Search
- Page Path
- HOME > Search
- Adrenal Gland
- Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
- Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
- Endocrinol Metab. 2021;36(3):553-563. Published online June 1, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1008

- 3,674 View
- 142 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thermal ablation is a good alternative treatment in patients who are unable to undergo adrenalectomy. Even though the Asian Conference on Tumor Ablation (ACTA) has been held for many years, adrenal ablation guidelines have not been established. No guidelines for adrenal ablation are established in American and European countries, either. The aim of this review was to introduce the first version of ACTA guidelines for adrenal tumor ablation.
-
Citations
Citations to this article as recorded by- Treatment of primary aldosteronism: Clinical practice guidelines of the Taiwan Society of Aldosteronism
Chi-Shin Tseng, Chieh-Kai Chan, Hsiang-Ying Lee, Chien-Ting Pan, Kang-Yung Peng, Shuo-Meng Wang, Kuo-How Huang, Yao-Chou Tsai, Vin-Cent Wu, Jeff S. Chueh
Journal of the Formosan Medical Association.2024; 123: S125. CrossRef - Development and preclinical evaluation of multifunctional hydrogel for precise thermal protection during thermal ablation
Bowen Zheng, Peng Zhang, Qijun Lv, Tao Wu, Yadong Liu, Junjie Tang, Yanping Ma, Lili Cheng, Langtao Xu, Yizhen Wang, Yifan Xue, Jie Liu, Jie Ren
Bioactive Materials.2024; 31: 119. CrossRef - Case report of trans-renal ablation procedures for a recurrent pheochromocytoma in von Hippel-Lindau disease
Byung Kwan Park
Precision and Future Medicine.2023; 7(2): 90. CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef
- Treatment of primary aldosteronism: Clinical practice guidelines of the Taiwan Society of Aldosteronism

- Hypothalamus and Pituitary gland
- Best Achievements in Pituitary and Adrenal Diseases in 2020
- Chang Ho Ahn, Jung Hee Kim
- Endocrinol Metab. 2021;36(1):51-56. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2021.108
- 4,512 View
- 162 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
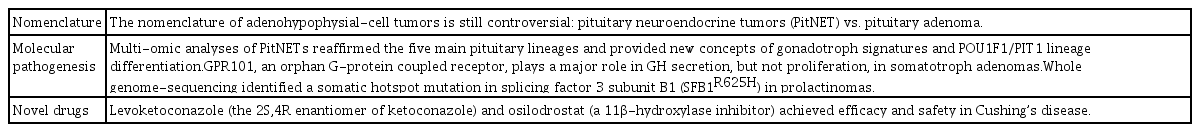
ePub - Significant progress in pituitary and adrenal diseases was made in 2020. This review presents major translational and clinical advances in research on pituitary and adrenal diseases, encompassing their epidemiology, pathogenesis, diagnosis, and clinical management. We address the controversy regarding the nomenclature of pituitary neuroendocrine tumors, omics-based molecular classification of pituitary adenomas, and novel drugs for Cushing’s disease in the field of pituitary diseases. In the field of adrenal diseases, we cover big data-driven epidemiology of adrenal tumors, steroid profiling as a new diagnostic tool, and the utility of scoring systems in the decision-making process of managing primary aldosteronism. This brief article will broaden readers’ understanding of pituitary and adrenal diseases.
-
Citations
Citations to this article as recorded by- Surgical management and outcomes of spinal metastasis of malignant adrenal tumor: A retrospective study of six cases and literature review
Xiangzhi Ni, Jing Wang, Jiashi Cao, Kun Zhang, Shuming Hou, Xing Huang, Yuanjin Song, Xin Gao, Jianru Xiao, Tielong Liu
Frontiers in Oncology.2023;[Epub] CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef
- Surgical management and outcomes of spinal metastasis of malignant adrenal tumor: A retrospective study of six cases and literature review

