Article type
- Page Path
- HOME > BROWSE ARTICLES > Article type
Response
- Diabetes, Obesity and Metabolism
- Association of Protein Z with Prediabetes and Type 2 Diabetes (Endocrinol Metab 2021;36:637-46, Yun-Ui Bae et al.)
- Ji Hong You, Yun-Ui Bae, Ho Chan Cho
- Endocrinol Metab. 2021;36(5):1149-1150. Published online September 16, 2021
- DOI: https://doi.org/10.3803/EnM.2021.502
- [Original]
- 2,654 View
- 76 Download

Letter
- Diabetes, Obesity and Metabolism
- Association of Protein Z with Prediabetes and Type 2 Diabetes (Endocrinol Metab 2021;36:637-46, Yun-Ui Bae et al.)
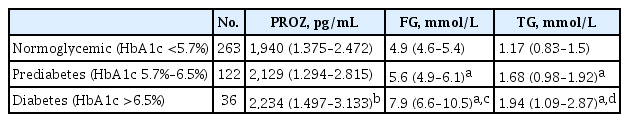
- Tiffany Pascreau, Maia Tchikviladze, Emilie Jolly, Sara Zia-Chahabi, Bertrand Lapergue, Marc Vasse
- Endocrinol Metab. 2021;36(5):1147-1148. Published online August 25, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1204
- 5,151 View
- 91 Download

Brief Report
- Diabetes, Obesity and Metabolism
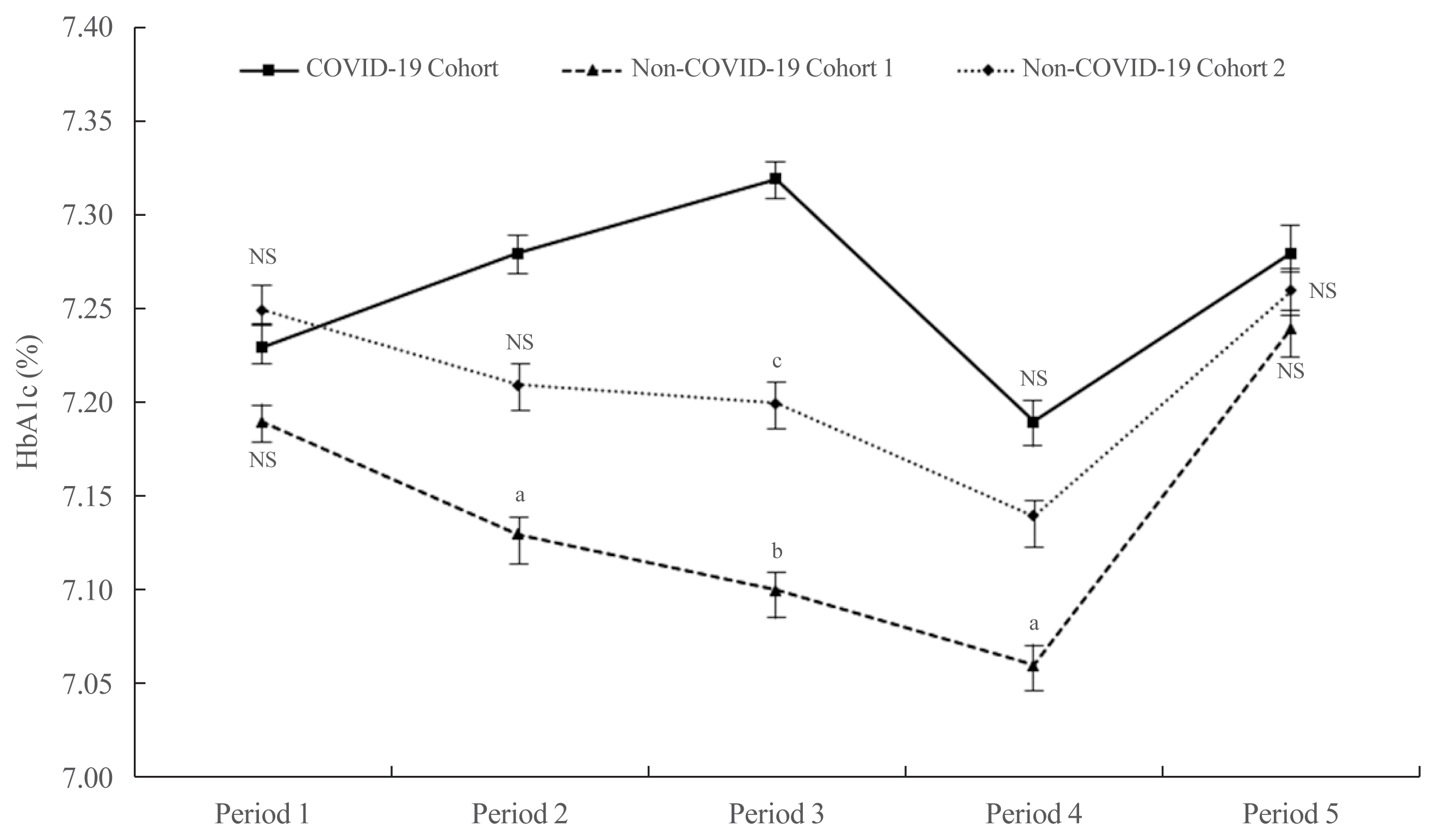
- Year-Long Trend in Glycated Hemoglobin Levels in Patients with Type 2 Diabetes during the COVID-19 Pandemic
- Jonghwa Jin, Seong Wook Lee, Won-Ki Lee, Jae-Han Jeon, Jung-Guk Kim, In-Kyu Lee, Yeon-Kyung Choi, Keun-Gyu Park
- Endocrinol Metab. 2021;36(5):1142-1146. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1154
- 3,835 View
- 148 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - It has been suggested that the coronavirus disease 2019 (COVID-19) pandemic has had a negative impact on glycemic control in patients with type 2 diabetes mellitus (T2DM). However, no study has examined yearly trends in glycated hemoglobin (HbA1c) levels after the start of the COVID-19 outbreak. Here, we performed a retrospective analysis of HbA1c concentrations during the early period of the COVID-19 outbreak (COVID-19 cohort) and then compared the yearly trend in the mean HbA1c level, along with fluctuations in HbA1c levels, with those during previous years (non-COVID-19 cohorts). We observed that the mean HbA1c level in patients with T2DM increased during the first 6 months of the COVID-19 outbreak. After 6 months, HbA1c levels in the COVID-19 cohort returned to levels seen in the non-COVID-19 cohorts. The data suggest that vulnerable patients with T2DM should be monitored closely during the early period of a pandemic to ensure they receive appropriate care.
-
Citations
Citations to this article as recorded by- A Hybrid Model of In-Person and Telemedicine Diabetes Education and Care for Management of Patients with Uncontrolled Type 2 Diabetes Mellitus: Findings and Implications from a Multicenter Prospective Study
Ayla M. Tourkmani, Turki J. Alharbi, Abdulaziz M. Bin Rsheed, Azzam F. Alotaibi, Mohammed S. Aleissa, Sultan Alotaibi, Amal S. Almutairi, Jancy Thomson, Ahlam S. Alshahrani, Hadil S. Alroyli, Hend M. Almutairi, Mashael A. Aladwani, Eman R. Alsheheri, Hyfa
Telemedicine Reports.2024; 5(1): 46. CrossRef - The indirect impact of the COVID-19 pandemic on people with type 2 diabetes mellitus and without COVID-19 infection: Systematic review and meta-analysis
Zhuoran Hu, Hin Moi Youn, Jianchao Quan, Lily Luk Siu Lee, Ivy Lynn Mak, Esther Yee Tak Yu, David Vai-Kiong Chao, Welchie Wai Kit Ko, Ian Chi Kei Wong, Gary Kui Kai Lau, Chak Sing Lau, Cindy Lo Kuen Lam, Eric Yuk Fai Wan
Primary Care Diabetes.2023; 17(3): 229. CrossRef - Evaluating Effects of Virtual Diabetes Group Visits in Community Health Centers During the COVID-19 Pandemic
Tracy Dinh, Erin M Staab, Daisy Nuñez, Mengqi Zhu, Wen Wan, Cynthia T Schaefer, Amanda Campbell, Michael Quinn, Arshiya A Baig
Journal of Patient Experience.2023;[Epub] CrossRef - Cardiovascular-related health behavior changes: lessons from the COVID-19 pandemic and post-pandemic challenges
Inha Jung, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(4): 99. CrossRef
- A Hybrid Model of In-Person and Telemedicine Diabetes Education and Care for Management of Patients with Uncontrolled Type 2 Diabetes Mellitus: Findings and Implications from a Multicenter Prospective Study

