Articles
- Page Path
- HOME > Endocrinol Metab > Volume 30(2); 2015 > Article
-
Review ArticleNew Directions in Chronic Disease Management
- Hun-Sung Kim1,2, Jae-Hyoung Cho1,2, Kun-Ho Yoon1,2
-
Endocrinology and Metabolism 2015;30(2):159-166.
DOI: https://doi.org/10.3803/EnM.2015.30.2.159
Published online: June 30, 2015
1Department of Medical Informatics, College of Medicine, The Catholic University of Korea, Seoul, Korea.
2Department of Endocrinology and Metabolism, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- Corresponding author: Kun-Ho Yoon. Department of Endocrinology and Metabolism, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-gu, Seoul 137-701, Korea. Tel: +82-2-2258-8262, Fax: +82-2-2258-8297, yoonk@catholic.ac.kr
• Received: May 19, 2015 • Revised: May 26, 2015 • Accepted: May 29, 2015
Copyright © 2015 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- ABSTRACT
- INTRODUCTION
- HOW CAN WE MINIMIZE THE COMPLICATIONS OF CHRONIC DISEASE AND IMPROVE THE QUALITY OF CARE?
- CLINICAL APPLICATIONS OF U-HEALTHCARE
- HEALTH ECONOMICS: HOW CAN WE REDUCE THE COST OF MEDICAL CARE?
- WHAT ARE THE LIMITATIONS OF U-HEALTHCARE?
- THE ROLE OF POLICYMAKERS
- HOW DO WE START?
- CONCLUSIONS
- ACKNOWLEDGEMENTS
- Article information
- References
ABSTRACT
- A worldwide epidemic of chronic disease, and complications thereof, is underway, with no sign of abatement. Healthcare costs have increased tremendously, principally because of the need to treat chronic complications of non-communicable diseases including cardiovascular disease, blindness, end-stage renal disease, and amputation of extremities. Current healthcare systems fail to provide an appropriate quality of care to prevent the development of chronic complications without additional healthcare costs. A new paradigm for prevention and treatment of chronic disease and the complications thereof is urgently required. Several clinical studies have clearly shown that frequent communication between physicians and patients, based on electronic data transmission from medical devices, greatly assists in the management of chronic disease. However, for various reasons, these advantages have not translated effectively into real clinical practice. In the present review, we describe current relevant studies, and trends in the use of information technology for chronic disease management. We also discuss limitations and future directions.
- The incidence of chronic disease, including diabetes mellitus, hypertension, dyslipidemia, and cardiovascular disease, has increased rapidly as industrialization becomes ubiquitous [12]. The worldwide diabetic population is projected to increase from 366 million in 2011 to 552 million in 2030 [3]. Diabetes is already a major healthcare burden; the annual mortality is estimated to be 4.6 million [4]. In South Korea, the prevalence of diabetes among adults aged 30 years or over is about 12.4%, and the estimated number of diabetic subjects 4 million [5]. It is essential to improve medical services to ensure effective high-quality medical treatment; this obviously increases both demand and cost. Further increases in the incidence of chronic disease and accompanying complications are inevitable unless the current system is changed. The social and economic expense of change must be accepted.
- In patients with chronic diseases, prevention of various complications is generally more important than treating the disease per se. However, this is extraordinarily expensive. For example, the annual cost of treating diabetic complications in the United States is 45 billion US dollar (USD) [67]. Complications can be prevented if chronically diseased patients maintain healthy lifestyles. Thus, an ideal management system would allow remote 24-hour communication between the patient and a medical support team, to jointly plan lifestyle behavior and to monitor aspects of the disease. However, this is currently impossible.
- Current healthcare systems focus on treatment-based care. A new focus on the prevention of chronic diseases is essential. Healthy high-risk subjects must be taught how to manage their lifestyles; they need information on diet and exercise. Current medical systems lack the resources to focus on lifestyles, being restricted in time, by place, and by cost. Diet and exercise interventions must be integrated into the daily lives of all diabetic patients. In South Korea, only 29.5% of such patients attain the target glycated hemoglobin (HbA1c) level (below 6.5%); diabetes management is thus generally unsuccessful.
- Driven by such needs, various U-healthcare systems have been developed and their clinical benefits assessed [891011121314]. The widely used expression "ubiquitous healthcare" (U-healthcare) combines the word "ubiquitous" (simultaneously present anytime, anywhere)" with "healthcare." U-healthcare uses fixed or mobile networking to ensure access to healthcare or medical services anywhere, at any time. U-healthcare has attracted increasing interest; it is recognized that chronic diseases require continuous management, integrated into daily life. Such diseases cannot be efficiently managed using hospital-centered treatment methods.
