Articles
- Page Path
- HOME > Endocrinol Metab > Volume 30(3); 2015 > Article
-
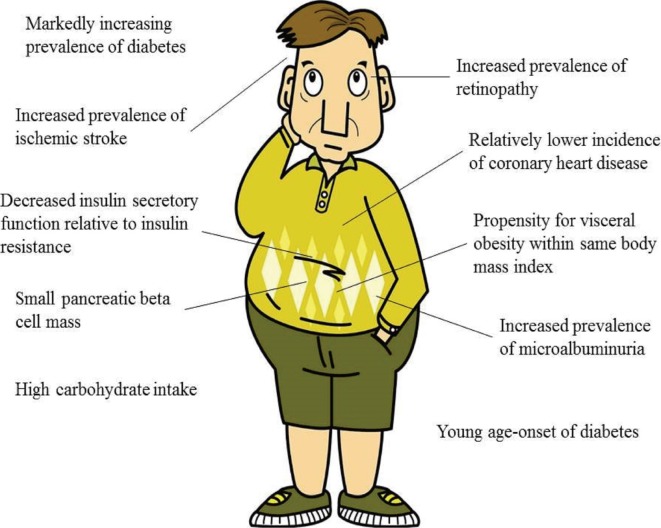
Review ArticleDiabetes in Asians
- Eun-Jung Rhee
-
Endocrinology and Metabolism 2015;30(3):263-269.
DOI: https://doi.org/10.3803/EnM.2015.30.3.263
Published online: September 22, 2015
Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Corresponding author: Eun-Jung Rhee. Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 29 Saemunan-ro, Jongno-gu, Seoul 03181, Korea. Tel: +82-2-2001-2485, Fax: +82-2-2001-1588, hongsiri@hanmail.net
• Received: August 19, 2015 • Revised: August 23, 2015 • Accepted: August 30, 2015
Copyright © 2015 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- ABSTRACT
- INTRODUCTION
- EPIDEMIOLOGY OF DIABETES IN ASIANS
- INCREASING PREVALENCE OF OBESITY
- YOUNG AGE OF ONSET OF DIABETES
- INCREASED PROPENSITY FOR VISCERAL OBESITY
- IMPAIRED INSULIN SECRETORY CAPACITY RELATIVE TO INSULIN RESISTANCE
- LIFESTYLE, ENVIRONMENTAL, AND OTHER FACTORS
- ETHNIC DIFFERENCES IN THE DEVELOPMENT OF DIABETIC COMPLICATIONS
- DIFFERENCES IN RESPONSES TO TREATMENT
- CONCLUSIONS
- Article information
- References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Multifactorial risk factors for hospital readmissions among patients with symptoms of advanced heart failure
Chetna Malhotra, Isha Chaudhry, Yeo Khung Keong, Kheng Leng David Sim
ESC Heart Failure.2024; 11(2): 1144. CrossRef - Public awareness of war on diabetes campaign and its association with behavioural outcomes
Rajeswari Sambasivam, Edimansyah Abdin, P V AshaRani, Kumarasan Roystonn, Fiona Devi, Peizhi Wang, Eng Sing Lee, Chee Fang Sum, Mythily Subramaniam
Health Education Research.2024;[Epub] CrossRef - Extending the diabetic retinopathy screening intervals in Singapore: methodology and preliminary findings of a cohort study
Amudha Aravindhan, Eva K. Fenwick, Aurora Wing Dan Chan, Ryan Eyn Kidd Man, Ngiap Chuan Tan, Wei Teen Wong, Wern Fern Soo, Shin Wei Lim, Sabrina Yi-Mei Wee, Charumathi Sabanayagam, Eric Finkelstein, Gavin Tan, Haslina Hamzah, Bibhas Chakraborty, Sanchalik
BMC Public Health.2024;[Epub] CrossRef - Increased risk of incident diabetes after therapy with immune checkpoint inhibitor compared with conventional chemotherapy: A longitudinal trajectory analysis using a tertiary care hospital database
Minyoung Lee, Kyeongseob Jeong, Yu Rang Park, Yumie Rhee
Metabolism.2023; 138: 155311. CrossRef - β-hydroxybutyrate as a biomarker of β-cell function in new-onset type 2 diabetes and its association with treatment response at 6 months
Minyoung Lee, Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes & Metabolism.2023; 49(4): 101427. CrossRef - Diabetic retinopathy as a potential risk factor for ptosis: A 13-year nationwide population-based cohort study in Taiwan
Chun-Ju Lin, Alan Y. Hsu, Peng-Tai Tien, Cheng-Hsien Chang, Chun-Ting Lai, Ning-Yi Hsia, Yu-Cih Yang, Henry Bair, Huan-Sheng Chen, Wen-Lu Chen, Yi-Yu Tsai
Frontiers in Epidemiology.2023;[Epub] CrossRef - Factors contributing to the adverse drug reactions associated with the dipeptidyl peptidase-4 (DPP-4) inhibitors: A scoping review
Swetha R. Reghunath, Muhammed Rashid, Viji Pulikkel Chandran, Girish Thunga, K.N. Shivashankar, Leelavathi D. Acharya
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(7): 102790. CrossRef - Perils and Pitfalls With Associations in Heart Failure, Particularly in HF-pEF
Peter E. Carson
JACC: Asia.2023; 3(4): 622. CrossRef - Efficacy and safety of luseogliflozin in Caucasian patients with type 2 diabetes: results from a phase III, randomized, placebo-controlled, clinical trial
Marina Shestakova, Boris Kvasnikov, Ekaterina Erina, Elena Isachenko, Alexander Andreev
BMJ Open Diabetes Research & Care.2023; 11(3): e003290. CrossRef - Assessment of the Risk of Type 2 Diabetes Mellitus Among a Rural Population in South India Using the Indian Diabetic Risk Score
