 20 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
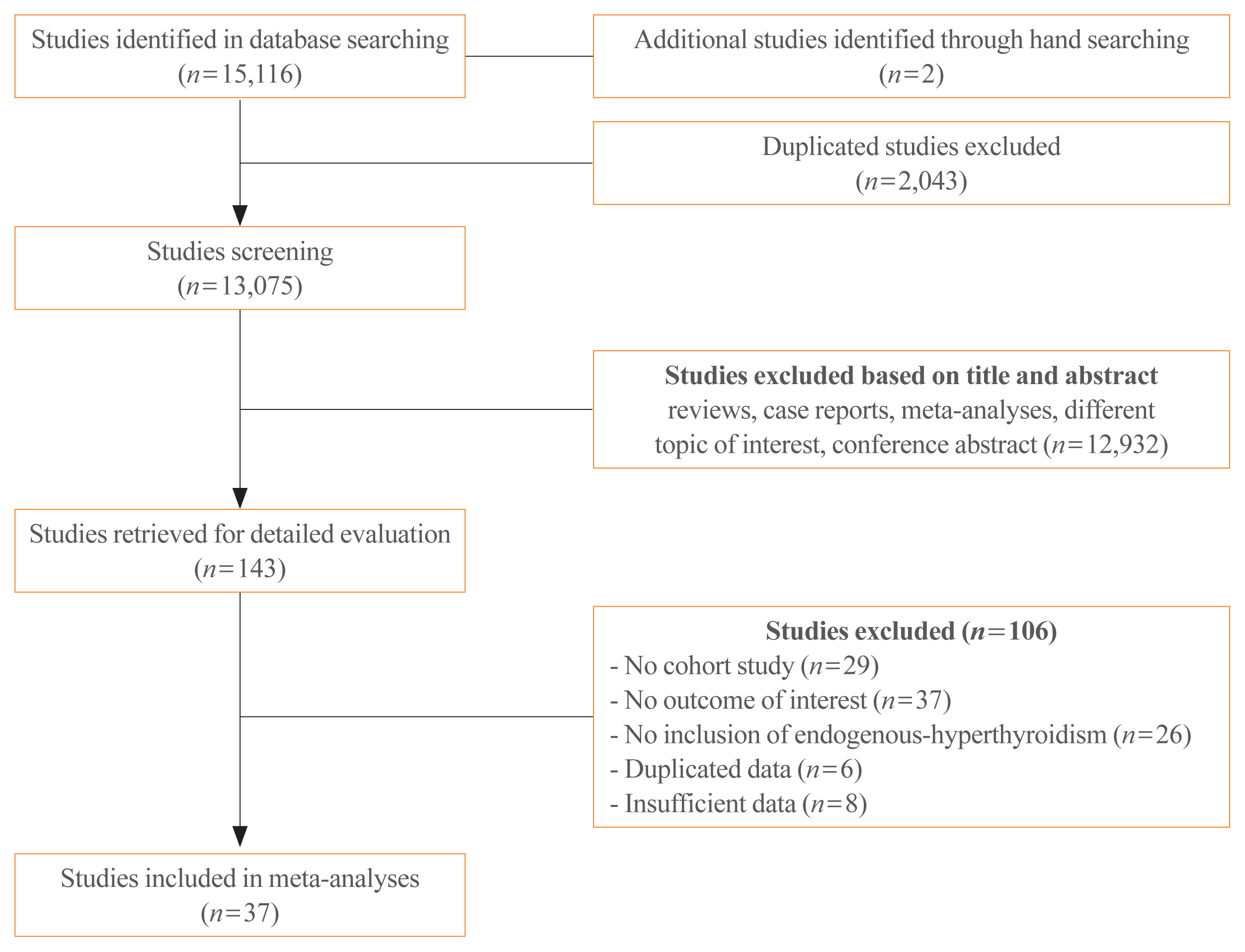
Whether hyperthyroidism is an independent risk factor for cardiovascular events remains controversial. We aimed to evaluate the association of overt and subclinical hyperthyroidism with the risk of ischemic heart disease (IHD), stroke, heart failure, and cardiovascular mortality.
Methods
Studies regarding the association between hyperthyroidism and cardiovascular events were searched on PubMed and Embase databases. The cardiovascular disease (CVD) risk was classified as high and low, based on pre-existing diseases, including history of coronary, cerebral, or peripheral artery disease; heart failure; atrial fibrillation; diabetes mellitus; or chronic kidney disease.
Results
Thirty-seven cohort studies were included in this meta-analysis. The pooled hazard ratio for subjects with overt hyperthyroidism compared with the control group was 1.11 (95% confidence interval [CI], 1.03 to 1.19) for IHD, 1.35 (95% CI, 1.03 to 1.75) for stroke, and 1.20 (95% CI, 1.00 to 1.46) for cardiovascular mortality. For subjects with subclinical hyperthyroidism, the pooled hazard ratio was 1.24 (95% CI, 1.07 to 1.45) for IHD, when compared with the control group. Subgroup analysis by CVD risk showed that the risk of stroke in overt hyperthyroidism was increased in the low CVD risk group; however, these association was not observed in the high CVD risk group. Similarly, the risk of IHD in subjects with subclinical hyperthyroidism was significantly increased in the low CVD risk group.
Conclusion
Overt hyperthyroidism is associated with increased risk of IHD, stroke, and cardiovascular mortality, and subclinical hyperthyroidism is associated with increased risk of IHD. These associations were particularly observed in the low risk CVD group without underlying CVD. -
Citations
Citations to this article as recorded by- Trends in Prevalence of Thyroid Dysfunction and its Associations With Mortality Among US Participants, 1988-2012
Xiaowen Zhang, Yong Wang, Hongwei Wang, Xinlin Zhang
The Journal of Clinical Endocrinology & Metabolism.2024; 109(2): e657. CrossRef - Adequacy of thyroid hormone replacement for people with hypothyroidism in real‐world settings: A systematic review and meta‐analysis of observational studies
Agathoklis Efthymiadis, Matthew Henry, Dimitrios Spinos, Marianthi Bourlaki, Alexandros Tsikopoulos, Angeliki Bourazana, Anastasios Bastounis, Konstantinos Tsikopoulos
Clinical Endocrinology.2024; 100(5): 488. CrossRef - Thyroid Disorders and Peripheral Arterial Disease
Katica Bajuk Studen, Simona Gaberscek, Katja Zaletel, Ales Blinc, Miso Sabovic, Gerit-Holger Schernthaner, Panagiotis Anagnostis, Pier Luigi Antignani, Mojca Jensterle, Dimitri P Mikhailidis, Pavel Poredos
Current Vascular Pharmacology.2024; 22(1): 36. CrossRef - Higher Risk of Incident Hyperthyroidism in Patients With Atrial Fibrillation
Pang-Shuo Huang, Jen-Fang Cheng, Jien-Jiun Chen, Yi-Chih Wang, Juey-Jen Hwang, Cho-Kai Wu, Chia-Ti Tsai
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): 92. CrossRef - Eurasian clinical guidelines for the diagnosis and treatment of secondary (symptomatic) forms of arterial hypertension (2022)
I. E. Chazova, N. M. Chikhladze, N. V. Blinova, Zh. E. Belaya, N. M. Danilov, E. M. Elfimova, A. Yu. Litvin, L. Ya. Rozhinskaya, N. Yu. Sviridenko, M. Yu. Shvetsov, V. A. Azizov, E. A. Grigorenko, N. P. Mit’kovskaja, I. I. Mustafaev, A. G. Polupanov, A. S
Eurasian heart journal.2023; (1): 6. CrossRef -
Sympathetic Activation Promotes Cardiomyocyte Apoptosis in a Rabbit Susceptibility Model of Hyperthyroidism-Induced Atrial Fibrillation via the p38 MAPK Signaling Pathway
Jialin Zheng, Shijian Zhao, Qishi Yang, Yantao Wei, Jianmei Li, Tao Guo
Critical Reviews in Eukaryotic Gene Expression.2023; 33(5): 17. CrossRef - Cardiovascular outcomes in subclinical thyroid disease: an update
Matthew D. Ettleson
Current Opinion in Endocrinology, Diabetes & Obesity.2023; 30(5): 218. CrossRef - Lower free triiodothyronine levels are associated with higher all-cause and cardiovascular mortality in people with diabetes-NHANES 2007–2012
Chang Liu, Zhong Xin, Lin Hua
Diabetes Research and Clinical Practice.2023; 202: 110811. CrossRef - Hyperthyroidism
Sun Y. Lee, Elizabeth N. Pearce
JAMA.2023; 330(15): 1472. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef - Risks of suboptimal and excessive thyroid hormone replacement across ages
U. Feldt-Rasmussen, G. Effraimidis, S. Bliddal, M. Klose
Journal of Endocrinological Investigation.2023; 47(5): 1083. CrossRef - Association of Mild Thyroid Dysfunction and Adverse Prognosis Among Chinese Patients With Acute ST Segment Elevation Myocardial Infarction
Mei-Fang Li, Ze-Tao Wei, Shuai Li, Qi-Ming Feng, Jing-Bo Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Cardiovascular Effects of Subclinical Hyperthyroidism following Percutaneous Coronary Intervention
Ricardo Correa, Ricardo Villela
Clinical Thyroidology.2022; 34(6): 240. CrossRef - Weight Gain and Body Composition Changes during the Transition of Thyroid Function in Patients with Graves’ Disease Undergoing Radioiodine Treatment
Zhenqin Cai, Qiyu Chen, Yan Ling, Henrik Falhammar
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Minor perturbations of thyroid homeostasis and major cardiovascular endpoints—Physiological mechanisms and clinical evidence
Patrick Müller, Melvin Khee-Shing Leow, Johannes W. Dietrich
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Role of thyroid hormones-induced oxidative stress on cardiovascular physiology
María Laura Barreiro Arcos
Biochimica et Biophysica Acta (BBA) - General Subjects.2022; 1866(12): 130239. CrossRef - Yearly Incidence of Stroke and Bleeding in Atrial Fibrillation with Concomitant Hyperthyroidism: A National Discharge Database Study
Juqian Zhang, Arnaud Bisson, Grégoire Fauchier, Alexandre Bodin, Julien Herbert, Pierre Henri Ducluzeau, Gregory Y. H. Lip, Laurent Fauchier
Journal of Clinical Medicine.2022; 11(5): 1342. CrossRef - Platelet abnormalities in autoimmune thyroid diseases: A systematic review and meta-analysis
Yu-tian Cao, Kai-yu Zhang, Jing Sun, Yan Lou, Tian-su Lv, Xinyi Yang, Wen-hui Zhang, Jiang-yi Yu, Qi-biao Wu, Xi-qiao Zhou
Frontiers in Immunology.2022;[Epub] CrossRef - Subclinical Hyperthyroidism: A Review of the Clinical Literature
Karen Tsai, Angela M. Leung
Endocrine Practice.2021; 27(3): 254. CrossRef - Thyroid and heart, a clinically relevant relationship
G. Corona, L. Croce, C. Sparano, L. Petrone, A. Sforza, M. Maggi, L. Chiovato, M. Rotondi
Journal of Endocrinological Investigation.2021; 44(12): 2535. CrossRef - Antithyroid Drug Treatment in Graves’ Disease
Jae Hoon Chung
Endocrinology and Metabolism.2021; 36(3): 491. CrossRef - Cardiovascular Outcomes in Thyroid Cancer Patients Treated With Thyroidectomy: A Meta-Analysis