INTRODUCTION
- It is essential to reduce healthcare expenditure but maintain healthcare quality. Diabetic patients are at high risk of the development of various complications and are thus in need of constant management. Diabetic complications, such as cardiovascular disease, account for the major proportion of treatment costs, which can obviously be reduced by preventing the development of complications [15]. Many reports have shown that aggressive diabetes management saves medical costs [1617] and need not affect the quality of care. Prevention of complications, early treatment triggered by close monitoring of blood glucose levels, proactive education on diet and exercise, and regular monitoring, are all essential to manage diabetes effectively and at minimal cost. Also, detection and intensive treatment of early-stage diabetes greatly contribute to reducing the incidence and cost of long-term complications [18].
- In the United States, it has been estimated that U-healthcare could save over 457 million USD annually if the model became widely accepted [1920]. U-healthcare cannot currently replace direct consultation and treatment, but a telemonitoring or telecoaching approach to the treatment of chronic disease [212223] such as diabetes mellitus would be very helpful for patients who have already been diagnosed and treated in hospital. Regular hospital visits would continue, but health at home would be managed via telemonitoring or telecoaching using simple electronic devices. Patients remain connected to their physicians and receive medical assistance as needed. Such a system would be useful when lifestyle management is important, as is true of patients with diabetes mellitus.
- The clinical guidelines for the treatment and management of diabetes are well established. Prescriptions, and lifestyle-related health management (diet and/or exercise) can be entrusted to nurses without compromising the quality of care. Patient compliance with chronic disease management is essential [24]; customized treatment plans focusing on prevention and management rather than treatment are required. Frequent contact with a readily available management team, which may include physicians, nurses, dietitians, exercise specialists, and professionals in related fields, enhances psychological stability; this is the rationale behind "humanistic" or "whole-person" treatment. A team effort improves education and monitoring. Again, frequent communication is important, as is access to information from both the hospital and the patient's home. The patient can report frequently on his/her condition.
HOW CAN WE MINIMIZE THE COMPLICATIONS OF CHRONIC DISEASE AND IMPROVE THE QUALITY OF CARE?
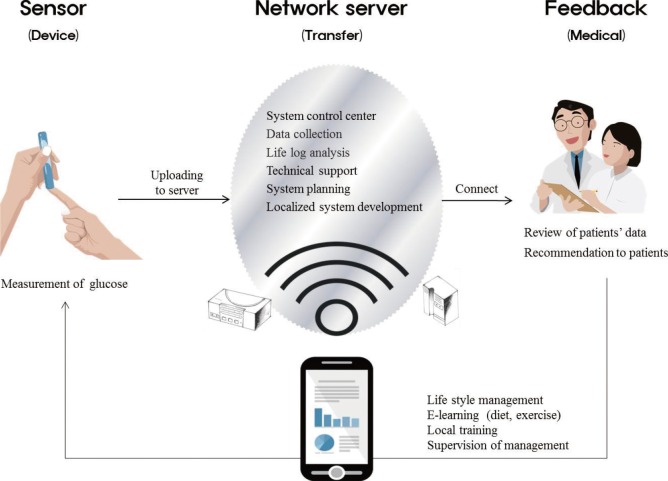
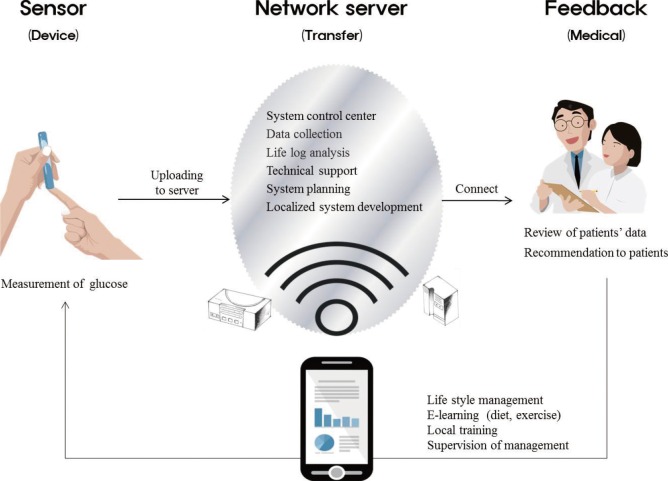
- Medical care needs to change from uni- to bi-directional. Developments in information technology (IT) and the development of many new medical devices have encouraged recent research projects on healthcare communication [252627282930]. U-healthcare combines IT and medicine, allows contact anytime with health management and medical services, and is being introduced both domestically and internationally (primarily targeting diabetics) [31323334353637]. Patients with chronic diseases, such as diabetes or hypertension, are still required to visit medical professionals every 3 to 4 months, but U-healthcare aids in management between hospital visits. Via a mobile phone or the Internet, patient places personal information (blood sugar level, drug use, and hypoglycemic status) onto a server, and the data are then delivered to a U-healthcare center. A medical team next reads and analyzes the information, and a medical team member responds if a problem is apparent (Fig. 1) [35363738]. Many patients have already expressed the desire to participate in U-healthcare [35], and an Internet-based glucose monitoring (IBGM) system has been developed. In one study, a significant decrease in the level of HbA1c was evident in diabetic patients who used the system for 3 months; indeed, those with higher baseline HbA1c levels benefitted particularly [39]. Furthermore, a 3-month trial yielded benefits that lasted for up to 30 months [40]. Thus, IBGM not only reduced HbA1c levels but caused such levels to become stabilized. It appears that the program motivated patients to manage blood sugar levels continuously. Thus, U-healthcare was successful. Similar results have been obtained in other studies [25262728293031323334353637383940].