Angeline Jeyaseeli V, Ganesan R, Dhibika Mathivanan, Allen Prabagaran P
Cureus.2023;[Epub] CrossRef - Association of skeletal muscle mass and risk of hypertension in Korean adults: secondary analysis of data from the community-based prospective cohort study
So Young Bu
Frontiers in Nutrition.2023;[Epub] CrossRef - Metabolically unhealthy individuals, either with obesity or not, have a higher risk of critical coronavirus disease 2019 outcomes than metabolically healthy individuals without obesity
Nam Hoon Kim, Kyeong Jin Kim, Jimi Choi, Sin Gon Kim
Metabolism.2022; 128: 154894. CrossRef - Cardiovascular disease prediction model for Indonesian adult population with prediabetes and diabetes mellitus: The Bogor Cohort study of Noncommunicable Diseases Risk Factors
Marcel H.R. Sibarani, Ika P. Wijaya, Aulia Rizka, Pradana Soewondo, Woro Riyadina, Ekowati Rahajeng, Sudikno, Dante S. Harbuwono, Dicky L. Tahapary
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(1): 102330. CrossRef - One‐year trends from the LANDMARC trial: A 3‐year, pan‐India, prospective, longitudinal study on the management and real‐world outcomes of type 2 diabetes mellitus
Ashok K. Das, Sanjay Kalra, Shashank Joshi, Ambrish Mithal, Prasanna Kumar K. M., Ambika G. Unnikrishnan, Hemant Thacker, Bipin Sethi, Subhankar Chowdhury, Romik Ghosh, Sukanya Krishnan, Arjun Nair, Senthilnathan Mohanasundaram, Shalini K. Menon, Vaibhav
Endocrinology, Diabetes & Metabolism.2022;[Epub] CrossRef - Genistein—Opportunities Related to an Interesting Molecule of Natural Origin
Ewa Garbiec, Judyta Cielecka-Piontek, Magdalena Kowalówka, Magdalena Hołubiec, Przemysław Zalewski
Molecules.2022; 27(3): 815. CrossRef - Association of ADIPOQ Single-Nucleotide Polymorphisms with the Two Clinical Phenotypes Type 2 Diabetes Mellitus and Metabolic Syndrome in a Kinh Vietnamese Population
Steven Truong, Nam Quang Tran, Phat Tung Ma, Chi Khanh Hoang, Bao Hoang Le, Thang Dinh, Luong Tran, Thang Viet Tran, Linh Hoang Gia Le, Hoang Anh Vu, Thao Phuong Mai, Minh Duc Do
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 307. CrossRef - Increasing Age Associated with Higher Dipeptidyl Peptidase-4 Inhibition Rate Is a Predictive Factor for Efficacy of Dipeptidyl Peptidase-4 Inhibitors
Sangmo Hong, Chang Hee Jung, Song Han, Cheol-Young Park
Diabetes & Metabolism Journal.2022; 46(1): 63. CrossRef - COVID-19 Independent Risk Factors for Unfavorable Disease Progression: A Cross-Sectional Study from Romania
Ruxandra Laza, Voichita Elena Lazureanu, Virgil Filaret Musta, Narcisa Daniela Nicolescu, Corina Vernic, Anca Tudor, Roxana Critu, Laura Vilceanu, Roxana Paczeyka, Valerica Bica Profir, Adelina Raluca Marinescu, Alexandra Mocanu, Talida Georgiana Cut, Dan
International Journal of General Medicine.2022; Volume 15: 2025. CrossRef - Trends in Prediabetes and Non-Alcoholic Fatty Liver Disease Associated with Abdominal Obesity among Korean Children and Adolescents: Based on the Korea National Health and Nutrition Examination Survey between 2009 and 2018
Kyungchul Song, Goeun Park, Hye Sun Lee, Myeongseob Lee, Hae In Lee, Jungmin Ahn, Eunbyoul Lee, Han Saem Choi, Junghwan Suh, Ahreum Kwon, Ho-Seong Kim, Hyun Wook Chae
Biomedicines.2022; 10(3): 584. CrossRef - Risk and Risk Factors for Postpartum Type 2 Diabetes Mellitus in Women with Gestational Diabetes: A Korean Nationwide Cohort Study
Mi Jin Choi, Jimi Choi, Chae Weon Chung
Endocrinology and Metabolism.2022; 37(1): 112. CrossRef - Not Control but Conquest: Strategies for the Remission of Type 2 Diabetes Mellitus
Jinyoung Kim, Hyuk-Sang Kwon
Diabetes & Metabolism Journal.2022; 46(2): 165. CrossRef - Mobile Text Message Design and Delivery Preferences of Patients with Type 2 Diabetes: A Social Marketing Approach
Cigdem Sahin, Karen L. Courtney, P. J. Naylor, Ryan E. Rhodes