Eun Kyung Lee, Hwa Young Ahn, Eu Jeong Ku, Won Sang Yoo, Young Ki Lee, Kee-Hyun Nam, Young Jun Chai, Shinje Moon, Yuh-Seog Jung
The Journal of Clinical Endocrinology & Metabolism.2021;[Epub] CrossRef
- Trends in Prevalence of Thyroid Dysfunction and its Associations With Mortality Among US Participants, 1988-2012

- Atrial Fibrillation in Patients with Hyperthyroidism.
- Ju Yong Lee, Chang Ho Song, Byeung Su Yu, Choon Hee Chung, Yoon Sok Chung, Hyeon Man Kim
- J Korean Endocr Soc. 1995;10(1):52-57. Published online November 6, 2019
- 1,216 View
- 47 Download
-
 Abstract
Abstract
 PDF
PDF - Hyperthyroidism is a well known cause of atrial fibrillation. It is also known that control of hyperthyroidism can usually curb thyrotoxic atrial fibrillation and restore sinus rhythm. In this study, 282 patients with hyperthyroidism were investigated to quantify the incidence of atrial fibrillation, and to identify the vulnerable groups. In addition, we compared two groups of subjects with atrial fibrillation-one group with hyperthyroidism and the other group without - to study their reversion rate to sinus rhythm. Lastly, we investigated the factors affecting reversion to sinus rhythm in patients with thyrotoxic atrial fibrillation.The results were follows;1) Among 282 patients with hyperthyroidism, 35 cases(12.4%) had atrial fibrillation. Atrial fibrillations were more prevalent among male patient(19.4%) and elderly patients(42.9%) than female patients(10.0%) and young patients(10.0%).2) Reversion to normal sinus rhythm in patients with thyrotoxic atrial fibrillation(39.3%) was significantly higher than that in patients without hyperthyroidism(17.4%, p<0.001).3) Reversion to normal sinus rhythm was achieved within 28 weeks from the beginnig of antithyroid treatment in patients with thyrotoxic atrial fibrillation. Although there were no significant differences in mean age, sex ratio, and initial and follow-up thyroid hormone levels between the reversion group and non-reversion group, associated heart diseases were more prevalent in the latter group(18.2% vs. 47.1%).It can be concluded that thyrotoxic atrial fibrillations were more common in male patient and elderly patient groups, and could be frequently reverted to normal sinus rhythm by antithyroid treatment. We also suggest that the duration of artrial fibrillation(from intial onset of the condition), and associated heart diseases, may be important predictive factors for the reversion of atrial fibrillation in patients with hyperthyroidism.

- Thyroid
- Digital Medicine in Thyroidology: A New Era of Managing Thyroid Disease
- Jae Hoon Moon, Steven R. Steinhubl
- Endocrinol Metab. 2019;34(2):124-131. Published online June 24, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.2.124
- 5,402 View
- 135 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Digital medicine has the capacity to affect all aspects of medicine, including disease prediction, prevention, diagnosis, treatment, and post-treatment management. In the field of thyroidology, researchers are also investigating potential applications of digital technology for the thyroid disease. Recent studies using artificial intelligence (AI)/machine learning (ML) have reported reasonable performance for the classification of thyroid nodules based on ultrasonographic (US) images. AI/ML-based methods have also shown good diagnostic accuracy for distinguishing between benign and malignant thyroid lesions based on cytopathologic findings. Assistance from AI/ML methods could overcome the limitations of conventional thyroid US and fine-needle aspiration cytology. A web-based database has been developed for thyroid cancer care. In addition to its role as a nationwide registry of thyroid cancer, it is expected to serve as a clinical platform to facilitate better thyroid cancer care and as a research platform providing comprehensive disease-specific big data. Evidence has been found that biosignal monitoring with wearable devices may predict thyroid dysfunction. This real-world thyroid function monitoring could aid in the management and early detection of thyroid dysfunction. In the thyroidology field, research involving the range of digital medicine technologies and their clinical applications is expected to be even more active in the future.
-
Citations
Citations to this article as recorded by- AI in Thyroid Cancer Diagnosis: Techniques, Trends, and Future Directions
Yassine Habchi, Yassine Himeur, Hamza Kheddar, Abdelkrim Boukabou, Shadi Atalla, Ammar Chouchane, Abdelmalik Ouamane, Wathiq Mansoor
Systems.2023; 11(10): 519. CrossRef - Empirical Method for Thyroid Disease Classification Using a Machine Learning Approach
Tahir Alyas, Muhammad Hamid, Khalid Alissa, Tauqeer Faiz, Nadia Tabassum, Aqeel Ahmad, Gulnaz Afzal
BioMed Research International.2022; 2022: 1. CrossRef - Deep Learning Based Classification of Wrist Cracks from X-ray Imaging
Jahangir Jabbar, Muzammil Hussain, Hassaan Malik, Abdullah Gani, Ali Haider Khan, Muhammad Shiraz
Computers, Materials & Continua.2022; 73(1): 1827. CrossRef - Diagnostic Performance of Kwak, EU, ACR, and Korean TIRADS as Well as ATA Guidelines for the Ultrasound Risk Stratification of Non-Autonomously Functioning Thyroid Nodules in a Region with Long History of Iodine Deficiency: A German Multicenter Trial
Philipp Seifert, Simone Schenke, Michael Zimny, Alexander Stahl, Michael Grunert, Burkhard Klemenz, Martin Freesmeyer, Michael C. Kreissl, Ken Herrmann, Rainer Görges
Cancers.2021; 13(17): 4467. CrossRef - Association between Thyroid Function and Heart Rate Monitored by Wearable Devices in Patients with Hypothyroidism
Ki-Hun Kim, Juhui Lee, Chang Ho Ahn, Hyeong Won Yu, June Young Choi, Ho-Young Lee, Won Woo Lee, Jae Hoon Moon
Endocrinology and Metabolism.2021; 36(5): 1121. CrossRef - Deep Learning based Classification of Thyroid Cancer using Different Medical Imaging Modalities : A Systematic Review
Maheen Ilyas, Hassaan Malik, Muhammad Adnan, Umair Bashir, Wajahat Anwaar Bukhari, Muhammad Imran Ali Khan, Adnan Ahmad
VFAST Transactions on Software Engineering.2021; 9(4): 1. CrossRef - Ultrasound risk stratification systems for thyroid nodule: between lights and shadows, we are moving towards a new era
Pierpaolo Trimboli, Cosimo Durante
Endocrine.2020; 69(1): 1. CrossRef - Associations of Thyroid Hormones and Resting Heart Rate in Patients
Referred to Coronary Angiography
Eva Steinberger, Stefan Pilz, Christian Trummer, Verena Theiler-Schwetz, Markus Reichhartinger, Thomas Benninger, Marlene Pandis, Oliver Malle, Martin H. Keppel, Nicolas Verheyen, Martin R. Grübler, Jakob Voelkl, Andreas Meinitzer, Winfried März
Hormone and Metabolic Research.2020; 52(12): 850. CrossRef
- AI in Thyroid Cancer Diagnosis: Techniques, Trends, and Future Directions

- Thyroid
- Graves' Disease: Can It Be Cured?