- To participate in IBGM, a patient must have access to a computer with an Internet connection. Thus, patients in rural areas where the Internet is not accessible, or elderly patients unfamiliar with computers or the Internet, are unable to access U-healthcare. IBGM can be performed only in urban areas with readily available Internet connections. In addition, this U-healthcare is accompanied by continual direct, personal treatment, including visits to medical professionals. Therefore, patients with poor accessibility to specialized medical institutions cannot use U-healthcare. Flexibility and accessibility must be improved to support systematic diabetes management more effectively. A new system featuring personal data assistants with inbuilt blood sugar-monitoring capacities was trialled at a public health center in a farming community with limited access to medical professionals and treatment. HbA1c levels improved significantly [41], confirming that IBGM was indeed effective at managing diabetes in a rural area with only a public health clinic. This illustrates the benefits of linking medical care to a mobile device.
CLINICAL APPLICATIONS OF U-HEALTHCARE
- The economic benefit of a U-healthcare system must become clear if the system is to be widely accepted. In other words, it must be shown that the medical and social cost reductions achieved are greater than the expenses associated with establishment, application, and maintenance of the system. Such costs include commercialization, provision of new devices, the labor of medical teams, systems maintenance, and server management. Any measure enhancing patient care and satisfaction, while minimizing personal expense, must be cost-effective [42]. Artificial intelligence systems minimizing the medical manpower necessary for effective patient management are required. Such software would maximally reduce social and medical expenses. In fact, such a program (System for Automatic Verification, or SAVE) was recently applied in clinical research, and reduced physician labor by 50%, thus affording efficiency, stability, and economic benefit. SAVE will contribute to commercialization of U-healthcare systems by reducing labor costs [43].
HEALTH ECONOMICS: HOW CAN WE REDUCE THE COST OF MEDICAL CARE?
- Provision of medical services
- Many medical institutions and their affiliated physicians lack an awareness of U-healthcare, and distrust it. Many will view a new technology such as U-healthcare negatively, particularly when this is not profitable. Incentives are required. Also, currently, a physician would be absolutely liable for any medical accident associated with U-healthcare.
- Physicians are accustomed to treating patients in their offices or hospitals. Currently, most doctors lack the experience and knowledge necessary for management of patients outside a hospital. This is particularly so when medical services are expanded to include lifestyle management (e.g., diet and exercise) and encouragement of patient compliance (e.g., with administrative requests and disease management). Doctors lacking the necessary experience will require expert medical and systems support.
- Medical service customers
- A patient may be reluctant to entrust private health-related information and health status reports to a U-healthcare system in the absence of legal standards and/or institutional support. U-healthcare credibility must be established by providing empirical evidence that engenders trust, defines any personal costs, and establishes a financial system both allowing and compelling a patient to pay reasonable costs. Investment by leading companies, and governmental promotion, are necessary.
WHAT ARE THE LIMITATIONS OF U-HEALTHCARE?
Low compliance by medical institutions and physicians
Lack of clinical trust, experience, and knowledge
- Policymakers create legal and institutional acceptance, provide essential support, and make the changes necessary for establishment of U-healthcare. The current boundaries of telemedicine must be broadened. Today, U-healthcare focuses principally on lifestyle management. The training of, and the roles played by, healthcare workers who are not physicians but, rather, nutritionists and exercise specialists, must be regulated. In addition, new specialists, such as U-healthcare nurses, must be trained, and the rules of in-house treatment, including that performed by visiting nurses, must be relaxed, particularly on military bases and in remote or medically underdeveloped areas.
- Who is liable?
- Liability is ambiguous if a medical accident not associated with diagnosis or treatment (e.g., equipment failure or a communication problem) occurs during U-healthcare. Medical professionals will refuse to engage in such care unless the law clearly places any liability elsewhere.
- Acceptance of U-healthcare by health insurance providers
- Currently, U-healthcare is not covered by many medical insurers, including the Korean national health indemnity provider. Therefore, costs fall on consumers and (some) local governments. Telemedicine will not become readily available or accepted if the care remains unrecognized by medical insurers.
