Search
- Page Path
- HOME > Search
- Miscellaneous
- COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
- Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim, the Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2021;36(4):757-765. Published online August 17, 2021
- DOI: https://doi.org/10.3803/EnM.2021.404
- 10,271 View
- 417 Download
- 19 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since the first outbreak of coronavirus disease 2019 (COVID-19), ongoing efforts have been made to discover an efficacious vaccine against COVID-19 to combat the pandemic. In most countries, both mRNA and DNA vaccines have been administered, and their side effects have also been reported. The clinical course of COVID-19 and the effects of vaccination against COVID-19 are both influenced by patients’ health status and involve a systemic physiological response. In view of the systemic function of endocrine hormones, endocrine disorders themselves and the therapeutics used to treat them can influence the outcomes of vaccination for COVID-19. However, there are very limited data to support the development of clinical guidelines for patients with specific medical backgrounds based on large clinical trials. In the current severe circumstances of the COVID-19 pandemic, position statements made by clinical specialists are essential to provide appropriate recommendations based on both medical evidence and clinical experiences. As endocrinologists, we would like to present the medical background of COVID-19 vaccination, as well as precautions to prevent the side effects of COVID-19 vaccination in patients with specific endocrine disorders, including adrenal insufficiency, diabetes mellitus, osteoporosis, autoimmune thyroid disease, hypogonadism, and pituitary disorders.
-
Citations
Citations to this article as recorded by- COVID-19 mRNA vaccine may trigger subacute thyroiditis
Mehmet Sözen, Ömercan Topaloğlu, Berrin Çetinarslan, Alev Selek, Zeynep Cantürk, Emre Gezer, Damla Köksalan, Taner Bayraktaroğlu
Human Vaccines & Immunotherapeutics.2024; 17(12): 5120. CrossRef - The role of co-morbidities in the development of an AEFI after COVID-19 vaccination in a large prospective cohort with patient-reported outcomes in the Netherlands
C. Ouaddouh, J.W. Duijster, T. Lieber, F.P.A.M. van Hunsel
Expert Opinion on Drug Safety.2024; 23(3): 323. CrossRef - Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
Hyeyeon Moon, Sunghwan Suh, Mi Kyoung Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Prior immunization status of COVID-19 patients and disease severity: A multicenter retrospective cohort study assessing the different types of immunity
Javaria Aslam, Faisal Shahzad Khan, Muhammad Talha Haris, Hewad Hewadmal, Maryam Khalid, Mohammad Y. Alshahrani, Qurrat-ul-ain Aslam, Irrum Aneela, Urooj Zafar
Vaccine.2023; 41(2): 598. CrossRef - Mortality and Severity of Coronavirus Disease 2019 in Patients with Long-Term Glucocorticoid Therapy: A Korean Nationwide Cohort Study
Eu Jeong Ku, Keeho Song, Kyoung Min Kim, Gi Hyeon Seo, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(2): 253. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Inactivated SARS-CoV-2 vaccination does not disturb the clinical course of Graves’ disease: An observational cohort study
Shichen Xu, Huixin Yu, Xian Cheng, Jing Wu, Jiandong Bao, Li Zhang
Vaccine.2023; 41(38): 5648. CrossRef - Adrenal Crisis Associated With COVID-19 Vaccination in Patients With Adrenal Insufficiency
Yukako Kurematsu, Takako Mohri, Sadanori Okada, Yutaka Takahashi
JCEM Case Reports.2023;[Epub] CrossRef - Adverse Events Associated with COVID-19 Vaccination in Adolescents with Endocrinological Disorders: A Cross-Sectional Study
İbrahim Mert Erbaş, İrem Ceren Erbaş, Gözde Akın Kağızmanlı, Kübra Yüksek Acinikli, Özge Besci, Korcan Demir, Ece Böber, Nurşen Belet, Ayhan Abacı
Journal of Clinical Research in Pediatric Endocrinology.2023; 15(3): 248. CrossRef - Neue Aspekte der Glukokortikoidsubstitution bei Nebennierenrindeninsuffizienz
Tina Kienitz, Gesine Meyer
Der Internist.2022; 63(1): 12. CrossRef - Endocrine Follow-up During Post-Acute COVID-19: Practical Recommendations Based on Available Clinical Evidence
Rimesh Pal, Ameya Joshi, Sanjay K. Bhadada, Mainak Banerjee, Suresh Vaikkakara, Satinath Mukhopadhyay
Endocrine Practice.2022; 28(4): 425. CrossRef - Safety of Inactivated and mRNA COVID-19 Vaccination Among Patients Treated for Hypothyroidism: A Population-Based Cohort Study
Xi Xiong, Carlos King Ho Wong, Ivan Chi Ho Au, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Kristy Tsz Kwan Lau, Chi Ho Lee, Yu Cho Woo, David Tak Wai Lui, Ian Chi Kei Wong
Thyroid.2022; 32(5): 505. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Adrenal Crisis Secondary to COVID-19 Vaccination in a Patient With Hypopituitarism
Nikolina Markovic, Anila Faizan, Chirag Boradia, Sridhar Nambi
AACE Clinical Case Reports.2022; 8(4): 171. CrossRef - The Effect of Inactivated SARS-CoV-2 Vaccines on TRAB in Graves’ Disease
LingHong Huang, ZhengRong Jiang, JingXiong Zhou, YuPing Chen, HuiBin Huang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Osteoporosis in Patients With Respiratory Diseases
Yue Ma, Shui Qiu, Renyi Zhou
Frontiers in Physiology.2022;[Epub] CrossRef - Pilot Findings on SARS-CoV-2 Vaccine-Induced Pituitary Diseases: A Mini Review from Diagnosis to Pathophysiology
Ach Taieb, El Euch Mounira
Vaccines.2022; 10(12): 2004. CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - No need of glucocorticoid dose adjustment in patients with adrenal insufficiency before COVID-19 vaccine
Tania Pilli, Cristina Dalmiglio, Gilda Dalmazio, Alfonso Sagnella, Raffaella Forleo, Lucia Brilli, Fabio Maino, Cristina Ciuoli, Maria Grazia Castagna
European Journal of Endocrinology.2022; 187(1): K7. CrossRef - Diabetes and COVID-19 Vaccination
Hae Dong Choi, Jun Sung Moon
The Journal of Korean Diabetes.2021; 22(4): 221. CrossRef
- COVID-19 mRNA vaccine may trigger subacute thyroiditis

