Article type
- Page Path
- HOME > BROWSE ARTICLES > Article type
Original Articles
- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
- Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
- Endocrinol Metab. 2023;38(6):690-700. Published online October 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1782
- 1,342 View
- 91 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Acromegaly leads to various skeletal complications, and fragility fractures are emerging as a new concern in patients with acromegaly. Therefore, this study investigated the risk of fractures in Korean patients with acromegaly.
Methods
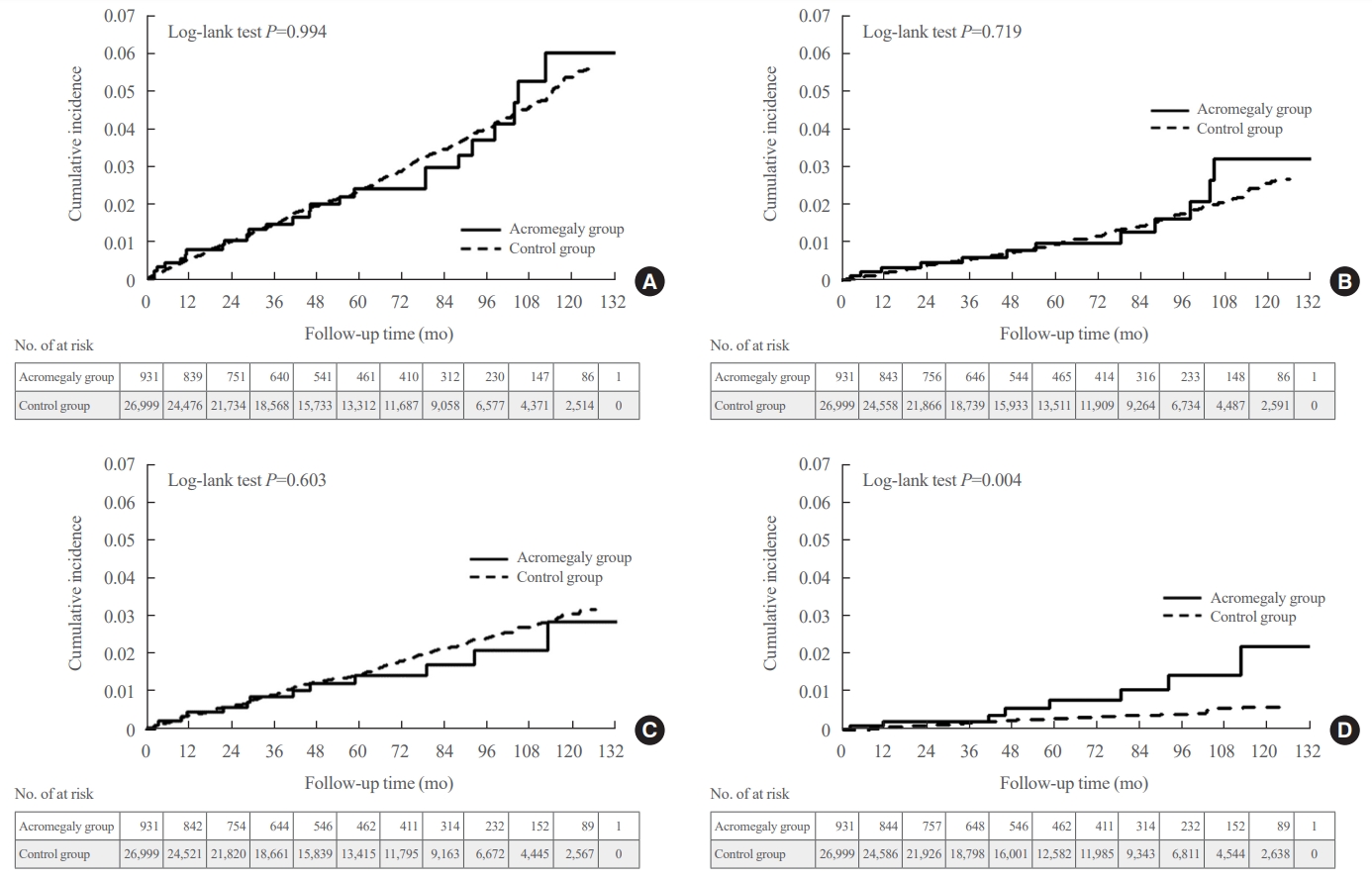
We used the Korean nationwide claims database from 2009 to 2019. A total of 931 patients with acromegaly who had never used an osteoporosis drug before and were treated with surgery alone were selected as study participants, and a 1:29 ratio of 26,999 age- and sex-matched osteoporosis drug-naïve controls without acromegaly were randomly selected from the database.
Results
The mean age was 46.2 years, and 50.0% were male. During a median follow-up of 54.1 months, there was no difference in the risks of all, vertebral, and non-vertebral fractures between the acromegaly and control groups. However, hip fracture risk was significantly higher (hazard ratio [HR], 2.73; 95% confidence interval [CI], 1.32 to 5.65), and non-hip and non-vertebral fractures risk was significantly lower (HR, 0.40; 95% CI, 0.17 to 0.98) in patients with acromegaly than in controls; these results remained robust even after adjustment for socioeconomic status and baseline comorbidities. Age, type 2 diabetes mellitus, cardio-cerebrovascular disease, fracture history, recent use of acid-suppressant medication, psychotropic medication, and opioids were risk factors for all fractures in patients with acromegaly (all P<0.05).
Conclusion
Compared with controls, patients surgically treated for acromegaly had a higher risk of hip fractures. The risk factors for fracture in patients with acromegaly were consistent with widely accepted risk factors in the general population.

- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
- Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
- Endocrinol Metab. 2023;38(6):679-689. Published online December 6, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1760
- 1,168 View
- 65 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Limited longitudinal evidence exists regarding the potential association between smoking status and hip fracture among individuals with type 2 diabetes. We investigated this association using large-scale, nationwide cohort data for the Korean population.
Methods
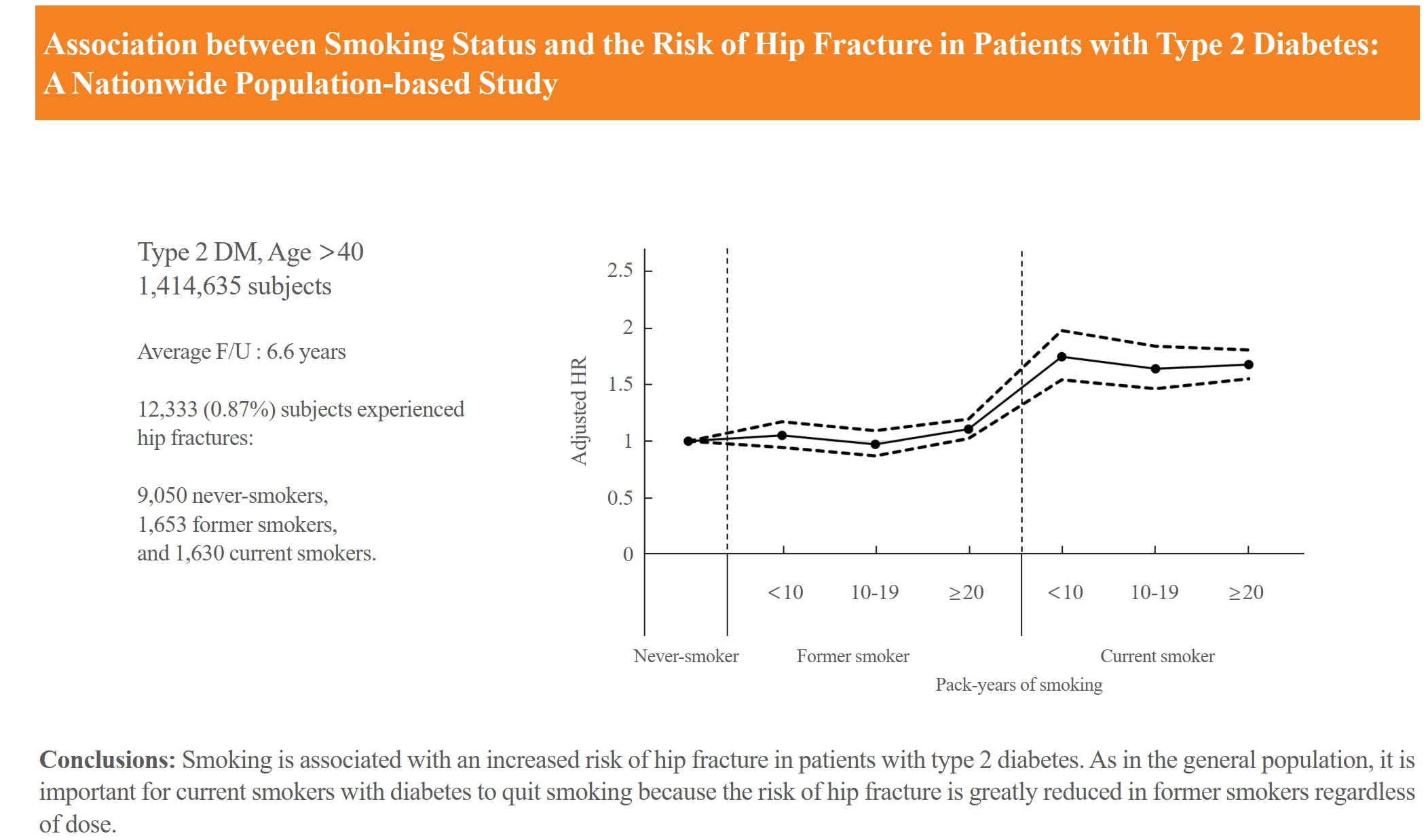
This nationwide cohort study included 1,414,635 adults aged 40 and older who received Korean National Health Insurance Service health examinations between 2009 and 2012. Subjects with type 2 diabetes were categorized according to their smoking status, amount smoked (pack-years), number of cigarettes smoked per day, and duration of smoking. The results are presented as hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between smoking status parameters and risk of hip fracture in multivariable Cox proportional hazard regression analysis.
Results
Compared with never-smokers, an increased adjusted HR (aHR) for hip fracture was observed in current smokers (1.681; 95% CI, 1.578 to 1.791), and a comparable aHR for hip fracture was found in former smokers (1.065; 95% CI, 0.999 to 1.136). For former smokers who had smoked 20 pack-years or more, the risk was slightly higher than that for never-smokers (aHR, 1.107; 95% CI, 1.024 to 1.196). The hip fracture risk of female former smokers was similar to that of female current smokers, but the hip fracture risk in male former smokers was similar to that of male never-smokers.
Conclusion
Smoking is associated with an increased risk of hip fracture in patients with type 2 diabetes. Current smokers with diabetes should be encouraged to quit smoking because the risk of hip fracture is greatly reduced in former smokers.

- Calcium & bone metabolism
- Age-Dependent Association of Height Loss with Incident Fracture Risk in Postmenopausal Korean Women
- Chaewon Lee, Hye-Sun Park, Yumie Rhee, Namki Hong
- Endocrinol Metab. 2023;38(6):669-678. Published online September 1, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1734
- 1,476 View
- 87 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Height loss is a simple clinical measure associated with increased fracture risk. However, limited data exists on the association between height loss and fracture risk in postmenopausal Korean women. It is unknown whether this association varies with age.
Methods
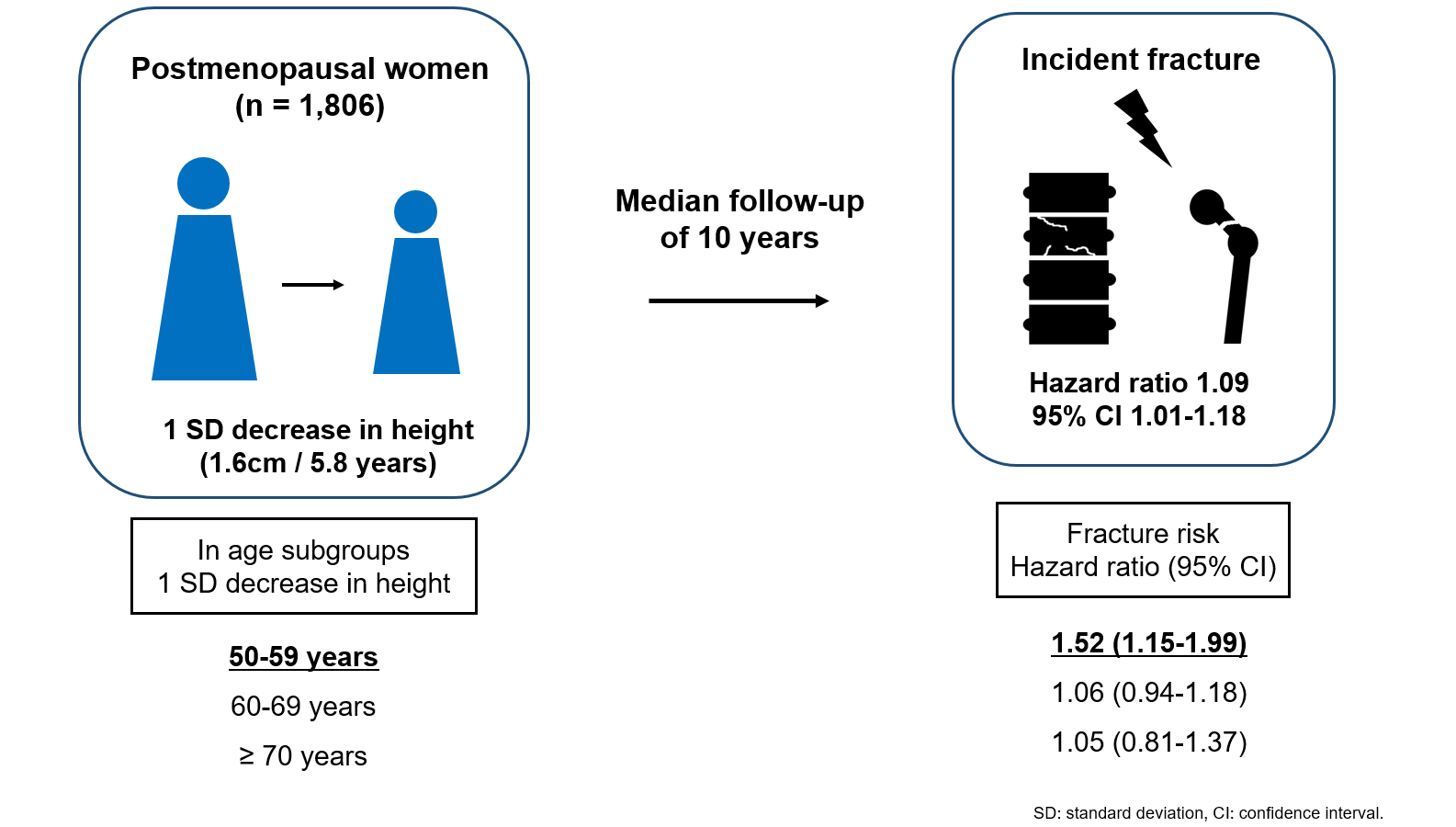
Data on height loss over a 6-year period were collected from a community-based longitudinal follow-up cohort (Ansung cohort of the Korean Genome and Epidemiology Study). Incident fractures were defined based on self-reported fractures after excluding those due to severe trauma or toes/fingers. The association between incident fractures and height loss was investigated using a Cox proportional hazards model.
Results
During a median follow-up of 10 years after the second visit, 259/1,806 participants (median age, 64 years) experienced incident fractures. Overall, a 1 standard deviation (SD) decrease in height (1.6 cm/median 5.8 years) was associated with 9% increased risk of fracture (hazard ratio [HR], 1.09; P=0.037), which lost statistical significance after adjustment for covariates. When stratified into age groups (50–59, 60–69, 70 years or older), a 1 SD decrease in height remained a robust predictor of fracture in the 50 to 59 years age group after adjusting for covariates (adjusted hazard ratio [aHR], 1.52; P=0.003), whereas height loss was not an independent predictor of fracture in the 60 to 69 (aHR, 1.06; P=0.333) or the 70 years or older age groups (aHR, 1.05; P=0.700; P for interaction <0.05, for all).
Conclusion
Height loss during the previous 6 years was associated with an increased 10-year fracture risk in postmenopausal women in their 50s.