Journal of Technology in Behavioral Science.2022; 7(4): 415. CrossRef - Unmet Needs of Glycaemic Control and Risk Factors of Residual Hyperglycaemia in a Chinese Population with Type 2 Diabetes Initiating Basal Insulin: A Post Hoc Analysis of the FPG GOAL Study
Xin Wang, Guangyu Wu, Dan Shen, Xia Zhang, Wenying Yang
Advances in Therapy.2022; 39(6): 2820. CrossRef - Type 2 diabetes epidemic and key risk factors in Qatar: a mathematical modeling analysis
Susanne F Awad, Amine A Toumi, Kholood A Al-Mutawaa, Salah A Alyafei, Muhammad A Ijaz, Shamseldin A H Khalifa, Suresh B Kokku, Amit C M Mishra, Benjamin V Poovelil, Mounir B Soussi, Katie G El-Nahas, Abdulla O Al-Hamaq, Julia A Critchley, Mohammed H Al-Th
BMJ Open Diabetes Research & Care.2022; 10(2): e002704. CrossRef - Identification of Type 2 Diabetes Risk and the Impact of Nutrition Education Among College Lecturers
M. Vijayalaks, T. Sivapriya
Journal of Applied Sciences.2022; 22(3): 117. CrossRef - The burden and risks of emerging complications of diabetes mellitus
Dunya Tomic, Jonathan E. Shaw, Dianna J. Magliano
Nature Reviews Endocrinology.2022; 18(9): 525. CrossRef - Practical Guidance on Basal Insulin Initiation and Titration in Asia: A Delphi-Based Consensus
Siew Pheng Chan, Azizul Hasan Aamir, Yong Mong Bee, Chaicharn Deerochanawong, Elizabeth Paz-Pacheco, Fatma Tiu, Siew Hui Foo, Kevin E. K. Tan, Toan Q. Le, Made Ratna Saraswati, Pongamorn Bunnag, Roy Panusunan Sibarani, Syed Abbas Raza, Nam Quang Tran
Diabetes Therapy.2022; 13(8): 1511. CrossRef - Crisis of the Asian gut: associations among diet, microbiota, and metabolic diseases
Phatthanaphong THERDTATHA, Akari SHINODA, Jiro NAKAYAMA
Bioscience of Microbiota, Food and Health.2022; 41(3): 83. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Asian Best Practices for Care of Diabetes in Elderly (ABCDE)
Sanjay Kalra, Minakshi Dhar, Faria Afsana, Pankaj Aggarwal, Than Than Aye, Ganapathy Bantwal, Manash Barua, Saptarshi Bhattacharya, Ashok Kumar Das, Sambit Das, Arundhati Dasgupta, Guruprasad Dhakal, Atul Dhingra, Fatemeh Esfahanian, Sharvil Gadve, Jubbin
Review of Diabetic Studies.2022; 18(2): 100. CrossRef - Lifestyle factors associated with muscle quality in community‐dwelling older people with type 2 diabetes in Japan and Taiwan: a cross‐sectional study
Yuko Yamaguchi, Chieko Greiner, Shu‐Chun Lee, Hirochika Ryuno, Hsin‐Yen Yen, Chiou‐Fen Lin, Ting‐I Lee, Pi‐Hsia Lee
Psychogeriatrics.2022; 22(5): 736. CrossRef - Assessment of the relationship between prediabetes and low skeletal mass based on blood creatinine level
S. I. Ibragimova, G. O. Nuskabayeva, Z. N. Shalkharova, K. Zh. Sadykova, G. A. Junusbekova, M. Oran
Diabetes mellitus.2022; 25(3): 226. CrossRef - Challenges in the diagnosis of insulin resistance: Focusing on the role of HOMA-IR and Tryglyceride/glucose index
Dicky Levenus Tahapary, Livy Bonita Pratisthita, Nissha Audina Fitri, Cicilia Marcella, Syahidatul Wafa, Farid Kurniawan, Aulia Rizka, Tri Juli Edi Tarigan, Dante Saksono Harbuwono, Dyah Purnamasari, Pradana Soewondo
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(8): 102581. CrossRef - Diabetes Prevalence, Risk Factors, and Care in Asian American and Pacific Islanders of Texas: Data From the 2015–2019 Behavioral Risk Factors Surveillance System
Angelina P. Nguyen, Alona D. Angosta, Weiming Ke, Thy M. Khong, Connie C. Tran, Miyong T. Kim
The Science of Diabetes Self-Management and Care.2022; 48(5): 387. CrossRef - Aldehyde Dehydrogenase 2 Activator Augments the Beneficial Effects of Empagliflozin in Mice with Diabetes-Associated HFpEF
Guodong Pan, Bipradas Roy, Shailendra Giri, David E. Lanfear, Rajarajan A. Thandavarayan, Ashrith Guha, Pablo A. Ortiz, Suresh Selvaraj Palaniyandi
International Journal of Molecular Sciences.2022; 23(18): 10439. CrossRef - Insulin secretion and action with increasing age - A comparison between Middle Eastern immigrants and native Swedes
Nadine Fadhel Dhaher, Nael Shaat, Anton Nilsson, Louise Bennet
