Search
- Page Path
- HOME > Search
- Thyroid
- Diagnosis and Management of Thyroid Disease during Pregnancy and Postpartum: 2023 Revised Korean Thyroid Association Guidelines
- Hwa Young Ahn, Ka Hee Yi
- Endocrinol Metab. 2023;38(3):289-294. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1696
- 6,618 View
- 714 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
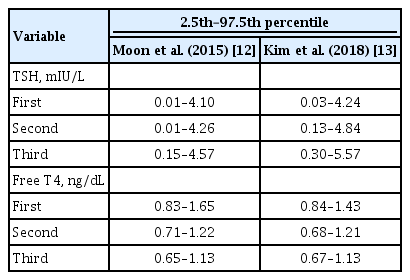
ePub - Thyroid hormone plays a critical role in fetal growth and development, and thyroid dysfunction during pregnancy is associated with several adverse outcomes, such as miscarriage and preterm birth. In this review, we introduce and explain three major changes in the revised Korean Thyroid Association (KTA) guidelines for the diagnosis and management of thyroid disease during pregnancy: first, the normal range of thyroid-stimulating hormone (TSH) during pregnancy; second, the treatment of subclinical hypothyroidism; and third, the management of euthyroid pregnant women with positive thyroid autoantibodies. The revised KTA guidelines adopt 4.0 mIU/L as the upper limit of TSH in the first trimester. A TSH level between 4.0 and 10.0 mIU/L, combined with free thyroxine (T4) within the normal range, is defined as subclinical hypothyroidism, and a TSH level over 10 mIU/L is defined as overt hypothyroidism regardless of the free T4 level. Levothyroxine treatment is recommended when the TSH level is higher than 4 mIU/L in subclinical hypothyroidism, regardless of thyroid peroxidase antibody positivity. However, thyroid hormone therapy to prevent miscarriage is not recommended in thyroid autoantibody-positive women with normal thyroid function.
-
Citations
Citations to this article as recorded by- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2023; 38(4): 381. CrossRef - Maternal isolated hypothyroxinemia in the first trimester is not associated with adverse pregnancy outcomes, except for macrosomia: a prospective cohort study in China
Jing Du, Linong Ji, Xiaomei Zhang, Ning Yuan, Jianbin Sun, Dan Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia

- Miscellaneous
- Clinical Characteristics, Management, and Potential Biomarkers of Endocrine Dysfunction Induced by Immune Checkpoint Inhibitors
- Shintaro Iwama, Tomoko Kobayashi, Hiroshi Arima
- Endocrinol Metab. 2021;36(2):312-321. Published online April 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1007
- 5,536 View
- 268 Download
- 15 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
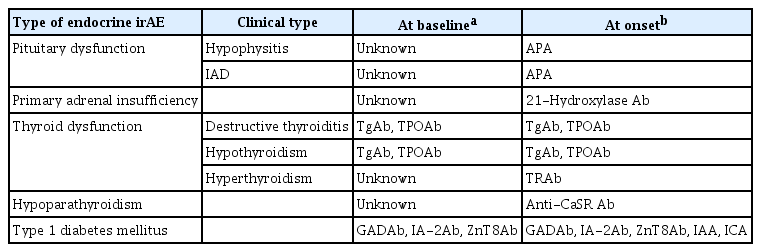
ePub - Immune-related adverse events (irAEs) affecting the endocrine glands are among the most frequent irAEs induced by immune checkpoint inhibitors (ICIs) and include hypopituitarism, primary adrenal insufficiency, thyrotoxicosis, hypothyroidism, hypoparathyroidism, and type 1 diabetes mellitus. Since the incidence and clinical features of endocrine irAEs vary according to the ICI used, it is important to understand the characteristics of these irAEs and to manage each one appropriately. Since some endocrine irAEs, including adrenal crisis and diabetic ketoacidosis, are potentially life-threatening, predicting the risk of endocrine irAEs before their onset is critical. Several autoantibodies have been detected in patients who develop endocrine irAEs, among which anti-thyroid antibodies may be predictive biomarkers of thyroid dysfunction. In this review, we describe the clinical features of each endocrine irAE induced by ICIs and discuss their potential biomarkers, including autoantibodies.