Editorial
- Diabetes, obesity and metabolism
- Potential of γ-Glutamyl Transferase as a Novel Risk Factor for Cardiovascular Disease
- Sang Youl Rhee
- Endocrinol Metab. 2023;38(6):667-668. Published online December 22, 2023
- DOI: https://doi.org/10.3803/EnM.2023.602
- 823 View
- 37 Download

Review Articles
- Calcium & bone metabolism
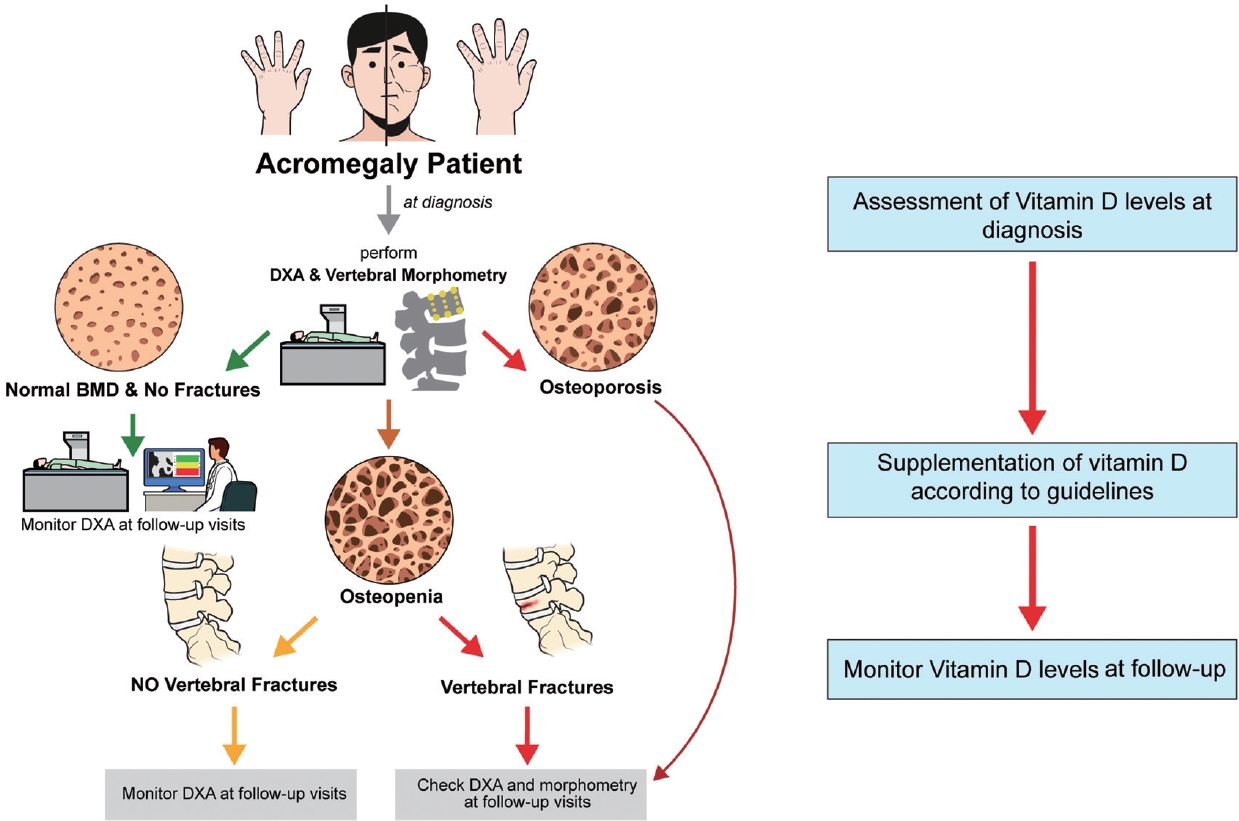
- Acromegaly and Bone: An Update
- Andrea Giustina
- Endocrinol Metab. 2023;38(6):655-666. Published online December 22, 2023
- DOI: https://doi.org/10.3803/EnM.2023.601
- 1,306 View
- 108 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since our discovery in 2006 that acromegaly is associated with an increased risk of vertebral fractures, many authors have confirmed this finding in both cross-sectional and prospective studies. Due to the high epidemiological and clinical impact of this newly discovered comorbidity of acromegaly, this topic has progressively become more important and prominent over the years, and the pertinent literature has been enriched by new findings on the pathophysiology and treatment. The aim of this narrative review was to discuss these novel findings, integrating them with the seminal observations, in order to give the reader an updated view of how the field of acromegaly and bone is developing, from strong clinical observations to a mechanistic understanding and possible prevention and treatment.
-
Citations
Citations to this article as recorded by- New insights into the vitamin D/PTH axis in endocrine-driven metabolic bone diseases
Luigi di Filippo, John P. Bilezikian, Ernesto Canalis, Umberto Terenzi, Andrea Giustina
Endocrine.2024;[Epub] CrossRef
- New insights into the vitamin D/PTH axis in endocrine-driven metabolic bone diseases

