Article type
- Page Path
- HOME > BROWSE ARTICLES > Article type
Review Articles
- Adrenal Gland
- Recent Updates on the Management of Adrenal Incidentalomas
- Seung Shin Park, Jung Hee Kim
- Endocrinol Metab. 2023;38(4):373-380. Published online August 16, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1779
- 7,005 View
- 1,417 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Adrenal incidentalomas represent an increasingly common clinical conundrum with significant implications for patients. The revised 2023 European Society of Endocrinology (ESE) guideline incorporates cutting-edge evidence for managing adrenal incidentalomas. This paper provides a concise review of the updated contents of the revised guideline. In the 2023 guideline, in patients without signs and symptoms of overt Cushing’s syndrome, a post-dexamethasone cortisol level above 50 nmol/L (>1.8 μg/dL) should be considered as mild autonomous cortisol secretion. Regarding the criteria of benign adrenal adenomas, a homogeneous adrenal mass with ≤10 Hounsfield units on non-contrast computed tomography requires no further follow-up, irrespective of its size. The updated guideline also discusses steroid metabolomics using tandem mass spectrometry to discriminate malignancy. It underscores the importance of high-volume surgeons performing adrenalectomy and emphasizes the pivotal role of a multidisciplinary team approach in deciding the treatment plan for indeterminate adrenal masses. The guideline advocates for more proactive surgical treatment for indeterminate adrenal masses in young patients (<40 years) and pregnant women. This review of the 2023 ESE guideline underscores the ongoing evolution of the adrenal incidentaloma management landscape, emphasizing the need for further research and adaptation of diagnostic and therapeutic strategies.

- Diabetes, obesity and metabolism
- Intrarenal Mechanisms of Sodium-Glucose Cotransporter-2 Inhibitors on Tubuloglomerular Feedback and Natriuresis
- Eun Sil Koh, Gheun-Ho Kim, Sungjin Chung
- Endocrinol Metab. 2023;38(4):359-372. Published online July 24, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1764
- 2,612 View
- 431 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - When sodium-glucose cotransporter-2 (SGLT2) inhibitors were first introduced a decade ago, no one expected them to have substantial effects beyond their known glucose-lowering effects, until the emergence of evidence of their robust renal and cardiovascular benefits showing that they could attenuate progression of kidney disease, irrespective of diabetes, as well as prevent the development of acute kidney injury. Still, the precise and elaborate mechanisms underlying the major organ protection of SGLT2 inhibitors remain unclear. SGLT2 inhibitors inhibit the reabsorption of sodium and glucose in the proximal tubule of the kidney and then recovers tubuloglomerular feedback, whereby SGLT2 inhibitors reduce glomerular hyperfiltration. This simple demonstration of their beneficial effects has perplexed experts in seeking more plausible and as yet undisclosed explanations for the whole effects of SGLT2 inhibitors, including metabolism reprogramming and the modulation of hypoxia, inflammation, and oxidative stress. Given that the renal benefits of SGLT2 inhibitors in patients with kidney disease but without diabetes were comparable to those seen in patients with diabetes, it may be reasonable to keep the emphasis on their hemodynamic actions. In this context, the aim of the present review is to provide a comprehensive overview of renal hemodynamics in individuals with diabetes who are treated with SGLT2 inhibitors, with a focus on natriuresis associated with the regulation of tubuloglomerular feedback and potential aquaresis. Throughout the discussion of alterations in renal sodium and water transports, particular attention will be given to the potential enhancement of adenosine and its receptors following SGLT2 inhibition.
-
Citations
Citations to this article as recorded by- Results from a cross-specialty consensus on optimal management of patients with chronic kidney disease (CKD): from screening to complications
Mustafa Arici, Samir Helmy Assaad-Khalil, Marcello Casaccia Bertoluci, Jason Choo, Yau-Jiunn Lee, Magdalena Madero, Guillermo Javier Rosa Diez, Vicente Sánchez Polo, Sungjin Chung, Teerawat Thanachayanont, Carol Pollock
BMJ Open.2024; 14(3): e080891. CrossRef - Chronic Kidney Disease and SGLT2 Inhibitors
Eun Sil Koh, Sungjin Chung
The Journal of Korean Diabetes.2024; 25(1): 16. CrossRef - Genitourinary Tract Infections in Patients Taking SGLT2 Inhibitors
Veraprapas Kittipibul, Zachary L. Cox, Supavit Chesdachai, Mona Fiuzat, JoAnn Lindenfeld, Robert J. Mentz
Journal of the American College of Cardiology.2024; 83(16): 1568. CrossRef - Synopsis of the Korean Society of Nephrology 2023 Practical Recommendations for the Management of Diabetic Kidney Disease
Sungjin Chung
The Korean Journal of Medicine.2023; 98(6): 270. CrossRef
- Results from a cross-specialty consensus on optimal management of patients with chronic kidney disease (CKD): from screening to complications