- Incentives for healthcare institutions are low
- Although prevention of complications greatly aids in chronic disease management, the incentives for hospitals to prioritize such practices are low. Any emphasis on prevention and management of complications is often insignificant, except in public health programs. In some developed countries, including the United States, the United Kingdom, and Germany, the newer approach is becoming a focus of standard medical services, driven by incentives offered to medical institutions and physicians who reduce medical expenses by practicing preventative methods [44454647].
- Protection of personal health information
- U-healthcare is possible only if health information is secure but also available outside of medical institutions. The collection, handling, distribution, and use of personal health information gathered via the Internet must be safeguarded; urgent research is needed.
THE ROLE OF POLICYMAKERS
- The amount of time a patient spends with medical professional(s) is currently extremely limited. Can both lifestyle and medical needs be managed via one consultation every 3 months with a medical professional? A diabetic patient has a primary need to be healthy, and a secondary desire to make lifestyle changes after diagnosis. Demands form when financial conditions allow and the will to take action develops. As disease management changes focus from treatment of acute disease to a management-based treatment plan [12], the demand for health management may exponentially increase, but the systems in place to support the demands are inadequate. If a "low-cost" lifestyle management system were available, this would afford the opportunity to maintain and improve life, and would reduce the enormous social and economic costs of healthcare.
- How can U-healthcare be developed and implemented? This form of care, the new paradigm of chronic disease management, will require extensive innovations in medical equipment, wireless communications, computer databases, and software processing large amounts of data. The U-healthcare system has three particular requirements (Fig. 1): monitoring devices and sensors that measure biometric data; networks that transmit data; and medical analyses of, and responses to, the data. U-healthcare will be in increasing demand when all three requirements are met. Mobile devices like Smartphones and tablets are becoming ubiquitous and increasingly powerful. Sensing devices and networks will become more sophisticated, enhancing medical applications in chronic disease management. Currently, both the necessary sensing devices and networking facilities are inadequate. Evidence-based improvements and proof of successful clinical application are essential. Governments should financially support commercial concerns and hospitals that combine to empirically demonstrate the effectiveness of U-healthcare. Simultaneously, a large clinical research team should be formed. The team should include representatives of government; corporations producing and developing the necessary equipment, services, and systems; and hospitals and clinics supporting U-healthcare. Committed long-term governmental support is essential to ensure the immediate application of programs that are demonstrably effective and stable.
- Since we are bringing in a new system, we shouldn't expect that everything will go well. The process should start small and then grow rapidly. There must be more clinical trials to have definite clinical evidence. Medical staffs in hospitals have to be in charge of the clinical research and provide technical supports and patents. The government and Insurance companies should build a guideline and reward of the new system and apply them to local clinics.
HOW DO WE START?
- Although non-trivial problems remain, it is clear that U-healthcare is very attractive when diabetes is to be treated. Although not all required changes can be simultaneously introduced, it appears that some such changes will undergo clinical testing and implementation in the near future. After U-healthcare treating diabetes has pioneered, other various conditions or diseases such as hypertension [4849], obesity [505152], cardiac patients [53545556], and cancer [575859] can be similarly managed. Such initiatives will be rapidly introduced when the benefits of U-healthcare in diabetes treatment become evident.
- New forms of management of chronic disease are under development. These exploit cellular and social networks, analyze large amounts of data, and feature genomic sequencing. The entry of IT into medical treatment is inevitable; many countries are already competing to be the leader.
- Excellence and innovation are required to become globally competitive. South Korea, which has excellent IT infrastructure, can become a world leader in the field, adding to the nation's international reputation. Also, the technology may allow early diagnosis of chronic diseases, which can then be treated promptly, reducing the risk of later complications. U-healthcare and the associated technology will be commercially very valuable, and innovations in equipment, sensors, and communications infrastructure may be expected.
CONCLUSIONS
-
Acknowledgements
- This research was supported by the R&D Program for Society of the National Research Foundation (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2013M3C8A2A0 2078507).
ACKNOWLEDGEMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
Article information
- 1. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:1681–1688. ArticlePubMed
- 2. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129–2140. ArticlePubMed
- 3. International Diabetes Federation. International Diabetes Federation 2011 [Internet]; Brussels: International Diabetes Federation; c2014. cited 2015 Jun 3. Available from: http://www.idf.org.
- 4. International Diabetes Federation. IDF Diabetes Atlas Fifth Edition [Internet]; Brussels: International Diabetes Federation; c2014. cited 2012 Jun 25. Available from: www.diabetesatlas.org.
