Effects of Resistance Exercise on Bone Health
Article information
Abstract
The prevalence of chronic diseases including osteoporosis and sarcopenia increases as the population ages. Osteoporosis and sarcopenia are commonly associated with genetics, mechanical factors, and hormonal factors and primarily associated with aging. Many older populations, particularly those with frailty, are likely to have concurrent osteoporosis and sarcopenia, further increasing their risk of disease-related complications. Because bones and muscles are closely interconnected by anatomy, metabolic profile, and chemical components, a diagnosis should be considered for both sarcopenia and osteoporosis, which may be treated with optimal therapeutic interventions eliciting pleiotropic effects on both bones and muscles. Exercise training has been recommended as a promising therapeutic strategy to encounter the loss of bone and muscle mass due to osteosarcopenia. To stimulate the osteogenic effects for bone mass accretion, bone tissues must be exposed to mechanical load exceeding those experienced during daily living activities. Of the several exercise training programs, resistance exercise (RE) is known to be highly beneficial for the preservation of bone and muscle mass. This review summarizes the mechanisms of RE for the preservation of bone and muscle mass and supports the clinical evidences for the use of RE as a therapeutic option in osteosarcopenia.
INTRODUCTION
In an aging society, the prevalence of osteoporosis and osteopenia continues to increase progressively, particularly in older patients [1]. Osteoporosis is characterized by a decreased bone mass and an increased risk of fragility fractures [2]. According to the World Health Organization (WHO) criteria, osteoporosis and osteopenia are defined as the lowest bone mineral density (BMD) T-score of ≤−2.5 and −2.5 to 1.0 measured at the lumbar spine or hip, respectively [3]. Sarcopenia is defined as the age-related decrease in skeletal muscle mass, function, and strength [4]. There are several proposed diagnostic criteria of sarcopenia, in which sarcopenia is diagnosed using the criteria of low muscle mass and low muscle function (either low strength and/or low physical performance) [5], or based on a low whole-body or appendicular fat-free mass in combination of poor physical performance [6]. Similar to osteoporosis and osteopenia, sarcopenia is also frequently diagnosed in frail, older patients, thus resulting in a significant burden on the patients and is widely considered as a public health problem [78]. Sarcopenia and osteoporosis are associated with physical disability and have common risk factors and biological pathways [9]. The combination of these two diseases leads to exacerbation of negative health effects. Sarcopenia further increases fracture risk through increasing risk of fall in patients who already have vulnerability of bones due to osteoporosis [10]. On this basis, recently the term ‘osteosarcopenia’ has been proposed for patients with both sarcopenia and osteoporosis. Osteosarcopenia is a potentially preventable and treatable disease; therefore, there have been many efforts to search for optimal therapeutic interventions exerting pleiotropic effects on bones and muscles.
Exercise training has been recommended as a low-cost and safe non-pharmacological intervention strategy for the conservation of musculoskeletal health [11]. Although specific mechanisms via which exercise improves bone health are not fully elucidated yet, it is widely accepted that mechanical load induced by exercise training increases the muscle mass, produces mechanical stress in the skeleton, and enhances the osteoblast activity [1213]. However, not all exercise modalities are equally osteogenic. For exercise training to elicit an osteogenic effect, the mechanical load applied to bones should exceed that encountered during daily activities [14]. Weight-bearing impact exercise such as hopping and jumping, and/or progressive resistance exercise (RE), alone or in combination can improve the bone health in adults [11]. Among them, RE has been highlighted as the most promising intervention to maintain or increase bone mass and density [15]. This is because a variety of muscular loads are applied on the bone during RE, which generate stimuli and promote an osteogenic response of the bone [16].
However, bone strength is determined by not only BMD but also bone quality factors including bone microarchitecture, geometry, and turnover. Although dual-energy X-ray absorptiometry (DXA) has been the most widely used clinical tool to assess bone strength by measuring BMD, it does not capture the bone quality. To date, previous review articles regarding the skeletal effects of RE mainly focused on the BMD alone and there were limited interest in bone quality and strength. Therefore, in this article, we review the previously published studies, including both in vitro and animal studies and those with clinical data, on the effects of RE on musculoskeletal health, in particular, on bone strength.