Corrigendum
- Thyroid
- Corrigendum: Abstract and Text Correction. Thyroid Stimulating Hormone Reference Range and Prevalence of Thyroid Dysfunction in the Korean Population: Korea National Health and Nutrition Examination Survey 2013 to 2015
- Won Gu Kim, Won Bae Kim, Gyeongji Woo, Hyejin Kim, Yumi Cho, Tae Yong Kim, Sun Wook Kim, Myung-Hee Shin, Jin Woo Park, Hai-Lin Park, Kyungwon Oh, Jae Hoon Chung
- Endocrinol Metab. 2023;38(3):357. Published online May 16, 2023
- DOI: https://doi.org/10.3803/EnM.2023.301
- Corrects: Endocrinol Metab 2017;32(1):106
- 1,239 View
- 60 Download

Original Articles
- Thyroid
- Thyroid Hormone Reference Intervals among Healthy Individuals In Lanzhou, China
- Yan Lu, Wen-Xia Zhang, De-Hong Li, Lian-Hua Wei, Yu-Jun Zhang, Fu-Na Shi, Shen Zhou
- Endocrinol Metab. 2023;38(3):347-356. Published online June 14, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1638
- 1,940 View
- 115 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
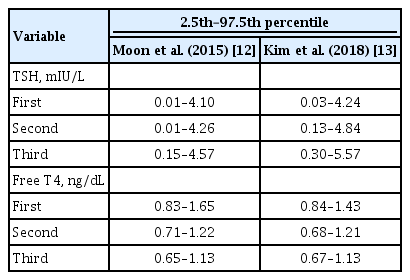
ePub - Background
The common reference intervals (RIs) for thyroid hormones currently used in China are provided by equipment manufacturers. This study aimed to establish thyroid hormone RIs in the population of Lanzhou, a city in the subplateau region of northwest China, and compare them with previous reports and manufacturer-provided values.
Methods
In total, 3,123 individuals (1,680 men, 1,443 women) from Lanzhou, an iodine-adequate area of China, perceived as healthy were selected. The Abbott Architect analyzer was used to determine the serum concentration of thyroid hormones. The 95% RI was estimated using the 2.5th and 97.5th percentiles as the lower and upper reference limits, respectively.
Results
The serum levels of thyroid-stimulating hormone (TSH), total triiodothyronine (TT3), antithyroglobulin (ATG) antibody, and antithyroid peroxidase (ATPO) antibody levels were significantly correlated with sex (P<0.05). TSH, total thyroxine (TT4), and ATPO levels were significantly correlated with age (P<0.05). The serum levels of TSH, ATG, and ATPO in men were significantly lower than in women; in contrast, the serum TT3 level was significantly higher in men than in women (P<0.05). Serum TSH, TT3, TT4, and ATG levels differed across age groups (P<0.05), but no such variation was observed for ATG levels (P>0.05). The established RIs of TSH, ATG, and ATPO in this study differed between sexes (P<0.05). The thyroid hormone RIs established herein were inconsistent with the manufacturer-provided values.
Conclusion
The RIs of thyroid hormones in the healthy population of Lanzhou were inconsistent with those in the manufacturer’s manual. Validated sex-specific values are required for diagnosing thyroid diseases.