- 5. Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, Song KH, Won JC, Lim S, Choi SH, Jang MJ, Kim Y, Oh K, Kim DJ, Cha BY. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J 2013;37:349–357. ArticlePubMedPMC
- 6. Caro JJ, Ward AJ, O'Brien JA. Lifetime costs of complications resulting from type 2 diabetes in the U.S. Diabetes Care 2002;25:476–481. ArticlePubMed
- 7. American Diabetes Association. Economic consequences of diabetes mellitus in the U.S. in 1997. Diabetes Care 1998;21:296–309. ArticlePubMed
- 8. Kim HS, Lee KH, Kim H, Kim JH. Using mobile phones in healthcare management for the elderly. Maturitas 2014;79:381–388. ArticlePubMed
- 9. Kim HS, Hwang Y, Lee JH, Oh HY, Kim YJ, Kwon HY, Kang H, Kim H, Park RW, Kim JH. Future prospects of health management systems using cellular phones. Telemed J E Health 2014;20:544–551. ArticlePubMedPMC
- 10. Ekberg J, Timpka T, Bang M, Froberg A, Halje K, Eriksson H. Cell phone-supported cognitive behavioural therapy for anxiety disorders: a protocol for effectiveness studies in frontline settings. BMC Med Res Methodol 2011;11:3ArticlePubMedPMCPDF
- 11. Winkler S, Schieber M, Lucke S, Heinze P, Schweizer T, Wegertseder D, Scherf M, Nettlau H, Henke S, Braecklein M, Anker SD, Koehler F. A new telemonitoring system intended for chronic heart failure patients using mobile telephone technology: feasibility study. Int J Cardiol 2011;153:55–58. ArticlePubMed
- 12. Hurling R, Catt M, Boni MD, Fairley BW, Hurst T, Murray P, Richardson A, Sodhi JS. Using internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. J Med Internet Res 2007;9:e7ArticlePubMedPMC
- 13. Shetty AS, Chamukuttan S, Nanditha A, Raj RK, Ramachandran A. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS): a pilot study. J Assoc Physicians India 2011;59:711–714. PubMed
- 14. Demaerschalk BM, Vargas JE, Channer DD, Noble BN, Kiernan TE, Gleason EA, Vargas BB, Ingall TJ, Aguilar MI, Dodick DW, Bobrow BJ. Smartphone teleradiology application is successfully incorporated into a telestroke network environment. Stroke 2012;43:3098–3101. ArticlePubMed
- 15. Brown JB, Pedula KL, Bakst AW. The progressive cost of complications in type 2 diabetes mellitus. Arch Intern Med 1999;159:1873–1880. ArticlePubMed
- 16. Steffens B. Cost-effective management of type 2 diabetes: providing quality care in a cost-constrained environment. Am J Manag Care 2000;6(13 Suppl):S697–S703. PubMed
- 17. Heller SR, Clarke P, Daly H, Davis I, McCulloch DK, Allison SP, Tattersall RB. Group education for obese patients with type 2 diabetes: greater success at less cost. Diabet Med 1988;5:552–556. ArticlePubMed
- 18. Bjork S. The cost of diabetes and diabetes care. Diabetes Res Clin Pract 2001;54(Suppl 1):S13–S18. ArticlePubMed
- 19. Starren J, Hripcsak G, Sengupta S, Abbruscato CR, Knudson PE, Weinstock RS, Shea S. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) project: technical implementation. J Am Med Inform Assoc 2002;9:25–36. ArticlePubMedPMCPDF
- 20. Shea S, Starren J, Weinstock RS, Knudson PE, Teresi J, Holmes D, Palmas W, Field L, Goland R, Tuck C, Hripcsak G, Capps L, Liss D. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) Project: rationale and design. J Am Med Inform Assoc 2002;9:49–62. ArticlePubMedPMCPDF
- 21. Fingeret MC, Vidrine DJ, Arduino RC, Gritz ER. The association between body image and smoking cessation among individuals living with HIV/AIDS. Body Image 2007;4:201–206. ArticlePubMedPMC
- 22. Carroll AE, DiMeglio LA, Stein S, Marrero DG. Contracting and monitoring relationships for adolescents with type 1 diabetes: a pilot study. Diabetes Technol Ther 2011;13:543–549. ArticlePubMedPMC
- 23. Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J Med Internet Res 2012;14:e31ArticlePubMedPMC
- 24. Lim S, Kim SY, Kim JI, Kwon MK, Min SJ, Yoo SY, Kang SM, Kim HI, Jung HS, Park KS, Ryu JO, Shin H, Jang HC. A survey on ubiquitous healthcare service demand among diabetic patients. Diabetes Metab J 2011;35:50–57. ArticlePubMedPMC
- 25. Petrie KJ, Perry K, Broadbent E, Weinman J. A text message programme designed to modify patients' illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol 2012;17:74–84. ArticlePubMed
