Search
- Page Path
- HOME > Search
- Hypothalamus and Pituitary Gland
- Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
- Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
- Endocrinol Metab. 2022;37(2):359-368. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1384
- 4,457 View
- 185 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Discontinuing growth hormone (GH) treatment during the transition to adulthood has been associated with adverse health outcomes in patients with childhood-onset growth hormone deficiency (CO-GHD). This study investigated the metabolic changes associated with interrupting GH treatment in adolescents with CO-GHD during the transition period.
Methods
This study included 187 patients with CO-GHD who were confirmed to have adult GHD and were treated at six academic centers in Korea. Data on clinical parameters, including anthropometric measurements, metabolic profiles, and bone mineral density (BMD) at the end of childhood GH treatment, were collected at the time of re-evaluation for GHD and 1 year after treatment resumption.
Results
Most patients (n=182, 97.3%) had organic GHD. The median age at treatment discontinuation and re-evaluation was 15.6 and 18.7 years, respectively. The median duration of treatment interruption was 2.8 years. During treatment discontinuation, body mass index Z-scores and total cholesterol, low-density lipoprotein, and non-high-density lipoprotein (HDL) cholesterol levels increased, whereas fasting glucose levels decreased. One year after GH treatment resumption, fasting glucose levels, HDL cholesterol levels, and femoral neck BMD increased significantly. Longer GH interruption (>2 years, 60.4%) resulted in worse lipid profiles at re-evaluation. The duration of interruption was positively correlated with fasting glucose and non-HDL cholesterol levels after adjusting for covariates.
Conclusion
GH treatment interruption during the transition period resulted in worse metabolic parameters, and a longer interruption period was correlated with poorer outcomes. GH treatment should be resumed early in patients with CO-GHD during the transition period. -
Citations
Citations to this article as recorded by- Ghrelin regulating liver activity and its potential effects on liver fibrosis and Echinococcosis
Jiang Zhu, Tanfang Zhou, Meng Menggen, Kalibixiati Aimulajiang, Hao Wen
Frontiers in Cellular and Infection Microbiology.2024;[Epub] CrossRef - Composición de la microbiota en pacientes con déficit de hormona de crecimiento antes y después de recibir tratamiento
Patricia García Navas, María Yolanda Ruíz del Prado, Pablo Villoslada Blanco, Emma Recio Fernández, María Ruíz del Campo, Patricia Pérez Matute
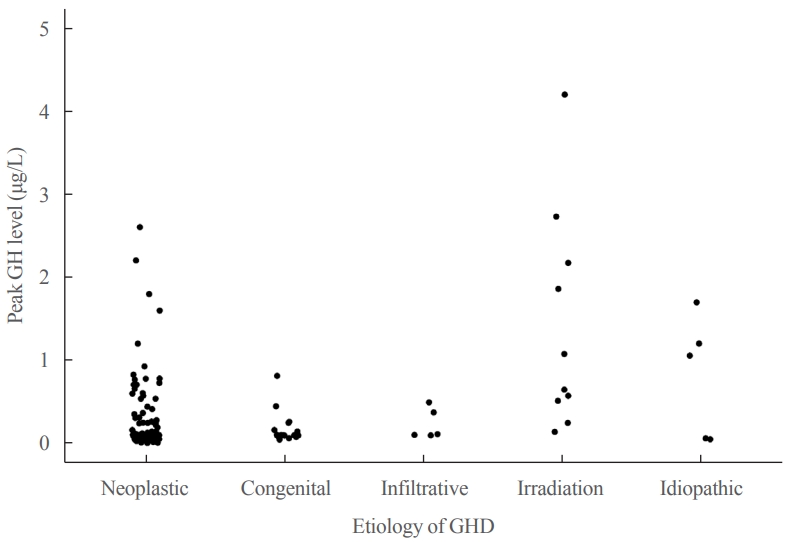