EXERCISE PROGRAMS AND PREVENTION OF BONE LOSS
Exercise programs are classified as static weight-bearing exercises (e.g., single-leg standing), high-impact weight-bearing exercises (e.g., jogging, running, dancing, jumping, and vibration platform), low-impact weight-bearing exercises (e.g., walking and Tai Chi), high-impact non-weight-bearing exercises (e.g., progressive RE), low-impact non-weight-bearing exercises (e.g., swimming) and combination exercises [17].
Prolonged aerobic training (e.g., swimming, cycling, and walking) is widely beneficial to all body systems, but there are clinical evidences suggesting that none of these activities provide an adequate stimulus to bones [181920]. Since high-impact weight-bearing exercise is not always suitable for older adults due to the risk of musculoskeletal impairment in this population [21]; thus, low-impact non-weight-bearing exercise such as swimming has been recommended in this population. However, non-weight-bearing aerobic exercise applies no or very low impact on bones, and shows lesser osteogenic responses than weight-bearing aerobic exercise in older adults [22].
Regular walking, which is frequently prescribed to prevent osteoporosis, also has little or no effect on prevention of bone loss [23]. This could be attributed that low-impact loading force applied during walking does not elicit loads of a sufficient magnitude, rate, or distribution to stimulate bone cells to lead to an adaptive skeletal response. In addition, there is evidence that frequent walking can expose the previously sedentary or frail older adults to an increased risk of falling, thereby increasing the risk of fracture [242526]. Thus, despite the benefits of regular walking on aerobic fitness, adiposity, and other cardiometabolic factors, walking alone is insufficient to optimize the musculoskeletal health [18].
Other physical exercise programs including moderate- to high-impact or multi-directional weight-bearing activities have been shown to maintain or improve the hip and spine areal BMD (aBMD) in older patients [272829]. However, these types of exercise may be contraindicated in individuals with severe osteoporosis or a recent history of fracture, although no clinical trials have evaluated the feasibility and efficacy of such exercises in high-risk patients.
WHAT IS RESISTANCE EXERCISE?
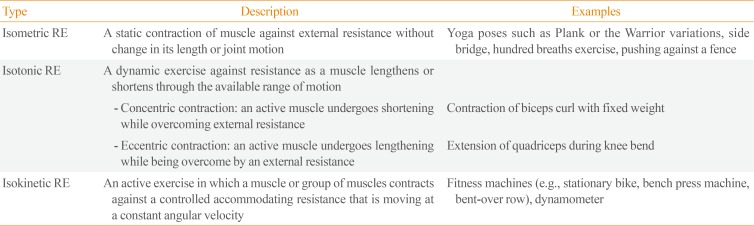
RE is defined as a physical conditioning program that enhances fitness, health, and sports performance, using a variety of training modalities such as free weights, weight machines, medicine balls, elastic bands, and different movement velocities (Table 1). The RE interventions including weighted lunges, hip abduction/adduction, knee extension/flexion, plantar-/dorsi-flexion, back extension, reverse chest fly, and abdominal exercises or a smaller number of compound movements of squats and deadlifts, target the major muscle groups attached to the hip and spine. The magnitude of mechanical load is important for bone formation, and RE elicits a magnitude of strain that exceeds the threshold required for increased bone modeling [30]. RE has been frequently prescribed because it has been consistently shown to be safe and effective for improving muscle mass, size, and strength in middle-aged and older adults, including the frail elderly and even those with a history of fracture [3132]. The intensity and type of RE should be individualized according to tolerance and ability of adults, particularly in the presence of pain. At least two sets of one exercise for each major muscle group should be performed at a target intensity of eight to 12 repetition maximum (RM); however, for some individuals who are previously sedentary or unfamiliar with RE, it should be started at a lower intensity. In terms of frequency of RE, the WHO global recommendation for older patients of the 65 years and above age group suggests that muscle-strengthening activities, involving major muscle groups, should be done on 2 or more days a week [33].