Heliyon.2022; 8(10): e10913. CrossRef - Spatial association of socio-demographic, environmental factors and prevalence of diabetes mellitus in middle-aged and elderly people in Thailand
Suparat Tappo, Wongsa Laohasiriwong, Nattapong Puttanapong
Geospatial Health.2022;[Epub] CrossRef - Association of KCNJ11 and ABCC8 single-nucleotide polymorphisms with type 2 diabetes mellitus in a Kinh Vietnamese population
Nam Quang Tran, Steven D. Truong, Phat Tung Ma, Chi Khanh Hoang, Bao Hoang Le, Thang Tat Ngo Dinh, Luong Van Tran, Thang Viet Tran, Linh Hoang Gia Le, Khuong Thai Le, Hien Thanh Nguyen, Hoang Anh Vu, Thao Phuong Mai, Minh Duc Do
Medicine.2022; 101(46): e31653. CrossRef - Nutritional Quality of Gluten-Free Bakery Products Labeled Ketogenic and/or Low-Carb Sold in the Global Market
Nicola Gasparre, Antonella Pasqualone, Marina Mefleh, Fatma Boukid
Foods.2022; 11(24): 4095. CrossRef - Prevalence of Disease-Related Undernutrition on Hospital Admission and Its Association With Functionality and Length of Hospital Stay in Multiethnic Suriname
Geertrui A. van der Held-Horinga, Josine M. Stuber, Meerte-Sigrid MacDonald-Ottevanger, Armand R. van Kanten, Lenny M. W. Nahar-van Venrooij
Topics in Clinical Nutrition.2021; 36(1): 23. CrossRef - Diabetes among tuberculosis patients and its impact on tuberculosis treatment in South Asia: a systematic review and meta-analysis
Sanju Gautam, Nipun Shrestha, Sweta Mahato, Tuan P. A. Nguyen, Shiva Raj Mishra, Gabriele Berg-Beckhoff
Scientific Reports.2021;[Epub] CrossRef - Best Achievements in Clinical Medicine in Diabetes and Dyslipidemia in 2020
Eun-Jung Rhee, Mee-Kyung Kim, Won-Young Lee
Endocrinology and Metabolism.2021; 36(1): 41. CrossRef - The Association Between Pleural Empyema and Peripheral Arterial Disease in Younger Patients: A Retrospective National Population-Based Cohort Study
Tzu-Yuan Wang, Hsin-Hung Chen, Chun-Hung Su, Sheng-Pang Hsu, Chun-Wei Ho, Ming-Chia Hsieh, Cheng-Li Lin, Chia-Hung Kao
Frontiers in Medicine.2021;[Epub] CrossRef - Trends of Diabetes and Prediabetes Prevalence among Korean Adolescents From 2007 to 2018
Ji Hyun Kim, Jung Sub Lim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Gut Microbiome of Indonesian Adults Associated with Obesity and Type 2 Diabetes: A Cross-Sectional Study in an Asian City, Yogyakarta
Phatthanaphong Therdtatha, Yayi Song, Masaru Tanaka, Mariyatun Mariyatun, Maisaroh Almunifah, Nancy Eka Putri Manurung, Siska Indriarsih, Yi Lu, Koji Nagata, Katsuya Fukami, Tetsuo Ikeda, Yuan-Kun Lee, Endang Sutriswati Rahayu, Jiro Nakayama
Microorganisms.2021; 9(5): 897. CrossRef - Structural effects driven by rare point mutations in amylin hormone, the type II diabetes-associated peptide
Wendy S. Mendes, Octavio L. Franco, Sergio A. Alencar, William F. Porto
Biochimica et Biophysica Acta (BBA) - General Subjects.2021; 1865(8): 129935. CrossRef - Validation study of the ACS NSQIP surgical risk calculator for two procedures in Japan
Meixi Ma, Yaoming Liu, Mitsukazu Gotoh, Arata Takahashi, Shigeru Marubashi, Yasuyuki Seto, Itaru Endo, Clifford Y. Ko, Mark E. Cohen
The American Journal of Surgery.2021; 222(5): 877. CrossRef - Oral health and longitudinal changes in fasting glucose levels: A nationwide cohort study
Tae-Jin Song, Yoonkyung Chang, Jimin Jeon, Jinkwon Kim, David M. Ojcius
PLOS ONE.2021; 16(6): e0253769. CrossRef - Dose-Dependent Effect of Smoking on Risk of Diabetes Remains after Smoking Cessation: A Nationwide Population-Based Cohort Study in Korea
Se Eun Park, Mi Hae Seo, Jung-Hwan Cho, Hyemi Kwon, Yang-Hyun Kim, Kyung-Do Han, Jin-Hyung Jung, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2021; 45(4): 539. CrossRef - Liu Wei Di Huang Wan and the Delay of Insulin Use in Patients with Type 2 Diabetes in Taiwan: A Nationwide Study
Hsin-Hung Chen, Chien-Tung Wu, Yueh-Ting Tsai, Chun-Wei Ho, Ming-Chia Hsieh, Jung-Nien Lai, Kanwal Rehman