Original Articles
- Adrenal Gland
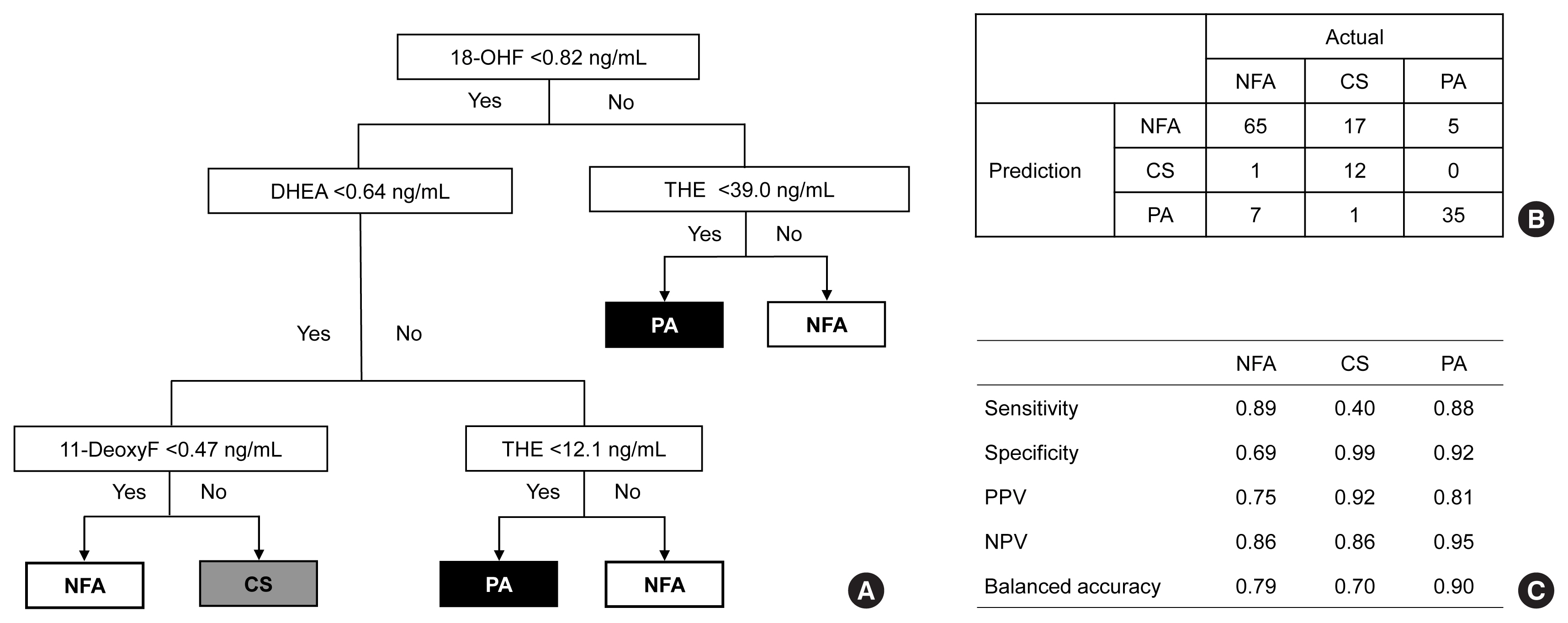
- Metabolic Subtyping of Adrenal Tumors: Prospective Multi-Center Cohort Study in Korea
- Eu Jeong Ku, Chaelin Lee, Jaeyoon Shim, Sihoon Lee, Kyoung-Ah Kim, Sang Wan Kim, Yumie Rhee, Hyo-Jeong Kim, Jung Soo Lim, Choon Hee Chung, Sung Wan Chun, Soon-Jib Yoo, Ohk-Hyun Ryu, Ho Chan Cho, A Ram Hong, Chang Ho Ahn, Jung Hee Kim, Man Ho Choi
- Endocrinol Metab. 2021;36(5):1131-1141. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1149
- 5,033 View
- 208 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Conventional diagnostic approaches for adrenal tumors require multi-step processes, including imaging studies and dynamic hormone tests. Therefore, this study aimed to discriminate adrenal tumors from a single blood sample based on the combination of liquid chromatography-mass spectrometry (LC-MS) and machine learning algorithms in serum profiling of adrenal steroids.
Methods
The LC-MS-based steroid profiling was applied to serum samples obtained from patients with nonfunctioning adenoma (NFA, n=73), Cushing’s syndrome (CS, n=30), and primary aldosteronism (PA, n=40) in a prospective multicenter study of adrenal disease. The decision tree (DT), random forest (RF), and extreme gradient boost (XGBoost) were performed to categorize the subtypes of adrenal tumors.
Results
The CS group showed higher serum levels of 11-deoxycortisol than the NFA group, and increased levels of tetrahydrocortisone (THE), 20α-dihydrocortisol, and 6β-hydroxycortisol were found in the PA group. However, the CS group showed lower levels of dehydroepiandrosterone (DHEA) and its sulfate derivative (DHEA-S) than both the NFA and PA groups. Patients with PA expressed higher serum 18-hydroxycortisol and DHEA but lower THE than NFA patients. The balanced accuracies of DT, RF, and XGBoost for classifying each type were 78%, 96%, and 97%, respectively. In receiver operating characteristics (ROC) analysis for CS, XGBoost, and RF showed a significantly greater diagnostic power than the DT. However, in ROC analysis for PA, only RF exhibited better diagnostic performance than DT.
Conclusion
The combination of LC-MS-based steroid profiling with machine learning algorithms could be a promising one-step diagnostic approach for the classification of adrenal tumor subtypes. -
Citations
Citations to this article as recorded by- Treating Primary Aldosteronism-Induced Hypertension: Novel Approaches and Future Outlooks
Nathan Mullen, James Curneen, Padraig T Donlon, Punit Prakash, Irina Bancos, Mark Gurnell, Michael C Dennedy
Endocrine Reviews.2024; 45(1): 125. CrossRef - Steroid profiling in adrenal disease
Danni Mu, Dandan Sun, Xia Qian, Xiaoli Ma, Ling Qiu, Xinqi Cheng, Songlin Yu
Clinica Chimica Acta.2024; 553: 117749. CrossRef - Serum and hair steroid profiles in patients with nonfunctioning pituitary adenoma undergoing surgery: A prospective observational study
Seung Shin Park, Yong Hwy Kim, Ho Kang, Chang Ho Ahn, Dong Jun Byun, Man Ho Choi, Jung Hee Kim
The Journal of Steroid Biochemistry and Molecular Biology.2023; 230: 106276. CrossRef - Recent Updates on the Management of Adrenal Incidentalomas
Seung Shin Park, Jung Hee Kim
Endocrinology and Metabolism.2023; 38(4): 373. CrossRef - LC-MS based simultaneous profiling of adrenal hormones of steroids, catecholamines, and metanephrines
Jongsung Noh, Chaelin Lee, Jung Hee Kim, Seung Woon Myung, Man Ho Choi
Journal of Lipid Research.2023; 64(11): 100453. CrossRef - 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung
Endocrinology and Metabolism.2023; 38(6): 597. CrossRef - Toward Systems-Level Metabolic Analysis in Endocrine Disorders and Cancer
Aliya Lakhani, Da Hyun Kang, Yea Eun Kang, Junyoung O. Park
Endocrinology and Metabolism.2023; 38(6): 619. CrossRef - Prevalence and Characteristics of Adrenal Tumors in an Unselected Screening Population
Ying Jing, Jinbo Hu, Rong Luo, Yun Mao, Zhixiao Luo, Mingjun Zhang, Jun Yang, Ying Song, Zhengping Feng, Zhihong Wang, Qingfeng Cheng, Linqiang Ma, Yi Yang, Li Zhong, Zhipeng Du, Yue Wang, Ting Luo, Wenwen He, Yue Sun, Fajin Lv, Qifu Li, Shumin Yang
Annals of Internal Medicine.2022; 175(10): 1383. CrossRef
- Treating Primary Aldosteronism-Induced Hypertension: Novel Approaches and Future Outlooks

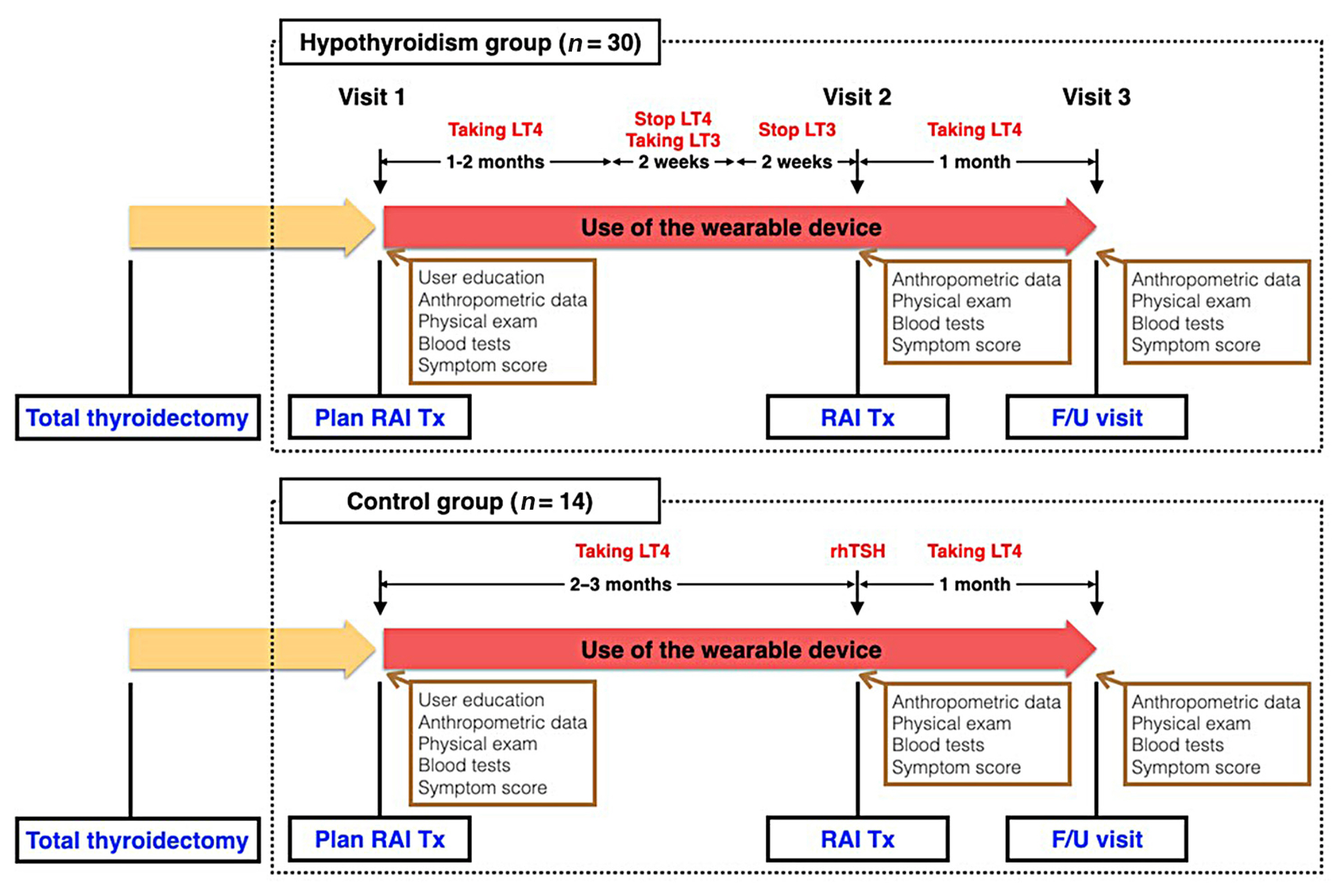
- Thyroid
- Association between Thyroid Function and Heart Rate Monitored by Wearable Devices in Patients with Hypothyroidism
- Ki-Hun Kim, Juhui Lee, Chang Ho Ahn, Hyeong Won Yu, June Young Choi, Ho-Young Lee, Won Woo Lee, Jae Hoon Moon
- Endocrinol Metab. 2021;36(5):1121-1130. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1216
- 5,375 View
- 155 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Heart rate (HR) monitored by a wearable device (WD) has demonstrated its clinical feasibility for thyrotoxicosis subjects. However, the association of HR monitored by wearables with hypothyroidism has not been examined. We assessed the association between serum thyroid hormone concentration and three WD-HR parameters in hypothyroid subjects.
Methods
Forty-four subjects scheduled for radioactive iodine therapy (RAI Tx) after thyroid cancer surgery were included. Thirty subjects were prepared for RAI Tx by thyroid hormone withdrawal (hypothyroidism group) and 14 subjects by recombinant human thyrotropin (control group). Three WD-HR parameters were calculated from the HR data collected during rest, during sleep, and from 2:00 AM to 6:00 AM, respectively. We analyzed the changes in conventionally measured resting HR (On-site rHR) and WDHR parameters relative to thyroid hormone levels.
Results
Serum free thyroxine (T4) levels, On-site rHR, and WD-HR parameters were lower in the hypothyroid group than in the control group at the time of RAI Tx. WD-HR parameters also reflected minute changes in free T4 levels. A decrease in On-site rHR and WD-HR parameters by one standard deviation (On-site rHR, approximately 12 bpm; WD-HR parameters, approximately 8 bpm) was associated with a 0.2 ng/dL decrease in free T4 levels (P<0.01) and a 2-fold increase of the odds ratio of hypothyroidism (P<0.01). WD-HR parameters displayed a better goodness-of-fit measure (lower quasi-information criterion value) than On-site rHR in predicting the hypothyroidism.
Conclusion
This study identified WD-HR parameters as informative and easy-to-measure biomarkers to predict hypothyroidism. -
Citations
Citations to this article as recorded by- Application of wearables for remote monitoring of oncology patients: A scoping review
Katharina Cloß, Marlo Verket, Dirk Müller-Wieland, Nikolaus Marx, Katharina Schuett, Edgar Jost, Martina Crysandt, Fabian Beier, Tim H Brümmendorf, Guido Kobbe, Julia Brandts, Malte Jacobsen
DIGITAL HEALTH.2024;[Epub] CrossRef - Thyroid hormone action during GABAergic neuron maturation: The quest for mechanisms
Sabine Richard, Juan Ren, Frédéric Flamant
Frontiers in Endocrinology.2023;[Epub] CrossRef - A machine learning-assisted system to predict thyrotoxicosis using patients’ heart rate monitoring data: a retrospective cohort study
Kyubo Shin, Jongchan Kim, Jaemin Park, Tae Jung Oh, Sung Hye Kong, Chang Ho Ahn, Joon Ho Moon, Min Joo Kim, Jae Hoon Moon
Scientific Reports.2023;[Epub] CrossRef
- Application of wearables for remote monitoring of oncology patients: A scoping review