- Adrenal gland
- Minimally Invasive Adrenal Surgery
- JungHak Kwak, Kyu Eun Lee
- Endocrinol Metab. 2020;35(4):774-783. Published online December 23, 2020
- DOI: https://doi.org/10.3803/EnM.2020.404
- 5,089 View
- 155 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
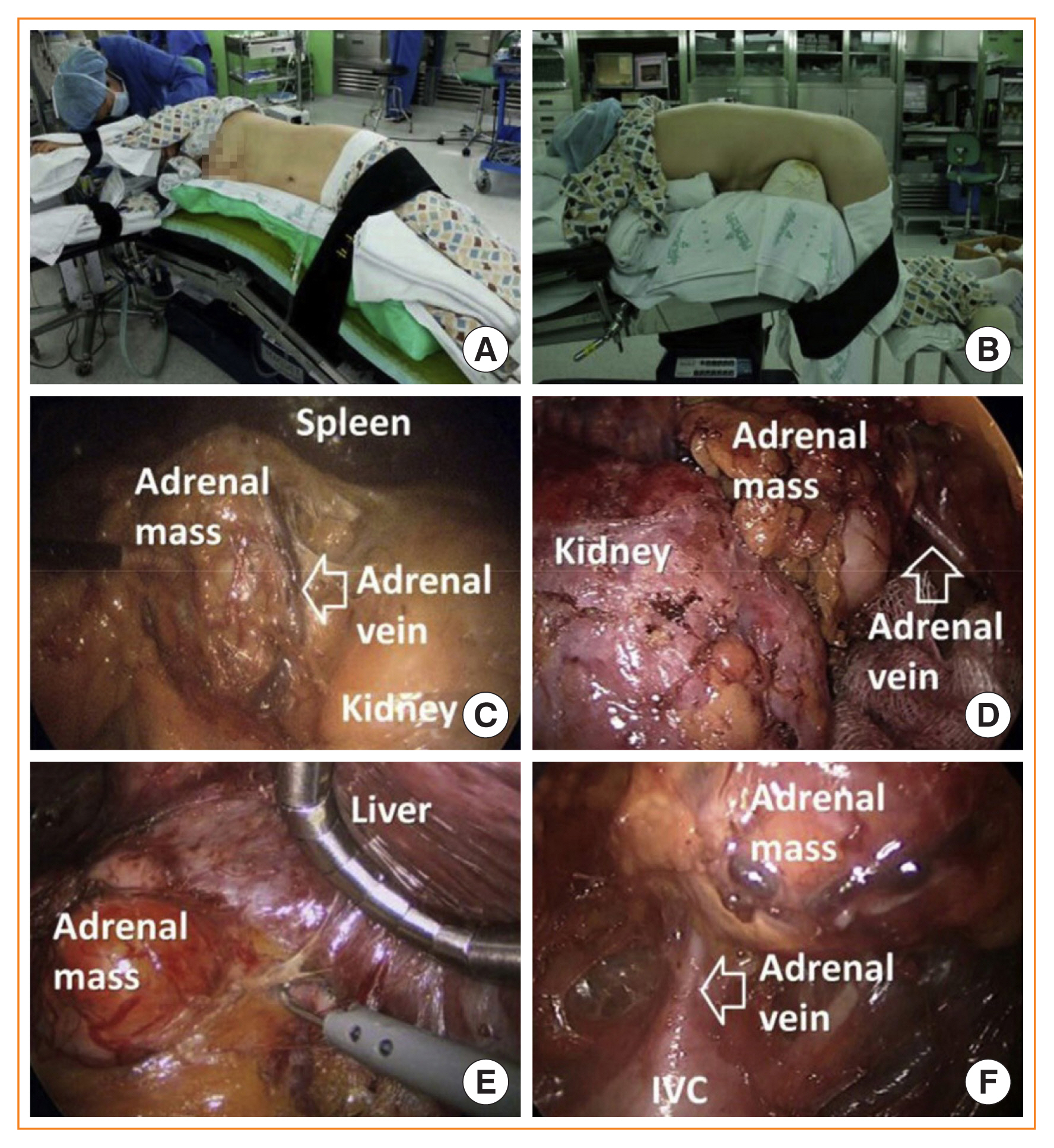
ePub - Since the introduction of minimally invasive surgery, laparoscopic adrenalectomy has become the main treatment option for adrenal masses. Various studies have reported that laparoscopic adrenalectomy showed fewer postoperative complications and faster recovery than conventional open adrenalectomy. Laparoscopic adrenalectomy can be performed through either the transperitoneal approach or the retroperitoneoscopic approach, which are widely used in most adrenal surgical procedures. Furthermore, with the development of minimally invasive surgery, organ-sparing adrenalectomy has recently emerged as a way to conserve functional adrenal gland tissue. According to recent data, organ-sparing adrenalectomy shows promising surgical, functional, and oncological outcomes including less intraoperative blood loss, maintenance of adrenal function, and low recurrence. Partial adrenalectomy was initially proposed for bilateral adrenal tumors in patients with hereditary disease to avoid chronic adrenal insufficiency. However, it has also gained popularity for the treatment of unilateral adrenal disease involving a small adrenal tumor because even patients with a unilateral adrenal gland may develop adrenal insufficiency in stressful situations. Therefore, partial adrenalectomy has become increasingly common to avoid lifelong steroid replacement and recurrence in most cases, especially in bilateral adrenal disease. This review article evaluates the current evidence on minimally invasive adrenalectomy and organ-preserving partial adrenalectomy.
-
Citations
Citations to this article as recorded by- Treating Primary Aldosteronism-Induced Hypertension: Novel Approaches and Future Outlooks
Nathan Mullen, James Curneen, Padraig T Donlon, Punit Prakash, Irina Bancos, Mark Gurnell, Michael C Dennedy
Endocrine Reviews.2024; 45(1): 125. CrossRef - Modified versus three-level technique of retroperitoneal laparoscopic adrenalectomy for all patients with adrenal lesions ≤ 6cm: a retrospective, case-controlled study