- Miscellaneous
- Clinical Characteristics, Management, and Potential Biomarkers of Endocrine Dysfunction Induced by Immune Checkpoint Inhibitors
- Shintaro Iwama, Tomoko Kobayashi, Hiroshi Arima
- Endocrinol Metab. 2021;36(2):312-321. Published online April 27, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1007
- 5,419 View
- 265 Download
- 14 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
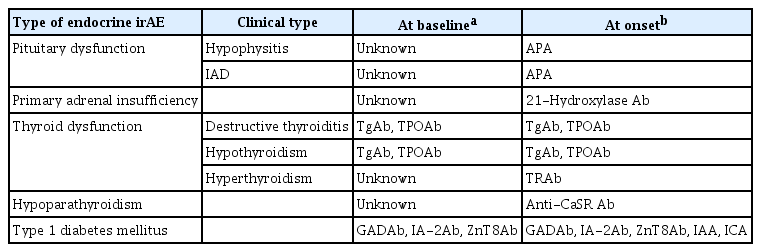
ePub - Immune-related adverse events (irAEs) affecting the endocrine glands are among the most frequent irAEs induced by immune checkpoint inhibitors (ICIs) and include hypopituitarism, primary adrenal insufficiency, thyrotoxicosis, hypothyroidism, hypoparathyroidism, and type 1 diabetes mellitus. Since the incidence and clinical features of endocrine irAEs vary according to the ICI used, it is important to understand the characteristics of these irAEs and to manage each one appropriately. Since some endocrine irAEs, including adrenal crisis and diabetic ketoacidosis, are potentially life-threatening, predicting the risk of endocrine irAEs before their onset is critical. Several autoantibodies have been detected in patients who develop endocrine irAEs, among which anti-thyroid antibodies may be predictive biomarkers of thyroid dysfunction. In this review, we describe the clinical features of each endocrine irAE induced by ICIs and discuss their potential biomarkers, including autoantibodies.
-
Citations
Citations to this article as recorded by- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events
Tomoko Kobayashi, Shintaro Iwama, Hiroshi Arima
Endocrine Journal.2024; 71(1): 23. CrossRef - A case of rapidly progressive insulin-dependent diabetes mellitus without islet autoantibodies developed over two years after the first dose of nivolumab
Kota Nishihama, Yuko Okano, Chisa Inoue, Kanako Maki, Kazuhito Eguchi, Soichiro Tanaka, Atsuro Takeshita, Mei Uemura, Taro Yasuma, Toshinari Suzuki, Esteban C. Gabazza, Yutaka Yano
Diabetology International.2024;[Epub] CrossRef - Endocrinopathies associated with immune checkpoint inhibitor use
Anupam Kotwal, Randol Kennedy, Nupur Kikani, Sonali Thosani, Whitney Goldner, Afreen Shariff
Endocrine Practice.2024;[Epub] CrossRef - Recovery from insulin dependence in immune checkpoint inhibitor‐associated diabetes mellitus: A case report
Marie Okubo, Yuji Hataya, Kanta Fujimoto, Toshio Iwakura, Naoki Matsuoka
Journal of Diabetes Investigation.2023; 14(1): 147. CrossRef - Case Report: A Rising Cause of New-Onset Endocrinopathies After Immunotherapy
Charity Tan, Sarah Hendricks, Kristina Hernandez, Martha Benavides, Rupinderjit Samra
The Journal for Nurse Practitioners.2023; 19(5): 104582. CrossRef - Risk of Thyroid Dysfunction in PD-1 Blockade Is Stratified by the Pattern of TgAb and TPOAb Positivity at Baseline
Xin Zhou, Shintaro Iwama, Tomoko Kobayashi, Masahiko Ando, Hiroshi Arima
The Journal of Clinical Endocrinology & Metabolism.2023; 108(10): e1056. CrossRef - Severe thyrotoxicosis induced by tislelizumab: a case report and literature review
Liman Huo, Chao Wang, Haixia Ding, Xuelian Shi, Bin Shan, Ruoying Zhou, Ping Liang, Juan Hou
Frontiers in Oncology.2023;[Epub] CrossRef - Life-Threatening Endocrinological Immune-Related Adverse Events of Immune Checkpoint Inhibitor Therapy
Aleksandra Basek, Grzegorz K. Jakubiak, Grzegorz Cieślar, Agata Stanek
Cancers.2023; 15(24): 5786. CrossRef - Increased Risk of Thyroid Dysfunction by PD-1 and CTLA-4 Blockade in Patients Without Thyroid Autoantibodies at Baseline
Shintaro Iwama, Tomoko Kobayashi, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Masahiko Ando, Xin Zhou, Ayana Yamagami, Takeshi Onoue, Yohei Kawaguchi, Takashi Miyata, Mariko Sugiyama, Hiroshi Takagi, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tets
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): e1620. CrossRef - Biomarkers and risk factors for the early prediction of immune-related adverse events: a review
Ying Zhang, Xiaoling Zhang, Weiling Li, Yunyi Du, Wenqing Hu, Jun Zhao
Human Vaccines & Immunotherapeutics.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors as a Threat to the Hypothalamus–Pituitary Axis: A Completed Puzzle
Agnese Barnabei, Andrea Corsello, Rosa Maria Paragliola, Giovanni Maria Iannantuono, Luca Falzone, Salvatore Maria Corsello, Francesco Torino
Cancers.2022; 14(4): 1057. CrossRef - Elevated TSH Level, TgAb, and Prior Use of Ramucirumab or TKIs as Risk Factors for Thyroid Dysfunction in PD-L1 Blockade
Tomoko Kobayashi, Shintaro Iwama, Ayana Yamagami, Yoshinori Yasuda, Takayuki Okuji, Masaaki Ito, Xin Zhou, Masahiko Ando, Takeshi Onoue, Takashi Miyata, Mariko Sugiyama, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Tetsunari Hase, Masahiro Morise, Taka
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4115. CrossRef - Preconditioning of the immune system modulates the response of papillary thyroid cancer to immune checkpoint inhibitors
Fabiana Pani, Yoshinori Yasuda, Sylvie T Rousseau, Kevin C Bermea, Solmaz Roshanmehr, Rulin Wang, Srinivasan Yegnasubramanian, Patrizio Caturegli, Luigi Adamo
Journal for ImmunoTherapy of Cancer.2022; 10(12): e005538. CrossRef - Survival benefit of endocrine dysfunction following immune checkpoint inhibitors for nonthyroidal cancers
Anupam Kotwal, Mabel Ryder
Current Opinion in Endocrinology, Diabetes & Obesity.2021; 28(5): 517. CrossRef
- Clinical characteristics and potential biomarkers of thyroid and pituitary immune-related adverse events

- Miscellaneous
- Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
- Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon, Hwa Young Ahn, Hoon Sung Choi, Sang Mo Hong, Dong Yeob Shin, Ji A Seo, Se Hwa Kim, Seungjoon Oh, Sung Hoon Yu, Byung Joon Kim, Choong Ho Shin, Sung-Woon Kim, Chong Hwa Kim, Eun Jig Lee
- Endocrinol Metab. 2020;35(2):272-287. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.272
- 9,383 View
- 426 Download
- 13 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
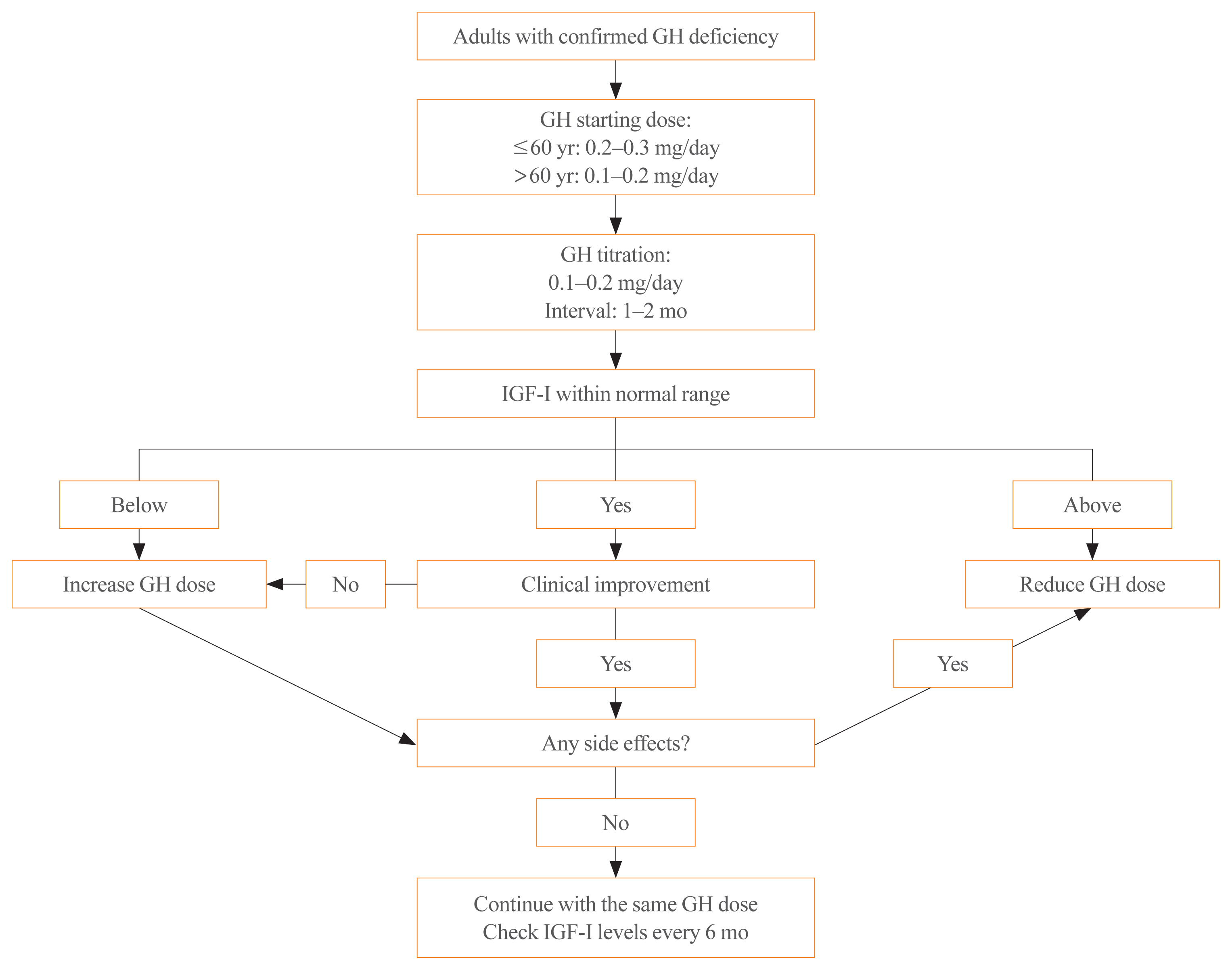
ePub - Growth hormone (GH) deficiency is caused by congenital or acquired causes and occurs in childhood or adulthood. GH replacement therapy brings benefits to body composition, exercise capacity, skeletal health, cardiovascular outcomes, and quality of life. Before initiating GH replacement, GH deficiency should be confirmed through proper stimulation tests, and in cases with proven genetic causes or structural lesions, repeated GH stimulation testing is not necessary. The dosing regimen of GH replacement therapy should be individualized, with the goal of minimizing side effects and maximizing clinical improvements. The Korean Endocrine Society and the Korean Society of Pediatric Endocrinology have developed a position statement on the diagnosis and treatment of GH deficiency. This position statement is based on a systematic review of evidence and expert opinions.
-
Citations
Citations to this article as recorded by- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Ghina Tsurayya, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, Muhammad Iqhrammullah
Children.2024; 11(2): 227. CrossRef - Evaluation of Adult Height in Patients with Non-Permanent Idiopathic GH Deficiency
Agnese Murianni, Anna Lussu, Chiara Guzzetti, Anastasia Ibba, Letizia Casula, Mariacarolina Salerno, Marco Cappa, Sandro Loche
Endocrines.2023; 4(1): 169. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Continuous Glucose Monitoring: A Possible Aid for Detecting Hypoglycemic Events during Insulin Tolerance Tests
Soo Yeun Sim, Moon Bae Ahn
Sensors.2023; 23(15): 6892. CrossRef - The risk patients with AGHD have of developing CVD
Eisha Javed, Maha Zehra, Naz Elahi
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 19: 200221. CrossRef - Diagnosis of GH Deficiency Without GH Stimulation Tests
Anastasia Ibba, Sandro Loche
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
Endocrinology and Metabolism.2022; 37(2): 359. CrossRef - A Radiomics-Based Model with the Potential to Differentiate Growth Hormone Deficiency and Idiopathic Short Stature on Sella MRI
Taeyoun Lee, Kyungchul Song, Beomseok Sohn, Jihwan Eom, Sung Soo Ahn, Ho-Seong Kim, Seung-Koo Lee
Yonsei Medical Journal.2022; 63(9): 856. CrossRef - Phenotypic spectrum of patients with mutations in CHD7: clinical implications of endocrinological findings
Ja Hye Kim, Yunha Choi, Soojin Hwang, Gu-Hwan Kim, Han-Wook Yoo, Jin-Ho Choi
Endocrine Connections.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Laron syndrome: clinic, diagnostics (а clinical case)
P.M. Lіashuk, R.P. Lіashuk, N.I. Stankova, M.B. Kudina
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 193. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - Asian Conference on Tumor Ablation guidelines for renal cell carcinoma
Byung Kwan Park, Shu-Huei Shen, Masashi Fujimori, Yi Wang
Investigative and Clinical Urology.2021; 62(4): 378. CrossRef - Diagnosis and Treatment of Adult Growth Hormone Deficiency
Jung Hee Kim
The Korean Journal of Medicine.2021; 96(5): 400. CrossRef
- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial

- A Clinical Study on Hypopitutiarism: Significance of Combined Pituitary Stimulation Test.
- Bo Youn Cho, Hong Gyu Lee, Chang Soon Koh, Hyung Kyu Park, Sook Kyung Kim, Chan Soo Shin, Seong Yeon Kim, Jae Seok Chun, Kyung Soo Park, Hyeon Kyu Kim, Sun Wook Kim
- J Korean Endocr Soc. 1996;11(3):268-276. Published online November 7, 2019
- 1,228 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Hypopituitarism can be caused by various diseases. Its clinical manifestations vary, depending on the extent and severity of the pituitary hormone deficiency. And some patients may initially present with SIADH-like features. Combined pituitary stimulation test has been used for the diagnosis of hypopituitarism and subsequent hormone replacement therapy. However, the test is laborious, expensive and uncomfortable to the patients, So we performed this study to know whether combined pituitary stimulation test can be replaced with clinical features and simple basal hormone concentrations. Methods: Fifty-four patients who were diagnosed as hypopituitarism by combined pituitary stimulation test were included in this study. Clinical features and basal hormone data were compared with the results of combined pituitary stimulation test for the evaluation of pituitary-gonadal, pituitary-thyroid, and pituitary-adrenal axes, using X2 test. Results: 1) In pituitary-gonadal axis, the evaluation of clinical features and basal gonad hormone concentrations were significantly consistent with stimulation test(p<0.05), 2) In pituitary-thyroid axis, the evaluation of basal thyroid hormone concentrations were more helpful than stimulation test though results of the two tests were not consistent. 3) In pituitary-adrenal axis, all patients whose basal cortisol concentrations were low showed inadequate responses to stimulation test. However, stimulation test revealed adrenal insufficiency in some patients with normal basal cortisol concentrations. 4) 9 patients who presented with SIADH-like features were older than the others and had all corticotropin deficiency. Conclusion: In patients with suspected hypopituitarism, the evaluation of clinical features and basal hormone concentrations can be sufficient for the diagnosis of hypopituitarism and hormone replacement therapy. However, stimulation test is necessary to investigate adrenal function in patients with normal basal cortisol concentrations. And hypopituitarism should be considered in old patients who present with SIADH-like features.

- Clinical Characteristics of Patients with Adrenal Insufficiency in a General Hospital
- Ye Yeon Lee, Nan Hee Cho, Jong Won Lee, Nam Kyung Kim, Hye Soon Kim, Mi-Kyung Kim
- Endocrinol Metab. 2017;32(1):83-89. Published online February 28, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.83
- 4,398 View
- 59 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Adrenal insufficiency (AI) is a life-threatening disorder caused by the deficiency of adrenal steroid hormones. This retrospective cross-sectional study investigated the characteristics of patients with AI in Korea.
Methods All consecutive patients with suspected AI who received care at a tertiary referral center in Korea in 2014 and underwent adrenocorticotropic hormone stimulation or insulin-tolerance testing were identified through a review of medical charts. Patients diagnosed with AI were enrolled. Their demographic, clinical, and treatment details were extracted.
Results Of 771 patients with suspected AI, 183 (23.7%) received a definitive diagnosis. The most common reason for testing was the presence of suspicious AI-related symptoms (30.0%), followed by a history of steroid medications (23.5%). Their mean age was 66.7 years, and females predominated (67.8%). The most common symptoms were general weakness, anorexia, arthralgia, and fever. Approximately half (53.6%) had a history of steroid use. Hydrocortisone was the most common treatment (71.6%), with most patients taking a 30 mg dose (44.2%). The most common dose frequency was twice a day (78.6%). Fourteen patients were treated for adrenal crisis (
n =10, 5.5%) or an intercurrent illness (n =4, 2.2%).Conclusion AI may have been caused by steroid medication use in many of the patients included in this study. The detection of AI can be improved by careful history-taking and being alert to the possibility that a patient has used steroids.
-
Citations
Citations to this article as recorded by- Risk of Mental Illnesses in Patients With Hypopituitarism: A Nationwide Population-Based Cohort Study
I-Hua Wei, Chih-Chia Huang
Psychiatry Investigation.2022; 19(6): 418. CrossRef - The Role of the Pharmacist in Optimizing Cancer Immunotherapy: A Retrospective Study of Nivolumab Adverse Events
Bradley D. Menz, Jacinta L. Johnson, Davina F. Gillard, William Chong, Michael B. Ward
Journal of Pharmacy Practice.2021; 34(3): 386. CrossRef - Clinical and biochemical factors to predict biochemical adrenal insufficiency in hospitalized patients with indeterminate cortisol levels: a retrospective study
Worapaka Manosroi, Natapong Kosachunhanan, Pichitchai Atthakomol
BMC Endocrine Disorders.2020;[Epub] CrossRef - Possible adrenal insufficiency among fatigue patients in a psychosomatic medical clinic
Sunao Matsubayashi, Nobuhiro Nakatake, Takeshi Hara
Endocrine Journal.2020; 67(1): 53. CrossRef - Encountering COVID-19 as Endocrinologists
Eun-Jung Rhee, Jung Hee Kim, Sun Joon Moon, Won-Young Lee
Endocrinology and Metabolism.2020; 35(2): 197. CrossRef - Glucocorticoid management of adrenal insufficiency in the United Kingdom: assessment using real-world data
Kamran Iqbal, Kate Halsby, Robert D Murray, Paul V Carroll, Robert Petermann
Endocrine Connections.2019; 8(1): 20. CrossRef
- Risk of Mental Illnesses in Patients With Hypopituitarism: A Nationwide Population-Based Cohort Study