- 26. Liu WT, Huang CD, Wang CH, Lee KY, Lin SM, Kuo HP. A mobile telephone-based interactive self-care system improves asthma control. Eur Respir J 2011;37:310–317. ArticlePubMed
- 27. Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respir Med 2010;104:166–171. ArticlePubMed
- 28. Lund S, Hemed M, Nielsen BB, Said A, Said K, Makungu MH, Rasch V. Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster-randomised controlled trial. BJOG 2012;119:1256–1264. ArticlePubMed
- 29. Ly KH, Carlbring P, Andersson G. Behavioral activation-based guided self-help treatment administered through a smartphone application: study protocol for a randomized controlled trial. Trials 2012;13:62ArticlePubMedPMCPDF
- 30. Fukuoka Y, Kamitani E, Dracup K, Jong SS. New insights into compliance with a mobile phone diary and pedometer use in sedentary women. J Phys Act Health 2011;8:398–403. ArticlePubMedPMC
- 31. Bell AM, Fonda SJ, Walker MS, Schmidt V, Vigersky RA. Mobile phone-based video messages for diabetes self-care support. J Diabetes Sci Technol 2012;6:310–319. ArticlePubMedPMC
- 32. Zolfaghari M, Mousavifar SA, Pedram S, Haghani H. The impact of nurse short message services and telephone follow-ups on diabetic adherence: which one is more effective? J Clin Nurs 2012;21:1922–1931. ArticlePubMed
- 33. Curran K, Nichols E, Xie E, Harper R. An intensive insulinotherapy mobile phone application built on artificial intelligence techniques. J Diabetes Sci Technol 2010;4:209–220. ArticlePubMedPMC
- 34. Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, Earle KA. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare 2009;15:125–128. ArticlePubMed
- 35. Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communication using a mobile phone with a glucometer for glucose control in type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. J Telemed Telecare 2009;15:77–82. ArticlePubMed
- 36. Kim HS, Choi W, Baek EK, Kim YA, Yang SJ, Choi IY, Yoon KH, Cho JH. Efficacy of the smartphone-based glucose management application stratified by user satisfaction. Diabetes Metab J 2014;38:204–210. ArticlePubMedPMC
- 37. Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform 2008;77:399–404. ArticlePubMed
- 38. Cho JH, Kim HS, Han JH, Lee JH, Oh JA, Choi YH, Yoon KH. Ubiquitous diabetes management system via interactive communication based on information technologies: clinical effects and perspectives. Korean Diabetes J 2010;34:267–273. ArticlePubMedPMC
- 39. Kwon HS, Cho JH, Kim HS, Song BR, Ko SH, Lee JM, Kim SR, Chang SA, Kim HS, Cha BY, Lee KW, Son HY, Lee JH, Lee WC, Yoon KH. Establishment of blood glucose monitoring system using the internet. Diabetes Care 2004;27:478–483. ArticlePubMed
- 40. Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, Yoo SJ, Song KH, Son HS, Kim HS, Lee WC, Cha BY, Son HY, Yoon KH. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care 2006;29:2625–2631. ArticlePubMed
- 41. Cho JH, Kwon HS, Kim HS, Oh JA, Yoon KH. Effects on diabetes management of a health-care provider mediated, remote coaching system via a PDA-type glucometer and the Internet. J Telemed Telecare 2011;17:365–370. ArticlePubMed
- 42. Cho JH, Lee JH, Oh JA, Kang MJ, Choi YH, Kwon HS, Chang SA, Cha BY, Son HY, Yoon KH. Complication reducing effect of the information technology-based diabetes management system on subjects with type 2 diabetes. J Diabetes Sci Technol 2008;2:76–81. ArticlePubMedPMC
- 43. Cho JH, Choi YH, Kim HS, Lee JH, Yoon KH. Effectiveness and safety of a glucose data-filtering system with automatic response software to reduce the physician workload in managing type 2 diabetes. J Telemed Telecare 2011;17:257–262. ArticlePubMed
- 44. Busse R. Disease management programs in Germany's statutory health insurance system. Health Aff (Millwood) 2004;23:56–67. Article
- 45. Stock SA, Redaelli M, Lauterbach KW. Disease management and health care reforms in Germany: does more competition lead to less solidarity? Health Policy 2007;80:86–96. ArticlePubMed
- 46. Fleetcroft R, Parekh-Bhurke S, Howe A, Cookson R, Swift L, Steel N. The UK pay-for-performance programme in primary care: estimation of population mortality reduction. Br J Gen Pract 2010;60:e345–e352. ArticlePubMedPMC
