Search
- Page Path
- HOME > Search
- Thyroid
- Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
- Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
- Endocrinol Metab. 2023;38(6):729-738. Published online November 2, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1769
- 1,083 View
- 72 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study investigates the association between thyroid function and frailty in the old patients using representative data.
Methods
The study was conducted using data from the Korea National Health and Nutrition Examination Survey conducted from 2013 to 2015. The study population included 2,416 participants aged 50 years and older with available thyroid function test data. Frailty assessment was performed using the Fried frailty phenotype. The prevalence of frailty was analyzed across different thyroid diseases and thyroid function parameters.
Results
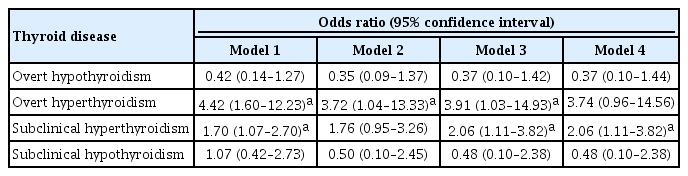
The significant association between thyroid dysfunction and frailty was observed in overt hyperthyroidism and subclinical hyperthyroidism. After adjusting for various factors, the association between thyroid dysfunction and frailty remained significant. On the other hand, overt hypothyroidism did not show a significant association with frailty in the adjusted analysis. For individuals with overt hyperthyroidism and subclinical hyperthyroidism, higher levels of free thyroxine (FT4) were significantly associated with an increased risk of frailty (aOR >999; 95% CI, >999 to 999). Among individuals with overt hypothyroidism, lower level of FT4 levels and high thyrotropin (TSH) levels showed a significant association with frailty risk (FT4: aOR, <0.01; TSH: aOR, 999). In participants with subclinical hypothyroidism, there were no significant associations between parameters for thyroid and frailty risk.
Conclusion
These findings suggest that thyroid dysfunction, particularly overt hyperthyroidism and subclinical hyperthyroidism, may be associated with an increased risk of frailty in the old patients. -
Citations
Citations to this article as recorded by- Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China
Heng Wan, Genfeng Yu, Yajun He, Siyang Liu, Xingying Chen, Yuqi Jiang, Hualin Duan, Xu Lin, Lan Liu, Jie Shen
Annals of Medicine.2024;[Epub] CrossRef
- Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China

- Thyroid
- Association between Iodine Intake, Thyroid Function, and Papillary Thyroid Cancer: A Case-Control Study
- Kyungsik Kim, Sun Wook Cho, Young Joo Park, Kyu Eun Lee, Dong-Wook Lee, Sue K. Park
- Endocrinol Metab. 2021;36(4):790-799. Published online August 11, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1034
- 4,711 View
- 236 Download
- 9 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to assess the effects of iodine intake, thyroid function, and their combined effect on the risk of papillary thyroid cancer (PTC) and papillary thyroid microcarcinoma (PTMC).
Methods
A case-control study was conducted including 500 community-based controls who had undergone a health check-up, and 446 overall PTC cases (209 PTC and 237 PTMC) from the Thyroid Cancer Longitudinal Study. Urinary iodine concentration (UIC), was used as an indicator of iodine intake, and serum for thyroid function. The risk of PTC and PTMC was estimated using unconditional logistic regression.
