Search
- Page Path
- HOME > Search
- Adrenal Gland
- Aldosterone Immunoassay-Specific Cutoff Value for Seated Saline Suppression Test for Diagnosing Primary Aldosteronism
- So Yoon Kwon, Jiyun Park, So Hee Park, So Hyun Cho, You-Bin Lee, Soo-Youn Lee, Jae Hyeon Kim
- Endocrinol Metab. 2022;37(6):938-942. Published online December 6, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1535
- 1,757 View
- 193 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
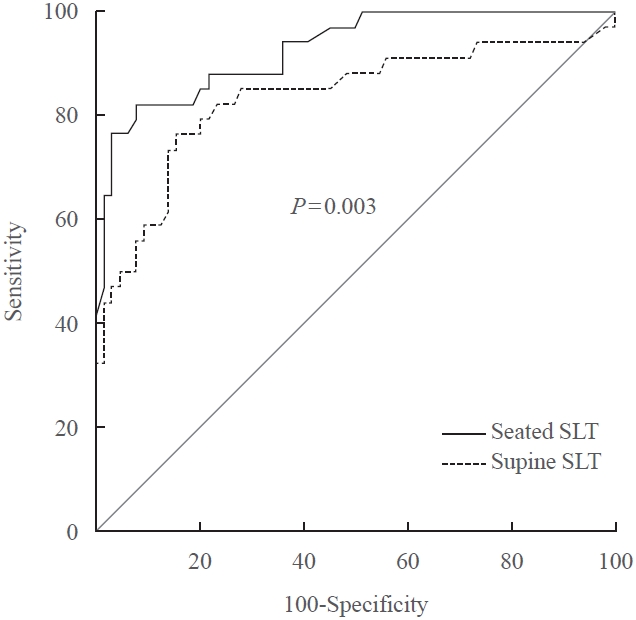
ePub - A seated saline loading test (SLT) using liquid chromatography-tandem mass spectrometry (LC-MS/MS) is one of the most accepted confirmatory tests of primary aldosteronism. However, LC-MS/MS is time-consuming and is not widely available in diagnostic laboratories compared to immunoassay. With immunoassay, it is unknown whether SLT in the seated position is more accurate than that of the supine position, and a cutoff value of post-seated SLT plasma aldosterone concentration (PAC) must be established in the Korean population. Ninety-eight patients underwent SLT in both positions, and post-SLT PAC was measured by LC-MS/MS and radioimmunoassay. We confirmed primary aldosteronism if post-seated SLT PAC by LC-MS/MS exceeded 5.8 ng/dL. The area under the receiver operating characteristic curve was greater for seated than supine SLT (0.928 vs. 0.834, P=0.003). The optimal cutoff value of post-seated SLT by radioimmunoassay was 6.6 ng/dL (sensitivity 83.3%, specificity 92.2%).
-
Citations
Citations to this article as recorded by- Investigating the cut-off values of captopril challenge test for primary aldosteronism using the novel chemiluminescent enzyme immunoassay method: a retrospective cohort study
Yuta Tezuka, Kei Omata, Yoshikiyo Ono, Kengo Kambara, Hiroki Kamada, Sota Oguro, Yuto Yamazaki, Celso E. Gomez-Sanchez, Akihiro Ito, Hironobu Sasano, Kei Takase, Tetsuhiro Tanaka, Hideki Katagiri, Fumitoshi Satoh