-
Citations
Citations to this article as recorded by- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events
Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima
Endocrine Journal.2024; 71(1): 23. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - Endocrinopathies Associated With Immune Checkpoint Inhibitor Use
Anupam Kotwal, Randol Kennedy, Nupur Kikani, Sonali Thosani, Whitney Goldner, Afreen Shariff
Endocrine Practice.2024;[Epub] CrossRef - Recovery from insulin dependence in immune checkpoint inhibitor‐associated diabetes mellitus: A case report
Marie Okubo, Yuji Hataya, Kanta Fujimoto, Toshio Iwakura, Naoki Matsuoka
Journal of Diabetes Investigation.2023; 14(1): 147. CrossRef - Case Report: A Rising Cause of New-Onset Endocrinopathies After Immunotherapy
Charity Tan, Sarah Hendricks, Kristina Hernandez, Martha Benavides, Rupinderjit Samra
The Journal for Nurse Practitioners.2023; 19(5): 104582. CrossRef - Risk of Thyroid Dysfunction in PD-1 Blockade Is Stratified by the Pattern of TgAb and TPOAb Positivity at Baseline
Xin Zhou, Shintaro Iwama, Tomoko Kobayashi, Masahiko Ando, Hiroshi Arima
The Journal of Clinical Endocrinology & Metabolism.2023; 108(10): e1056. CrossRef - Severe thyrotoxicosis induced by tislelizumab: a case report and literature review
Liman Huo, Chao Wang, Haixia Ding, Xuelian Shi, Bin Shan, Ruoying Zhou, Ping Liang, Juan Hou
Frontiers in Oncology.2023;[Epub] CrossRef - Life-Threatening Endocrinological Immune-Related Adverse Events of Immune Checkpoint Inhibitor Therapy
Aleksandra Basek, Grzegorz K. Jakubiak, Grzegorz Cieślar, Agata Stanek
Cancers.2023; 15(24): 5786. CrossRef - Increased Risk of Thyroid Dysfunction by PD-1 and CTLA-4 Blockade in Patients Without Thyroid Autoantibodies at Baseline
Shintaro Iwama, Tomoko Kobayashi, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Masahiko Ando, Xin Zhou, Ayana Yamagami, Takeshi Onoue, Yohei Kawaguchi, Takashi Miyata, Mariko Sugiyama, Hiroshi Takagi, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tets
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): e1620. CrossRef - Biomarkers and risk factors for the early prediction of immune-related adverse events: a review
Ying Zhang, Xiaoling Zhang, Weiling Li, Yunyi Du, Wenqing Hu, Jun Zhao
Human Vaccines & Immunotherapeutics.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors as a Threat to the Hypothalamus–Pituitary Axis: A Completed Puzzle
Agnese Barnabei, Andrea Corsello, Rosa Maria Paragliola, Giovanni Maria Iannantuono, Luca Falzone, Salvatore Maria Corsello, Francesco Torino
Cancers.2022; 14(4): 1057. CrossRef - Elevated TSH Level, TgAb, and Prior Use of Ramucirumab or TKIs as Risk Factors for Thyroid Dysfunction in PD-L1 Blockade
Tomoko Kobayashi, Shintaro Iwama, Ayana Yamagami, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Xin Zhou, Masahiko Ando, Takeshi Onoue, Takashi Miyata, Mariko Sugiyama, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tetsunari Hase, Masahiro Morise, Taka
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4115. CrossRef - Preconditioning of the immune system modulates the response of papillary thyroid cancer to immune checkpoint inhibitors
Fabiana Pani, Yoshinori Yasuda, Sylvie T Rousseau, Kevin C Bermea, Solmaz Roshanmehr, Rulin Wang, Srinivasan Yegnasubramanian, Patrizio Caturegli, Luigi Adamo
Journal for ImmunoTherapy of Cancer.2022; 10(12): e005538. CrossRef - Survival benefit of endocrine dysfunction following immune checkpoint inhibitors for nonthyroidal cancers
Anupam Kotwal, Mabel Ryder
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 517. CrossRef
- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events

- Clinical Study
- Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
- Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
- Endocrinol Metab. 2019;34(3):268-274. Published online September 26, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.3.268
- 6,881 View
- 130 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Graves' disease (GD) is an autoimmune thyroid disorder caused by antibodies stimulating the thyrotropin (TSH) receptor. TSH receptor antibody (TRAb) measurement is useful for predicting GD relapse after antithyroid drug (ATD) treatment. However, the association of other thyroid autoantibodies with GD relapse remains obscure.