Results
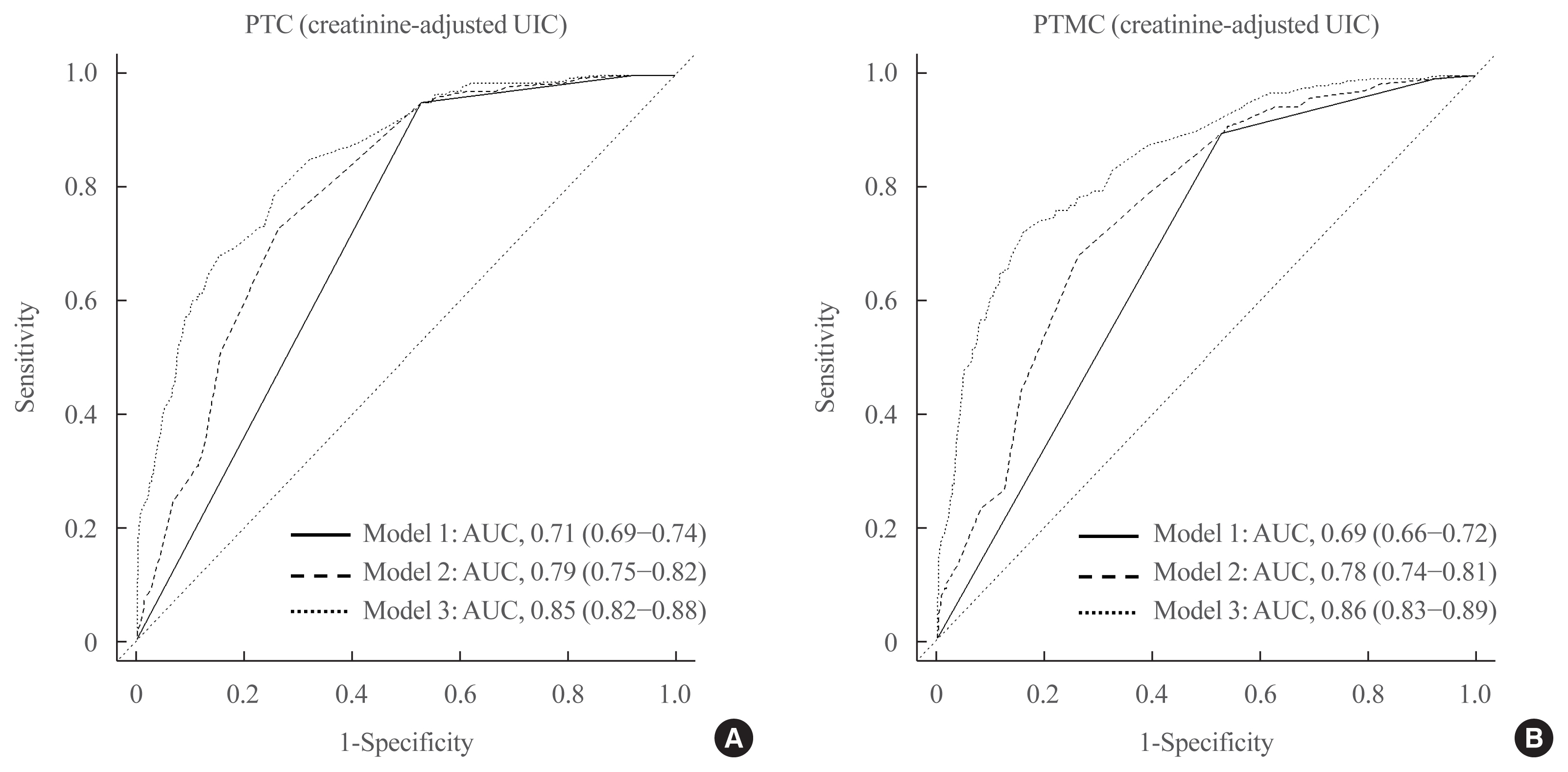
Excessive iodine intake (UIC ≥220 μg/gCr) was associated with both PTC (odds ratio [OR], 18.13 95% confidence interval [CI], 8.87 to 37.04) and PTMC (OR, 8.02; 95% CI, 4.64 to 13.87), compared to adequate iodine intake (UIC, 85 to 219 μg/gCr). Free thyroxine (T4) levels ≥1.25 ng/dL were associated with PTC (OR, 1.97; 95% CI, 1.36 to 2.87) and PTMC (OR, 2.98; 95% CI, 2.01 to 4.41), compared to free T4 levels of 0.7 to 1.24 ng/dL. Individuals with excessive iodine intake and high free T4 levels had a greatly increased OR of PTC (OR, 43.48; 95% CI, 12.63 to 149.62), and PTMC (OR, 26.96; 95% CI, 10.26 to 70.89), compared to individuals with adequate iodine intake and low free T4 levels.
