Solitary Skin Metastasis of Papillary Thyroid Carcinoma
Article information
Abstract
A solitary skin metastasis is a rare manifestation of papillary thyroid carcinoma (PTC). A 55-year-old woman presented with a movable subcutaneous nodule in her anterior neck for several months. Three years ago, she underwent total thyroidectomy and remnant ablation for classical PTC (pT3N0M0) and was under thyroxine suppression therapy without any evidence of recurrent disease. The subcutaneous nodule was 0.4 cm in size, firm, and movable without any change in the overlying skin. Recurrent PTC was confirmed after excision biopsy. Eight months after, she got a new nodule along the previous excision site. After punch biopsy, metastatic PTC was confirmed in the deep dermis and was re-excised with a clear resection margin. This is the first report of a case of solitary skin metastasis of PTC in Korea. Although solitary skin metastasis of PTC is rare, it should be considered in patients with a skin nodule.
INTRODUCTION
Papillary thyroid carcinoma (PTC) is the most common type of endocrine malignancy and cervical lymph node (LN) metastasis is very common in PTC. Distant metastasis occurs in 4% to 23% of differentiated thyroid carcinoma patients [1]. The major sites of metastatic PTC are the lung, bone, and central nervous system [2,3,4,5]. Rarely, distant metastasis to the eye, breast, liver, kidney, and muscle have been reported [2]. Skin metastasis of PTC is a rare manifestation (approximately <1%) and usually accompanied with disseminated metastatic disease [2,6]. Previously, there were only two cases of solitary skin metastasis (without evidence of metastases to other organ sites) of PTC [7,8], and we could not find any report of such this case in Korea.
Thyroid fine needle aspiration (FNA) is the standard tool for detecting thyroid cancer [9]. There are complications of FNA such as persistent pain, hematoma, infection, vasovagal reaction, and recurrent laryngeal nerve palsy [10]. Needle tract implantation of tumor cells is a complication of FNA although the incidence is very low [11]. The clinical significance of needle tract tumor implantation was ignored because tumor seeding can be surgically removed without recurrence [11].
Here, we present the case of a 55-year-old woman with a recurrent solitary skin metastasis of PTC on the right anterior neck that developed 3 years after initial therapy.
CASE REPORT
A 55-year-old woman initially complained of a palpable nodule in the right anterior neck. She had no family history of thyroid disease and no exposure to external radiation. Neck ultrasound (US) showed the approximately 3.1 cm size hypoechoic nodule with lobulation and microcalcification in the upper pole of the right thyroid lobe. There was no definite metastatic LN in the cervical area. The result of FNA cytology from the thyroid nodule revealed malignant cells of PTC.
The patient underwent total thyroidectomy with central cervical LN dissection in December 2008. The histopathology demonstrated a single PTC in the upper to middle portion of the right thyroid lobe. The tumor mass was well-demarcated and the size was 3.0 cm in the longest dimension. There was microscopic perithyroidal soft tissue extension and the external resection margin was involved by tumor in microscopic examination. There was no cervical LN metastasis among 14 removed central LNs. She was also treated with high-dose radioiodine remnant ablation (5.5 GBq). At that time, serum thyroglobulin (Tg) level was 0.08 µg/L, thyroid stimulating hormone (TSH) level was 76.8 mIU/L, and anti-Tg antibody level was 93.9 IU/L (reference range, 0 to 60). Diagnostic whole body scan (WBS) showed only a focal remnant uptake in the thyroid bed.
During follow-up, she had no evidence of recurrence based on serum stimulated Tg levels (0.08 µg/L), diagnostic WBS and neck US. After 3 years of follow-up, she presented with a palpable small nodule on the right anterior neck. The nodule was firm, elastic, nontender, and the size was 0.4×0.6 cm (Fig. 1A). After excisional biopsy, the cutaneous nodule was submitted for histopathological examination.

Gross and histological findings of solitary skin metastasis after initial surgery and radioiodine remnant ablation for papillary thyroid carcinoma (PTC). (A) A 0.4×0.6 cm sized cutaneous nodule on the anterior neck. (B, C) Histopathological findings after H&E stain of skin metastasis of PTC (×10 and ×400). (D, E) Histopathological findings after thyroid transcriptional factor 1 immunostaining (×10 and ×400). (F, G) Histopathological findings after thyroglobulin immunostaining (×10 and ×400).