Methods This retrospective study enrolled patients with GD who were initially treated with ATD. TRAb, thyroid peroxidase antibody (TPOAb), and thyroglobulin antibody (TgAb) were measured at the initial diagnosis and at the time of ATD discontinuation.
Results A total of 55 patients were enrolled. The mean age was 49.7 years, and 39 patients (70.9%) were female. Antibody positivity at diagnosis was 90.9%, 69.1%, and 61.9% for TRAb, TPOAb, TgAb, respectively. Median ATD treatment period was 15.1 months. At the time of ATD withdrawal, TRAb titers decreased uniformly overall. Conversely, TPOAb and TgAb showed various changes. After withdrawal of ATD, 19 patients (34.5%) experienced relapse. No clinical features or laboratory results were significantly related to relapse in the overall patient group. However, in the TPOAb positive group at diagnosis, increasing titer of TPOAb or TgAb after ATD treatment was significantly and independently related to relapse free survival (TPOAb: hazard ratio [HR], 17.99; 95% confidence interval [CI], 1.66 to 195.43;
P =0.02) (TgAb: HR, 5.73; 95% CI, 1.21 to 27.26;P =0.03).Conclusion Changes in TPOAb or TgAb titers during treatment might be useful for predicting relapse after ATD treatment in patients with positive TPOAb at diagnosis.
-
Citations
Citations to this article as recorded by- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Clinical significance of thyroglobulin antibodies and thyroid peroxidase antibodies in Graves’ disease: a cross-sectional study
Masahito Katahira, Taku Tsunekawa, Akira Mizoguchi, Mariko Yamaguchi, Kahori Tsuru, Hiromi Takashima, Ryoma Terada
Hormones.2023; 22(2): 253. CrossRef - The Clinical Implications of Anti-thyroid Peroxidase Antibodies in Graves’ Disease in Basrah
Emad S Alhubaish, Nassar T Alibrahim, Abbas A Mansour
Cureus.2023;[Epub] CrossRef - Influence of Thyroid Peroxidase Antibodies Serum Levels in Graves' Disease: A Retrospective Cohort Study
Maria L Guia Lopes, Carlos Tavares Bello, José P Cidade, Clotilde Limbert, Joao Sequeira Duarte
Cureus.2023;[Epub] CrossRef - Interpretation of Thyroid Autoantibodies in Hyperthyroidism
Han-Sang Baek, Dong-Jun Lim
The Korean Journal of Medicine.2023; 98(3): 132. CrossRef - Usefulness of Real-Time Quantitative Microvascular Ultrasonography for Differentiation of Graves’ Disease from Destructive Thyroiditis in Thyrotoxic Patients
Han-Sang Baek, Ji-Yeon Park, Chai-Ho Jeong, Jeonghoon Ha, Moo Il Kang, Dong-Jun Lim
Endocrinology and Metabolism.2022; 37(2): 323. CrossRef - Differential Diagnosis of Thyrotoxicosis by Machine Learning Models with Laboratory Findings
Jinyoung Kim, Han-Sang Baek, Jeonghoon Ha, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Dong-Jun Lim, Ki-Hyun Baek
Diagnostics.2022; 12(6): 1468. CrossRef - The relationship between atherosclerotic disease and relapse during ATD treatment
Xinxin Zhu, Yaguang Zhang, Xiaoyu Zhao, Xiaona Zhang, Zixuan Ru, Yanmeizhi Wu, Xu Yang, Boyu Hou, Hong Qiao
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Programmed Cell Death-Ligand 1 (PD-L1) gene Single Nucleotide Polymorphism in Graves’ Disease and Hashimoto’s Thyroiditis in Korean Patients
Jee Hee Yoon, Min-ho Shin, Hee Nam Kim, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2021; 36(3): 599. CrossRef - Low frequency of IL-10-producing B cells and high density of ILC2s contribute to the pathological process in Graves’ disease, which may be related to elevated-TRAb levels
Xiaoyun Ji, Jie Wan, Rong Chen, Huixuan Wang, Lan Huang, Shwngjun Wang, Zhaoliang Su, Huaxi Xu