- Hypothalamus and pituitary gland
- Update on Current Evidence for the Diagnosis and Management of Nonfunctioning Pituitary Neuroendocrine Tumors
- Elizabeth Whyte, Masahiro Nezu, Constance Chik, Toru Tateno
- Endocrinol Metab. 2023;38(6):631-654. Published online November 15, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1838

- 2,241 View
- 140 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Pituitary neuroendocrine tumors (PitNETs) are the third most frequently diagnosed intracranial tumors, with nonfunctioning PitNETs (nfPitNETs) accounting for 30% of all pituitary tumors and representing the most common type of macroPitNETs. NfPitNETs are usually benign tumors with no evidence of hormone oversecretion except for hyperprolactinemia secondary to pituitary stalk compression. Due to this, they do not typically present with clinical syndromes like acromegaly, Cushing’s disease or hyperthyroidism and instead are identified incidentally on imaging or from symptoms of mass effects (headache, vision changes, apoplexy). With the lack of effective medical interventions, first-line treatment is transsphenoidal surgical resection, however, nfPitNETs often have supra- or parasellar extension, and total resection of the tumor is often not possible, resulting in residual tumor regrowth or reoccurrence. While functional PitNETs can be easily followed for recurrence using hormonal biomarkers, there is no similar parameter to predict recurrence in nfPitNETs, hence delaying early recognition and timely management. Therefore, there is a need to identify prognostic biomarkers that can be used for patient surveillance and as therapeutic targets. This review focuses on summarizing the current evidence on nfPitNETs, with a special focus on potential new biomarkers and therapeutics.

- Miscellaneous
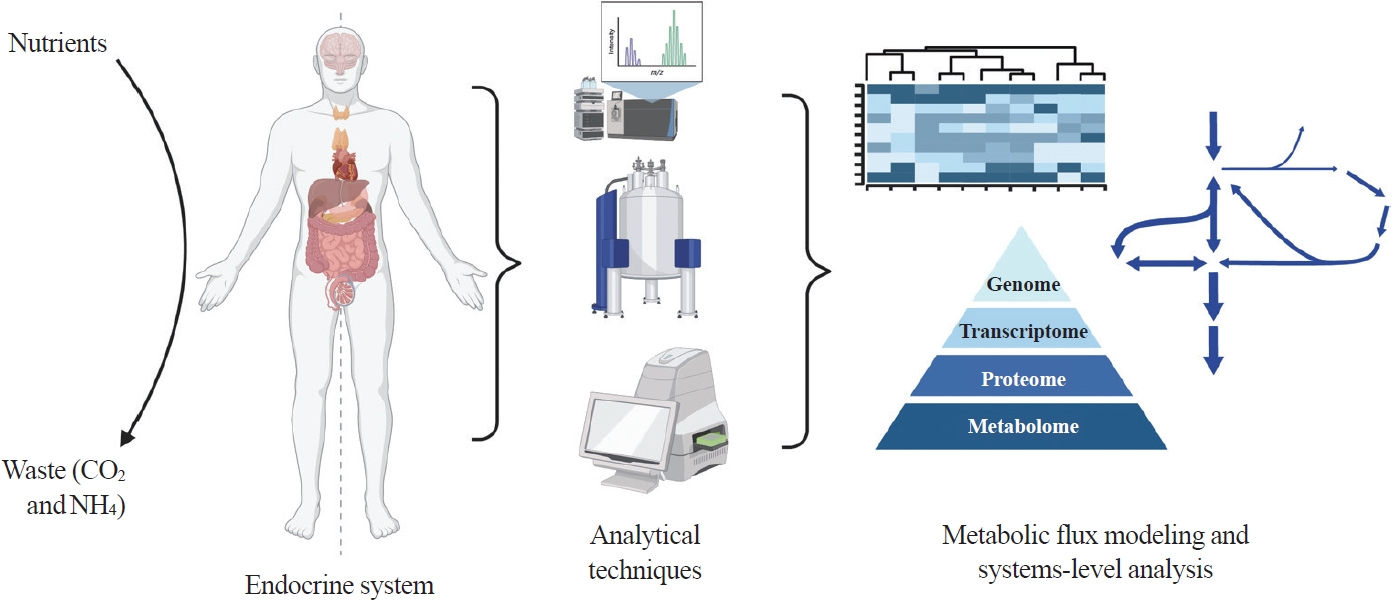
- Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer
- Aliya Lakhani, Da Hyun Kang, Yea Eun Kang, Junyoung O. Park
- Endocrinol Metab. 2023;38(6):619-630. Published online November 21, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1814
- 2,442 View
- 110 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Metabolism is a dynamic network of biochemical reactions that support systemic homeostasis amidst changing nutritional, environmental, and physical activity factors. The circulatory system facilitates metabolite exchange among organs, while the endocrine system finely tunes metabolism through hormone release. Endocrine disorders like obesity, diabetes, and Cushing’s syndrome disrupt this balance, contributing to systemic inflammation and global health burdens. They accompany metabolic changes on multiple levels from molecular interactions to individual organs to the whole body. Understanding how metabolic fluxes relate to endocrine disorders illuminates the underlying dysregulation. Cancer is increasingly considered a systemic disorder because it not only affects cells in localized tumors but also the whole body, especially in metastasis. In tumorigenesis, cancer-specific mutations and nutrient availability in the tumor microenvironment reprogram cellular metabolism to meet increased energy and biosynthesis needs. Cancer cachexia results in metabolic changes to other organs like muscle, adipose tissue, and liver. This review explores the interplay between the endocrine system and systems-level metabolism in health and disease. We highlight metabolic fluxes in conditions like obesity, diabetes, Cushing’s syndrome, and cancers. Recent advances in metabolomics, fluxomics, and systems biology promise new insights into dynamic metabolism, offering potential biomarkers, therapeutic targets, and personalized medicine.
-
Citations
Citations to this article as recorded by- Editorial: Tumor metabolism and programmed cell death
Dan-Lan Pu, Qi-Nan Wu
Frontiers in Endocrinology.2024;[Epub] CrossRef
- Editorial: Tumor metabolism and programmed cell death