- Clinical Study
- Electrolyte Imbalance in Patients with Sheehan's Syndrome
- Chur Hoan Lim, Ji Hyun Han, Joon Jin, Ji Eun Yu, Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
- Endocrinol Metab. 2015;30(4):502-508. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.502
- 4,831 View
- 45 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated the prevalence of electrolyte imbalance and the relationship between serum electrolyte and anterior pituitary hormone levels in patients with Sheehan's syndrome.
Methods In a retrospective study, we investigated 78 patients with Sheehan's syndrome. We also included 95 normal control subjects who underwent a combined anterior pituitary hormone stimulation test and showed normal hormonal responses.
Results In patients with Sheehan's syndrome, the serum levels of sodium, potassium, ionized calcium, magnesium, and inorganic phosphate were significantly lower than those in control subjects. The prevalence of hyponatremia, hypokalemia, hypocalcemia, hypomagnesemia, and hypophosphatemia in patients with Sheehan's syndrome was 59.0% (
n =46), 26.9% (n =21), 35.9% (n =28), 47.4% (n =37), and 23.1% (n =18), respectively. Levels of sodium and ionized calcium in serum were positively correlated with levels of all anterior pituitary hormones (allP <0.05). Levels of potassium in serum were positively correlated with adrenocorticotrophic hormone (ACTH) and growth hormone (GH) levels (allP <0.05). Levels of inorganic phosphate in serum were positively correlated with levels of thyroid-stimulating hormone, prolactin, and GH (allP <0.05), and levels of magnesium in serum were positively correlated with delta ACTH (P <0.01).Conclusion Electrolyte imbalance was common in patients with Sheehan's syndrome. Furthermore, the degree of anterior pituitary hormone deficiency relates to the degree of electrolyte disturbance in patients with this disease.
-
Citations
Citations to this article as recorded by- Myopathic syndrome revealing a rare condition: Sheehan syndrome, a case-based review
Elena Gradinaru, Catalin Furculescu, Andreea Trandafir, Daniela Opris-Belinski, Ioana Cristina Saulescu
Clinical Rheumatology.2023; 42(6): 1705. CrossRef - Partial Sheehan’s syndrome with abdominal tuberculosis presented with pancytopenia and fluctuating thyroid profile: a case report
Prashant Yadav, Md Anwarul Bari, Akash Saha, Sushmita Yadav, Amzad H. Khan
Annals of Medicine & Surgery.2023; 85(3): 548. CrossRef - Acute pituitary crisis after lumbar surgery: A case report
Hui Wang, Xingrui Gong
Medicine.2023; 102(48): e36294. CrossRef - Long-term hepatic and cardiac health in patients diagnosed with Sheehan’s syndrome
Liza Das, Jayaprakash Sahoo, Neelam Dahiya, Sunil Taneja, Sanjay Kumar Bhadada, Mohammad Hayat Bhat, Paramjeet Singh, Vanita Suri, Bashir Ahmad Laway, Pinaki Dutta
Pituitary.2022; 25(6): 971. CrossRef - Clinical, endocrine, metabolic profile, and bone health in Sheehan's syndrome
Soumita Mandal, Pradip Mukhopadhyay, Mainak Banerjee, Sujoy Ghosh
Indian Journal of Endocrinology and Metabolism.2020; 24(4): 338. CrossRef - A rare endocrine cause of electrical storm - a case report
Sunny D Shinde, Girish R Sabnis, Charan P Lanjewar, Prafulla G Kerkar
European Heart Journal - Case Reports.2017;[Epub] CrossRef - Sheehan syndrome
Züleyha Karaca, Bashir A. Laway, Hatice S. Dokmetas, Hulusi Atmaca, Fahrettin Kelestimur
Nature Reviews Disease Primers.2016;[Epub] CrossRef
- Myopathic syndrome revealing a rare condition: Sheehan syndrome, a case-based review