- Wilmar M. Wiersinga
- Endocrinol Metab. 2019;34(1):29-38. Published online March 21, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.1.29
- 16,157 View
- 511 Download
- 44 Web of Science
- 46 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Whether or not Graves' hyperthyroidism can be really cured, depends on the definition of “cure.” If eradication of thyroid hormone excess suffices for the label “cure,” then all patients can be cured because total thyroidectomy or high doses of 131I will abolish hyperthyroidism albeit at the expense of creating another disease (hypothyroidism) requiring lifelong medication with levothyroxine. I would not call this a “cure,” which I would like to define as a state with stable thyroid stimulating hormone (TSH), free thyroxine, and triiodothyronine serum concentrations in the normal range in the absence of any thyroid medication. Surgery and radioiodine are unlikely to result in so-defined cures, as their preferable aim as stated in guidelines is to cause permanent hypothyroidism. Discontinuation of antithyroid drugs is followed by 50% recurrences within 4 years; before starting therapy the risk of recurrences can be estimated with the Graves' Recurrent Events After Therapy (GREAT) score. At 20-year follow-up about 62% had developed recurrent hyperthyroidism, 8% had subclinical hypothyroidism, and 3% overt hypothyroidism related to TSH receptor blocking antibodies and thyroid peroxidase antibodies. Only 27% was in remission, and might be considered cured. If the definition of “cure” would also include the disappearance of thyroid antibodies in serum, the proportion of cured patients would become even lower.
-
Citations
Citations to this article as recorded by- Multifunctional nanoparticle-mediated combining therapy for human diseases
Xiaotong Li, Xiuju Peng, Makhloufi Zoulikha, George Frimpong Boafo, Kosheli Thapa Magar, Yanmin Ju, Wei He
Signal Transduction and Targeted Therapy.2024;[Epub] CrossRef - Prenatal double-hit with aluminium and cadmium mediate testicular atrophy and hypothalamic hypoplasia: the role of oxido-nitrergic stress and endocrine perturbations
Emmanuel Okhue, Helen Ejiro Kadiri, Patrick Chukwuyenum Ichipi-Ifukor, Benneth Ben-Azu, Samuel Ogheneovo Asagba, Fidelis Ifeakachuku Achuba, John Chukwuma Oyem
BioMetals.2024; 37(2): 477. CrossRef - Surgical outcome after thyroidectomy due to Graves’ disease and Lugol iodine treatment: a retrospective register-based cohort study
Fredric Hedberg, Henrik Falhammar, Jan Calissendorff, Robert Bränström
Endocrine.2024;[Epub] CrossRef - Graves disease is associated with increased risk of clinical Alzheimer’s disease: evidence from the Medicare system
Arseniy Pavlovich Yashkin, Stanislav Kolpakov, Svetlana Ukraintseva, Anatoliy Yashin, Igor Akushevich
Clinical Diabetes and Endocrinology.2024;[Epub] CrossRef - A 2023 International Survey of Clinical Practice Patterns in the Management of Graves Disease: A Decade of Change
Danilo Villagelin, David S Cooper, Henry B Burch
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Predictors of Prolonged Euthyroidism After Radioactive Iodine Treatment for Graves’ Disease: A Pilot Study
Jin-Ying Lu, Kuan-Hua Chen, Shyang-Rong Shih, Fang-Yu Wen, Wan-Chen Wu, Ting-Chu Chen, Fu-Chang Hu
Endocrine Practice.2023; 29(2): 89. CrossRef - Case of Graves’ disease recovery
Andrey Valerievich Ushakov
Journal of Clinical and Translational Endocrinology: Case Reports.2023; 27: 100139. CrossRef - Outcomes of Radioactive Iodine Versus Surgery for the Treatment of Graves’ Disease: a Systematic Review and Meta-analysis
Mohamed AbdAlla Salman, Mohamed Moustafa Assal, Ahmed Salman, Mohammed Elsherbiney
Indian Journal of Surgery.2023;[Epub] CrossRef - Association between high mobility group box-1 circulation level and Graves' ophthalmopathy
Mohammad Robikhul Ikhsan, Nyoman Kertia, Supanji Supanji, Bambang Udji djoko Rianto, Dhite Bayu Nugroho
F1000Research.2023; 12: 767. CrossRef - New-onset and relapsed Graves’ disease following COVID-19 vaccination: a comprehensive review of reported cases
Kan Chen, Yiyang Gao, Jing Li
European Journal of Medical Research.2023;[Epub] CrossRef - REVIEW OF SARS-CORONAVIRUS-2 REPERCUSSIONS ON THYROID GLAND IN THE CONTEXT OF HYPERTHYROIDISM
SHUBHAM SINGH, MONIKA, RUPA MAZUMDER, AVIJIT MAZUMDER
International Journal of Applied Pharmaceutics.2023; : 17. CrossRef - Effectiveness and potential mechanism of Jiawei-Xiaoyao-San for hyperthyroidism: a systematic review
Wenxin Ma, Xiaowen Zhang, Ruotong Zhao, Yang Tang, Xiaoyun Zhu, Longkun Liu, Mingyuan Xu, Ge Wang, Peiyue Peng, Jianping Liu, Zhaolan Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Associations of serum keratin 1 with thyroid function and immunity in Graves’ disease
Chao-Wen Cheng, Wen-Fang Fang, Jiunn-Diann Lin, Appuwawadu Mestri Nipun Lakshitha de Silva
PLOS ONE.2023; 18(11): e0289345. CrossRef - Management of Graves’ hyperthyroidism: present and future
Luigi Bartalena, Eliana Piantanida, Daniela Gallo, Silvia Ippolito, Maria Laura Tanda
Expert Review of Endocrinology & Metabolism.2022; 17(2): 153. CrossRef - The Prediction Model Using Thyroid-stimulating Immunoglobulin Bioassay For Relapse of Graves’ Disease
Han-Sang Baek, Jaejun Lee, Chai-Ho Jeong, Jeongmin Lee, Jeonghoon Ha, Kwanhoon Jo, Min-Hee Kim, Jae Hyoung Cho, Moo Il Kang, Dong-Jun Lim
Journal of the Endocrine Society.2022;[Epub] CrossRef - Efficacy of Radioiodine Therapy in Patients With Primary Hyperthyroidism: An Institutional Review From Pakistan
Asim Munir Alvi, Umal Azmat, Waqas Shafiq, Abdul Hannan Ali Rasheed, Ahmed Imran Siddiqi, Sardar Khan, Sara Ashfaq, Hira Irfan , Humayun Bashir, Muhammad Abu Bakar, Kashif Asghar
Cureus.2022;[Epub] CrossRef - Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
Endocrinology and Metabolism.2022; 37(3): 524. CrossRef - Endocrine Surgery and Pediatic Surgery Partnership Reduces Complication Rate of Pediatric Thyroidectomy
Ali Sayan, Mehmet Üstün, Mehmet Mert, Cem Karaali, Gökhan Köylüoğlu
Journal of Dr Behcet Uz Children s Hospital.2022; 12(2): 164. CrossRef - Thyroid-related adverse events induced by immune checkpoint inhibitors
Alexandra Chera, Andreea Lucia Stancu, Octavian Bucur
Frontiers in Endocrinology.2022;[Epub] CrossRef - A case of Hashimoto's thyroiditis following Graves' disease
Ibtissem Oueslati, Salma Salhi, Meriem Yazidi, Fatma Chaker, Melika Chihaoui
Clinical Case Reports.2022;[Epub] CrossRef - Changes in the T and B lymphocyte subset profiles upon treatment of patients with Graves’ disease with radioactive iodine
A. A. Savchenko, M. A. Dudina, S. A. Dogadin, A. G. Borisov, I. V. Kudryavtsev, D. V. Fomina, V. D. Belenyuk
Medical Immunology (Russia).2022; 24(5): 1007. CrossRef - A survey of the young person’s experience of Graves’ disease and its management
Laura Claire Lane, Judith Rankin, Tim Cheetham
Clinical Endocrinology.2021; 94(2): 330. CrossRef - Serum T3 Level and Duration of Minimum Maintenance Dose Therapy Predict Relapse in Methimazole-Treated Graves Disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Rajata Rajatanavin, Thep Himathongkam