Hypertension Research.2024;[Epub] CrossRef
- Investigating the cut-off values of captopril challenge test for primary aldosteronism using the novel chemiluminescent enzyme immunoassay method: a retrospective cohort study

- Adrenal Gland
- Clinical and Technical Aspects in Free Cortisol Measurement
- Man Ho Choi
- Endocrinol Metab. 2022;37(4):599-607. Published online August 19, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1549
- 4,661 View
- 288 Download
- 9 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
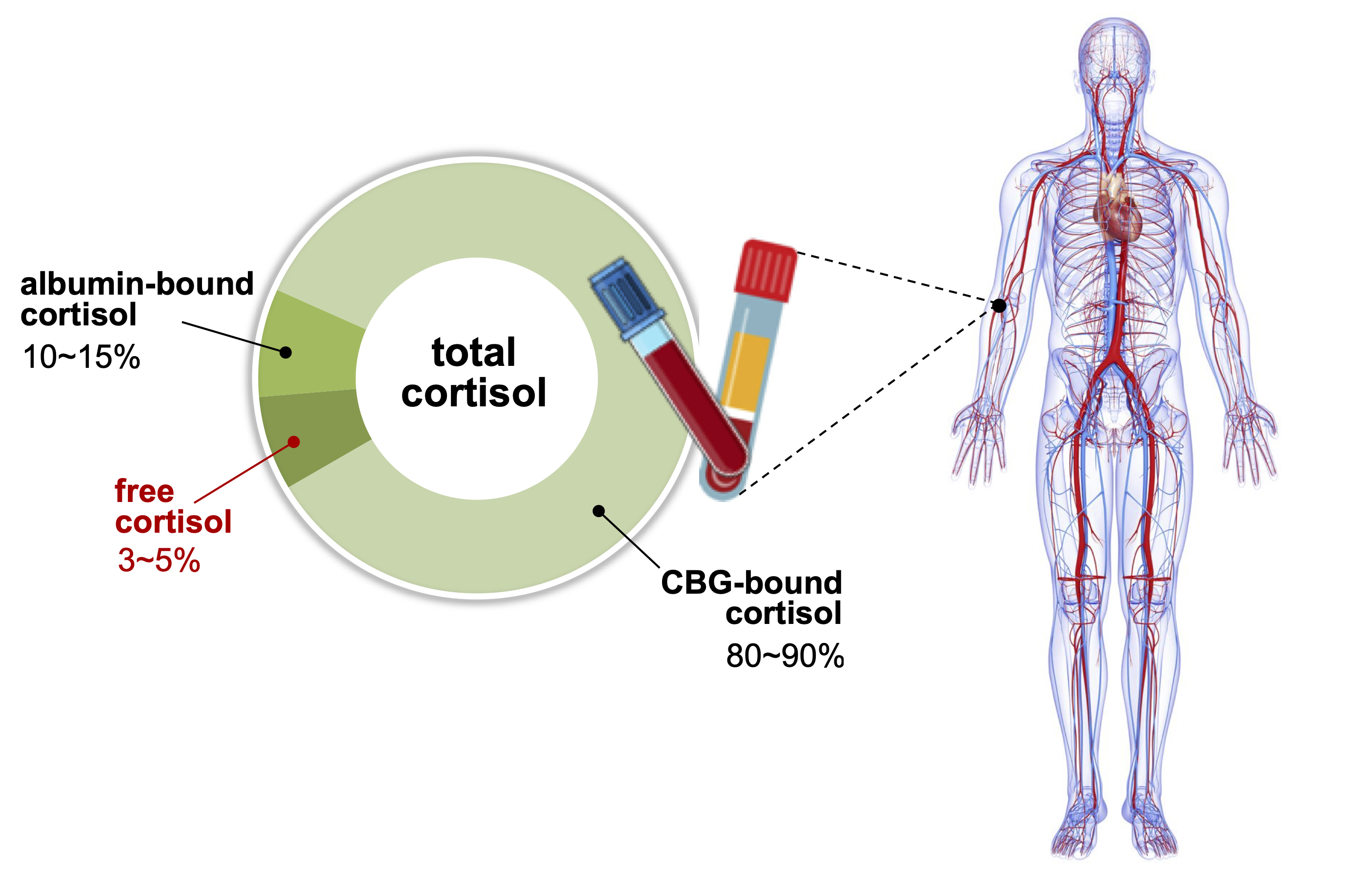
ePub - Accurate measurement of cortisol is critical in adrenal insufficiency as it reduces the risk associated with misdiagnosis and supports the optimization of stress dose. Comprehensive assays have been developed to determine the levels of bioactive free cortisol and their clinical and analytical efficacies have been extensively discussed because the level of total cortisol is affected by changes in the structure or circulating levels of corticoid-binding globulin and albumin, which are the main reservoirs of cortisol in the human body. Antibody-based immunoassays are routinely used in clinical laboratories; however, the lack of molecular specificity in cortisol assessment limits their applicability to characterize adrenocortical function. Improved specificity and sensitivity can be achieved by mass spectrometry coupled with chromatographic separation methods, which is a cutting-edge technology to measure individual as well as a panel of steroids in a single analytical run. The purpose of this review is to introduce recent advances in free cortisol measurement from the perspectives of clinical specimens and issues associated with prospective analytical technologies.