Special Article
- Adrenal gland
- 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
- Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung, The Committee of Clinical Practice Guideline of Korean Endocrine Society, The Korean Adrenal Study Group of Korean Endocrine Society
- Endocrinol Metab. 2023;38(6):597-618. Published online October 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1789

- 3,426 View
- 479 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Primary aldosteronism (PA) is a common, yet underdiagnosed cause of secondary hypertension. It is characterized by an overproduction of aldosterone, leading to hypertension and/or hypokalemia. Despite affecting between 5.9% and 34% of patients with hypertension, PA is frequently missed due to a lack of clinical awareness and systematic screening, which can result in significant cardiovascular complications. To address this, medical societies have developed clinical practice guidelines to improve the management of hypertension and PA. The Korean Endocrine Society, drawing on a wealth of research, has formulated new guidelines for PA. A task force has been established to prepare PA guidelines, which encompass epidemiology, pathophysiology, clinical presentation, diagnosis, treatment, and follow-up care. The Korean clinical guidelines for PA aim to deliver an evidence-based protocol for PA diagnosis, treatment, and patient monitoring. These guidelines are anticipated to ease the burden of this potentially curable condition.
-
Citations
Citations to this article as recorded by- Correlation of Histopathologic Subtypes of Primary Aldosteronism with Clinical Phenotypes and Postsurgical Outcomes
Chang Ho Ahn, You-Bin Lee, Jae Hyeon Kim, Young Lyun Oh, Jung Hee Kim, Kyeong Cheon Jung
The Journal of Clinical Endocrinology & Metabolism.2023;[Epub] CrossRef
- Correlation of Histopathologic Subtypes of Primary Aldosteronism with Clinical Phenotypes and Postsurgical Outcomes

Original Articles
- Thyroid
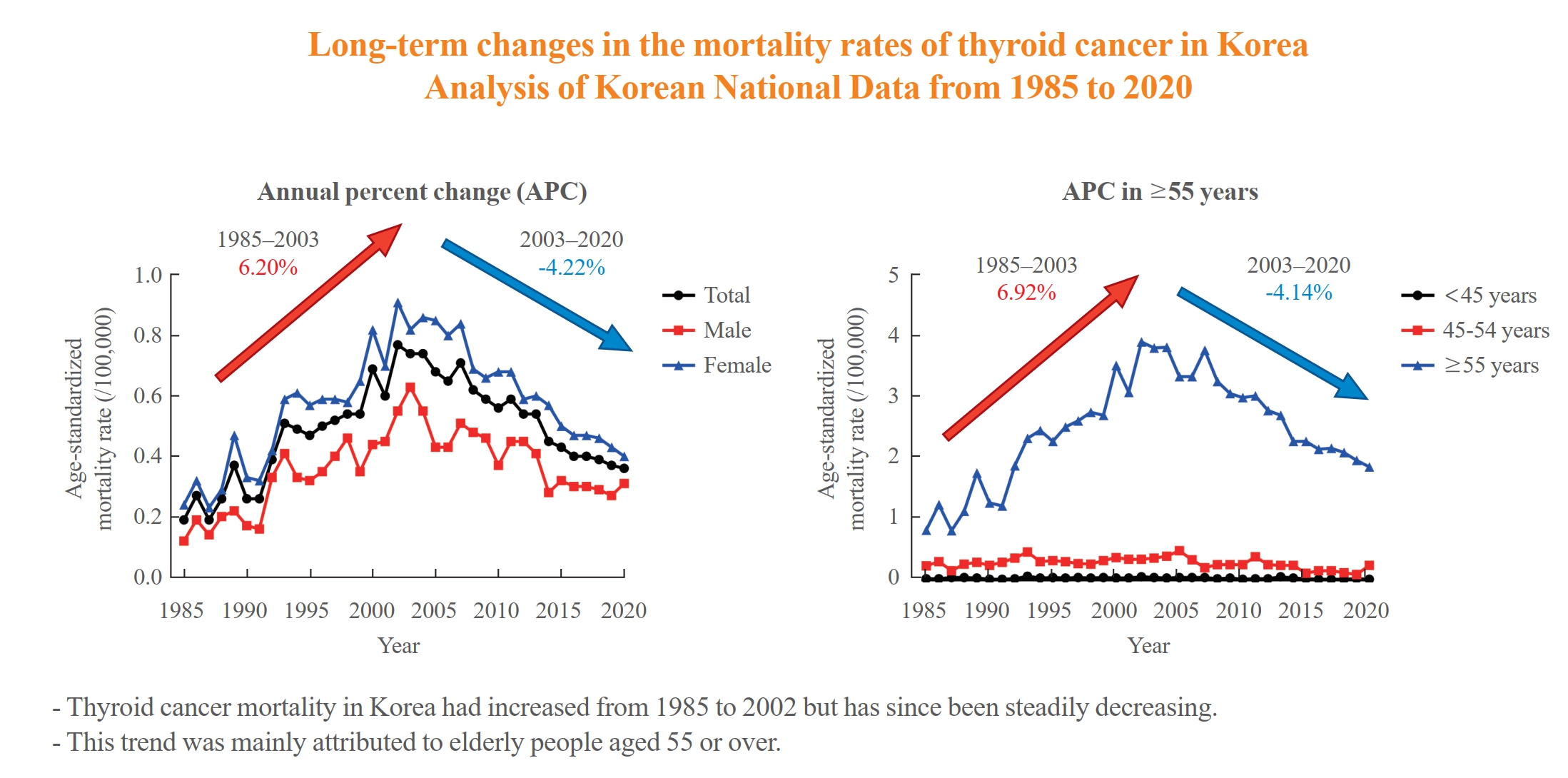
- Long-Term Changes in the Mortality Rates of Thyroid Cancer in Korea: Analysis of Korean National Data from 1985 to 2020
- Yun Mi Choi, Min-Ju Kim, Jiwoo Lee, Mi Kyung Kwak, Min Ji Jeon, Tae Yong Kim, Eun-Gyoung Hong, Won Bae Kim, Won Gu Kim
- Endocrinol Metab. 2023;38(5):588-595. Published online September 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1723
- 1,442 View
- 87 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Thyroid cancer mortality has been largely overlooked as relatively stable given the large gap between thyroid cancer incidence and mortality. This study evaluated long-term trends in age-standardized mortality rates (ASMRs) throughout Korea and compared them with mortality data reported by the Surveillance, Epidemiology, and End Results (SEER).
Methods
Cancer-specific mortality data from 1985 to 2020 were obtained from Statistics Korea. ASMRs from thyroid cancer were calculated based on the Korean mid-year resident registration population of 2005. We assessed SEER*Explorer and downloaded the mortality data.
Results
The ASMR increased from 0.19 to 0.77/100,000 between 1985 and 2002 but decreased continuously to 0.36/100,000 in 2020. The annual percent change (APC) in the ASMR between 1985 and 2003 and between 2003 and 2020 was 6.204 and −4.218, respectively, with similar patterns observed in both men and women. The ASMR of the SEER showed a modest increase from 1988 to 2016 and then stabilized. In subgroup analysis, the ASMR of the old age group (≥55 years) increased significantly from 0.82 in 1985 to 3.92/100,000 in 2002 (APC 6.917) but then decreased again to 1.86/100,000 in 2020 (APC −4.136). ASMRs according to the age group in the SEER showed a relatively stable trend even in the elderly group.
Conclusion
The ASMR of thyroid cancer in Korea had increased from 1985 to 2002 but has since been steadily decreasing. This trend was mainly attributed to elderly people aged 55 or over. The absolute APC value of Korea was much higher than that of the SEER. -
Citations
Citations to this article as recorded by- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef - A Clinical Audit of Thyroid Hormonal Replacement After Total Thyroidectomy
Islam Mansy, Abdelfatah M Elsenosy, Eslam M Hassan, Mujtaba Zakria
Cureus.2023;[Epub] CrossRef
- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma

- Calcium & bone metabolism
- Characteristics Associated with Bone Loss after Spinal Cord Injury: Implications for Hip Region Vulnerability
- Sora Han, Sungjae Shin, Onyoo Kim, Namki Hong
- Endocrinol Metab. 2023;38(5):578-587. Published online October 10, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1795

- 1,275 View
- 51 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
In individuals with spinal cord injury (SCI), bone loss progresses rapidly to the area below the level of injury, leading to an increased risk of fracture. However, there are limited data regarding SCI-relevant characteristics for bone loss and the degree of bone loss in individuals with SCI compared with that in non-SCI community-dwelling adults.
Methods
Data from men with SCI who underwent dual-energy X-ray absorptiometry at the National Rehabilitation Center (2008 to 2020) between 12 and 36 months after injury were collected and analyzed. Community-dwelling men were matched 1:1 for age, height, and weight as the control group, using data from the Korea National Health and Nutrition Examination Survey (KNHANES, 2008 to 2011).
Results
A comparison of the SCI and the matched control group revealed significantly lower hip region T-scores in the SCI group, whereas the lumbar spine T-score did not differ between groups. Among the 113 men with SCI, the paraplegia group exhibited significantly higher Z-scores of the hip region than the tetraplegia group. Participants with motor-incomplete SCI showed relatively preserved Z-scores of the hip region compared to those of the lumbar region. Moreover, in participants with SCI, the percentage of skeletal muscle displayed a moderate positive correlation with femoral neck Z-scores.
Conclusion
Men with SCI exhibited significantly lower bone mineral density of the hip region than community-dwelling men. Paraplegia rather than tetraplegia, and motor incompleteness rather than motor completeness were protective factors in the hip region. Caution for loss of skeletal muscle mass or increased adiposity is also required.

- Diabetes, obesity and metabolism
- Coronary Artery Calcium Score as a Sensitive Indicator of Cardiovascular Disease in Patients with Type 2 Diabetes Mellitus: A Long-Term Cohort Study
- Dae-Jeong Koo, Mi Yeon Lee, Sun Joon Moon, Hyemi Kwon, Sang Min Lee, Se Eun Park, Cheol-Young Park, Won-Young Lee, Ki Won Oh, Sung Rae Cho, Young-Hoon Jeong, Eun-Jung Rhee
- Endocrinol Metab. 2023;38(5):568-577. Published online October 10, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1770

- 1,510 View
- 112 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Coronary artery calcium score (CACS) has become an important tool for evaluating cardiovascular disease (CVD). This study evaluated the significance of CACS for future CVD through more than 10 years of follow-up in asymptomatic Korean populations with type 2 diabetes mellitus (T2DM) known to have a relatively low CACS burden.
Methods
We enrolled 981 asymptomatic T2DM patients without CVD at baseline who underwent CACS evaluation using multidetector computed tomography between January 2008 and December 2014. They were grouped into five predefined CACS categories based on Agatston scores and followed up by August 2020. The primary endpoint was incident CVD events, including coronary, cerebrovascular, and peripheral arterial disease.
Results
The relative risk of CVD was significantly higher in patients with CACS ≥10, and the significance persisted after adjustment for known confounders. A higher CACS category indicated a higher incidence of future CVD: hazard ratio (95% confidence interval) 4.09 (1.79 to 9.36), 12.00 (5.61 to 25.69), and 38.79 (16.43 to 91.59) for 10≤ CACS <100, 100≤ CACS <400, and CACS ≥400, respectively. During the 12-year follow-up period, the difference in event-free survival more than doubled as the category increased. Patients with CACS below 10 had very low CVD incidence throughout the follow-up. The receiver operating characteristic analysis showed better area under curve when the CACS cutoff was 10 than 100.
Conclusion
CACS can be a sensitive marker of CVD risk. Specifically, CACS above 10 is an indicator of CVD high-risk requiring more intensive medical treatment in Koreans with T2DM.