The low-power view of hematoxylin and eosin (H&E) staining revealed a papillary structure surrounded by a cystic lesion in the dermis. The high-power view showed a slightly edematous fibrovascular core and tumor cells with large nuclei, nuclear grooves, and cytoplasmic pseudoinclusions (Fig. 1B, C). Immunohistochemical (IHC) staining was done and it was positive for thyroid transcription factor 1 (TTF-1) (Fig. 1D, E). The IHC staining of Tg was also positive for this lesion (Fig. 1F, G). Thus, this cutaneous nodule was confirmed as the skin metastasis of PTC.
At the time of diagnosis of the first skin metastasis, serum Tg concentration was 0.08 µg/L, anti-Tg antibody level was 74.6 IU/L with serum TSH level of 2.0 mIU/L. Immediately after the diagnosis of skin metastasis, we searched other possible metastatic lesion by neck US, chest computed tomography (CT) and an F-18 fluorodeoxyglucose positron emission tomography scan (FDG-PET). There was no evidence of local tumor recurrence or distant metastasis of PTC (Fig. 2).
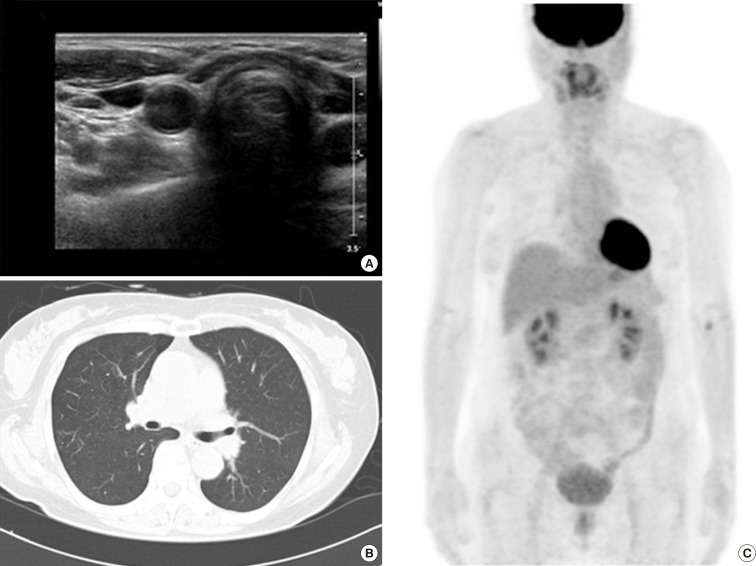
The results of imaging studies to evaluate the presence of local recurrence or distant metastasis at the time of initial skin metastasis. (A) Neck ultrasound findings. (B) Chest computed tomography. (C) F-18 fluorodeoxyglucose positron emission tomography scan.
Eight months after excision of the skin metastasis, she complained of a new palpable single nodule that was adjacent to the previous excisional biopsy site. Punch biopsy was performed and the pathological examination revealed a new metastatic PTC in the deep dermis. Neck US showed a 0.4 cm sized low echoic nodular lesion in the subcutaneous layer of the right anterior neck. There was increased vascularity in this nodular lesion in Doppler US. There was no evidence of any other local tumor recurrence or cervical LN metastasis. The patient underwent excision of the recurrent lesion, which was 0.3 cm in diameter and was confirmed as metastic PTC with a clear resection margin. After excision of the recurrent lesion, she did not have any evidence of recurrence during 4 months of follow-up.
DISCUSSION
Skin metastasis from PTC is a rare manifestation and the majority are located in the head and neck areas [12]. In 1964, skin metastasis of PTC was first reported [6]. One study reported only six cases of skin metastases from 731 patients with PTC (lesser than 1%) [13]. The scalp is the most common site of skin metastases [6]. Patients with skin metastases of PTC usually accompanied with disseminated disease and had poor prognosis [2,6]. The average survival periods of patients with skin metastases of thyroid cancer was only 19 months in 43 cases from 1964 to 1996 [6].