-
Citations
Citations to this article as recorded by- Highly Responsive Bioassay for Quantification of Glucocorticoids
Mathias Flensted Poulsen, Martin Overgaard, Christian Brix Folsted Andersen, Andreas Lodberg
Analytical Chemistry.2024; 96(5): 2000. CrossRef - An LC-MS/MS Method for the Simultaneous Quantification of Insulin, Cortisol, Glucagon-like Peptide 1, Ghrelin, and Osteocalcin
Zhichao Zhang, Hareem Siddiqi, Yu-Ping Huang, Shannon McClorry, Peng Ji, Daniela Barile, Carolyn M. Slupsky
Separations.2024; 11(2): 41. CrossRef - Determination of cortisol cut-off limits and steroid dynamics in the ACTH stimulation test: a comparative analysis using Roche Elecsys Cortisol II immunoassay and LC-MS/MS
Sema Okutan, Nanna Thurmann Jørgensen, Lars Engers Pedersen, Stina Willemoes Borresen, Linda Hilsted, Lennart Friis Hansen, Ulla Feldt-Rasmussen, Marianne Klose
Endocrine.2024;[Epub] CrossRef - Advancements in Cortisol Detection: From Conventional Methods to Next-Generation Technologies for Enhanced Hormone Monitoring
Visesh Vignesh, Bernardo Castro-Dominguez, Tony D. James, Julie M. Gamble-Turner, Stafford Lightman, Nuno M. Reis
ACS Sensors.2024;[Epub] CrossRef - Comparative analysis of salivary cortisol measurements using different assay methods in relation to serum-free cortisol measurement
Anna Lee, Sooah Jang, Sanghoo Lee, Hyun-Kyung Park, In-Young Kim, Ryunsup Ahn, Jeong-Ho Seok, Kyoung-Ryul Lee
Practical Laboratory Medicine.2024; 40: e00393. CrossRef - A dilute and shoot method for urinary free cortisol analysis by LC-MS/MS
Ying Shen, Xia Luo, Qing Guan, Liming Cheng
Journal of Chromatography B.2024; 1239: 124127. CrossRef - Osteopathic Manipulation as a Method of Cortisol Modification: A Systematic Review
Dylan Thibaut, Valentine Santarlas, Joseph Hoppes, Alejandra Vásquez-Castillo, Alexa Morrow, Eddie Oviedo, James Toldi
Cureus.2023;[Epub] CrossRef - Pitfalls in the Diagnosis and Management of Hypercortisolism (Cushing Syndrome) in Humans; A Review of the Laboratory Medicine Perspective
Kade C. Flowers, Kate E. Shipman
Diagnostics.2023; 13(8): 1415. CrossRef - Electrochemical sensors for cortisol detection: Principles, designs, fabrication, and characterisation
Gopi Karuppaiah, Min-Ho Lee, Shekhar Bhansali, Pandiaraj Manickam
Biosensors and Bioelectronics.2023; 239: 115600. CrossRef - The role of the hypothalamic-pituitary-adrenal axis in depression across the female reproductive lifecycle: current knowledge and future directions
Liisa Hantsoo, Kathleen M. Jagodnik, Andrew M. Novick, Ritika Baweja, Teresa Lanza di Scalea, Aysegul Ozerdem, Erin C. McGlade, Diana I. Simeonova, Sharon Dekel, Sara L. Kornfield, Michelle Nazareth, Sandra J. Weiss
Frontiers in Endocrinology.2023;[Epub] CrossRef - РІВЕНЬ СТРЕСУ В ДІТЕЙ ШКІЛЬНОГО ВІКУ З COVID-19
Г. А. Павлишин, О. І. Панченко
Здобутки клінічної і експериментальної медицини.2023; (4): 119. CrossRef - Corticotropin-stimulated steroid profiles to predict shock development and mortality in sepsis: From the HYPRESS study
Josef Briegel, Patrick Möhnle, Didier Keh, Johanna M. Lindner, Anna C. Vetter, Holger Bogatsch, Dorothea Lange, Sandra Frank, Ludwig C. Hinske, Djillali Annane, Michael Vogeser, Michael Bauer, Thorsten Brenner, Patrick Meybohm, Markus Weigand, Matthias Gr
Critical Care.2022;[Epub] CrossRef
- Highly Responsive Bioassay for Quantification of Glucocorticoids

- Endocrine Research
- Comparison of Thyroglobulin Measurements Using Three Different Immunoassay Kits: A BRAMHS Tg-Plus RIA Kit, a BRAMHS hTg Sensitive Kryptor Kit, and a Beckman Coulter ACCESS Immunoassay Kit
- Mijin Kim, Min Ji Jeon, Won Gu Kim, Jong Jin Lee, Jin-Sook Ryu, Eun-Jung Cho, Dae-Hyun Ko, Woochang Lee, Sail Chun, Won-Ki Min, Tae Yong Kim, Young Kee Shong, Won Bae Kim
- Endocrinol Metab. 2016;31(3):462-468. Published online August 2, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.462
- 5,008 View
- 49 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Second-generation thyroglobulin immunometric assays (Tg-IMAs) have been developed with improved sensitivity. Our aim was to compare the diagnostic value of Tg-IMA measurements using a Kryptor (BRAHMS AG) kit (Tg-K) and an ACCESS (Beckman Coulter) kit (Tg-A) with that of the first-generation Tg measurement using a Tg-plus (BRAHMS AG) kit (Tg+).