- Thyroid
- Comparison of Korean vs. American Thyroid Imaging Reporting and Data System in Malignancy Risk Assessment of Indeterminate Thyroid Nodules
- Sunyoung Kang, Seul Ki Kwon, Hoon Sung Choi, Min Joo Kim, Young Joo Park, Do Joon Park, Sun Wook Cho
- Endocrinol Metab. 2021;36(5):1111-1120. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1208
- 3,959 View
- 126 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
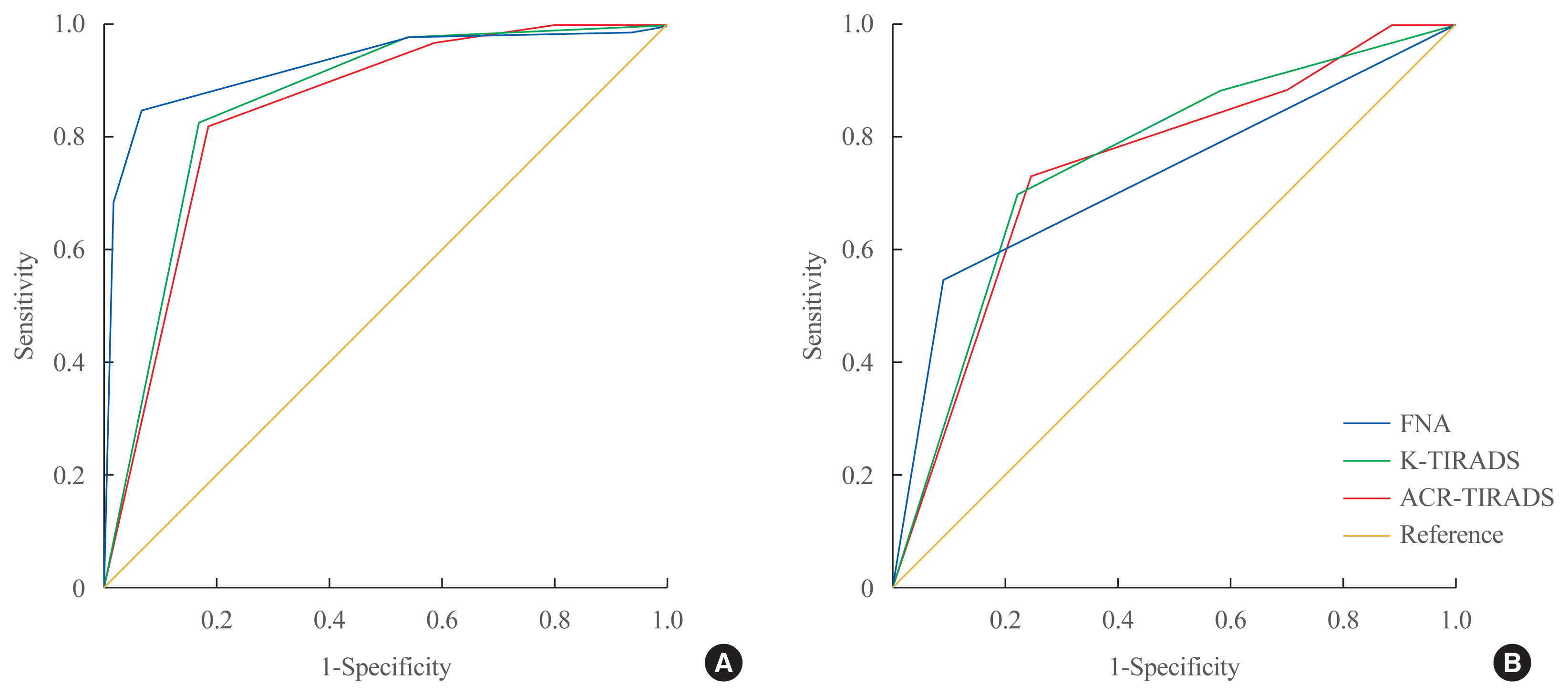
The management of cytologically indeterminate thyroid nodules is challenging for clinicians. This study aimed to compare the diagnostic performance of the Korean Thyroid Imaging Reporting and Data Systems (K-TIRADS) with that of the American College of Radiology (ACR)-TIRADS for predicting the malignancy risk of indeterminate thyroid nodules.
Methods
Thyroid nodules diagnosed by fine-needle aspiration (FNA) followed by surgery or core needle biopsy at a single referral hospital were enrolled.
Results
Among 200 thyroid nodules, 78 (39.0%) nodules were classified as indeterminate by FNA (Bethesda category III, IV, and V), and 114 (57.0%) nodules were finally diagnosed as malignancy by surgery or core needle biopsy. The area under the curve (AUC) was higher for FNA than for either TIRADS system in all nodules, while all three methods showed similar AUCs for indeterminate nodules. However, for Bethesda category III nodules, applying K-TIRADS 5 significantly increased the risk of malignancy compared to a cytological examination alone (50.0% vs. 26.5%, P=0.028), whereas applying ACR-TIRADS did not lead to a change.
Conclusion
K-TIRADS and ACR-TIRADS showed similar diagnostic performance in assessing indeterminate thyroid nodules, and K-TIRADS had beneficial effects for malignancy prediction in Bethesda category III nodules. -
Citations
Citations to this article as recorded by- Is the nodule location a predictive risk factor for cancer in AUS/FLUS thyroid nodules? A retrospective cohort study
Saad M. Alqahtani, Bassam A. Altalhi, Yousef S. Alalawi, Saif S. Al-Sobhi
Asian Journal of Surgery.2024;[Epub] CrossRef - Diagnostic Performance of Various Ultrasound Risk Stratification Systems for Benign and Malignant Thyroid Nodules: A Meta-Analysis
Ji-Sun Kim, Byung Guk Kim, Gulnaz Stybayeva, Se Hwan Hwang
Cancers.2023; 15(2): 424. CrossRef - The impact of thyroid imaging reporting and data system on the management of Bethesda III thyroid nodules
Saad M. Alqahtani, Saif S. Al-Sobhi, Mohammed A. Alturiqy, Riyadh I. Alsalloum, Hindi N. Al-Hindi
Journal of Taibah University Medical Sciences.2023; 18(3): 506. CrossRef - Diagnostic Performance of Six Ultrasound Risk Stratification Systems for Thyroid Nodules: A Systematic Review and Network Meta-Analysis
Do Hyun Kim, Sung Won Kim, Mohammed Abdullah Basurrah, Jueun Lee, Se Hwan Hwang
American Journal of Roentgenology.2023; 220(6): 791. CrossRef - Diagnostic efficiency among Eu-/C-/ACR-TIRADS and S-Detect for thyroid nodules: a systematic review and network meta-analysis
Longtao Yang, Cong Li, Zhe Chen, Shaqi He, Zhiyuan Wang, Jun Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Comparison of diagnostic performance of two ultrasound risk stratification systems for thyroid nodules: a systematic review and meta-analysis
Yun Jin Kang, Hee Sun Ahn, Gulnaz Stybayeva, Ju Eun Lee, Se Hwan Hwang
La radiologia medica.2023; 128(11): 1407. CrossRef - Diagnostic Performance of ACR and Kwak TI-RADS for Benign and Malignant Thyroid Nodules: An Update Systematic Review and Meta-Analysis
Yun Jin Kang, Gulnaz Stybayeya, Ju Eun Lee, Se Hwan Hwang
Cancers.2022; 14(23): 5961. CrossRef - Comparison of Thyroid Imaging Reporting and Data Systems in Malignancy Risk Stratification of Indeterminate Thyroid Nodules
Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(5): 974. CrossRef
- Is the nodule location a predictive risk factor for cancer in AUS/FLUS thyroid nodules? A retrospective cohort study