Journal of the Endocrine Society.2021;[Epub] CrossRef - Dosimetry-guided radioiodine therapy of hyperthyroidism: long-term experience and implications for guidelines
Thomas Leitha, Manuela Schartel, Ingrid Hurtl, Rudolf Bednar, Franz König, Karl Mayrhofer, Flavia Pietschmann
Nuclear Medicine Communications.2021; 42(2): 150. CrossRef - Practice patterns and outcomes in the management of Thai patients with Graves’ disease
Yotsapon Thewjitcharoen, Krittadhee Karndumri, Waralee Chatchomchuan, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanathayanoroj, Nampetch Lekpittaya, Worawit Kittipoom, Tawee Anuntakulnatee, Somboon Vongterapak, Siriwan Butadej, Soontaree Nakas
Thyroid Research.2021;[Epub] CrossRef - Un case report letterario di tireotossicosi in La coscienza di Zeno di Italo Svevo
Francesco Trimarchi, Luigi Bartalena, Stefano Arieti, Roberto Toni
L'Endocrinologo.2021; 22(2): 149. CrossRef - Medical treatment of thyrotoxicosis
Lorenzo SCAPPATICCIO, Giuseppe BELLASTELLA, Maria I. MAIORINO, Luca GIOVANELLA, Katherine ESPOSITO
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2021;[Epub] CrossRef - Hiccups as a Rare Presentation of Thyrotoxicosis Triaged by an Epidural Steroid Injection
Omar Al-Radideh, Iyad Farouji, Theodore DaCosta, Hossam Abed, Nicholas Baranestky
Cureus.2021;[Epub] CrossRef - Long-term antithyroid drug therapy
David S. Cooper
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 510. CrossRef - The Continuum of Thyroid Disorders Related to Immune Checkpoint Inhibitors: Still Many Pending Queries
Maria V. Deligiorgi, Sofia Sagredou, Lampros Vakkas, Dimitrios T. Trafalis
Cancers.2021; 13(21): 5277. CrossRef - Recurrence of Graves’ Disease: What Genetics of HLA and PTPN22 Can Tell Us
Daniela Vejrazkova, Josef Vcelak, Eliska Vaclavikova, Marketa Vankova, Katerina Zajickova, Jana Vrbikova, Michaela Duskova, Petra Pacesova, Zdenek Novak, Bela Bendlova
Frontiers in Endocrinology.2021;[Epub] CrossRef - Most Patients with Graves’ Disease Treated with Antithyroid Drugs Eventually Require Additional Therapies
Mary H. Samuels
Clinical Thyroidology.2020; 32(1): 9. CrossRef - Patterns of Use, Efficacy, and Safety of Treatment Options for Patients with Graves' Disease: A Nationwide Population-Based Study
Juan P. Brito, Stephanie Payne, Naykky Singh Ospina, Rene Rodriguez-Gutierrez, Spyridoula Maraka, Lindsey R. Sangaralingham, Nicole M. Iñiguez-Ariza, Victor M. Montori, Marius N. Stan
Thyroid.2020; 30(3): 357. CrossRef - Long-Term Treatment of Hyperthyroidism with Antithyroid Drugs: 35 Years of Personal Clinical Experience
Fereidoun Azizi
Thyroid.2020; 30(10): 1451. CrossRef - Predictive factors for early hypothyroidism following the radioactive iodine therapy in Graves’ disease patients
Rui-Ting Hu, De-Shan Liu, Bin Li
BMC Endocrine Disorders.2020;[Epub] CrossRef - The Concept of Cure in Thyroid Diseases
Fereidoun Azizi
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Der Biomarker TSH bei Schilddrüsenautonomien
K. Passek, N. Zulauf, E. Wanke, G. M. Oremek
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie.2020; 70(4): 177. CrossRef - Management of Graves’ Hyperthyroidism: More Than a Century of Progression
Hengameh Abdi, Atieh Amouzegar
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Corticosteroid Pulse Therapy for Graves' Ophthalmopathy Reduces the Relapse Rate of Graves' Hyperthyroidism
Rosario Le Moli, Pasqualino Malandrino, Marco Russo, Fabrizio Lo Giudice, Francesco Frasca, Antonino Belfiore, Riccardo Vigneri
Frontiers in Endocrinology.2020;[Epub] CrossRef - Prediction of Relapse After Antithyroid Drugs Withdrawal: A Narrative Review
Pei-Wen Wang
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Radioiodine-131 therapy (RIT) in benign thyroid diseases: Personalized prescription based on objectives with optional use of pharmacological modulators
J. Clerc
Médecine Nucléaire.2020; 44(4): 250. CrossRef - Predicting the Risk of Graves Disease Relapse: Commentary on “Thyroid Peroxidase Antibody Positivity is Associated with Relapse-Free Survival Following Antithyroid Drug Treatment for Graves Disease”
D. Gallo, M.L. Tanda, E. Piantanida
Endocrine Practice.2020; 26(9): 1039. CrossRef - Integrating Five Feature Types Extracted From Ultrasonograms to Improve the Prediction of Thyroid Papillary Carcinoma
Renxiang Zhu, Zhongyu Wang, Yifan Zhang, Bingxin Yu, Mingran Qi, Xin Feng, Chenjun Wu, Yuxuan Cui, Lan Huang, Fan Li, Fengfeng Zhou
IEEE Access.2019; 7: 101820. CrossRef - Serum TSH Receptor Antibodies Fall Gradually and Only Rarely Switch Functional Activity in Treated Graves’ Disease
Mary H. Samuels
Clinical Thyroidology.2019; 31(8): 330. CrossRef - Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinology and Metabolism.2019; 34(3): 268. CrossRef - A transgenic mouse that spontaneously develops pathogenic TSH receptor antibodies will facilitate study of antigen-specific immunotherapy for human Graves’ disease
Sandra M. McLachlan, Basil Rapoport
Endocrine.2019; 66(2): 137. CrossRef
- Multifunctional nanoparticle-mediated combining therapy for human diseases

- Thyroid
- Prevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
- Hyemi Kwon, Jin-hyung Jung, Kyung-Do Han, Yong-Gyu Park, Jung-Hwan Cho, Da Young Lee, Ji Min Han, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2018;33(2):260-267. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.260
- 6,408 View
- 128 Download
- 37 Web of Science
- 37 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background The incidence of thyroid nodules has increased worldwide in recent years. Thyroid dysfunction is a potential risk factor for hypercholesterolemia, cardiovascular disease, osteoporosis, arrhythmia, and neuropsychiatric disease. This study investigated the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism in Koreans.
Methods In this nationwide population-based cohort study, 51,834,660 subjects were included using the National Health Information database from 2006 to 2015, after the exclusion of subjects with thyroid cancer.
Results The prevalence in Korea in 2015 of thyroid nodules, hypothyroidism in patients taking thyroid hormone, and hyperthyroidism in patients undergoing treatment was 15.82/1,000 population, 15.94/1,000 population, and 2.76/1,000 population, respectively. All these diseases were more prevalent among women than among men. The number of incident cases of these three thyroid diseases steadily increased from 2006 to 2012, and then decreased through 2015. The incidence of thyroid nodules, hypothyroidism treated with thyroid hormone, and treated hyperthyroidism was 6.79/1,000 population, 1.76/1,000 population, and 0.55/1,000 population, respectively, in Korea in 2015. The use of methimazole continuously increased, from 33% of total antithyroid drug prescriptions in 2006 to 74.4% in 2015, and it became the most frequently prescribed antithyroid drug in Korea. In contrast, the use of propylthiouracil continuously decreased.
Conclusion This was the first nationwide study of the prevalence and annual incidence of thyroid nodules, hypothyroidism, and hyperthyroidism to take into account recent changes and to include the current status of patients receiving treatment.