- Adrenal gland
- Diagnosis and Treatment of Hypopituitarism
- Seong Yeon Kim
- Endocrinol Metab. 2015;30(4):443-455. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.443
- 13,329 View
- 384 Download
- 49 Web of Science
- 59 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hypopituitarism is a chronic endocrine illness that caused by varied etiologies. Clinical manifestations of hypopituitarism are variable, often insidious in onset and dependent on the degree and severity of hormone deficiency. However, it is associated with increased mortality and morbidity. Therefore, early diagnosis and prompt treatment is necessary. Hypopituitarism can be easily diagnosed by measuring basal pituitary and target hormone levels except growth hormone (GH) and adrenocorticotropic hormone (ACTH) deficiency. Dynamic stimulation tests are indicated in equivocal basal hormone levels and GH/ACTH deficiency. Knowledge of the use and limitations of these stimulation tests is mandatory for proper interpretation. It is necessary for physicians to inform their patients that they may require lifetime treatment. Hormone replacement therapy should be individualized according to the specific needs of each patient, taking into account possible interactions. Long-term endocrinological follow-up of hypopituitary patients is important to monitor hormonal replacement regimes and avoid under- or overtreatment.
-
Citations
Citations to this article as recorded by- Pituitary stem cells: past, present and future perspectives
María Inés Pérez Millán, Leonard Y. M. Cheung, Florencia Mercogliano, Maria Andrea Camilletti, Gonzalo T. Chirino Felker, Lucia N. Moro, Santiago Miriuka, Michelle L. Brinkmeier, Sally A. Camper
Nature Reviews Endocrinology.2024; 20(2): 77. CrossRef - Idiopathic isolated adrenocorticotropic hormone deficiency: a systematic review of a heterogeneous and underreported disease
E. Van Mieghem, C. De Block, C. De Herdt
Pituitary.2024; 27(1): 23. CrossRef - Perioperative growth hormone levels as an early predictor of new-onset secondary adrenal insufficiency following transsphenoidal pituitary tumor resection
Fon-Yih Tsuang, Shyang-Rong Shih, Ham-Min Tseng, Huan-Chih Wang
Asian Journal of Surgery.2024; 47(4): 1746. CrossRef - A comprehensive review of the new FIGO classification of ovulatory disorders
Adam H Balen, Jennifer Tamblyn, Karolina Skorupskaite, Malcolm G Munro
Human Reproduction Update.2024;[Epub] CrossRef - Panhypopituitarism caused by a suprasellar germinoma: A case report
Jelena Roganovic, Lea Saric, Silvije Segulja, Ana Dordevic, Mia Radosevic
World Journal of Clinical Cases.2024; 12(10): 1844. CrossRef - Decreased mannan-binding lectin level in adults with hypopituitarism; dependence on appropriate hormone replacement therapies
Aleksandra E. Matusiak, Jan Stępniak, Andrzej Lewiński, Małgorzata Karbownik-Lewińska
Frontiers in Immunology.2023;[Epub] CrossRef - Post-Operative Medium- and Long-Term Endocrine Outcomes in Patients with Non-Functioning Pituitary Adenomas—Machine Learning Analysis
Ziad Hussein, Robert W. Slack, Hani J. Marcus, Evangelos B. Mazomenos, Stephanie E. Baldeweg
Cancers.2023; 15(10): 2771. CrossRef - Central Endocrine Complications Among Childhood Cancer Survivors Treated With Radiation Therapy: A PENTEC Comprehensive Review
Greg Wheeler, Clemens Grassberger, Josephine Samers, Mary Dwyer, Kirsty Wiltshire, Patricia Daly, Beatriz Alvarez, Belinda A. Campbell, Amanda J. Kerr, Tomas Kron, Frances K. Duane, Margaret Zacharin, Peter Downie, Elizabeth Kyriakou, Cecile M. Ronckers,
International Journal of Radiation Oncology*Biology*Physics.2023;[Epub] CrossRef - The TRH test provides valuable information in the diagnosis of central hypothyroidism in patients with known pituitary disease and low T4 levels
Sara Ellegaard Christensen, Liv Norma Smith, Christian Alexander H. Rosendal, Helga Angela Gulisano, Kåre Schmidt Ettrup, Peter Vestergaard, Eigil Husted Nielsen, Jesper Scott Karmisholt, Jakob Dal
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sheehan’s syndrome unveiled after decades without a diagnosis: A case report
Hadi Rabee’, Tamara Braik, Rezeq Alnatour, Alaa Shamlawi, Ammar Rashed
SAGE Open Medical Case Reports.2023;[Epub] CrossRef - PAN-HIPOPITUITARISMO SECUNDÁRIO A INFECÇÃO POR SARS-COV-2: RELATO DE CASO
Rosyane Luz Rufino De Lima, Viviane dos Reis Vieira Yance
REVISTA FOCO.2023; 16(12): e3832. CrossRef - Navigating the “specific etiology” steatohepatitis category: Evaluation and management of nonalcoholic/nonmetabolic dysfunction–associated steatohepatitis
Mohammad Qasim Khan, Sara Hassan, Blanca C. Lizaola-Mayo, Mamatha Bhat, Kymberly D. Watt
Hepatology.2023;[Epub] CrossRef - Regulation of the Hypothalamic-Pituitary-Testicular Axis: Pathophysiology of Hypogonadism
Aditi Sharma, Channa N. Jayasena, Waljit S. Dhillo
Endocrinology and Metabolism Clinics of North America.2022; 51(1): 29. CrossRef - Penetrating brain injury with hypopituitarism
Rachel D. Appelbaum, Kristina E. Neri, Kristin A. Rebo, Samuel P. Carmichael
Trauma Case Reports.2022; 38: 100628. CrossRef - Risk of Mental Illnesses in Patients With Hypopituitarism: A Nationwide Population-Based Cohort Study
I-Hua Wei, Chih-Chia Huang
Psychiatry Investigation.2022; 19(6): 418. CrossRef - Pituitary Apoplexy and Subdural Hematoma after Caesarean Section
Van Trung Hoang, The Huan Hoang, Thanh Tam Thi Nguyen, Vichit Chansomphou, Duc Thanh Hoang, Kyousuke Takeuchi
Case Reports in Obstetrics and Gynecology.2022; 2022: 1. CrossRef - A Unique Case Mimicking Sepsis
Vivek Dave, Anish Joshi
Journal of Acute Care.2022; 1(1): 29. CrossRef - Correlation between shift work and non-alcoholic fatty liver disease among male workers in the steel manufacturing company of Korea: a cross-sectional study
Kiseok Kim, Yong-Jin Lee, Soon-Chan Kwon, Young-Sun Min, Hyun Kyo Lee, Gwangin Baek, Sang Hyeon Kim, Eun-Chul Jang
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - Non-alcoholic fatty liver disease across endocrinopathies: Interaction with sex hormones
Sara Arefhosseini, Mehrangiz Ebrahimi-Mameghani, Farzad Najafipour, Helda Tutunchi
Frontiers in Endocrinology.2022;[Epub] CrossRef - Primary hypothyroidism and postmenopause as the causes of delayed diagnosis of panhypopituitarism in a patient with nonfunctional pituitary adenoma
E. G. Ryzhkova, D. O. Ladygina
Problems of Endocrinology.2022; 68(5): 32. CrossRef - Efficacy and Safety of Stereotactic Radiotherapy in Cushing’s Disease: A Single Center Experience
Tugce Apaydin, Hande Mefkure Ozkaya, Sebnem Memis Durmaz, Rasim Meral, Pinar Kadioglu
Experimental and Clinical Endocrinology & Diabetes.2021; 129(07): 482. CrossRef - Metabolic and Endocrine Challenges
Gennaro Martucci, Eleonora Bonicolini, Dhruv Parekh, Onn Shaun Thein, Mario Scherkl, Karin Amrein
Seminars in Respiratory and Critical Care Medicine.2021; 42(01): 078. CrossRef - The Effect of Pituitary Gland Disorders on Glucose Metabolism: From Pathophysiology to Management
Guy I. Sydney, Konstantinos Michalakis, Ilias P. Nikas, Eleftherios Spartalis, Stavroula A. Paschou
Hormone and Metabolic Research.2021; 53(01): 16. CrossRef - Congenital hypopituitarism in two brothers with a duplication of the ‘acrogigantism gene’ GPR101: clinical findings and review of the literature
Melitza S. M. Elizabeth, Annemieke J. M. H. Verkerk, Anita C. S. Hokken-Koelega, Joost A. M. Verlouw, Jesús Argente, Roland Pfaeffle, Sebastian J. C. M. M. Neggers, Jenny A. Visser, Laura C. G. de Graaff
Pituitary.2021; 24(2): 229. CrossRef - Association between Nonalcoholic Fatty Liver Disease and Endocrinopathies: Clinical Implications
Ana-Maria Singeap, Carol Stanciu, Laura Huiban, Cristina Maria Muzica, Tudor Cuciureanu, Irina Girleanu, Stefan Chiriac, Sebastian Zenovia, Robert Nastasa, Catalin Sfarti, Camelia Cojocariu, Anca Trifan, Branka Filipović
Canadian Journal of Gastroenterology and Hepatology.2021; 2021: 1. CrossRef - The evaluation of pituitary damage associated with cardiac arrest: An experimental rodent model
Yu Okuma, Tomoaki Aoki, Santiago J. Miyara, Kei Hayashida, Mitsuaki Nishikimi, Ryosuke Takegawa, Tai Yin, Junhwan Kim, Lance B. Becker, Koichiro Shinozaki
Scientific Reports.2021;[Epub] CrossRef - Functional Restoration of Pituitary after Pituitary Allotransplantation into Hypophysectomized Rats
Jai Ho Choi, Jung Eun Lee, Hong-Lim Kim, Seung Hyun Ko, Se Hoon Kim, Seung Ho Yang
Cells.2021; 10(2): 267. CrossRef - Experience of a Pituitary Clinic for US Military Veterans With Traumatic Brain Injury
Jonathan Lee, Lindsey J Anderson, Dorota Migula, Kevin C J Yuen, Lisa McPeak, Jose M Garcia
Journal of the Endocrine Society.2021;[Epub] CrossRef - Biogenic zinc-oxide nanoparticles of Moringa oleifera leaves abrogates rotenone induced neuroendocrine toxicity by regulation of oxidative stress and acetylcholinesterase activity
J.K. Akintunde, T.I. Farai, M.R. Arogundade, J.T. Adeleke
Biochemistry and Biophysics Reports.2021; 26: 100999. CrossRef - Heart Rate Variability in Postoperative Patients with Nonfunctioning Pituitary Adenoma
Jeonghoon Ha, Hansang Baek, Chaiho Jeong, Minsoo Yeo, Seung-Hwan Lee, Jae Hyoung Cho, Ki-Hyun Baek, Moo Il Kang, Dong-Jun Lim
Endocrinology and Metabolism.2021; 36(3): 678. CrossRef - Aetiologies and clinical patterns of hypopituitarism in Sudanese children
Samar Hassan, Renson Mukhwana, Salwa Musa, Areej Ibrahim, Omer Babiker, Mohamed Abdullah
Sudanese Journal of Paediatrics.2021; : 53. CrossRef - Recent advances in proteomics and its implications in pituitary endocrine disorders
Arghya Banerjee, Atul Goel, Abhidha Shah, Sanjeeva Srivastava
Biochimica et Biophysica Acta (BBA) - Proteins and Proteomics.2021; 1869(11): 140700. CrossRef - Morning Serum Cortisol as a Predictor for the HPA Axis Recovery in Cushing’s Disease
Q. Cui, D. Liu, B. Xiang, Q. Sun, L. Fan, M. He, Y. Wang, X. Zhu, H. Ye, Giorgio Borretta
International Journal of Endocrinology.2021; 2021: 1. CrossRef - Three different faces of TACI mutations
Sukru Cekic, Fatih Cicek, Yasin Karali, Orhan Gorukmez, Erdal Eren, Sara Sebnem Kilic
Scandinavian Journal of Immunology.2020;[Epub] CrossRef - Treatment of a Woman with Inoperable Meningioma Using Mifepristone for 26 Years
Maria das Dores Medina-Lopes, Luiz Augusto Casulari
Case Reports in Neurological Medicine.2020; 2020: 1. CrossRef - Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon
Endocrinology and Metabolism.2020; 35(2): 272. CrossRef - Phenytoin- Medication That Warrants Deviation From Standard Approach for Thyroid Lab Interpretation
Vishwanath Pattan, Narsimha Candula, Ramesh Adhikari, Rahul Kashyap
Cureus.2020;[Epub] CrossRef - Pituitary Disorders in Pregnancy
Whitney W. Woodmansee
Neurologic Clinics.2019; 37(1): 63. CrossRef - A clinical case of partial hypopituitarism
T. E. Pomytkina
Fundamental and Clinical Medicine.2019; 4(3): 122. CrossRef - Mesencephalic Astrocyte-Derived Neurotrophic Factor (MANF) Is Highly Expressed in Mouse Tissues With Metabolic Function
Tatiana Danilova, Emilia Galli, Emmi Pakarinen, Erik Palm, Päivi Lindholm, Mart Saarma, Maria Lindahl
Frontiers in Endocrinology.2019;[Epub] CrossRef - Functional survival of rat pituitary gland in hypothermic storage for pituitary transplantation
Jai Ho Choi, Jung Eun Lee, Se Hoon Kim, Hong-Lim Kim, Sin Soo Jeun, Seung Ho Yang
Pituitary.2019; 22(4): 353. CrossRef - Fertility after transsphenoidal surgery in patients with prolactinomas: A meta-analysis
Nayan Lamba, Nadia Noormohamed, Thomas Simjian, Mona Y. Alsheikh, Alykhan Jamal, Joanne Doucette, Hasan Zaidi, Timothy R. Smith, Rania A. Mekary
Clinical Neurology and Neurosurgery.2019; 176: 53. CrossRef - Traumatic brain injury and hypopituitarism
Sarah Leeder
Advances in Clinical Neuroscience & Rehabilitation.2019;[Epub] CrossRef - Long-acting FC-fusion rhGH (GX-H9) shows potential for up to twice-monthly administration in GH-deficient adults
Cheol Ryong Ku, Thierry Brue, Katharina Schilbach, Stanislav Ignatenko, Sandor Magony, Yoon-Sok Chung, Byung-Joon Kim, Kyu Yeon Hur, Ho-Cheol Kang, Jung Hee Kim, Min Seon Kim, Aldona Kowalska, Marek Bolanowski, Marek Ruchala, Svetozar Damjanovic, Juraj Pa
European Journal of Endocrinology.2018; 179(3): 169. CrossRef - Prolactinomas Resistant to Treatment With Dopamine Agonists: Long-Term Follow-Up of Six Cases
Maria de Fátima de Magalhães Gonzaga, Lucas Faria de Castro, Luciana Ansaneli Naves, José Luiz Mendonça, Benicio Oton de Lima, Iruena Kessler, Luiz Augusto Casulari
Frontiers in Endocrinology.2018;[Epub] CrossRef - Oxytocin and Naltrexone Successfully Treat Hypothalamic Obesity in a Boy Post-Craniopharyngioma Resection
Eugenie A Hsu, Jennifer L Miller, Francisco A Perez, Christian L Roth
The Journal of Clinical Endocrinology & Metabolism.2018; 103(2): 370. CrossRef - Spectrum of Sellar and Parasellar Region Lesions: A retrospective study from Basrah, Iraq
Abbas Ali Mansour, Ali Hussain Ali Alhamza, Ammar Mohammed Saeed Abdullah Almomin, Ibrahim Abbood Zaboon, Nassar Taha Yaseen Alibrahim, Rudha Naser Hussein, Muayad Baheer Kadhim, Haider Ayad Yassin Alidrisi, Hussein Ali Nwayyir, Adel Gassab Mohammed, Dhey
F1000Research.2018; 7: 430. CrossRef - Delayed Complications After Transsphenoidal Surgery for Pituitary Adenomas
Gmaan Alzhrani, Walavan Sivakumar, Min S. Park, Philipp Taussky, William T. Couldwell
World Neurosurgery.2018; 109: 233. CrossRef - Hypopituitarism: Case Study Involving Hypernatremia Prompting Discovery of a Pituitary Disorder in a Patient With Lymphoma
Jace Johnny
Clinical Journal of Oncology Nursing.2018; 22(4): E115. CrossRef - Reflex and reflective testing strategies for early detection of pituitary dysfunction
Manal Elnenaei, Derek Minney, David B. Clarke, Andrew Kumar-Misir, Syed Ali Imran
Clinical Biochemistry.2018; 54: 78. CrossRef - Clinical Parameters to Distinguish Silent Corticotroph Adenomas from Other Nonfunctioning Pituitary Adenomas
Daham Kim, Cheol Ryong Ku, Se Hee Park, Ju Hyung Moon, Eui Hyun Kim, Sun Ho Kim, Eun Jig Lee
World Neurosurgery.2018; 115: e464. CrossRef - The Incidence of Anterior Pituitary Hormone Deficiencies in Patients with Pituitary Microadenoma and Idiopathic Hyperprolactinaemia. A Retrospective Single Centre Study
Journal of Clinical Review & Case Reports.2018;[Epub] CrossRef - Spectrum of Pituitary disorders: A retrospective study from Basrah, Iraq
Abbas Ali Mansour, Ali Hussain Ali Alhamza, Ammar Mohammed Saeed Abdullah Almomin, Ibrahim Abbood Zaboon, Nassar Taha Yaseen Alibrahim, Rudha Naser Hussein, Muayad Baheer Kadhim, Haider Ayad Yassin Alidrisi, Hussein Ali Nwayyir, Adel Gassab Mohammed, Dhey
F1000Research.2018; 7: 430. CrossRef - Growth Hormone & Hypopituitarism
Lahiry Sandeep
Journal of Analytical & Pharmaceutical Research.2017;[Epub] CrossRef - Using the Complexity of Hypopituitarism Aetiology to Understand and Teach Hormone Function in Endocrinology
Ayisha Qureshi
MOJ Anatomy & Physiology.2017;[Epub] CrossRef - Delayed diagnosis of pituitary stalk interruption syndrome with severe recurrent hyponatremia caused by adrenal insufficiency
Kyung Mi Jang, Cheol Woo Ko
Annals of Pediatric Endocrinology & Metabolism.2017; 22(3): 208. CrossRef - Indicaciones e interpretación diagnóstica de las pruebas funcionales hipofisarias
C. Tasende Fernández, M.J. Rodríguez Troyano, D.S. Trifu, P. Gómez Montes
Medicine - Programa de Formación Médica Continuada Acreditado.2016; 12(15): 865. CrossRef - Hypopituitarism in the elderly: a narrative review on clinical management of hypothalamic–pituitary–gonadal, hypothalamic–pituitary–thyroid and hypothalamic–pituitary–adrenal axes dysfunction
L. Curtò, F. Trimarchi
Journal of Endocrinological Investigation.2016; 39(10): 1115. CrossRef - Hipopituitarismo. Panhipopituitarismo
N. Peláez Torres, D.S. Trifu, M.P Gómez Montes, E. Atienza Sánchez
Medicine - Programa de Formación Médica Continuada Acreditado.2016; 12(15): 857. CrossRef
- Pituitary stem cells: past, present and future perspectives