- Thyroid
- Lobeglitazone, A Peroxisome Proliferator-Activated Receptor-Gamma Agonist, Inhibits Papillary Thyroid Cancer Cell Migration and Invasion by Suppressing p38 MAPK Signaling Pathway
- Jun-Qing Jin, Jeong-Sun Han, Jeonghoon Ha, Han-Sang Baek, Dong-Jun Lim
- Endocrinol Metab. 2021;36(5):1095-1110. Published online October 14, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1155
- 4,692 View
- 159 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
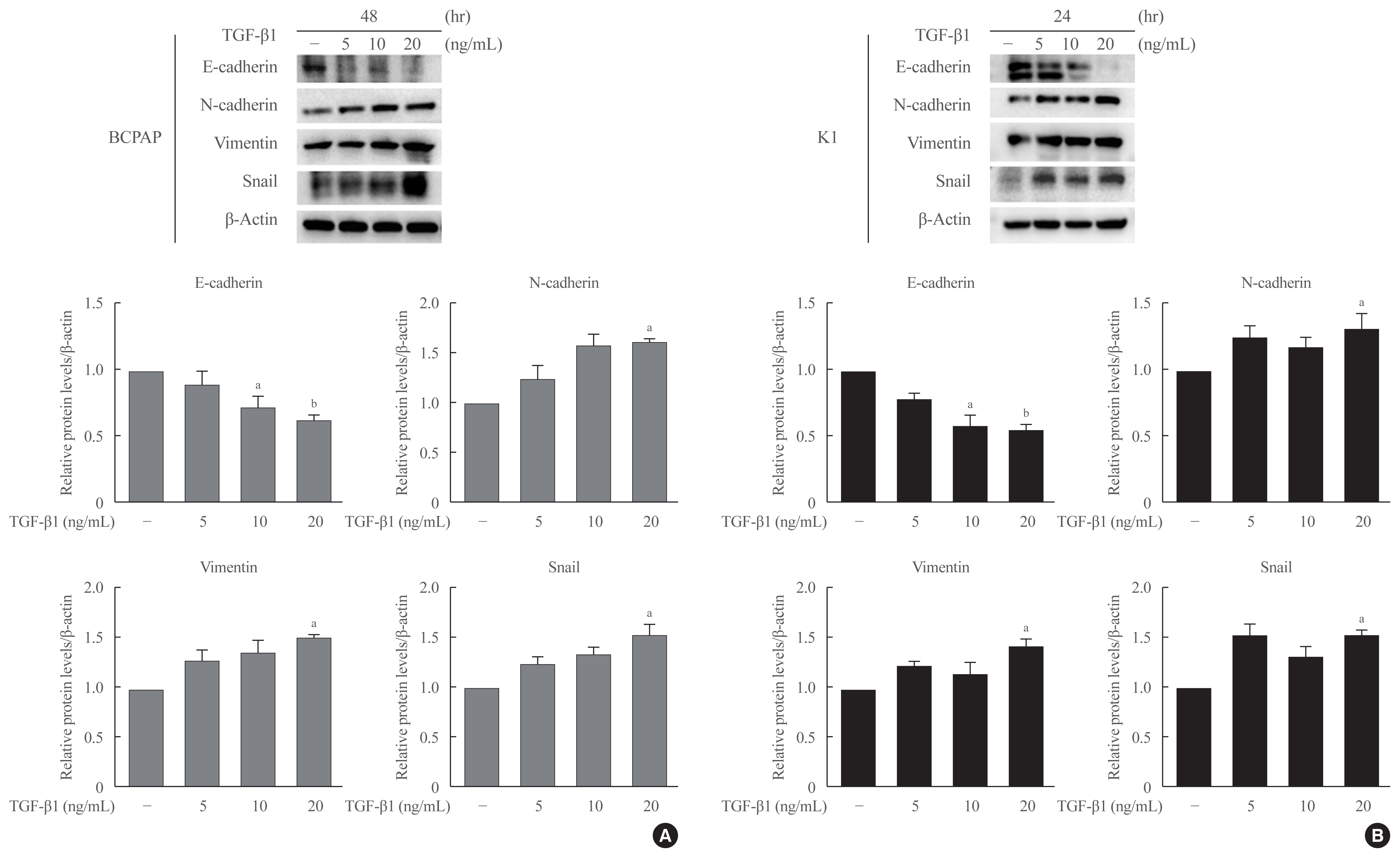
Peroxisome proliferator-activated receptor-gamma (PPAR-γ) ligands have been widely shown to correlate with epithelial-mesenchymal transition (EMT) and cancer progression. Lobeglitazone (LGZ) is a novel ligand of PPAR-γ; and its role in EMT and metastasis in papillary thyroid carcinoma (PTC) is poorly understood. We aimed to investigate the role of LGZ in metastatic behavior of PTC cells.
Methods
Half maximal inhibitory concentration (IC50) values of LGZ in BRAF-mutated PTC cell lines (BCPAP and K1) were determined using MTT assay. Rosiglitazone (RGZ), the PPAR-γ ligand was used as a positive control. The protein expression of PPAR-γ, cell-surface proteins (E-cadherin, N-cadherin), cytoskeletal protein (Vimentin), transcription factor (Snail), p38 mitogenactivated protein kinase (MAPK), extracellular signal-regulated kinase (ERK) 1/2 pathway, and matrix metalloproteinase (MMP)-2 expression were measured using Western blotting. Changes in E-cadherin expression were also determined using immunocytochemistry. Cell migration and invasion were analyzed using wound healing and Matrigel invasion assays.
Results
Treatment with LGZ or RGZ significantly inhibited transforming growth factor-beta1 (TGF-β1)-induced EMT-associated processes such as fibroblast-like morphological changes, EMT-related protein expression, and increased cell migration and invasion in BCPAP and K1 cells. LGZ restored TGF-β1-induced loss of E-cadherin, as observed using immunocytochemistry. Furthermore, LGZ and RGZ suppressed TGF-β1-induced MMP-2 expression and phosphorylation of p38 MAPK, but not ERK1/2. Although there was no change in PPAR-γ expression after treatment with LGZ or RGZ, the effect of downstream processes mediated by LGZ was hampered by GW9662, a PPAR-γ antagonist.
Conclusion
LGZ inhibits TGF-β1-induced EMT, migration, and invasion through the p38 MAPK signaling pathway in a PPAR-γ-dependent manner in PTC cells. -
Citations
Citations to this article as recorded by- Diabetes Mellitus and Thyroid Cancers: Risky Correlation, Underlying Mechanisms and Clinical Prevention
Rongqian Wu, Junping Zhang, Guilin Zou, Shanshan Li, Jinying Wang, Xiaoxinlei Li, Jixiong Xu
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 809. CrossRef - Clinicopathological Evaluation of Papillary Thyroid Microcarcinoma
Ando Takahito, Kimihito Fujii, Hirona Banno, Masayuki Saito, Yukie Ito, Mirai Ido, Manami Goto, Yukako Mouri, Junko Kousaka, Tsuneo Imai, Shogo Nakano
Cureus.2024;[Epub] CrossRef - Pioglitazone, a peroxisome proliferator‑activated receptor γ agonist, induces cell death and inhibits the proliferation of hypoxic HepG2 cells by promoting excessive production of reactive oxygen species
Guohao Huang, Mengfan Zhang, Manzhou Wang, Wenze Xu, Xuhua Duan, Xinwei Han, Jianzhuang Ren
Oncology Letters.2024;[Epub] CrossRef - The Activation of PPARγ by (2Z,4E,6E)-2-methoxyocta-2,4,6-trienoic Acid Counteracts the Epithelial–Mesenchymal Transition Process in Skin Carcinogenesis
Enrica Flori, Sarah Mosca, Giorgia Cardinali, Stefania Briganti, Monica Ottaviani, Daniela Kovacs, Isabella Manni, Mauro Truglio, Arianna Mastrofrancesco, Marco Zaccarini, Carlo Cota, Giulia Piaggio, Mauro Picardo
Cells.2023; 12(7): 1007. CrossRef - Cumulative exposure to metabolic syndrome increases thyroid cancer risk in young adults: a population-based cohort study
Jinyoung Kim, Kyungdo Han, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
The Korean Journal of Internal Medicine.2023; 38(4): 526. CrossRef - Drug repositioning in thyroid cancer treatment: the intriguing case of anti-diabetic drugs
Alessia Greco, Francesca Coperchini, Laura Croce, Flavia Magri, Marsida Teliti, Mario Rotondi
Frontiers in Pharmacology.2023;[Epub] CrossRef - Fish and the Thyroid: A Janus Bifrons Relationship Caused by Pollutants and the Omega-3 Polyunsaturated Fatty Acids
Salvatore Benvenga, Fausto Famà, Laura Giovanna Perdichizzi, Alessandro Antonelli, Gabriela Brenta, Francesco Vermiglio, Mariacarla Moleti
Frontiers in Endocrinology.2022;[Epub] CrossRef - Identifying and categorizing compounds that reduce corneal transforming growth factor beta induced protein levels: a scoping review
Gabriella Guo Sciriha, Janet Sultana, Joseph Borg
Expert Review of Clinical Pharmacology.2022; 15(12): 1423. CrossRef
- Diabetes Mellitus and Thyroid Cancers: Risky Correlation, Underlying Mechanisms and Clinical Prevention

- Thyroid
- Whole-Exome Sequencing in Papillary Microcarcinoma: Potential Early Biomarkers of Lateral Lymph Node Metastasis
- Mijin Kim, Chae Hwa Kwon, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, Kyung-Un Choi, In Joo Kim, Meeyoung Park, Bo Hyun Kim
- Endocrinol Metab. 2021;36(5):1086-1094. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1132
- 3,562 View
- 108 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
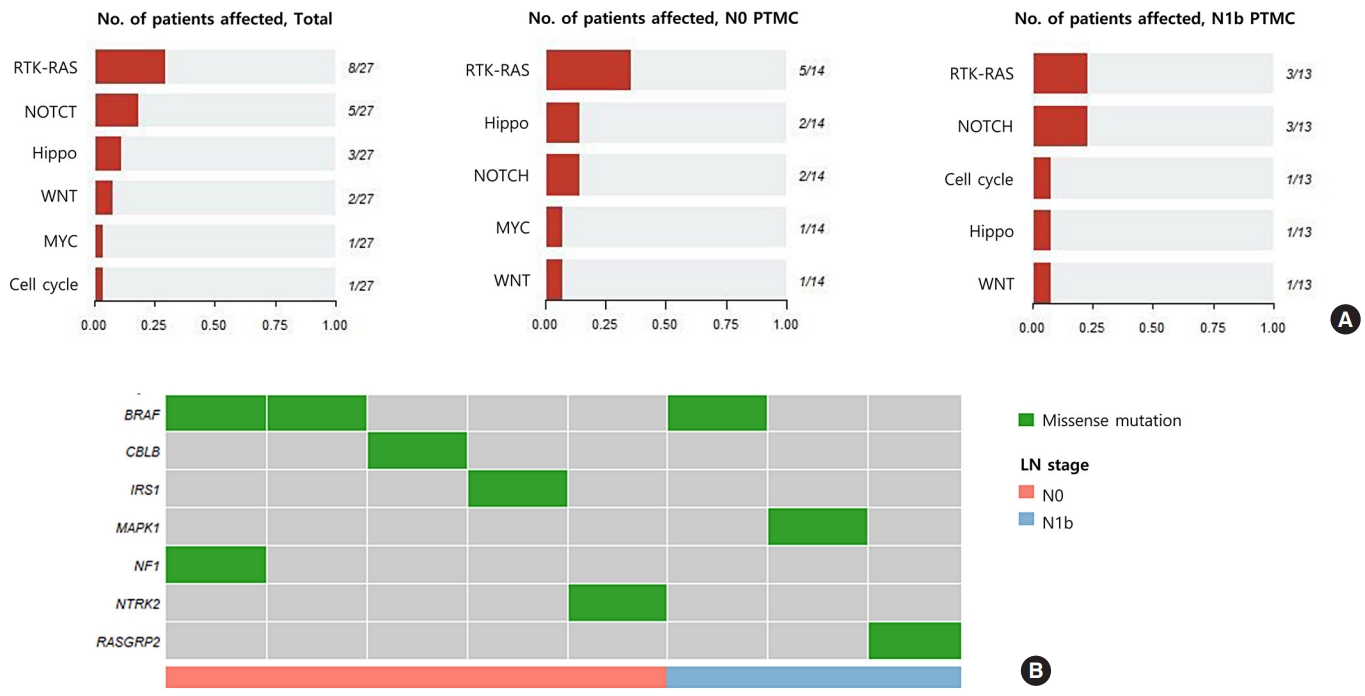
Early identification of patients with high-risk papillary thyroid microcarcinoma (PTMC) that is likely to progress has become a critical challenge. We aimed to identify somatic mutations associated with lateral neck lymph node (LN) metastasis (N1b) in patients with PTMC.
Methods
Whole-exome sequencing (WES) of 14 PTMCs with no LN metastasis (N0) and 13 N1b PTMCs was performed using primary tumors and matched normal thyroid tissues.
Results
The mutational burden was comparable in N0 and N1b tumors, as the median number of mutations was 23 (range, 12 to 46) in N0 and 24 (range, 12 to 50) in N1b PTMC (P=0.918). The most frequent mutations were detected in PGS1, SLC4A8, DAAM2, and HELZ in N1b PTMCs alone, and the K158Q mutation in PGS1 (four patients, Fisher’s exact test P=0.041) was significantly enriched in N1b PTMCs. Based on pathway analysis, somatic mutations belonging to the receptor tyrosine kinase-RAS and NOTCH pathways were most frequently affected in N1b PTMCs. We identified four mutations that are predicted to be pathogenic in four genes based on Clinvar and Combined Annotation-Dependent Depletion score: BRAF, USH2A, CFTR, and PHIP. A missense mutation in CFTR and a nonsense mutation in PHIP were detected in N1b PTMCs only, although in one case each. BRAF mutation was detected in both N0 and N1b PTMCs.
Conclusion
This first comprehensive WES analysis of the mutational landscape of N0 and N1b PTMCs identified pathogenic genes that affect biological functions associated with the aggressive phenotype of PTMC. -
Citations
Citations to this article as recorded by- What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?
Bobby White, Pawel Swietach
Pflügers Archiv - European Journal of Physiology.2024; 476(4): 673. CrossRef - Feasibility of whole‐exome sequencing in fine‐needle aspiration specimens of papillary thyroid microcarcinoma for the identification of novel gene mutations
Liyuan Ma, Luying Gao, Ya Hu, Xiaoyi Li, Chunhao Liu, Jiang Ji, Xinlong Shi, Aonan Pan, Yuang An, Nengwen Luo, Yu Xia, Yuxin Jiang
Clinical Genetics.2024; 105(5): 567. CrossRef - Multi-omics analysis reveals a molecular landscape of the early recurrence and early metastasis in pan-cancer
Dan-ni He, Na Wang, Xiao-Ling Wen, Xu-Hua Li, Yu Guo, Shu-heng Fu, Fei-fan Xiong, Zhe-yu Wu, Xu Zhu, Xiao-ling Gao, Zhen-zhen Wang, Hong-jiu Wang
Frontiers in Genetics.2023;[Epub] CrossRef - Comprehensive Long-Read Sequencing Analysis Discloses the Transcriptome Features of Papillary Thyroid Microcarcinoma
Yanqiang Wang, Binbin Zou, Yanyan Zhang, Jin Zhang, Shujing Li, Bo Yu, Zhekun An, Lei Li, Siqian Cui, Yutong Zhang, Jiali Yao, Xiuzhi Shi, Jing Liu
The Journal of Clinical Endocrinology & Metabolism.2023;[Epub] CrossRef
- What can we learn about acid-base transporters in cancer from studying somatic mutations in their genes?