Anales de Pediatría.2024;[Epub] CrossRef - Relationship between the Stimulated Peak Growth Hormone Level and Metabolic Parameters in Children with Growth Hormone Deficiency
Seong Yong Lee
The Ewha Medical Journal.2023;[Epub] CrossRef - Dyslipidaemia and growth hormone deficiency – A comprehensive review
Matthias Hepprich, Fahim Ebrahimi, Emanuel Christ
Best Practice & Research Clinical Endocrinology & Metabolism.2023; 37(6): 101821. CrossRef
- Ghrelin regulating liver activity and its potential effects on liver fibrosis and Echinococcosis

- Clinical Study
- Cross-Sectional and Longitudinal Examination of Insulin Sensitivity and Secretion across Puberty among Non-Hispanic Black and White Children
- Shannon E. Marwitz, Megan V. Gaines, Sheila M. Brady, Sarah J. Mi, Miranda M. Broadney, Susan Z. Yanovski, Van S. Hubbard, Jack A. Yanovski
- Endocrinol Metab. 2020;35(4):847-857. Published online November 18, 2020
- DOI: https://doi.org/10.3803/EnM.2020.771
- 4,117 View
- 86 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
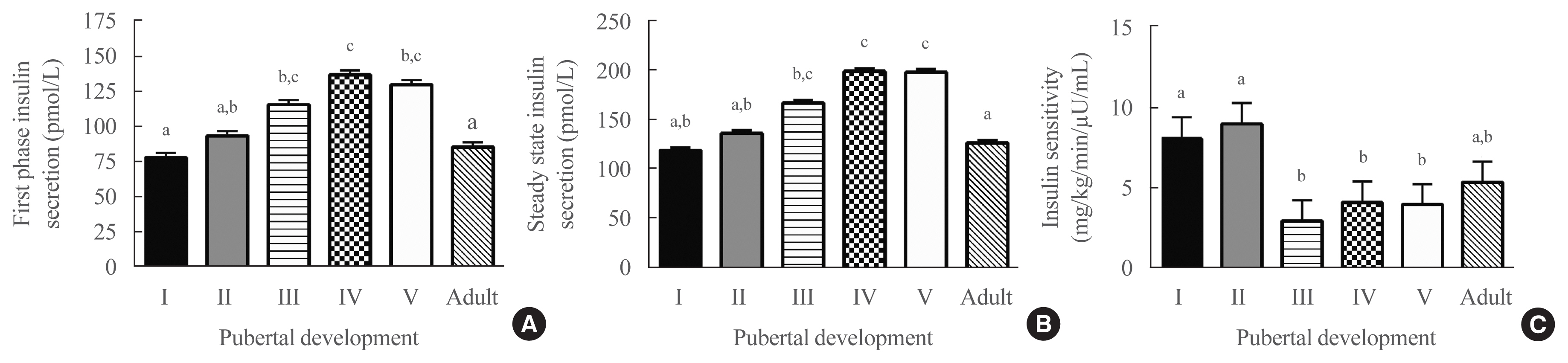
Few studies using criterion measures of insulin sensitivity (SI) and insulin secretory capacity (ISC) have been conducted across puberty to adulthood. We examined how SI and ISC change from pre-puberty through adulthood.
Methods
Hyperglycemic clamp studies were performed in a convenience sample of non-Hispanic Black (NHB) and White children evaluated at age 6 to 12 years and at approximately 5-year intervals into adulthood (maximum age 27 years). SI and ISC (first-phase and steady-state insulin secretion) were determined cross-sectionally in 133 unique participants across puberty and in adulthood. Additionally, longitudinal changes in SI and ISC were compared at two timepoints among three groups defined by changes in pubertal development: pre-pubertal at baseline and late-pubertal at follow-up (n=27), early-pubertal at baseline and late-pubertal at follow-up (n=27), and late-pubertal at baseline and adult at follow-up (n=24).
Results
Cross-sectionally, SI was highest in pre-puberty and early puberty and lowest in mid-puberty (analysis of covariance [ANCOVA] P=0.001). Longitudinally, SI decreased from pre-puberty to late puberty (P<0.001), then increased somewhat from late puberty to adulthood. Cross-sectionally, first-phase and steady-state ISC increased during puberty and decreased in adulthood (ANCOVA P<0.02). Longitudinally, steady-state and first-phase ISC increased from pre-puberty to late puberty (P<0.007), and steady-state ISC decreased from late puberty to adulthood. The NHB group had lower SI (P=0.003) and greater first-phase and steady-state ISC (P≤0.001), independent of pubertal development.