Evidence-Based Complementary and Alternative Medicine.2021; 2021: 1. CrossRef - Lixisenatide is effective and safe as add-on treatment to basal insulin in Asian individuals with type 2 diabetes and different body mass indices: a pooled analysis of data from the GetGoal Studies
Wenhuan Feng, Weimin Wang, Ran Meng, Guangyu Wu, Minlu Zhang, Xia Zhang, Huiqiu Yin, Dalong Zhu
BMJ Open Diabetes Research & Care.2021; 9(1): e002290. CrossRef - Secular Trends in Dietary Intake over a 20-Year Period in People with Type 2 Diabetes in Japan: A Comparative Study of Two Nationwide Registries; Japan Diabetes Complications Study (JDCS) and Japan Diabetes Clinical Data Management Study (JDDM)
Mizuki Takeuchi, Chika Horikawa, Mariko Hatta, Yasunaga Takeda, Rina Nedachi, Izumi Ikeda, Sakiko Morikawa, Noriko Kato, Hiroki Yokoyama, Rei Aida, Shiro Tanaka, Chiemi Kamada, Yukio Yoshimura, Toshiko Saito, Kazuya Fujihara, Atsushi Araki, Hirohito Sone
Nutrients.2021; 13(10): 3428. CrossRef - Risk of Diabetes in Subjects with Positive Fecal Immunochemical Test: A Nationwide Population-Based Study
Kwang Woo Kim, Hyun Jung Lee, Kyungdo Han, Jung Min Moon, Seung Wook Hong, Eun Ae Kang, Jooyoung Lee, Hosim Soh, Seong-Joon Koh, Jong Pil Im, Joo Sung Kim
Endocrinology and Metabolism.2021; 36(5): 1069. CrossRef - Impact of the different biliopancreatic limb length on diabetes and incretin hormone secretion following distal gastrectomy in gastric cancer patients
Ji Yeon Park, Oh Kyoung Kwon, Jae-Han Jeon, Yeon-Kyung Choi, Ki Bum Park
Scientific Reports.2021;[Epub] CrossRef - Association between body mass index and survival in Taiwanese heart failure patients with and without diabetes mellitus
Yu Ying Lu, Victor Chien Chia Wu, Pao-Hsien Chu, Chien-Te Ho, Chieh-Yu Chang
Medicine.2021; 100(48): e28114. CrossRef - Diabetes prevalence and risk factors of early-onset adult diabetes: results from the Indonesian family life survey
Justine Tanoey, Heiko Becher
Global Health Action.2021;[Epub] CrossRef - Bariatric surgery is expensive but improves co-morbidity: 5-year assessment of patients with obesity and type 2 diabetes
T Wu, S K H Wong, B T T Law, E Grieve, O Wu, D K H Tong, D K W Leung, E K W Ng, C L K Lam, C K H Wong
British Journal of Surgery.2021; 108(5): 554. CrossRef - Longitudinal Study of Diabetic Differences between International Migrants and Natives among the Asian Population
Heng Piao, Jae Moon Yun, Aesun Shin, Belong Cho
Biomolecules & Therapeutics.2020; 28(1): 110. CrossRef - History of Diabetes Mellitus and Risk of Breast Cancer in Asian Women: A Meta-Epidemiological Analysis of Population-Based Cohort Studies
Jong-Myon Bae
Journal of Menopausal Medicine.2020; 26(1): 29. CrossRef - Type 2 Diabetes and Chronic Conditions Disparities in Medicare Beneficiaries in the State of Michigan
John M. Clements, Mariana Rosca, Carla Cavallin, Shelby Falkenhagen, Thomas Ittoop, Christina K. Jung, Megan Mazzella, Joseph A. Reed, Megan Schluentz, Caleb VanDyke
The American Journal of the Medical Sciences.2020; 359(4): 218. CrossRef - Increased Mortality Burden in Young Asian Subjects with Dysglycemia and Comorbidities
Eun-Jung Rhee, Inha Jung, Hyemi Kwon, Se Eun Park, Yang-Hyun Kim, Kyung-Do Han, Yong-Gyu Park, Won-Young Lee
Journal of Clinical Medicine.2020; 9(4): 1042. CrossRef - Improved oral hygiene is associated with decreased risk of new-onset diabetes: a nationwide population-based cohort study
Yoonkyung Chang, Ji Sung Lee, Ki-Jung Lee, Ho Geol Woo, Tae-Jin Song
Diabetologia.2020; 63(5): 924. CrossRef - Serum γ-glutamyltransferase as an independent predictor for incident type 2 diabetes in middle-aged and older adults: Findings from the KoGES over 12 years of follow-up
Jun-Hyuk Lee, Hye Sun Lee, Yong-Jae Lee
Nutrition, Metabolism and Cardiovascular Diseases.2020; 30(9): 1484. CrossRef SGLT2 Inhibitors as Add-On Therapy to Metformin for People with Type 2 Diabetes: A Review of Placebo-Controlled Trials in Asian versus Non-Asian Patients
