Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Nuclear Factor-Kappa B Regulation of Osteoclastogenesis and Osteoblastogenesis
- Brendan F. Boyce, Jinbo Li, Zhenqiang Yao, Lianping Xing
- Endocrinol Metab. 2023;38(5):504-521. Published online September 26, 2023
- DOI: https://doi.org/10.3803/EnM.2023.501
- 2,045 View
- 95 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
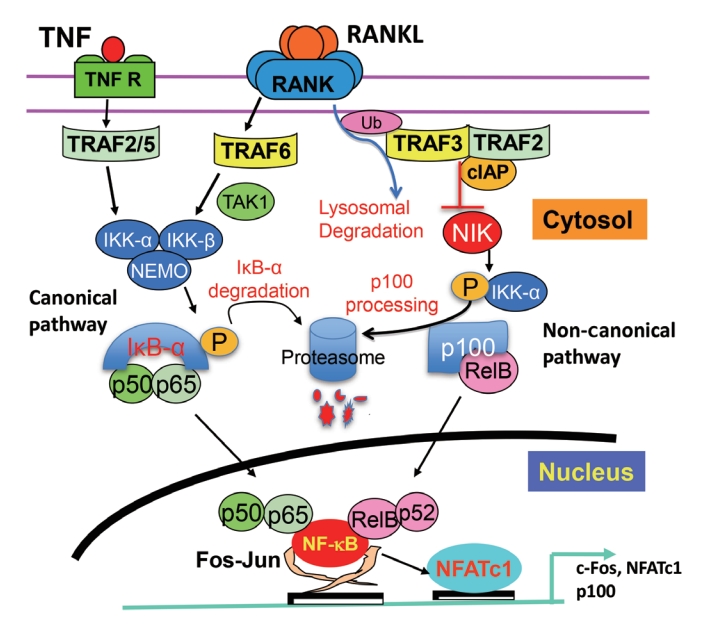
ePub - Maintenance of skeletal integrity requires the coordinated activity of multinucleated bone-resorbing osteoclasts and bone-forming osteoblasts. Osteoclasts form resorption lacunae on bone surfaces in response to cytokines by fusion of precursor cells. Osteoblasts are derived from mesenchymal precursors and lay down new bone in resorption lacunae during bone remodeling. Nuclear factorkappa B (NF-κB) signaling regulates osteoclast and osteoblast formation and is activated in osteoclast precursors in response to the essential osteoclastogenic cytokine, receptor activator of NF-κB ligand (RANKL), which can also control osteoblast formation through RANK-RANKL reverse signaling in osteoblast precursors. RANKL and some pro-inflammatory cytokines, including tumor necrosis factor (TNF), activate NF-κB signaling to positively regulate osteoclast formation and functions. However, these cytokines also limit osteoclast and osteoblast formation through NF-κB signaling molecules, including TNF receptor-associated factors (TRAFs). TRAF6 mediates RANKL-induced osteoclast formation through canonical NF-κB signaling. In contrast, TRAF3 limits RANKL- and TNF-induced osteoclast formation, and it restricts transforming growth factor β (TGFβ)-induced inhibition of osteoblast formation in young and adult mice. During aging, neutrophils expressing TGFβ and C-C chemokine receptor type 5 (CCR5) increase in bone marrow of mice in response to increased NF-κB-induced CC motif chemokine ligand 5 (CCL5) expression by mesenchymal progenitor cells and injection of these neutrophils into young mice decreased bone mass. TGFβ causes degradation of TRAF3, resulting in decreased glycogen synthase kinase-3β/β-catenin-mediated osteoblast formation and age-related osteoporosis in mice. The CCR5 inhibitor, maraviroc, prevented accumulation of TGFβ+/CCR5+ neutrophils in bone marrow and increased bone mass by inhibiting bone resorption and increasing bone formation in aged mice. This paper updates current understanding of how NF-κB signaling is involved in the positive and negative regulation of cytokine-mediated osteoclast and osteoblast formation and activation with a focus on the role of TRAF3 signaling, which can be targeted therapeutically to enhance bone mass.
-
Citations
Citations to this article as recorded by- The Role of Rosavin in the Pathophysiology of Bone Metabolism
Piotr Wojdasiewicz, Paweł Turczyn, Anna Lach-Gruba, Łukasz A. Poniatowski, Daryush Purrahman, Mohammad-Reza Mahmoudian-Sani, Dariusz Szukiewicz
International Journal of Molecular Sciences.2024; 25(4): 2117. CrossRef - The role of monocyte/macrophage chemokines in pathogenesis of osteoarthritis: A review
Hao Luo, Linfeng Li, Song Han, Tao Liu
International Journal of Immunogenetics.2024;[Epub] CrossRef - The effect of low-level laser therapy on osteoclast differentiation: Clinical implications for tooth movement and bone density
Chun-Yi Huang, Huynh Hoai Thuong Le, Hsiao-Chi Tsai, Chih-Hsin Tang, Jian-Hong Yu
Journal of Dental Sciences.2024;[Epub] CrossRef - Genetic Deficiency of the Long Pentraxin 3 Affects Osteogenesis and Osteoclastogenesis in Homeostatic and Inflammatory Conditions
Valentina Granata, Dario Strina, Maria Lucia Schiavone, Barbara Bottazzi, Alberto Mantovani, Antonio Inforzato, Cristina Sobacchi
International Journal of Molecular Sciences.2023; 24(23): 16648. CrossRef
- The Role of Rosavin in the Pathophysiology of Bone Metabolism

- Calcium & Bone Metabolism
- A Key Metabolic Regulator of Bone and Cartilage Health
- Elizabeth Pérez-Hernández, Jesús Javier Pastrana-Carballo, Fernando Gómez-Chávez, Ramesh C. Gupta, Nury Pérez-Hernández
- Endocrinol Metab. 2022;37(4):559-574. Published online August 8, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1443
- 7,743 View
- 337 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
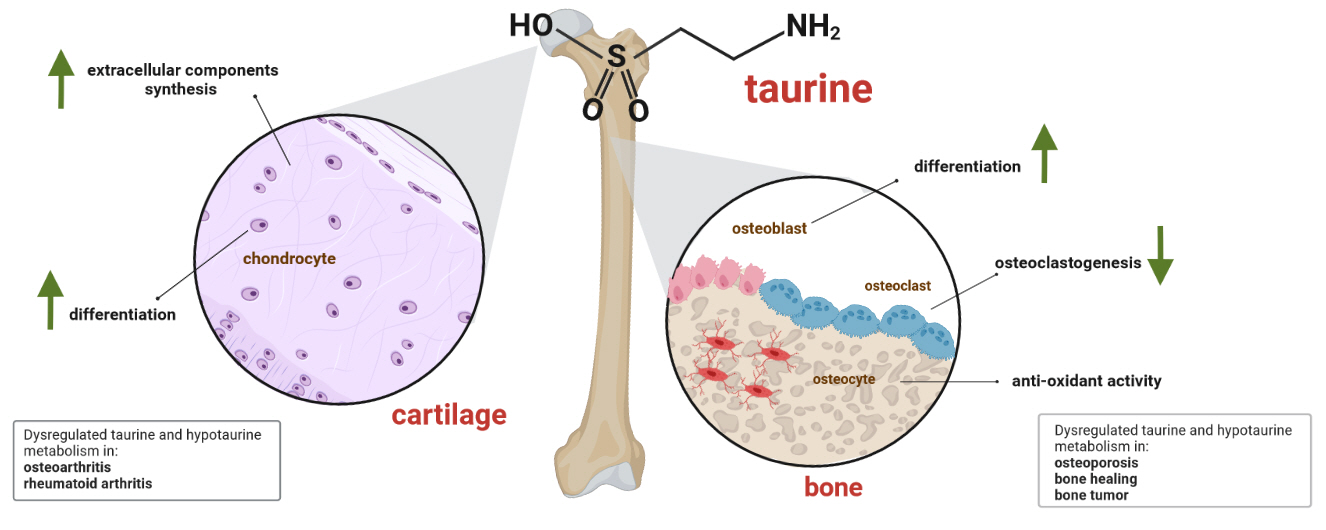
ePub - Taurine, a cysteine-derived zwitterionic sulfonic acid, is a common ingredient in energy drinks and is naturally found in fish and other seafood. In humans, taurine is produced mainly in the liver, and it can also be obtained from food. In target tissues, such as the retina, heart, and skeletal muscle, it functions as an essential antioxidant, osmolyte, and antiapoptotic agent. Taurine is also involved in energy metabolism and calcium homeostasis. Taurine plays a considerable role in bone growth and development, and high-profile reports have demonstrated the importance of its metabolism for bone health. However, these reports have not been collated for more than 10 years. Therefore, this review focuses on taurine–bone interactions and covers recently discovered aspects of taurine’s effects on osteoblastogenesis, osteoclastogenesis, bone structure, and bone pathologies (e.g., osteoporosis and fracture healing), with due attention to the taurine–cartilage relationship.
-
Citations
Citations to this article as recorded by- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis
Mengxing Yin, Dezhi Zhou, Fu Jia, Xiaosan Su, Xiufang Li, Ruifen Sun, Junmin Li
Journal of Orthopaedic Surgery and Research.2023;[Epub] CrossRef - An in-silico approach to the potential modulatory effect of taurine on sclerostin (SOST) and its probable role during osteoporosis
Mazumder Adhish, I. Manjubala
Journal of Biomolecular Structure and Dynamics.2023; : 1. CrossRef - Flattening the biological age curve by improving metabolic health: to taurine or not to taurine, that’ s the question
Kwok M. Ho, Anna Lee, William Wu, Matthew T.V. Chan, Lowell Ling, Jeffrey Lipman, Jason Roberts, Edward Litton, Gavin M. Joynt, Martin Wong
Journal of Geriatric Cardiology.2023; 20(11): 813. CrossRef
- Metabolomics analysis of the potential mechanism of Yi-Guan-Jian decoction to reverse bone loss in glucocorticoid-induced osteoporosis

- Bone Metabolism
- Osteoblasts Are the Centerpiece of the Metastatic Bone Microenvironment
- Hyo Min Jeong, Sun Wook Cho, Serk In Park
- Endocrinol Metab. 2016;31(4):485-492. Published online December 20, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.485
- 3,856 View
- 46 Download
- 13 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The tumor microenvironment is comprised of diverse stromal cell populations in addition to tumor cells. Increasing evidence now clearly supports the role of microenvironment stromal cells in tumor progression and metastasis, yet the regulatory mechanisms and interactions among tumor and stromal cells remain to be elucidated. Bone metastasis is the major problem in many types of human malignancies including prostate, breast and lung cancers, and the biological basis of bone metastasis let alone curative approaches are largely undetermined. Among the many types of stromal cells in bone, osteoblasts are shown to be an important player. In this regard, osteoblasts are a key target cell type in the development of bone metastasis, but there are currently no drugs or therapeutic approaches are available that specifically target osteoblasts. This review paper summarizes the current knowledge on osteoblasts in the metastatic tumor microenvironment, aiming to provide clues and directions for future research endeavor.