Autoimmunity.2020; 53(2): 78. CrossRef - Implication of VDR rs7975232 and FCGR2A rs1801274 gene polymorphisms in the risk and the prognosis of
autoimmune thyroid diseases in the Tunisian population
S Mestiri, I Zaaber, I Nasr, H Marmouch
Balkan Journal of Medical Genetics.2020; 23(1): 69. CrossRef - Thyroid Peroxidase Antibody Positivity is Associated With Relapse-Free Survival Following Antithyroid Drug Treatment for Graves Disease
Christopher A. Muir, Graham R.D. Jones, Jerry R. Greenfield, Andrew Weissberger, Katherine Samaras
Endocrine Practice.2020; 26(9): 1026. CrossRef - Predicting the Risk of Graves Disease Relapse: Commentary on “Thyroid Peroxidase Antibody Positivity is Associated with Relapse-Free Survival Following Antithyroid Drug Treatment for Graves Disease”
D. Gallo, M.L. Tanda, E. Piantanida
Endocrine Practice.2020; 26(9): 1039. CrossRef
- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study

- Diabetes
- Latent Autoimmune Diabetes in Adults: Current Status and New Horizons
- Paolo Pozzilli, Silvia Pieralice
- Endocrinol Metab. 2018;33(2):147-159. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.147
- 14,031 View
- 371 Download
- 52 Web of Science
- 46 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Autoimmune diabetes is a heterogeneous disease which can arise at any age. Subjects with adult-onset autoimmune diabetes who do not necessitate insulin-therapy for at least 6 months after diagnosis are demarcated as having latent autoimmune diabetes in adults (LADA). This condition is more heterogeneous than young-onset autoimmune diabetes and shares clinical and metabolic characteristics with both type 2 and type 1 diabetes. Patients with LADA are considered by having highly variable β-cell destruction, different degrees of insulin resistance and heterogeneous titre and pattern of islet autoantibody, suggesting different pathophysiological pathways partially explaining the heterogeneous phenotypes of LADA. To date the heterogeneity of LADA does not allow to establish
a priori treatment algorithm and no specific guidelines for LADA therapy are available. These subjects are mostly treated as affected by type 2 diabetes, a factor that might lead to the progression to insulin-dependency quickly. A personalised medicine approach is necessary to attain optimal metabolic control and preserve β-cell function to decrease the risk of long-term diabetes complications. Recent data concerning the use of oral antidiabetic agents as dipeptidyl peptidase 4 inhibitors and glucagon-like peptide 1 receptor agonists indicate up-and-coming results in term of protect C-peptide levels and improving glycaemic control. This review summarises current knowledge on LADA, emphasising controversies regarding its pathophysiology and clinical features. Moreover, we discuss data available about novel therapeutic approaches that can be considered for prevention of β-cell loss in LADA.-
Citations
Citations to this article as recorded by- Utility of Fasting C-Peptide for the Diagnostic Differentiation of Patients with Type 1, Type 2 Diabetes, MODY, and LADA
Ricardo Alemán-Contreras, Rita A. Gómez-Díaz, Maura E. Noyola-García, Rafael Mondragón-González, Niels Wacher, Aldo Ferreira-Hermosillo
Life.2024; 14(5): 550. CrossRef - Drug candidates and potential targets of Curculigo spp. compounds for treating diabetes mellitus based on network pharmacology, molecular docking and molecular dynamics simulation
Abdul Halim Umar, Diah Ratnadewi, Mohamad Rafi, Yohana Caecilia Sulistyaningsih, Hamim Hamim, Wisnu Ananta Kusuma