André J Scheen
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 2765. CrossRef- Introducing physiology of diabetes to American Asian middle school and high school students
Jennifer L. Zuercher, Chaya Gopalan
Advances in Physiology Education.2020; 44(4): 587. CrossRef - Nonalcoholic fatty liver disease and alcohol-related liver disease: From clinical aspects to pathophysiological insights
Kenichi Ikejima, Kazuyoshi Kon, Shunhei Yamashina
Clinical and Molecular Hepatology.2020; 26(4): 728. CrossRef - The Menstrual Disturbances in Endocrine Disorders: A Narrative Review
Marzieh Saei Ghare Naz, Marzieh Rostami Dovom, Fahimeh Ramezani Tehrani
International Journal of Endocrinology and Metabolism.2020;[Epub] CrossRef - Update on Monogenic Diabetes in Korea
Ye Seul Yang, Soo Heon Kwak, Kyong Soo Park
Diabetes & Metabolism Journal.2020; 44(5): 627. CrossRef - Is Environmental and Occupational Particulate Air Pollution Exposure Related to Type-2 Diabetes and Dementia? A Cross-Sectional Analysis of the UK Biobank
Eirini Dimakakou, Helinor J. Johnston, George Streftaris, John W. Cherrie
International Journal of Environmental Research and Public Health.2020; 17(24): 9581. CrossRef - Type 2 Diabetes Mellitus in China
Dongwan Zhu, Johanna T. Dwyer, Chung-Mei Ouyang
Nutrition Today.2020; 55(6): 304. CrossRef - Interaction between oxidative stress and diabetes: a mini-review
Royana Singh, Ashish Ashish, Arunim Shah, Shubhrendu Shekhar Pandey
Journal of Diabetes, Metabolic Disorders & Control.2020; 7(2): 58. CrossRef - “Omics” and “epi-omics” underlying the β-cell adaptation to insulin resistance
Dario F. De Jesus, Rohit N. Kulkarni
Molecular Metabolism.2019; 27: S42. CrossRef - Prevalence of Diabetes by Race and Ethnicity in the United States, 2011-2016
Yiling J. Cheng, Alka M. Kanaya, Maria Rosario G. Araneta, Sharon H. Saydah, Henry S. Kahn, Edward W. Gregg, Wilfred Y. Fujimoto, Giuseppina Imperatore
JAMA.2019; 322(24): 2389. CrossRef - History of Diabetes Mellitus and Risk of Prostate Cancer: A Meta-Epidemiological Study of Population-Based Cohort Studies in East Asian Men
Jong-Myon Bae
The Korean Journal of Urological Oncology.2019; 17(3): 119. CrossRef - Effect of canagliflozin on the overall clinical state including insulin resistance in Japanese patients with type 2 diabetes mellitus
Yoko Koike, Shin-Ichiro Shirabe, Hajime Maeda, Ayako Yoshimoto, Keiko Arai, Atsushi Kumakura, Koichi Hirao, Yasuo Terauchi
Diabetes Research and Clinical Practice.2019; 149: 140. CrossRef - Lilly Insulin Glargine Versus Lantus® in Type 2 Diabetes Mellitus Patients: India and East Asia Subpopulation Analyses of the ELEMENT 5 Study
Viswanathan Mohan, Kyu Jeung Ahn, Young Min Cho, Rakesh Kumar Sahay, Chien-Ning Huang, Sanjay Kalra, Manoj Chadha, Indranil Bhattacharya, So Yeon Kim, Erik Spaepen
Clinical Drug Investigation.2019; 39(8): 745. CrossRef - Lilly Insulin Glargine Versus Lantus® in Insulin-Naïve and Insulin-Treated Adults with Type 2 Diabetes: A Randomized, Controlled Trial (ELEMENT 5)
Robyn K. Pollom, Liza L. Ilag, Lyndon B. Lacaya, Tina M. Morwick, Ramón Ortiz Carrasquillo
Diabetes Therapy.2019; 10(1): 189. CrossRef - International comparison of trends in patients commencing renal replacement therapy by primary renal disease
Vianda S Stel, Ryan Awadhpersad, Maria Pippias, Manuel Ferrer‐Alamar, Patrik Finne, Simon D Fraser, James G Heaf, Marc H Hemmelder, Alberto Martínez‐Castelao, Johan de Meester, Runolfur Palsson, Friedrich C Prischl, Mårten Segelmark, Jamie P Traynor, Rafa
Nephrology.2019; 24(10): 1064. CrossRef - Relation between Baseline Height and New Diabetes Development: A Nationwide Population-Based Study
Eun-Jung Rhee, Jung-Hwan Cho, Hyemi Kwon, Se-Eun Park, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Won-Young Lee
Diabetes & Metabolism Journal.2019; 43(6): 794. CrossRef - An update on the safety and efficacy of oral antidiabetic drugs: DPP-4 inhibitors and SGLT-2 inhibitors