-
Citations
Citations to this article as recorded by- Bone marrow adipocytes and lung cancer bone metastasis: unraveling the role of adipokines in the tumor microenvironment
Jian Li, Jialu Wu, Yanni Xie, Xijie Yu
Frontiers in Oncology.2024;[Epub] CrossRef - Circulating biomarkers for diagnosis and therapeutic monitoring in bone metastasis
Min-Kyoung Song, Serk In Park, Sun Wook Cho
Journal of Bone and Mineral Metabolism.2023; 41(3): 337. CrossRef - Mobilization of monocytic myeloid-derived suppressor cells is regulated by PTH1R activation in bone marrow stromal cells
Eun Jung Lee, Kyoung Jin Lee, Seungpil Jung, Kyong Hwa Park, Serk In Park
Bone Research.2023;[Epub] CrossRef - 2E‐Decene‐4,6‐diyn‐1‐ol‐acetate inhibits osteoclastogenesis through mitogen‐activated protein kinase‐c‐Fos‐NFATc1 signalling pathways
Young Ran Park, Xiang‐Dong Su, Saroj Kumar Shrestha, Seo Young Yang, Yunjo Soh
Clinical and Experimental Pharmacology and Physiology.2022; 49(3): 341. CrossRef - The let-7f-5p–Nme4 pathway mediates tumor necrosis factor α-induced impairment in osteogenesis of bone marrow-derived mesenchymal stem cells
Ying-Jie Zhao, Zheng-Chao Gao, Xi-Jing He, Jing Li
Biochemistry and Cell Biology.2021; 99(4): 488. CrossRef - Circulating Osteocalcin-Positive Cells as a Novel Diagnostic Biomarker for Bone Metastasis in Breast Cancer Patients
Kyung-Hun Lee, Kyoung Jin Lee, Tae-Yong Kim, Febby Hutomo, Hyun Jin Sun, Gi Jeong Cheon, Serk In Park, Sun Wook Cho, Seock-Ah Im
Journal of Bone and Mineral Research.2020; 35(10): 1838. CrossRef - The Early Results of Vertebral Pathological Compression Fracture of Extra- nodal Lymphoma with HIV-positive Patients Treated by Percutaneous Kyphoplasty
Sheng Sun, Biao Xu, Qiang Zhang, Chang-song Zhao, Rui Ma, Jie He, Yao Zhang
Current HIV Research.2020; 18(4): 248. CrossRef - Sema4D expression and secretion are increased by HIF-1α and inhibit osteogenesis in bone metastases of lung cancer
Wu-gui Chen, Jing Sun, Wei-wei Shen, Si-zhen Yang, Ying Zhang, Xu Hu, Hao Qiu, Shang-cheng Xu, Tong-wei Chu
Clinical & Experimental Metastasis.2019; 36(1): 39. CrossRef - Dual targeting c-met and VEGFR2 in osteoblasts suppresses growth and osteolysis of prostate cancer bone metastasis
Changki Lee, Young Mi Whang, Preston Campbell, Patrick L. Mulcrone, Florent Elefteriou, Sun Wook Cho, Serk In Park
Cancer Letters.2018; 414: 205. CrossRef - Targeting the tumour stroma to improve cancer therapy
Kenneth C. Valkenburg, Amber E. de Groot, Kenneth J. Pienta
Nature Reviews Clinical Oncology.2018; 15(6): 366. CrossRef - Bone Microenvironment and Role of Rank-Rankl-Opg in Breast Cancer Metastasis in Bone
Hongwei Zhang
Journal of Cancer Prevention & Current Research.2017;[Epub] CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Bone marrow adipocytes and lung cancer bone metastasis: unraveling the role of adipokines in the tumor microenvironment

- Bone Metabolism
- Dissecting Tumor-Stromal Interactions in Breast Cancer Bone Metastasis
- Yibin Kang
- Endocrinol Metab. 2016;31(2):206-212. Published online May 13, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.206
- 4,929 View
- 52 Download
- 34 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Bone metastasis is a frequent occurrence in breast cancer, affecting more than 70% of late stage cancer patients with severe complications such as fracture, bone pain, and hypercalcemia. The pathogenesis of osteolytic bone metastasis depends on cross-communications between tumor cells and various stromal cells residing in the bone microenvironment. Several growth factor signaling pathways, secreted micro RNAs (miRNAs) and exosomes are functional mediators of tumor-stromal interactions in bone metastasis. We developed a functional genomic approach to systemically identified molecular pathways utilized by breast cancer cells to engage the bone stroma in order to generate osteolytic bone metastasis. We showed that elevated expression of vascular cell adhesion molecule 1 (VCAM1) in disseminated breast tumor cells mediates the recruitment of pre-osteoclasts and promotes their differentiation to mature osteoclasts during the bone metastasis formation. Transforming growth factor β (TGF-β) is released from bone matrix upon bone destruction, and signals to breast cancer to further enhance their malignancy in developing bone metastasis. We furthered identified Jagged1 as a TGF-β target genes in tumor cells that engaged bone stromal cells through the activation of Notch signaling to provide a positive feedback to promote tumor growth and to activate osteoclast differentiation. Substantially change in miRNA expression was observed in osteoclasts during their differentiation and maturation, which can be exploited as circulating biomarkers of emerging bone metastasis and therapeutic targets for the treatment of bone metastasis. Further research in this direction may lead to improved diagnosis and treatment strategies for bone metastasis.
-
Citations
Citations to this article as recorded by- Osteoclast Cancer Cell Metabolic Cross-talk Confers PARP Inhibitor Resistance in Bone Metastatic Breast Cancer
Huijuan Fan, Zhanao Xu, Ke Yao, Bingxin Zheng, Yuan Zhang, Xuxiang Wang, Tengjiang Zhang, Xuan Li, Haitian Hu, Bin Yue, Zeping Hu, Hanqiu Zheng
Cancer Research.2024; 84(3): 449. CrossRef - Bone Marrow Mesenchymal Stem Cells Restrain the Migration and Invasion of Breast Cancer Cells by Up-Regulating miR-2158 and Inactivating RAI2/NLRP3 Pathway
Meiyu Xu, Shen Ye, Zhiqiang Tang, Shuai Gong
Journal of Biomaterials and Tissue Engineering.2023; 13(1): 162. CrossRef - Association of RANKL and EGFR gene expression with bone metastases in patients with metastatic non-small cell lung cancer
Anita J.W.M. Brouns, Lizza E.L. Hendriks, Iris J. Robbesom-van den Berge, Annemariek J.H.M. Driessen, Guido M.J.M. Roemen, Britt L.J. van Herpen, Zoë Dekkers, Bas Heitzer, Daphne J.G. Leunissen, Laura Moonen, Ragnar Lunde, Marcel Westenend, Marjolein van
Frontiers in Oncology.2023;[Epub] CrossRef - BMAL1 induces colorectal cancer metastasis by stimulating exosome secretion
Pengjuan Dong, Yaping Wang, Yutong Liu, Chunting Zhu, Jiaxin Lin, Ruizhe Qian, Luchun Hua, Chao Lu
Molecular Biology Reports.2022; 49(1): 373. CrossRef - Chemokines network in bone metastasis: Vital regulators of seeding and soiling
Gunjan Sharma, Ramesh Pothuraju, Ranjana Kumari Kanchan, Surinder Kumar Batra, Jawed Akhtar Siddiqui
Seminars in Cancer Biology.2022; 86: 457. CrossRef - The Signaling Pathways Associated With Breast Cancer Bone Metastasis
Xuelian Song, Changran Wei, Xiangqi Li
Frontiers in Oncology.2022;[Epub] CrossRef - Effects of 8-week noncontinuous aerobic exercise on the levels of CCL2, CCL5, and their respective receptors in female BALB/C mice suffering from breast cancer
Mehrnoosh Esmailiyan, Mehdi Kargarfard, Fahimeh Esfarjani, Golnaz Vaseghi
International Journal of Preventive Medicine.2022; 13(1): 55. CrossRef - Non‐coding RNAs in bone remodelling and bone metastasis: Mechanisms of action and translational relevance
Margherita Puppo, Hanna Taipaleenmäki, Eric Hesse, Philippe Clézardin
British Journal of Pharmacology.2021; 178(9): 1936. CrossRef - Sympathetic activity in breast cancer and metastasis: partners in crime
Francisco Conceição, Daniela M. Sousa, Joana Paredes, Meriem Lamghari
Bone Research.2021;[Epub] CrossRef - Extracellular Vesicles in Tumors: A Potential Mediator of Bone Metastasis
Shenglong Li, Wei Wang
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Bone marrow niches in the regulation of bone metastasis
Fenfang Chen, Yujiao Han, Yibin Kang
British Journal of Cancer.2021; 124(12): 1912. CrossRef - Exosomal miR-19a and IBSP cooperate to induce osteolytic bone metastasis of estrogen receptor-positive breast cancer
Kerui Wu, Jiamei Feng, Feng Lyu, Fei Xing, Sambad Sharma, Yin Liu, Shih-Ying Wu, Dan Zhao, Abhishek Tyagi, Ravindra Pramod Deshpande, Xinhong Pei, Marco Gabril Ruiz, Hiroyuki Takahashi, Shunsuke Tsuzuki, Takahiro Kimura, Yin-yuan Mo, Yusuke Shiozawa, Ravi
Nature Communications.2021;[Epub] CrossRef - Circulating Osteocalcin‐Positive Cells as a Novel Diagnostic Biomarker for Bone Metastasis in Breast Cancer Patients
Kyung‐Hun Lee, Kyoung Jin Lee, Tae‐Yong Kim, Febby Hutomo, Hyun Jin Sun, Gi Jeong Cheon, Serk In Park, Sun Wook Cho, Seock‐Ah Im
Journal of Bone and Mineral Research.2020; 35(10): 1838. CrossRef - Polymer nanomedicines
Jindřich Kopeček, Jiyuan Yang
Advanced Drug Delivery Reviews.2020; 156: 40. CrossRef - Osteolytic metastasis in breast cancer: effective prevention strategies
Chandi C Mandal
Expert Review of Anticancer Therapy.2020; 20(9): 797. CrossRef - The Tumor Microenvironment of Primitive and Metastatic Breast Cancer: Implications for Novel Therapeutic Strategies
Giovanni Zarrilli, Gianluca Businello, Maria Vittoria Dieci, Silvia Paccagnella, Valentina Carraro, Rocco Cappellesso, Federica Miglietta, Gaia Griguolo, Valentina Guarneri, Marcello Lo Mele, Matteo Fassan
International Journal of Molecular Sciences.2020; 21(21): 8102. CrossRef - Identification and validation of DOCK4 as a potential biomarker for risk of bone metastasis development in patients with early breast cancer
Jules A Westbrook, Steven L Wood, David A Cairns, Kathryn McMahon, Renu Gahlaut, Helene Thygesen, Mike Shires, Stephanie Roberts, Helen Marshall, Maria R Oliva, Mark J Dunning, Andrew M Hanby, Peter J Selby, Valerie Speirs, Georgia Mavria, Robert E Colema
The Journal of Pathology.2019; 247(3): 381. CrossRef - The Relationship between Exosomes and Cancer: Implications for Diagnostics and Therapeutics
Wendy W. Weston, Timothy Ganey, H. Thomas Temple
BioDrugs.2019; 33(2): 137. CrossRef - In Vivo Assessment of VCAM-1 Expression by SPECT/CT Imaging in Mice Models of Human Triple Negative Breast Cancer
Montemagno, Dumas, Cavaillès, Ahmadi, Bacot, Debiossat, Soubies, Djaïleb, Leenhardt, Leiris, Dufies, Pagès, Hernot, Devoogdt, Perret, Riou, Fagret, Ghezzi, Broisat
Cancers.2019; 11(7): 1039. CrossRef - Notch and breast cancer metastasis: Current knowledge, new sights and targeted therapy (Review)
Yu Zhang, Zi‑Yan Xie, Xuan‑Tong Guo, Xing‑Hua Xiao, Li‑Xia Xiong
Oncology Letters.2019;[Epub] CrossRef - NPNT promotes early-stage bone metastases in breast cancer by regulation of the osteogenic niche
Dongsheng Wang, Chenglong Zhao, Liangliang Gao, Yao Wang, Xin Gao, Liang Tang, Kun Zhang, Zhenxi Li, Jing Han, Jianru Xiao
Journal of Bone Oncology.2018; 13: 91. CrossRef - Placental exosomes: A proxy to understand pregnancy complications
Jin Jin, Ramkumar Menon
American Journal of Reproductive Immunology.2018;[Epub] CrossRef - Understanding the Bone in Cancer Metastasis
Jaime Fornetti, Alana L Welm, Sheila A Stewart
Journal of Bone and Mineral Research.2018; 33(12): 2099. CrossRef - Role of Tumor-Derived Chemokines in Osteolytic Bone Metastasis
Salvatore J. Coniglio
Frontiers in Endocrinology.2018;[Epub] CrossRef - The role of exosomes in cancer metastasis
Teresa Bernadette Steinbichler, József Dudás, Herbert Riechelmann, Ira-Ida Skvortsova
Seminars in Cancer Biology.2017; 44: 170. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Impaired Bone Matrix Alignment Induced by Breast Cancer Metastasis
Aiko Sekita, Aira Matsugaki, Takayoshi Nakano
Journal of the Japan Institute of Metals.2017; 81(6): 308. CrossRef - SMURF2 regulates bone homeostasis by disrupting SMAD3 interaction with vitamin D receptor in osteoblasts
Zhan Xu, Matthew B. Greenblatt, Guang Yan, Heng Feng, Jun Sun, Sutada Lotinun, Nicholas Brady, Roland Baron, Laurie H. Glimcher, Weiguo Zou
Nature Communications.2017;[Epub] CrossRef - Bone Microenvironment and Role of Rank-Rankl-Opg in Breast Cancer Metastasis in Bone
Hongwei Zhang
Journal of Cancer Prevention & Current Research.2017;[Epub] CrossRef - Tumor–Stroma Interactions in Bone Metastasis: Molecular Mechanisms and Therapeutic Implications
Hanqiu Zheng, Wenyang Li, Yibin Kang
Cold Spring Harbor Symposia on Quantitative Biology.2016; 81: 151. CrossRef - Breast cancer cells obtain an osteomimetic featureviaepithelial-mesenchymal transition that have undergone BMP2/RUNX2 signaling pathway induction
Cong-Cong Tan, Gui-Xi Li, Li-Duan Tan, Xin Du, Xiao-Qing Li, Rui He, Qing-Shan Wang, Yu-Mei Feng
Oncotarget.2016; 7(48): 79688. CrossRef - Heterotypic models of osteosarcoma recapitulate tumor heterogeneity and biological behavior
Milcah C. Scott, Hirotaka Tomiyasu, John R. Garbe, Ingrid Cornax, Clarissa Amaya, M Gerard O'Sullivan, Subbaya Subramanian, Brad A. Bryan, Jaime F. Modiano
Disease Models & Mechanisms.2016;[Epub] CrossRef - Osteoblasts Are the Centerpiece of the Metastatic Bone Microenvironment
Hyo Min Jeong, Sun Wook Cho, Serk In Park
Endocrinology and Metabolism.2016; 31(4): 485. CrossRef
- Osteoclast Cancer Cell Metabolic Cross-talk Confers PARP Inhibitor Resistance in Bone Metastatic Breast Cancer

- Bone Metabolism
- NF-κB-Mediated Regulation of Osteoclastogenesis
- Brendan F. Boyce, Yan Xiu, Jinbo Li, Lianping Xing, Zhenqiang Yao
- Endocrinol Metab. 2015;30(1):35-44. Published online March 27, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.1.35
- 7,689 View
- 139 Download
- 224 Web of Science
- 216 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Osteoclasts are multinucleated cells formed mainly on bone surfaces in response to cytokines by fusion of bone marrow-derived myeloid lineage precursors that circulate in the blood. Major advances in understanding of the molecular mechanisms regulating osteoclast formation and functions have been made in the past 20 years since the discovery that their formation requires nuclear factor-kappa B (NF-κB) signaling and that this is activated in response to the essential osteoclastogenic cytokine, receptor activator of NF-κB ligand (RANKL), which also controls osteoclast activation to resorb (degrade) bone. These studies have revealed that RANKL and some pro-inflammatory cytokines, including tumor necrosis factor, activate NF-κB and downstream signaling, including c-Fos and nuclear factor of activated T-cells, cytoplasmic 1 (NFATc1), and inhibition of repressors of NFATc1 signaling, to positively regulate osteoclast formation and functions. However, these cytokines also activate NF-κB signaling that can limit osteoclast formation through the NF-κB signaling proteins, TRAF3 and p100, and the suppressors of c-Fos/NFATc1 signaling, IRF8, and RBP-J. This paper reviews current understanding of how NF-κB signaling is involved in the positive and negative regulation of cytokine-mediated osteoclast formation and activation.