Conclusion
This study confirms that SI decreases and ISC increases transiently during puberty and shows that these changes largely resolve in adulthood. -
Citations
Citations to this article as recorded by- Exploratory Longitudinal Analysis of the Circulating CHIT1 Activity in Pediatric Patients with Obesity
Ioana Țaranu, Nicoleta Răcătăianu, Cristina Drugan, Cristina-Sorina Cătană, Andreea-Manuela Mirea, Diana Miclea, Sorana D. Bolboacă
Children.2023; 10(1): 124. CrossRef - Insulin Clearance in Health and Disease
Sonia M. Najjar, Sonia Caprio, Amalia Gastaldelli
Annual Review of Physiology.2023; 85(1): 363. CrossRef - Influence of puberty on relationships between body composition and blood pressure: a cross-sectional study
Esther A. Kwarteng, Lisa M. Shank, Loie M. Faulkner, Lucy K. Loch, Syeda Fatima, Suryaa Gupta, Hannah E. Haynes, Kaitlin L. Ballenger, Megan N. Parker, Sheila M. Brady, Anna Zenno, Marian Tanofsky-Kraff, Jack A. Yanovski
Pediatric Research.2023; 94(2): 781. CrossRef - Distribution of OGTT-Related Variables in Patients with Cystic Fibrosis from Puberty to Adulthood: An Italian Multicenter Study
Andrea Foppiani, Fabiana Ciciriello, Arianna Bisogno, Silvia Bricchi, Carla Colombo, Federico Alghisi, Vincenzina Lucidi, Maria Ausilia Catena, Mariacristina Lucanto, Andrea Mari, Giorgio Bedogni, Alberto Battezzati
Journal of Personalized Medicine.2023; 13(3): 469. CrossRef - Fat-free/lean body mass in children with insulin resistance or metabolic syndrome: a systematic review and meta-analysis
Diana Paola Córdoba-Rodríguez, Iris Iglesia, Alejandro Gomez-Bruton, Gerardo Rodríguez, José Antonio Casajús, Hernan Morales-Devia, Luis A. Moreno
BMC Pediatrics.2022;[Epub] CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - An update of the consensus statement on insulin resistance in children 2010
Veronica Maria Tagi, Sona Samvelyan, Francesco Chiarelli
Frontiers in Endocrinology.2022;[Epub] CrossRef - Dietary sugar restriction reduces hepatic de novo lipogenesis in boys with fatty liver disease
Stephanie T. Chung, Sheela N. Magge
Journal of Clinical Investigation.2021;[Epub] CrossRef
- Exploratory Longitudinal Analysis of the Circulating CHIT1 Activity in Pediatric Patients with Obesity

- Obesity and Metabolism
- Epidemiology of Childhood Obesity in Korea
- Kyoung Hwa Ha, Dae Jung Kim
- Endocrinol Metab. 2016;31(4):510-518. Published online November 3, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.510
- 6,083 View
- 74 Download
- 42 Web of Science
- 39 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Over the past several decades, the prevalence of obesity has increased dramatically worldwide and is increasing not only in developed countries, but also in developing countries. This increase may lead to an increase in the incidence of chronic diseases throughout the lifespan. In Korean children and adolescents, the prevalence of obesity increased from 6.8% in 1998 to 10.0% in 2013. Obesity is a state that more commonly influences children and adolescents of lower socioeconomic status (SES) than those with a higher SES. However, the prevalence of metabolic syndrome in a nationally representative sample of Korean adolescents decreased from 1998 to 2012. According to the Diabetes Fact Sheet of the Korean Diabetes Association, the prevalence of type 2 diabetes among children aged 18 years or younger was 153.5 per 100,000 in 2006 and 205.0 per 100,000 in 2013. Obesity is a complex disease influenced by many interacting factors, such as adipocytokines, lipopolysaccharide-binding protein, adenovirus 36 infection, birth weight, lifestyle, and endocrine-disrupting chemicals. Obesity in youth can adversely impact practically every organ system and lead to serious consequences, such as metabolic, gastrointestinal, pulmonary, cardiovascular, and psychosocial complications. Therefore, coordinated efforts by governments, organizations, communities, and individuals are needed to prevent and treat childhood obesity. In particular, a long-term policy to improve the social environment will also be necessary.