- Diabetes, obesity and metabolism
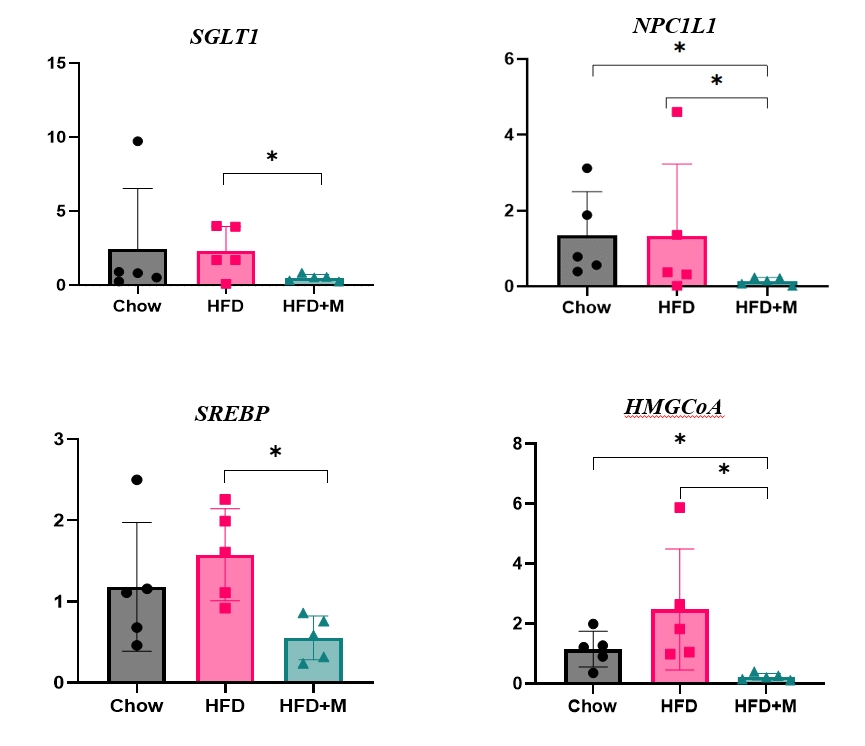
- Protective Effects of Melatonin in High-Fat Diet-Induced Hepatic Steatosis via Decreased Intestinal Lipid Absorption and Hepatic Cholesterol Synthesis
- Hyungjune Ku, Yeonji Kim, Alvin Lyle Kim, Garam Lee, Youngsik Choi, Bukyung Kim
- Endocrinol Metab. 2023;38(5):557-567. Published online September 1, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1672
- 1,944 View
- 93 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The preventative effect of melatonin on the development of obesity and the progression of fatty liver under a high-fat diet (HFD) has been well elucidated through previous studies. We investigated the mechanism behind this effect regarding cholesterol biosynthesis and regulation of cholesterol levels.
Methods
Mice were divided into three groups: normal chow diet (NCD); HFD; and HFD and melatonin administration group (HFD+M). We assessed the serum lipid profile, mRNA expression levels of proteins involved in cholesterol synthesis and reabsorption in the liver and nutrient transporters in the intestines, and cytokine levels. Additionally, an in vitro experiment using HepG2 cells was performed.
Results
Expression of hepatic sterol regulatory element-binding protein 2 (SREBP-2), 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR), and low-density lipoprotein receptor (LDLR) demonstrated that melatonin administration significantly reduces hepatic cholesterol synthesis in mice fed an HFD. Expression of intestinal sodium-glucose transporter 1 (SGLT1), glucose transporter 2 (GLUT2), GLUT5, and Niemann-pick C1-like 1 (NPC1L1) demonstrated that melatonin administration significantly reduces intestinal carbohydrate and lipid absorption in mice fed an HFD. There were no differences in local and circulatory inflammatory cytokine levels among the NCD, HFD, and HFD+M group. HepG2 cells stimulated with palmitate showed reduced levels of SREBP, LDLR, and HMGCR indicating these results are due to the direct mechanistic effect of melatonin on hepatocytes.
Conclusion
Collectively, these data indicate the mechanism behind the protective effects of melatonin from weight gain and liver steatosis under HFD is through a reduction in intestinal caloric absorption and hepatic cholesterol synthesis highlighting its potential in the treatment of obesity and fatty liver disease. -
Citations
Citations to this article as recorded by- Influence of dark deprivation on the ultrastructure and mitochondrial apparatus of rat hepatocytes
D Areshidze
Morphology.2024;[Epub] CrossRef
- Influence of dark deprivation on the ultrastructure and mitochondrial apparatus of rat hepatocytes

- Diabetes, obesity and metabolism
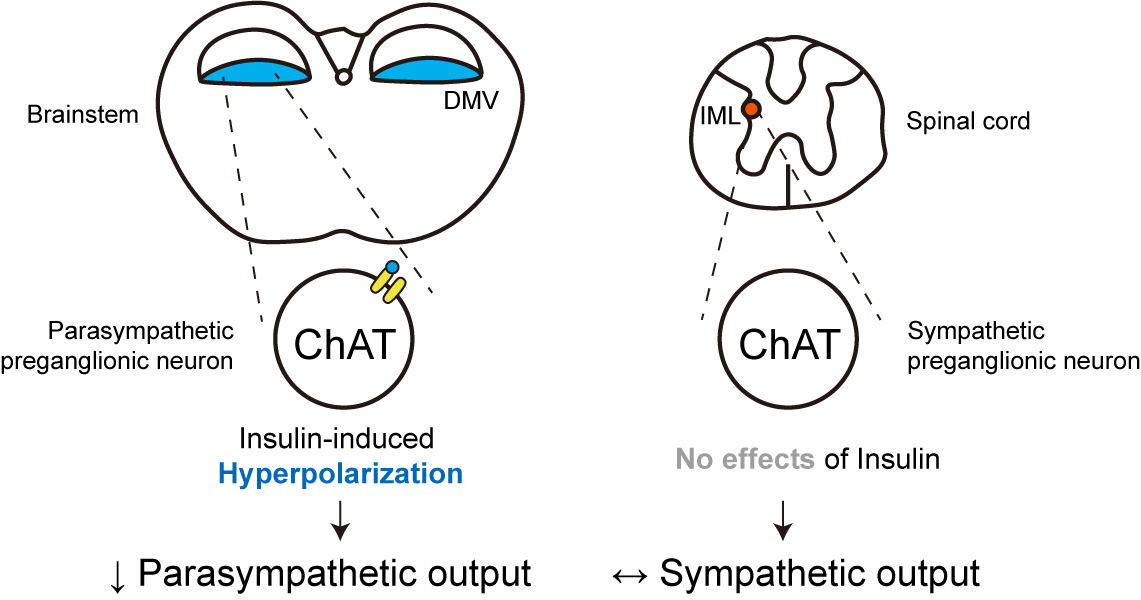
- Insulin Preferentially Regulates the Activity of Parasympathetic Preganglionic Neurons over Sympathetic Preganglionic Neurons
- Uisu Hyun, Yoon Young Kweon, Jong-Woo Sohn
- Endocrinol Metab. 2023;38(5):545-556. Published online September 26, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1725
- 1,356 View
- 76 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Insulin is a peptide hormone that regulates post-prandial physiology, and it is well known that insulin controls homeostasis at least in part via the central nervous system. In particular, insulin alters the activity of neurons within the autonomic nervous system. However, currently available data are mostly from unidentified brainstem neurons of the dorsal motor nucleus of the vagus nerve (DMV).
Methods
In this study, we used several genetically engineered mouse models to label distinct populations of neurons within the brainstem and the spinal cord for whole-cell patch clamp recordings and to assess several in vivo metabolic functions.
Results
We first confirmed that insulin directly inhibited cholinergic (parasympathetic preganglionic) neurons in the DMV. We also found inhibitory effects of insulin on both the excitatory and inhibitory postsynaptic currents recorded in DMV cholinergic neurons. In addition, GABAergic neurons of the DMV and nucleus tractus solitarius were inhibited by insulin. However, insulin had no effects on the cholinergic sympathetic preganglionic neurons of the spinal cord. Finally, we obtained results suggesting that the insulininduced inhibition of parasympathetic preganglionic neurons may not play a critical role in the regulation of glucose homeostasis and gastrointestinal motility.
Conclusion
Our results demonstrate that insulin inhibits parasympathetic neuronal circuitry in the brainstem, while not affecting sympathetic neuronal activity in the spinal cord.