- Thyroid
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
- Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
- Endocrinol Metab. 2023;38(3):338-346. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1664

- 1,680 View
- 100 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To determine whether baseline thyroid-stimulating immunoglobulin (TSI) bioassay or its early response upon treatment with an anti-thyroid drug (ATD) can predict prognosis of Graves’ disease (GD) in real-world practice.
Methods
This retrospective study enrolled GD patients who had previous ATD treatment with TSI bioassay checked at baseline and at follow-up from April 2010 to November 2019 in one referral hospital. The study population were divided into two groups: patients who experienced relapse or continued ATD (relapse/persistence), and patients who experienced no relapse after ATD discontinuation (remission). The slope and area under the curve at 1st year (AUC1yr) of thyroid-stimulating hormone receptor antibodies including TSI bioassay and thyrotropin-binding inhibitory immunoglobulin (TBII) were calculated as differences between baseline and second values divided by time duration (year).
Results
Among enrolled 156 study subjects, 74 (47.4%) had relapse/persistence. Baseline TSI bioassay values did not show significant differences between the two groups. However, the relapse/persistence group showed less decremental TSI bioassay in response to ATD than the remission group (–84.7 [TSI slope, –198.2 to 8.2] vs. –120.1 [TSI slope, –204.4 to –45.9], P=0.026), whereas the TBII slope was not significantly different between the two groups. The relapse/persistence group showed higher AUC1yr of TSI bioassay and TBII in the 1st year during ATD treatment than the remission group (AUC1yr for TSI bioassay, P=0.0125; AUC1yr for TBII,P =0.001).
Conclusion
Early changes in TSI bioassay can better predict prognosis of GD than TBII. Measurement of TSI bioassay at beginning and follow-up could help predict GD prognosis. -
Citations
Citations to this article as recorded by- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef
- Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study

- Diabetes, obesity and metabolism
- Efficacy of Gemigliptin Add-on to Dapagliflozin and Metformin in Type 2 Diabetes Patients: A Randomized, Double-Blind, Placebo-Controlled Study (SOLUTION)
- Byung Wan Lee, KyungWan Min, Eun-Gyoung Hong, Bon Jeong Ku, Jun Goo Kang, Suk Chon, Won-Young Lee, Mi Kyoung Park, Jae Hyeon Kim, Sang Yong Kim, Keeho Song, Soon Jib Yoo
- Endocrinol Metab. 2023;38(3):328-337. Published online June 28, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1688
- 2,341 View
- 253 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study evaluated the efficacy and safety of add-on gemigliptin in patients with type 2 diabetes mellitus (T2DM) who had inadequate glycemic control with metformin and dapagliflozin.
Methods
In this randomized, placebo-controlled, parallel-group, double-blind, phase III study, 315 patients were randomized to receive either gemigliptin 50 mg (n=159) or placebo (n=156) with metformin and dapagliflozin for 24 weeks. After the 24-week treatment, patients who received the placebo were switched to gemigliptin, and all patients were treated with gemigliptin for an additional 28 weeks.
Results
The baseline characteristics were similar between the two groups, except for body mass index. At week 24, the least squares mean difference (standard error) in hemoglobin A1c (HbA1c) changes was –0.66% (0.07) with a 95% confidence interval of –0.80% to –0.52%, demonstrating superior HbA1c reduction in the gemigliptin group. After week 24, the HbA1c level significantly decreased in the placebo group as gemigliptin was administered, whereas the efficacy of HbA1c reduction was maintained up to week 52 in the gemigliptin group. The safety profiles were similar: the incidence rates of treatment-emergent adverse events up to week 24 were 27.67% and 29.22% in the gemigliptin and placebo groups, respectively. The safety profiles after week 24 were similar to those up to week 24 in both groups, and no new safety findings, including hypoglycemia, were noted.
Conclusion
Add-on gemigliptin was well tolerated, providing comparable safety profiles and superior efficacy in glycemic control over placebo for long-term use in patients with T2DM who had poor glycemic control with metformin and dapagliflozin.