Journal of Biomolecular Structure and Dynamics.2023; 41(17): 8544. CrossRef - Development and validation of a clinical score for identifying patients with high risk of latent autoimmune adult diabetes (LADA): The LADA primary care-protocol study
Pilar Vich-Pérez, Juan Carlos Abánades-Herranz, Gustavo Mora-Navarro, Ángela María Carrasco-Sayalero, Miguel Ángel Salinero-Fort, Ignacio Sevilla-Machuca, Mar Sanz-Pascual, Cristina Álvarez Hernández-Cañizares, Carmen de Burgos-Lunar, Vijayaprakash Suppia
PLOS ONE.2023; 18(2): e0281657. CrossRef - Diagnostic Dilemmas and Current Treatment Approaches in Latent Onset
Autoimmune Diabetes in Adults: A Concise Review
Lakshmi Chandran, Ankul Singh S., Chitra Vellapandian
Current Diabetes Reviews.2023;[Epub] CrossRef - Characteristics of adult-onset auto-immune type 1 diabetes
Faten Hadj Kacem, Ameni Jerbi, Bibi Twaheerah Allymamod, Wafa Bel Abed, Mouna Mnif, Nadia Charfi, Mouna Elleuch, Nabila Rekik, Hatem Masmoudi, Mohamed Abid
The American Journal of the Medical Sciences.2023; 366(1): 49. CrossRef - The role of cholecalciferol deficiency in the development of latent autoimmune diabetes in adults
I.O. Tsaryk, N.V. Pashkovska
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2023; 19(4): 259. CrossRef - Newly diagnosed type 1 diabetes mellitus in a human immunodeficiency virus-infected patient with antiretroviral therapy-induced immune reconstitution inflammatory syndrome: a case report
Min-ChunYeh, Han-Chuan Chuang, Shuen-Fu Weng, Chung-Huei Hsu, Chen-Ling Huang, Yu-Pei Lin, Yan-Yu Lin, Yu-Shan Hsieh
BMC Infectious Diseases.2023;[Epub] CrossRef - A Review on Latent Autoimmune Diabetes in Adults
Vijay Ravikumar, Ariba Ahmed, Ashish Anjankar
Cureus.2023;[Epub] CrossRef - Exploring Immune Therapies in a Twin Case of Latent Autoimmune Diabetes in Adults and Generalized Granuloma Annulare
Brian W. Connor, Sarah E.B. Smith, Andrea Kalus
Clinical Diabetes.2023; 41(4): 583. CrossRef - Innate immunity in latent autoimmune diabetes in adults
Juan Huang, James Alexander Pearson, F. Susan Wong, Li Wen, Zhiguang Zhou
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Endocrine Manifestations and New Developments in Mitochondrial Disease
Yi Shiau Ng, Albert Zishen Lim, Grigorios Panagiotou, Doug M Turnbull, Mark Walker
Endocrine Reviews.2022; 43(3): 583. CrossRef - Two Fifth-Generation Fighter Pilots Discovered with Latent Autoimmune Diabetes
Joe X. Zhang, Jacob Berry, Nathan M. Kim, Justin J. Gray, Savannah Fotheringham, Tom J. Sauerwein
Aerospace Medicine and Human Performance.2022; 93(2): 106. CrossRef - A Case of Late Diagnosis of Latent Autoimmune Diabetes in Adults
Joana R Costa, Ana Mestre, Mariana S Miranda, Frederica H Ferreira, Yahia Abuowda
Cureus.2022;[Epub] CrossRef - Class I MHC Polymorphisms Associated with Type 2 Diabetes in the Mexican Population
Paola Mendoza-Ramírez, Mildred Alejandra López-Olaiz, Adriana Lizeth Morales-Fernández, María Isabel Flores-Echiveste, Antonio de Jesus Casillas-Navarro, Marco Andrés Pérez-Rodríguez, Felipe de Jesús Orozco-Luna, Celso Cortés-Romero, Laura Yareni Zuñiga,
Genes.2022; 13(5): 772. CrossRef - Efficacy and safety of sitagliptin and insulin for latent autoimmune diabetes in adults: A systematic review and meta‐analysis
Tong Lin, Yinhe Cai, Liting Tang, Youwei Lian, Min Liu, Chaonan Liu
Journal of Diabetes Investigation.2022; 13(9): 1506. CrossRef - Partial Remission of Diabetes in a Young Adult While Testing Positive for Several Islet Cell Autoantibodies: A Case Report, Literature Review, and Patient Perspective
Samson O Oyibo
Cureus.2022;[Epub] CrossRef - Latent Autoimmune Diabetes in Adults and Metabolic Syndrome—A Mini Review