The greatest skeletal benefits from RE have been achieved when the resistance was progressively increased over time, the magnitude of mechanical load was high (around 80% to 85% one RM) [34], exercise was performed at least twice a week, and large muscles crossing the hip and spine were targeted [3536]. The spine may be more responsive to RE than the hip [37]. Power training (high-intensity RE) may be indirectly beneficial to bone because of a slightly greater effect on muscle strength and functional performance than regular training [38]. Power training maintained BMD in postmenopausal women without increasing risk of injury or pain [3940]. Multicomponent interventions that include muscle power training improved the physical status of frail older adults, and prevented disability and other adverse outcomes [41]. However, current exercise guidelines for osteoporosis recommend only moderate-intensity exercises (70% to 80% one RM, eight to 15 repetitions) for individual muscle groups which are insufficient to generate mechanical strain to stimulate an osteogenic response [42].
PROPOSED MECHANISMS INVOLVED IN THE MUSCULOSKELETAL EFFECT OF RESISTANCE EXERCISE
Preservation of the skeletal muscle
Skeletal muscle contractility can be reduced by prolonged inactivity, and/or muscle wasting state, which result in profound deteriorations in muscle myofibrillar mass, muscle strength, and mobility [43]. Tensile and/or compressive stress that is generated during RE preferentially stimulates muscle protein synthesis (MPS) involved in muscle contraction [44]. Previous studies suggest that mechanistic target of rapamycin complex 1 (mTORC1) is considered as the critical factor to integrate various stimulators, including mechanical strains, nutrients, and growth factors, for the activation of signaling pathway to initiate muscle protein translation [45]. Clear evidence exists demonstrating an association between RE and muscle hypertrophy by promoting an increase in systemic growth factors such as insulin-like growth factor 1, thereby activating a PI3K-Akt-mTORC1 signaling pathway to stimulate MPS [464748495051]. However, there have been recent studies showing growth factor-independent mTORC1 activation, which suggest that intrinsic mechanosensitive molecules exert more important role as drivers of muscle protein accretion [52535455]. Based on the findings from in vitro or animal studies, there are yet unidentified mechanosensing proteins acting on the zeta isoform of diacylglycerol kinase, resulting in the conversion of diacylglycerol to phosphatidic acid which then directly activates the mTORC1 [5657]. There are also yet unidentified kinases phosphorylating the tuberous sclerosis complex-2, which allow the Ras homolog enriched in brain to be in its guanosine triphosphate bound state that can directly activate mTORC1 [58]. However, the knowledge on RE-induced mechanotransduction for MPS in humans is still highly limited.
RE significantly increases the cross-sectional area of trained muscles and consequently their force and power [5960]. Based on results obtained from the Advanced Resistance Exercise Device, RE can prevent significant loss of muscle and bone with prolonged exposure to microgravity during spaceflight [61]. RE interventions are also effective in augmenting skeletal muscle mass, increasing muscle strength, and/or improving functional performance in the older population [626364]. However, in older adults, the responsiveness to RE is blunted compared with younger adults [65666768]. This may be attributed to the blunted MPS rate in response to a single bout of RE in older adults [69]. Furthermore, this anabolic resistance may be due to some changes in gene expression and anabolic signaling; an attenuated anabolic hormone response to RE is observed in older adults compared with younger adults [70]. For determining the effect of RE on the reduction of fall and fracture risk, further large-scale studies are needed to be investigated [7172].