- Thyroid
- Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(5):1078-1085. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1151

- 3,838 View
- 110 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Hürthle cell carcinoma (HCC), a type of thyroid carcinoma, is rare in South Korea, and few studies have investigated its prognosis.
Methods
This long-term multicenter retrospective cohort study evaluated the clinicopathological features and clinical outcomes in patients with HCC who underwent thyroid surgery between 1996 and 2009.
Results
The mean age of the 97 patients included in the study was 50.3 years, and 26.8% were male. The mean size of the primary tumor was 3.2±1.8 cm, and three (3.1%) patients had distant metastasis at initial diagnosis. Ultrasonographic findings were available for 73 patients; the number of nodules with low-, intermediate-, and high suspicion was 28 (38.4%), 27 (37.0%), and 18 (24.7%), respectively, based on the Korean-Thyroid Imaging Reporting and Data System. Preoperatively, follicular neoplasm (FN) or suspicion for FN accounted for 65.2% of the cases according to the Bethesda category, and 13% had malignancy or suspicious for malignancy. During a median follow-up of 8.5 years, eight (8.2%) patients had persistent/recurrent disease, and none died of HCC. Older age, gross extrathyroidal extension (ETE), and widely invasive types of tumors were significantly associated with distant metastasis (all P<0.01). Gross ETE (hazard ratio [HR], 27.7; 95% confidence interval [CI], 2.2 to 346.4; P=0.01) and widely invasive classification (HR, 6.5; 95% CI, 1.1 to 39.4; P=0.04) were independent risk factors for poor disease-free survival (DFS).
Conclusion
The long-term prognosis of HCC is relatively favorable in South Korea from this study, although this is not a nation-wide data, and gross ETE and widely invasive cancer are significant prognostic factors for DFS. The diagnosis of HCC by ultrasonography and cytopathology remains challenging. -
Citations
Citations to this article as recorded by- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma
Lindsay A. Bischoff, Ian Ganly, Laura Fugazzola, Erin Buczek, William C. Faquin, Bryan R. Haugen, Bryan McIver, Caitlin P. McMullen, Kate Newbold, Daniel J. Rocke, Marika D. Russell, Mabel Ryder, Peter M. Sadow, Eric Sherman, Maisie Shindo, David C. Shonk
JAMA Otolaryngology–Head & Neck Surgery.2024; 150(3): 265. CrossRef - Oncocytic carcinoma of the thyroid: Conclusions from a 20‐year patient cohort
Nelson R. Gruszczynski, Shahzeb S. Hasan, Ana G. Brennan, Julian De La Chapa, Adithya S. Reddy, David N. Martin, Prem P. Batchala, Edward B. Stelow, Eric M. Dowling, Katherine L. Fedder, Jonathan C. Garneau, David C. Shonka
Head & Neck.2024;[Epub] CrossRef - Hurthle cell carcinoma: a rare variant of thyroid malignancy – a case report
Yuvraj Adhikari, Anupama Marasini, Nawaraj Adhikari, Laxman D. Paneru, Binit Upadhaya Regmi, Manita Raut
Annals of Medicine & Surgery.2023; 85(5): 1940. CrossRef - Hürthle Cell Carcinoma: Single Center Analysis and Considerations for Surgical Management Based on the Recent Literature
Costanza Chiapponi, Milan J.M. Hartmann, Matthias Schmidt, Michael Faust, Christiane J. Bruns, Anne M. Schultheis, Hakan Alakus
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Risk of Diabetes in Subjects with Positive Fecal Immunochemical Test: A Nationwide Population-Based Study
- Kwang Woo Kim, Hyun Jung Lee, Kyungdo Han, Jung Min Moon, Seung Wook Hong, Eun Ae Kang, Jooyoung Lee, Hosim Soh, Seong-Joon Koh, Jong Pil Im, Joo Sung Kim
- Endocrinol Metab. 2021;36(5):1069-1077. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1119
- 3,595 View
- 97 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
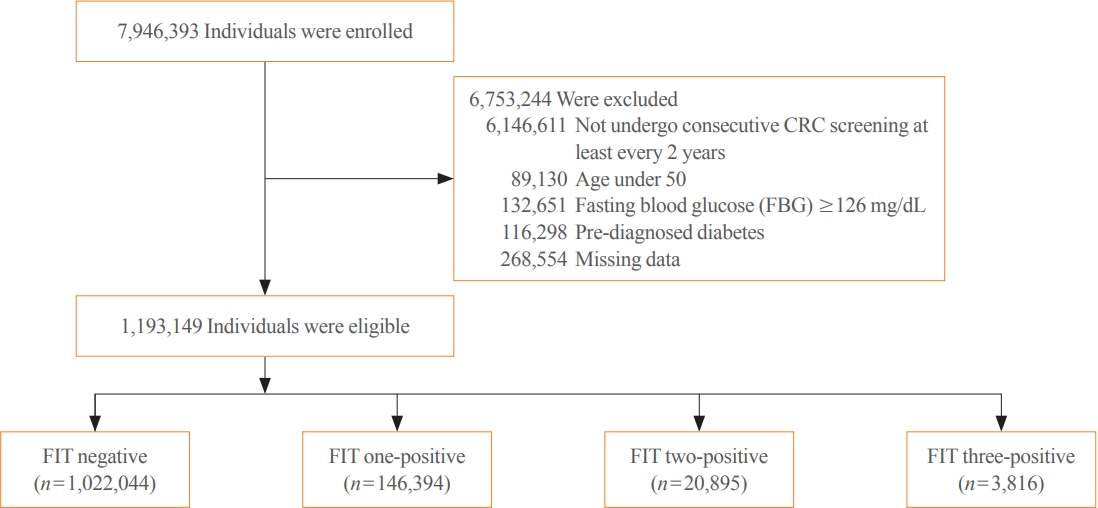
Positive fecal immunochemical test (FIT) results have been recently suggested as a risk factor for systemic inflammation. Diabetes induces inflammation in the gastrointestinal tract via several ways. We investigated the association between FIT results and the incidence of diabetes.
Methods
A total of 7,946,393 individuals aged ≥50 years from the National Cancer Screening Program database who underwent FIT for colorectal cancer (CRC) screening from 2009 to 2012 were enrolled. The primary outcome was newly diagnosed diabetes based on the International Classification of Disease 10th revision codes and administration of anti-diabetic medication during the follow-up period.
Results
During a mean follow-up of 6.5 years, the incidence rates of diabetes were 11.97, 13.60, 14.53, and 16.82 per 1,000 personyears in the FIT negative, one-positive, two-positive, and three-positive groups, respectively. The hazard ratios (HRs) for the incidence of diabetes were 1.14 (95% confidence interval [CI], 1.12 to 1.16; HR, 1.21; 95% CI, 1.16 to 1.27; and HR, 1.40; 95% CI, 1.28 to 1.55) in the one-positive, two-positive, and three-positive FIT groups compared with the FIT negative group, respectively. The effect was consistent in individuals with normal fasting blood glucose (adjusted HR 1.55 vs. 1.14, P for interaction <0.001).
Conclusion
Positive FIT results were associated with a significantly higher risk of diabetes, suggesting that the FIT can play a role not only as a CRC screening tool, but also as a surrogate marker of systemic inflammation; thus, increasing the diabetes risk. -
Citations
Citations to this article as recorded by- Uncovering a dose-response relationship between positive fecal immunochemical test (FIT) and all-cause, cardiovascular and cancer-related mortality
Chi Pang Wen, Min Kuang Tsai, June Han Lee, Hung Yi Chiou, Christopher Wen, Ta-Wei David Chu, Chien Hua Chen
European Journal of Internal Medicine.2024; 120: 69. CrossRef - Faecal haemoglobin concentrations are associated with all-cause mortality and cause of death in colorectal cancer screening
Lasse Kaalby, Ulrik Deding, Issam Al-Najami, Gabriele Berg-Beckhoff, Thomas Bjørsum-Meyer, Tinne Laurberg, Aasma Shaukat, Robert J. C. Steele, Anastasios Koulaouzidis, Morten Rasmussen, Morten Kobaek-Larsen, Gunnar Baatrup
BMC Medicine.2023;[Epub] CrossRef - Positive Results from the Fecal Immunochemical Test Can Be Related to Dementia: A Nationwide Population-Based Study in South Korea
Yu Kyung Jun, Seung Woo Lee, Kwang Woo Kim, Jung Min Moon, Seong-Joon Koh, Hyun Jung Lee, Joo Sung Kim, Kyungdo Han, Jong Pil Im
Journal of Alzheimer's Disease.2023; 91(4): 1515. CrossRef - Faecal Haemoglobin Estimated by Faecal Immunochemical Tests—An Indicator of Systemic Inflammation with Real Clinical Potential
Karen N. Barnett, Gavin R. C. Clark, Robert J. C. Steele, Callum G. Fraser
Diagnostics.2021; 11(11): 2093. CrossRef
- Uncovering a dose-response relationship between positive fecal immunochemical test (FIT) and all-cause, cardiovascular and cancer-related mortality