Minxiong Hu, Yangbiao Wu, Xiao Xu, Wenchao Cai, Jiangui Lin, Wanghai Cai, Honghong Pan, Zesong Yang, Liefu Ye, Jinfeng Wu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Ultrasound-guided Transversus Abdominis Plane Block is Effective as Laparoscopic Trocar site infiltration in Postoperative Pain Management in Patients Undergoing Adrenal Surgery
Giuseppe Cavallaro, Sergio Gazzanelli, Angelo Iossa, Francesco De Angelis, Alessia Fassari, Alessandra Micalizzi, Luigi Petramala, Daniele Crocetti, Francesco Circosta, Antonio Concistrè, Claudio Letizia, Giorgio De Toma, Andrea Polistena
The American Surgeon™.2023; 89(11): 4401. CrossRef - Outcome of Partial Adrenalectomy in MEN2 Syndrome: Personal Experience and Systematic Review of Literature
Priscilla Francesca Procopio, Francesco Pennestrì, Carmela De Crea, Nikolaos Voloudakis, Rocco Bellantone, Marco Raffaelli
Life.2023; 13(2): 425. CrossRef - Impact of Current Technology in Laparoscopic Adrenalectomy: 20 Years of Experience in the Treatment of 254 Consecutive Clinical Cases
Giovanni Conzo, Renato Patrone, Luigi Flagiello, Antonio Catauro, Alessandra Conzo, Chiara Cacciatore, Federico Maria Mongardini, Giovanni Cozzolino, Rosetta Esposito, Daniela Pasquali, Giuseppe Bellastella, Katherine Esposito, Ludovico Docimo
Journal of Clinical Medicine.2023; 12(13): 4384. CrossRef - Safety and effectiveness of minimally invasive adrenalectomy versus open adrenalectomy in patients with large adrenal tumors (≥5 cm): A meta-analysis and systematic review
Lijian Gan, Chunyang Meng, Kangsen Li, Lei peng, Jinze Li, Ji Wu, Yunxiang Li
International Journal of Surgery.2022; 104: 106779. CrossRef - Retroperitoneal laparoscopic partial adrenalectomy (RLPA) for 20-40 mm nonfunctional adrenal tumors in the day surgery mode
Xuwen Li, Haibo Xi, Yue Yu, Wei Liu, Xiaoping Zhu, Zhixian Gong, Bin Fu, Gongxian Wang, Xiaochen Zhou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Cirugía laparoscópica en incidentaloma suprarrenal para el cirujano general: serie de casos
Martín Adrián Bolívar-Rodríguez, Marcel Antonio Cázarez-Aguilar, Pedro Alejandro Magaña-Zavala, Francisco Magaña-Olivas, José Martín Niebla-Moreno
Revista Mexicana de Cirugía Endoscópica.2021; 22(1): 8. CrossRef
- Treating Primary Aldosteronism-Induced Hypertension: Novel Approaches and Future Outlooks