Increased bone strength through mechanical loading
Mechanical loading is a fundamental factor for bone mass accretion. The principle of the loading phenomenon was first developed by Frost [73] and is also known as the Mechanostat theory. This theory suggests that the bone possesses an inherent biological system to elicit bone formation in response to high mechanical strains, thereby strengthening the bone. This system involves the bone cells, mainly osteocytes, that can detect and respond to mechanical loading. Osteocytes play a key role in the remodeling process by sensing the mechanical loads, and transmitting the information to the osteoblasts and osteoclasts, which then maintain the skeletal homeostasis [74]. Sclerostin is a protein produced in osteocytes, which plays a central role in regulating the formation of bone. It functions as a Wnt antagonist, blocking the canonical Wnt/β-catenin signaling pathway. Wnt-signaling pathway leads to increased osteoprogenitor cell populations and decreased apoptosis of mature osteoblasts. Mechanical loading downregulates sclerostin expression in bones, thereby increasing osteoblastic bone formation and decreasing bone resorption by the inhibition of osteoclast activity [75]. Bone formation is increased in regions of high strain, in particular, the periosteal bone surface, whereas bone turnover and porosity are reduced. Consequently, mechanical loading can lead to increase in the cross-sectional area and tissue density of bones. In addition, this theory indicates that the skeletal effect of mechanical loading is site-specific, with greater response at skeletal sites where loading impacts are greater. The majority of weight-bearing exercise elicit physical loading to the lower limbs; as expected, positive skeletal effects on hip regions have been reported in previous studies and literature reviews [7677]. Further to this, it has been suggested that bone adaptation to mechanical loading affects not only the BMD but also geometric markers of bone strength [7879]. This would bear relevance for fracture prevention because bone fragility is a consequence of both material and structural abnormalities of the skeleton [808182].
To generate the adaptive response of bone (osteogenesis) to mechanical loading, sufficient magnitude, rate, and frequency of loading are necessary. Many animal studies showed that loading must be dynamic not static [83], induce high frequency strains [8485], and be applied rapidly [86]. If adequate intensity of loading is achieved, relatively few loading repetitions are sufficient to generate an adaptive skeletal response [87]. Because osteocytes are desensitized due to repetitive loading, short bouts with interval for rest are more beneficial than the same number of loads performed all at once [88]. Furthermore, because bone adapts to customary patterns of loading such as one-directional movement, diversification of loading such as multi-directional training is required to stimulate an adaptive skeletal response [89].
While there is no clear evidence from life-long studies, it is suggested that adaptations to mechanical loading in the youth are translated to greater bone strength over a lifetime [90]. Bones become less sensitive to mechanical loading after skeletal maturity is reached at 18 to 25 years of age. Consequently, the skeleton is more responsive to exercise in childhood than in adulthood and old age [91]. Although theoretically the effect of exercise training seems to be less in adulthood than in childhood, considering the previous clinical evidences indicating the capability of weight-bearing activities on reducing bone loss in adult osteoporosis, these activities are also meaningful in adults.
CLINICAL EVIDENCE OF THE EFFECTS OF RESISTANCE EXERCISE FOR BONE STRENGTH
A previous systematic review reported that performing RE two to three times a week for 1 year demonstrated the maintenance or increase of aBMD at the lumbar spine and hip in postmenopausal women [15]. In a subgroup analysis of the Cochrane review and previous meta-analyses, RE has resulted in a significant improvement of BMD in the lumbar spine and femur neck in postmenopausal women [179293]. A combination of RE and weight-bearing aerobic exercise (e.g., running, skipping, jumping, or high-impact aerobics) is recommended as RE training provides muscular loading while weight-bearing aerobic exercise provides additional mechanical loading to the bone above gravity. Concretely, this combination has improved multiple musculoskeletal outcomes including aBMD, muscle mass, and strength, in older women as well as men [769495]. A systematic review and meta-analysis has summarized that the majority of previous studies with combined RE training with high-impact or weight-bearing exercises have shown an improved aBMD in the lumbar spine and femur neck in postmenopausal women [35,96]. In a systemic review investigating the effects of exercise on aBMD in middle-aged and older men, RE alone or in combination with high-impact loading activities maintained or increased aBMD in accordance with postmenopausal women [77]. These findings were consistent with the results from a meta-analysis of randomized controlled trials in older adults [29]. Taken together, RE alone or in combination with other interventions may be ideal to preserve bone loss or even increase BMD in both lumbar spine and femoral neck, not only in postmenopausal women or middle-aged men but also in the older population.