-
Citations
Citations to this article as recorded by- New-onset atrial fibrillation in seropositive rheumatoid arthritis: association with disease-modifying anti-rheumatic drugs treatment
Hyung Woo Kim, Minkyung Han, Inkyung Jung, Sung Soo Ahn
Rheumatology.2024; 63(3): 630. CrossRef - Nonalcoholic Fatty Liver Disease and the Risk of Thyroid Cancer Among Young Adults in South Korea
Hyemi Kwon, Kyung-Do Han, Sun Joon Moon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1095. CrossRef - Endocrine and metabolic comorbidities in primary cicatricial alopecia: A nationwide population‐based study
Da‐Ae Yu, Seong Rae Kim, Soo Ick Cho, Ohsang Kwon
The Journal of Dermatology.2024; 51(3): 429. CrossRef - Risk of non-thyroidal autoimmune diseases in patients with Graves’ disease: a nationwide retrospective cohort study
Seo Young Sohn, Jiyeon Ahn, Min Kyung Lee, Jae Hyuk Lee, Ji-Won Kwon, Ji-Min Kweon, Ju-Yeun Lee
Rheumatology.2024;[Epub] CrossRef - Cancer Risk in Graves Disease with Radioactive131I Treatment: A Nationwide Cohort Study
Kyeong Jin Kim, Jimi Choi, Kyoung Jin Kim, Eyun Song, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim
Journal of Nuclear Medicine.2024; : jnumed.123.266531. CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - Myotonic dystrophy type 1 in South Korea: a comprehensive analysis of cancer and comorbidity risks
Incheol Seo, Jin-Mo Park
Neurological Sciences.2024;[Epub] CrossRef - Association of ITM2A rs1751094 polymorphism on X chromosome in Korean pediatric patients with autoimmune thyroid disease
Won K. Cho, In‐Cheol Baek, Sung E. Kim, Mirae Kim, Tai‐Gyu Kim, Byung‐Kyu Suh
Immunity, Inflammation and Disease.2023;[Epub] CrossRef - Preoperative Risk Stratification of Follicular-patterned Thyroid Lesions on Core Needle Biopsy by Histologic Subtyping and RAS Variant-specific Immunohistochemistry
Meejeong Kim, Sora Jeon, Chan Kwon Jung
Endocrine Pathology.2023; 34(2): 247. CrossRef - Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Acromegaly and the long-term fracture risk of the vertebra and hip: a national cohort study
Hyemi Kwon, Kyung-Do Han, Bong-Sung Kim, Sun Joon Moon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Osteoporosis International.2023; 34(9): 1591. CrossRef - Association of Thyroid Hormone Medication Adherence With Risk of Dementia
Saemi Han, Seogsong Jeong, Seulggie Choi, Sun Jae Park, Kyae Hyung Kim, Gyeongsil Lee, Yoosun Cho, Joung Sik Son, Sang Min Park
The Journal of Clinical Endocrinology & Metabolism.2023; 109(1): e225. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Comprehensive analysis of chemokine gene polymorphisms in Korean children with autoimmune thyroid disease
Chungwoo Shin, In-Cheol Baek, Won Kyoung Cho, Tai-Gyu Kim, Byung-Kyu Suh
Scientific Reports.2023;[Epub] CrossRef - Analysis of the status of treatment of benign thyroid diseases — a public health problem aggravated in the COVID-19 pandemic era
Giulianno Molina Melo, Antonio José Gonçalves, Fernando Walder, Carolina Ferraz, Murilo Catafesta Neves, Marcio Abrahão, Onivaldo Cervantes
Brazilian Journal of Otorhinolaryngology.2022; 88(6): 982. CrossRef - Graves’ disease and the risk of Parkinson’s disease: a Korean population-based study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Jinyoung Youn, Ji Oh Mok, Chul-Hee Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Brain Communications.2022;[Epub] CrossRef - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Endocrinology and Metabolism.2022; 37(2): 281. CrossRef - Incidence of hypothyroidism after treatment for breast cancer: A Korean population-based study
Jongmoo Park, Choongrak Kim, Yongkan Ki, Wontaek Kim, Jiho Nam, Donghyun Kim, Dahl Park, Hosang Jeon, Dong Woon Kim, Ji Hyeon Joo, Claudio Andaloro
PLOS ONE.2022; 17(6): e0269893. CrossRef - Genome-wide association study of hyperthyroidism based on electronic medical record from Taiwan
Ting-Yuan Liu, Wen-Ling Liao, Tzu-Yuan Wang, Chia-Jung Chan, Jan-Gowth Chang, Yu-Chia Chen, Hsing-Fang Lu, Hsien-Hui Yang, Shih-Yin Chen, Fuu-Jen Tsai
Frontiers in Medicine.2022;[Epub] CrossRef - Graves’ disease, its treatments, and the risk of atrial fibrillation: A Korean population-based study
Yoon Young Cho, Bongseong Kim, Dughyun Choi, Chul-Hee Kim, Dong Wook Shin, Jee Soo Kim, Seung-Jung Park, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Risk of autoimmune diseases in recurrent aphthous ulcer patients: A nationwide population study
Young Chan Lee, Su Jin Jeong, Young‐Gyu Eun, Ran Song, In‐Hwan Oh
Oral Diseases.2021; 27(6): 1443. CrossRef - Hyperthyroidism Prevalence in China After Universal Salt Iodization
Chuyuan Wang, Yongze Li, Di Teng, Xiaoguang Shi, Jianming Ba, Bing Chen, Jianling Du, Lanjie He, Xiaoyang Lai, Yanbo Li, Haiyi Chi, Eryuan Liao, Chao Liu, Libin Liu, Guijun Qin, Yingfen Qin, Huibiao Quan, Bingyin Shi, Hui Sun, Xulei Tang, Nanwei Tong, Gui
Frontiers in Endocrinology.2021;[Epub] CrossRef - Comorbidity network analysis related to obesity in middle-aged and older adults: findings from Korean population-based survey data
Hye Ah Lee, Hyesook Park
Epidemiology and Health.2021; 43: e2021018. CrossRef - Prevalence of Hyperthyroidism and Hypothyroidism and its Correlation with Serum Antithyroglobulin among patients in Kirkuk-Iraq
Sabah Mohammed Salih, Wijdan Abdullameer Kamel, Mohammed Talat Abbas, Kasim Sakran Abass
Journal Of Advanced Pharmacy Education And Research.2021; 11(2): 57. CrossRef - A nationwide study of patients with monoclonal gammopathy of undetermined significance with a 10-year follow-up in South Korea
Ka-Won Kang, Ji Eun Song, Byung-Hyun Lee, Min Ji Jeon, Eun Sang Yu, Dae Sik Kim, Se Ryeon Lee, Hwa Jung Sung, Chul Won Choi, Yong Park, Byung Soo Kim
Scientific Reports.2021;[Epub] CrossRef - Incidence and Mortality of Myocardial Infarction and Stroke in Patients with Hyperthyroidism: A Nationwide Cohort Study in Korea
Hyun Jung Kim, Taeuk Kang, Min Ji Kang, Hyeong Sik Ahn, Seo Young Sohn
Thyroid.2020; 30(7): 955. CrossRef - Vitamin D supplementation does not prevent the recurrence of Graves’ disease
Yoon Young Cho, Yun Jae Chung
Scientific Reports.2020;[Epub] CrossRef - Binding and Activity of Tetrabromobisphenol A Mono-Ether Structural Analogs to Thyroid Hormone Transport Proteins and Receptors
Xiao-Min Ren, Linlin Yao, Qiao Xue, Jianbo Shi, Qinghua Zhang, Pu Wang, Jianjie Fu, Aiqian Zhang, Guangbo Qu, Guibin Jiang
Environmental Health Perspectives.2020;[Epub] CrossRef - Epidemiology of metabolic syndrome and its components in Chinese patients with a range of thyroid-stimulating hormone concentrations
Kun Tang, Qiao Zhang, Nian-chun Peng, Miao Zhang, Shu-jing Xu, Hong Li, Ying Hu, Chun-ju Xue, Li-xin Shi
Journal of International Medical Research.2020; 48(11): 030006052096687. CrossRef - The Association of Overt and Subclinical Hyperthyroidism with the Risk of Cardiovascular Events and Cardiovascular Mortality: Meta-Analysis and Systematic Review of Cohort Studies
Seo Young Sohn, Eunyoung Lee, Min Kyung Lee, Jae Hyuk Lee
Endocrinology and Metabolism.2020; 35(4): 786. CrossRef - Prevalence of Thyroid Disease in Patients Surgically Treated for Pituitary Disease
Kim, Cho, Ku, Jung, Moon, Kim, Shin, Kim, Lee
Journal of Clinical Medicine.2019; 8(8): 1142. CrossRef - Association of Thyroid-Stimulating Hormone and Thyroid Hormones with Cardiometabolic Risk Factors in Euthyroid Children and Adolescents Aged 10–18 Years: A Population-Based Study
Cheol Gyu Ma, Young Suk Shim
Scientific Reports.2019;[Epub] CrossRef - Weight change is significantly associated with risk of thyroid cancer: A nationwide population-based cohort study
Hyemi Kwon, Kyung-Do Han, Cheol-Young Park
Scientific Reports.2019;[Epub] CrossRef - Evaluation of the relationship of subclinical hypothyroidism with metabolic syndrome and its components in adolescents: a population-based study
Min-Kyung Lee, Yoo Mee Kim, Seo-Young Sohn, Jae-Hyuk Lee, Young Jun Won, Se Hwa Kim
Endocrine.2019; 65(3): 608. CrossRef - Autoimmune thyroiditis and central serous chorioretinopathy may have a relation
Brijesh Takkar, Harsha Saxena, Anubha Rathi, Rekha Singh
Medical Hypotheses.2018; 121: 180. CrossRef
- New-onset atrial fibrillation in seropositive rheumatoid arthritis: association with disease-modifying anti-rheumatic drugs treatment

- Thyroid
- Validity and Reliability of the Korean Version of the Hyperthyroidism Symptom Scale
- Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
- Endocrinol Metab. 2018;33(1):70-78. Published online March 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.1.70
- 4,051 View
- 55 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Thyrotoxicosis is a common disease resulting from an excess of thyroid hormones, which affects many organ systems. The clinical symptoms and signs are relatively nonspecific and can vary depending on age, sex, comorbidities, and the duration and cause of the disease. Several symptom rating scales have been developed in an attempt to assess these symptoms objectively and have been applied to diagnosis or to evaluation of the response to treatment. The aim of this study was to assess the reliability and validity of the Korean version of the hyperthyroidism symptom scale (K-HSS).
Methods Twenty-eight thyrotoxic patients and 10 healthy subjects completed the K-HSS at baseline and after follow-up at Seoul National University Bundang Hospital. The correlation between K-HSS scores and thyroid function was analyzed. K-HSS scores were compared between baseline and follow-up in patient and control groups. Cronbach's α coefficient was calculated to demonstrate the internal consistency of K-HSS.