-
Citations
Citations to this article as recorded by- Photo biomodulation of dental derived stem cells to ameliorate regenerative capacity: In vitro study
Alaa Medhat, Medhat A. El-Zainy, Iman Fathy
The Saudi Dental Journal.2024; 36(2): 347. CrossRef - Cucumber seed polypeptides regulate RANKL-induced osteoclastogenesis through OPG/RANKL/RANK and NF-κB
Tao Yu, Xiao Liu, Meng Jiang, Yuanyue Li, Heng Su, Ben Niu
In Vitro Cellular & Developmental Biology - Animal.2024; 60(1): 54. CrossRef - MCP‐5 suppresses osteoclast differentiation through Ccr5 upregulation
Jung Ha Kim, Kabsun Kim, Inyoung Kim, Semun Seong, Jeong‐Tae Koh, Nacksung Kim
Journal of Cellular Physiology.2024;[Epub] CrossRef - S-nitrosoglutathione reductase-dependent p65 denitrosation promotes osteoclastogenesis by facilitating recruitment of p65 to NFATc1 promoter
Shumin Liu, Qian Lu, Min Wang, Huilin Guo, Yiwen Wang, Jingwen Nong, Shuo Wang, Haibin Xia, Ting Xia, Huifang Sun
Bone.2024; 181: 117036. CrossRef - A Missense Variant in TP53 Could Be a Genetic Biomarker Associated with Bone Tissue Alterations
Ricardo Usategui-Martín, Nadia Galindo-Cabello, Salvador Pastor-Idoate, José María Fernández-Gómez, Álvaro del Real, Diego Ferreño, Rebeca Lapresa, Francisco Martín-Rodriguez, José A. Riancho, Ángeles Almeida, José Luis Pérez-Castrillón
International Journal of Molecular Sciences.2024; 25(3): 1395. CrossRef - Cellular and Exosomal MicroRNAs: Emerging Clinical Relevance as Targets for Breast Cancer Diagnosis and Prognosis
Faith Mokobi Zablon, Parth Desai, Kristen Dellinger, Shyam Aravamudhan
Advanced Biology.2024;[Epub] CrossRef - Discovery of a Potent Antiosteoporotic Drug Molecular Scaffold Derived from Angelica sinensis and Its Bioinspired Total Synthesis
Jian Zou, Zuo-Cheng Qiu, Qiang-Qiang Yu, Jia-Ming Wu, Yong-Heng Wang, Ke-Da Shi, Yi-Fang Li, Rong-Rong He, Ling Qin, Xin-Sheng Yao, Xin-Luan Wang, Hao Gao
ACS Central Science.2024; 10(3): 628. CrossRef - Roles and mechanisms of optineurin in bone metabolism
Junjie Jin, Ruiqi Huang, Yixing Chang, Xuejie Yi
Biomedicine & Pharmacotherapy.2024; 172: 116258. CrossRef - Therapeutic potential of a prominent dihydroxyflavanone pinocembrin for osteolytic bone disease: In vitro and in vivo evidence
Guoju Hong, Shuqiang Li, Guanqiang Zheng, Xiaoxia Zheng, Qunzhang Zhan, Lin Zhou, Qiushi Wei, Wei He, Zhenqiu Chen
Journal of Orthopaedic Translation.2024; 45: 197. CrossRef - Hydroxychavicol Inhibits In Vitro Osteoclastogenesis via the Suppression of NF-κB Signaling Pathway
Sirada Srihirun, Satarat Mathithiphark, Chareerut Phruksaniyom, Pitchanun Kongphanich, Wisutthaporn Inthanop, Thanaporn Sriwantana, Salunya Tancharoen, Nathawut Sibmooh, Pornpun Vivithanaporn
Biomolecules & Therapeutics.2024; 32(2): 205. CrossRef - Inhibition of NF-κB and ERK signaling pathways in osteoclasts and M1 macrophage polarization: Mechanistic insights into the anti-osteoporotic effects of Pseudolaric acid B
Liyan Liu, Cheng Xiang, Tao Li, Ziyue Zhao, Tao Xiao, Zhengxiao Ouyang
Life Sciences.2024; 345: 122592. CrossRef - Bone Equilibria and Disruptions
Harold Jacob Pieter van Bosse
Journal of the Pediatric Orthopaedic Society of North America.2024; : 100059. CrossRef - HDAC5-Mediated Acetylation of p100 Suppresses Its Processing
Jianqi Wang, Shuainan Wu, Lu Liu, Ying Pang, Zhaobao Li, Hong Mu
International Dental Journal.2023; 73(3): 387. CrossRef - HSP90β promotes osteoclastogenesis by dual-activation of cholesterol synthesis and NF-κB signaling
Hui-Min Cheng, Mingming Xing, Ya-Ping Zhou, Weitao Zhang, Zeyu Liu, Lan Li, Zuguo Zheng, Yuanchen Ma, Pingping Li, Xiaoxuan Liu, Ping Li, Xiaojun Xu
Cell Death & Differentiation.2023; 30(3): 673. CrossRef - Oligosaccharides from Sargassum thunbergii inhibit osteoclast differentiation via regulation of IRF-8 signaling
Weihua Jin, Fen Chen, Qiufu Fang, Genxiang Mao, Yizhong Bao
Experimental Gerontology.2023; 172: 112057. CrossRef - ADR3, a next generation i-body to human RANKL, inhibits osteoclast formation and bone resorption
Heng Qiu, Christopher Hosking, Emel Rothzerg, Ariela Samantha, Kai Chen, Vincent Kuek, Haiming Jin, Sipin Zhu, Alice Vrielink, Kevin Lim, Michael Foley, Jiake Xu
Journal of Biological Chemistry.2023; 299(2): 102889. CrossRef - In vitrobiological evaluation of epigallocatechin gallate (EGCG) release from three-dimensional printed (3DP) calcium phosphate bone scaffolds
Yongdeok Jo, Naboneeta Sarkar, Susmita Bose
Journal of Materials Chemistry B.2023; 11(24): 5503. CrossRef - The Roles of TRAF3 in Immune Responses
Mengjiao Lin, Xiaoli Ji, Yan Lv, Dawei Cui, Jue Xie, Dimitri Poddighe
Disease Markers.2023; 2023: 1. CrossRef - (S)-2-(Cyclobutylamino)-N-(3-(3,4-dihydroisoquinolin-2(1H)-yl)-2-hydroxypropyl)isonicotinamide Attenuates RANKL-Induced Osteoclast Differentiation by Inhibiting NF-κB Nuclear Translocation
Mina Ding, Eunjin Cho, Zhihao Chen, Sang-Wook Park, Tae-Hoon Lee
International Journal of Molecular Sciences.2023; 24(5): 4327. CrossRef - Safranal inhibits estrogen-deficiency osteoporosis by targeting Sirt1 to interfere with NF-κB acetylation
Sun-Ren Sheng, Yu-Hao Wu, Zi-Han Dai, Chen Jin, Gao-Lu He, Shu-Qing Jin, Bi-Yao Zhao, Xin Zhou, Cheng-Long Xie, Gang Zheng, Nai-Feng Tian
Phytomedicine.2023; 114: 154739. CrossRef - Discovery of PMSA Derivative 11 as a Novel Lead Compound for Therapeutic Treatment of Osteoporosis In Vitro and In Vivo
Zhihao Chen, Karthik Rajan Rajamanickam, Mina Ding, Sang Kyoon Kim, Sang-wook Park, Eunae Kim, Sunwoo Lee, Tae-Hoon Lee
Journal of Medicinal Chemistry.2023; 66(10): 6766. CrossRef - Sesamol improves bone mass in ovary intact growing and adult rats but accelerates bone deterioration in the ovariectomized rats
Kalpana Patel, SVVS Ravi Mangu, Shinde Vijay Sukhdeo, Kunal Sharan
The Journal of Nutritional Biochemistry.2023; 119: 109384. CrossRef - Unraveling the potential of 3D bioprinted immunomodulatory materials for regulating macrophage polarization: State-of-the-art in bone and associated tissue regeneration
Sayan Deb Dutta, Tejal V. Patil, Keya Ganguly, Aayushi Randhawa, Ki-Taek Lim
Bioactive Materials.2023; 28: 284. CrossRef - Fanca deficiency is associated with alterations in osteoclastogenesis that are rescued by TNFα
Alessia Oppezzo, Lovely Monney, Henri Kilian, Lofti Slimani, Frédérique Maczkowiak-Chartois, Filippo Rosselli
Cell & Bioscience.2023;[Epub] CrossRef - TMBIM6 deficiency leads to bone loss by accelerating osteoclastogenesis
Sun-Ju Yi, You-Jee Jang, Seokchan Lee, Sung-Jin Cho, Kyuho Kang, Jae-Il Park, Han-Jung Chae, Hyung-Ryong Kim, Kyunghwan Kim
Redox Biology.2023; 64: 102804. CrossRef - The role of E3 ubiquitin ligases in bone homeostasis and related diseases
Yuechao Dong, Yangshan Chen, Guixing Ma, Huiling Cao
Acta Pharmaceutica Sinica B.2023; 13(10): 3963. CrossRef - Bioactive silica nanoparticles target autophagy, NF-κB, and MAPK pathways to inhibit osteoclastogenesis
Jamie Arnst, Zhaocheng Jing, Cameron Cohen, Shin-Woo Ha, Manjula Viggeswarapu, George R. Beck
Biomaterials.2023; 301: 122238. CrossRef - Comparative Study of the Cytokine Profiles of Serum and Tissues from Patients with the Ossification of the Posterior Longitudinal Ligament
Li-Yu Fay, Chao-Hung Kuo, Hsuan-Kan Chang, Mei-Yin Yeh, Chih-Chang Chang, Chin-Chu Ko, Tsung-Hsi Tu, Yi-Hsuan Kuo, Wang-Yu Hsu, Chien-Hui Hung, Ching-Jung Chen, Jau-Ching Wu, May-Jywan Tsai, Wen-Cheng Huang, Henrich Cheng, Meng-Jen Lee
Biomedicines.2023; 11(7): 2021. CrossRef - Protaetia brevitarsis Extract Attenuates RANKL-Induced Osteoclastogenesis by Inhibiting the JNK/NF-κB/PLCγ2 Signaling Pathway
Hye-Yeon Jang, Jeong-Mi Kim, Jong-Suk Kim, Byeong-Soo Kim, Young-Rae Lee, Jun Sang Bae
Nutrients.2023; 15(14): 3193. CrossRef - Madecassic acid suppresses osteoclast differentiation and bone resorption by inhibiting RANKL‐induced NF‐κB, JNK and NFAT signaling pathways
Peiru Su, Xiangya Luo, Chunping Zeng, Lin Zhou
Rheumatology & Autoimmunity.2023; 3(4): 220. CrossRef - Guided Bone Regeneration Using Barrier Membrane in Dental Applications
Kakyung Kim, Yingchao Su, Allan J. Kucine, Ke Cheng, Donghui Zhu
ACS Biomaterials Science & Engineering.2023; 9(10): 5457. CrossRef - Irisin as an agent for protecting against osteoporosis: A review of the current mechanisms and pathways
Xinli Hu, Zheng Wang, Wei Wang, Peng Cui, Chao Kong, Xiaolong Chen, Shibao Lu
Journal of Advanced Research.2023;[Epub] CrossRef - Anti-Osteoporotic Potential of Water Extract of Anethum graveolens L. Seeds
Seon-A Jang, Sung-Ju Lee, Youn-Hwan Hwang, Hyunil Ha
Nutrients.2023; 15(19): 4302. CrossRef - Synthesis and evaluation of 2-NMPA derivatives as potential agents for prevention of osteoporosis in vitro and in vivo
Zhihao Chen, Devaneyan Joseph, Mina Ding, Swapnil Pandurang Bhujbal, Robin Prakash Sirvin Rajan, Eunae Kim, Sang-wook Park, Sunwoo Lee, Tae-Hoon Lee
European Journal of Medicinal Chemistry.2023; 260: 115767. CrossRef - A novel Glycyrrhiza glabra extract liquiritin targeting NFATc1 activity and ROS levels to counteract ovariectomy-induced osteoporosis and bone loss in murine model
Guoju Hong, Lin Zhou, Guanqiang Zheng, Xiaoxia Zheng, Zhenqiu Chen, Wei He, Qiushi Wei
Frontiers in Pharmacology.2023;[Epub] CrossRef - Wearable Device for Cumulative Chlorobenzene Detection and Accessible Mitigation Strategies
Aryan Mago, Yeon-Suk Yang, Jae-Hyuck Shim, Aijaz Ahmad John
Sensors.2023; 23(18): 7904. CrossRef - Natural drug asiaticoside inhibits osteoclast differentiation and promotes repair of steroid-induced osteonecrosis of femoral head via RANKL pathway
Haijian Wu, Bowen Guo, Hongfa Zhong, Hui Ying
Materials Express.2023; 13(11): 1855. CrossRef - Regulating Macrophages through Immunomodulatory Biomaterials Is a Promising Strategy for Promoting Tendon-Bone Healing
Haihan Gao, Liren Wang, Haocheng Jin, Zhiqi Lin, Ziyun Li, Yuhao Kang, Yangbao Lyu, Wenqian Dong, Yefeng Liu, Dingyi Shi, Jia Jiang, Jinzhong Zhao