Niansi Pan, Shimei Yang, Xiaohong Niu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Prevalence and factors associated with latent autoimmune diabetes in adults (LADA): a cross-sectional study
Anselmo M. Manisha, Aminiel R. Shangali, Sayoki G. Mfinanga, Erasto V. Mbugi
BMC Endocrine Disorders.2022;[Epub] CrossRef - Diabetic ketoacidosis as first presentation of latent autoimmune diabetes in adults in a patient with hashitoxicosis as first presentation of Hashimoto’s thyroiditis: a case report
Maria Xenou, Ioannis Zoupas, Dimitrios Lygnos, Evangelos Fousteris
Journal of Medical Case Reports.2022;[Epub] CrossRef - Latent Autoimmune Diabetes in Adults (LADA): From Immunopathogenesis to Immunotherapy
Jingyi Hu, Rong Zhang, Hailan Zou, Lingxiang Xie, Zhiguang Zhou, Yang Xiao
Frontiers in Endocrinology.2022;[Epub] CrossRef - Adult-onset autoimmune diabetes
Raffaella Buzzetti, Ernesto Maddaloni, Jason Gaglia, R. David Leslie, F. Susan Wong, Bernhard O. Boehm
Nature Reviews Disease Primers.2022;[Epub] CrossRef - Diagnostic camouflage: A case report on Latent autoimmune diabetics of adulthood
Sandhya kiran Neupane, Prakash Paudel Jaishi, Divyaa Koirala, Arjun Kandel, Prabhat Kiran Neupane
Annals of Medicine and Surgery.2022; 82: 104699. CrossRef - A Mechanistic Insight on Phytoconstituents Delivering Hypoglycemic Activity: A Comprehensive Overview
Shraddha Singh Raghav, Bhavna Kumar, Neeraj Kumar Sethiya, Ankur Kaul
Future Pharmacology.2022; 2(4): 511. CrossRef - Diagnostic dilemmas in young onset diabetes mellitus
Avijit Saha, Parna Roy
Annals of Medical Science and Research.2022; 1(3): 111. CrossRef - Prevalence of diabetes-associated autoantibodies among patients presenting with type 2 diabetes and related metabolic differences
Fatemeh Moosaie, Neda Meftah, Niloofar Deravi, Kosar Abouhamzeh, Fatemeh Dehghani Firouzabadi, Pegah Khaloo, Mohammad Ali Mansournia, Seyede Marzie Fatemi Abhari, Manouchehr Nakhjavani, Alireza Esteghamati
Primary Care Diabetes.2021; 15(1): 169. CrossRef - The association of human leukocyte antigen class II (HLA II) haplotypes with the risk of Latent autoimmune diabetes of adults (LADA): Evidence based on available data
Wenjun Chen, Xinlin Chen, Minting Zhang, Zunnan Huang
Gene.2021; 767: 145177. CrossRef - A practical approach to the clinical challenges in initiation of basal insulin therapy in people with type 2 diabetes
Thomas Forst, Pratik Choudhary, Doron Schneider, Bruno Linetzky, Paolo Pozzilli
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Bewusstseinsstörung, Tachypnoe und Tachykardie bei einem 71-jährigen Patienten mit Diabetes mellitus Typ 2
S. Großmann, U. Hoffmann, C. Girlich
Der Internist.2021; 62(6): 672. CrossRef - Good Glycemic Outcomes Following Bariatric Surgery Among Patients With Type 2 Diabetes, Obesity, and Low-Titer GAD Antibodies
Ruveena Kaur, David Kim, Richard Cutfield, Michael Booth, Lindsay Plank, Rinki Murphy
Diabetes Care.2021; 44(2): 607. CrossRef - Slowly evolving, immune-mediated diabetes in 14-year-old patient: a case report
M. R. Ragimov, D. D. Omelchuk, L. I. Ibragimova, O. S. Derevyanko, T. V. Nikonova
Diabetes mellitus.2021; 24(1): 70. CrossRef - Combination of vitamin D and dipeptidyl peptidase-4 inhibitors (VIDPP-4i) as an immunomodulation therapy for autoimmune diabetes
Marcelo Maia Pinheiro, Felipe Moura Maia Pinheiro, Susana Nogueira Diniz, Andrea Fabbri, Marco Infante
International Immunopharmacology.2021; 95: 107518. CrossRef - Current view of diagnosis and treatment of latent autoimmune diabetes in adults
Jana Urbanová, Ludmila Brunerová, Jana Malinovská, Barbora Pelechová, Ludmila Koberová, Jan Brož