- Adrenal gland
- Clinical Characteristics, Management, and Outcome of 22 Cases of Primary Hypophysitis
- Sun Mi Park, Ji Cheol Bae, Ji Young Joung, Yoon Young Cho, Tae Hun Kim, Sang-Man Jin, Sunghwan Suh, Kyu Yeon Hur, Kwang-Won Kim
- Endocrinol Metab. 2014;29(4):470-478. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.470
- 4,205 View
- 41 Download
- 26 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Primary hypophysitis causes varying degrees of endocrine dysfunction and mass effect. The natural course and best treatment have not been well established.
Methods Medical records of 22 patients who had been diagnosed with primary hypophysitis between January 2001 and March 2013 were retrospectively reviewed. Based on the anatomical location, we classified the cases as adenohypophysitis (AH), infundibuloneurohypophysitis (INH), and panhypophysitis (PH). Clinical presentation, endocrine function, pathologic findings, magnetic resonance imaging findings, and treatment courses were reviewed.
Results Among 22 patients with primary hypophysitis, 81.8% (18/22) had involvement of the posterior pituitary lobe. Two patients of the AH (2/3, 66.6%) and three patients of the PH (3/10, 30%) groups initially underwent surgical mass reduction. Five patients, including three of the PH (3/10, 33.3%) group and one from each of the AH (1/3, 33.3%) and INH (1/9, 11.1%) groups, initially received high-dose glucocorticoid treatment. Nearly all of the patients treated with surgery or high-dose steroid treatment (9/11, 82%) required continuous hormone replacement during the follow-up period. Twelve patients received no treatment for mass reduction due to the absence of acute symptoms and signs related to a compressive mass effect. Most of them (11/12, 92%) did not show disease progression, and three patients recovered partially from hormone deficiency.
Conclusion Deficits of the posterior pituitary were the most common features in our cases of primary hypophysitis. Pituitary endocrine defects responded less favorably to glucocorticoid treatment and surgery. In the absence of symptoms related to mass effect and with the mild defect of endocrine function, it may not require treatment to reduce mass except hormone replacement.
-
Citations
Citations to this article as recorded by- Secondary xanthogranulomatous hypophysitis mimicking a pituitary macroadenoma: a case report
Salma Salhi, Ibtissem Oueslati, Yasmine Mouelhi, Alia Zehani, Nidhameddine Kchir, Elyes Kamoun, Meriem Yazidi, Melika Chihaoui
Journal of International Medical Research.2024;[Epub] CrossRef - Glucocorticoid therapy as first-line treatment in primary hypophysitis: a systematic review and individual patient data meta-analysis
Brijesh Krishnappa, Ravikumar Shah, Saba Samad Memon, Chakra Diwaker, Anurag R Lila, Virendra A Patil, Nalini S Shah, Tushar R Bandgar
Endocrine Connections.2023;[Epub] CrossRef - Hypophysitis, the Growing Spectrum of a Rare Pituitary Disease
Fabienne Langlois, Elena V Varlamov, Maria Fleseriu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(1): 10. CrossRef - Outcomes of Initial Management Strategies in Patients With Autoimmune Lymphocytic Hypophysitis: A Systematic Review and Meta-analysis
Diane Donegan, Zeb Saeed, Danae A Delivanis, Mohammad Hassan Murad, Juergen Honegger, Felix Amereller, Seda Hanife Oguz, Dana Erickson, Irina Bancos
The Journal of Clinical Endocrinology & Metabolism.2022; 107(4): 1170. CrossRef - Early Pulse Glucocorticoid Therapy and Improved Hormonal Outcomes in Primary Hypophysitis
Brijesh Krishnappa, Ravikumar Shah, Vijaya Sarathi, Anurag Ranjan Lila, Manjeet Kaur Sehemby, Virendra A. Patil, Shilpa Sankhe, Nalini Shah, Tushar Bandgar
Neuroendocrinology.2022; 112(2): 186. CrossRef - Preoperative differentiation of hypophysitis and pituitary adenomas using a novel clinicoradiologic scoring system
Kyla Wright, Hyon Kim, Travis Hill, Matthew Lee, Cordelia Orillac, Nikita Mogar, Donato Pacione, Nidhi Agrawal
Pituitary.2022; 25(4): 602. CrossRef - Hypophysitis
Diane Donegan, Jürgen Honegger
Endocrine Practice.2022; 28(9): 901. CrossRef - Rare Case of a Disappearing Pituitary Adenoma During the Coronavirus Disease 2019 (COVID-19) Pandemic
David P. Bray, C. Arturo Solares, Nelson M. Oyesiku
World Neurosurgery.2021; 146: 148. CrossRef - Diabetes insipidus secondary to sellar/parasellar lesions
Anna Angelousi, Chrysoula Mytareli, Paraskevi Xekouki, Eva Kassi, Konstantinos Barkas, Ashley Grossman, Gregory Kaltsas
Journal of Neuroendocrinology.2021;[Epub] CrossRef - Clinical presentation and management of hypophysitis: An observational study of case series
Marouan Karrou, Salma Benyakhlef, Achwak Alla, Najoua Messaoudi, Asmae Oulad Amar, Siham Rouf, Imane Kamaoui, Noureddine Oulali, Faycal Moufid, Naima Abda, Hanane Latrech
Surgical Neurology International.2021; 12: 304. CrossRef - Clinical aspects of autoimmune hypothalamitis, a variant of autoimmune hypophysitis: Experience from one center
Qian Wei, Guoqing Yang, Zhaohui Lue, Jingtao Dou, Li Zang, Yijun Li, Jin Du, Weijun Gu, Yiming Mu
Journal of International Medical Research.2020; 48(3): 030006051988783. CrossRef - Primary and Ipilimumab-induced Hypophysitis: A Single-center Case Series
Paul Atkins, Ehud Ur
Endocrine Research.2020; 45(4): 246. CrossRef - Hypophysitis (Including IgG4 and Immunotherapy)
Anna Angelousi, Krystallenia Alexandraki, Marina Tsoli, Gregory Kaltsas, Eva Kassi
Neuroendocrinology.2020; 110(9-10): 822. CrossRef - Hypophysitis in the era of immune checkpoint inhibitors and immunoglobulin G4-related disease
Leen Wehbeh, Sama Alreddawi, Roberto Salvatori
Expert Review of Endocrinology & Metabolism.2019; 14(3): 167. CrossRef - Immune check point inhibitors-induced hypophysitis: a retrospective analysis of the French Pharmacovigilance database
Julie Garon-Czmil, Nadine Petitpain, Franck Rouby, Marion Sassier, Samy Babai, Mélissa Yéléhé-Okouma, Georges Weryha, Marc Klein, Pierre Gillet
Scientific Reports.2019;[Epub] CrossRef - Clinical Features, Magnetic Resonance Imaging, and Treatment Experience of 20 Patients with Lymphocytic Hypophysitis in a Single Center
Qiang Zhu, Ke Qian, Guijun Jia, Gang Lv, Jisheng Wang, Liyong Zhong, Shuqing Yu
World Neurosurgery.2019; 127: e22. CrossRef - Idiopathic granulomatous hypophysitis presenting with galactorrhea, headache, and nausea in a woman: a case report and review of the literature
Guive Sharifi, Mohammad Reza Mohajeri-Tehrani, Behrouz Navabakhsh, Bagher Larijani, Touraj Valeh
Journal of Medical Case Reports.2019;[Epub] CrossRef - Paciente de 31 años con polidipsia
A.R. Benavides Aramburu, M. Seguí Díaz
Medicina de Familia. SEMERGEN.2018; 44(2): e77. CrossRef - Primary hypophysitis and other autoimmune disorders of the sellar and suprasellar regions
Sriram Gubbi, Fady Hannah-Shmouni, Constantine A. Stratakis, Christian A. Koch
Reviews in Endocrine and Metabolic Disorders.2018; 19(4): 335. CrossRef - Primary lymphocytic hypophysitis: Clinical characteristics and treatment of 50 cases in a single centre in China over 18 years
Shuchang Wang, Linjie Wang, Yong Yao, Feng Feng, Hongbo Yang, Zhiyong Liang, Kan Deng, Hui You, Jian Sun, Bing Xing, Zimeng Jin, Renzhi Wang, Hui Pan, Huijuan Zhu
Clinical Endocrinology.2017; 87(2): 177. CrossRef - Clinical presentation and outcome of children with central diabetes insipidus associated with a self‐limited or transient pituitary stalk thickening, diagnosed as infundibuloneurohypophysitis
J. Schaefers, M. Cools, K. De Waele, I. Gies, V. Beauloye, P. Lysy, I. Francois, D. Beckers, J. De Schepper
Clinical Endocrinology.2017; 87(2): 171. CrossRef - Intrachiasmatic abscess caused by IgG4-related hypophysitis
Georgios F. Hadjigeorgiou, Eva Løbner Lund, Lars Poulsgaard, Ulla Feldt-Rasmussen, Åse Krogh Rasmussen, Marianne Wegener, Kåre Fugleholm
Acta Neurochirurgica.2017; 159(11): 2229. CrossRef - Granulomatous and lymphocytic hypophysitis – are they immunologically distinct?
Shilpa Rao, Anita Mahadevan, Tanmoy Maiti, Manish Ranjan, Shivayogi Durgad Shwetha, Arimappamagan Arivazhagan, Jitender Saini
APMIS.2016; 124(12): 1072. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Secondary xanthogranulomatous hypophysitis mimicking a pituitary macroadenoma: a case report