Results The mean age of the participants was 34.7±9.8 years and 13 (34.2%) were men. K-HSS scores demonstrated a significant positive correlation with serum free thyroxine concentration and decreased significantly with improved thyroid function. K-HSS scores were highest in subclinically thyrotoxic subjects, lower in patients who were euthyroid after treatment, and lowest in the control group at follow-up, but these differences were not significant. Cronbach's α coefficient for the K-HSS was 0.86.
Conclusion The K-HSS is a reliable and valid instrument for evaluating symptoms of thyrotoxicosis in Korean patients.
-
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Effect of increased levothyroxine dose on depressive mood in older adults undergoing thyroid hormone replacement therapy
Jae Hoon Moon, Ji Won Han, Tae Jung Oh, Sung Hee Choi, Soo Lim, Ki Woong Kim, Hak Chul Jang
Clinical Endocrinology.2020; 93(2): 196. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Thyroid Stimulating Hormone Reference Range and Prevalence of Thyroid Dysfunction in the Korean Population: Korea National Health and Nutrition Examination Survey 2013 to 2015
- Won Gu Kim, Won Bae Kim, Gyeongji Woo, Hyejin Kim, Yumi Cho, Tae Yong Kim, Sun Wook Kim, Myung-Hee Shin, Jin Woo Park, Hai-Lin Park, Kyungwon Oh, Jae Hoon Chung
- Endocrinol Metab. 2017;32(1):106-114. Published online January 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.106
- Correction in: Endocrinol Metab 2023;38(3):357
- 7,987 View
- 202 Download
- 73 Web of Science
- 79 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background No nationwide epidemiological study evaluating the prevalence of subclinical and overt forms of hypothyroidism and hyperthyroidism has yet been conducted in Korea. This study aimed to evaluate the reference range of serum thyroid stimulating hormone (TSH) and the national prevalence of thyroid dysfunctions in Korea.
Methods Nation-wide cross-sectional data were analyzed from a representative sample of the civilian, non-institutionalized Korean population (
n =6,564) who underwent blood testing for thyroid function and anti-thyroid peroxidase antibody (TPOAb) as part of the Korea National Health and Nutrition Examination Survey VI (2013 to 2015).Results The reference interval of serum TSH in the Korean reference population was 0.62 to 6.68 mIU/L. Based on this reference interval, the prevalence of overt and subclinical hypothyroidism was 0.73% (males 0.40%, females 1.10%) and 3.10% (males 2.26%, females 4.04%), respectively. The prevalence of hypothyroidism increased with age until the age group between 50 to 59 years. Positive TPOAb were found in 7.30% of subjects (males 4.33%, females 10.62%). The prevalence of overt and subclinical hypothyroidism TPOAb-positive subjects was 5.16% and 10.88%, respectively. The prevalence of overt and subclinical hyperthyroidism was 0.54% (males 0.30%, females 0.81%) and 2.98% (males 2.43%, females, 3.59%), respectively.
Conclusion The Serum TSH reference levels in the Korean population were higher than the corresponding levels in Western countries. Differences were found in the prevalence of hypothyroidism and hyperthyroidism according to age, sex, and TPOAb positivity. This study provides important baseline information for understanding patterns of thyroid dysfunction and diseases in Korea.
-
Citations
Citations to this article as recorded by- Deciphering the roles of triiodothyronine (T3) and thyroid-stimulating hormone (TSH) on cardiac electrical remodeling in clinical and experimental hypothyroidism
Oscar Casis, Leire Echeazarra, Beatriz Sáenz-Díez, Mónica Gallego
Journal of Physiology and Biochemistry.2024; 80(1): 1. CrossRef - The Impact of Physical Activity on Thyroid Health: Insights From Representative Data in Korea
Jeongmin Lee, Han-Sang Baek, Kwanhoon Jo, Min-Hee Kim, Jung Min Lee, Sang Ah Chang, Dong-Jun Lim
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Subclinical thyroid dysfunction and chronic kidney disease: a nationwide population-based study
Hye Jeong Kim, Sang Joon Park, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo
BMC Nephrology.2023;[Epub] CrossRef - Association between iodine intake and metabolic syndrome in euthyroid adult in an iodine-replete area: a nationwide population-based study
Hye Jeong Kim, Suyeon Park, Sang Joon Park, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo
Endocrine Journal.2023; 70(4): 393. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Subclinical Hypothyroidism
Hyun Kyung Chung, Eu Jeong Ku, Won Sang Yoo, Yea Eun Kang, Kyeong Jin Kim, Bo Hyun Kim, Tae-Yong Kim, Young Joo Park, Chang Ho Ahn, Jee Hee Yoon, Eun Kyung Lee, Jong Min Lee, Eui Dal Jung, Jae Hoon Chung, Yun Jae Chung, Won Bae Kim, Ka Hee Yi, Ho-Cheol Ka
International Journal of Thyroidology.2023; 16(1): 32. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2023; 38(4): 381. CrossRef - Association between shift work and the risk of hypothyroidism in adult male workers in Korea: a cohort study
Seonghyeon Kwon, Yesung Lee, Eunhye Seo, Daehoon Kim, Jaehong Lee, Youshik Jeong, Jihoon Kim, Jinsook Jeong, Woncheol Lee
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef - Depressão e hipotireoidismo: Uma revisão sistemática
Eduarda Silva Souza, Rosangela Soares Chriguer, Maria Cristina Mazzaia
Revista Portuguesa de Investigação Comportamental e Social.2023;[Epub] CrossRef - Comparison of Thyroid-Stimulating Hormone Results from Eight Different Reagents and Assay-Specific Korean Reference Interval for Subclinical Hypothyroidism Treatment
Won Sang Yoo, Sollip Kim, Young Joo Park, Sang Hoon Song, Kyunghoon Lee, Eun Kyung Lee, Jehoon Lee, Ho-Young Lee, Yun Jae Chung, Hyun Kyung Chung, Jin Chul Paeng, Minje Han, Ho-Cheol Kang
International Journal of Thyroidology.2023; 16(2): 166. CrossRef - Comparison of Five Different Criteria for Diagnosis of Subclinical Hypothyroidism in a Large-Scale Chinese Population
Yan-song Zheng, Sheng-yong Dong, Yan Gong, Jia-hong Wang, Fei Wang, Qiang Zeng
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association of thyroid autoimmunity with nonalcoholic fatty liver disease in euthyroid middle‐aged subjects: A population‐based study
Hye Jeong Kim, Sang Joon Park, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo
Journal of Gastroenterology and Hepatology.2022; 37(8): 1617. CrossRef - Heart Failure and Stroke Risks in Users of Liothyronine With or Without Levothyroxine Compared with Levothyroxine Alone: A Propensity Score-Matched Analysis
Wook Yi, Bo Hyun Kim, Mijin Kim, Jinmi Kim, Myungsoo Im, Soree Ryang, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
Thyroid.2022; 32(7): 764. CrossRef - Association of free thyroxine with obstructive lung pattern in euthyroid middle-aged subjects: A population-based study
Hye Jeong Kim, Sang Joon Park, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh, Myung Hi Yoo, Dong Keon Yon
PLOS ONE.2022; 17(7): e0270126. CrossRef - Long working hours and the risk of hypothyroidism in healthy Korean workers: a cohort study
Yesung Lee, Woncheol Lee, Hyoung-Ryoul Kim
Epidemiology and Health.2022; 44: e2022104. CrossRef - Association of breastfeeding with thyroid function and autoimmunity in postmenopausal women
Sung-Woo Kim, Ji-Hyun Lee, Ho-Sang Shon, Eonju Jeon, Tae-Yong Kim
Endocrine.2021; 71(1): 130. CrossRef - Distributions of serum thyroid-stimulating hormone in 2020 thyroid disease-free adults from areas with different iodine levels: a cross-sectional survey in China
B. Ren, S. Wan, L. Liu, M. Qu, H. Wu, H. Shen
Journal of Endocrinological Investigation.2021; 44(5): 1001. CrossRef - Low Thyroid-stimulating Hormone Levels Are Associated With Annoying Tinnitus in Adult Women: Korea National Health and Nutrition Examination Surveys
So Young Kim, Chanyang Min, Hyung-Jong Kim, Hyo Geun Choi
Otology & Neurotology.2021; 42(4): e408. CrossRef - Risk of All-Cause Mortality in Levothyroxine-Treated Hypothyroid Patients: A Nationwide Korean Cohort Study
Seo Young Sohn, Gi Hyeon Seo, Jae Hoon Chung
Frontiers in Endocrinology.2021;[Epub] CrossRef - Decreased Expression of Ileal Thyroid Hormone Transporters in a Hypothyroid Patient: A Case Report
Chae Won Chung, Eun Young Mo, Gyung Seo Jung, Yoo Hyung Kim, Sun Wook Cho, Do Joon Park, Jeong Mo Bae, Young Joo Park
Frontiers in Endocrinology.2021;[Epub] CrossRef - Korea National Health and Nutrition Examination Survey, 20th anniversary: accomplishments and future directions
Kyungwon Oh, Yoonjung Kim, Sanghui Kweon, Soyeon Kim, Sungha Yun, Suyeon Park, Yeon-Kyeng Lee, Youngtaek Kim, Ok Park, Eun Kyeong Jeong
Epidemiology and Health.2021; 43: e2021025. CrossRef - Association between triglyceride-glucose index and thyroid function in euthyroid adults: The Korea National Health and Nutritional Examination Survey 2015