- Diabetes, Obesity and Metabolism
- Musclin Is Related to Insulin Resistance and Body Composition, but Not to Body Mass Index or Cardiorespiratory Capacity in Adults
- Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis Valbuena, Andrés F. Milán, María C. Trillos-Almanza, Sergio Granados, Miguel Peña, Mauricio Estrada-Castrillón, Juan C. Aristizábal, Raúl Narvez-Sanchez, Jaime Gallo-Villegas, Juan C. Calderón
- Endocrinol Metab. 2021;36(5):1055-1068. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1104
- 5,007 View
- 136 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We studied whether musclin function in humans is related to glycemic control, body composition, and cardiorespiratory capacity.
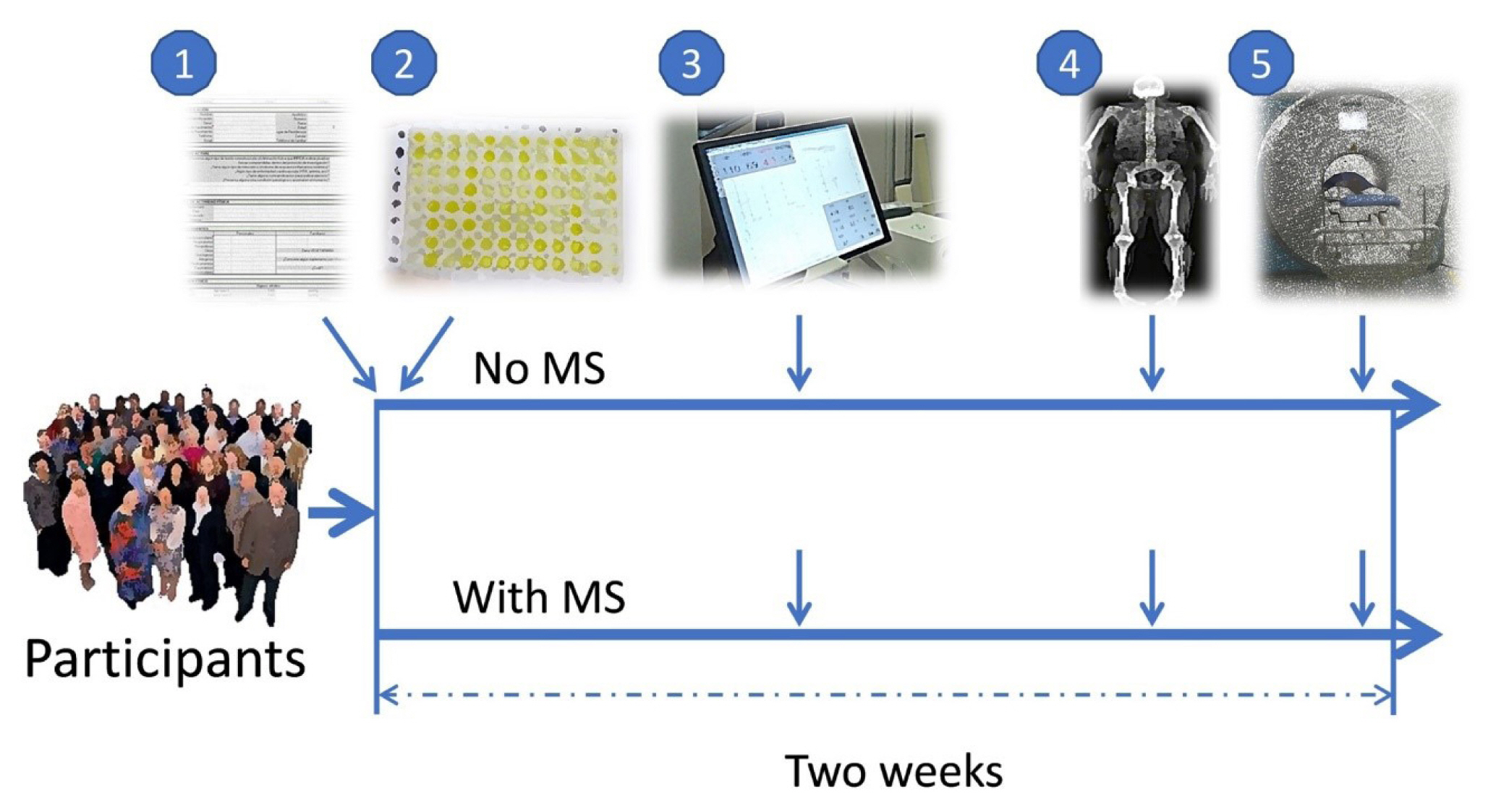
Methods
A cross-sectional study was performed in sedentary adults with or without metabolic syndrome (MS). Serum musclin was measured by enzyme-linked immunosorbent assay. Insulin resistance (IR) was evaluated by the homeostatic model assessment (HOMA-IR). Body composition was determined by dual-energy X-ray absorptiometry and muscle composition by measuring carnosine in the thigh, a surrogate of fiber types, through proton magnetic resonance spectroscopy. Cardiorespiratory capacity was assessed through direct ergospirometry.
Results
The control (n=29) and MS (n=61) groups were comparable in age (51.5±6.5 years old vs. 50.7±6.1 years old), sex (72.4% vs. 70.5% women), total lean mass (58.5%±7.4% vs. 57.3%±6.8%), and peak oxygen consumption (VOpeak) (31.0±5.8 mL O2./kg.min vs. 29.2±6.3 mL O2/kg.min). Individuals with MS had higher body mass index (BMI) (30.6±4.0 kg/m2 vs. 27.4± 3.6 kg/m2), HOMA-IR (3.5 [95% confidence interval, CI, 2.9 to 4.6] vs. 1.7 [95% CI, 1.1 to 2.0]), and musclin (206.7 pg/mL [95% CI, 122.7 to 387.8] vs. 111.1 pg/mL [95% CI, 63.2 to 218.5]) values than controls (P˂0.05). Musclin showed a significant relationship with HOMA-IR (β=0.23; 95% CI, 0.12 to 0.33; P˂0.01), but not with VOpeak, in multiple linear regression models adjusted for age, sex, fat mass, lean mass, and physical activity. Musclin was significantly associated with insulin, glycemia, visceral fat, and regional muscle mass, but not with BMI, VCO2peak, maximum heart rate, maximum time of work, or carnosine.
Conclusion
In humans, musclin positively correlates with insulinemia, IR, and a body composition profile with high visceral adiposity and lean mass, but low body fat percentage. Musclin is not related to BMI or cardiorespiratory capacity. -
Citations
Citations to this article as recorded by- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation
Wonjun Cho, Heeseung Oh, Sung Woo Choi, A. M. Abd El-Aty, Fatma Yeşilyurt, Ji Hoon Jeong, Tae Woo Jung
Inflammation.2024; 47(1): 1. CrossRef - Glucose restriction enhances oxidative fiber formation: A multi-omic signal network involving AMPK and CaMK2
Kaiyi Zhang, Ning Xie, Huaqiong Ye, Jiakun Miao, Boce Xia, Yu Yang, Huanqi Peng, Shuang Xu, Tianwen Wu, Cong Tao, Jinxue Ruan, Yanfang Wang, Shulin Yang
iScience.2024; 27(1): 108590. CrossRef - Myokines: metabolic regulation in obesity and type 2 diabetes
Zhi-Tian Chen, Zhi-Xuan Weng, Jiandie D Lin, Zhuo-Xian Meng
Life Metabolism.2024;[Epub] CrossRef - Epidemiological, mechanistic, and practical bases for assessment of cardiorespiratory fitness and muscle status in adults in healthcare settings
Jaime A. Gallo-Villegas, Juan C. Calderón
European Journal of Applied Physiology.2023; 123(5): 945. CrossRef - Serum Levels of Myonectin Are Lower in Adults with Metabolic Syndrome and Are Negatively Correlated with Android Fat Mass
Jorge L. Petro, María Carolina Fragozo-Ramos, Andrés F. Milán, Juan C. Aristizabal, Jaime A. Gallo-Villegas, Juan C. Calderón
International Journal of Molecular Sciences.2023; 24(8): 6874. CrossRef - The correlation of serum musclin with diabetic nephropathy
Jie Zhang, Jing Shi, Zengguang Cheng, Wenchao Hu
Cytokine.2023; 167: 156211. CrossRef - Efficacy of high-intensity interval- or continuous aerobic-training on insulin resistance and muscle function in adults with metabolic syndrome: a clinical trial
Jaime Gallo-Villegas, Leonardo A. Castro-Valencia, Laura Pérez, Daniel Restrepo, Oscar Guerrero, Sergio Cardona, Yeliana L. Sánchez, Manuela Yepes-Calderón, Luis H. Valbuena, Miguel Peña, Andrés F. Milán, Maria C. Trillos-Almanza, Sergio Granados, Juan C.
European Journal of Applied Physiology.2022; 122(2): 331. CrossRef - Reactive Oxygen and Nitrogen Species (RONS) and Cytokines—Myokines Involved in Glucose Uptake and Insulin Resistance in Skeletal Muscle
Paola Llanos, Jesus Palomero
Cells.2022; 11(24): 4008. CrossRef
- Musclin Mitigates the Attachment of HUVECs to THP-1 Monocytes in Hyperlipidemic Conditions through PPARα/HO-1-Mediated Attenuation of Inflammation