Conclusion
Excessive iodine intake using creatinine-adjusted UIC and high free T4 levels may have a synergistic effect on PTC and PTMC. Considering both iodine intake and thyroid function is important to assess PTC and PTMC risk. -
Citations
Citations to this article as recorded by- Association between urinary iodine concentration and the risk of papillary thyroid cancer by sex and age: a case–control study
Yerin Hwang, Hyun-Kyung Oh, Jae Hoon Chung, Sun Wook Kim, Jung-Han Kim, Jee Soo Kim, Myung-Hee Shin
Scientific Reports.2023;[Epub] CrossRef - Association between iodine nutrition and cervical lymph node metastasis of papillary thyroid microcarcinoma
Hengqiang Zhao, Jin Hu, Le Cui, Yiping Gong, Tao Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sex-specific Associations between Body Mass Index and Thyroid Cancer Incidence among Korean Adults
Kyoung-Nam Kim, Kyungsik Kim, Sangjun Lee, Sue K. Park
Cancer Epidemiology, Biomarkers & Prevention.2023; 32(9): 1227. CrossRef - Nomogram Model Based on Iodine Nutrition and Clinical Characteristics of Papillary Thyroid Carcinoma to Predict Lateral Lymph Node Metastasis
Junrong Wang, Yuzhang Gao, Yuxuan Zong, Weitong Gao, Xueying Wang, Ji Sun, Susheng Miao
Cancer Control.2023;[Epub] CrossRef - Content of Copper, Iron, Iodine, Rubidium, Strontium and Zinc in Thyroid Malignant Nodules and Thyroid Tissue adjacent to Nodules
Vladimir Zaichick, Qiping Dong
Journal of Clinical and Diagnostic Pathology.2022; 1(4): 7. CrossRef - Distinguish Thyroid Malignant from Benign Alterations using Trace Element Contents in Nodular Tissue determined by Neutron Activation and Inductively Coupled Plasma Mass Spectrometry
Vladimir Zaichick
Journal of Clinical and Diagnostic Pathology.2022; 1(4): 18. CrossRef - Seaweed and Iodine Intakes and SLC5A5 rs77277498 in Relation to Thyroid Cancer
Tung Hoang, Eun Kyung Lee, Jeonghee Lee, Yul Hwangbo, Jeongseon Kim
Endocrinology and Metabolism.2022; 37(3): 513. CrossRef - Iodine nutrition and papillary thyroid cancer
Xueqi Zhang, Fan Zhang, Qiuxian Li, Chuyao Feng, Weiping Teng
Frontiers in Nutrition.2022;[Epub] CrossRef - The relationship between urinary iodine concentration and papillary thyroid cancer: A systematic review and meta-analysis
Xueqi Zhang, Fan Zhang, Qiuxian Li, Renaguli Aihaiti, Chuyao Feng, Deshi Chen, Xu Zhao, Weiping Teng
Frontiers in Endocrinology.2022;[Epub] CrossRef - Screening and validation of lymph node metastasis risk-factor genes in papillary thyroid carcinoma
Qiaoyue Zhang, Jing Li, Hengyan Shen, Xinyu Bai, Tao Zhang, Ping Liu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnosis of Thyroid Malignancy using Levels of Chemical Element Contents in Nodular Tissue
Vladimir Zaichick
Journal of Health Care and Research.2022; 3(1): 16. CrossRef - Associations of Habitual Mineral Intake with New-Onset Prediabetes/Diabetes after Acute Pancreatitis
Claire F. Norbitt, Wandia Kimita, Juyeon Ko, Sakina H. Bharmal, Maxim S. Petrov
Nutrients.2021; 13(11): 3978. CrossRef
- Association between urinary iodine concentration and the risk of papillary thyroid cancer by sex and age: a case–control study

- Thyroid
- Insights from a Prospective Follow-up of Thyroid Function and Autoimmunity among COVID-19 Survivors
- David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung, Karen Siu Ling Lam
- Endocrinol Metab. 2021;36(3):582-589. Published online June 8, 2021
- DOI: https://doi.org/10.3803/EnM.2021.983
- 10,838 View
- 265 Download
- 32 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The occurrence of Graves’ disease and Hashimoto thyroiditis after coronavirus disease 2019 (COVID-19) raised concerns that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may trigger thyroid autoimmunity. We aimed to address the current uncertainties regarding incident thyroid dysfunction and autoimmunity among COVID-19 survivors.