The skin metastatic deposits of PTC typically present as slowly growing erythematous or flesh colored nodules [14]. Definitive identification of these nodules requires an index of suspicion, and skin biopsy including IHC stains [3,7,12]. Surgical excision was done in most cases of skin metastases [8]. Additional treatment approaches include radioactive iodine, appropriate suppressive therapy with L-thyroxine, and external radiation therapy to the localized area [6].
The propensity of thyroid cancer skin metastases to localize to the upper body is documented in the majority of cases [6,12,14] and may related to local vascular factors essential for the highly complex nature of metastasis formation (initial tumor recruitment of local vasculature, followed by angiogenic switch; the tumor establishes its own vascular network through the secretion of various angiogenic factors and the removal or suppression of angiogenesis inhibitors) [15]. The rich dermal capillary network of the scalp, face, chest, and choroid may initially trap the tumor cell emboli from the circulation and then provide an environment for successful formation of metastic foci [15]. However, the mechanism of solitary skin metastasis of PTC has not yet to be fully proven.
In this report, we showed a rare case of recurrent solitary skin metastasis of PTC without any evidence of recurrent or metastatic disease elsewhere. Previously, there had been only two cases of solitary skin metastasis of PTC [7,8]. In one report, an 82-year-old man presented with a 4 cm, painless subcutaneus nodule on the neck at 11 years after initial treatment of PTC [7]. In pathological examination, this lesion was identified as metastatic PTC with strong nuclear TTF-1 reactivity and focal cytoplasmic Tg staining. She had no other evidence of disseminated disease. In the other report, a 69-year-old woman had a 4.4 mm sized small solid subcutaneous nodule on surgical cicatrix of the neck US at 10 years after initial treatment of PTC [8]. Nine years later, this skin lesion appeared remarkably enlarged (11.5 ×6.1×9.6 mm) and pathological examination revealed a metastasis of PTC. There was no evidence of distant metastasis in posttherapeutic WBS after adjuvant radioiodine therapy [8]. In these cases, however, there was no information about the presence of initial cervical LN metastasis and serum Tg concentration in follow-up periods. In this case, there was no cervical LN metastasis among 14 removed central LNs at initial diagnosis. During follow-up, she had no evidence of recurrence based on serum stimulated Tg levels (0.08 µg/L), diagnostic WBS and neck US. Furthermore, she had no any evidence of distant metastasis by neck US, chest CT, and FDG-PET at that time. As far as we know, this is the first case report with solitary skin metastasis of PTC in Korea.
We considered the possibility that the skin nodule was a needle tract implantation. However, it is impossible to distinguish between spontaneous skin metastasis and needle tract implantation [11]. There are some cases of needle tract implantation of thyroid cancer after diagnostic thyroid FNA. In one study, there were seven cases (0.14%) of needle tract implantation of PTC among 4,912 patients who were diagnosed as PTC after FNA at Kuma Hospital in Japan [16]. In most cases, the tumor seeding can be surgically removed without recurrence and there is no apparent association with the tumor seeding and prognosis of PTC [11,16].
A previous study suggested that some clinicopathological findings are more relevant to needle tract implantation than metastasis [10]. These include: (1) recurrence at the site of FNB; (2) linear arrangement of the skin and/or muscular seeding(s) and a thyroid nodule; (3) implanted tumor location away from the surgical incision; (4) absence of capsular or vascular invasion or nodal/distant metastasis; (5) existence of scar tissue surrounding the implant; (6) absence of lymphoid or neurovascular tissue (which rules out the possibility of lymphatic metastasis or perineural invasion); and (7) a central haemorrhagic papule on the implanted lesion, suggestive of a previous needle injury. In our case, there was no vascular invasion, nodal/distant metastasis, and lymphoid or neurovascular tissue. Therefore, this case may be considered as needle tract implantation rather than skin metastasis.
In conclusion, it is important to include the possibility of metastatic thyroid carcinoma, although a single skin nodule presents. Solitary skin metastasis is rare but it should be considered in patients with a skin nodule, even if there was no evidence of recurrent or metastatic PTC during the follow-up.
ACKNOWLEDGMENTS
This study was supported by the Research Grant NRF-2012 R1A1A2038383 from the National Research Foundation of Korea.
Notes
No potential conflict of interest relevant to this article was reported.