Journal of Functional Biomaterials.2022; 13(4): 243. CrossRef - Trim14 promotes osteoclastogenesis and noncanonical NF‐κB activation by targeting p100/p52 in chronic periodontitis
Jian Zhang, Xiuya Lin, Yang Sun, Jianming Wei, Jiankun Wu
Oral Diseases.2022; 28(7): 1958. CrossRef - Nanomaterials for neurodegenerative diseases: Molecular mechanisms guided design and applications
Tianzhong Li, Xueyan Hou, Yu Qi, Xiaohan Duan, Pengcheng Yan, Haoru Zhu, Zhongjian Xie, Han Zhang
Nano Research.2022; 15(4): 3299. CrossRef - 3D printing monetite-coated Ti-6Al-4V surface with osteoimmunomodulatory function to enhance osteogenesis
Linquan Zhou, Jiacheng You, Zhenyu Wang, Yang Gu, Dehui Chen, Bin Lin, Xin Zhao, Jiemin Lin, Jinxin Lin, Wenge Liu
Biomaterials Advances.2022; 134: 112562. CrossRef - D(-)-salicin inhibits RANKL-induced osteoclast differentiation and function in vitro
Yu Xiao, Yansi Xian, Xinmei Hu, Zhongquan Qi
Fitoterapia.2022; 157: 104981. CrossRef - CaP-based anti-inflammatory HIF-1α siRNA-encapsulating nanoparticle for rheumatoid arthritis therapy
Xuesong Liu, Ruru Guo, Shicheng Huo, Huan Chen, Qingxiang Song, Gan Jiang, Ye Yu, Jialin Huang, Shaowei Xie, Xiaoling Gao, Liangjing Lu
Journal of Controlled Release.2022; 343: 314. CrossRef - Anti-Osteoporosis Effect of Perilla frutescens Leaf Hexane Fraction through Regulating Osteoclast and Osteoblast Differentiation
Kanokkarn Phromnoi, Supachai Yodkeeree, Komsak Pintha, Sariya Mapoung, Maitree Suttajit, Chalermpong Saenjum, Pornngarm Dejkriengkraikul
Molecules.2022; 27(3): 824. CrossRef - Biomaterial-induced pathway modulation for bone regeneration
Steven Vermeulen, Zeinab Tahmasebi Birgani, Pamela Habibovic
Biomaterials.2022; 283: 121431. CrossRef - Proteasome inhibition-enhanced fracture repair is associated with increased mesenchymal progenitor cells in mice
Hengwei Zhang, Xing Li, Jiatong Liu, Xi Lin, Lingpeng Pei, Brendan F. Boyce, Lianping Xing, Gianpaolo Papaccio
PLOS ONE.2022; 17(2): e0263839. CrossRef - α-Asarone Attenuates Osteoclastogenesis and Prevents Against Oestrogen-Deficiency Induced Osteoporosis
Hao Tian, Tao Jiang, Kai Yang, Ruonan Ning, Tianqi Wang, Qi Zhou, Niandong Qian, Ping Huang, Lei Guo, Min Jiang, Xiaobing Xi, Xing Xu, Lianfu Deng
Frontiers in Pharmacology.2022;[Epub] CrossRef - Regulation of osteoclast-mediated bone resorption by microRNA
Ling Ji, Xinyi Li, Shushu He, Song Chen
Cellular and Molecular Life Sciences.2022;[Epub] CrossRef - Wheel-Running Exercise Protects Ovariectomized Mice from Bone Loss via IFN-γ-Mediated Suppression of the NF-κB and MAPK Pathways
Hao Shen, Jiaheng He, Xuwei Ling, Chang Liu, Yi Wang, Xiongjinfu Zhang, Xu He, Huilin Yang, Mimi Chen, Qin Shi, Dimitrios Draganidis
Oxidative Medicine and Cellular Longevity.2022; 2022: 1. CrossRef - Transcriptomic Analysis Provides Insights to Reveal the bmp6 Function Related to the Development of Intermuscular Bones in Zebrafish
Huan Xu, Guangxiang Tong, Ting Yan, Le Dong, Xiaoxing Yang, Dongyu Dou, Zhipeng Sun, Tianqi Liu, Xianhu Zheng, Jian Yang, Xiaowen Sun, Yi Zhou, Youyi Kuang
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - The Roles of RANK/RANKL/OPG in Cardiac, Skeletal, and Smooth Muscles in Health and Disease
Laetitia Marcadet, Zineb Bouredji, Anteneh Argaw, Jérôme Frenette
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Strontium Functionalized in Biomaterials for Bone Tissue Engineering: A Prominent Role in Osteoimmunomodulation
Jiaqian You, Yidi Zhang, Yanmin Zhou
Frontiers in Bioengineering and Biotechnology.2022;[Epub] CrossRef - Unkeito Suppresses RANKL-Mediated Osteoclastogenesis via the Blimp1–Bcl6 and NF-κB Signaling Pathways and Enhancing Osteoclast Apoptosis
Ke Fang, Yuki Murakami, Seiji Kanda, Takaki Shimono, Anh Tuan Dang, Mitsuaki Ono, Toshimasa Nishiyama
International Journal of Molecular Sciences.2022; 23(14): 7814. CrossRef - Immunomodulation Effect of Biomaterials on Bone Formation
Tong Zhao, Zhuangzhuang Chu, Jun Ma, Liping Ouyang
Journal of Functional Biomaterials.2022; 13(3): 103. CrossRef - Update on the pathogenesis and genetics of Paget’s disease of bone
Luigi Gennari, Domenico Rendina, Daniela Merlotti, Guido Cavati, Christian Mingiano, Roberta Cosso, Maria Materozzi, Filippo Pirrotta, Veronica Abate, Marco Calabrese, Alberto Falchetti
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Praeruptorin B inhibits osteoclastogenesis by targeting GSTP1 and impacting on the S-glutathionylation of IKKβ
Kebin Xu, Ziyi Chen, Jialong Hou, Chenlin Dong, Chengge Shi, Linglin Gao, Zhixian Huang, Ge Shen, Te Wang, Yan Zhou
Biomedicine & Pharmacotherapy.2022; 154: 113529. CrossRef - How zoledronic acid improves osteoporosis by acting on osteoclasts
Biao Wang, Yi Zhan, Liang Yan, Dingjun Hao
Frontiers in Pharmacology.2022;[Epub] CrossRef - CpG Oligodeoxynucleotides Inhibit RANKL-Induced Osteoclast Formation by Upregulating A20 Deubiquitinase in RAW 264.7 Cells
Seong-Kyu Kim, Jung-Yoon Choe, Ki-Yeun Park, Nadra Nilsen
Mediators of Inflammation.2022; 2022: 1. CrossRef - Zuogui Pill Ameliorates Glucocorticoid-Induced Osteoporosis through ZNF702P-Based ceRNA Network: Bioinformatics Analysis and Experimental Validation
Peng Zhang, Honglin Chen, Qi Shang, Guifeng Chen, Jiahui He, Gengyang Shen, Xiang Yu, Zhida Zhang, Wenhua Zhao, Guangye Zhu, Jinglin Huang, De Liang, Jingjing Tang, Jianchao Cui, Zhixiang Liu, Xiaobing Jiang, Hui Ren, Jun Jiang
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Sec-O-Glucosylhamaudol Inhibits RANKL-Induced Osteoclastogenesis by Repressing 5-LO and AKT/GSK3β Signaling
Jinjin Cao, Ming-Xue Zhou, Xinyan Chen, Menglu Sun, Congmin Wei, Qisheng Peng, Zhou Cheng, Wanchun Sun, Hongbing Wang
Frontiers in Immunology.2022;[Epub] CrossRef - MOTS-c, the Most Recent Mitochondrial Derived Peptide in Human Aging and Age-Related Diseases
Zahra Mohtashami, Mithalesh K. Singh, Nasim Salimiaghdam, Mustafa Ozgul, M. Cristina Kenney
International Journal of Molecular Sciences.2022; 23(19): 11991. CrossRef - Topography-mediated immunomodulation in osseointegration; Ally or Enemy
Sajjad Shirazi, Sriram Ravindran, Lyndon F. Cooper
Biomaterials.2022; 291: 121903. CrossRef - Modulating glycosphingolipid metabolism and autophagy improves outcomes in pre-clinical models of myeloma bone disease
Houfu Leng, Hanlin Zhang, Linsen Li, Shuhao Zhang, Yanping Wang, Selina J. Chavda, Daria Galas-Filipowicz, Hantao Lou, Adel Ersek, Emma V. Morris, Erdinc Sezgin, Yi-Hsuan Lee, Yunsen Li, Ana Victoria Lechuga-Vieco, Mei Tian, Jian-Qing Mi, Kwee Yong, Qing
Nature Communications.2022;[Epub] CrossRef - Breaking the vicious cycle between tumor cell proliferation and bone resorption by chloroquine-loaded and bone-targeted polydopamine nanoparticles
Yitong Wang, Hui Chen, Kaili Lin, Ting Ying, Quan Huang, Xiaopan Cai, Jianru Xiao, Qiang Zhang, Yiyun Cheng
Science China Materials.2021; 64(2): 474. CrossRef - Delineating role of NF‐κB and interacting cytokines during prostate cancer‐induced osteoclastogenesis
Mohit Jadli, Kulbhushan Thakur, Nikita Aggarwal, Arun Chhokar, Rakhi Bibban, Tejveer Singh, Anjali Bhat, Alok C. Bharti
Journal of Cellular Biochemistry.2021; 122(2): 259. CrossRef - Dectin‐1–mediated suppression of RANKL‐induced osteoclastogenesis by glucan from baker's yeast
Shiika Hara, Yoshie Nagai‐Yoshioka, Ryota Yamasaki, Yoshiyuki Adachi, Yuko Fujita, Kouji Watanabe, Kenshi Maki, Tatsuji Nishihara, Wataru Ariyoshi
Journal of Cellular Physiology.2021; 236(7): 5098. CrossRef - Impact of low bone mass and antiresorptive therapy on antibiotic efficacy in a rat model of orthopedic device‐related infection
Keith Thompson, Linda Freitag, Ursula Styger, Karin Camenisch, Stephan Zeiter, Daniel Arens, R. Geoff Richards, Thomas F. Moriarty, Vincent A. Stadelmann
Journal of Orthopaedic Research.2021; 39(2): 415. CrossRef - RANKL as the master regulator of osteoclast differentiation
Hiroshi Takayanagi
Journal of Bone and Mineral Metabolism.2021; 39(1): 13. CrossRef - Bone Morphogenetic Protein-2 Promotes Osteoclasts-mediated Osteolysis via Smad1 and p65 Signaling Pathways
Xiong Miao, Jiabin Yuan, Jinhui Wu, Jiaoyang Zheng, Weina Zheng, Fei Wang, Chao Wang, Xiaoming Li, Shu Liu, Zhicai Shi, Jingfeng Li
Spine.2021; 46(4): E234. CrossRef - Effects of Caffeic Acid and Its Derivatives on Bone: A Systematic Review
Sophia Ogechi Ekeuku, Kok-Lun Pang, Kok-Yong Chin
Drug Design, Development and Therapy.2021; Volume 15: 259. CrossRef - 2-NPPA Mitigates Osteoclastogenesis via Reducing TRAF6-Mediated c-fos Expression
Zhihao Chen, Mina Ding, Eunjin Cho, Jihyoun Seong, Sunwoo Lee, Tae-Hoon Lee
Frontiers in Pharmacology.2021;[Epub] CrossRef - Dental pulp–derived stem cells inhibit osteoclast differentiation by secreting osteoprotegerin and deactivating AKT signalling in myeloid cells
Suman Kanji, Ripon Sarkar, Asmita Pramanik, Sudhir Kshirsagar, Carl J. Greene, Hiranmoy Das
Journal of Cellular and Molecular Medicine.2021; 25(5): 2390. CrossRef - Bone anti-resorptive effects of coumarins on RANKL downstream cellular signaling: a systematic review of the literature
Samia Jessica Silva Tavares, Vilma Lima
Fitoterapia.2021; 150: 104842. CrossRef - Isofraxidin Inhibits Receptor Activator of Nuclear Factor-κB Ligand–Induced Osteoclastogenesis in Bone Marrow–Derived Macrophages Isolated from Sprague–Dawley Rats by Regulating NF-κB/NFATc1 and Akt/NFATc1 Signaling Pathways
Wei Wang, Bo Wang
Cell Transplantation.2021; 30: 096368972199032. CrossRef - Smac-mimetics reduce numbers and viability of human osteoclasts
Ingrid Nyhus Moen, Marita Westhrin, Erling Håland, Markus Haug, Unni Nonstad, Merisa Klaharn, Therese Standal, Kristian K. Starheim
Cell Death Discovery.2021;[Epub] CrossRef - TNF is a homoeostatic regulator of distinct epigenetically primed human osteoclast
precursors
Cecilia Ansalone, John Cole, Sabarinadh Chilaka, Flavia Sunzini, Shatakshi Sood, Jamie Robertson, Stefan Siebert, Iain B McInnes, Carl S Goodyear
Annals of the Rheumatic Diseases.2021; 80(6): 748. CrossRef - The role of statins in the differentiation and function of bone cells