Methods
We included consecutive adult COVID-19 patients without known thyroid disorders, who were admitted to Queen Mary Hospital from July 21 to September 21, 2020 and had serum levels of thyroid-stimulating hormone, free thyroxine, free triiodothyronine (fT3), and anti-thyroid antibodies measured both on admission and at 3 months.
Results
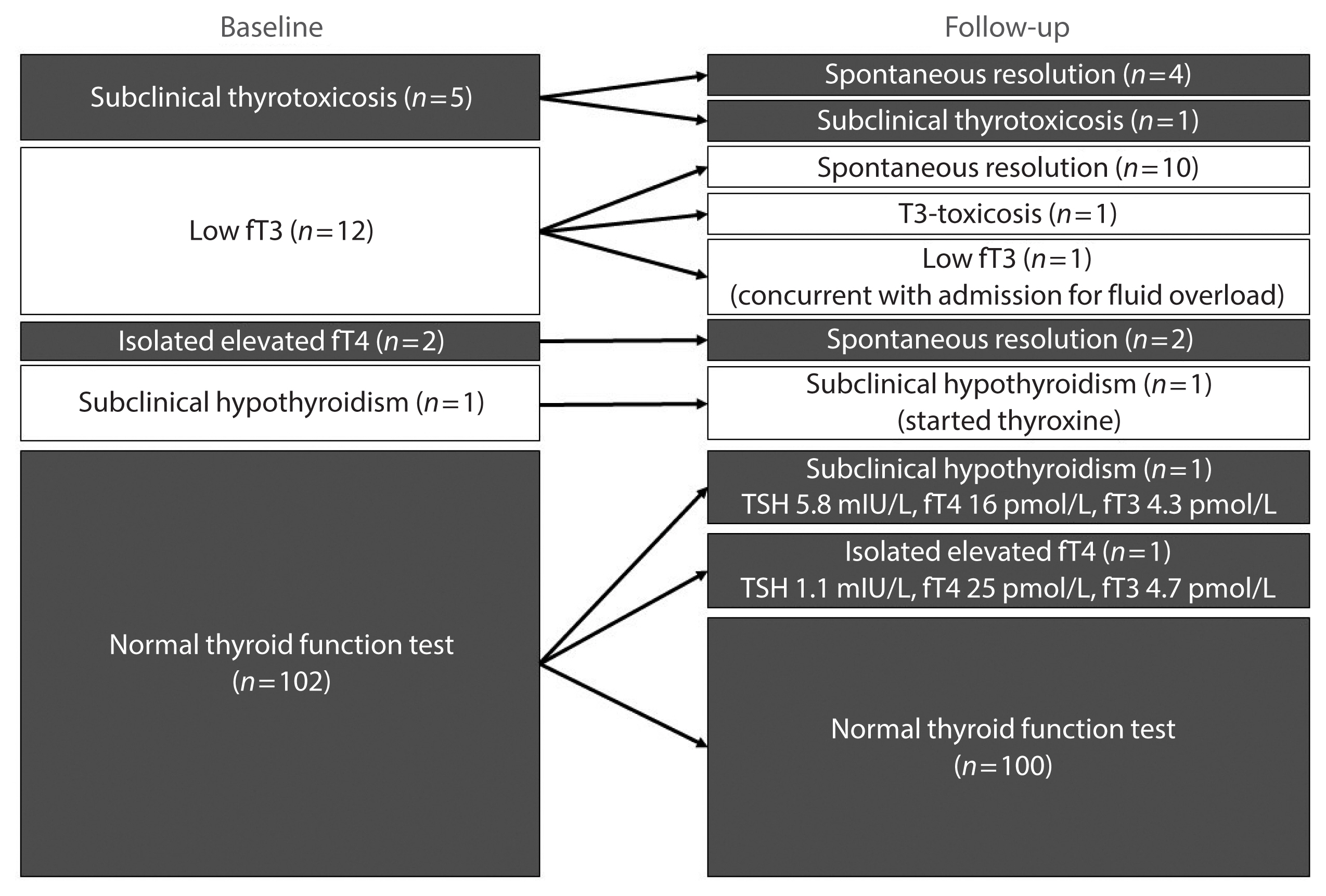
In total, 122 patients were included. Among 20 patients with abnormal thyroid function tests (TFTs) on admission (mostly low fT3), 15 recovered. Among 102 patients with initial normal TFTs, two had new-onset abnormalities that could represent different phases of thyroiditis. Among 104 patients whose anti-thyroid antibody titers were reassessed, we observed increases in anti-thyroid peroxidase (TPO) (P<0.001) and anti-thyroglobulin (P<0.001), but not anti-thyroid stimulating hormone receptor titers (P=0.486). Of 82 patients with negative anti-TPO findings at baseline, 16 had a significant interval increase in anti-TPO titer by >12 U, and four became anti-TPO-positive. Worse baseline clinical severity (P=0.018), elevated C-reactive protein during hospitalization (P=0.033), and higher baseline anti-TPO titer (P=0.005) were associated with a significant increase in anti-TPO titer.
Conclusion
Most patients with thyroid dysfunction on admission recovered during convalescence. Abnormal TFTs suggestive of thyroiditis occurred during convalescence, but infrequently. Importantly, our novel observation of an increase in anti-thyroid antibody titers post-COVID-19 warrants further follow-up for incident thyroid dysfunction among COVID-19 survivors. -