-
Citations
Citations to this article as recorded by- Sulfur Metabolism of the Gut Microbiome and Colorectal Cancer: The Threat to the Younger Generation
Ji-Yeon Moon, Bong-Hyeon Kye, Seung-Hyun Ko, Ri Na Yoo
Nutrients.2023; 15(8): 1966. CrossRef - Association between Obesity and Cardiovascular Disease Risk Factors in Different Age Groups of Adolescents: An Analysis of Data from the Korean National Health and Nutritional Examination Survey
Joowon Lee, Seul Gi Cha, Jue Seong Lee, Susan Taejung Kim, Young Hwan Song
Children.2023; 10(5): 827. CrossRef - The economic burden of adolescent internet addiction: A Korean health cost case study
Robert W. Mead, Edward Nall
The Social Science Journal.2023; : 1. CrossRef - Trends in socioeconomic inequalities in obesity among Korean adolescents: the Korea Youth Risk Behavior Web-based Survey (KYRBS) 2006 to 2020
Eunji Kim, Ga Bin Lee, Dong Keon Yon, Hyeon Chang Kim
Epidemiology and Health.2023; 45: e2023033. CrossRef - Protective Effects of Melatonin in High-Fat Diet-Induced Hepatic Steatosis via Decreased Intestinal Lipid Absorption and Hepatic Cholesterol Synthesis
Hyungjune Ku, Yeonji Kim, Alvin Lyle Kim, Garam Lee, Youngsik Choi, Bukyung Kim
Endocrinology and Metabolism.2023; 38(5): 557. CrossRef - Time Trends in the Prevalence of Atopic Dermatitis in Korean Children According to Age
Ji Young Lee, Jihyun Kim, Kangmo Ahn
Allergy, Asthma & Immunology Research.2022; 14(1): 123. CrossRef - Additive Effects of Exercise or Nutrition Intervention in a 24-Month Multidisciplinary Treatment with a Booster Intervention for Children and Adolescents with Overweight or Obesity: The ICAAN Study
Sarah Woo, Young-Su Ju, Young-Gyun Seo, Yoon-Myung Kim, Hyunjung Lim, Kyung-Hee Park
Nutrients.2022; 14(2): 387. CrossRef - Effectiveness of obesity interventions among South Korean children and adolescents and importance of the type of intervention component: a meta-analysis
Siyoung Choe, Jaesin Sa, Jean-Philippe Chaput, Deokjin Kim
Clinical and Experimental Pediatrics.2022; 65(2): 98. CrossRef - Effects of a 12-Week Diet versus Diet plus Aerobic and Resistance Exercise Program on Acylated and Desacylated Ghrelin, and Ghrelin O-Acyltransferase in Adolescent Girls with Obesity
Hyun Jun Kim, Young Jin Tak, Sang Yeoup Lee, Jeong Pyo Seo
International Journal of Environmental Research and Public Health.2022; 19(3): 1480. CrossRef - Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018 (Diabetes Metab J 2021;45:880-9)
Dae Jung Kim
Diabetes & Metabolism Journal.2022; 46(2): 349. CrossRef - Adenovirus 36 infection and daycare starting age are associated with adiposity in children and adolescents
Ana Carolina Lobor Cancelier, Nikhil V. Dhurandhar, Swetha Peddibhotla, Richard L. Atkinson, Helena C.G. Silva, Daisson J. Trevisol, Fabiana Schuelter-Trevisol
Jornal de Pediatria.2021; 97(4): 420. CrossRef - The association of obstructive sleep apnea with dyslipidemia in Korean children and adolescents: a single-center, cross-sectional study
Eun Kyeong Kang, Min Jeong Jang, Ki Duk Kim, Young Min Ahn
Journal of Clinical Sleep Medicine.2021; 17(8): 1599. CrossRef - Trajectories in glycated hemoglobin and body mass index in children and adolescents with diabetes using the common data model
Yun Jeong Lee, Sooyoung Yoo, Soyoung Yi, Seok Kim, Chunggak Lee, Jihoon Cho, Soyeon Ahn, Sunkyu Choi, Hee Hwang, Young Ah Lee, Choong Ho Shin, Hyung-Jin Yoon, Kwangsoo Kim, Eunhye Song, Jin Ho Choi, Han Wook Yoo, Young-Hak Kim, Ji Seon Oh, Eun-Ae Kang, Ga