Elizabeth Mary Lamos, Maka Hedrington, Stephen N Davis
Expert Opinion on Drug Safety.2019; 18(8): 691. CrossRef - Associations of physical activity levels and screen time with oral glucose tolerance test profiles in Singaporean women of reproductive age actively trying to conceive: the S‐PRESTO study
J. Y. Bernard, S. Ng, P. Natarajan, S. L. Loy, I. M. Aris, M. T. Tint, Y.‐S. Chong, L. Shek, J. Chan, K. M. Godfrey, C. M. Khoo, M. K.‐S. Leow, F. Müller‐Riemenschneider, S.‐Y. Chan
Diabetic Medicine.2019; 36(7): 888. CrossRef - Prevalence of diabetic micro vascular complications at a tertiary care unit of Karachi, Pakistan
Mujeeb Abro, Awn Bin Zafar, Asher Fawwad, Nida Mustafa, Bilal Tahir, Musarrat Riaz, Abdul Basit
International Journal of Diabetes in Developing Countries.2019; 39(2): 325. CrossRef - Physical and sensory characterisation of noodles with added native and denatured pea protein isolate
M.S.M. Wee, D.E. Loud, V.W.K. Tan, C.G. Forde
Food Chemistry.2019; 294: 152. CrossRef - Adverse Drug Reaction Profile of SGLT2 Inhibitor-Associated Diabetic Ketosis/Ketoacidosis in Singapore and their Precipitating Factors
Michael Limenta, Christine S. C. Ho, Jalene W. W. Poh, Su-Yen Goh, Dorothy S. L. Toh
Clinical Drug Investigation.2019; 39(7): 683. CrossRef - MILLETS IN METABOLIC SYNDROME- TIME TO TAP THE POTENTIAL
Akshay Rao, Divya Prabhu, Vishwanath Krishnamurthy, Anil Kumar Thimmaiah
Journal of Evidence Based Medicine and Healthcare.2019; 6(17): 1284. CrossRef - Location of cerebral atherosclerosis: Why is there a difference between East and West?
Jong S Kim, Yeon-Jung Kim, Sung-Ho Ahn, Bum J Kim
International Journal of Stroke.2018; 13(1): 35. CrossRef - Precision medicine approach: Empagliflozin for diabetic cardiomyopathy in mice with aldehyde dehydrogenase (ALDH) 2 * 2 mutation, a specific genetic mutation in millions of East Asians
Guodong Pan, Mandar Deshpande, Haiyan Pang, Suresh Selvaraj Palaniyandi
European Journal of Pharmacology.2018; 839: 76. CrossRef - Type I Collagen-Derived Injectable Conductive Hydrogel Scaffolds as Glucose Sensors
Ranjithkumar Ravichandran, Jose G. Martinez, Edwin W. H. Jager, Jaywant Phopase, Anthony P. F. Turner
ACS Applied Materials & Interfaces.2018; 10(19): 16244. CrossRef - Low serum levels of High-Density Lipoprotein cholesterol (HDL-c) as an indicator for the development of severe postpartum depressive symptoms
Raji Ramachandran Pillai, Anand Babu Wilson, Nancy R. Premkumar, Shivanand Kattimani, Haritha Sagili, Soundravally Rajendiran, Manuel Portero-Otin
PLOS ONE.2018; 13(2): e0192811. CrossRef - Sitagliptin and Fractures in Type 2 Diabetes: A Nationwide Population-Based Propensity-Matching Study
Shih-Yi Lin, Wu-Huei Hsu, Cheng-Chieh Lin, Cheng-Li Lin, Chun-Hao Tsai, Hung-Chieh Yeh, Chung-Y. Hsu, Chia-Hung Kao
Frontiers in Pharmacology.2018;[Epub] CrossRef - Clinical correlates and pharmacological management of Asian patients with concomitant diabetes mellitus and heart failure
Yvonne May Fen Chia, Tiew-Hwa Katherine Teng, Chanchal Chandramouli, Jonathan Yap, Michael MacDonald, Carolyn S. P. Lam
Heart Failure Reviews.2018; 23(3): 461. CrossRef - Increase in relative skeletal muscle mass over time and its inverse association with metabolic syndrome development: a 7-year retrospective cohort study
Gyuri Kim, Seung-Eun Lee, Ji Eun Jun, You-Bin Lee, Jiyeon Ahn, Ji Cheol Bae, Sang-Man Jin, Kyu Yeon Hur, Jae Hwan Jee, Moon-Kyu Lee, Jae Hyeon Kim
Cardiovascular Diabetology.2018;[Epub] CrossRef - Initial combination therapy with vildagliptin plus metformin in drug-naïve patients with T2DM: a 24-week real-life study from Asia
Manoj Chawla, Tae Ho Kim, Roberto C. Mirasol, Pathan Faruque, Kathryn Cooke, Peggy Hours-Zesiger, Abhijit Shete