Sajad Chamani, Luca Liberale, Leila Mobasheri, Fabrizio Montecucco, Khalid Al‐Rasadi, Tannaz Jamialahmadi, Amirhossein Sahebkar
European Journal of Clinical Investigation.2021;[Epub] CrossRef - Biological Evaluation and Transcriptomic Analysis of Corylin as an Inhibitor of Osteoclast Differentiation
Anna Xiao-Dan Yu, Jian Xiao, Shi-Zheng Zhao, Xiang-Peng Kong, Kenneth Kin-Leung Kwan, Brody Zhong-Yu Zheng, Kevin Qi-Yun Wu, Tina Ting-Xia Dong, Karl Wah-Keung Tsim
International Journal of Molecular Sciences.2021; 22(7): 3540. CrossRef - Testing the efficacy of a human full-length OPG-Fc analog in a severe model of cardiotoxin-induced skeletal muscle injury and repair
Zineb Bouredji, Dounia Hamoudi, Laetitia Marcadet, Anteneh Argaw, Jérôme Frenette
Molecular Therapy - Methods & Clinical Development.2021; 21: 559. CrossRef - β-Boswellic Acid Inhibits RANKL-Induced Osteoclast Differentiation and Function by Attenuating NF-κB and Btk-PLCγ2 Signaling Pathways
Gyeong Do Park, Yoon-Hee Cheon, So Young Eun, Chang Hoon Lee, Myeung Su Lee, Ju-Young Kim, Hae Joong Cho
Molecules.2021; 26(9): 2665. CrossRef - A novel RANKL‐targeted flavonoid glycoside prevents osteoporosis through inhibiting NFATc1 and reactive oxygen species
Guoju Hong, Zhenqiu Chen, Xiaorui Han, Lin Zhou, Fengxiang Pang, Rishana Wu, Yingshan Shen, Xiaoming He, Zhinan Hong, Ziqi Li, Wei He, Qiushi Wei
Clinical and Translational Medicine.2021;[Epub] CrossRef - Oxymatrine Attenuates Osteoclastogenesis via Modulation of ROS-Mediated SREBP2 Signaling and Counteracts Ovariectomy-Induced Osteoporosis
Chao Jiang, Qingliang Ma, Shiyu Wang, Yang Shen, An Qin, Shunwu Fan, Zhiwei Jie
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - S100 Calcium-Binding Protein P Secreted from Megakaryocytes Promotes Osteoclast Maturation
Seung-Hoon Lee, Hye Jung Ihn, Eui Kyun Park, Jung-Eun Kim
International Journal of Molecular Sciences.2021; 22(11): 6129. CrossRef - Sesamolin Protects Mice From Ovariectomized Bone Loss by Inhibiting Osteoclastogenesis and RANKL-Mediated NF-κB and MAPK Signaling Pathways
Xue Yang, Jiamin Liang, Ziyi Wang, Yuangang Su, Yunfei Zhan, Zuoxing Wu, Jing Li, Xuedong Li, Runfeng Chen, Jinmin Zhao, Jiake Xu, Qian Liu, Bo Zhou
Frontiers in Pharmacology.2021;[Epub] CrossRef - Regulation of Osteoclastogenesis and Bone Resorption by miRNAs
Kazuki Inoue, Courtney Ng, Yuhan Xia, Baohong Zhao
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Genomic locus proteomic screening identifies the NF-κB signaling pathway components NFκB1 and IKBKG as transcriptional regulators of Ripk3 in endothelial cells
Siqi Gao, Matthew Menendez, Katarzyna Kurylowicz, Courtney T. Griffin, Ramani Ramchandran
PLOS ONE.2021; 16(6): e0253519. CrossRef - IL-3 inhibits rat osteoclast differentiation induced by TNF-α and other pro-osteoclastogenic cytokines
Vikrant Piprode, Kanupriya Singh, Anil Kumar, Snehal R. Joshi, Mohan R. Wani
Journal of Biosciences.2021;[Epub] CrossRef - Water Extract of Mentha arvensis L. Attenuates Estrogen Deficiency-Induced Bone Loss by Inhibiting Osteoclast Differentiation
Seon-A Jang, Youn-Hwan Hwang, Hyun Yang, Jin Ah Ryuk, Taesoo Kim, Hyunil Ha
Frontiers in Pharmacology.2021;[Epub] CrossRef - Exosomal tumor necrosis factor‐α from hepatocellular cancer cells (Huh‐7) promote osteoclast differentiation
Ching‐Hao Li, Kalaiselvi Palanisamy, Xin Li, Shao‐Hua Yu, I‐Kuan Wang, Chi‐Yuan Li, Kuo‐Ting Sun
Journal of Cellular Biochemistry.2021; 122(11): 1749. CrossRef - Curcuminoid (CRE-Ter)/Liposome as delivery platform for anti-osteoclastogenesis via NF-κB/ERK pathways in RANKL-induced RAW 264.7 cells through PLA foams
Yutthana Pengjam, Pharkphoom Panichayupakaranant, Varaporn Tanrattanakul
Heliyon.2021; 7(9): e07823. CrossRef - Osteoblast lineage cells and periodontal ligament fibroblasts regulate orthodontic tooth movement that is dependent on Nuclear Factor-kappa B (NF-kB) activation
Hyeran Helen Jeon, Chia-Ying Yang, Min Kyung Shin, Jingyi Wang, Juhin Hiren Patel, Chun-Hsi Chung, Dana T. Graves
The Angle Orthodontist.2021; 91(5): 664. CrossRef - Exosomal miR-19a and IBSP cooperate to induce osteolytic bone metastasis of estrogen receptor-positive breast cancer
Kerui Wu, Jiamei Feng, Feng Lyu, Fei Xing, Sambad Sharma, Yin Liu, Shih-Ying Wu, Dan Zhao, Abhishek Tyagi, Ravindra Pramod Deshpande, Xinhong Pei, Marco Gabril Ruiz, Hiroyuki Takahashi, Shunsuke Tsuzuki, Takahiro Kimura, Yin-yuan Mo, Yusuke Shiozawa, Ravi
Nature Communications.2021;[Epub] CrossRef - Non-polar lipid from greenshell mussel (Perna canaliculus) inhibits osteoclast differentiation
Parkpoom Siriarchavatana, Marlena C. Kruger, Matthew R. Miller, Hong Tian, Frances M. Wolber
Bone Reports.2021; 15: 101132. CrossRef - The Role of Osteokines in Sarcopenia: Therapeutic Directions and Application Prospects
Wenhao Lu, Wenfeng Xiao, Wenqing Xie, Xin Fu, Linyuan Pan, Hongfu Jin, Yongle Yu, Yi Zhang, Yusheng Li
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - IRF2 enhances RANKL-induced osteoclast differentiation via regulating NF-κB/NFATc1 signaling
Inyoung Kim, Jung Ha Kim, Kabsun Kim, Semun Seong, Keun-Bae Lee, Nacksung Kim
BMB Reports.2021; 54(9): 482. CrossRef - Nanovibrational stimulation inhibits osteoclastogenesis and enhances osteogenesis in co-cultures
John W. Kennedy, P. Monica Tsimbouri, Paul Campsie, Shatakshi Sood, Peter G. Childs, Stuart Reid, Peter S. Young, Dominic R. M. Meek, Carl S. Goodyear, Matthew J. Dalby
Scientific Reports.2021;[Epub] CrossRef - Propionibacterium freudenreichii Inhibits RANKL-Induced Osteoclast Differentiation and Ameliorates Rheumatoid Arthritis in Collagen-Induced Arthritis Mice
Jiah Yeom, Dong Joon Yim, Seongho Ma, Young-Hee Lim
Microorganisms.2021; 10(1): 48. CrossRef - Identification of Critical Functional Modules and Signaling Pathways in Osteoporosis
Xiaowei Jiang, Pu Ying, Yingchao Shen, Yiming Miu, Wenbin Kong, Tong Lu, Qiang Wang
Current Bioinformatics.2021; 16(1): 90. CrossRef - Osteogenic and Anti-Osteoclastogenic Properties of the Curcuminoid, CRE-Bin: Ex Vivo Experiments
Jakkapong Inchai, Amornkan Numit, Suticha Chunta, Piyawut Swangphon, Pharkphoom Panichayupakaranant, Yutthana Pengjam
SSRN Electronic Journal .2021;[Epub] CrossRef - Biological and structural effects after intraosseous infiltrations of age‐dependent platelet‐rich plasma: An in vivo study
Diego Delgado, Ane Garate, Pello Sánchez, Ane Miren Bilbao, Gontzal García del Caño, Joan Salles, Mikel Sánchez
Journal of Orthopaedic Research.2020; 38(9): 1931. CrossRef - Muscle weakness and selective muscle atrophy in osteoprotegerin-deficient mice
Dounia Hamoudi, Zineb Bouredji, Laetitia Marcadet, Hideo Yagita, Louis-Bénédict Landry, Anteneh Argaw, Jérôme Frenette
Human Molecular Genetics.2020; 29(3): 483. CrossRef - The Loss of Profilin 1 Causes Early Onset Paget's Disease of Bone
Federica Scotto di Carlo, Laura Pazzaglia, Teresa Esposito, Fernando Gianfrancesco
Journal of Bone and Mineral Research.2020; 35(8): 1387. CrossRef - Characterization of Dysregulated lncRNA-Associated ceRNA Network Reveals Novel lncRNAs With ceRNA Activity as Epigenetic Diagnostic Biomarkers for Osteoporosis Risk
Meijie Zhang, Luyang Cheng, Yina Zhang
Frontiers in Cell and Developmental Biology.2020;[Epub] CrossRef - Osteoimmunology: A Current Update of the Interplay Between Bone and the Immune System
Christian Guder, Sascha Gravius, Christof Burger, Dieter C. Wirtz, Frank A. Schildberg
Frontiers in Immunology.2020;[Epub] CrossRef - Multifactorial effects of hyperglycaemia, hyperinsulinemia and inflammation on bone remodelling in type 2 diabetes mellitus
V.A. Shahen, M. Gerbaix, S. Koeppenkastrop, S.F. Lim, K.E. McFarlane, Amanda N.L. Nguyen, X.Y. Peng, N.B. Weiss, T.C. Brennan-Speranza
Cytokine & Growth Factor Reviews.2020; 55: 109. CrossRef - The Role of Ca2+-NFATc1 Signaling and Its Modulation on Osteoclastogenesis
Jung Yun Kang, Namju Kang, Yu-Mi Yang, Jeong Hee Hong, Dong Min Shin
International Journal of Molecular Sciences.2020; 21(10): 3646. CrossRef - The Inhibition of Inflammatory Signaling Pathway by Secretory Leukocyte Protease Inhibitor can Improve Spinal Cord Injury
Renzhe Tang, Benson O. A. Botchway, Yanfeng Meng, Yong Zhang, Conghui Zhou, Junsong Jiang, Xuehong Liu
Cellular and Molecular Neurobiology.2020; 40(7): 1067. CrossRef - Osteoclast signaling-targeting miR-146a-3p and miR-155-5p are downregulated in Paget's disease of bone
Elizabeth Stephens, Michèle Roy, Martine Bisson, Hoang Dong Nguyen, Michelle S. Scott, Gilles Boire, Luigi Bouchard, Sophie Roux
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2020; 1866(10): 165852. CrossRef - Osteoimmunomodulatory effects of biomaterial modification strategies on macrophage polarization and bone regeneration
Yajuan Xie, Cheng Hu, Yi Feng, Danfeng Li, Tingting Ai, Yulei Huang, Xiaodan Chen, Lijia Huang, Jiali Tan
Regenerative Biomaterials.2020; 7(3): 233. CrossRef - A review of the latest insights into the mechanism of action of strontium in bone
Daniella Marx, Alireza Rahimnejad Yazdi, Marcello Papini, Mark Towler
Bone Reports.2020; 12: 100273. CrossRef - Regulatory network mediated by RBP‐J/NFATc1‐miR182 controls inflammatory bone resorption
Kazuki Inoue, Xiaoyu Hu, Baohong Zhao
The FASEB Journal.2020; 34(2): 2392. CrossRef - Cedrol attenuates collagen-induced arthritis in mice and modulates the inflammatory response in LPS-mediated fibroblast-like synoviocytes
Xue Chen, Jian Shen, Jun-ming Zhao, Jian Guan, Wei Li, Qiang-min Xie, Yu-qing Zhao
Food & Function.2020; 11(5): 4752. CrossRef - Tablysin-15 inhibits osteoclastogenesis and LPS-induced bone loss via attenuating the integrin αvβ3 pathway
Qingye Zeng, Wancheng Lu, Zhenhui Deng, Jiena Wu, Ruiyin Guo, Xueqing Xu
Chemico-Biological Interactions.2020; 327: 109179. CrossRef - The role of cytokines in bone remodeling and the pathogenesis of postmenopausal osteoporosis