Scientific Reports.2021;[Epub] CrossRef - Comparison of eating habits and inappropriate weight control efforts of secondary school students enrolled in a weight control program
EunKyo Kang, Soojeong Kim, Young Ho Yun
Nutrition Research and Practice.2021; 15(5): 628. CrossRef - Association between childhood obesity and familial salt intake: analysis of data from Korean National Health and Nutrition Examination Survey, 2014–2017
Byung Min Yoo, Mijin Kim, Min Jae Kang
Endocrine Journal.2021; 68(9): 1127. CrossRef - Regional Adolescent Obesity and Overweight Status in Korea from 2018–2019: Comparison between Two Data Sources
Dong-Hee Ryu, Su-Jin Lee
Healthcare.2021; 9(12): 1751. CrossRef - Family Factors and Obesity in Relation to Mental Health Among Korean Children and Adolescents
Hye-Mi Noh, Jane Park, Eun-Ju Sung, Young Soo Ju, Hye-Ja Lee, Yoon-Kyoung Jeong, Kyung Hee Park
Journal of Child and Family Studies.2020; 29(5): 1284. CrossRef - Distribution of Tri-Ponderal Mass Index and its Relation to Body Mass Index in Children and Adolescents Aged 10 to 20 Years
Hong Kyu Park, Young Suk Shim
The Journal of Clinical Endocrinology & Metabolism.2020; 105(3): e826. CrossRef - The change in prevalence of suspected non-alcoholic fatty liver disease in Korean adolescents from 2001 to 2017
Seung Ha Park, Yong Eun Park, Jin Lee, Joon Hyuk Choi, Nae Yun Heo, Jongha Park, Tae Oh Kim, Jun Seong Hwang, Eunju Kim, Eun Hye Oh, Hang Jea Jang, Ha Young Park, Hyun Kuk Kim
Paediatrics and International Child Health.2020; 40(3): 166. CrossRef - Effect of inactivated Bifidobacterium longum intake on obese diabetes model mice (TSOD)
Mahmoud Ben Othman, Kazuichi Sakamoto
Food Research International.2020; 129: 108792. CrossRef - Self and parent-proxy rated health-related quality of life (HRQoL) in youth with obesity: are parents good surrogates?
Delicia Shu Qin Ooi, Kah Yin Loke, Cindy Wei Li Ho, Yvonne Yijuan Lim, Veronica Tay, Vijaya Karuppiah, Andrew Anjian Sng, Lester Yousheng Lai, Yung Seng Lee, Konstadina Griva
Quality of Life Research.2020; 29(8): 2171. CrossRef - Chinese men living in urban areas of Shijiazhuang, Hebei at higher risk of overweight or obesity
De-Xian Kong, Xiao-feng Su, Jing-wei Zhao, Lian Chen, Ling-bing Meng, Zhen-xi Zhang, Sen Yang, Lei Zhang, Ya-bin Liu
Journal of International Medical Research.2020; 48(8): 030006052094588. CrossRef - Association between Parent’s Metabolic Syndrome and 12- to18-Year-Old Offspring’s Overweight: Results from the Korea National Health and Nutrition Examination Survey (K-NHANES) 2009–2016
Na Yeong Lee, Kyungdo Han, Yoonji Lee, Seulki Kim, Seonhwa Lee, Yujung Choi, Moon bae Ahn, Shin Hee Kim, Won Kyoung Cho, Kyoung Soon Cho, Min Ho Jung, Yong-Gyu Park, Byung-Kyu Suh, Silvia Monticone
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Incidence and Prevalence of Type 1 Diabetes Mellitus among Korean Children and Adolescents between 2007 and 2017: An Epidemiologic Study Based on a National Database
Hyun Wook Chae, Gi Hyeon Seo, Kyungchul Song, Han Saem Choi, Junghwan Suh, Ahreum Kwon, Sangmi Ha, Ho-Seong Kim
Diabetes & Metabolism Journal.2020; 44(6): 866. CrossRef - Quick assessment with controlled attenuation parameter for hepatic steatosis in children based on MRI-PDFF as the gold standard
Jaeseung Shin, Myung-Joon Kim, Hyun Joo Shin, Haesung Yoon, Seung Kim, Hong Koh, Mi-Jung Lee
BMC Pediatrics.2019;[Epub] CrossRef - Changing patterns of multiple sclerosis in Korea: Toward a more baseline MRI lesions and intrathecal humoral immune responses