- Thyroid
- Percutaneous Adrenal Radiofrequency Ablation: A Short Review for Endocrinologists
- Byung Kwan Park
- Endocrinol Metab. 2020;35(4):750-755. Published online December 2, 2020
- DOI: https://doi.org/10.3803/EnM.2020.880

- 4,496 View
- 125 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Image-guided radiofrequency ablation (RFA) has been accepted as a minimally invasive treatment for adrenal tumors in patients who are unable to undergo adrenalectomy. Accordingly, this treatment has become more readily available for treating functioning or non-functioning adrenal masses. Thus, endocrinologists need a better understanding of percutaneous RFA of adrenal tumors. The purpose of this review is to briefly describe the basic mechanism of RFA, indications and contraindications, patient preparation prior to RFA, type of complications, how to avoid complications, RFA procedures, and treatment outcomes.
-
Citations
Citations to this article as recorded by- Clinical Features and Etiology of Recurrent Hypertension after Adrenalectomy
Xilan Dong, Qianhui Ling, Jin Bian, Yuehua Li, Mengjia Chen, Sufang Hao, Wenjun Ma, Huimin Zhang, Jun Cai, Ying Lou
Cardiovascular Innovations and Applications.2024;[Epub] CrossRef - Short-term outcome of adrenal radiofrequency ablation of adrenal cysts: a single-center experience
Shin Jeong Pak, Yu-mi Lee, Pyo Nyun Kim, Byung-Chang Kim, Jae Won Cho, Won Woong Kim, Tae-Yon Sung, Ki-wook Chung, Suck Joon Hong
Scientific Reports.2023;[Epub] CrossRef - Case report of trans-renal ablation procedures for a recurrent pheochromocytoma in von Hippel-Lindau disease
Byung Kwan Park
Precision and Future Medicine.2023; 7(2): 90. CrossRef - Efficacy and safety of radiofrequency ablation in the treatment of inoperable patients with pulmonary malignant nodules
Peng Qie, Xuejiao Xun, Xiaodong Nie, Qifan Yin, Hongshang Cui, Lijun Liu, Huien Wang
ANZ Journal of Surgery.2023; 93(12): 2969. CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef - Minimally invasive techniques in benign and malignant adrenal tumors
Ahmet Bulent Dogrul, Omer Cennet, Anıl Hilmi Dincer
World Journal of Clinical Cases.2022; 10(35): 12812. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - The role and place of mini-invasive methods of local tumor destruction in adrenal gland surgery
I.A. Kurganov, D.Yu. Bogdanov, S.I. Emelyanov, M.Sh. Mamistvalov
Endoskopicheskaya khirurgiya.2021; 27(6): 43. CrossRef
- Clinical Features and Etiology of Recurrent Hypertension after Adrenalectomy

- Adrenal gland
- Is Follow-up of Adrenal Incidentalomas Always Mandatory?
- Giuseppe Reimondo, Alessandra Muller, Elisa Ingargiola, Soraya Puglisi, Massimo Terzolo
- Endocrinol Metab. 2020;35(1):26-35. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.26