G. A. Ignatenko, I. G. Nemsadze, E. D. Mirovich, A. V. Churilov, E. A. Maylyan, I. S. Glazkov, Z. S. Rumyantceva
Medical Herald of the South of Russia.2020; 11(2): 6. CrossRef - Effect of echinalkamide identified from Echinacea purpurea (L.) Moench on the inhibition of osteoclastogenesis and bone resorption
Bo Yoon Chang, Seul Ki Lee, Da Eun Kim, Jin Hye Bae, Thanh Tam Ho, So-Young Park, Mi Kyeong Lee, Sung Yeon Kim
Scientific Reports.2020;[Epub] CrossRef - A Synthetic Peptide, CK2.3, Inhibits RANKL-Induced Osteoclastogenesis through BMPRIa and ERK Signaling Pathway
John Nguyen, Semaj Kelly, Ryan Wood, Brian Heubel, Anja Nohe
Journal of Developmental Biology.2020; 8(3): 12. CrossRef - Betulinic Acid Protects From Bone Loss in Ovariectomized Mice and Suppresses RANKL-Associated Osteoclastogenesis by Inhibiting the MAPK and NFATc1 Pathways
Jiyong Wei, Yicheng Li, Qian Liu, Yanni Lan, Chengming Wei, Kun Tian, Liwei Wu, Chunbo Lin, Jiake Xu, Jinmin Zhao, Yuan Yang
Frontiers in Pharmacology.2020;[Epub] CrossRef - Polyphenols from grape pomace induce osteogenic differentiation in mesenchymal stem cells
Elisa Torre, Giorgio Iviglia, Clara Cassinelli, Marco Morra, Nazario Russo
International Journal of Molecular Medicine.2020;[Epub] CrossRef - Mathematical modeling of canonical and non-canonical NF-κB pathways in TNF stimulation
Bing Ji, Yao Zhang, Changqing Zhen, Michael J Fagan, Qing Yang
Computer Methods and Programs in Biomedicine.2020; 196: 105677. CrossRef - Collagen VIα2 chain deficiency causes trabecular bone loss by potentially promoting osteoclast differentiation through enhanced TNFα signaling
Hai T. Pham, Vardit Kram, Qurratul-Ain Dar, Taishi Komori, Youngmi Ji, Payam Mohassel, Jachinta Rooney, Li Li, Tina M. Kilts, Carsten Bonnemann, Shireen Lamande, Marian F. Young
Scientific Reports.2020;[Epub] CrossRef - Medicinal plants used against various inflammatory biomarkers for the management of rheumatoid arthritis
Shareen Singh, Thakur Gurjeet Singh, Kriti Mahajan, Sonia Dhiman
Journal of Pharmacy and Pharmacology.2020; 72(10): 1306. CrossRef - The regulatory role of the RANKL/RANK/OPG signaling pathway in the mechanisms of tooth eruption in patients with impacted teeth
Ludmila Brodetska, Larysa Natrus, Olha Lisakovska, Olexandr Kaniura, Liudmyla Iakovenko, Irina Skrypnyk, Petro Flis
BMC Oral Health.2020;[Epub] CrossRef - Activation of Nell-1 in BMSC Sheet Promotes Implant Osseointegration Through Regulating Runx2/Osterix Axis
Kaichen Lai, Yue Xi, Xue Du, Zhiwei Jiang, Yongzheng Li, Tingben Huang, Xiaoyan Miao, Huiming Wang, Ying Wang, Guoli Yang
Frontiers in Cell and Developmental Biology.2020;[Epub] CrossRef - Epigenetic Regulators Involved in Osteoclast Differentiation
Kristina Astleford, Emily Campbell, Andrew Norton, Kim C. Mansky
International Journal of Molecular Sciences.2020; 21(19): 7080. CrossRef - NIK inhibitor impairs chronic periodontitis via suppressing non-canonical NF-κB and osteoclastogenesis
Jiang Wang, Bo Wang, Xin Lv, Lei Wang
Pathogens and Disease.2020;[Epub] CrossRef - Cell-Type Targeted NF-kappaB Inhibition for the Treatment of Inflammatory Diseases
Bettina Sehnert, Harald Burkhardt, Stefan Dübel, Reinhard E. Voll
Cells.2020; 9(7): 1627. CrossRef - Intrinsic Restriction of TNF-Mediated Inflammatory Osteoclastogenesis and Bone Resorption
Baohong Zhao
Frontiers in Endocrinology.2020;[Epub] CrossRef - Grape Seed Proanthocyanidin Extract Prevents Bone Loss via Regulation of Osteoclast Differentiation, Apoptosis, and Proliferation
Sung Chul Kwak, Yoon-Hee Cheon, Chang Hoon Lee, Hong Young Jun, Kwon-Ha Yoon, Myeung Su Lee, Ju-Young Kim
Nutrients.2020; 12(10): 3164. CrossRef Relationship Between Metabolic Syndrome and Bone Health – An Evaluation of Epidemiological Studies and Mechanisms Involved
Kok-Yong Chin, Sok Kuan Wong, Sophia Ogechi Ekeuku, Kok-Lun Pang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 3667. CrossRef- The Beneficial Effect of Boswellic Acid on Bone Metabolism and Possible Mechanisms of Action in Experimental Osteoporosis
Bandar E. Al-Dhubiab, Snehal S. Patel, Mohamed A. Morsy, Harika Duvva, Anroop B. Nair, Pran Kishore Deb, Jigar Shah
Nutrients.2020; 12(10): 3186. CrossRef - Inhibition of Osteoclast Differentiation by Carotenoid Derivatives through Inhibition of the NF-κB Pathway
Shlomit Odes-Barth, Marina Khanin, Karin Linnewiel-Hermoni, Yifat Miller, Karina Abramov, Joseph Levy, Yoav Sharoni
Antioxidants.2020; 9(11): 1167. CrossRef - Myostatin Promotes Osteoclastogenesis by Regulating Ccdc50 Gene Expression and RANKL-Induced NF-κB and MAPK Pathways
Xin Zhi, Qian Chen, Shaojun Song, Zhengrong Gu, Wenqiang Wei, Huiwen Chen, Xiao Chen, Weizong Weng, Qirong Zhou, Jin Cui, Liehu Cao
Frontiers in Pharmacology.2020;[Epub] CrossRef - Noncanonical NF-κB Signaling Pathway in Liver Diseases
Qianhui Chen, Xinyu Lu, Xiaoyong Zhang
Journal of Clinical and Translational Hepatology.2020; 000(000): 1. CrossRef - Hdac3 regulates bone modeling by suppressing osteoclast responsiveness to RANKL
David H.H. Molstad, Anna M. Mattson, Dana L. Begun, Jennifer J. Westendorf, Elizabeth W. Bradley
Journal of Biological Chemistry.2020; 295(51): 17713. CrossRef - Insertion Mutation in Tnfrsf11a Causes a Paget's Disease–Like Phenotype in Heterozygous Mice and Osteopetrosis in Homozygous Mice
Nerea Alonso, Sachin Wani, Lorraine Rose, Rob J. van't Hof, Stuart H. Ralston, Omar M.E. Albagha
Journal of Bone and Mineral Research.2020; 36(7): 1376. CrossRef - Rictor Is a Novel Regulator of TRAF6/TRAF3 in Osteoclasts
Song Xu, Shihai Li, Xianming Liu, Kang Tan, Jiahuan Zhang, Kai Li, Xiaochun Bai, Yue Zhang
Journal of Bone and Mineral Research.2020; 36(10): 2053. CrossRef - KLF2 (kruppel-like factor 2 [lung]) regulates osteoclastogenesis by modulating autophagy
Dipranjan Laha, Moonmoon Deb, Hiranmoy Das
Autophagy.2019; 15(12): 2063. CrossRef - Dissecting the Role of NF-κb Protein Family and Its Regulators in Rheumatoid Arthritis Using Weighted Gene Co-Expression Network
Jamal S. M. Sabir, Abdelfatteh El Omri, Babajan Banaganapalli, Majed A. Al-Shaeri, Naser A. Alkenani, Mumdooh J. Sabir, Nahid H. Hajrah, Houda Zrelli, Lukasz Ciesla, Khalidah K. Nasser, Ramu Elango, Noor Ahmad Shaik, Muhummadh Khan
Frontiers in Genetics.2019;[Epub] CrossRef - Bench-to-bedside strategies for osteoporotic fracture: From osteoimmunology to mechanosensation
Yong Xie, Licheng Zhang, Qi Xiong, Yanpan Gao, Wei Ge, Peifu Tang
Bone Research.2019;[Epub] CrossRef - Platelet‐rich fibrin/biphasic calcium phosphate impairs osteoclast differentiation and promotes apoptosis by the intrinsic mitochondrial pathway in chronic periodontitis
Anil Kumar, Jaideep Mahendra, Shila Samuel, Jayamathi Govindraj, Tholcopiyan Loganathan, Yaongamphi Vashum, Little Mahendra, Thiagarajan Krishnamoorthy
Journal of Periodontology.2019; 90(1): 61. CrossRef - Cyclin‐dependent kinase 8/19 inhibition suppresses osteoclastogenesis by downregulating RANK and promotes osteoblast mineralization and cancellous bone healing
Mehdi Amirhosseini, Magnus Bernhardsson, Pernilla Lång, Göran Andersson, Johan Flygare, Anna Fahlgren
Journal of Cellular Physiology.2019; 234(9): 16503. CrossRef - Short-term pharmacologic RAGE inhibition differentially affects bone and skeletal muscle in middle-aged mice
Hannah M. Davis, Alyson L. Essex, Sinai Valdez, Padmini J. Deosthale, Mohammad W. Aref, Matthew R. Allen, Andrea Bonetto, Lilian I. Plotkin
Bone.2019; 124: 89. CrossRef - Association of SNP-SNP Interactions Between RANKL, OPG, CHI3L1, and VDR Genes With Breast Cancer Risk in Egyptian Women
Olfat G. Shaker, Mahmoud A. Senousy
Clinical Breast Cancer.2019; 19(1): e220. CrossRef - Sialoglycoproteins Isolated from the Eggs of Gadus morhua Inhibit Bone Resorption in Ovariectomized Rats by Suppressing the MAPK and NF-κB Pathways
Lei Mao, Yiming Wang, Meiling Wang, Yufeng Dai, Jingfeng Wang, Changhu Xue
Journal of Ocean University of China.2019; 18(5): 1174. CrossRef - Mathematical modelling of bone remodelling cycles including the NFκB signalling pathway
Bing Ji, Yao Zhang, Changqing Zhen, Michael J. Fagan, Qing Yang
Computers in Biology and Medicine.2019; 107: 257. CrossRef - Astilbin prevents bone loss in ovariectomized mice through the inhibition of RANKL‐induced osteoclastogenesis
Haiming Jin, Qingqing Wang, Kai Chen, Ke Xu, Hao Pan, Feifan Chu, Zhen Ye, Ziyi Wang, Jennifer Tickner, Heng Qiu, Chao Wang, Jacob Kenny, Huazi Xu, Te Wang, Jiake Xu
Journal of Cellular and Molecular Medicine.2019; 23(12): 8355. CrossRef - Regulation of Osteoclast Differentiation and Skeletal Maintenance by Histone Deacetylases
Bora Faulkner, Kristina Astleford, Kim Mansky
Molecules.2019; 24(7): 1355. CrossRef - Benzylideneacetone Derivatives Inhibit Osteoclastogenesis and Activate Osteoblastogenesis Independently Based on Specific Structure–Activity Relationship
Triveni Pativada, Myung Hwan Kim, Jung-Hun Lee, Seong Su Hong, Chun Whan Choi, Yun-Hyeok Choi, Woo Jung Kim, Da-Woon Song, Serk In Park, Eun Jung Lee, Bo-Yeon Seo, Hankyeom Kim, Hong Kyu Kim, Kee Ho Lee, Sung K. Ahn, Jin-Mo Ku, Gil Hong Park
Journal of Medicinal Chemistry.2019; 62(13): 6063. CrossRef - The Coumarin Derivative 5′-Hydroxy Auraptene Suppresses Osteoclast Differentiation via Inhibiting MAPK and c-Fos/NFATc1 Pathways
Basem M. Abdallah, Enas M. Ali, Hany Elsawy, Gehan M. Badr, Ashraf M. Abdel-Moneim, Abdullah M. Alzahrani
BioMed Research International.2019; 2019: 1. CrossRef - Characterizing how probiotic Lactobacillus reuteri 6475 and lactobacillic acid mediate suppression of osteoclast differentiation
Darin Quach, Narayanan Parameswaran, Laura McCabe, Robert A. Britton
Bone Reports.2019; 11: 100227. CrossRef - RIPK1 inhibition attenuates experimental autoimmune arthritis via suppression of osteoclastogenesis
Jooyeon Jhun, Seung Hoon Lee, Se-Young Kim, Jaeyoon Ryu, Ji Ye Kwon, Hyun Sik Na, KyoungAh Jung, Su-Jin Moon, Mi-La Cho, Jun-Ki Min
Journal of Translational Medicine.2019;[Epub] CrossRef - The IRF2BP2-KLF2 axis regulates osteoclast and osteoblast differentiation