Hyun-June Shin, Jae-Won Hyun, Su-Hyun Kim, Min Su Park, Eun Hee Sohn, Seol-Hee Baek, Byung-Jo Kim, Kyomin Choi, Jeeyoung Oh, Joong-Yang Cho, Ohyun Kwon, Woojun Kim, Jee-Eun Kim, Ju-Hong Min, Byoung Joon Kim, Sun-Young Oh, Jong Seok Bae, Kee Hong Park, Jun
Multiple Sclerosis and Related Disorders.2019; 35: 209. CrossRef - Serum osteocalcin levels in overweight children
Seok Bin Oh, Won Young Lee, Hyo-Kyoung Nam, Young-Jun Rhie, Kee-Hyoung Lee
Annals of Pediatric Endocrinology & Metabolism.2019; 24(2): 104. CrossRef - Associations between lipid profiles of adolescents and their mothers based on a nationwide health and nutrition survey in South Korea
Ji Hyung Nam, Jaeyong Shin, Sung-In Jang, Ji Hyun Kim, Kyu-Tae Han, Jun Kyu Lee, Yun Jeong Lim, Eun-Cheol Park
BMJ Open.2019; 9(3): e024731. CrossRef - Association of Weight Control Behaviors with Body Mass Index in Korean Adolescents: A Quantile Regression Approach
Sun-Mi Chae, Mi Ja Kim, Chang Gi Park, Ji-Young Yeo, Ji-Hye Hwang, Insook Kwon, Soo-Yeon Han
Journal of Pediatric Nursing.2018; 40: e18. CrossRef - Associations between birth weight, obesity, fat mass and lean mass in Korean adolescents: the Fifth Korea National Health and Nutrition Examination Survey
Myunggee Kang, Jung Eun Yoo, Kyuwoong Kim, Seulggie Choi, Sang Min Park
BMJ Open.2018; 8(2): e018039. CrossRef - Thyroid function in obese Korean children and adolescents: Korea National Health and Nutrition Examination Survey 2013–2015
Young Min An, Soon Jeong Moon, Soon Ki Kim, Young Ju Suh, Ji Eun Lee
Annals of Pediatric Endocrinology & Metabolism.2018; 23(3): 141. CrossRef - Validation of Dietary Reference Intakes for predicting energy requirements in elementary school-age children
Eun-Kyung Kim, Didace Ndahimana, Kazuko Ishikawa-Takata, Sangjik Lee, Hyungryul Kim, Kiwon Lim, In-Sook Lee, Shigeho Tanaka, Ye-Jin Kim, Yeon-Jung Choi, Mun-Jeong Ju, Jonghoon Park
Nutrition Research and Practice.2018; 12(4): 336. CrossRef - Family-based treatment for obesity in tweens: a three-year longitudinal follow-up study
Hongsik J. Cheon, Jay R. Fraser, Trang Kieu Nguyen
International Journal of Advertising.2018; 37(4): 548. CrossRef - Anti-obesity effects of Clausena excavata in high-fat diet-induced obese mice
Young-Rak Cho, Jung A. Lee, Yoon Yeon Kim, Jae-Shin Kang, Jae-Ho Lee, Eun-Kyung Ahn
Biomedicine & Pharmacotherapy.2018; 99: 253. CrossRef - Hypertension Risk of Obesity and Abdominal Obesity in High School Students
Yu jin Kwak, Ji Hyen Lee, Young Mi Hong, Hae Soon Kim
The Ewha Medical Journal.2018; 41(1): 13. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Management of childhood obesity
Shin-Hye Kim, Mi-Jung Park
Journal of the Korean Medical Association.2017; 60(3): 233. CrossRef - Prevalences and Management of Diabetes and Pre-diabetes among Korean Teenagers and Young Adults: Results from the Korea National Health and Nutrition Examination Survey 2005–2014
Eun-Hee Cho, Dayeon Shin, Keun-Hyok Cho, Junguk Hur
Journal of Korean Medical Science.2017; 32(12): 1984. CrossRef - Prevalence and risk factors for type 2 diabetes mellitus with Prader–Willi syndrome: a single center experience
Aram Yang, Jinsup Kim, Sung Yoon Cho, Dong-Kyu Jin
Orphanet Journal of Rare Diseases.2017;[Epub] CrossRef
- Sulfur Metabolism of the Gut Microbiome and Colorectal Cancer: The Threat to the Younger Generation

- Relationship between Childhood and Adolescent Obesity and Remnant Lipoprotein.