- Diabetes, obesity and metabolism
- Association between Serum Amyloid A Levels and Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis
- Ting Liu, Meng Li, Chunying Cui, Jielin Zhou
- Endocrinol Metab. 2023;38(3):315-327. Published online June 7, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1621
- 2,083 View
- 102 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
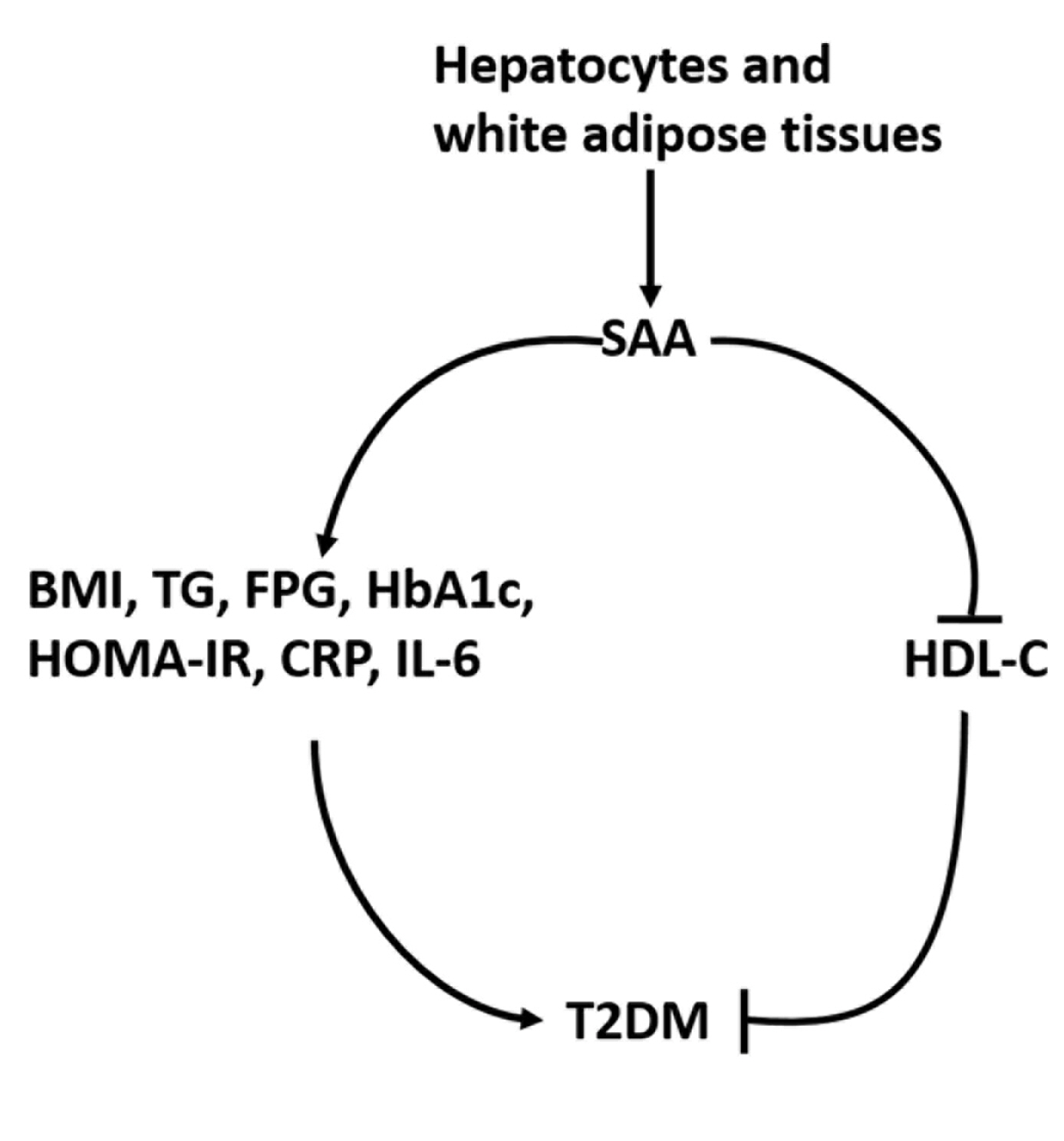
ePub - Background
To date, consistent data have not been reported on the association between serum amyloid A (SAA) levels and type 2 diabetes mellitus (T2DM). The purpose of this study was to systematically summarize their relationship.
Methods
Databases including PubMed, Cochrane Library, Embase, Web of Science, and MEDLINE were searched until August 2021. Cross-sectional and case-control studies were included.
Results
Twenty-one studies with 1,780 cases and 2,070 controls were identified. SAA levels were significantly higher in T2DM patients than in healthy groups (standardized mean difference [SMD], 0.68; 95% confidence interval [CI], 0.39 to 0.98). A subgroup analysis showed that the mean age of participants and the continent that participants were from were related to differences in SAA levels between cases and controls. Furthermore, in T2DM patients, SAA levels were positively associated with body mass index (r=0.34; 95% CI, 0.03 to 0.66), triglycerides (r=0.12; 95% CI, 0.01 to 0.24), fasting plasma glucose (r=0.26; 95% CI, 0.07 to 0.45), hemoglobin A1c (r=0.24; 95% CI, 0.16 to 0.33), homeostasis model assessment for insulin resistance (r=0.22; 95% CI, 0.10 to 0.34), C-reactive protein (r=0.77; 95% CI, 0.62 to 0.91), and interleukin-6 (r=0.42; 95% CI, 0.31 to 0.54), but negatively linked with highdensity lipoprotein cholesterol (r=–0.23; 95% CI, –0.44 to –0.03).
Conclusion
The meta-analysis suggests that high SAA levels may be associated with the presence of T2DM, as well as lipid metabolism homeostasis and the inflammatory response. -
Citations
Citations to this article as recorded by- Correlation between insulin resistance and the rate of neutrophils-lymphocytes, monocytes-lymphocytes, platelets-lymphocytes in type 2 diabetic patients
Yuanyuan Zhang, Huaizhen Liu
BMC Endocrine Disorders.2024;[Epub] CrossRef - Antioxidant and Anti-Inflammatory Functions of High-Density Lipoprotein in Type 1 and Type 2 Diabetes
Damien Denimal
Antioxidants.2023; 13(1): 57. CrossRef
- Correlation between insulin resistance and the rate of neutrophils-lymphocytes, monocytes-lymphocytes, platelets-lymphocytes in type 2 diabetic patients