Citations
Citations to this article as recorded by- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis
Sadra Ashrafi, Hossein Hatami, Razieh Bidhendi-Yarandi, Mohammad Hossein Panahi
BMC Endocrine Disorders.2024;[Epub] CrossRef - Does COVID-19 affect thyroid more than non-COVID-19 infections? A retrospective study
Yasemin Ucal, Muhittin Serdar, Hande Karpuzoğlu, Neval Yurttutan Uyar, Meltem Kilercik, Mustafa Serteser, Aysel Ozpinar
Turkish Journal of Biochemistry.2024;[Epub] CrossRef - Thyroiditis and COVID-19: focus on pediatric age. A narrative review
F. d’Aniello, M. E. Amodeo, A. Grossi, G. Ubertini
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - The most common persistent symptoms in patients with COVID-19 who were evaluated in the Internal Medicine polyclinic
Zeynep KOÇ, Seydahmet AKIN
The European Research Journal.2023; 9(1): 97. CrossRef - Clinical assessment of children with long COVID syndrome
Réka Garai, Péter Krivácsy, Vivien Herczeg, Fanni Kovács, Bálint Tél, Judit Kelemen, Anna Máthé, Eszter Zsáry, Johanna Takács, Dániel Sándor Veres, Attila J. Szabó
Pediatric Research.2023; 93(6): 1616. CrossRef - T Cell Receptor Sequences Amplified during Severe COVID-19 and Multisystem Inflammatory Syndrome in Children Mimic SARS-CoV-2, Its Bacterial Co-Infections and Host Autoantigens
Robert Root-Bernstein, Elizabeth Churchill, Shelby Oliverio
International Journal of Molecular Sciences.2023; 24(2): 1335. CrossRef - A Literature Review on SARS-CoV-2 and Other Viruses in Thyroid Disorders: Environmental Triggers or No-Guilty Bystanders?