- 6,501 View
- 250 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Adrenal masses are mainly detected unexpectedly by an imaging study performed for reasons unrelated to any suspect of adrenal diseases. Such masses are commonly defined as “adrenal incidentalomas” and represent a public health challenge because they are increasingly recognized in current medical practice. Management of adrenal incidentalomas is currently matter of debate. Although there is consensus on the need of a multidisciplinary expert team evaluation and surgical approach in patients with significant hormonal excess and/or radiological findings suspicious of malignancy demonstrated at the diagnosis or during follow-up, the inconsistency between official guidelines and the consequent diffuse uncertainty on management of small adrenal incidentalomas still represents a considerable problem in terms of clinical choices in real practice. The aim of the present work is to review the proposed strategies on how to manage patients with adrenal incidentalomas that are not candidates to immediate surgery. The recent European Society of Endocrinology/European Network for the Study of Adrenal Tumors guidelines have supported the view to avoid surveillance in patients with clear benign adrenal lesions <4 cm and/or without any hormonal secretion; however, newer prospective studies are needed to confirm safety of this strategy, in particular in younger patients.
-
Citations
Citations to this article as recorded by- Adrenal Incidentaloma—Innocent Bystander or Intruder?
Laurence Amar, Inga Harbuz-Miller, Adina F Turcu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1303. CrossRef - Diagnosing and managing adrenal incidentalomas
Justine Herndon, Irina Bancos
JAAPA.2023; 36(5): 12. CrossRef - Tumor enlargement in adrenal incidentaloma is related to glaucoma: a new prognostic feature?
M. Caputo, T. Daffara, A. Ferrero, M. Romanisio, E. Monti, C. Mele, M. Zavattaro, S. Tricca, A. Siani, A. Clemente, C. Palumbo, S. De Cillà, A. Carriero, A. Volpe, P. Marzullo, G. Aimaretti, F. Prodam
Journal of Endocrinological Investigation.2023; 47(2): 377. CrossRef - The Role of Biomarkers in Adrenocortical Carcinoma: A Review of Current Evidence and Future Perspectives
Maja Mizdrak, Tina Tičinović Kurir, Joško Božić
Biomedicines.2021; 9(2): 174. CrossRef - An Adrenocortical Carcinoma Evolving After Nine Years of Latency From a Small Adrenal Incidentaloma
Harpreet S Kohli, Sukesh Manthri, Shikha Jain, Rahul Kashyap, Sheng Chen, Thoyaja Koritala, Aysun Tekin, Ramesh Adhikari, Raghavendra Tirupathi, Aram Barbaryan, Simon Zec, Hanyin Wang, Stephanie Welle, Pavan Devulapally, Mack Sheraton, Manpreet Kaur, Vish
Cureus.2021;[Epub] CrossRef - Diagnostic algorithm of the subclinical forms of adrenal neoplasms
Sofya G. Blyumina, Pavel N. Romashchenko, Igor S. Zheleznyak
Bulletin of the Russian Military Medical Academy.2021; 23(3): 67. CrossRef
- Adrenal Incidentaloma—Innocent Bystander or Intruder?

- A Case of an Adrenal Hemangioma Mimicking a Pancreatic Tail Tumor.
- Yun kyong Jeon, Ji Ryang Kim, Yong Seong An, Ji Hae Kwon, Yang Ho Kang, Seok Man Son, In Ju Kim, Yong Ki Kim
- J Korean Endocr Soc. 2008;23(1):62-65. Published online February 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.1.62
- 1,632 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Adrenal hemangiomas are rare non-functioning tumors that originate from the retroperitoneal organs. They are generally asymptomatic, and are usually discovered at autopsy. In 1955, Johnson and Jeppensen reported the first case of a surgically removed adrenal hemangioma. We report a case of adrenal hemangioma that mimicked a pancreatic tail tumor, as detected by computed tomography. We made a diagnosis of an adrenal hemangioma from endoscopic ultrasonography and confirmed the diagnosis following a laparascopic adrenalectomy. If one is suspicious of an adrenal hemangioma, one needs to assess the lesion from every aspect. With the advancement of diagnostic techniques in arteriography, ultrasound, and computed tomography, the frequency of preoperative recognition and diagnosis is on the increase. Still, it is difficult to diagnose an adrenal hemangioma just from an imaging study. One should consider performing surgery for removal of the tumor to rule out a malignancy, and to prevent traumatic rupture. With the case presentation, we review the clinical, radiographic, and pathological features of adrenal hemangiomas.


 KES
KES

 First
First Prev
Prev