Inyoung Kim, Jung Ha Kim, Kabsun Kim, Semun Seong, Nacksung Kim
BMB Reports.2019; 52(7): 469. CrossRef - Aminothiazoles inhibit osteoclastogenesis and PGE2 production in LPS‐stimulated co‐cultures of periodontal ligament and RAW 264.7 cells, and RANKL‐mediated osteoclastogenesis and bone resorption in PBMCs
Anna Kats, Natalija Gerasimcik, Tuomas Näreoja, Jonas Nederberg, Simon Grenlöv, Ekaterina Lagnöhed, Suchita Desai, Göran Andersson, Tülay Yucel‐Lindberg
Journal of Cellular and Molecular Medicine.2019; 23(2): 1152. CrossRef - Regulator of G protein signaling 12 enhances osteoclastogenesis by suppressing Nrf2-dependent antioxidant proteins to promote the generation of reactive oxygen species
Andrew Ying Hui Ng, Ziqing Li, Megan M Jones, Shuting Yang, Chunyi Li, Chuanyun Fu, Chengjian Tu, Merry Jo Oursler, Jun Qu, Shuying Yang
eLife.2019;[Epub] CrossRef - Molecular mechanisms linking peri-implantitis and type 2 diabetes mellitus revealed by transcriptomic analysis
Tianliang Yu, Aneesha Acharya, Nikos Mattheos, Simin Li, Dirk Ziebolz, Gerhard Schmalz, Rainer Haak, Jana Schmidt, Yu Sun
PeerJ.2019; 7: e7124. CrossRef - Madecassoside inhibits estrogen deficiency‐induced osteoporosis by suppressing RANKL‐induced osteoclastogenesis
Qingqing Wang, Lingya Yao, Ke Xu, Haiming Jin, Kai Chen, Ziyi Wang, Qian Liu, Zhen Cao, Jacob kenny, Yuhao Liu, Jennifer Tickner, Huazi Xu, Jiake Xu
Journal of Cellular and Molecular Medicine.2019; 23(1): 380. CrossRef - Pharmacological Inhibition of NFκB Reduces Prostate Cancer Related Osteoclastogenesis In Vitro and Osteolysis Ex Vivo
Silvia Marino, Ryan T. Bishop, Giovana Carrasco, John G. Logan, Boya Li, Aymen I. Idris
Calcified Tissue International.2019; 105(2): 193. CrossRef - TGFβ-induced degradation of TRAF3 in mesenchymal progenitor cells causes age-related osteoporosis
Jinbo Li, Akram Ayoub, Yan Xiu, Xiaoxiang Yin, James O. Sanders, Addisu Mesfin, Lianping Xing, Zhenqiang Yao, Brendan F. Boyce
Nature Communications.2019;[Epub] CrossRef - A simple and robust reporter gene assay for measuring the bioactivity of anti-RANKL therapeutic antibodies
Chuanfei Yu, Lan Wang, Yongbo Ni, Junzhi Wang
RSC Advances.2019; 9(69): 40196. CrossRef - Tatarinan T, an α‐asarone‐derived lignin, attenuates osteoclastogenesis induced by RANKL via the inhibition of NFATc1/c‐Fos expression
Yuxin Zhang, Zhi Wang, Xiaona Xie, Shaoming Wang, Yingjian Wang, Guihua Quan, Hongbing Wang, Wan‐chun Sun
Cell Biology International.2019; 43(12): 1471. CrossRef - The Effect of Curcumin on the Differentiation of Mesenchymal Stem Cells into Mesodermal Lineage
Armita Mahdavi Gorabi, Nasim Kiaie, Saeideh Hajighasemi, Tannaz Jamialahmadi, Muhammed Majeed, Amirhossein Sahebkar
Molecules.2019; 24(22): 4029. CrossRef - Reactive Oxygen Species in Osteoclast Differentiation and Possible Pharmaceutical Targets of ROS-Mediated Osteoclast Diseases
Taiwo Samuel Agidigbi, Chaekyun Kim
International Journal of Molecular Sciences.2019; 20(14): 3576. CrossRef - Identification of anti-inflammatory components in Sinomenii Caulis based on spectrum-effect relationship and chemometric methods
Lan-Jin Wang, Zheng-Meng Jiang, Ping-Ting Xiao, Jian-Bo Sun, Zhi-Ming Bi, E-Hu Liu
Journal of Pharmaceutical and Biomedical Analysis.2019; 167: 38. CrossRef - I-BET151 suppresses osteoclast formation and inflammatory cytokines secretion by targetting BRD4 in multiple myeloma
Ning-Hong Guo, Ji-Fu Zheng, Fu-Ming Zi, Jing Cheng
Bioscience Reports.2019;[Epub] CrossRef - The polyadenylation inhibitor cordycepin reduces pain, inflammation and joint pathology in rodent models of osteoarthritis
Sadaf Ashraf, Masar Radhi, Peter Gowler, James J. Burston, Raj D. Gandhi, Graeme J. Thorn, Anna M. Piccinini, David A. Walsh, Victoria Chapman, Cornelia H. de Moor
Scientific Reports.2019;[Epub] CrossRef - An anti-RANKL treatment reduces muscle inflammation and dysfunction and strengthens bone in dystrophic mice
Dounia Hamoudi, Laetitia Marcadet, Antoine Piette Boulanger, Hideo Yagita, Zineb Bouredji, Anteneh Argaw, Jérôme Frenette
Human Molecular Genetics.2019; 28(18): 3101. CrossRef - Dual-Purpose Magnesium-Incorporated Titanium Nanotubes for Combating Bacterial Infection and Ameliorating Osteolysis to Realize Better Osseointegration
Ying Yang, Lihong Liu, Hang Luo, Dou Zhang, Shaorong Lei, Kechao Zhou
ACS Biomaterials Science & Engineering.2019; 5(10): 5368. CrossRef - Inhibition of Osteoclastogenesis by Thioredoxin-Interacting Protein-Derived Peptide (TN13)
Mi Kim, Won Kim, Jae-Eun Byun, Jung Choi, Suk Yoon, Inpyo Choi, Haiyoung Jung
Journal of Clinical Medicine.2019; 8(4): 431. CrossRef - Formononetin Regulates Multiple Oncogenic Signaling Cascades and Enhances Sensitivity to Bortezomib in a Multiple Myeloma Mouse Model
Chulwon Kim, Jong Hyun Lee, Jeong-Hyeon Ko, Arunachalam Chinnathambi, Sulaiman Ali Alharbi, Omar H.M. Shair, Gautam Sethi, Kwang Seok Ahn
Biomolecules.2019; 9(7): 262. CrossRef - Longan fruit increase bone mineral density in zebrafish and ovariectomized rat by suppressing RANKL-induced osteoclast differentiation
Younglim Son, Eun Mi Lee, Do Yup Lee, Jong Hun Lee, Sangtaek Oh
Phytomedicine.2019; 59: 152910. CrossRef - From Osteoclast Differentiation to Osteonecrosis of the Jaw: Molecular and Clinical Insights
Anesi, Generali, Sandoni, Pozzi, Grande
International Journal of Molecular Sciences.2019; 20(19): 4925. CrossRef -
Tetrandrine attenuates the bone erosion in collagen‐induced arthritis rats by inhibiting osteoclastogenesis
via
spleen tyrosine kinase
Yugai Jia, Yumeng Miao, Mengfan Yue, Mei Shu, Zhifeng Wei, Yue Dai
The FASEB Journal.2018; 32(6): 3398. CrossRef - Bone turnover markers and novel biomarkers in lung cancer bone metastases
Jiangli Lang, Qian Zhao, Yuedong He, Xijie Yu
Biomarkers.2018; 23(6): 518. CrossRef - Flavopiridol Protects Bone Tissue by Attenuating RANKL Induced Osteoclast Formation
Zi’ang Hu, Yilei Chen, Lijiang Song, Jasper H. N. Yik, Dominik R. Haudenschild, Shunwu Fan
Frontiers in Pharmacology.2018;[Epub] CrossRef - PRMT1 mediates RANKL-induced osteoclastogenesis and contributes to bone loss in ovariectomized mice
Joo-Hee Choi, Ah-Ra Jang, Dong-il Kim, Min-Jung Park, Seul-Ki Lim, Myung-Sun Kim, Jong-Hwan Park
Experimental & Molecular Medicine.2018; 50(8): 1. CrossRef - Lumichrome inhibits osteoclastogenesis and bone resorption through suppressing RANKL‐induced NFAT activation and calcium signaling
Chuan Liu, Zhen Cao, Wen Zhang, Jennifer Tickner, Heng Qiu, Chao Wang, Kai Chen, Ziyi Wang, Renxiang Tan, Shiwu Dong, Jiake Xu
Journal of Cellular Physiology.2018; 233(11): 8971. CrossRef - Shared epitope–aryl hydrocarbon receptor crosstalk underlies the mechanism of gene–environment interaction in autoimmune arthritis
Jiaqi Fu, Sarah V. Nogueira, Vincent van Drongelen, Patrick Coit, Song Ling, Edward F. Rosloniec, Amr H. Sawalha, Joseph Holoshitz
Proceedings of the National Academy of Sciences.2018; 115(18): 4755. CrossRef - LRP1 Suppresses Bone Resorption in Mice by Inhibiting the RANKL-Stimulated NF-κB and p38 Pathways During Osteoclastogenesis
Di Lu, Jianshuang Li, Huadie Liu, Gabrielle E Foxa, Kevin Weaver, Jie Li, Bart O Williams, Tao Yang
Journal of Bone and Mineral Research.2018; 33(10): 1773. CrossRef - Effects of Vitamin D on Skeletal Muscle and Athletic Performance
Geoffrey D. Abrams, David Feldman, Marc R. Safran
Journal of the American Academy of Orthopaedic Surgeons.2018; 26(8): 278. CrossRef - TRIM38 regulates NF-κB activation through TAB2 degradation in osteoclast and osteoblast differentiation
Kabsun Kim, Jung Ha Kim, Inyoung Kim, Semun Seong, Nacksung Kim
Bone.2018; 113: 17. CrossRef - Isosteviol Derivative Inhibits Osteoclast Differentiation and Ameliorates Ovariectomy-Induced Osteoporosis
Huey-En Tzeng, Po-Hao Huang, Chun-Hao Tsai, Gregory J Tsay, Yi-Ju Lee, Tsurng-Juhn Huang, Tzu-Hung Lin, Ying-Ming Chiu, Yi-Ying Wu
Scientific Reports.2018;[Epub] CrossRef - 3′‐Sialyllactose as an inhibitor of p65 phosphorylation ameliorates the progression of experimental rheumatoid arthritis
Li‐Jung Kang, Eun‐Soo Kwon, Kwang Min Lee, Chanmi Cho, Jae‐In Lee, Young Bae Ryu, Tae Hyun Youm, Jimin Jeon, Mi Ra Cho, Seon‐Yong Jeong, Sang‐Rae Lee, Wook Kim, Siyoung Yang
British Journal of Pharmacology.2018; 175(23): 4295. CrossRef - Mepazine Inhibits RANK-Induced Osteoclastogenesis Independent of Its MALT1 Inhibitory Function
Laura Meloni, Lynn Verstrepen, Marja Kreike, Jens Staal, Yasmine Driege, Inna Afonina, Rudi Beyaert
Molecules.2018; 23(12): 3144. CrossRef - Activated protein C suppresses osteoclast differentiation via endothelial protein C receptor, protease-activated receptor-1, sphingosine 1-phosphate receptor, and apolipoprotein E receptor 2
Kakunoshin Yoshida, Nobuyuki Akita, Takayuki Okamoto, Kunihiro Asanuma, Atsumasa Uchida, Akihiro Sudo, Motomu Shimaoka, Koji Suzuki, Tatsuya Hayashi
Thrombosis Research.2018; 163: 30. CrossRef - Dietary nutraceuticals as backbone for bone health
Manoj K. Pandey, Subash C. Gupta, Deepkamal Karelia, Patrick J. Gilhooley, Mehdi Shakibaei, Bharat B. Aggarwal
Biotechnology Advances.2018; 36(6): 1633. CrossRef - Irisin promotes proliferation but inhibits differentiation in osteoclast precursor cells
Yaxian Ma, Xiaoyong Qiao, Rujun Zeng, Ran Cheng, Jun Zhang, Yunyao Luo, Ying Nie, Ying Hu, Zhilan Yang, Jing Zhang, Lin Liu, Wenming Xu, Charles C. Xu, Liangzhi Xu
The FASEB Journal.2018; 32(11): 5813. CrossRef - Inhibitory-κB Kinase (IKK) α and Nuclear Factor-κB (NFκB)-Inducing Kinase (NIK) as Anti-Cancer Drug Targets
Andrew Paul, Joanne Edwards, Christopher Pepper, Simon Mackay
Cells.2018; 7(10): 176. CrossRef - Rooibos tea extracts inhibit osteoclast formation and activity through the attenuation of NF-κB activity in RAW264.7 murine macrophages
Shaakirah Moosa, Abe E. Kasonga, Vishwa Deepak, Sumari Marais, Innocentia B. Magoshi, Megan J. Bester, Marlena C. Kruger, Magdalena Coetzee