- 47. Brink S. The Diabetes Prevention Program: how the participants did it. Health Aff (Millwood) 2009;28:57–62. ArticlePubMed
- 48. Park MJ, Kim HS, Kim KS. Cellular phone and Internet-based individual intervention on blood pressure and obesity in obese patients with hypertension. Int J Med Inform 2009;78:704–710. ArticlePubMed
- 49. Marquez Contreras E, de la Figuera von Wichmann M, Gil Guillen V, Ylla-Catala A, Figueras M, Balana M, Naval J. Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert). Aten Primaria 2004;34:399–405. ArticlePubMedPMC
- 50. Park MJ, Kim HS. Evaluation of mobile phone and Internet intervention on waist circumference and blood pressure in post-menopausal women with abdominal obesity. Int J Med Inform 2012;81:388–394. ArticlePubMed
- 51. Soureti A, Murray P, Cobain M, Chinapaw M, van Mechelen W, Hurling R. Exploratory study of web-based planning and mobile text reminders in an overweight population. J Med Internet Res 2011;13:e118ArticlePubMedPMC
- 52. Yoo HJ, Park MS, Kim TN, Yang SJ, Cho GJ, Hwang TG, Baik SH, Choi DS, Park GH, Choi KM. A Ubiquitous Chronic Disease Care system using cellular phones and the internet. Diabet Med 2009;26:628–635. ArticlePubMed
- 53. Scherr D, Kastner P, Kollmann A, Hallas A, Auer J, Krappinger H, Schuchlenz H, Stark G, Grander W, Jakl G, Schreier G, Fruhwald FM. MOBITEL Investigators. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res 2009;11:e34ArticlePubMedPMC
- 54. Wakefield BJ, Ward MM, Holman JE, Ray A, Scherubel M, Burns TL, Kienzle MG, Rosenthal GE. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemed J E Health 2008;14:753–761. ArticlePubMed
- 55. Sack S, V Hehn A, Krukenberg A, Wieneke H, Erbel R. The Herz Handy: a new telemedical service concept for heart patients. Herzschrittmacherther Elektrophysiol 2005;16:165–175. ArticlePubMedPDF
- 56. Salvador CH, Pascual Carrasco M, Gonzalez de Mingo MA, Munoz Carrero A, Marquez Montes J, Sosa Martin L, Cavero MA, Fernandez Lozano I, Monteagudo JL. Airmed-cardio: a GSM and Internet services-based system for out-of-hospital follow-up of cardiac patients. IEEE Trans Inf Technol Biomed 2005;9:73–85. ArticlePubMed
- 57. Greaney ML, Puleo E, Sprunck-Harrild K, Bennett GG, Cunningham MA, Gillman MW, Coeling M, Emmons KM. Electronic reminders for cancer prevention: factors associated with preference for automated voice reminders or text messages. Prev Med 2012;55:151–154. ArticlePubMedPMC
- 58. Maguire R, McCann L, Miller M, Kearney N. Nurse's perceptions and experiences of using of a mobile-phone-based Advanced Symptom Management System (ASyMS) to monitor and manage chemotherapy-related toxicity. Eur J Oncol Nurs 2008;12:380–386. ArticlePubMed
- 59. Kearney N, McCann L, Norrie J, Taylor L, Gray P, McGee-Lennon M, Sage M, Miller M, Maguire R. Evaluation of a mobile phone-based, advanced symptom management system (ASyMS) in the management of chemotherapy-related toxicity. Support Care Cancer 2009;17:437–444. ArticlePubMedPDF
References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Change in coronary heart disease hospitalization after chronic disease management: a programme policy in China
Jingmin Zhu, Wei Wang, Jun Wang, Liang Zhu
Health Policy and Planning.2023; 38(2): 161. CrossRef - Evaluating the effect of the COVID-19 pandemic on hypertension and diabetes care in South Korea: an interrupted time series analysis
Boram Sim, Sunmi Kim, Eun Woo Nam
BMC Public Health.2023;[Epub] CrossRef - Towards Telemedicine Adoption in Korea: 10 Practical Recommendations for Physicians
Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - A family nurse-led intervention for reducing health services’ utilization in individuals with chronic diseases: The ADVICE pilot study
Serenella Savini, Paolo Iovino, Dario Monaco, Roberta Marchini, Tiziana Di Giovanni, Giuseppe Donato, Ausilia Pulimeno, Carmela Matera, Giuseppe Quintavalle, Carlo Turci
International Journal of Nursing Sciences.2021; 8(3): 264. CrossRef - Palmitoylethanolamide: A Natural Compound for Health Management
Paul Clayton, Mariko Hill, Nathasha Bogoda, Silma Subah, Ruchitha Venkatesh