Francesca Gorini, Cristina Vassalle
International Journal of Environmental Research and Public Health.2023; 20(3): 2389. CrossRef - Thyroid dysfunction as a long-term post-COVID-19 complication in mild-to-moderate COVID-19
Vesselina Yanachkova, Teodora Stankova, Radiana Staynova
Biotechnology & Biotechnological Equipment.2023; 37(1): 194. CrossRef - The Influence of SARS-CoV-2 Infection on the Thyroid Gland
Aleksandra Piekarska, Marta Góral, Marta Kozula, Aleksandra Jawiarczyk-Przybyłowska, Katarzyna Zawadzka, Marek Bolanowski
Biomedicines.2023; 11(2): 614. CrossRef - Thyroid Function Abnormalities and Outcomes in Hospitalized Patients
with COVID-19 Infection: A Cross-Sectional Study
Deepika Patel, Dukhabandhu Naik, Sadishkumar Kamalanathan, Kadhiravan Tamilarasu, Jayaprakash Sahoo, Ayan Roy, Chandhana Merugu, Varun Suryadevara
Hormone and Metabolic Research.2023; 55(03): 169. CrossRef - The Spectrum of Thyroid Function Tests and Autoantibodies During Hospitalization and After Six Months of Discharge in COVID-19 Patients: Does COVID-19 Trigger Autoimmunity?
Ziynet Alphan Uc, Pinar Yagcı, Zelal Adibelli, Cevdet Duran
Endocrine Research.2023; 48(2-3): 44. CrossRef - Increased prevalence of autoimmune thyroid disease after COVID-19: A single-center, prospective study
Alessandro Rossini, Sara Cassibba, Francesca Perticone, Simone Vasilij Benatti, Serena Venturelli, Greta Carioli, Arianna Ghirardi, Marco Rizzi, Tiziano Barbui, Roberto Trevisan, Silvia Ippolito
Frontiers in Endocrinology.2023;[Epub] CrossRef - A prospective follow-up of thyroid volume and thyroiditis features on ultrasonography among survivors of predominantly mild to moderate COVID-19
Man Him Matrix Fung, David Tak Wai Lui, Keith Wan Hang Chiu, Sherman Haynam Lee, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Chun Yiu Law, Kelvin Kai Wang To, Ching W
PeerJ.2023; 11: e15034. CrossRef - Study on Clinicopathological Features and Risk Factors of Patients with Multiple Primary Breast Cancers and Thyroid Disease
Jie Li, Yonghong Liu, Jian Jin, Qingfeng Shi, Yanting Ji, Bo Zhang, Pengfei Hu, Jinghua Pan
Mediators of Inflammation.2023; 2023: 1. CrossRef - Beyond Acute COVID-19: Investigating the Incidence of Subacute Thyroiditis in Long COVID-19 in Korea
Jeongmin Lee, Gi Hyeon Seo, Keeho Song
Endocrinology and Metabolism.2023; 38(4): 455. CrossRef - Thyroid Autoimmunity and SARS-CoV-2 Infection
Poupak Fallahi, Giusy Elia, Francesca Ragusa, Sabrina Rosaria Paparo, Armando Patrizio, Eugenia Balestri, Valeria Mazzi, Salvatore Benvenga, Gilda Varricchi, Laura Gragnani, Chiara Botrini, Enke Baldini, Marco Centanni, Clodoveo Ferri, Alessandro Antonell
Journal of Clinical Medicine.2023; 12(19): 6365. CrossRef - Autoimmune complications of COVID‐19
Niloufar Yazdanpanah, Nima Rezaei
Journal of Medical Virology.2022; 94(1): 54. CrossRef - The Independent Association of TSH and Free Triiodothyronine Levels With Lymphocyte Counts Among COVID-19 Patients
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Chloe Yu Yan Cheung, Carol Ho Yi Fong, Chun Yiu Law, Kelvin Kai Wang To, Ching Wan Lam, Kathryn Choon Beng Tan, Yu Cho Woo, Ivan Fan Ngai Hung,
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comment on Khunti et al. COVID-19, Hyperglycemia, and New-Onset Diabetes. Diabetes Care 2021;44:2645–2655
Carmine Gazzaruso, Adriana Coppola, Pietro Gallotti, Ileana Terruzzi, Tiziana Montalcini, Livio Luzi
Diabetes Care.2022; 45(2): e45. CrossRef - The potential impact of COVID-19 on thyroid gland volumes among COVID-19 survivors
Emre Urhan, Zuleyha Karaca, Canan Sehit Kara, Zeynep Ture Yuce, Kursad Unluhizarci
Endocrine.2022; 76(3): 635. CrossRef - Systematic review of COVID-19 and autoimmune thyroiditis
Esra Tutal, Resat Ozaras, Hakan Leblebicioglu
Travel Medicine and Infectious Disease.2022; 47: 102314. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Should we expect a wave of type 1 diabetes following SARS‐CoV‐2 pandemic?