- Diabetes, obesity and metabolism
- Effects of Weight Loss and Interaction with Physical Activity on Risks of Cardiovascular Outcomes in Individuals with Type 2 Diabetes
- Claudia R. L. Cardoso, Nathalie C. Leite, Gil F. Salles
- Endocrinol Metab. 2023;38(3):305-314. Published online May 31, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1690

- 2,494 View
- 136 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the effects of weight loss during follow-up on cardiovascular outcomes in a type 2 diabetes cohort and tested interactions with clinical and laboratory variables, particularly physical activity, that could impact the associations.
Methods
Relative weight changes were assessed in 651 individuals with type 2 diabetes and categorized as ≥5% loss, <5% loss, or gain. Associations between weight loss categories and incident cardiovascular outcomes (total cardiovascular events [CVEs], major adverse cardiovascular events [MACEs], and cardiovascular mortality) were assessed using multivariable Cox regression with interaction analyses.
Results
During the initial 2 years, 125 individuals (19.2%) lost ≥5% of their weight, 180 (27.6%) lost <5%, and 346 (53.1%) gained weight. Over a median additional follow-up of 9.3 years, 188 patients had CVEs (150 MACEs) and 106 patients died from cardiovascular causes. Patients with ≥5% weight loss had a significantly lower risk of total CVEs (hazard ratio [HR], 0.52; 95% confidence interval, 0.33 to 0.89; P=0.011) than those who gained weight, but non-significant lower risks of MACEs or cardiovascular deaths. Patients with <5% weight loss had risks similar to those with weight gain. There were interactions between weight loss and physical activity. In active individuals, ≥5% weight loss was associated with significantly lower risks for total CVEs (HR, 0.20; P=0.004) and MACEs (HR, 0.21; P=0.010), whereas in sedentary individuals, no cardiovascular protective effect of weight loss was evidenced.
Conclusion
Weight loss ≥5% may be beneficial for cardiovascular disease prevention, particularly when achieved with regular physical activity, even in high-risk individuals with long-standing type 2 diabetes. -
Citations
Citations to this article as recorded by- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(3): 302. CrossRef - Effects of body weight variability on risks of macro- and microvascular outcomes in individuals with type 2 diabetes: The Rio de Janeiro type 2 diabetes cohort
Claudia R.L. Cardoso, Nathalie C. Leite, Gil F. Salles
Diabetes Research and Clinical Practice.2023; 205: 110992. CrossRef
- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data

