Search
- Page Path
- HOME > Search
Original Articles
- Thyroid
- Evaluation of Iodine Status among Korean Patients with Papillary Thyroid Cancer Using Dietary and Urinary Iodine
- Ji Yeon Choi, Joon-Hyop Lee, YoonJu Song
- Endocrinol Metab. 2021;36(3):607-618. Published online June 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1005
- 3,927 View
- 122 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Concerns have been raised regarding thyroid disorders caused by excessive iodine in Koreans, who have iodine-rich diets. This study evaluated iodine status using dietary iodine intake and urinary iodine in papillary thyroid cancer (PTC) patients.
Methods
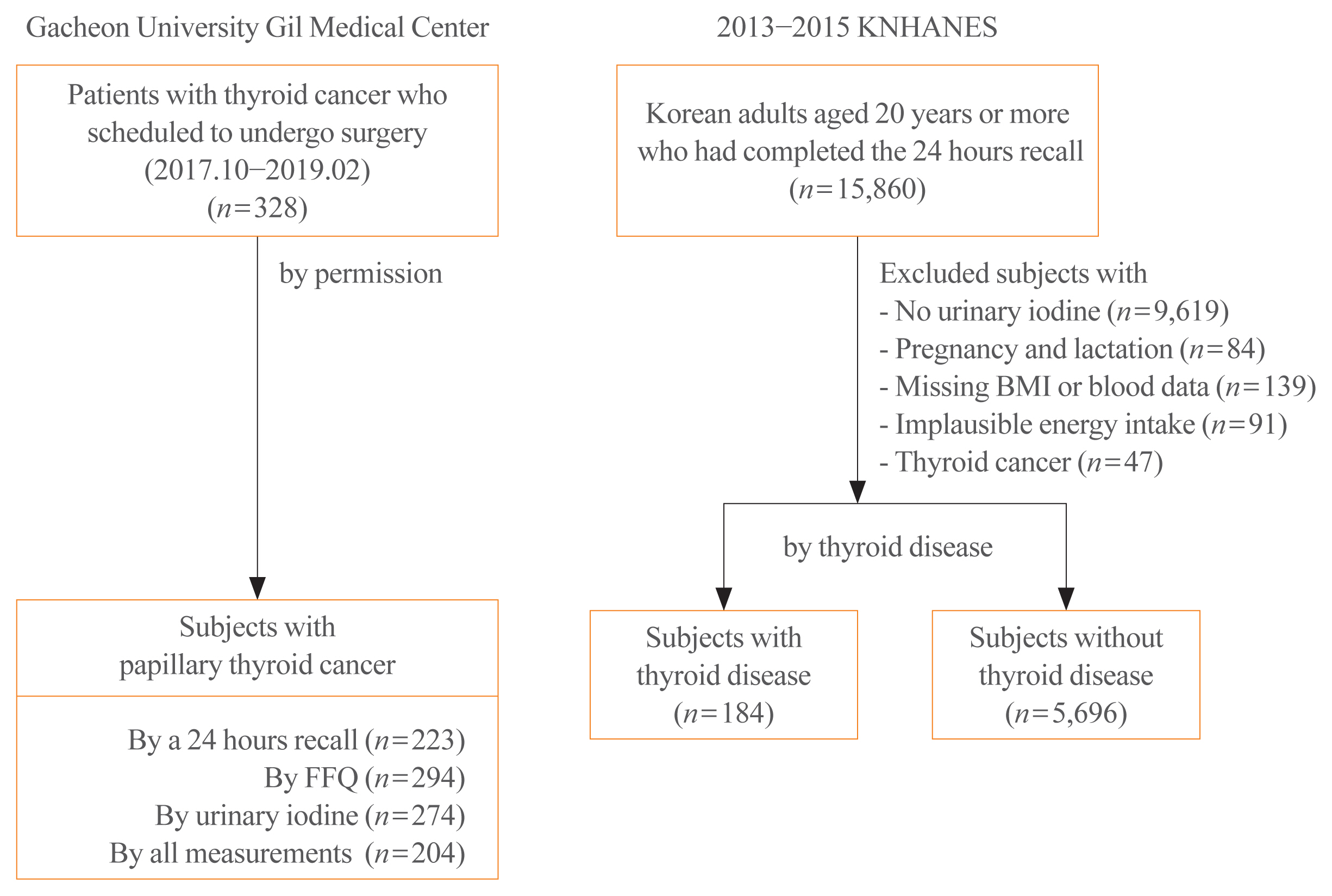
Dietary data of PTC patients were assessed using a 24-hour recall and food frequency questionnaire (FFQ), and urinary iodine concentrations (UICs) were also obtained. To compare the iodine status of PTC patients, Korean adults with or without thyroid disease from the Korea National Health and Nutrition Examination Survey, which had 24-hour recall data and urinary iodine measurements, were analyzed.
Results
The median daily iodine intake by 24-hour recall was 341.7 μg/day in PTC patients, similar to the levels of other Korean adults. Based on UICs, the prevalence of excessive iodine was 54.4% in PTC patients, which was similar to the prevalence among subjects with thyroid disease (55.4%) but slightly higher than that in subjects without thyroid disease (47.7%). Based on dietary iodine by 24-hour recall, the prevalence of excessive iodine intake was 7.2%, which was higher than that among subjects with (4.4%) or without (3.9%) thyroid disease. The dietary iodine intake based on 24-hour recall was closely correlated with the UIC (r=0.4826) in PTC patients, but dietary iodine by FFQ was not significantly correlated with either 24-hour recall or UIC-based dietary iodine.
Conclusion
Excessive iodine intake was more common in PTC patients than in subjects without thyroid disease. Further longitudinal research is necessary to elucidate the role of dietary iodine in PTC. -
Citations
Citations to this article as recorded by- Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma
Hengqiang Zhao, Jin Hu, Le Cui, Yiping Gong, Tao Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effect of iodine restriction on short-term changes in thyroid function in patients with subclinical hypothyroidism
Obin Kwon, Dong Yeob Shin, Eun Jig Lee
Journal of Nutrition and Health.2022; 55(2): 250. CrossRef - Iodine nutrition and papillary thyroid cancer
Xueqi Zhang, Fan Zhang, Qiuxian Li, Chuyao Feng, Weiping Teng
Frontiers in Nutrition.2022;[Epub] CrossRef
- Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma

- Clinical Report of Effects of Pre and Post-partum Thyroiditis (PPT).
- Yong Wook Cho, Myung Seo Kang, Young Soo Cha, Jin Hwan Kook, Yoo Ri Kim, Pil Won Park, Wee Hyun Lee, Jung Eun Lim, Yo Won Cho
- J Korean Endocr Soc. 1997;12(4):541-549. Published online January 1, 2001
- 975 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Excessive iodine intake increases the occurrence of autoimmune thyroid disorders by enhancing immunogenecity of iodine-rich thyroglobulin, In Korea, most of postpartum women take a large amount of iodine-rich seaweed. Although the excessive iodine intake may affect the thyroid function, only a few reports were available concering iodine intake, especially on postpartum period. METHODS: A prospective study was undertaken in 146 of normal delivered postpartum women. Dietary intake and urinary excretion of iodine, serum T3, T4, TSH, anti-TPO Ab and anti-Tg Ab were measured before and 1, 6, 12 and 24 weeks after delivery. Iodine intake was analyzed by one-to-one interview using 24hr recall and food frequency questionnaire. RESULTS: 1. PPT was occurred in 6 (10.3%) postparturn women, It presented as hypothyroidism alone in 1 (16.7%), transient thyrotoxicosis followed by hypothyroidisrn in 3 (50.0%), and thyrotoxicosis alone in 2 (33.3%) of the follwed-up patients. 2. During pregnancy, no difference was found in age, serum T3, T4 and TSH between PPT and normal thyroid function group. 3. In PPT group, anti-TPO and anti-Tg Ab were significantly higher than those of normal thyroid function group during pregnancy, and their sensitivity for PPT was 40% and 33%, respectively. But there was no correlation between dietary iodine intake and the titer of thyroid auto-antibodies. 4. There was no correlation between pre and post-partum dietary iodine intake and occurrence of PPT. CONCLUSION: In Korea, the incidence of PPT was slightly higher than other nations. The sensitivity of thyroid auto-antibodies was too low to use for prediction of PPT. Pre and post-partum iodine intake had no effect on the occurrence of PPT and post-partum thyroid function.


 KES
KES

 First
First Prev
Prev