Laura Montefusco, Andrea Mario Bolla, Paolo Fiorina
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - COVID-19 and Thyroid Function: A Bi-Directional Two-Sample Mendelian Randomization Study
Gloria Hoi-Yee Li, Ching-Man Tang, Ching-Lung Cheung
Thyroid.2022; 32(9): 1037. CrossRef - Development of a prediction score (ThyroCOVID) for identifying abnormal thyroid function in COVID-19 patients
D. T. W. Lui, C. H. Lee, W. S. Chow, A. C. H. Lee, A. R. Tam, C. Y. Y. Cheung, C. H. Y. Fong, S. T. M. Kwok, C. Y. Law, K. K. W. To, C. W. Lam, K. C. B. Tan, Y. C. Woo, I. F. N. Hung, K. S. L. Lam
Journal of Endocrinological Investigation.2022; 45(11): 2149. CrossRef - Symptomatic Bradycardia Manifesting as Acute Hypothyroidism Following COVID-19 Infection: A Case Report
Jaydip Desai, Arsh N Patel, Courtney L Evans, Molly Triggs, Fulton Defour
Cureus.2022;[Epub] CrossRef - Schilddrüse und SARS-CoV-2
Georg Zettinig
Journal für Klinische Endokrinologie und Stoffwechsel.2022; 15(3): 100. CrossRef - Thyroid diseases are associated with coronavirus disease 2019 infection
Yutian Tian, Junyu Zhao, Tingting Wang, Haipeng Wang, Jinming Yao, Song Wang, Yaru Mou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Thyrotropin Levels in Patients with Coronavirus Disease 2019: Assessment during Hospitalization and in the Medium Term after Discharge
Abdallah Al-Salameh, Noémie Scherman, Imane Adda, Juliette André, Yoann Zerbib, Julien Maizel, Jean-Daniel Lalau, Etienne Brochot, Claire Andrejak, Rachel Desailloud
Life.2022; 12(12): 2014. CrossRef - Long COVID in Patients With Mild to Moderate Disease: Do Thyroid Function and Autoimmunity Play a Role?
David Tak Wai Lui, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Chun Yiu Law, Eunice Ka Hong Leung, Kelvin Kai Wang To, Kathryn Choon Beng Tan, Yu Cho Woo, Ching Wan Lam, Ivan Fan Ngai Hung,
Endocrine Practice.2021; 27(9): 894. CrossRef - Hashimoto’s thyroiditis following SARS-CoV-2 infection
Rafael Silvestre Knack, Taliê Hanada, Renata Silvestre Knack, Kamilla Mayr
BMJ Case Reports.2021; 14(8): e244909. CrossRef - Higher SARS-CoV-2 viral loads correlated with smaller thyroid volumes on ultrasound among male COVID-19 survivors
David Tak Wai Lui, Matrix Man Him Fung, Keith Wan Hang Chiu, Chi Ho Lee, Wing Sun Chow, Alan Chun Hong Lee, Anthony Raymond Tam, Polly Pang, Tip Yin Ho, Carol Ho Yi Fong, Connie Hong Nin Loong, Wade Wei Wong, Cassandra Yuen Yan Lee, Chun Yiu Law, Kelvin K
Endocrine.2021; 74(2): 205. CrossRef - SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases
Avaniyapuram Kannan Murugan, Ali S Alzahrani
Journal of Inflammation Research.2021; Volume 14: 6191. CrossRef - POST-COVID ENDOCRINOPATHY :ABOUT A CASE ENDOCRINOPATHIE POST- COVID :À PROPOS D’UN CAS
S. Rafi, G. Elmghari, N, Elansari
INDIAN JOURNAL OF APPLIED RESEARCH.2021; : 13. CrossRef
- The prevalence of thyroid disorders in COVID-19 patients: a systematic review and meta-analysis

- Clinical Study
- Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study
- Mijin Kim, Bo Hyun Kim, Hyungi Lee, Min Hee Jang, Jeong Mi Kim, Eun Heui Kim, Yun Kyung Jeon, Sang Soo Kim, In Joo Kim
- Endocrinol Metab. 2020;35(1):106-114. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.106
- 6,085 View
- 119 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Studies on the relationship between thyroid function and anemia in the euthyroid range are scarce. We aimed to evaluate the association between anemia and serum free thyroxine (fT4) and thyrotropin (TSH) in euthyroid adults.