Editorial
- Diabetes, obesity and metabolism
- Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
- Seung-Hwan Lee
- Endocrinol Metab. 2023;38(3):302-304. Published online June 28, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1751
- 924 View
- 78 Download

Review Articles
- Calcium & bone metabolism
- Skeletal Senescence with Aging and Type 2 Diabetes
- Joshua Nicholas Farr
- Endocrinol Metab. 2023;38(3):295-301. Published online June 14, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1727

- 2,637 View
- 125 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Osteoporosis and type 2 diabetes (T2D) are common diseases that often coexist. While both of these diseases are associated with poor bone quality and increased fracture risk, their pathogenesis of increased fracture risk differs and is multifactorial. Mounting evidence now indicates that key fundamental mechanisms that are central to both aging and energy metabolism exist. Importantly, these mechanisms represent potentially modifiable therapeutic targets for interventions that could prevent or alleviate multiple complications of osteoporosis and T2D, including poor bone quality. One such mechanism that has gained increasing momentum is senescence, which is a cell fate that contributes to multiple chronic diseases. Accumulating evidence has established that numerous boneresident cell types become susceptible to cellular senescence with old age. Recent work also demonstrates that T2D causes the premature accumulation of senescent osteocytes during young adulthood, at least in mice, although it remains to be seen which other bone-resident cell types become senescent with T2D. Given that therapeutically removing senescent cells can alleviate age-related bone loss and T2D-induced metabolic dysfunction, it will be important in future studies to rigorously test whether interventions that eliminate senescent cells can also alleviate skeletal dysfunction in context of T2D, as it does with aging.
-
Citations
Citations to this article as recorded by- Single-cell sequencing reveals an important role of SPP1 and microglial activation in age-related macular degeneration
Shizhen Lei, Mang Hu, Zhongtao Wei
Frontiers in Cellular Neuroscience.2024;[Epub] CrossRef - The synergistic effect of diabetes mellitus and osteoporosis on the all-cause mortality: a cohort study of an American population
Weihua Li, Siyu Xie, Shengdong Zhong, Liting Lan
Frontiers in Endocrinology.2024;[Epub] CrossRef - Identification of systemic biomarkers and potential drug targets for age-related macular degeneration
Shizhen Lei, Mang Hu, Zhongtao Wei
Frontiers in Aging Neuroscience.2024;[Epub] CrossRef
- Single-cell sequencing reveals an important role of SPP1 and microglial activation in age-related macular degeneration

- Thyroid
- Diagnosis and Management of Thyroid Disease during Pregnancy and Postpartum: 2023 Revised Korean Thyroid Association Guidelines
- Hwa Young Ahn, Ka Hee Yi
- Endocrinol Metab. 2023;38(3):289-294. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1696
- 6,345 View
- 696 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thyroid hormone plays a critical role in fetal growth and development, and thyroid dysfunction during pregnancy is associated with several adverse outcomes, such as miscarriage and preterm birth. In this review, we introduce and explain three major changes in the revised Korean Thyroid Association (KTA) guidelines for the diagnosis and management of thyroid disease during pregnancy: first, the normal range of thyroid-stimulating hormone (TSH) during pregnancy; second, the treatment of subclinical hypothyroidism; and third, the management of euthyroid pregnant women with positive thyroid autoantibodies. The revised KTA guidelines adopt 4.0 mIU/L as the upper limit of TSH in the first trimester. A TSH level between 4.0 and 10.0 mIU/L, combined with free thyroxine (T4) within the normal range, is defined as subclinical hypothyroidism, and a TSH level over 10 mIU/L is defined as overt hypothyroidism regardless of the free T4 level. Levothyroxine treatment is recommended when the TSH level is higher than 4 mIU/L in subclinical hypothyroidism, regardless of thyroid peroxidase antibody positivity. However, thyroid hormone therapy to prevent miscarriage is not recommended in thyroid autoantibody-positive women with normal thyroid function.
-
Citations
Citations to this article as recorded by- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2023; 38(4): 381. CrossRef - Maternal isolated hypothyroxinemia in the first trimester is not associated with adverse pregnancy outcomes, except for macrosomia: a prospective cohort study in China
Jing Du, Linong Ji, Xiaomei Zhang, Ning Yuan, Jianbin Sun, Dan Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia

Corrigendum
- Miscellaneous
- Corrigendum: Affiliation Correction. Development and Validation of a Risk Scoring System Derived from Meta-Analyses for Papillary Thyroid Cancer
- Sunghwan Suh, Tae Sik Goh, Yun Hak Kim, Sae-Ock Oh, Kyoungjune Pak, Ju Won Seok, In Joo Kim
- Endocrinol Metab. 2023;38(2):287. Published online April 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.202
- Corrects: Endocrinol Metab 2020;35(2):435
- 888 View
- 58 Download

Letter
- Thyroid
- Thyroid Disorder: A Possible Forgotten Clinical Feature of Monkeypox
- Beuy Joob, Viroj Wiwanitkit
- Endocrinol Metab. 2023;38(2):285-286. Published online September 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1566
- 21,578 View
- 109 Download
- 1 Web of Science

Image of Interest
- Thyroid
- Propylthiouracil-Induced Antineutrophil Cytoplasmic Antibody-Positive Vasculitis and Agranulocytosis: A Rare Case with Life-Threatening Multiple Systemic Manifestations
- Da Hyun Kang, Mi-Kyung Song, Sang-Hyeon Ju, Song-I Lee, Yea Eun Kang
- Endocrinol Metab. 2023;38(2):282-284. Published online March 13, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1643
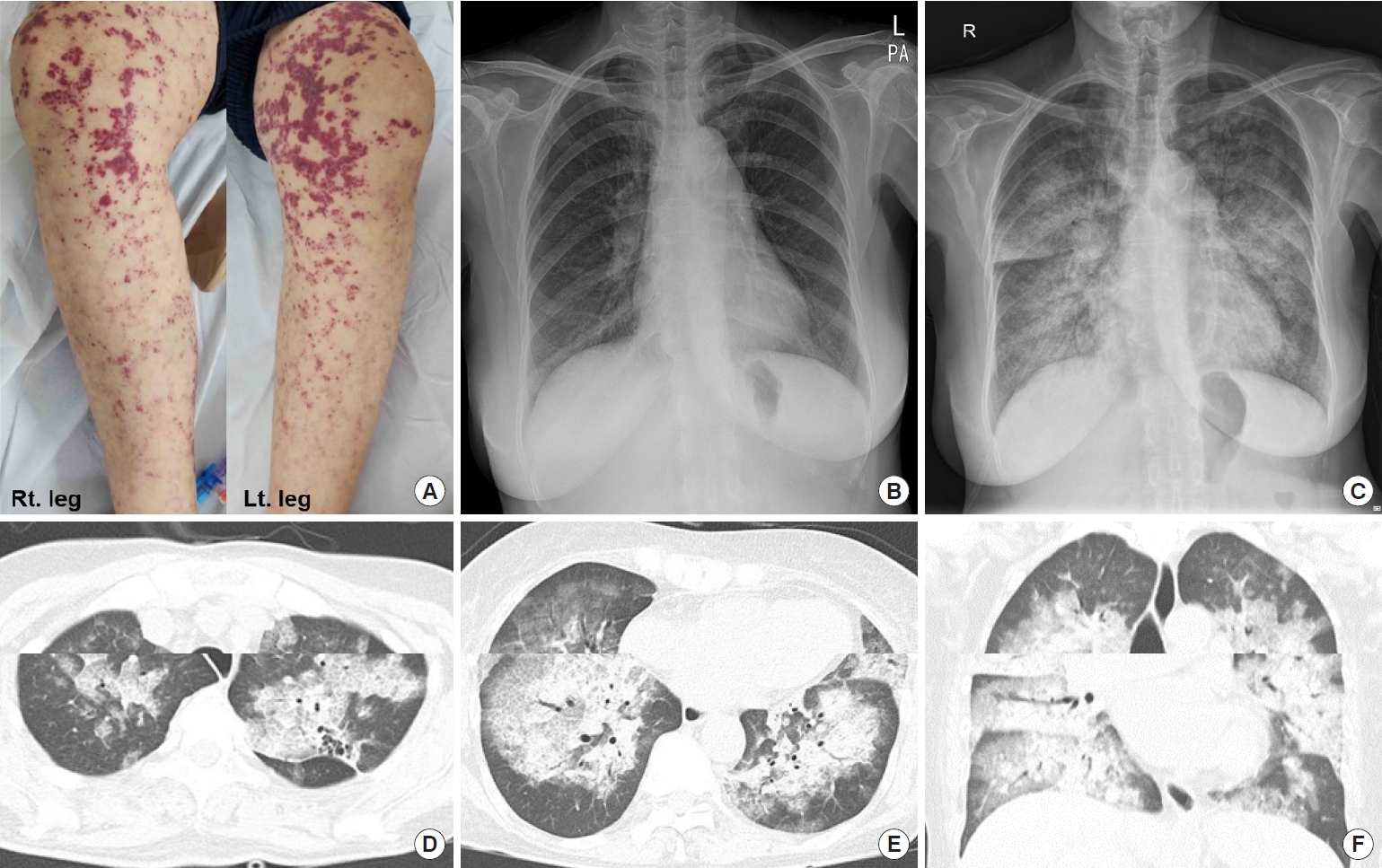
- 1,183 View
- 91 Download
- 1 Crossref