- Pancytopenia Associated with Hypopituitarism in an Acromegaly Patient: A Case Report and a Review of the Literature.
- Jung Hee Koh, Yong Jae Lee, Ji Hyun Kang, Bo Kwang Choi, Yun Kyung Jeon, Sang Soo Kim, Bo Hyun Kim, In Joo Kim
- Endocrinol Metab. 2012;27(4):308-313. Published online December 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.4.308
- 2,084 View
- 28 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - We present the case of a patient with acromegaly who had pancytopenia with hypopituitarism secondary to the excision of a pituitary macroadenoma and radiation therapy. A 28-year-old man presented with pancytopenia and serum electrolyte abnormalities. He was diagnosed with acromegaly and underwent surgery and gamma-knife radiotherapy for a pituitary macroadenoma at the age of 22 years. A recent brain magnetic resonance imaging showed an empty sella, and the basal hormonal profile demonstrated deficiencies of pituitary hormones except thyrotropin. As presenting pancytopenia, his bone marrow biopsy showed hypocellular marrow. The total number of hemocytes increased after hydrocortisone replacement. Hypopituitarism was a possible cause of pancytopenia, and glucocorticoids had crucial effects on converting pancytopenia to normal in this case.
-
Citations
Citations to this article as recorded by- A 24-Year-Old Male with Gigantism, Growth Hormone Deficiency, Suspected Clivus Chordoma, Primary Hypothyroidism, Hypogonadism and Pancytopenia
W.A. Arsana, M.I. Diah Pramudianti
INDONESIAN JOURNAL OF CLINICAL PATHOLOGY AND MEDICAL LABORATORY.2019; 26(2): 249. CrossRef - Hormones and the Bone Marrow: Panhypopituitarism and Pancytopenia in a Man with a Pituitary Adenoma
Dianna Lang, Jennifer S. Mead, David B. Sykes
Journal of General Internal Medicine.2015; 30(5): 692. CrossRef
- A 24-Year-Old Male with Gigantism, Growth Hormone Deficiency, Suspected Clivus Chordoma, Primary Hypothyroidism, Hypogonadism and Pancytopenia

- A Case of Sheehan's Syndrome with Pancytopenia.
- Hyun Suk Lee, Byung Woon Kwon, Jin Hyung Han, Hee Jin Kim
- Endocrinol Metab. 2012;27(1):54-58. Published online March 1, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.1.54
- 2,557 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Sheehan's syndrome is characterized by varying degrees of anterior pituitary dysfunction due to postpartum ischemic necrosis of the pituitary gland after massive bleeding. The spectrum of clinical presentation of Sheehan's syndrome is broad, with changes from nonspecific complaints, such as weakness, fatigue, and anemia, to severe pituitary insufficiency resulting in coma and death. Normochromic anemia is commonly associated with Sheehan's syndrome, but pancytopenia is rarely observed in patients with Sheehan's syndrome. We describe a 57-year-old woman with Sheehan's syndrome who presented with pancytopenia that was treated by hormone replacement with levothyroxine and glucocorticoid.

- A Case of Pituitary Abscess that was Difficult to Diagnose due to Repeated Symptomatic Responses to Every Corticosteroid Administration.
- Jin Sun Jang, Jae Seung Yun, Jung Ah Shin, Min Hee Kim, Dong Jun Lim, Jae Hyung Cho, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Ho Young Son, Yong Kil Hong
- Endocrinol Metab. 2011;26(1):72-77. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.72
- 1,615 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Pituitary abscess is a rare pathology, but it is a potentially life-threatening condition. Therefore, timely intervention, including antibiotics and an operation, can prevent the morbidity and mortality in such cases. A 31-year-old woman, who was 16 months after her second delivery, presented with intermittent headache for 3 months. Amenorrhea, polyuria and polydipsia were noticed and the endocrinological hormone studies were compatible with panhypopituitarism and diabetes insipidus. Pituitary MRI demonstrated a 2.3 cm sized cystic mass with an upper small nodular lesion. Her symptoms such as headache and fever were repeatedly improved whenever corticosteroid was administered, which led us to suspect the diagnosis of an inflammatory condition like lymphocytic hypophysitis. During the hormone replacement therapy, her cystic pituitary mass had grown and her symptoms progressively worsened for another two months. The patient underwent trans-sphenoidal exploration and she turned out to have a pituitary abscess. At the 3-month follow-up, amenorrhea was noticed and her residual function of the pituitary was tested by a combined pituitary stimulation test. The results were compatible with panhypopituitarism. She received levothyroxine 100 microg, prednisolone 5 mg and desmopressin spray and she is being observed at the out-patient clinic. The authors experienced a patient with primary pituitary abscess that was confirmed pathologically and we report on its clinical course with a literature review.