Methods Data on 5,352 participants aged ≥19 years were obtained from the Korea National Health and Nutrition Examination Survey VI (2013 to 2015). Anemia was defined as hemoglobin (Hb) <13 and <12 g/dL for men and women, respectively.
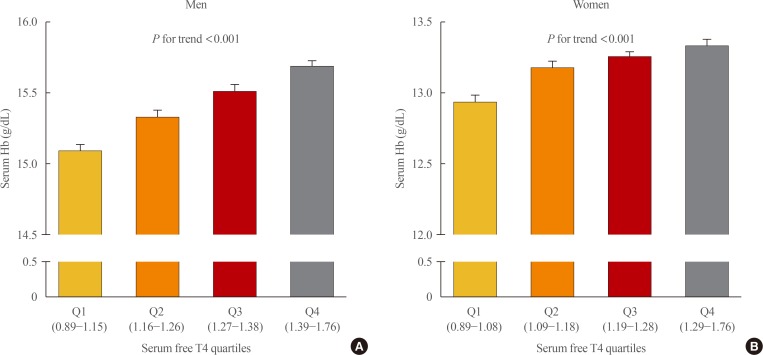
Results Overall, 6.1% of participants had anemia, and more women (9.9%) had anemia than men (2.8%,
P <0.001). In multivariate analysis, serum fT4 levels, but not TSH, were positively associated with serum Hb levels in both sexes (P <0.001, each). Serum Hb levels linearly reduced across decreasing serum fT4 quartile groups in both sexes (P <0.001, each). After adjusting for potential confounding factors, participants with low-normal fT4 had 4.4 (P =0.003) and 2.8 times (P <0.001) higher risk for anemia than those with high-normal fT4 among men and women, respectively. When participants were divided into two groups at 50 years of age, in younger participants, men and women with the first quartile were at higher risk of anemia than men with the second quartile (odds ratio [OR], 3.3;P =0.029) and women with the forth quartile (OR, 3.2;P <0.001), respectively. This association was not observed in older participants.Conclusion These results suggest that a low-normal level of serum fT4 was associated with a lower serum Hb level and a higher risk of anemia in euthyroid adults, especially in younger participants.
-
Citations
Citations to this article as recorded by- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank
Nicolien A van Vliet, Annelies E P Kamphuis, Wendy P J den Elzen, Gerard J Blauw, Jacobijn Gussekloo, Raymond Noordam, Diana van Heemst
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e643. CrossRef - Thyroid function, pernicious anemia and erythropoiesis: a two-sample Mendelian randomization study
Alisa D Kjaergaard, Alexander Teumer, Eirini Marouli, Panos Deloukas, Aleksander Kuś, Rosalie Sterenborg, Bjørn O Åsvold, Marco Medici, Christina Ellervik
Human Molecular Genetics.2022; 31(15): 2548. CrossRef - Changes of hematological indices in patients with diffuse toxic goiter
F. H. Saidova, L. M. Ahmedova, Zh. B. Aslanova, N. A. Najafov
Klinicheskaia khirurgiia.2021; 88(3-4): 76. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Zheng Feei Ma
Endocrinology and Metabolism.2020; 35(2): 484. CrossRef - Association between Serum Free Thyroxine and Anemia in Euthyroid Adults: A Nationwide Study (Endocrinol Metab 2020;35:106-14, Mijin Kim et al.)
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2020; 35(3): 669. CrossRef
- Thyroid Function and Risk of Anemia: A Multivariable-Adjusted and Mendelian Randomization Analysis in the UK Biobank


 KES
KES

 First
First Prev
Prev