- Yong Jun Choi, Young Eun Jo, Yun Kyung Kim, Sang Mi Ahn, Seung Hee Baik, Sun Hye Jung, Hae Jin Kim, Yoon Sok Chung, Kwan Woo Lee, Dae Jung Kim
- J Korean Endocr Soc. 2006;21(4):311-318. Published online August 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.4.311
- 1,927 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Remnant lipoproteins are the lipolytic degradation product of the triglyceride-rich lipoproteins produced by the liver (very-low-density lipoprotein cholesterol) and intestine (chylomicrons). Recent studies have demonstrated a correlation between remnant lipoproteins and cardiovascular risk. Our study assessed the relationship between obesity and remnant lipoproteins and evaluated the factors related to remnant lipoprotein in children and adolescents. METHODS: Body mass index (BMI), waist circumference, systolic and diastolic blood pressures, body fat mass, total abdominal fat, visceral and subcutaneous fat areas, total cholesterol, triglyceride (TG), LDL cholesterol (LDL-C), HDL cholesterol (HDL-C) and remnant lipoprotein cholesterol (RLP-C) were measured in 135 children and adolescents (67 boys and 68 girls). Plasma RLP fractions were isolated using an immunoaffinity gel containing specific anti-apoB-100 and anti-apoA-I antibodies. The subjects were divided into three groups: the low (< 50 percentile), mid (50~84 percentile), and high (> or = 85 percentile) BMI groups. RESULTS: RLP-C was significantly correlated with age, sex, BMI, waist circumference, systolic and diastolic blood pressures, visceral and subcutaneous fat areas, visceral fat area to subcutaneous fat area ratio (VSR), total cholesterol, TG, HDL-C, apoB, and HOMA-IR. From a multivariate regression analysis, TG (beta = 0.928, P < 0.001) was found to be independently correlated with RLP-C. After excluding TG as an independent variable, a multivariate regression analysis revealed that the HOMA-IR (beta=0.231, P=0.007) and systolic blood pressure (beta=0.169, P=0.046) were independently associated with RLP-C. CONCLUSION: RLP-C was significantly higher in obese children and adolescents. TG, systolic blood pressure, and insulin resistance were related to remnant lipoproteins. -
Citations
Citations to this article as recorded by- Epidemiology of Childhood Obesity in Korea
Kyoung Hwa Ha, Dae Jung Kim
Endocrinology and Metabolism.2016; 31(4): 510. CrossRef
- Epidemiology of Childhood Obesity in Korea

- The Association between the Depression and the Perception of Obesity by Adolescent Girls.
- Moo Jung Park, Eun Ah Lee, Sang Ho Lee, Jong In Kim, So Yeon Ryu, Ki Soon Kim
- J Korean Endocr Soc. 1997;12(2):295-307. Published online January 1, 2001
- 1,034 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was performed to find the association between the depression and perception of obesity by adolescent girls in Jung Eup City, Chollapukdo. The data were collected by questionnaire from July to October, 1996. RESULTS: 1. While the obesity rate of the girls by BMI criteria was 6.0%, 41.1% of girls perceived that they were obese. 2. Forty-eight percent of respondents tried weight control already, and as the method of weight control 33.3% tried exercise, 27.2% reduced food, 23.6% avoided snack before going to bed. 3. while 39.3% among those whose BMI was lower than 20 and 54.2% among those with BMI 20-24 tried weight control, only 5.1% among those who perceived their bodies as slim tried weight control. 4. By the analysis of self-rating depression scale (SDS) only 14.8% was normal without depression and the rest showed high SDS scale; 36.9% as mild, 38.5% as moderate, and 9.7% as severe state of depression. 5. While no statistically significant difference of SDS scores by the size of BMI was shown, significant different of SDS scores was shown among groups with different perception of their obesity and practice of weight control. 6. As a result of stepwise multiple regression analysis, dieting, perceived body image, and body mass index were significantly associated with depression of the adolescent girls. CONCLUSION: Adolescent girls who perceived themselves overweight regardless of actual weight were more likely to diet than other girls. And these characteristics had an influence on the depression of the adolescents. It is suggested that appropriate education should be required to prevent thoughtless weight control of the adolescents and to maintain mental health of the adolescents.


 KES
KES

 First
First Prev
Prev