Exercise training could enhance bone strength, independent of changes in BMD, through alterations in bone structure and/or localized adaptation in bone distribution at the sites subjected to the greatest strain [27,97]. During exercise, an increase in cortical thickness due to load-induced periosteal apposition and, to a lesser extent, due to reduced endocortical resorption, will increase the resistance of a bone to bending [90]. However, most of the adult trials have used DXA to examine bone changes after exercise. It should be noted that using aBMD as measured by DXA leads to concerns regarding the inherent inaccuracies of this method for measurement. Further to this, bone strength is determined by not only bone mass but also bone size, shape, structure, and the material properties of collagen [98]. Because DXA captures only the bone mass, which accounts for a portion of bone strength, it has been argued that DXA-based exercise studies could underestimate the actual effects of mechanical loading on bone [99]. Considering that most of the beneficial effects of exercise in adult bones are characterized by changes in geometry, DXA is inadequate to provide information regarding important determinants of bone strength [100]. Hip geometry, which evaluates the bone macroarchitecture, can be assessed using a software program based on DXA images [101]. In a recent study using 3D hip software for femur geometry analysis, high-intensity RE combined with impact training showed significant improvements in the cortical thickness and bone mineral contents in the femur neck [102]. However, because hip structure analysis is also based on DXA hip images, inherent limitations of DXA still remain with this technique.
Consequently, there is a growing interest in using other bone imaging modalities such as quantitative computed tomography (QCT) to assess bone strength. QCT can help differentiate between cortical and trabecular compartments of bone, and their relative contribution to bone strength in vivo. In middle-aged and older men, an 18-month RE with weight-bearing impact activity showed significant increases in section modulus using QCT, which is regarded as an indicator of bone strength, cross-sectional area and aBMD at the femur neck [78]. Similarly, in a study conducted by Liu-Ambrose et al. [79], a significant increase was observed in the cortical bone density at the shaft region of both the tibia and radius in the peripheral QCT (pQCT) despite of no significant changes in the DXA measurements, in older women following a 6-month RE intervention. These results suggest the beneficial effect of RE on the cortical porosity with aging.
Unlike the cortical compartment, little is known regarding the impact of RE on trabecular bone compartment. The recently adopted lumbar spine trabecular bone score is a novel texture parameter for the assessment of trabecular bone microarchitecture based on the spinal DXA images through the measurement of pixel gray-level variations [103]. Furthermore, whether RE could increase volumetric BMD (vBMD) is still lack of evidence. A systemic review and meta-analysis of the effects of exercise on bone geometry and vBMD in postmenopausal women suggested exercise may decrease bone loss by maintaining cortical and trabecular vBMD [104]. However, all of six randomized controlled trials identified in the study had small sample sizes and were quite heterogeneous in terms of duration, type and intensity of exercise. Moreover, only two studies examined the effects of RE on vBMD, and there was no significant differences of pQCT parameters between RE group and control group in those studies [79,105]. To better understand the effect of RE on vBMD, further studies of longer duration and larger sample sizes will be required.
CONCLUSIONS
Exercise training, especially RE, is important for the maintenance of musculoskeletal health in an aging society. RE stimulates MPS by activating a PI3K-Akt-mTORC1 signaling pathway. It also exerts a mechanical load on bones consequently leading to increase in the bone strength. Based on the available information, RE, either alone or in combination with other interventions, may be the most optimal strategy to improve the muscle and bone mass in postmenopausal women, middle-aged men, or even the older population. Particularly, RE seems to be beneficial for the cortical bone. However, several concerns regarding the effects of RE on the musculoskeletal system remain to be addressed. RE is seldom prescribed with evidence-based criteria as there are no data on the anti-fracture effect of RE. Furthermore, the quantitative and qualitative adaptations of the nutrition therapy to exercise are largely ignored by the healthcare professionals. Therefore, further studies are needed to make rational, evidence-based choices and to make RE interventions feasible and effective, in particular, in older populations with compromised bone health due to sarcopenia and in those with a history of fragility fractures. To understand the differential effects of RE on the younger and older adults, the underlying mechanism of the anabolic resistance should be elucidated. In addition, if a sophisticated molecular mechanism related to the increasing muscle and bone mass due to RE can be identified in the future, it would be helpful to discover the novel therapeutic targets for osteosarcopenia.
ACKNOWLEDGMENTS
This work was supported by grants from the National Research Foundation of Korea (2017R1A2B2004708) and from Promising-Pioneering Researcher Program through Seoul National University (2017).
Notes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.