Wonsuk Choi, Ji Yong Park, A. Ram Hong, Jee Hee Yoon, Hee Kyung Kim, Ho-Cheol Kang, Sun Young Lee
PLOS ONE.2021; 16(7): e0254630. CrossRef - Association between Subclinical Hypothyroidism and Incident Hypertension in Women: A Systematic Review and Meta-Analysis
Jean Kim, Narut Prasitlumkum, Sandeep Randhawa, Dipanjan Banerjee
Journal of Clinical Medicine.2021; 10(15): 3318. CrossRef - Sex Difference in the Association between Sleep Duration and Thyroid Disease among South Korean Adults
Jeong Hyun Ahn, Jin Young Nam, Soojin Park
Journal of Health Informatics and Statistics.2021; 46(3): 337. CrossRef - The Association between the Dietary Inflammatory Index and Thyroid Function in U.S. Adult Males
Nuozhou Liu, Fang Ma, Ying Feng, Xue Ma
Nutrients.2021; 13(10): 3330. CrossRef - T4+T3 Combination Therapy: An Unsolved Problem of Increasing Magnitude and Complexity
Wilmar M. Wiersinga
Endocrinology and Metabolism.2021; 36(5): 938. CrossRef - Association between thyroid hormones and insulin resistance indices based on the Korean National Health and Nutrition Examination Survey
Yun Mi Choi, Min Kyung Kim, Mi Kyung Kwak, Dooman Kim, Eun-Gyoung Hong
Scientific Reports.2021;[Epub] CrossRef - Implication of thyroid function in periodontitis: a nationwide population-based study
Eyun Song, Min Jeong Park, Jung A. Kim, Eun Roh, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Scientific Reports.2021;[Epub] CrossRef - Association between thyroid hormone and components of metabolic syndrome in euthyroid Korean adults
Kyung A. Shin, Eun Jae Kim
Medicine.2021; 100(51): e28409. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study
Mijin Kim, Bo Hyun Kim, Hyungi Lee, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
Endocrinology and Metabolism.2020; 35(1): 106. CrossRef - Unmet Clinical Needs in the Treatment of Patients with Thyroid Cancer
Won Bae Kim, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong
Endocrinology and Metabolism.2020; 35(1): 14. CrossRef - Long Work Hours Are Associated with Hypothyroidism: A Cross-Sectional Study with Population-Representative Data
Young Ki Lee, Dong-eun Lee, Yul Hwangbo, You Jin Lee, Hyeon Chang Kim, Eun Kyung Lee
Thyroid.2020; 30(10): 1432. CrossRef - Subclinical thyroid dysfunction, bone mineral density, and osteoporosis in a middle-aged Korean population
K. Lee, S. Lim, H. Park, H.Y. Woo, Y. Chang, E. Sung, H.S. Jung, K.E. Yun, C.W. Kim, S. Ryu, M.J. Kwon
Osteoporosis International.2020; 31(3): 547. CrossRef - Update on Thyroid Hormone Levels and Thyroid Dysfunction in the Korean Population Based on Data from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
Jae Hoon Chung
Endocrinology and Metabolism.2020; 35(1): 7. CrossRef - Assessment of the relationship between knee ultrasound and clinical symptoms in patients with thyroid dysfunction
Bo Young Kim, Sung-Soo Kim, Hyeong Kyu Park, Hyun-Sook Kim
Journal of International Medical Research.2020; 48(1): 030006051989770. CrossRef - Association between urinary sodium levels and iodine status in Korea
Jonghwa Ahn, Jang Ho Lee, Jiwoo Lee, Ji Yeon Baek, Eyun Song, Hye-Seon Oh, Mijin Kim, Suyeon Park, Min Ji Jeon, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
The Korean Journal of Internal Medicine.2020; 35(2): 392. CrossRef - Association of Thyroid Status with Health-Related Quality of Life in Korean Older Adults
Minjung Han, Seulggie Choi, Sarang Kim, Ahryoung Ko, Joung Sik Son, Sang Min Park
Korean Journal of Family Medicine.2020; 41(1): 38. CrossRef - High neutrophil-to-lymphocyte ratio is associated with relapse in Graves’ disease after antithyroid drug therapy
Mijin Kim, Bo Hyun Kim, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
Endocrine.2020; 67(2): 406. CrossRef - Sex differences in subclinical hypothyroidism and associations with metabolic risk factors: a health examination-based study in mainland China
Li Jiang, Jinman Du, Weizhu Wu, Jianjiang Fang, Jufang Wang, Jinhua Ding
BMC Endocrine Disorders.2020;[Epub] CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2020; 35(3): 669. CrossRef - Urinary Iodine Concentration and Thyroid Peroxidase Antibodies in the Korean Population Using Korea National Health and Nutrition Examination Survey VI
Myung-Chul Chang
International Journal of Thyroidology.2020; 13(2): 155. CrossRef - Recent Issues Related to Thyroid Disease in Pregnancy
Jae Hoon Chung
International Journal of Thyroidology.2020; 13(2): 85. CrossRef - Epidemiology of thyroid disorders in the Lifelines Cohort Study (the Netherlands)
Hanneke J. C. M. Wouters, Sandra N. Slagter, Anneke C. Muller Kobold, Melanie M. van der Klauw, Bruce H. R. Wolffenbuttel, Silvia Naitza
PLOS ONE.2020; 15(11): e0242795. CrossRef - Hipertiroidi Hastalarında Tedavi Öncesi ve Sonrası Trombosit/Lenfosit ve Nötrofil/Lenfosit Oranlarının Değerlendirilmesi
Çiğdem CİNDOĞLU, Mehmet GÜLER, Mehmet Ali EREN, Tevfik SABUNCU
Harran Üniversitesi Tıp Fakültesi Dergisi.2020; 17(1): 104. CrossRef - Association between Sleep Duration and Subclinical Thyroid Dysfunction Based on Nationally Representative Data
Woojun Kim, Jeongmin Lee, Jeonghoon Ha, Kwanghoon Jo, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Moo-Il Kang, Min-Hee Kim
Journal of Clinical Medicine.2019; 8(11): 2010. CrossRef - High Normal Range of Free Thyroxine is Associated with Decreased Triglycerides and with Increased High-Density Lipoprotein Cholesterol Based on Population Representative Data
Jeongmin Lee, Jeonghoon Ha, Kwanhoon Jo, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Moo-Il Kang, Min-Hee Kim
Journal of Clinical Medicine.2019; 8(6): 758. CrossRef - Association High-Iodine-Containing Seaweed Soup Consumption after Birth and Subclinical Hypothyroidism in Korean Women: Korea National Health and Nutrition Examination Survey IV (2013–2015)
Hyunsam Kim, Ha Ni Lee, Jeonghoon Ha
International Journal of Thyroidology.2019; 12(2): 105. CrossRef - Reference Range and Sociodemographic Characteristics of TSH among Reproductive Age Women in Rural China
Qiang Su, Shikun Zhang, Mei Hu, Qiaomei Wang, Na Liu, Haiping Shen, Yiping Zhang, Man Zhang
Biological Trace Element Research.2019; 189(2): 336. CrossRef - Prevalence of Thyroid Disease in Patients Surgically Treated for Pituitary Disease
Kim, Cho, Ku, Jung, Moon, Kim, Shin, Kim, Lee
Journal of Clinical Medicine.2019; 8(8): 1142. CrossRef - Thyroid Dysfunction in Patients with Antineutrophil Cytoplasmic Antibody–associated Vasculitis: A Monocentric Retrospective Study
JAE YEON KIM, YONG-BEOM PARK, SANG-WON LEE
The Journal of Rheumatology.2019; 46(9): 1248. CrossRef - Thyroid dysfunction in patients with suspected or documented supraventricular tachyarrhythmia
Hye Bin Gwag, Ji Eun Jun, Youngjun Park, Seong Soo Lee, Seung-Jung Park, June Soo Kim, Kyoung-Min Park, Young Keun On
International Journal of Arrhythmia.2019;[Epub] CrossRef - Association between Iodine Nutrition Status and Thyroid Disease-Related Hormone in Korean Adults: Korean National Health and Nutrition Examination Survey VI (2013–2015)
Kim, Kwon, Kim, Hong, Park
Nutrients.2019; 11(11): 2757. CrossRef - Thyroid-stimulating hormone levels in the normal range and incident type 2 diabetes mellitus
T. I. de Vries, L. J. Kappelle, Y. van der Graaf, H. W. de Valk, G. J. de Borst, H. M. Nathoe, F. L. J. Visseren, Jan Westerink
Acta Diabetologica.2019; 56(4): 431. CrossRef - The Association between Low Vitamin D Status and Autoimmune Thyroid Disease in Korean Premenopausal Women: The 6th Korea National Health and Nutrition Examination Survey, 2013–2014
Choon-Young Kim, Yeon Ji Lee, Ji-Ho Choi, Soo Yeon Lee, Hye Young Lee, Da Hye Jeong, Yeon Jun Choi
Korean Journal of Family Medicine.2019; 40(5): 323. CrossRef - Associations between urine iodine and allergic diseases in the Korean National Health and Nutrition Examination Survey 2013–2015: A STROBE-compliant article
Young Bok Lee, Ji hyun Lee, Min Ji Kang, Dong Soo Yu, Kyung Do Han, Yong Gyu Park
Phytomedicine.2019; 62: 152937. CrossRef - The Relationship between Thyroid Function and Different Obesity Phenotypes in Korean Euthyroid Adults
Jeong Mi Kim, Bo Hyun Kim, Hyungi Lee, Eun Heui Kim, Mijin Kim, Jong Ho Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim, Yong Ki Kim
Diabetes & Metabolism Journal.2019; 43(6): 867. CrossRef - Sex-Dependent Association between Weight Change and Thyroid Dysfunction: Population-Level Analysis Using the Korean National Health and Nutrition Examination Survey
Eyun Song, Jonghwa Ahn, Hye-Seon Oh, Min Ji Jeon, Won Gu Kim, Won Bae Kim, Young Kee Shong, Tae Yong Kim
European Thyroid Journal.2019; 8(4): 202. CrossRef - Subclinical Hypothyroidism: is it Really Subclinical with Aging?