Current Medical Research and Opinion.2018; 34(9): 1605. CrossRef - Open‐label, randomized study comparing basal insulin peglispro and insulin glargine, in combination with oral antihyperglycemic medications, in insulin‐naïve Asian patients with type 2 diabetes
Takahisa Hirose, Zhihong Cai, Kwee Poo Yeo, Makoto Imori, Kenji Ohwaki, Takeshi Imaoka
Journal of Diabetes Investigation.2018; 9(1): 100. CrossRef - Cost-Effectiveness of the Interventions to Avoid Complications and Management in Diabetes Mellitus: A Narrative Review from South-East Asian Perspective
Shazia Qasim Jamshed, Akshaya Srikanth Bhagavathula, Abdul Kareem Al-Shami
Romanian Journal of Diabetes Nutrition and Metabolic Diseases.2018; 25(2): 197. CrossRef - Understanding Cultural Influences on Dietary Habits in Asian, Middle Eastern, and Latino Patients with Type 2 Diabetes: A Review of Current Literature and Future Directions
Natalie Mora, Sherita Hill Golden
Current Diabetes Reports.2017;[Epub] CrossRef - Diabetes prevention in the real world: Insights from the JDPP and J‐DOIT1
Naoki Sakane
Journal of General and Family Medicine.2017; 18(6): 325. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - How to PrepareEndocrinology and Metabolismfor Reapplication to MEDLINE
Sun Huh
Endocrinology and Metabolism.2017; 32(1): 58. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Prevalences and Management of Diabetes and Pre-diabetes among Korean Teenagers and Young Adults: Results from the Korea National Health and Nutrition Examination Survey 2005–2014
Eun-Hee Cho, Dayeon Shin, Keun-Hyok Cho, Junguk Hur
Journal of Korean Medical Science.2017; 32(12): 1984. CrossRef -
Endocrinology and Metabolism Is Indexed in the Emerging Sources Citation Index
Won-Young Lee
Endocrinology and Metabolism.2017; 32(3): 350. CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Increased risk for diabetes development in subjects with large variation in total cholesterol levels in 2,827,950 Koreans: A nationwide population-based study
Eun-Jung Rhee, Kyungdo Han, Seung-Hyun Ko, Kyung-Soo Ko, Won-Young Lee, Yan Li
PLOS ONE.2017; 12(5): e0176615. CrossRef - Concordance the hemoglobin glycation index with glycation gap using glycated albumin in patients with type 2 diabetes
Mee Kyoung Kim, Jee Sun Jeong, Hyuk-Sang Kwon, Ki Hyun Baek, Ki-Ho Song
Journal of Diabetes and its Complications.2017; 31(7): 1127. CrossRef - Itraconazole attenuates hepatic gluconeogenesis and promotes glucose uptake by regulating AMPK pathway
Ri‑Su Na, Cong Ma, Qiao‑Rui Liu, Li‑Ming Wu, Xu‑Lei Zheng, Zhi‑Wen Liu
Experimental and Therapeutic Medicine.2017;[Epub] CrossRef - Blood Pressure Is the Determinant for the Increased Risk for Intracranial Arterial Stenosis in Subjects with Elevated Glycated Hemoglobin Levels: The Kangbuk Samsung Health Study
Hyung-Geun Oh, Eun-Jung Rhee
Journal of Stroke and Cerebrovascular Diseases.2016; 25(11): 2729. CrossRef - Discordance in the levels of hemoglobin A1C and glycated albumin: Calculation of the glycation gap based on glycated albumin level
Mee Kyoung Kim, Kyung-Jin Yun, Hyuk-Sang Kwon, Ki Hyun Baek, Ki-Ho Song
Journal of Diabetes and its Complications.2016; 30(3): 477. CrossRef - Cutoff Point of HbA1c for Diagnosis of Diabetes Mellitus in Chinese Individuals
Bing Wang, Ming-Chuan Liu, Xin-Yu Li, Xu-Han Liu, Qiu-Xia Feng, Lu Lu, Zhu Zhu, Ying-Shu Liu, Wei Zhao, Zheng-Nan Gao, Noel Christopher Barengo
PLOS ONE.2016; 11(11): e0166597. CrossRef - High Prevalence and Heterogeneity of Diabetes in Patients With TB in South India
Hardy Kornfeld, Kim West, Kevin Kane, Satyavani Kumpatla, Rajesh Roy Zacharias, Carlos Martinez-Balzano, Wenjun Li, Vijay Viswanathan
Chest.2016; 149(6): 1501. CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Geniposide alleviates depression-like behavior via enhancing BDNF expression in hippocampus of streptozotocin-evoked mice
Junming Wang, Peili Duan, Ying Cui, Qing Li, Yanran Shi
Metabolic Brain Disease.2016; 31(5): 1113. CrossRef

 KES
KES
 PubReader
PubReader Cite
Cite