- Diabetes, Obesity and Metabolism
- Prognostic Value of Triglyceride and Glucose Index for Incident Type 2 Diabetes beyond Metabolic Health and Obesity
- Hwi Seung Kim, Jiwoo Lee, Yun Kyung Cho, Eun Hee Kim, Min Jung Lee, Hong-Kyu Kim, Joong-Yeol Park, Woo Je Lee, Chang Hee Jung
- Endocrinol Metab. 2021;36(5):1042-1054. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1184
- 5,214 View
- 132 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
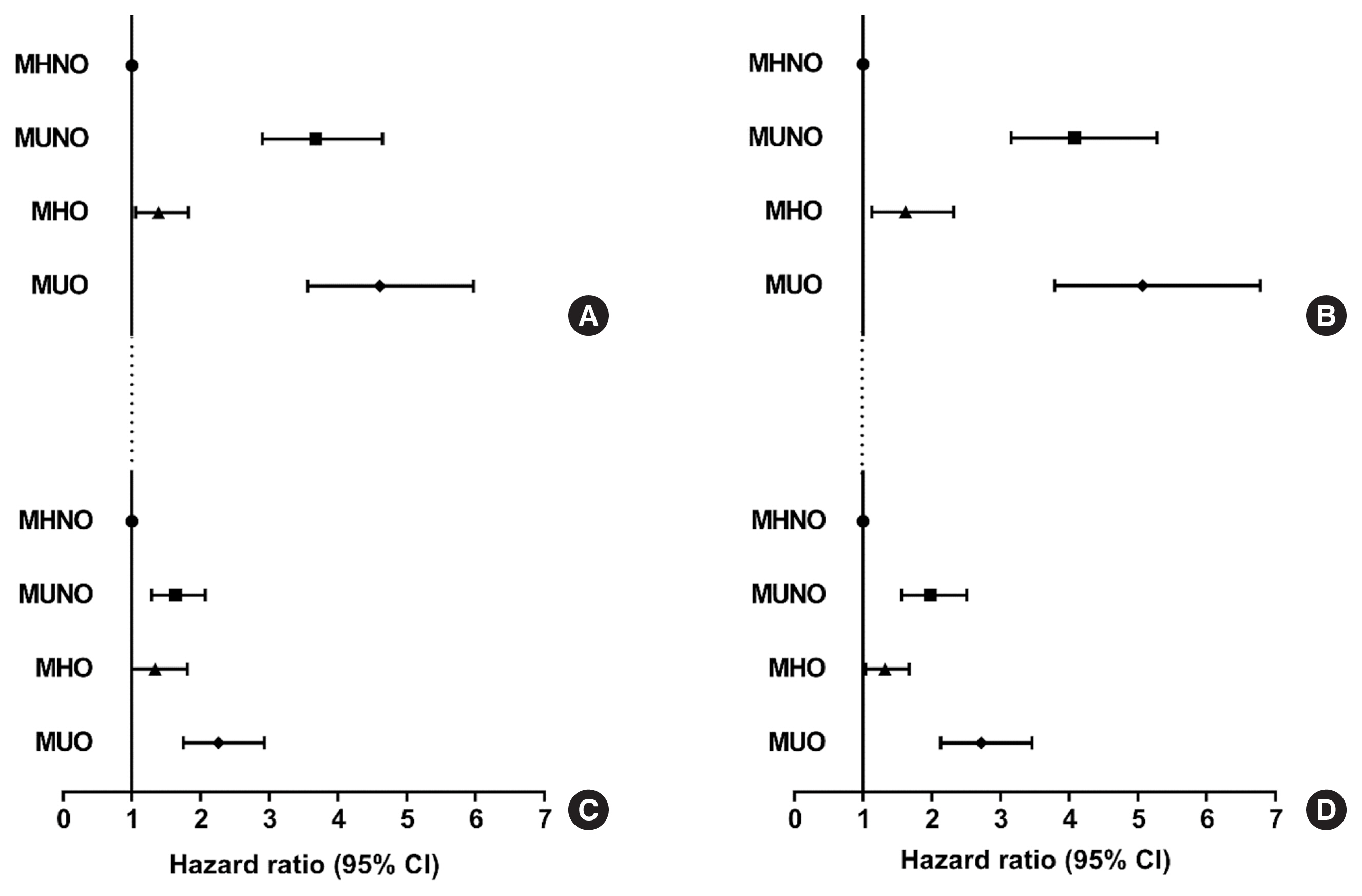
Metabolically healthy obese (MHO) phenotype is metabolically heterogeneous in terms of type 2 diabetes (T2D). Previously, the triglyceride and glucose (TyG) index has been considered for identifying metabolic health and future risk of T2D. This study aimed to evaluate the risk of incident T2D according to obesity status and metabolic health, categorized by four different criteria and the TyG index.
Methods
The study included 39,418 Koreans without T2D at baseline. The risk of T2D was evaluated based on four different definitions of metabolic health and obesity status and according to the baseline TyG index within each metabolic health and obesity group.
Results
During the median follow-up at 38.1 months, 726 individuals developed T2D. Compared with the metabolically healthy non-obese (MHNO) group with low TyG index, the MHO group with high TyG index showed increased risk of T2D in all four definitions of metabolic health with multivariate-adjusted hazard ratios of 2.57 (95% confidence interval [CI], 1.76 to 3.75), 3.72 (95% CI, 2.15 to 6.43), 4.13 (95% CI, 2.67 to 6.38), and 3.05 (95% CI, 2.24 to 4.15), when defined by Adult Treatment Panel III, Wildman, Karelis, and homeostasis model assessment (HOMA) criteria, respectively.
Conclusion
MHO subjects with high TyG index were at an increased risk of developing T2D compared with MHNO subjects, regardless of the definition of metabolic health. TyG index may serve as an additional factor for predicting the individual risk of incident T2D in MHO subjects.

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Cardiovascular Outcomes of Obesity According to Menopausal Status: A Nationwide Population-Based Study
- Bo Kyung Koo, Sang-Hyun Park, Kyungdo Han, Min Kyong Moon
- Endocrinol Metab. 2021;36(5):1029-1041. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1197
- 3,638 View
- 117 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
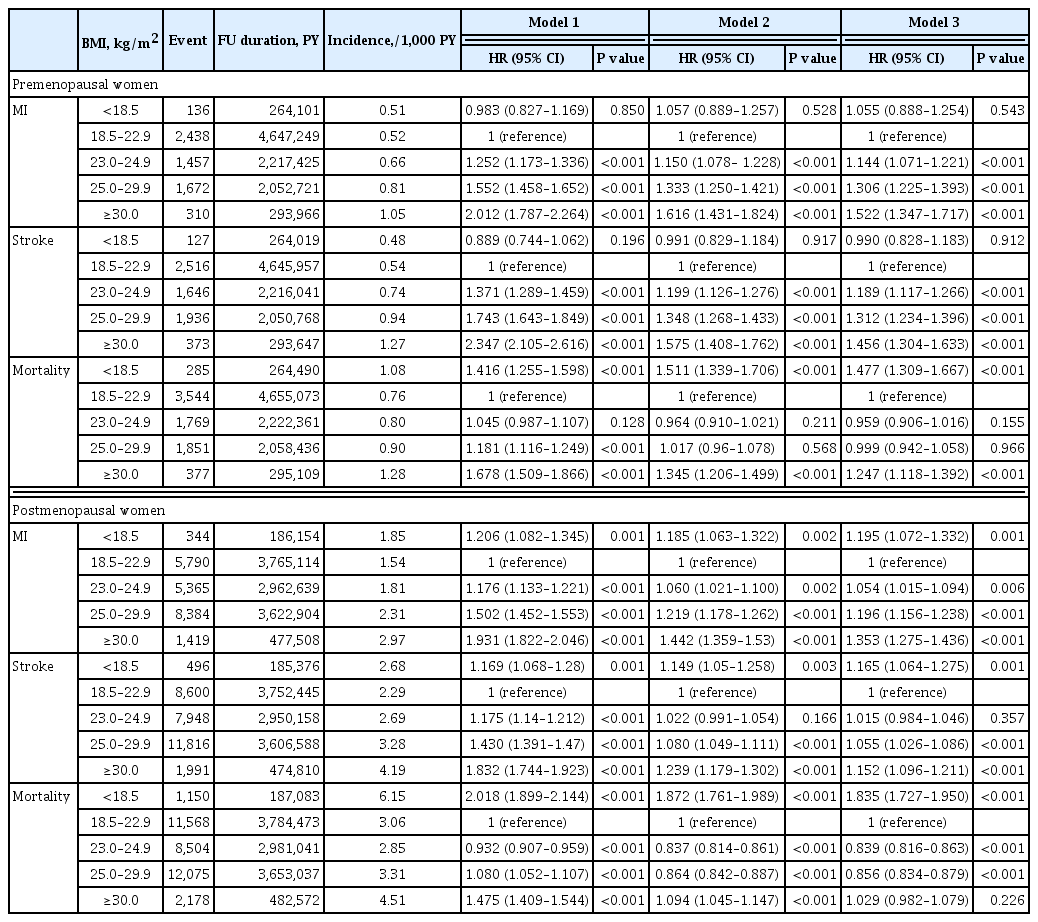
We estimated the effect of obesity on the incidence of cardiovascular disease (CVD) and mortality in women according to menopausal status.
Methods
Women aged 40 to 69 years under routine health check-ups provided by the National Health Insurance Service in 2009 were followed up till 2018 (n=2,208,559).
Results
In premenopausal women, a significant increment of mortality rate was found in underweight and obesity class II (hazard ratio [HR], 1.48; 95% confidence interval [CI], 1.31 to 1.67; and HR, 1.25; 95% CI, 1.12 to 1.39) compared to normal body mass index (BMI); overweight and obesity class I did not affect mortality rate. In postmenopausal women, obesity as well as overweight status reduced the risk of mortality compared to normal BMI (HR, 0.86; 95% CI, 0.83 to 0.88; and HR, 0.84; 95% CI, 0.82 to 0.86). By contrast, there was a linear association between CVD and BMI above the normal range irrespective of menopausal status, which was attenuated in diabetic women.
Conclusion
The current study replicated the J-shaped relationship between BMI and mortality, being more prominent in the postmenopausal group. The risk of CVD was linearly increased as BMI was increased above the normal range irrespective of menopausal status. -
Citations
Citations to this article as recorded by- Biosocial predictors and blood pressure goal attainment among postmenopausal women with hypertension
Geetha Kandasamy, Thangamani Subramani, Gigi Sam, Mona Almanasef, Tahani Almeleebia, Eman Shorog, Asma M. Alshahrani, Amjad Hmlan, Atheer Y. Al Suhaym, Kousalya Prabahar, Vinoth Prabhu Veeramani, Palanisamy Amirthalingam
Frontiers in Cardiovascular Medicine.2024;[Epub] CrossRef - A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 45. CrossRef - The effect of menopause on cardiovascular risk factors according to body mass index in middle-aged Korean women
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Aysha Almas
PLOS ONE.2023; 18(3): e0283393. CrossRef - Low‐quality muscle mass rather than normal‐quality muscle mass determines fibrosis progression in biopsy‐proven NAFLD
Yun Kyu Lee, Bo Kyung Koo, Sae Kyung Joo, Dong Hyeon Lee, Heejoon Jang, Jee Won Chai, Myoung Seok Lee, Si Won Jang, Young Ho So, Jeong Hwan Park, Mee Soo Chang, Won Kim
Alimentary Pharmacology & Therapeutics.2023; 58(3): 322. CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Non-pharmacologic treatment for obesity
Bo Kyung Koo
Journal of the Korean Medical Association.2022; 65(7): 400. CrossRef
- Biosocial predictors and blood pressure goal attainment among postmenopausal women with hypertension