Robin Gourmelon, Sandrine Donadio-Andréi, Karim Chikh, Muriel Rabilloud, Elisabetta Kuczewski, Anne-Sophie Gauchez, Anne Charrié, Pierre-Yves Brard, Raphaëlle Andréani, Jean-Cyril Bourre, Christine Waterlot, Domitille Guédel, Anne Mayer, Emmanuel Disse, C
Aging and disease.2019; 10(3): 520. CrossRef - Serum thyroid‐stimulating hormone levels and smoking status: Data from the Korean National Health and Nutrition Examination Survey VI
Suyeon Park, Won Gu Kim, Min Ji Jeon, Mijin Kim, Hye‐Seon Oh, Minkyu Han, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Clinical Endocrinology.2018; 88(6): 969. CrossRef - Sex-specific genetic influence on thyroid-stimulating hormone and free thyroxine levels, and interactions between measurements: KNHANES 2013–2015
Young Ki Lee, Dong Yeob Shin, Hyejung Shin, Eun Jig Lee, Silvia Naitza
PLOS ONE.2018; 13(11): e0207446. CrossRef - Ten Years of the Korean Thyroid Association: Achievement and Future
Young Joo Park, Young Shin Song, Ka Hee Yi
International Journal of Thyroidology.2018; 11(1): 1. CrossRef - Association between diffuse lymphocytic infiltration and papillary thyroid cancer aggressiveness according to the presence of thyroid peroxidase antibody and BRAFV600E mutation
Young Ki Lee, Kyeong Hye Park, Se Hee Park, Kwang Joon Kim, Dong Yeob Shin, Kee Hyun Nam, Woong Youn Chung, Eun Jig Lee
Head & Neck.2018; 40(10): 2271. CrossRef - Prevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
Hyemi Kwon, Jin-hyung Jung, Kyung-Do Han, Yong-Gyu Park, Jung-Hwan Cho, Da Young Lee, Ji Min Han, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 260. CrossRef - Evaluation of Thyroid Hormone Levels and Urinary Iodine Concentrations in Koreans Based on the Data from Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
Jae Hoon Chung
Endocrinology and Metabolism.2018; 33(2): 160. CrossRef - Thyroid-Stimulating Hormone Reference Ranges in the First Trimester of Pregnancy in an Iodine-Sufficient Country
Carmen Castillo, Nicole Lustig, Paula Margozzini, Andrea Gomez, María Paulina Rojas, Santiago Muzzo, Lorena Mosso
Endocrinology and Metabolism.2018; 33(4): 466. CrossRef - Male-specific association between subclinical hypothyroidism and the risk of non-alcoholic fatty liver disease estimated by hepatic steatosis index: Korea National Health and Nutrition Examination Survey 2013 to 2015
Jeongmin Lee, Jeonghoon Ha, Kwanhoon Jo, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Moo-Il Kang, Bong-Yun Cha, Min-Hee Kim
Scientific Reports.2018;[Epub] CrossRef - Sex differences in risk factors for subclinical hypothyroidism
Jeonghoon Ha, Jeongmin Lee, Kwanhoon Jo, Dong-Jun Lim, Moo Il Kang, Bong Yun Cha, Min-Hee Kim
Endocrine Connections.2018; 7(4): 511. CrossRef - Associations of Urinary Cotinine-Verified Active and Passive Smoking with Thyroid Function: Analysis of Population-Based Nationally Representative Data
Jihun Kang, Eunhee Kong, Jongsoon Choi
Thyroid.2018; 28(5): 583. CrossRef - Establishment of Korean Thyroid Association-10 Years of Development in Internal Medicine
Jae Hoon Chung
International Journal of Thyroidology.2018; 11(1): 7. CrossRef - Association between subclinical thyroid dysfunction and depressive symptoms in the Korean adult population: The 2014 Korea National Health and Nutrition Examination Survey
Jae Won Hong, Jung Hyun Noh, Dong-Jun Kim, Osama Ali Abulseoud
PLOS ONE.2018; 13(8): e0202258. CrossRef - Association Between Thyroid Dysfunction and Lipid Profiles Differs According to Age and Sex: Results from the Korean National Health and Nutrition Examination Survey
Hye-Seon Oh, Hyemi Kwon, Jonghwa Ahn, Eyun Song, Suyeon Park, Mijin Kim, Minkyu Han, Min Ji Jeon, Won Gu Kim, Won Bae Kim, Young Kee Shong, Eun-Jung Rhee, Tae Yong Kim
Thyroid.2018; 28(7): 849. CrossRef - The Relationship between Subclinical Thyroid Disease and Cardiovascular Disease Risk Score in Koreans
Hee Joong Lim, Seong Hee Ahn, Seongbin Hong, Young Ju Suh
Journal of Korean Medical Science.2017; 32(10): 1626. CrossRef - Changes in standardized mortality rates from thyroid cancer in Korea between 1985 and 2015: Analysis of Korean national data
Yun Mi Choi, Won Gu Kim, Hyemi Kwon, Min Ji Jeon, Minkyu Han, Tae Yong Kim, Young Kee Shong, Sang Mo Hong, Eun‐Gyoung Hong, Won Bae Kim
Cancer.2017; 123(24): 4808. CrossRef - Response: Thyroid Stimulating Hormone Reference Range and Prevalence of Thyroid Dysfunction in the Korean Population: Korea National Health and Nutrition Examination Survey 2013 to 2015 (Endocrinol Metab 2017;32:106-14, Won Gu Kim et al.)
Won Gu Kim, Jae Hoon Chung
Endocrinology and Metabolism.2017; 32(2): 304. CrossRef - Excessive Iodine Intake and Thyrotropin Reference Interval: Data from the Korean National Health and Nutrition Examination Survey
Min Ji Jeon, Won Gu Kim, Hyemi Kwon, Mijin Kim, Suyeon Park, Hye-Seon Oh, Minkyu Han, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(7): 967. CrossRef - Subclinical thyroid dysfunction and risk of carotid atherosclerosis
Hosu Kim, Tae Hyuk Kim, Hye In Kim, So Young Park, Young Nam Kim, Seonwoo Kim, Min-Ji Kim, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim, Moon-Kyu Lee, Yong-Ki Min, Jae Hoon Chung, Mira Kang, Sun Wook Kim, Tatsuo Shimosawa
PLOS ONE.2017; 12(7): e0182090. CrossRef - Letter: Thyroid Stimulating Hormone Reference Range and Prevalence of Thyroid Dysfunction in the Korean Population: Korea National Health and Nutrition Examination Survey 2013 to 2015 (Endocrinol Metab 2017;32:106-14, Won Gu Kim et al.)
Young Ki Lee, Dong Yeob Shin
Endocrinology and Metabolism.2017; 32(2): 302. CrossRef - Vitamin D deficiency affects thyroid autoimmunity and dysfunction in iodine-replete area: Korea national health and nutrition examination survey
Mijin Kim, Eyun Song, Hye-Seon Oh, Suyeon Park, Hyemi Kwon, Min Ji Jeon, Won Gu Kim, Won Bae Kim, Young Kee Shong, Tae Yong Kim
Endocrine.2017; 58(2): 332. CrossRef - Viral Hepatitis in South Korea
Stella C Pak, Yaseen Alastal, Zubair Khan, Umar Darr
Euroasian Journal of Hepato-Gastroenterology.2017; 7(2): 163. CrossRef
- Deciphering the roles of triiodothyronine (T3) and thyroid-stimulating hormone (TSH) on cardiac electrical remodeling in clinical and experimental hypothyroidism


 KES
KES

 First
First Prev
Prev