Vnitřní lékařství.2021; 67(2): 97. CrossRef - Alpha‐amylase as molecular target for treatment of diabetes mellitus: A comprehensive review
Navjot Kaur, Vanktesh Kumar, Surendra Kumar Nayak, Pankaj Wadhwa, Paranjit Kaur, Sanjeev Kumar Sahu
Chemical Biology & Drug Design.2021; 98(4): 539. CrossRef - CLINICAL AND IMMUNOLOGICAL ASPECTS OF VERIFICATION OF LATENT AUTOIMMUNE DIABETES IN ADULTS AT EARLY STAGES OF DISEASE MANIFESTATION
Tetiana М. Tykhonova, Igor V. Belozоrov, Nadiya Ye. Barabash, Larysa O. Martymianova
Wiadomości Lekarskie.2021; 74(7): 1707. CrossRef - Bacillus Calmette-Guerin 's beneficial impact on glucose metabolism: Evidence for broad based applications
Gabriella F. Shpilsky, Hiroyuki Takahashi, Anna Aristarkhova, Michele Weil, Nathan Ng, Kacie J. Nelson, Amanda Lee, Hui Zheng, Willem M. Kühtreiber, Denise L. Faustman
iScience.2021; 24(10): 103150. CrossRef - Multicentre analysis of hyperglycaemic hyperosmolar state and diabetic ketoacidosis in type 1 and type 2 diabetes
S. R. Tittel, K. M. Sondern, M. Weyer, T. Poeplau, B. M. Sauer, M. Schebek, K.-H. Ludwig, F. Hammer, E. Fröhlich-Reiterer, R. W. Holl
Acta Diabetologica.2020; 57(10): 1245. CrossRef - Pancreas Pathology of Latent Autoimmune Diabetes in Adults (LADA) in Patients and in a LADA Rat Model Compared With Type 1 Diabetes
Anne Jörns, Dirk Wedekind, Joachim Jähne, Sigurd Lenzen
Diabetes.2020; 69(4): 624. CrossRef - Past, present and future of latent autoimmune diabetes in adults
Bingwen Liu, Yufei Xiang, Zhenqi Liu, Zhiguang Zhou
Diabetes/Metabolism Research and Reviews.2020;[Epub] CrossRef - Adult-onset autoimmune diabetes in 2020: An update
Ernesto Maddaloni, Chiara Moretti, Carmen Mignogna, Raffaella Buzzetti
Maturitas.2020; 137: 37. CrossRef - Altered peripheral nerve structure and function in latent autoimmune diabetes in adults
Tushar Issar, Aimy Yan, Natalie C. G. Kwai, Ann M. Poynten, Adeniyi A. Borire, Ria Arnold, Arun V. Krishnan
Diabetes/Metabolism Research and Reviews.2020;[Epub] CrossRef - Low rate of latent autoimmune diabetes in adults (LADA) in patients followed for type 2 diabetes: A single center’s experience in Turkey
Abbas Ali Tam, Didem Ozdemir, Nagihan Bestepe, Fatma Dilek Dellal, Muhammet Cuneyt Bilginer, Sevgul Faki, Cemile Bicer, Reyhan Ersoy, Bekir Cakir
Archives of Endocrinology and Metabolism.2020;[Epub] CrossRef - Distinguishing between type 1 and type 2 diabetes
Alexandra E Butler, David Misselbrook
BMJ.2020; : m2998. CrossRef - Exogenous Insulin Injection-Induced Stiff-Person Syndrome in a Patient With Latent Autoimmune Diabetes: A Case Report and Literature Review
Yi-Yin Lee, Cheng-Wei Lin, I-Wen Chen
Frontiers in Endocrinology.2020;[Epub] CrossRef - Investigating optimal β‐cell‐preserving treatment in latent autoimmune diabetes in adults: Results from a 21‐month randomized trial
Ingrid K. Hals, Hanne Fiskvik Fleiner, Nina Reimers, Marianne C. Astor, Karin Filipsson, Zuheng Ma, Valdemar Grill, Anneli Björklund
Diabetes, Obesity and Metabolism.2019; 21(10): 2219. CrossRef - Immunological and clinical characteristics of latent autoimmune diabetes in the elderly
Silvina Yohena, Alberto Penas‐Steinhardt, Clara Muller, Natalia I. Faccinetti, Gloria E. Cerrone, Silvia Lovecchio, Edgardo Ridner, Silvina Valdez, Gustavo Frechtel
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - Autoimmunity in latent autoimmune diabetes in adults
Alessandro P. Delitala
AIMS Medical Science.2019; 6(2): 132. CrossRef
- Utility of Fasting C-Peptide for the Diagnostic Differentiation of Patients with Type 1, Type 2 Diabetes, MODY, and LADA


 KES
KES

 First
First Prev
Prev