Food & Function.2018; 9(6): 3301. CrossRef - Ferulic acid, a dietary polyphenol suppresses osteoclast differentiation and bone erosion via the inhibition of RANKL dependent NF-κB signalling pathway
Hari Madhuri Doss, Snigdha Samarpita, Ramamoorthi Ganesan, Mahaboobkhan Rasool
Life Sciences.2018; 207: 284. CrossRef - Gentiopicroside inhibits RANKL-induced osteoclastogenesis by regulating NF-κB and JNK signaling pathways
Fangqing Chen, Lin Xie, Ran Kang, Rongrong Deng, Zhipeng Xi, Daoxi Sun, Jin Zhu, Liming Wang
Biomedicine & Pharmacotherapy.2018; 100: 142. CrossRef - Hesperetin Prevents Bone Resorption by Inhibiting RANKL-Induced Osteoclastogenesis and Jnk Mediated Irf-3/c-Jun Activation
Qiang Zhang, Xinqiao Tang, Zhong Liu, Xiaoxia Song, Dan Peng, Wei Zhu, Zhengxiao Ouyang, Wanchun Wang
Frontiers in Pharmacology.2018;[Epub] CrossRef - Anemarrhena�asphodeloides Bunge ameliorates osteoporosis by suppressing osteoclastogenesis
Jae Lee, Mi Kim, Haesu Lee, Woong Yang
International Journal of Molecular Medicine.2018;[Epub] CrossRef - RANKL cytokine enhances TNF-induced osteoclastogenesis independently of TNF receptor associated factor (TRAF) 6 by degrading TRAF3 in osteoclast precursors
Zhenqiang Yao, Wei Lei, Rong Duan, Yanyun Li, Lu Luo, Brendan F. Boyce
Journal of Biological Chemistry.2017; 292(24): 10169. CrossRef - The Alpha 7 Nicotinic Acetylcholine Receptor of Deciduous Dental Pulp Stem Cells Regulates Osteoclastogenesis During Physiological Root Resorption
Lulu Wang, Zhifei Zhou, Yujiang Chen, Shuai Yuan, Yang Du, Xinke Ju, Lizheng Wu, Xiaojing Wang
Stem Cells and Development.2017; 26(16): 1186. CrossRef - Unexpected Bone Formation Produced by RANKL Blockade
Sergio Portal-Núñez, Aranzazu Mediero, Pedro Esbrit, Olga Sánchez-Pernaute, Raquel Largo, Gabriel Herrero-Beaumont
Trends in Endocrinology & Metabolism.2017; 28(10): 695. CrossRef - Def6 Restrains Osteoclastogenesis and Inflammatory Bone Resorption
Nikolaus Binder, Christine Miller, Masaki Yoshida, Kazuki Inoue, Shinichi Nakano, Xiaoyu Hu, Lionel B. Ivashkiv, Georg Schett, Alessandra Pernis, Steven R. Goldring, F. Patrick Ross, Baohong Zhao
The Journal of Immunology.2017; 198(9): 3436. CrossRef - Suppression of Osteoclastogenesis by Melatonin: A Melatonin Receptor-Independent Action
Hyung Kim, Ha Kim, Moon-Kyoung Bae, Yong-Deok Kim
International Journal of Molecular Sciences.2017; 18(6): 1142. CrossRef - The effects of downhill and uphill exercise training on osteogenesis-related factors in ovariectomy-induced bone loss
Yun-Seok Kang, Chun-Ho Kim, Jeong-Seok Kim
Journal of Exercise Nutrition & Biochemistry.2017; 21(3): 1. CrossRef - Small leucine rich proteoglycans, a novel link to osteoclastogenesis
Vardit Kram, Tina M. Kilts, Nisan Bhattacharyya, Li Li, Marian F. Young
Scientific Reports.2017;[Epub] CrossRef - Dihydromyricetin Protects against Bone Loss in Ovariectomized Mice by Suppressing Osteoclast Activity
Libo Zhao, Cong Cai, Jing Wang, Liming Zhao, Weijin Li, Changyu Liu, Hanfeng Guan, Yuanli Zhu, Jun Xiao
Frontiers in Pharmacology.2017;[Epub] CrossRef - MicroRNAs and Periodontal Homeostasis
X. Luan, X. Zhou, J. Trombetta-eSilva, M. Francis, A.K. Gaharwar, P. Atsawasuwan, T.G.H. Diekwisch
Journal of Dental Research.2017; 96(5): 491. CrossRef - Hypoxia‐inducible factor 1‐alpha does not regulate osteoclastogenesis but enhances bone resorption activity via prolyl‐4‐hydroxylase 2
Philippa A Hulley, Tammie Bishop, Aude Vernet, Jurgen E Schneider, James R Edwards, Nick A Athanasou, Helen J Knowles
The Journal of Pathology.2017; 242(3): 322. CrossRef - mTORC1 Inhibits NF-κB/NFATc1 Signaling and Prevents Osteoclast Precursor Differentiation, In Vitro and In Mice
Yue Zhang, Song Xu, Kai Li, Kang Tan, Kangyan Liang, Jian Wang, Junhui Shen, Wenchong Zou, Le Hu, Daozhang Cai, Changhai Ding, Mangmang Li, Guozhi Xiao, Bin Liu, Anling Liu, Xiaochun Bai
Journal of Bone and Mineral Research.2017; 32(9): 1829. CrossRef - Hepatocyte growth factor and alternative splice variants - expression, regulation and implications in osteogenesis and bone health and repair
Rachel N. Frisch, Kevin M. Curtis, Kristina K. Aenlle, Guy A. Howard
Expert Opinion on Therapeutic Targets.2016; 20(9): 1087. CrossRef - CCAAT/Enhancer-binding Protein α (C/EBPα) Is Important for Osteoclast Differentiation and Activity
Joel Jules, Wei Chen, Xu Feng, Yi-Ping Li
Journal of Biological Chemistry.2016; 291(31): 16390. CrossRef - Ginsenoside Re Inhibits Osteoclast Differentiation in Mouse Bone Marrow-Derived Macrophages and Zebrafish Scale Model
Chan-Mi Park, Hye-Min Kim, Dong Hyun Kim, Ho-Jin Han, Haneul Noh, Jae-Hyuk Jang, Soo-Hyun Park, Han-Jung Chae, Soo-Wan Chae, Eun Kyoung Ryu, Sangku Lee, Kangdong Liu, Haidan Liu, Jong-Seog Ahn, Young Ock Kim, Bo-Yeon Kim, Nak-Kyun Soung
Molecules and Cells.2016; 39(12): 855. CrossRef - RBP-J–Regulated miR-182 Promotes TNF-α–Induced Osteoclastogenesis
Christine H. Miller, Sinead M. Smith, Mahmoud Elguindy, Tuo Zhang, Jenny Z. Xiang, Xiaoyu Hu, Lionel B. Ivashkiv, Baohong Zhao
The Journal of Immunology.2016; 196(12): 4977. CrossRef - Mitochondria related peptide MOTS-c suppresses ovariectomy-induced bone loss via AMPK activation
Wei Ming, Gan Lu, Sha Xin, Lu Huanyu, Jiang Yinghao, Lei Xiaoying, Xu Chengming, Ruan Banjun, Wang Li, Lu Zifan
Biochemical and Biophysical Research Communications.2016; 476(4): 412. CrossRef - Vitamin D Level Between Calcium-Phosphorus Homeostasis and Immune System: New Perspective in Osteoporosis
Daniele Bellavia, Viviana Costa, Angela De Luca, Melania Maglio, Stefania Pagani, Milena Fini, Gianluca Giavaresi
Current Osteoporosis Reports.2016;[Epub] CrossRef - Diarylheptanoid from Curcuma comosa Roxb. suppresses RANKL-induced osteoclast differentiation by decreasing NFATc1 and c-Fos expression via MAPK pathway
Supatta Chawalitpong, Nilubon Sornkaew, Apichart Suksamrarn, Tanapat Palaga
European Journal of Pharmacology.2016; 788: 351. CrossRef - NF‐κB acts as a multifunctional modulator in bone invasion by oral squamous cell carcinoma
Eijiro Jimi, Shoichiro Kokabu, Takuma Matsubara, Chihiro Nakatomi, Kou Matsuo, Seiji Watanabe
Oral Science International.2016; 13(1): 1. CrossRef - DLX3 negatively regulates osteoclastic differentiation through microRNA-124
Na Zhao, Dong Han, Yang Liu, Yue Li, Li Zeng, Yixiang Wang, Hailan Feng
Experimental Cell Research.2016; 341(2): 166. CrossRef - Functional osteoclastogenesis: the baseline variability in blood donor precursors is not associated with age and gender
Eliana Pivetta, Bruna Wassermann, Pietro Bulian, Agostino Steffan, Alfonso Colombatti, Jerry Polesel, Paola Spessotto
Oncotarget.2015; 6(31): 31889. CrossRef - The Multiple Roles of Microrna-223 in Regulating Bone Metabolism
Yong Xie, Lihai Zhang, Yanpan Gao, Wei Ge, Peifu Tang
Molecules.2015; 20(10): 19433. CrossRef - Andrographolide Inhibits Ovariectomy-Induced Bone Loss via the Suppression of RANKL Signaling Pathways
Tao Wang, Qian Liu, Lin Zhou, Jin Yuan, Xixi Lin, Rong Zeng, Xiaonan Liang, Jinmin Zhao, Jiake Xu
International Journal of Molecular Sciences.2015; 16(11): 27470. CrossRef - Molecular and epigenetic basis of macrophage polarized activation
Chiara Porta, Elena Riboldi, Alessandro Ippolito, Antonio Sica
Seminars in Immunology.2015; 27(4): 237. CrossRef
- Photo biomodulation of dental derived stem cells to ameliorate regenerative capacity: In vitro study

- Regulation of Osteoclast Differentiation: Identification of osteoclast and macrophage fusion protein; DC-STAMP.
- Takeshi Miyamoto
- J Korean Endocr Soc. 2006;21(5):347-351. Published online October 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.5.347
- 1,462 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Osteoclasts are bone-resorbing multinuclear cells derived from hematopoietic stem cells or monocyte/ macrophage lineage cells. Recent identification of RANK/RANKL has provided new insights into the osteoclast differentiation pathway, enabling us to generate osteoclasts without stromal cells, which support osteoclastogenesis. In order to establish a pure osteoclast culture system, we identified the osteoclast precursor cell (c-Kit(+)c-Fms(+)RANK(-) cell), which is a common precursor cell of osteoclasts, macrophages and dendritic cells. Macrophages are induced by M-CSF alone, while a sequential stimulation of M-CSF followed by RANKL effectively induces osteoclast formation. Furthermore, dendritic cells are induced by GM-CSF or GM-CSF plus RANKL. Therefore, we were able to generate pure osteoclasts, macrophages or dendritic cells from the common precursor cell using specific combinations of cytokines. Using this culture system, we found that an adherent condition is critical for osteoclast differentiation. We also found that the osteoclastogenesis induced by M-CSF plus RANKL is completely inhibited by GM-CSF, and that these cells differentiate into a dendritic cell lineage. The osteoclast multinucleation is believed to be induced by cell-cell fusion of mononuclear osteoclasts. Although various molecules have been implicated in the cell-cell fusion of osteoclasts or macrophages, the essential molecule for cell fusion has not been identified. We identified that the dendritic cell-specific transmembrane protein (DC-STAMP) was an essential cell-cell fusion molecule for osteoclasts and foreign body giant cells, and that DC-STAMP deficient mice have no multinuclear osteoclasts. Here I review the osteoclast development from immature precursor cells to multinuclear osteoclasts.
-
Citations
Citations to this article as recorded by- Exosomal tumor necrosis factor‐α from hepatocellular cancer cells (Huh‐7) promote osteoclast differentiation
Ching‐Hao Li, Kalaiselvi Palanisamy, Xin Li, Shao‐Hua Yu, I‐Kuan Wang, Chi‐Yuan Li, Kuo‐Ting Sun
Journal of Cellular Biochemistry.2021; 122(11): 1749. CrossRef
- Exosomal tumor necrosis factor‐α from hepatocellular cancer cells (Huh‐7) promote osteoclast differentiation


 KES
KES

 First
First Prev
Prev