- Diabetes, obesity and metabolism
- Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
- Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
- Endocrinol Metab. 2023;38(5):538-544. Published online August 8, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1730
- 1,900 View
- 109 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Despite the well-recognized health benefits of fresh fruit consumption, there is still substantial uncertainty about its potential effects on glycemic control in patients with type 2 diabetes mellitus (T2DM).
Methods
We examined the association of fresh fruit consumption and glycemic control in patients with T2DM using data from the 6th Korea National Health and Nutrition Examination Survey. The study sample was divided into three groups based on weekly fruit consumption frequency for the analysis.
Results
Patients with the highest fruit intake were older than those in the other two groups, and women were more likely to consume fruits in general. Being a current smoker and weekly alcohol intake also showed negative correlations according to the fruit intake tertiles. Fruit consumption was positively correlated with better hemoglobin A1c (HbA1c) levels. Moreover, patients in the highest tertile of fruit intake were 3.48 times more likely to be in good glycemic control defined as HbA1c <7%.
Conclusion
We observed that fruit consumption can be helpful in glycemic control in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- The Relationship between Alcohol Consumption and Diabetes in Korean Adults
Gi Tae Kim, Jae Woong Sull
Biomedical Science Letters.2023; 29(3): 159. CrossRef
- The Relationship between Alcohol Consumption and Diabetes in Korean Adults

- Diabetes, obesity and metabolism
Big Data Articles (National Health Insurance Service Database) - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
- Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee, Committee of Big Data, Korean Endocrine Society
- Endocrinol Metab. 2023;38(5):525-537. Published online September 7, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1765
- 1,557 View
- 90 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
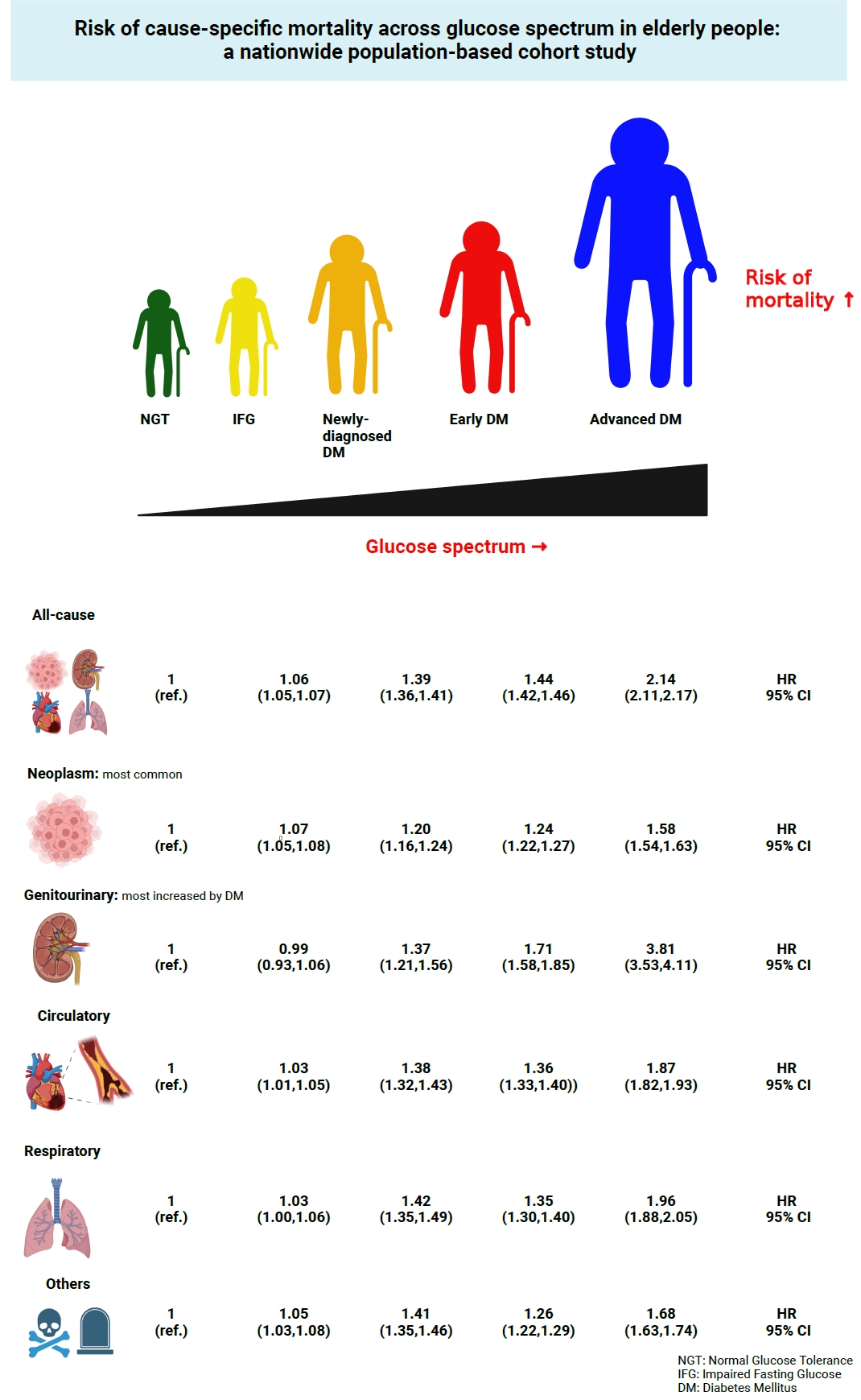
ePub - Background
This study investigated the risk of cause-specific mortality according to glucose tolerance status in elderly South Koreans.
Methods
A total of 1,292,264 individuals aged ≥65 years who received health examinations in 2009 were identified from the National Health Information Database. Participants were classified as normal glucose tolerance, impaired fasting glucose, newly-diagnosed diabetes, early diabetes (oral hypoglycemic agents ≤2), or advanced diabetes (oral hypoglycemic agents ≥3 or insulin). The risk of system-specific and disease-specific deaths was estimated using multivariate Cox proportional hazards analysis.
Results
During a median follow-up of 8.41 years, 257,356 deaths were recorded. Diabetes was associated with significantly higher risk of all-cause mortality (hazard ratio [HR], 1.58; 95% confidence interval [CI], 1.57 to 1.60); death due to circulatory (HR, 1.49; 95% CI, 1.46 to 1.52), respiratory (HR, 1.51; 95% CI, 1.47 to 1.55), and genitourinary systems (HR, 2.22; 95% CI, 2.10 to 2.35); and neoplasms (HR, 1.30; 95% CI, 1.28 to 1.32). Diabetes was also associated with a significantly higher risk of death due to ischemic heart disease (HR, 1.70; 95% CI, 1.63 to 1.76), cerebrovascular disease (HR, 1.46; 95% CI, 1.41 to 1.50), pneumonia (HR, 1.69; 95% CI, 1.63 to 1.76), and acute or chronic kidney disease (HR, 2.23; 95% CI, 2.09 to 2.38). There was a stepwise increase in the risk of death across the glucose spectrum (P for trend <0.0001). Stroke, heart failure, or chronic kidney disease increased the risk of all-cause mortality at every stage of glucose intolerance.
Conclusion
A dose-dependent association between the risk of mortality from various causes and severity of glucose tolerance was noted in the elderly population. -
Citations
Citations to this article as recorded by- The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef
- The Characteristics and Risk of Mortality in the Elderly Korean Population


 KES
KES

 First
First Prev
Prev