Brief Report
- Diabetes, obesity and metabolism
- Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
- Seung Min Chung, Min Kyu Kang, Jun Sung Moon, Jung Gil Park
- Endocrinol Metab. 2023;38(2):277-281. Published online March 13, 2023
- DOI: https://doi.org/10.3803/EnM.2022.1635

- 1,780 View
- 95 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This cross-sectional study enrolled 267 patients with metabolic risk factors and established non-alcoholic fatty liver disease in the prospective cohort. The performance of fibrosis-4 (FIB-4) score (≥1.3) to diagnose advanced fibrosis using transient elastography (liver stiffness measurement [LSM] ≥8 kPa) was analyzed. Comparing patients with type 2 diabetes (T2D, n=87) and without (n=180), not FIB-4, but LSM was significantly higher in T2D (P=0.026). The prevalence of advanced fibrosis was 17.2% in T2D and 12.8% in non-T2D. FIB-4 exhibited higher proportion of false negatives in T2D patients (10.9%) than those without (5.2%). The diagnostic performance of FIB-4 was suboptimal in T2D (area under curve [AUC], 0.653; 95% confidence interval [CI], 0.462 to 0.844) compared to that in non-T2D (AUC, 0.826; 95% CI, 0.724 to 0.927). In conclusion, patients with T2D might be beneficial to conduct transient elastography without screening to avoid missing advanced fibrosis.
-
Citations
Citations to this article as recorded by- Prevalence of High and Moderate Risk of Liver Fibrosis Among Patients With Diabetes at a Noncommunicable Diseases (NCD) Clinic in a Primary Healthcare Center in Northern India
Anubhav Mondal, Aninda Debnath, Ghurumourthy Dhandapani, Abhishek Sharma, Shveta Lukhmana, Geeta Yadav
Cureus.2023;[Epub] CrossRef
- Prevalence of High and Moderate Risk of Liver Fibrosis Among Patients With Diabetes at a Noncommunicable Diseases (NCD) Clinic in a Primary Healthcare Center in Northern India


 KES
KES

 First
First Prev
Prev