- Diabetes, Obesity and Metabolism
- Changes in Insulin Resistance Index and the Risk of Liver Fibrosis in Patients with Nonalcoholic Fatty Liver Disease without Diabetes: Kangbuk Samsung Health Study
- Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Endocrinol Metab. 2021;36(5):1016-1028. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1110
- 4,113 View
- 128 Download
- 5 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
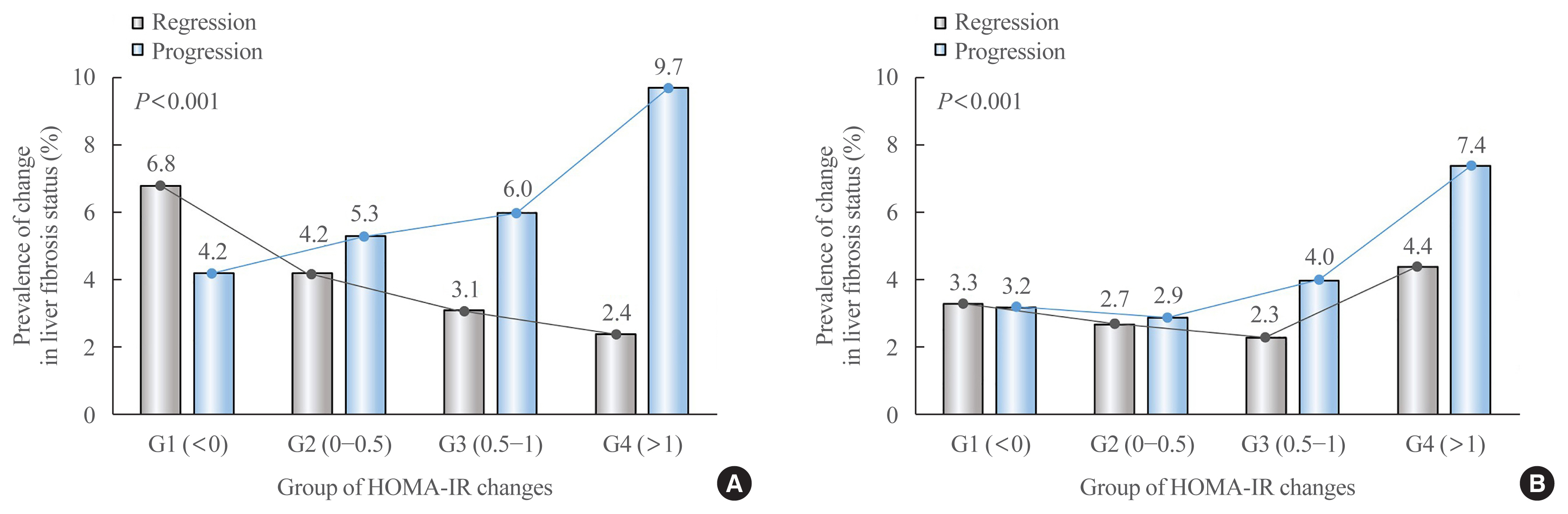
Fibrosis is the most important prognostic factor for nonalcoholic fatty liver disease (NAFLD). Insulin resistance plays a key role of fibrosis progression. We evaluated the association between changes in homeostasis model assessment of insulin resistance (HOMA-IR) values and changes in fibrosis status in NAFLD.
Methods
We analyzed the data of 15,728 participants with NAFLD (86% men, mean age 40.5 years) who had no diabetes at baseline and visited our centers for health check-ups both in 2012 and 2016. The participants were classified into four groups according to the degree of change in HOMA-IR values from baseline to the end of follow-up: G1 (<0), G2 (0–0.50), G3 (0.51–1.00), and G4 (>1.00). NAFLD was assessed by ultrasonography, and fibrosis status was evaluated by the NAFLD fibrosis score (NFS) and the aspartate aminotransferase to platelet ratio index (APRI).
Results
After the 4-year follow-up, the multivariable-adjusted odds ratio (OR) for progression of fibrosis probability increased with increasing HOMA-IR values (OR, 2.25; 95% confidence interval [CI], 1.87 to 2.71 for NFS; and OR, 2.55; 95% CI, 2.05 to 3.18 for APRI, G4). This tendency remained consistent throughout the subgroup analyses, except in those for female sex and a body mass index <25 kg/m2. The OR for regression of fibrosis probability decreased with increasing HOMA-IR values (OR, 0.33; 95% CI, 0.25 to 0.43 for NFS, G4).
Conclusion
Changes in HOMA-IR values were associated with changes in fibrosis status in patients with NAFLD without diabetes, which underscores the role of insulin resistance in liver fibrosis. -
Citations
Citations to this article as recorded by- Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis
Mohammad E. Khamseh, Mojtaba Malek, Soodeh Jahangiri, Sohrab Nobarani, Azita Hekmatdoost, Marieh Salavatizadeh, Samira Soltanieh, Haleh Chehrehgosha, Hoda Taheri, Zeinab Montazeri, Fereshteh Attaran, Faramarz Ismail-Beigi, Fariba Alaei-Shahmiri
Digestive Diseases and Sciences.2024; 69(4): 1430. CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - Factors Associated with Liver Fibrosis in Chinese Patients with Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease
Yu Luo, Cuiyu Wang, Tian Zhang, Xiaoyu He, Jianan Hao, Andong Shen, Hang Zhao, Shuchun Chen, Luping Ren
International Journal of General Medicine.2023; Volume 16: 293. CrossRef - Impact of COVID-19 Lockdown on Non-Alcoholic Fatty Liver Disease and Insulin Resistance in Adults: A before and after Pandemic Lockdown Longitudinal Study
Ángel Arturo López-González, Bárbara Altisench Jané, Luis Masmiquel Comas, Sebastiana Arroyo Bote, Hilda María González San Miguel, José Ignacio Ramírez Manent
Nutrients.2022; 14(14): 2795. CrossRef - Metabolic Score for Insulin Resistance Is Inversely Related to Incident Advanced Liver Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease
Jun-Hyuk Lee, Yu-Jin Kwon, Kyongmin Park, Hye Sun Lee, Hoon-Ki Park, Jee Hye Han, Sang Bong Ahn
Nutrients.2022; 14(15): 3039. CrossRef - Machine learning models including insulin resistance indexes for predicting liver stiffness in United States population: Data from NHANES
Kexing Han, Kexuan Tan, Jiapei Shen, Yuting Gu, Zilong Wang, Jiayu He, Luyang Kang, Weijie Sun, Long Gao, Yufeng Gao
Frontiers in Public Health.2022;[Epub] CrossRef - The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence?
Dae-Jeong Koo, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(4): 132. CrossRef
- Insulin Resistance/Sensitivity Measures as Screening Indicators of Metabolic-Associated Fatty Liver Disease and Liver Fibrosis

- Diabetes, Obesity and Metabolism
Big Data Articles (National Health Insurance Service Database) - Frequency of Exposure to Impaired Fasting Glucose and Risk of Mortality and Cardiovascular Outcomes
- Seung-Hwan Lee, Kyungdo Han, Hyuk-Sang Kwon, Mee Kyoung Kim
- Endocrinol Metab. 2021;36(5):1007-1015. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1218
- 3,784 View
- 126 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Metabolic abnormalities, such as impaired fasting glucose (IFG), are dynamic phenomena; however, it is unclear whether the timing of IFG exposure and cumulative exposure to IFG are related to cardiovascular disease (CVD) and mortality risk.
Methods
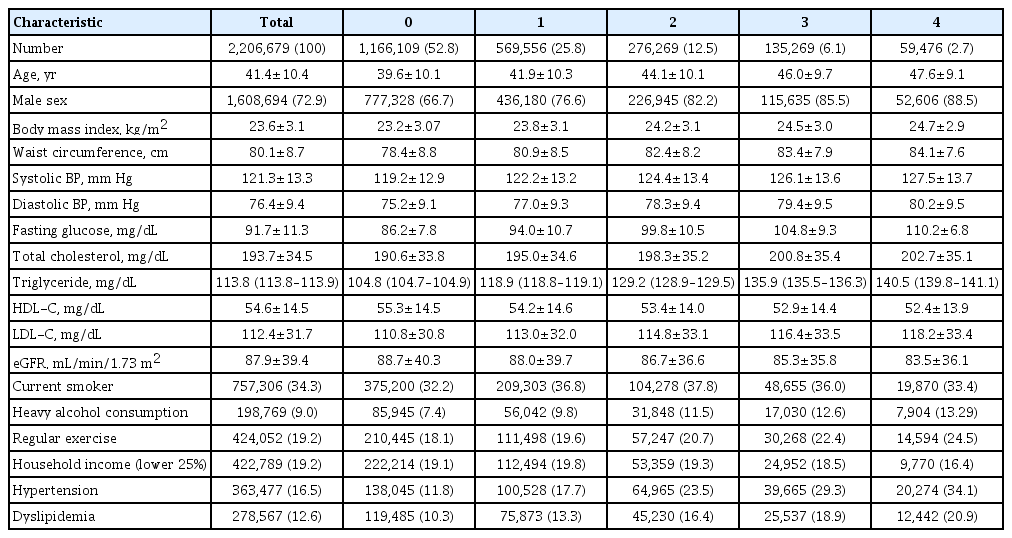
Data were extracted from a nationwide population-based cohort in South Korea for adults (n=2,206,679) who were free of diabetes and had 4 years of consecutive health examination data. Fasting blood glucose levels of 100 to 125 mg/dL were defined as IFG, and the number of IFG diagnoses for each adult in the 4-year period was tabulated as the IFG exposure score (range, 0 to 4). Adults with persistent IFG for the 4-year period received a score of 4.
Results
The median follow-up was 8.2 years. There were 24,820 deaths, 13,502 cases of stroke, and 13,057 cases of myocardial infarction (MI). IFG exposure scores of 1, 2, 3, and 4 were associated with all-cause mortality (multivariable-adjusted hazard ratio [aHR], 1.11; 95% confidence interval [CI], 1.08 to 1.15; aHR, 1.16; 95% CI, 1.12 to 1.20; aHR, 1.20; 95% CI, 1.15 to 1.25; aHR, 1.18; 95% CI, 1.11 to 1.25, respectively) compared with an IFG exposure score of 0. Adjusting for hypertension and dyslipidemia attenuated the slightly increased risk of MI or stroke associated with high IFG exposure scores, but significant associations for allcause mortality remained.
Conclusion
The intensity of IFG exposure was associated with an elevated risk of all-cause mortality, independent of cardiovascular risk factors. The association between IFG exposure and CVD risk was largely mediated by the coexistence of dyslipidemia and hypertension. -
Citations
Citations to this article as recorded by- A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Construction and Validation of a Model for Predicting Impaired Fasting Glucose Based on More Than 4000 General Population
Cuicui Wang, Xu Zhang, Chenwei Li, Na Li, Xueni Jia, Hui Zhao
International Journal of General Medicine.2023; Volume 16: 1415. CrossRef - Factors Affecting High Body Weight Variability
Kyungdo Han, Mee Kyoung Kim
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 163. CrossRef - Exposure to perfluoroalkyl and polyfluoroalkyl substances and risk of stroke in adults: a meta-analysis
Min Cheol Chang, Seung Min Chung, Sang Gyu Kwak
Reviews on Environmental Health.2023;[Epub] CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - A Longitudinal Retrospective Observational Study on Obesity Indicators and the Risk of Impaired Fasting Glucose in Pre- and Postmenopausal Women
Myung Ji Nam, Hyunjin Kim, Yeon Joo Choi, Kyung-Hwan Cho, Seon Mee Kim, Yong-Kyun Roh, Kyungdo Han, Jin-Hyung Jung, Yong-Gyu Park, Joo-Hyun Park, Do-Hoon Kim
Journal of Clinical Medicine.2022; 11(10): 2795. CrossRef - Current Trends of Big Data Research Using the Korean National Health Information Database
Mee Kyoung Kim, Kyungdo Han, Seung-Hwan Lee
Diabetes & Metabolism Journal.2022; 46(4): 552. CrossRef - Lipid cutoffs for increased cardiovascular disease risk in non-diabetic young people
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Kun-Ho Yoon, Seung-Hwan Lee
European Journal of Preventive Cardiology.2022; 29(14): 1866. CrossRef - Low-Density Lipoprotein Cholesterol Level, Statin Use and Myocardial Infarction Risk in Young Adults
Heekyoung Jeong, Kyungdo Han, Soon Jib Yoo, Mee Kyoung Kim
Journal of Lipid and Atherosclerosis.2022; 11(3): 288. CrossRef - Additive interaction of diabetes mellitus and chronic kidney disease in cancer patient mortality risk
Seohyun Kim, Gyuri Kim, Jae Hyeon Kim
Scientific Reports.2022;[Epub] CrossRef
- A nationwide cohort study on diabetes severity and risk of Parkinson disease


 KES
KES

 First
First Prev
Prev