Methods We enrolled 82 differentiated thyroid cancer patients who underwent total thyroidectomy with radioactive iodine remnant ablation and who underwent diagnostic whole body scan using recombinant human thyroid stimulating hormone (rhTSH). The Tg+, Tg-K, and Tg-A were measured before rhTSH administration during levothyroxine treatment (suppressed Tg) from the same sample. Serum Tg+ was measured after rhTSH stimulation (stimulated Tg).
Results Suppressed Tg+ was more significantly correlated with suppressed Tg-K (
R 2=0.919,P <0.001) than with suppressed Tg-A (R 2=0.536,P <0.001). The optimal cut-off values of suppressed Tg+, Tg-K, and Tg-A for predicting stimulated Tg+ of 1 ng/mL were 0.3, 0.2, and 0.2 ng/mL, respectively. The sensitivity, specificity, and accuracy of suppressed Tg+ were 67%, 100%, and 90%, respectively; those of suppressed Tg-K were 83%, 90%, and 88%; those of suppressed Tg-A were 96%, 82%, and 87%, respectively. The positive predictive and negative predictive values of Tg+ were 100% and 87%, respectively; those of Tg-K were 79% and 92%; and those of Tg-A were 73% and 98%.Conclusion We could not clearly demonstrate which kit had better diagnostic performance after comparison of first-generation Tg measurements with Tg-IMA measurements. Also, there were kit-to-kit variations between Tg-IMA kits. Suppressed Tg measured by Tg-IMA was insufficient to completely substitute for a stimulated Tg measurement.
-
Citations
Citations to this article as recorded by- Comparison of the diagnostic performances of US-guided fine needle aspiration cytology and thyroglobulin measurement for lymph node metastases in patients with differentiated thyroid carcinoma: a meta-analysis
Rong-Bin Liu, Da-Lei Zhou, Bo-Heng Xu, Xin-Hua Yang, Qing Liu, Xiao Zhang, Tao Tang, Zu-Lu Ye, Yue Li
European Radiology.2021; 31(5): 2903. CrossRef - Preoperative Serum Thyroglobulin and Its Correlation with the Burden and Extent of Differentiated Thyroid Cancer
Hosu Kim, So Young Park, Jun-Ho Choe, Jee Soo Kim, Soo Yeon Hahn, Sun Wook Kim, Jae Hoon Chung, Jaehoon Jung, Tae Hyuk Kim
Cancers.2020; 12(3): 625. CrossRef - Estimating the Growth Rate of Lung Metastases in Differentiated Thyroid Carcinoma: Response Evaluation Criteria in Solid Tumors or Doubling Time?
Eyun Song, Jonghwa Ahn, Min Ji Jeon, Sang Min Lee, Jeong Hyun Lee, Tae Yong Kim, Jung Hwan Baek, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2020; 30(3): 418. CrossRef - Impact of delayed radioiodine therapy in intermediate‐/high‐risk papillary thyroid carcinoma
Mijin Kim, Minkyu Han, Min Ji Jeon, Won Gu Kim, In Joo Kim, Jin‐Sook Ryu, Won Bae Kim, Young Kee Shong, Tae Yong Kim, Bo Hyun Kim
Clinical Endocrinology.2019; 91(3): 449. CrossRef - Tertiary Care Experience of Sorafenib in the Treatment of Progressive Radioiodine-Refractory Differentiated Thyroid Carcinoma: A Korean Multicenter Study
Mijin Kim, Tae Hyuk Kim, Dong Yeob Shin, Dong Jun Lim, Eui Young Kim, Won Bae Kim, Jae Hoon Chung, Young Kee Shong, Bo Hyun Kim, Won Gu Kim
Thyroid.2018; 28(3): 340. CrossRef - A Follow-Up Strategy for Patients with an Excellent Response to Initial Therapy for Differentiated Thyroid Carcinoma: Less Is Better
Min Ji Jeon, Mijin Kim, Suyeon Park, Hye-Seon Oh, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2018; 28(2): 187. CrossRef - Preoperative serum thyroglobulin predicts initial distant metastasis in patients with differentiated thyroid cancer
Hosu Kim, Young Nam Kim, Hye In Kim, So Young Park, Jun-Ho Choe, Jung-Han Kim, Jee Soo Kim, Jae Hoon Chung, Tae Hyuk Kim, Sun Wook Kim
Scientific Reports.2017;[Epub] CrossRef
- Comparison of the diagnostic performances of US-guided fine needle aspiration cytology and thyroglobulin measurement for lymph node metastases in patients with differentiated thyroid carcinoma: a meta-analysis


 KES
KES

 First
First Prev
Prev