International Journal of Molecular Sciences.2021; 22(10): 5305. CrossRef - Lack of Acceptance of Digital Healthcare in the Medical Market: Addressing Old Problems Raised by Various Clinical Professionals and Developing Possible Solutions
Jong Il Park, Hwa Young Lee, Hyunah Kim, Jisan Lee, Jiwon Shinn, Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Lessons from Temporary Telemedicine Initiated owing to Outbreak of COVID-19
Hun-Sung Kim
Healthcare Informatics Research.2020; 26(2): 159. CrossRef - Using Goal-Directed Design to Create a Mobile Health App to Improve Patient Compliance With Hypertension Self-Management: Development and Deployment
Huilong Duan, Zheyu Wang, Yumeng Ji, Li Ma, Fang Liu, Mingwei Chi, Ning Deng, Jiye An
JMIR mHealth and uHealth.2020; 8(2): e14466. CrossRef - Physical Activity for Prevention and Management of Sleep Disturbances
Ah Reum Jung, Jong Il Park, Hun-Sung Kim
Sleep Medicine Research.2020; 11(1): 15. CrossRef - Lessons from Use of Continuous Glucose Monitoring Systems in Digital Healthcare
Hun-Sung Kim, Kun-Ho Yoon
Endocrinology and Metabolism.2020; 35(3): 541. CrossRef - Recent Technology-Driven Advancements in Cardiovascular Disease Prevention in Korea
Jisan Lee, Hun-Sung Kim, Dai-Jin Kim
Cardiovascular Prevention and Pharmacotherapy.2019; 1(2): 43. CrossRef - Telemedicine-Based Health Coaching Is Effective for Inducing Weight Loss and Improving Metabolic Markers
Kelly E. Johnson, Michelle K. Alencar, Kathryn E. Coakley, Damon L. Swift, Nathan H. Cole, Christine M. Mermier, Len Kravitz, Fabiano T. Amorim, Ann L. Gibson
Telemedicine and e-Health.2019; 25(2): 85. CrossRef - Economical Mobile Healthcare and Wellness Application System
Mahendra Kumar Jangir, Karan Singh, Vishnu Shankar
SSRN Electronic Journal .2018;[Epub] CrossRef - Technology for Remote Health Monitoring in an Older Population: A Role for Mobile Devices
Kate Dupuis, Lia Tsotsos
Multimodal Technologies and Interaction.2018; 2(3): 43. CrossRef - Axial Myopia and Low HbA1c Level are Correlated and Have a Suppressive Effect on Diabetes and Diabetic Retinopathy
Hong Kyu Kim, Tyler Hyungtaek Rim, Jong Yun Yang, Soo Han Kim, Sung Soo Kim
Journal of Retina.2018; 3(1): 26. CrossRef - The Application of Medical Artificial Intelligence Technology in Rural Areas of Developing Countries
Jonathan Guo, Bin Li
Health Equity.2018; 2(1): 174. CrossRef - An Internet-based health gateway device for interactive communication and automatic data uploading: Clinical efficacy for type 2 diabetes in a multi-centre trial
Jae Hyoung Cho, Hun-Sung Kim, Seung Hyun Yoo, Chang Hee Jung, Woo Je Lee, Cheol Young Park, Hae Kyung Yang, Joong Yeol Park, Sung Woo Park, Kun Ho Yoon
Journal of Telemedicine and Telecare.2017; 23(6): 595. CrossRef - Impact of initial active engagement in self-monitoring with a telemonitoring device on glycemic control among patients with type 2 diabetes
Min-Kyung Lee, Kwang-Hyeon Lee, Seung-Hyun Yoo, Cheol-Young Park
Scientific Reports.2017;[Epub] CrossRef - An information and communication technology-based centralized clinical trial to determine the efficacy and safety of insulin dose adjustment education based on a smartphone personal health record application: a randomized controlled trial
Gyuri Kim, Ji Cheol Bae, Byoung Kee Yi, Kyu Yeon Hur, Dong Kyung Chang, Moon-Kyu Lee, Jae Hyeon Kim, Sang-Man Jin
BMC Medical Informatics and Decision Making.2017;[Epub] CrossRef - Satisfaction Survey on Information Technology-Based Glucose Monitoring System Targeting Diabetes Mellitus in Private Local Clinics in Korea
Hun-Sung Kim, So Jung Yang, Yoo Jin Jeong, Young-Eun Kim, Seok-Won Hong, Jae Hyoung Cho
Diabetes & Metabolism Journal.2017; 41(3): 213. CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Randomized, Open-Label, Parallel Group Study to Evaluate the Effect of Internet-Based Glucose Management System on Subjects with Diabetes in China
Hun-Sung Kim, Chenglin Sun, So Jung Yang, Lin Sun, Fei Li, In Young Choi, Jae-Hyoung Cho, Guixia Wang, Kun-Ho Yoon
Telemedicine and e-Health.2016; 22(8): 666. CrossRef - Current Clinical Status of Telehealth in Korea: Categories, Scientific Basis, and Obstacles
Hun-Sung Kim, Hyunah Kim, Suehyun Lee, Kye Hwa Lee, Ju Han Kim
Healthcare Informatics Research.2015; 21(4): 244. CrossRef

 KES
KES
 PubReader
PubReader Cite
Cite