- A Case of Ectopic Neurohypophysis Presenting with Hypogonadism.
- In Woon Baek, Ji Hyun Kim, Guk Jin Lee, Kyoung Eun Lee, Hae Lim Lee, Hye Won Lee, Nam Yong Kim, Yon Kwon Ihn, Seung Hyun Ko, Seung Hwan Lee, Je Ho Han
- Endocrinol Metab. 2011;26(1):67-71. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.67
- 2,197 View
- 27 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pituitary stalk interruption and ectopic neurohypophysis seen on magnetic resonance Imaging (MRI) are often associated with either isolated growth hormone (GH) deficiency or combined anterior pituitary hormone deficiency, but their pathogenesis is not clear and the clinical data regarding these anatomical defect is limited. We experienced a 23-year-old male with the absence of secondary sexual characteristics and this was accompanied with pituitary stalk dysgenesis and ectopic neurohypophysis. He received growth hormone for a year when he was 12 years old due to his short stature. Sella MRI showed no visible pituitary stalk with minimal high signal change, suggesting ectopic neurohypophysis. The combined pituitary stimulation test revealed blunted responses of growth hormone, follicle stimulating hormone and luteinizing hormone. For the hypogonadotropic hypogonadism, the patient was given testosterone intramuscularly and he gradually developed secondary sexual characteristics. We concluded that the hypogonadism and growth hormone deficiency in this patient was caused by hypopituitarism due to pituitary stalk dysgenesis and ecopic nuerohypophysis.
-
Citations
Citations to this article as recorded by- MRI of ectopic posterior pituitary gland with dysgenesis of pituitary stalk in a patient with hypogonadotropic hypogonadism
Ashim Kumar Lahiri, Ramanivas Sundareyan, David Jenkins, Anjumara Nilak
Radiology Case Reports.2018; 13(4): 764. CrossRef - Hypothalamic Hypopituitarism Caused by Pituitary Stalk Dysgenesis
Seong-Ju Lee, Hye-Jin Yoon, A-Reum Cho, Yoo-Jin Um, Keun-Young Park, Dong-Mee Lim, Byung-Joon Kim
Korean Journal of Medicine.2013; 85(4): 420. CrossRef
- MRI of ectopic posterior pituitary gland with dysgenesis of pituitary stalk in a patient with hypogonadotropic hypogonadism

- Clinical Characteristics of Langerhans Cell Histiocytosis with Hypothalamo-Pituitary Involvement.
- Eun Shil Hong, Jung Hun Ohn, Jung Hee Kim, Yul Hwang-Bo, Jin Joo Kim, Jung Hee Kwon, Jung Won Lee, Se Youn Choi, Eun Kyung Lee, Sun Wook Cho, Chan Soo Shin, Kyong Soo Park, Hak Chul Jang, Bo Youn Cho, Hong Kyu Lee, Choong Ho Shin, Sei Won Yang, Seong Yeon Kim
- Endocrinol Metab. 2011;26(1):38-43. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.38
- 1,928 View
- 23 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Langerhans cell histiocytosis (LCH) is a rare disease that involves a clonal proliferation of Langerhans cells. LCH has a predilection for hypothalamo-pituitary axis (HPA) dysfunction, and this leads to diabetes insipidus (DI) and/or anterior pituitary dysfunction. Here, we describe the endocrine dysfunction and clinical characteristics of adult patients with LCH and we analyzed the differences between an adult-onset type and a childhood-onset type. METHODS: The data was obtained from a retrospective chart review of the patients with LCH that involved the HPA and who attended Seoul National University Hospital. The patients were classified into the adult-onset type (age at the time of diagnosis > or = 16) and the childhood-onset type (age at the time of diagnosis < or = 15). RESULTS: Ten patients (9 males and 1 female) were diagnosed with LCH involving the HPA. Five patients were classified as an adultonset type and the other five patients were classified as a childhood-onset type. The median follow-up duration was 6 (3-12) years for the adult-onset type and 16 (15-22) years for the childhood-onset type. All the patients presented with DI as the initial manifestation of HPA involvement. Four adult-onset patients and three childhood-onset patients had a multi-system disease. Panhypopituitarism developed in three adult-onset patients and in one childhood-onset patient. The pituitary lesion of the three adult-onset patients had spread to the brain during the follow-up duration. In contrast, the pituitary lesion of the other two adult-onset patients without panhypopituitarism and all the childhood-onset patients had not changed. CONCLUSION: DI was the initial presentation symptom of HPA involvement. Anterior pituitary hormone deficiency followed in some patients. Compared with the childhood-onset patients, the adult-onset patients were more likely to have panhypopituitarism and a poor prognosis. -
Citations
Citations to this article as recorded by- Pulmonary Langerhans Cell Histiocytosis in an Adult Male Presenting with Central Diabetes Insipidus and Diabetes Mellitus: A Case Report
Yeun Seoung Choi, Jung Soo Lim, Woocheol Kwon, Soon-Hee Jung, Il Hwan Park, Myoung Kyu Lee, Won Yeon Lee, Suk Joong Yong, Seok Jeong Lee, Ye-Ryung Jung, Jiwon Choi, Ji Sun Choi, Joon Taek Jeong, Jin Sae Yoo, Sang-Ha Kim
Tuberculosis and Respiratory Diseases.2015; 78(4): 463. CrossRef - Adult Multisystem Langerhans Cell Histiocytosis Presenting with Central Diabetes Insipidus Successfully Treated with Chemotherapy
Jung-Eun Choi, Hae Ri Lee, Jung Hun Ohn, Min Kyong Moon, Juri Park, Seong Jin Lee, Moon-Gi Choi, Hyung Joon Yoo, Jung Han Kim, Eun-Gyoung Hong
Endocrinology and Metabolism.2014; 29(3): 394. CrossRef
- Pulmonary Langerhans Cell Histiocytosis in an Adult Male Presenting with Central Diabetes Insipidus and Diabetes Mellitus: A Case Report

- Correlation between Pituitary Insufficiency and Magnetic Resonance Imaging Finding in Non-Functioning Pituitary Adenomas.
- Hyun Min Kim, Cheol Ryong Ku, Eun Young Lee, Woo Kyung Lee, Jung Soo Lim, Sena Hwang, Mi Jung Lee, Seung Ku Lee, Sun Ho Kim, Eun Jig Lee
- Endocrinol Metab. 2010;25(4):310-315. Published online December 1, 2010
- DOI: https://doi.org/10.3803/EnM.2010.25.4.310
- 2,018 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Non-functioning pituitary adenomas (NFPAs) are characterized by the absence of clinical and biochemical evidence of pituitary hormone hypersecretion, and these tumors constitute approximately one third of all the tumors of the anterior pituitary. Recently, hormonal deficiencies have gradually evolved to become the leading presenting signs and symptoms in patients with NFPAs. We investigated pituitary hormonal insufficiencies according to the magnetic resonance imaging (MRI) findings in patients with NFPA. METHODS: We evaluated the patients who were newly diagnosed with NFPA from 1997 through 2009. Among them, we analyzed 387 patients who were tested for their combined pituitary function and who underwent MRI. The severity of the hypopituitarism was determined by the number of deficient axes of the pituitary hormones. On the MRI study, the maximal diameter of the tumor, Hardy's classification, the thickness of the pituitary gland and the presence of stalk compression were evaluated. RESULTS: The mean age was 46.85 +/- 12.93 years (range: 15-86) and 186 patients (48.1%) were male. As assessed on MRI, the tumor diameter was 27.87 +/- 9.93 mm, the thickness of the normal pituitary gland was 1.42 +/- 2.07 mm and stalk compression was observed in 201 patients (51.9%). Hypopituitarism was observed in 333 patients (86.0%). Deficiency for each pituitary hormone was most severe in the patients with Hardy type IIIA. Hypopituitarism was severe in the older age patients (P = 0.001) and the patients with a bigger tumor size (P < 0.001) and the presence of stalk compression (P < 0.001). However, the patients who had a thicker pituitary gland showed less severe hypopituitarism (P < 0.001). Multivariate analysis showed that age, tumor diameter and the thickness of pituitary gland were important determinants for pituitary deficiency (P = 0.004, P < 0.001, P = 0.022, respectively). CONCLUSION: The results suggest that the hormonal deficiencies in patient with NFPA were correlated with the MRI findings, and especially the tumor diameter and preservation of the pituitary gland. -
Citations
Citations to this article as recorded by- Clinical Parameters to Distinguish Silent Corticotroph Adenomas from Other Nonfunctioning Pituitary Adenomas
Daham Kim, Cheol Ryong Ku, Se Hee Park, Ju Hyung Moon, Eui Hyun Kim, Sun Ho Kim, Eun Jig Lee
World Neurosurgery.2018; 115: e464. CrossRef
- Clinical Parameters to Distinguish Silent Corticotroph Adenomas from Other Nonfunctioning Pituitary Adenomas

- A Case of Insulin Autoimmune Syndrome in a Patient with Partial Hypopituitarism.
- Obin Kwon, Eun Young Park, Jin Young Yoon, Kwang Joon Kim, Yong ho Lee, Jae Won Hong, Eun Jig Lee, Sung Kil Lim, Hyun Chul Lee, Bong Soo Cha
- J Korean Endocr Soc. 2009;24(4):281-286. Published online December 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.4.281
- 1,715 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Insulin autoimmune syndrome is one of the rare causes of hypoglycemia, and characterized by hyperinsulinemic hypoglycemia associated with high titer of antibodies to endogenous insulin. We report a case of insulin autoimmune syndrome in a 57-year-old woman, presenting with mental changes due to hypoglycemia. She had no history of diabetes or insulin administration. The serum C-peptide level was 4.69 ng/mL and the insulin concentration was 229.55 microU/mL, when fasting plasma glucose level was 32 mg/dL. The insulin-to-glucose ratio was 7.17, while there was no radiologic evidence of insulinoma. The insulin antibody level was over 100 microU/mL, resulting in the diagnosis of insulin autoimmune syndrome. Hormonal studies revealed partial hypopituitarism and a lack of glucagon-response to hypoglycemia. Hypoglycemia disappeared with replacement of prednisolone with levothyroxine therapy. Under secretion of growth hormone and of adrenocorticotropic hormone due to hypopituitarism were associated with insufficient counterregulation to hypoglycemia. One should keep in mind that insulin autoimmune syndrome or hypopituitarism is one cause of hypoglycemia in patients with no history of diabetes, and corticosteroid can be an effective treatment for both diseases.


 KES
KES

 First
First Prev
Prev



